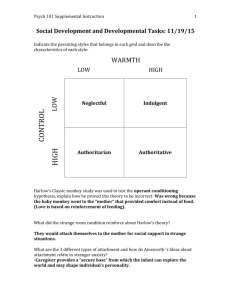
Downloaded - MH Child and Family Psychology | Lisa Marsland
advertisement

An Infant Mental Health Service: The Importance of the Early Years and Evidence-Based Practice. (This document gives detailed evidence for the importance of infant-parent psychotherapy, and related relationship-based interventions, as a therapeutic and preventative service for at-risk babies and their parents. Each section can stand alone; but helping small people seems to call for big explanations!) *** “Train up a child in the way he should go: and when he is old, he will not depart from it.” Proverbs, 22:6. Contents: Page number. 2. Introduction: why babies’ emotional needs have been sidelined. 4. In the beginning: evolution and early influences on the mind. 5. Neurobiological development: the significance of brain plasticity. 6. The importance of the attachment relationship: the first experiences can lead to resilience or disturbances. 11. The effect of trauma and neglect: the long-term consequences of disorganised attachment. 17. The roots of violence: how moral behaviour depends on early parenting. 18. Implications of the research data: a summary to this point. 19. Caregiving in jeopardy: a knowledge of risk-factors means help can be offered before a baby is traumatised, not after the event. 23. Early intervention services, an overview. 25. Economic benefits of very early intervention. 27. The components of an early intervention service: existing models of delivery. 32. Different approaches to infant mental health: evidence-based practice. 54. Conclusions. 56. References. 1 Introduction. Probably the most important period in everyone’s life is one they cannot remember. The first two or three years, the time before memory can be verbally tagged for later retrieval, set their stamp on all that comes after. This can be positive, as when a child gains the resource of being resilient in adversity so that later stressful events do not become a trauma; or negative, when a child’s early parenting has left a “basic fault” (Balint, 1968) because there was too great a discrepancy between the infant’s needs and the quality of caregiving that was available. This discrepancy easily gets lost or ignored. Karr-Morse and Wiley (1997:278) pinpoint three obstacles that seem to prevent us facing the unpleasant reality of an increasing number of babies. “The first of these may be grief, anger, or sadness from personal childhood experiences. Sometimes these are too painful to re-awaken. There may also be sadness and regret for the memories we may have inadvertently created for our own children. A third barrier to acting on this information is to feel overwhelmed by the depth and breadth of the problem.” It is hard to feel helpless, especially if we face the world from the point of view of these babies. Emde (2001:23) draws attention to why the plight of many babies can be hard to contemplate and so gets pushed aside. “It is often painful and difficult to recognise and address mental health problems in infants and young children.” Taking babies seriously opens Pandora’s Box. He lists four kinds of mental suffering that all would want to avoid and so might prefer not to think about. “Pain and distress from trauma, abuse, or loss of a caregiver; misery from neglect; suffering from cumulative stress; and suffering from lack of opportunity.” Distress can be relieved, but rescue or repair may be no more than myths created by wishful 2 thinking unless the help is immediate. The emotional environment of infancy, which from the baby’s point of view, consists of relationships with the parents, will be preserved on both a psychological and neurological level, for good or for ill. This can either be a disaster or a pathway to hope, as: “The essence of infant mental health work lies within the parent-child relationship.” (Solchany & Barnard, 2001:46) In many instances when an older child comes to the attention of specialist helping services provided by Education, Health or Social Services, it may appear difficult to differentiate between the effects of early experiences and reactions to current family dysfunction, which often predates the birth of the child anyway. Sometimes a simple change in parental understanding and attitude, or direct treatment of some form with the child, will enable the problem to become resolved. However, a significant population of children, whose effect and cost is out of all proportion to their number, cannot be helped in this way. It is just too late. This is why, as detailed below: “Early intervention for disadvantaged children and their families can be a sound economic investment.” (Barnett, 2000:605) Babies cannot wait; for if they have been adapting to an emotionally inimical setting for any length of time then the damage caused by inappropriate caregiving will not be undone by a change of circumstances, as is all too clear with many children who have been fostered or adopted, and so much more intensive and long-term interventions becomes necessary with a subsequently greater drain on resources. These are the children who do not make use of education, who disrupt the classroom and demand attention as they become either bullies or victims, who sometimes harm themselves as much as others. As teenagers they attract labels as an alternative to success: - conduct disorder, disruptive pupil, delinquent or disturbed, and mental health diagnostic categories get dropped around them out of desperation. 3 In the beginning. Babies are born ‘pre-programmed’ to seek out and adapt to the relationship that they have with their parents. This is a biological given, evolution’s answer to the prolonged period of helplessness in childhood and the need to adjust to the infinite possibilities created within a family in interaction with the wider culture. “Most of human knowledge cannot be anticipated in a species-specific genome … and thus brain development depends on genetically based avenues for incorporating experience into the developing brain.” (Shonkoff & Phillips, 2000:53) The human genetic package transmits initial flexibility, evolutionary success is adaptation to unforeseeable social diversity. Thus the genetic imperative for the baby is fit into what you find. “The child’s first relationship, the one with the mother, acts as a template, as it permanently moulds the individual’s capacities to enter into all later relationships. These early experiences shape the development of a unique personality, its adaptive capacities as well as vulnerabilities to and resistances against particular forms of future pathologies.” (Schore, 1994:1) Active, satisfying and reciprocal relationships with parents create the ‘taken for granted’ basis of a sense of identity, self-esteem, appreciation of others and self-control. “Human relationships, and the effects of relationships on relationships, are the building blocks of healthy development. From the moment of conception to the finality of death, intimate and caring relationships are the fundamental mediators of successful human adaptation.” (Shonkoff & Phillips, 2000:27) More than that, the quality and content of the baby’s relationship with his or her parents has a physical effect on the neurobiological structure of the child’s brain that will be enduring. 4 Neurobiological development. Research on brain development, which has re-written the textbooks over the last decade with the advent of new techniques for imaging the functioning brain, has shown that: “the infant’s transactions with the early socioemotional environment indelibly influence the evolution of brain structures responsible for the individual’s socioemotional functioning for the rest of the lifespan.” (Schore, 1994:540) KarrMorse and Wiley (1997:277), after an in-depth review of evidence from many different disciplines on the genesis of violent behaviour, return to the cellular level. “The strength and vulnerability of the human brain lie in its ability to shape itself to enable a particular human being to survive its environment. Our experiences, especially our earliest experiences, become biologically rooted in our brain structure and chemistry from the time of our gestation and most profoundly in the first month of life." (For a summary of recent research, see: Glaser, 2000; Balbernie, 2001.) The brain is at its most adaptable, or plastic, for the first two years after birth, during which time: “the primary caregiver acts as an external psychobiological regulator of the ‘experience-dependent’ growth of the infant’s nervous system. These early social events are imprinted into the neurobiological structures that are maturing during the brain growth spurt of the first two years of life, and therefore have far-reaching effects.” (Schore, 2001b:208). Thus: “From a basic biological perspective, the child’s neuronal system – the structure and functioning of the developing brain – is shaped by the parent’s more mature brain. This occurs within emotional communication.” (Siegal, 1999:278) The older the child becomes, then the harder it can be to ‘re-wire’ certain areas of the brain; which means that without intervention a child who has 5 experienced abuse or neglect as an infant will unwittingly continue with patterns of responses that are engraved in the mind, even if circumstances change. The importance of the attachment relationship. Attachment theory, developed by the British Psychiatrist and Psychoanalyst John Bowlby, has provided a framework for studies on both the immediate and long-term effects of early relationship experiences on the developing child. Attachment research has integrated the inner, psychological, world with the outer world of behaviour to demonstrate that: “the patterning or organization of attachment relationships during infancy is associated with characteristic processes of emotional regulation, social relatedness, access to autobiographical memory, and the development of selfreflection and narrative.” (Siegal, 1999:67) Attachment theory and a large body of research converge to agree that ‘an infant’s formation of an attachment to a caregiver is a key developmental task that influences not only the child’s representations of self and other, but also strategies for processing attachment-related thoughts and feelings… (and) may be related to risk for psychopathology or to psychological resilience in adulthood.’ (Dozier, Stovall-McLough and Albus, 2008:718) Following the creation by Ainsworth and colleagues (1978) of the Strange Situation Procedure, attachment behaviour was initially split into three observable categories. The majority of children (about 65%) demonstrate secure attachment, to be contrasted with anxious-avoidant, anxious-ambivalent and, a later conceptualisation, disorganised-disoriented (or controlling) patterns of attachment. The organised patterns of anxious attachment can be thought of as clusters of goal-directed activity 6 whose aim is to maintain the best available emotional and physical connection, as the child sees it, with the caregiver. ‘Each of the three patterns reflects a strategy for enlisting the caregiver in the service of alleviating stress. The secure infant explores freely and seeks contact with the attachment figure as necessary. The avoidant infant focuses on exploration, and monitors and maintains proximity to the attachment figure, but does not express attachment needs in order to avoid risking rejection. The resistant infant is preoccupied with the availability of an inconsistent caregiver, making repeated high-intensity demands to ensure that at least some of the latter elicit attention.’ (Goldberg, 2000:23) The different categories of attachment, once in place, demonstrate the dependant child’s ‘chosen’ method of affect regulation; this will have a big influence on internal and interpersonal processes. ‘Each attachment pattern reflects a different ecologically contingent strategy designed to solve adaptive problems posed by different rearing environments.’ (Simpson, 1999:125) Babies and toddlers, of course, have no means of making comparisons and so this is just the way the world of relationships and emotions goes and can be expected to carry on going. Secure attachment is a protective factor, conferring confidence and adaptability, although not a total guarantee of future mental health, and without this emotional resource neither child nor adult will feel free to make the most of their life’s possibilities. In later life secure children and adults can self-repair. An insecure child has too many anxieties that get in the way of investigating the world, so horizons stay safely near. Research makes it clear that: “In general, secure children show more concentrated exploration of novel stimuli and more focussed attention during tasks. Secure attachment provides the best-known psychological precondition for tensionfree playful exploration.” (Grossmann, et al., 1999:781) 7 By the time infants enter into their second year of life there are consistent observable differences in their behaviour that depend upon the level of security they have experienced in the relationship with their parents. Thompson (1999:274) gives a summary of decades of research to describe how: “securely attached children show greater enthusiasm, compliance, and positive affect (and less frustration and aggression) during shared tasks with their mother, as well as affective sharing and compliance during free play with their mothers. Securely attached infants tend to maintain more harmonious relations with parents in the second year.” Attachment provides the launch-pad, if it is firm and trustworthy then better the take-off and the more successful is the flight! This can be surprisingly long-lasting; as shown by a longitudinal study of high-risk infants where infant security was: “associated with the observed quality of participants’ romantic relationships in young adulthood.” (Roisman, Collins, Sroufe and Egeland, 2005) The three different categories of insecure, or anxious, attachment make the child increasingly vulnerable to life’s events; but apart from the most serious classification, insecure attachment by itself is not necessarily a disorder, although it can lead to one. Goldberg (2000:209) summarises how in the relevant research: “A very common finding is that the history of psychiatric patients is riddled with negative attachmentrelated experiences such as loss, abuse or conflict.” Insecure attachment is a risk factor that will interact with other risks present in the emotional and physical environment of the growing child; the level of attachment disturbance is equivalent to a level of vulnerability that is difficult to change without help. It is worth noting that a longitudinal study of high risk infants showed “substantial shifting towards insecurity 8 in late adolescence, particularly towards the dismissing classification.” (Weinfield, Whaley and Egeland, 2004:89) Conversely, early disorganised attachment was significantly related to late adolescent insecurity. Research shows how in adolescence insecurity is linked to conduct problems. (Allen, et al., 1997; Rosenstein and Horowitz, 1996) It is important to bear in mind that initial “good enough” attachment can be lost in the face of later adverse circumstances, initial secure attachment does not confer invulnerability. Children with problems related to insecure attachment begin to soak up statutory resources from early on when “externalising” behaviour (aggression, non-compliance, negative and immature behaviours, etc.) demands a response. (Speltz, et al., 1990) This is probably the largest group of children that Social Services, Special Education and the Child and Adolescent Mental Health Service are expected to deal with. “The social and economic costs of these types of disorders are staggering.” (Greenberg, et al., 1997:197) It has been estimated that: “In England the costs of mental ill-health are greater than the total costs of crime, and there is every reason to believe that this is also the case in the UK as a whole.” (Friedli and Parsonage, 2007:16) Studies have consistently demonstrated: “a high rate of insecure attachments among clinic-referred boys and their mothers.” (ibid, p. 216); the same applies to children in special educational provision (E. B. D. schools). A recent study compared emotionally disturbed children with two control groups from other school settings. Most of these children had been diagnosed as having attention deficit disorder, the rest as either conduct disorder or depression, with half the sample having more than one diagnosis. They were found to be: “strikingly different from their counterparts in regular classrooms in the extent to which they had experienced major disruptions in their 9 relationships with both mothers and fathers.” (Kobak et al., 2001:252) The different categories of insecure attachment predispose towards specific difficulties in later life. Avoidant attachment is a strategy often developed by an infant whose parents have discouraged overt signs of either affection or distress, and who do not readily offer sympathy or comfort. The conviction that others do not see you as someone worth loving, or even responding to, can lead to low self-esteem and subsequent aggression. Close relationships are avoided as the child gets older, and such adults may mask their insecurity by becoming addicted to work, acquisitions or achievement, or retreat behind obsessional and ritualistic behaviours. “Avoidant attachment would also seem to be a component of compulsive personality traits. At its extreme, the compulsive personality is the nightmare version of the uptight, authoritarian father who is determined to banish all emotions. He lives in a constricted world, his attentions narrowed to schedules, rules, and tidiness; and he is obsessed with trivia.” (Karen, 1994:391) The isolated child: “who also has an avoidant attachment history and perhaps certain genetic leanings, may, if things continue to go poorly, develop into a schizoid personality.” (ibid) Ambivalent, or resistant, attachment stems from the infant’s experience of inconsistent parenting when the child is never quite sure if his or her expressions of anxiety and distress will be suitably attended to. There is a lack of consistent nurturing and protection from the parent that makes it hard for the infant to feel that exploring the world is a safe option. Thus the child has a low threshold for distress, but no confidence that comfort will be forthcoming. When upset he or she tries to get close to the caregiver, but only to become angry and resist contact. This pattern can be 10 carried into adulthood and there reveals itself in relationship difficulties where there is either a withdrawal from others or a compulsion to be dependent. This is the hysterical personality who: “flees from intimacy, and, like the ambivalent child, she tends to be demanding or clingy, immature, and easily overwhelmed by her own emotions.” (Karen, 1994:392) A longitudinal study found that adolescents diagnosed with anxiety disorders were significantly more likely to have had resistant attachments with their parents when they were infants. (Warren, et al., 1997) Avoidant and ambivalent attachments may be anxious, but they have worked within the family and they are coherent and provide the child (and grown-up) with some sort of unconscious set of strategies for relating to others. These are internal working models of what once actually did, and is now expected to, occur in interpersonal exchanges. At least something is predictable, and a certain amount of meaning and satisfaction can be gained within mature relationships. This is not true for the most serious form of insecure attachment, labelled as disorganised and controlling, which is caused by pathological conditions and gives rise to pathological ways of relating. The effect of trauma and neglect. Disorganised attachment occurs when the parent either has so many unresolved emotional issues from their own past that they have no mental space left over for their baby or, graver, is a threat. The baby is biologically impelled to seek safety through closeness to the caregiver. When the parent is the source of fear (and this may be the result of neglect) the paradox cannot be resolved, there is no predictable solution and 11 the child’s faith in the world of relationships is demolished by their ‘scaregiver’ and he or she is left with no coherent means of relating to other people. “Abuse and neglect in the first years of life have a particularly pervasive impact. Pre-natal development and the first two years of life are the time when the genetic, organic, and neurochemical foundations for impulse control are being created. It is also the time when the capacity for rational thinking and sensitivity to other people are being rooted – or not – in the child’s personality.” (Karr-Morse & Wiley, 1997:45) The impact can show on a physical level almost immediately, as it has been found that the rate of disorganised attachment associated with failure to thrive is extremely high (Wood, et al., 2000). From a life-path perspective it has been clearly demonstrated that children who have suffered early neglect and abuse are far more likely to suffer from serious illnesses when they are adults, thus taking up an excessive and disproportional amount of health service resources, and they are also at a greatly increased risk of early death. (Felitti, et al., 1998) Disorganised attachment, frequently the result of maltreatment, becomes in itself a major risk factor that, in the ‘wrong’ circumstances, can disrupt many different areas of development. In a summary of research Moss et al. (1999:160) conclude that; “Disorganized/controlling attachment is predictive of the development of behavioural problems at preschool and school age in both high-risk and normal samples. Studies indicate that both externalizing and internalizing symptoms characterize the behaviour problems of disorganized school-aged children between 5 and 9 years of age. Although at preschool and early school age, it is primarily an aggressive, disruptive behaviour pattern that is associated with disorganization, anxieties and fears related to performance, abilities, and self-worth become more pronounced in middle 12 childhood." Disorganised attachment predominates in children referred to CAMHS. (Green, Stanley and Peters, 2007) Children who have been assessed as having disorganised attachment at 5-7 years have poorer skills at maths age 8 (Moss, et al. 1998) and show impaired formal operational skills and self-regulation at 17 years of age (Jacobson, et al. 1994). These two studies suggest that low self-esteem and lack of confidence in school mediated the poor performance, thus exacerbating the problems with self-esteem which is known to go with disorganised attachment anyway (Cassidy, 1988). A prospective study of a non-clinical population has examined the long-term consequences of different attachment patterns in children, differentiating between those with mother and father. (Verschueren and Marcoen, 1999; Verschueren, 2001) Children who had disorganised attachment with their fathers showed high levels of internalising behaviours when they were 5; and by 9 years of age (by teacher report) they had internalising problems, extremely poor social adjustment and low selfesteem. Children with disorganised maternal attachment (not the same ones) were six times more likely to be rejected by their peer group than average (more than twice the rate for avoidant children). If the child was unfortunate enough to have disorganised attachment with both parents they had both sets of difficulties. The problems associated with poor quality of attachment between child and parents begin to be visible almost straight away. “Children on trajectories towards serious externalizing problems are likely to have insecure, particularly disorganized, attachments in the first year.” (Shaw, et al., 1996:697) In addition, it is now accepted that: “severely compromised attachment histories are … associated with brain 13 organizations that are inefficient in regulating affective states and coping with stress, and therefore engender maladaptive infant mental health.” (Schore, 2001a:16) It is this ‘wired in’ compromised ability for self-control, a lack of coping mechanisms on a neurological level for dealing with internal and external stresses and frustrations, that confers a high vulnerability for later emotional, relational and mental health problems. The Minnasota Study has found that: - All types of abuse in the first years related to significant emotional problems in adolescence, and predicted the need for treatment. Out of all the children they had followed since birth 90% of the sample who had been maltreated qualified for at least 1 psychiatric diagnosis by age 17. It turned out that every form of abuse was related to delinquency, with a history of psychological unavailability being the strongest predictor. Neglect also predicted delinquency, although these children tended not to be angry or defiant. Witnessing parental violence correlated with externalising problems for boys at age 16 and internalising problems for girls. This was independent of other predictors such as abuse or neglect. (Sroufe, Egeland, Carlson and Collins, 2005) In addition, suicidal behaviour in adolescence is strongly influenced by unresolved-disorganised attachment, with girls being at highest risk. (Adam, et al. 1996) Child maltreatment does not spring from nowhere, and older children who come into the child protection system almost always have a history of grief going back to babyhood. The peak age for being murdered is under one. Early intervention, where vulnerable and over stressed parents can be identified and supported before the baby suffers, before their own emotionally barren and terrifying past becomes entangled in the relationship (and expectations) with their baby, is an essential preventative service if we want to avoid a steady growth in the number of referrals to adult mental health services. “Child abuse has a causal role in most mental health problems, including depression, anxiety disorders, PTSD, eating 14 disorders, substance abuse, personality disorders, and dissociative disorder. Psychiatric patients subjected to childhood sexual or physical abuse have earlier first admissions and longer and more frequent hospitalizations, spend longer time in seclusion, receive more medication, are more likely to self-mutilate, and have higher symptom severity.” (Read, Fink, Rudegeair, Felitti & Whitfield, 2008: 218) A recent summary of the research on the connections between early attachment experiences and adult psychopathology (Dozier, et al., 1999) looks at “attachment related circumstances” and their effect on later mental health problems. “Loss predicts multiple disorders, including depression, anxiety, and antisocial personality disorder … Depression is associated generally with the early loss of the mother. Major depression in particular … has been found to be related to permanent loss of a caregiver, whereas depression characterized by anger and other externalizing symptoms has been found to be related to separation. Anxiety appears to be associated more closely with threats of loss and instability than with permanent loss. Antisocial personality disorder is associated with loss through desertion, separation and divorce.” (p. 513) It appears that the quality of a child’s early parenting can put them on the pathway to different destinations. “Affective and anxiety disorders tend to be associated most frequently with parental rejection combined with loss. Antisocial personality disorders are most frequently associated with parental rejection, harsh discipline, and inadequate control. Eating disorders are associated with maternal rejection and overprotection combined with paternal neglect, and borderline personality disorder is associated most consistently with parental neglect.” (p. 514) Several longitudinal studies have demonstrated the link between difficult family 15 environments and their influence on the baby and the development of dissociative, borderline and conduct disorders in young adults (Lyons-Ruth, 2008). The early relationship between caregiver and baby will act as an external system for the child’s internal regulation of affect. Attachment is, in many ways, a measure of self-control. The growing infant, who began totally dependent on mother for soothing, stimulation and emotional regulation, gradually claims the ability to manage alone. In other words: “early development entails the gradual transition from extreme dependence on others to manage the world for us to acquiring the competencies needed to manage the world for oneself.” (Shonkoff & Phillips, 2000:121) Caregivers maintain the baby within comfortable, or acceptable, feeling states by intuitively recognising what their child is experiencing and how they can help to restore equilibrium. The parents’ ability to do this depends on their baby’s grandparents. In order to achieve such sensitivity the adult’s emotional awareness is a taken for granted resource that enables an automatic acknowledgement of need and a subsequent response. “A caretaker with a predisposition to see relationships in terms of mental contents permits the normal growth of the infant’s mental function. His or her mental state anticipated and acted on, the infant will be secure in attachment.” (Fonagy, et al., 1991:214) Comfort is not always an automatic presence; in dire circumstances it can seem unattainable. The secure child (and adult) has the psychological, and neurological, capacity to selfmodulate recognised affects. Responses to stressful or exciting circumstances can be thought about rather than acted out. “As a result of being exposed to the primary caregiver’s regulatory capacities, the infant’s expanding adaptive ability to evaluate 16 on a moment-to-moment basis stressful changes in the external environment, especially the social environment, allows him or her to begin to form coherent responses to cope with stressors.” (Schore, 2001a:14) However, when the infant has been exposed to relationships likely to engender disorganised, or controlling, attachment they have no choice about adapting to these emotional conditions, leading to: “brain organizations that are inefficient in regulating affective states and coping with stress.” (p. 16) An inability to think about others’ feelings coupled with an equal inability to control impulses will have serious long-term consequences. The roots of violence. Infants who have suffered adverse relationships become teenagers and adults who are grossly over-represented in the criminal justice system. This is not only a direct drain on resources, it also signifies a large population who are not in a position to contribute to the wider society (the same applies to those who never leave their dependency on mental health provision). Delinquent, antisocial and violent behaviour, frequently associated with no sense of either empathy or remorse, has been traced back to being on the receiving end of abuse and neglect during the first two years of life. (de Zulueta, 1993; Karr-Morse & Wiley, 1997) Even having a conscience cannot be taken for granted, as it has been demonstrated that this is cultivated by: “caregivers who are warm and provide clear expectations for child behaviour that are consistently reinforced.” (Shonkoff & Phillips, 2000:243) It has been found that attachment problems in adolescence predict later criminal behaviour (Allen, et al., 1996); and an attachment based study of prisoners with a 17 psychiatric disorder confirmed the hypothesis that: “ criminality arises in the context of weak bonding with individuals and social institutions and the relatively ready dismissal of attachment objects. Criminal behaviour may be seen as a socially maladaptive form of resolving trauma and abuse … Violent acts are committed in place of experienced anger concerning neglect, rejection and maltreatment. Committing antisocial acts is facilitated by a nonreflective stance regarding the victim.” (Fonagy, et al., 1997: 255) As de Zulueta (1993:76) puts it, violence: “is the manifestation of attachment behaviour gone wrong.” The ability to be mindful of another’s mind, and thus mind how you treat them, is derived from the infant’s relationship with their caregiver. Implications of the research data. If the early relationship between the baby and his or her parents is given the attention it deserves then this has two major implications. - Firstly, many later emotional and mental health problems can only be reworked in a similar fire as forged them. Longterm, intensive and (this time) thought-about relationships may be necessary to help those who carry the mental imprint of early trauma and neglect. For as long as the brain retains sufficient plasticity in the relevant areas then its neurochemical structure will continue to adapt to the effect of affect. Evidence suggests that psychotherapy: “probably initially changes the functional connections among neurones, and then later converts these functional changes into changes in the actual structure of the cerebral cortex itself.” (Vaughan, 1997:68) But less effort would have been called for when the mind was, by design, more readily adaptable. – Secondly, by recognising that the parent-infant relationship is the crucible for change and development, for good or ill, 18 we can look beyond the individuals to the wider conditions that impinge upon this relationship. Looking for reasons removes blame. Every parent always does the best they can for their baby within what is possible for them. A broader perspective, trying to understand rather than passing judgement, points to the importance of a catalogue of known risk factors. It is feasible to anticipate what sort of situation tends to lead to insecure attachment, and thus offer treatment or some other form of help before anything goes drastically wrong. That is, before responses get so ‘hard-wired’ into the brain that they become increasingly hard to change. Caregiving in jeopardy. There is a large body of research on risk factors, with general agreement on what these are and how they affect parenting. (e.g. Balbernie, 2002; Fonagy & Higgitt, 2000; Karr-Morse & Wiley, 1997; Osofsky & Thompson, 2000; Sameroff, 2000; Zeanah, et al., 1997) The parent-baby relationship is always located in a wider context, within which are found both risk and protective factors. These can harm the baby directly (e.g. pollution, unhealthy housing) but mostly are titrated into the relationship via their effects on the parents’ functioning, since they dictate the baby’s immediate experiences. Nurture and nature can no longer be regarded as discretely separate issues. “Genetic susceptibilities are activated and displayed in the context of environmental influences. Brain development is exquisitely tuned to environmental inputs that, in turn, shape its emerging architecture. The environment provided by the child’s first caregivers has profound effects on virtually every facet of early development, ranging from the 19 health and integrity of the baby at birth to the child’s readiness to start school at age 5.” (Shonkoff & Phillips, 2000:219) Some (but certainly not all) of the risk factors known to adversely affect the parent-baby relationship are: problems intrinsic to the baby, such as low birth weight or congenital abnormalities; a parent who lacks the ability to sensitively attune to the baby’s needs, who does not interact with their infant or maltreats him or her; one or both parents struggling with a mental health or addiction problem, or with a background of abuse, neglect or loss in their own childhood; inadequate income or sub-standard housing, family dysfunction and (extremely harmful) domestic violence; single teenage mother without support. (These examples from Landy, 2000:345; and see also Sameroff, 2000:12) So many factors external to the baby and parent can mess up their relationship that problems here can be taken as a sign that the child, without intervention, will grow up struggling with emotional harassment from many different directions. A working assumption that can direct both early and later intervention is that: “attachment disruption may be a marker or summary variable for a number of pathogenic factors in the child’s environment.” (Kobak et al., 2001:254) The baby has no comparisons, what is met is simply how the whole world is organised. You get born, you take your chance! “As a source of risk, the home may reflect an atmosphere of disorganization, neglect, or frank abuse. As a source of resilience and growth– promotion, it is characterized by regularized daily routines and both a physical and a psychological milieu that supports healthy child-caregiver interactions and rich opportunities for learning.” (Shonkoff & Phillips, 2000:345) 20 The research on risk factors means that babies who might be likely to have adverse developmental pathways through life, because of stresses in their initial relationship with their parents, can be identified early on. Even the unborn child cannot be assumed to be safe. The foetus can be directly harmed by a number of toxins (including the effects of stress on the mother) which can cause disability, regulatory disorders, attention difficulties or skill deficits; any one of which may make it hard for the neonate to settle into an attachment relationship. “Children born already impaired are more likely to be the brunt of destructive parenting behaviours and abuse.” (KarrMorse & Wiley, 1997:55) A major risk, the single biggest cause of cognitive delay in developed countries, is maternal alcohol consumption during pregnancy. It is now accepted that: “the teratogenic effects of alcohol are not limited to heavy chronic exposure, or to exposure during a specific time during the gestation period.” (Fitzgerald, et al., 2000:129) Over and above the effects of the drug on the embryo, a child born to parents with addiction problems may well develop attachment difficulties as addiction in any form flags up an attachment-related disorder, insofar as it gives the illusion of a ‘safe’ dependency where the object of desire is controllable. A vulnerable baby does not have to experience distress and damage that he or she cannot comprehend before help is offered. The greater the number of risk factors found in a family’s total ecology then the greater the need for immediate assistance. But sadly, the more a family is under stress then the harder it becomes to make full use of any help available. Only a relationship can change a relationship, but if you are ground down by inner and outer circumstances a new relationship is hard to contemplate. 21 Getting the first, prototypical, important relationship of anyone’s life more or less right is a necessity, not a luxury. This is the most sensible and economic time to put in therapeutic resources. And furthermore, unique to this stage of life, one can guarantee that the child both wants to co-operate and has not got stuck in the trap of gaining self-esteem from antisocial acts. This is society’s best chance to help itself. “The interactive process most protective against later violent behaviour begins in the first year after birth: the formation of a secure attachment relationship with a primary caregiver. Here in one relationship lies the foundation of three key protective factors that mitigate against later aggression: the learning of empathy or emotional attachment to others; the opportunity to learn control and balance feelings, especially those that can be destructive; and the opportunity to develop capacities for higher levels of cognitive processing.” (Karr-Morse & Wiley, 1997:184) The analysis of risk factors, which: “is an exercise in estimating probabilities, not finding causes” (Sameroff, 2000:28), shows clearly how the relationships within a family can be distorted by external pressures which need intervention on a social level as much (if not more) as their emotional consequences need help on a personal level. For instance, the single most important broad risk factor that predicts later maladjustment is poverty (Brooks-Gunn, et al., 2000; Halpern, 1993) since this amplifies and concentrates all the other risks. “Low income creates a particularly stressful context in which positive interactions with children are threatened, and punitive or otherwise negative relationships may result. The high prevalence of depression, attachment difficulties, and posttraumatic stress among mothers living in poverty serves to undermine their development of empathy, sensitivity, and responsiveness to their children, which can lead to diminished parenting behaviours 22 and thus decreased learning opportunities and poorer developmental outcomes.” (Shonkoff & Phillips, 2000:353) The effects of inadequate financial resources can be partially addressed in many instances, as can other adverse factors, but ultimately it takes individualised responsive care to change a pattern of caregiving. Early intervention services: an overview. The major review by the American National Research Council (part of the National Academy of Sciences) of many different lines of research carried out on the development of children, summarises a conservative core of replicated findings over thirty years of evaluating early intervention programmes. (Shonkoff & Phillips, 2000:342) To paraphrase slightly, and omitting their extensive references, these are as follows: Well-designed and successfully implemented interventions can enhance the shortterm performance of children living in poverty. Such interventions can promote significant short-term gains on standardised cognitive and social measures for young children with developmental delays or disabilities. Short-term impacts on the cognitive development of young children living in highrisk environments are greater when the intervention is goal-directed and childfocussed in comparison to generic family support programs. Measured, short-term impacts on the cognitive and social development of young children with developmental disabilities are greater when the intervention is more structured and focussed on the child-caregiver relationship. 23 Short-term I.Q. gains associated with high-quality preschool interventions for children living in poverty typically fade out during middle childhood, after the intervention has been completed; however, long-term benefits in higher academic achievement , lower rates of grade retention (repeating a year), and decreased referral for special education services have been replicated. Extended longitudinal investigations into the adolescent and adult years are relatively uncommon but provide documentation of differences between the intervention and control groups for economically disadvantaged children in high school graduation, income, welfare dependence, and criminal behaviour. Analyses of the economic costs and benefits of early childhood intervention for lowincome children have demonstrated medium- and long-term benefits to families as well as savings in public expenditure for special education, welfare assistance, and criminal justice. On the other hand, there appears to be a relative lack of evidence that wide-scale projects that broadly target a general population have much long-term effect. At the end of a review of American Federal and State interventions, such as Head Start, Farran (2000:525) finds it disheartening that: “A great deal of money was spent on programs that have not been shown to be more effective than doing nothing at all.” This is a reminder that families do not exist in isolation. Where a child appears to have a disadvantaged start in life the whole context of the baby-parent relationship needs to be taken into account. “Competence is the result of a complex interplay between children with a range of personalities, the variations in their families, and their economic, social, and community resources.” (Sameroff, 24 2000:9) There are a large number of therapeutic interventions that have been demonstrated to help the relationship between parent and infant, but results cannot be sustained in a vacuum. None of the programmes reviewed by Farran (2000:525): “made any difference to the income, housing conditions, or employment of the parents involved, despite the fact that the families were often chosen because they had extremely low incomes.” Exactly the same adverse influences that have impinged on the adult members of the family will probably continue to exert an effect on the child throughout his or her development, making specific predictions difficult unless wider issues (such as standards of education and employment prospects) are also tackled head on. “That is to say, significant medium- and long-term benefits of early childhood intervention may be viewed as a continuing developmental pathway that is contingent on a chain of positive effects that increase the probability of remaining on track.” (Shonkoff & Phillips, 2000:352) Perhaps it will not be possible to gauge the most important long-tern effect of early intervention until follow-up studies are carried out on these infants when they have become parents in turn. Economic benefits of very early intervention. There are a number of studies which have demonstrated the long-term cost benefits of helping vulnerable families provide the sort of emotional environment for their babies and toddlers that in general leads to secure attachment. Parenting is only meant to be ‘good enough’. For instance, the Perry Pre-school Highscope Programme has data spanning forty years, showing that for every $1 spent in setting up and running their pre-school nursery initiative in a high-risk area they find that almost $13 were saved in terms of later services not accessed when participants were followed up at age 40. 25 (High/Scope Perry Preschool Program, follow-up report in 2005, on line) Another longitudinal study, described below, known as the Elmira Home Visiting Project has shown that early specialised support for vulnerable first-time mothers had paid back its costs by four years. At a 15 year follow up the savings exceeded the costs of the program by a factor of four. (Olds et al, 1999) The Children’s Trust Fund in Michigan targets the prevention of maltreatment as: “Research shows that for every $1 spent on child abuse and neglect prevention, $7 will not be spent on publiclyfunded, crisis-oriented programming such as protective services, foster care, special education, and counseling with the exception of juvenile delinquency or adult incarceration” (www.michigan.gov/ctf/0,1607,7-196--232496--,00.html) The expense of not intervening is in the direct and indirect costs of such later antisocial behaviour as is associated with conduct disorder. It had been calculated that a young adult who eventually suffers social exclusion due to conduct problem will costs the country three and a half times more than someone with no problem; while conduct disorder will incur costs of ten times higher than having no problem. (Scott, Knapp, Henderson & Maughan, 2001) A conservative estimate (so it will grow year on year) is that preventing conduct disorders in those children who are most disturbed would save around £150,000 of lifetime costs for each individual; and promoting positive mental health in those children with moderate mental health would yield lifetime cost benefits to each of about £75,000. (Friedli and Parsonage, 2007) This analysis did not take into account the monetary implications the negative effects these children have upon others, such as all the disruption they cause in the classroom and the long-term effects of the violence they may inflict on other – not least future partners and children. Taking the above figures, the total value of the benefits of prevention in a 26 one-year cohort of children in the UK is £5.25 billion, and the value of promoting positive mental health comes to £23.625 billion. (Ibid, p. 20) A recent study by the New Economics Foundation (2009) for Action for Children, ‘Backing the Future’ shows the clear economic benefits of early intervention, clearly differentiating the different benefits to society, with the long-term savings being several magnitudes greater than the costs of setting up preventative services. Early intervention is still well worth the effort and allocation of resources even if the immediate success rate seems relatively low. “To be worth undertaking, the intervention thus needs a success rate of only one in 25 for conduct disorder and one in 55 for conduct problems. In other words, the potential benefits are so large relative to costs that intervention is worthwhile, even if its effectiveness is very limited.” (Friedli and Parsonage, 2007) Sinclair, writing for The Work Foundation and coming from a background in practical economics, is clear. “Dysfunctional parenting and children at risk represent classic market failure. This is where the government will get the greatest rate of returns for money invested.” (Sinclair, 2007:54) Simply preventing the occurrence of early child maltreatment or, if that has been impossible, offering prompt and appropriate treatment has a long-term benefit that is enormous in terms of services not called upon to intervene in the child’s future. A host of research from different disciplines converges to show how early trauma is ‘the frequent cause of physical and mental illness, school underachievement and failure, substance abuse, maltreatment, and criminal behavior.’ (Harris, Lieberman and Marans, 2007:393) The components of an early intervention service. 27 Two reviews examine what appears to be necessary for early intervention services for high-risk parents and babies if they are to meet the needs of this group (Zero to Three, 1998, 18 (4); Shonkoff & Phillips, 2000:360-367). The guiding principle of early intervention is that services need to be carefully tailored to their client population, there is no single answer. For instance, findings from a home visiting service for highrisk mothers and babies indicated: “that higher-risk mothers benefited more from a mental health curriculum than an educational curriculum whereas lower-risk mothers benefited more from the educational curriculum than the mental health curriculum.” (Berlin, et. al., 1998:13) There is a second and equally important principle that is at the heart of practical service delivery. Any intervention, regardless of technique or theory, is only as effective as the quality of the relationships that the infant mental health practitioners can build up with the families they become involved with. “New relational experiences in therapy are the core of the healing process. The presence of an authentic, empathic, and responsive connection between client and therapist can foster healing and the subsequent development of a sense of relational competence for the client, which entails the ability to bring about change, and the experience of feeling effective in connection. In mother-infant therapy, this sense of efficacy is transposed to the mother moving out of isolation and into a more reciprocal and satisfying relationship with her baby.” (Paris, Spielman and Bolton, 2009:305) Services can be roughly divided between those that are centre-based and those that are delivered in the home. “Center-based services are more likely than home-based programs to target children directly – especially in terms of their cognitive and language development.” (Berlin, et. al., 1998:7) Whereas: “Home-based services, which virtually always include the child’s principle caregiver, may be especially well- 28 suited to enhancing parents’ well-being and the child-parent relationship.” (ibid, p. 6) However, infant mental health work has to always be tailored to the setting and needs of the families involved so that, for instance, successful help can equally be given to high risk mothers and their babies within a prison (Baradon, et al., 2008). Whatever the setting, it is important that services are targeted appropriately, the aim of every provision should be clear. “For young children where development may be compromised by an impoverished, disorganized, or abusive environment … interventions that are tailored to specific needs have been shown to be more effective in producing desired child and family outcomes than services that provide generic advice and support.” (Shonkoff & Phillipps, 2000:360) Evidence also supports the principle that proactive programmes, those which are truly preventative, beginning either pre-natally or at birth, have the greatest and most sustained effect, “There is a strong indication that while gains made through proactive interventions are sustained, and even increased, over time those made through reactive interventions tend to fade” (MacLeod and Nelson, 2000:1141). Such services can be either universal or targeted on an individual basis. The earlier we intervene the better. The best results are attained with strength-based approaches that focus on parental empowerment and involvement. The UK Sure Start initiative has evolved into an early intervention that combines centre based provision with outreach work delivered to the surrounding community. Although the initial evaluation of the myriad of different Sure Start schemes was disappointing, this has changed with time. One reason is that the service delivery is now based in Children’s Centres and the first wave of families accessing these early interventions has been worked through and now help can be consistently on offer 29 from conception to pre-school age. Children’s Centres are perfectly placed to deliver ‘wrap around’ services ranging from specialist infant mental health teams to the full gamut of different parenting groups available. Studies comparing outcomes for children in Secure Start areas with those lacking this input have found that the former ‘showed better social development, exhibiting more positive social behaviour and greater independence/self regulation than their counterparts in non-Sure Start areas….Also, families in Sure Start areas reported using more child and familyrelated services than families in non-Sure Start areas.’ (Melhuish, Belsky and Barnes, 2010:160) Even if an intervention seems to fit the bill, there is no guarantee it will deliver results unless the service created is appropriately funded and staffed. There can be an “implementation gap” set up by: “the discrepancy between the intervention that program designers plan and the intervention that families receive.” (Barnard, 1998:23) This can lead to a lower than expected take-up of services. “The impact of quality has been shown to be particularly important for children from families who bear the burden of multiple risk-factors” (Shonkoff & Phillips, 2000:362). Everyone wants the best for their baby, but many have no choice about what is on offer. The intensity and duration of any intervention are obviously important, but as aspects of quality they are hard to measure. Few researchers have addressed these variables, as there are frequently ethical implications to conducting randomised experimental studies on a vulnerable, clinical, population. However, there are some suggestive data. It has been found that I.Q. scores measured at 36 months increased with the amount of times a child attended a day centre, the number of home visits and the frequency with 30 which parents attended relevant meetings. (Ramey, et al., 1992) Greater involvement with helping services, whether in the home or a centre, was also associated with higher ratings of the family home environment when the child was one year old, and higher I.Q. scores at age three. For proactive preventative interventions, “which measured child maltreatment as an outcome; effect sizes increased as the length of the intervention increased” (MacLeod and Nelson, 2000:1143). Mothers who actively participated in the Prenatal / Early Infancy Project for two years were less likely to abuse their children than those mothers who had only been engaged for nine months. And a fifteen years later follow-up showed an inverse relation between the amount of service received and a number of negative maternal outcomes, including child maltreatment, repeat pregnancy, welfare dependence, substance abuse and brushes with the law. (Olds, et al., 1997, Olds, 2006) Two studies of a home visiting service for infants in families living in poverty, where one used random assignment to set up a treatment and control group, found that weekly visits resulted in higher child development test scores than fortnightly visits, which in turn obtained higher scores than monthly visits. (Powell & Grantham-McGregor, 1989) It seems a truism to stress that quality of service provision is entirely dependent on the calibre of the staff. “Early intervention service providers carry out intensive and emotionally demanding work. Their personal characteristics – especially their ability to be emotionally available and empathic – and their training and work experience influence the ways in which they deliver services” (Berlin, et al., 1998:8). Infant mental health services demand a core of specialised knowledge and skills congruent with the wide range of risk factors and developmental issues that need to be considered. Good reflective supervision is essential to avoid the risk of defensive 31 avoidance, vicarious traumatisation and burnout. In many ways only a dedicated, specialised, well-functioning team can hope to move between such matters as discordant attachment relationships, adult mental health and substance abuse, and the problems forced upon a family by poverty. “In this context, the ultimate impact of any intervention is dependent upon both staff expertise and the quality and continuity of the personal relationship established between the service provider and the family that is being served” (Shonkoff & Phillips, 2000:365). Different approaches to infant mental health. It appears, then, that well-planned and well-funded services for babies and parents at risk can redirect a likely developmental pathway along a new, healthier direction. “Programs that combine child-focussed educational activities with explicit attention to parent-child interaction patterns and relationship building appear to have the greatest impacts” (Shonkoff & Phillips, 2000:379). Whereas: “services that are supported by more modest budgets and are based on generic support, often without a clear delineation of intervention strategies matched directly to measurable objectives, appear to be less effective for families facing significant risk.” (ibid) Early intervention can have a differing emphasis on two approaches: the first is prevention 32 (targeting a population, or a family, identified by risk factor analysis), and the second is treatment (working with referred cases where something has already gone amiss). This is a rather artificial divide, since in practice both goals are compatible with each other within a single programme; e.g. working with families at risk will inevitably reveal ‘hidden’ disturbances that need to be referred on to a more specialised therapeutic service. However, conceptualising early intervention services in this way does provide a framework for examining the results of projects that were set up with different aims and methods. Preventative services will usually be either centre- or home-based, just as most treatment options are either clinic- or home-based as well. (And many families will be able to make use of either site for different services.) An example of a centre-based early intervention/preventative service is the Carolina Abecedarian Project where high-risk children received intensive early education five days a week, beginning at six weeks and ending at five years. Two groups of similar babies were selected, all with mothers who had educational difficulties. The control group, who only received free milk and nappies, were all (except one) eventually assessed as being retarded or of borderline intelligence. In the intervention group all the children tested within the normal range of intelligence by age three; by age 15 they scored significantly higher in general knowledge, reading and mathematics, and only 24% (48% in the control group) needed special education services. (Campbell & Ramey, 1994 & 1995) Furthermore, (according to the project’s website) when the children reached 21 years of age 35% of the intervention group were at college, compared to 14% in the control group; and 65% were in employment compared to 50% in the other group. The children whose mothers had the lowest I.Q. appeared to gain the most from this 33 intervention, and those who had a follow-up programme into elementary school benefited further still. An exception to the home or centre quandary might be services for teenage mothers which can be established within a school setting where the additional provision of good quality childcare would ensure that the young women could finish their education as well. The ‘Chances for Children’ Teen Parent-Infant Project in New York has successfully implemented and, using a control group, evaluated such a programme. They provide individual, dyadic and play therapies along with parenting groups and support for the nursery staff. They have found that the young mothers they had worked with improved their interactions with their infants ‘in the areas of responsiveness, affective availability, and directiveness. In addition, infants in the treatment group were found to increase their interest in mother, respond more positively to physical contact, and improve their general emotional tone, which the comparison infants did not’ (Mayers, Hagar-Budny and Buckner, 2008:332). The same positive results were found in a subset of young mothers who remained depressed, showing that even then it is still possible to improve mother-infant interactions. Early intervention with high risk, very vulnerable, families needs to be a multi-agency concern; and the better different agencies work together then the more long-lasting and positive are the results for the infants in these families. A good example, which has been evaluated a number of different times (including focus groups with the mothers involved), is the Canadian initiative for helping families where there is maternal substance abuse. This is called ‘Breaking the Cycle’ (BTC), and was launched by seven partner organisations in 1995. “Positive results of the BTC approach include (a) enhanced birth and perinatal outcomes for infants of substance- 34 involved mothers who are engaged earlier in pregnancy, (b) enhanced developmental outcomes of children who are involved, (c) enhanced parenting confidence and competence, (d) enhanced treatment outcomes, and (e) decreased rates of separation of mothers and children” (Motz, Leslie and DeMarchi, 2007:20). The intervention focus is on the mother-infant relationship and involves a range of different programmes based on a single-access model which includes street access and home visiting. Most group-based parenting programmes (or classes) will of necessity be based in a Children’s Centre of some sort. The Mellow Parenting, and especially Mellow Babies for the under-ones, approach is designed specifically for families where there is a relationship problem with a small child, and has been particularly successful in helping mothers and infants improve the quality of their relationship. (Puckering, 2004) The greater majority of parenting skills classes are geared to, and are more useful for, those with older children; and it could be argued that there is an inherent difference of attitude and outlook between a group and a class, with the former being less intrinsically humiliating for the parents. Mellow Parenting and Babies is an intensive and containing day-long group experience extending over many weeks that engages with a high risk group of families where child protection issues are paramount, domestic violence is present, where the mother has conflictual relationships with her family of origin, is experiencing behavioural problems with her child and may be struggling with psychological difficulties of her own. This programme has consistently engaged hard-to-reach families and has demonstrated positive changes in mother-child interactions, children’s behavioural problems and their intellectual development. A pilot study that applied a slightly modified version 35 of Mellow Parenting to a group of mothers suffering from post-natal depression has had encouraging results. The depressed mood of the mothers changed significantly, observed positive interactions increased and negative reactions went down. ‘The Mellow babies group intervention can improve both the mental health of women with postnatal depression and their interaction with their babies. (Puckering, 2009:161) The immediate advantage of this group approach is that each mother who attends immediately feels less isolated and guilty that she alone finds parenting a challenge. Another, perhaps more technophile, group approach that has been consistently able to improve the quality of the relationship between parents and their small children is the “Circle of Security” intervention, delivered as part of an Early Head Start project. This method carefully reviews with parents the video recordings of the Strange Situation procedure which each member has done with their child as part of this group-based programme. One of the goals of this method is to teach a user friendly version of attachment theory to the parents, and this can be based upon what all have observed in the replays of the Strange Situation procedures. This clinical service has been based firmly on a combination of attachment and object relations theory. “The underlying structure of the COS protocol consists of providing a secure base from which caregivers can both learn about the attachment needs of their children and explore their own internal obstacles to meeting those needs” (Cooper, et al. 2005:146). Initial outcomes appear to be promising; and this programme is currently under evaluation in a number of different sites. Away from a centre and into the home, a 20 year research project following the outcome of the Nurse Home Visitation Program is a good example of a preventative 36 intervention targeting an at risk population in the community. However, the families chosen were very limited, and the help was only offered to low income unmarried first time mothers; this would be ethically inappropriate within the context of the universal system of NHS provision, and so generalising the exact model to the UK setting is not entirely valid. However, as the NHS is being dismantled and becoming a collection of isolated franchises, this objection does not hold much water. The Nurse Home Visitation Program involved two randomised trials (in Elmira, New York, and Memphis, Tennessee), plus one other which is still in progress (in Denver). The investigators (Olds, et al., 1999:44) have concluded that: “The program benefits the neediest families (low income unmarried mothers) but provides little benefit to the wider population. Among low-income unmarried women, the program helps reduce rates of childhood injuries and ingestions that may be associated with child abuse and neglect, and helps mothers defer subsequent pregnancies and move into the workforce. Long-term follow-up of families in Elmira indicates that nurse-visited mothers were less likely to abuse or neglect their children or to have rapid successive pregnancies. Having fewer children enabled women to find work, become economically self-sufficient, and eventually avoid substance abuse and criminal behaviour. The children benefited too. By the time the children were 15 years of age, compared with the control group, they had fewer arrests and convictions, smoked and drank less, and had fewer sexual partners.” The home visiting began before birth and: “Compared with counterparts randomly assigned to receive comparison services, women who were nurse-visited experienced greater informal and formal social support, smoked fewer cigarettes, had better diets, and exhibited fewer kidney infections by the end of pregnancy.” (p.45) Four years after their children had been born the cost of the programme was less than the savings that had been made. This 37 manualised intervention: “explicitly promoted sensitive, responsive, and engaged caregiving in the early years of a child’s life.” (p.48) It was found that the biggest obstacle to benefiting from the service was the presence of domestic violence, with treatment effect diminishing as the level of violence increased. (Eckenrode, et al., 2000) This strength-based programme of intervention has been re-named the NurseFamily Partnership and rolled out in the U. K. where it is already showing positive gains for some vulnerable families struggling with a gamut of adverse experiences. (Rowe, 2009) Another home-based programme that worked with high risk adolescent and nonadolescent mothers evaluated results after six months of teaching parenting skills and the basics of child development while also making a link with local community resources. (Culp, et al. 1998) It was shown that these mothers significantly improved their knowledge of the taught subjects and their empathic responsiveness, also there was more involvement with the community and home safety was enhanced as well. The same approach (and curriculum) was applied again to an intervention group of 204 and a control group of 150 first-time mothers. (Culp, et al., 2004) Compared to the control group the intervention mothers showed the same gains as before, and also demonstrated a better understanding of non-corporal punishment along with behaviours that were more accepting and respectful of their infants. The equivalent professionals in the UK are Health Visitors, who have the enormous advantage over home visitors in America as they are universal, ‘invisible’ and nonstigmatising. It is literally vital that this invaluable service remains taken for granted. Once Health Visitors chuck some of the check lists they become the most important 38 adult mental health resource we have, the only problem being that the results of their work take a couple of decades to show up! The Solihull Approach has shown that Health Visitors who are trained in this form of reflective practice are able to work more effectively with children with less complex sleeping, feeding, toileting and behavioural difficulties and so prevent the need to refer them to CAMHS. (Douglas and Ginty, 2001) Health visitors and others trained in this approach consider that it improves perception and practice; and for the families involved there is a significant reduction in the severity of presenting difficulties, a reduction inparental anxiety and improvements in child behaviour. (summarised in Douglas and Rheeston, 2009.) It is also a methodology that appears to improve the ability to identify and help resolve minor problems in young children. (Milford, Kleve, Lea and Greenwood, 2006) A study based on a different but compatible approach where high risk families study were given an 18 month programme of weekly health visitor contact, using the Family Partnership Model (Davis, Day and Bidmead, 2002), suggests that “this intensive home-visiting programme may improve parenting in vulnerable families and increase identification of abuse and neglect in infancy.” (Barlow, et al., 2007:232) This model stresses the interpersonal skills and personal characteristics needed in order to work in a relationship based way with vulnerable families, since ‘the process of helping, including the development of the working relationship, is determined by what both the helper and parents bring to the interaction.’(Davis, 2009:69) A bridge to a purely treatment-based programme is provided by the relationship-based intervention for very high risk mothers set up in Los Angeles. This involved a randomised trial to create a similar comparison group who were only given paediatric appointments. These were all mothers who almost invariably would have come to the 39 attention of an infant mental health service, had one been available. The project workers were all mental health professionals with experience in child development and the family systems approach. The primary goal of the intervention was: “to offer the mother the experience of a stable trustworthy relationship that conveys understanding of her situation, and that promotes her sense of self-efficacy through a variety of specific interventions.” (Heinicke, et al., 1999:356) When compared with the control group: “The mothers became more responsive to the needs of their infants and more effectively encouraged their autonomy and task involvement. Moreover, the children in the intervention as opposed to non-intervention group were more secure, autonomous, and task involved on a variety of indices at 12 months.” (p. 371) The two groups were compared again when the children were two years old, by which time: “the mothers experiencing the intervention, in comparison with those that did not, also used more appropriate forms of control, and their children responded more positively to these controls. Mothers who did not experience the help of the intervention had significantly more difficulty controlling their child if it was a boy as opposed to a girl. They used the least appropriate methods of control and the boys responded more negatively to these controls.” (Heinicke, et al., 2001:458) A similar clinical-type intervention was carried out in Holland, the difference being that the risk factor resided in the infant, not in the surrounding family. The aim of the programme was to help mothers with infants who demonstrated an irritable temperament, since there is evidence that negative emotionality in babies leads on to later behavioural problems. Mothers were helped to respond more to both positive and negative emotions in their child, and at the same time encouraged to show less intrusive behaviour and detached lack of involvement. The quality of attachment 40 between parent and child appears to be enhanced by the parent’s ability and willingness to be sensitively responsive to their child. This was confirmed by the finding that: “more toddlers whose mothers participated in the intervention were securely attached than there were securely attached control group dyads.” (van den Boom, 1995:1809) At age two years, the mothers in the intervention group still demonstrated a greater responsiveness and involvement with their toddlers. And at three years both parents were more attuned to their child than those in the control group. “Intervention children continued to be more secure in their relationship with their mother, exhibited less behaviour problems, and were better able to maintain a positive relationship with the peer than the control group children.” (p. 1811) Helping parents respond in a more sensitive, or thoughtful, way to their infants promotes secure attachment. Depressed mothers are another high-risk group, as when the condition is severe it will interfere with the ability to tune into their baby’s signals and provide a sensitive and emotionally nurturing caregiving environment. Post-natal depression is linked to an increase in insecure attachment in toddlers, behavioural disturbance at home, less creative play and greater levels of disturbed or disruptive behaviour at primary school, poor peer relationships, and a decrease in self-control with an increase in aggression. (Cummings & Davies, 1994; Murray, 1997; Sinclair & Murray, 1998; Murray et al., 1999; Zeanah et al., 1997) Direct psychotherapy with depressed mothers has been shown to increase their capacity to recognise emotional expressions, including negative ones, and be more accurate in affective language communication. (Free, et al., 1996) Although this could be expected to improve the quality of attachment, this was not measured. However, another study that compared the effect of toddler-parent 41 psychotherapy between two, randomly assigned, groups of mothers with a major depressive disorder found that attachment was improved by the end of treatment. The two groups were further compared with another where the mothers had no mental health problems. “Toddlers of depressed mothers who received TPP evidenced rates of secure attachment that were no different from those of the non-depressed control group following the conclusion of this intervention.” (Cicchetti, et al., 1999:58) These were mothers with a relatively high level of income, education and family support who may well have been: “better able to utilize an insight-oriented mode of therapy than women confronted with a multitude of daily living challenges.” (p. 59). The authors of the study go on to speculate that: “as mothers become freed from the ‘ghosts from their pasts’ their internal working models became more positive and they were increasingly able to focus on the present, including their relationship with their child.” As a contrast, another approach to infant mental health intervention is provided by Interaction Guidance, which does not rely on insight to bring about change in the parent-baby relationship. This technique uses video feedback in order to encourage positive aspects of caregiver-infant interaction, helping parents: “in gaining enjoyment from their child and in developing an understanding of their child’s behaviour and development through interactive play experience.” (McDonough, 1993:414) This form of treatment was specifically tailored to reach families overburdened with multiple risks, and probably exemplifies the strength-based philosophy intrinsic to all infant mental health therapy more than any other approach. (McDonough, 2004). It does not explicitly focus on exploring the caregiver’s internal representational world of feelings and memories, although such material will be 42 addressed if it arises during the course of work. “This nonintrusive method of family treatment has proven to be especially successful for infants with failure to thrive, regulation disorders, and organic problems. Parents who are either resistant to participating in other forms of psychotherapy, or young, inexperienced, or cognitively limited respond positively to this treatment approach.” (McDonough, 1993:414) Interaction Guidance has also been successfully used to improve sensitivity and decrease the amount of disrupted communication between mothers and babies with feeding problems (Benoit et al., 2001); and a slightly modified version has been shown to help mothers with postnatal depression re-connect with their babies (Vik and Braten, 2009). This technique has been shown to bring about surprisingly rapid positive changes in disruptive caregiving behaviour, and this was measurable after the first session. (Madigan, Hawkins, Goldberg and Benoit, 2006) Video feedback of mothers and infants using a split screen technique, so that both faces can be viewed simultaneously while they play together, has also been shown to be effective in a brief treatment intervention that combines a psychoanalytic approach with an in-depth analysis of immediate interactions. (Beebe, 2003) Microanalysis of the recorded intercommunication within the excerpt of play reveals patterns of affect regulation that can inform a psychodynamic weaving together of the presenting difficulties, the observed behaviour of the dyad and the parent’s own early history. The technique of Interaction Guidance, with its use of video recordings to emphasise responsive and pleasurable mother-infant interactions, can be either clinic- or homebased; and it is sometimes used in conjunction with, rather than as an alternative to, more psychodynamic methods of treatment. A meta-analysis of early, attachmentbased, interventions suggests that disorganised attachment is most successfully 43 addressed by using sensitivity-focussed feedback. (Bakermans-Kranenburg, van Ijzendoorn and Juffer, 2005) Attachment-based video feedback was the intervention of choice in a study that used a randomised control group and targeted high risk families in order to prevent externalising problems in pre-school children. The children were aged 7 to 10 months when the treatment took place, and video was used, in their words, to promote positive parenting. There were two post-intervention tests at one month after, and then at age 40 months; and compared with the control group those in the trial had less preschool clinical externalising and total behavioural problems. (Velderman, et al., 2006) The evidence-based clinical work of this group along with its background in research (at Leiden University) has led to a successful programme to enhance parental sensitivity called ‘Video-feedback Intervention to Promote Positive Parenting’, or VIPP. (Juffer, Bakermans-Kranenburg and van IJzendoorn, 2007) This is a focussed and relatively short-term intervention with a number of slight variations, and it has been applied to adopted infants as well as babies of mothers with an eating disorder and mothers coping with a baby suffering from skin disorders. This strategy has been subject to more RCTs than you can shake a stick at! Video feedback, in combination with infant-parent psychotherapy, has also been used successfully to treat mothers suffering from PTSD following a history of violence-related trauma. (Schechter, 2004; Schechter, et al., 2006) It was found that the baby’s felt-to-be-intolerable distress, or current domestic violence, would trigger past traumatic memories for the mother, which then became confused with her current perception of the child. This intervention, over only thee visits, was able to significantly reduce the degree of negativity and of distortion of maternal attributions. 44 An example of how different strategies and methods can be applied is a childguidance clinic in Stockholm that uses both Interaction Guidance and infant-parent psychotherapy to help mothers and babies, with the additional provision of three long group sessions each week. They have carried out an in-depth follow-up evaluation of their work. Out of ten randomly chosen mother-infant pairs that were looked at only one had not made considerable progress during treatment. (Karlsson & Skagerberg, 1999) A combination of intervention methods appeared to achieve the most gains. Similarly, in the U.K the Sunderland Project, where Health Visitors were trained in the use of Patricia Crittenden’s “Care Index” and how to apply this to brief video recordings of mother-baby play, a multi-disciplinary mixed intervention strategy has clearly been shown to achieve measurable improvements in a high-risk population. Svanberg, (2005) concludes that: “The process of video-feedback and the support of the health visitor, who in his/her turn was supported and supervise by the parentinfant psychologists, enabled these parents to increase their own sensitivity sufficiently to support their child’s development towards a secure attachment and a more resilient future.” This approach roughly doubled the proportion of secure attachment in the intervention group where the mothers’ sensitivity and the infants’ cooperativeness increased significantly compared with a control group receiving routine care. (summarised in Svanberg, 2009) Unfortunately, in spite of the fact that a careful evaluation of the Sunderland Infant Programme has demonstrated clear and considerable long-term savings to health and social services (more than the costs), it has been closed down. A research project in Geneva has compared the results achieved by brief insight oriented, infant-parent psychotherapy with those attained by the more behaviourist 45 method of video feedback using Interaction Guidance. In the process, both forms of intervention were demonstrated to bring about appreciable, positive, changes in the mother-infant relationship. Since the study was carried out on families who had been referred to a child guidance clinic it was felt to be unethical to have a control group, although comparisons could be made with a non-clinical but otherwise matched sample. The results of both forms of treatment were evaluated, and: “marked symptom relief was observed in several areas, with the greatest improvements in sleeping, feeding and digestion (i.e. symptoms affecting physiological functions).” (Robert-Tissot, et al., 1996:105) In general, mothers became less intrusive and infants more co-operative, with maternal sensitivity to the baby’s signals increasing after treatment. “The results of the study indicate that brief mother-infant psychotherapies were effective in treating cases consulting for early functional disorders.” (p. 108) The only differences between the two approaches were that Interaction Guidance brought about more change in mothers’ sensitivity, while psychodynamic therapy had a greater impact on maternal self-esteem. It could be argued that the two different approaches of Interaction Guidance and infant-parent psychotherapy were in fact identical in task, and each improved parental ‘reflective function’. “A caretaker with a predisposition to see relationships in terms of mental content permits the normal growth of the infant’s mental function. His or her mental state anticipated and acted on, the infant will be secure in attachment.” (Fonagy, Steele, Steele, Moran and Higgitt, 1991:214). Recent research demonstrates that: “negative maternal caregiving behaviour is inversely correlated with maternal reflective functioning. (Grienenberger, Kelly and Slade, 2005:304) A gain in reflective function may lie behind all successful interventions that aim to improve the 46 sensitive responsiveness that is seen to be the basis of secure attachment. It has been demonstrated that: “maternal reflective function, measured at 10 months, is likewise linked to infant attachment security measured at 14 months using the Strange Situation.” (Slade, et al. 2005:293) A study examining reflectivity, mind-mindedness and behaviour in parents concluded that ‘directing attention towards supporting the mother’s capacity to effectively mentalize is likely to hold positive consequences for both her mental experiences of the child and the relationship as well as for her parenting behaviour during interaction.’ (Rosenblum, McDonough, Sameroff and Muzic, 2008:374) A research project showed that mothers of pre-school children with behavioural and emotional difficulties who participated in a clinical intervention that increased their insightfulness had children whose problems decreased; whereas mothers who did not gain from this had children whose behaviour problems increased. (Oppenheim, Goldsmith and Koren-Karie, 2004) A service for vulnerable families in New Haven, Connecticutt, is based on the principle of enhancing reflective functioning. This is a weekly home-visiting intervention called the Minding the Baby Program, and is focussed on the mother-infant dyad. A preliminary evaluation (Slade, Sadler and Mayes, 2005) indicates a marked gain in maternal reflective function in relation to the spectrum of their child’s developmental domains, and (using the Strange Situation) no children with disorganised attachment. For the mothers, the trend is towards lower levels of depression and post-traumatic stress symptoms along with higher levels of self-efficacy. In psychodynamic infant-parent psychotherapy the ‘patient’ is the relationship between baby and caregiver. It is to be expected that this approach would directly affect maternal self-esteem, since emotional difficulties from past relationships are 47 addressed within the context of a new relationship which is secure enough to both withstand and encourage exploration. “The quality of the relationship between therapist and parent is perhaps the more crucial in infant-parent psychotherapy than in any other form of treatment, because it is intended to be a mutative factor in the parent’s relationship with his or her child. “ (Lieberman & Pawl, 1993:430) In a study designed to evaluate the effectiveness of infant-parent psychotherapy, which compared an intervention group of mothers and infants with a similar control group, it was found that: “Mothers who formed a strong positive relationship with the intervener tended to be more empathic to their infants at outcome, and their children in turn tended to show less avoidance on reunion.” (p.434) However, the most important treatment variable turned out to be the mother’s ability: “to use infantparent psychotherapy to explore her feelings towards herself and toward her child.” (ibid) The two randomly assigned groups of mother-infant dyads where the child had been assessed as demonstrating insecure attachment were further compared with a second control group of securely attached infants and their mothers in order to examine outcomes. Evaluation took place when the child was two years old, after one year of treatment. “The intervention group performed significantly better than the anxious controls in the outcome measures and was essentially indistinguishable from the control group.” (p. 440) Those mothers who became most engaged in the therapeutic process became more actively attuned to their children, who in turn: “showed less anger and avoidance, more security of attachment, and more reciprocal partnership in the negotiation of mother-child conflict.” (p. 441) Again, it is relationships that change relationships. This intervention evolved into an intervention for three to five year olds traumatised by domestic abuse; and in a randomised clinical trial these children ‘improved significantly more than children receiving case 48 management plus treatment as usual in the community, both in decreased total behavioural problems and decreased PTSD symptoms.’ (Lieberman, Van Horn and Ippen, 2005:1246) These ‘improvements in children’s behavior problems and maternal symptoms as the result of treatment with child parent psychotherapy continue to be evident 6 months after the termination of treatment when compared to the control group.’ (Lieberman, Ippen and Van Horn, 2006:916) The methodology of this approach has been covered in detail in a recent book (Lieberman and Van Horn, 2008), and it has been successfully applied to situations of domestic violence in the perinatal period (Lieberman, Diaz and Van Horn, 2009). Parent infant psychotherapy was the main therapeutic modality applied to improve the relationship between mother and child in high risk families in the Florida Infant Mental Health Pilot Programme. This intervention targeted families with infants at risk of abuse and neglect who were likely to be removed from their parents or where this had actually occurred. There was no control group; and given that the project was funded by the legislature this would not have been ethical. Fifty nine percent of the programmes participants were court-ordered to participate, and many had already a record of maltreating their children. The results are impressive because of the wide range of family arrangements that fell within the scheme, which was thus less “choosy” and far more clinically realistic than many other research projects. At the end of this pilot study ‘there were no further reports of abuse or neglect during the treatment period and up to post-assessment for participants. There was a major reduction in reports of child abuse and neglect…from 97% of children prior to treatment to none of the children completing treatment during the first three years of the pilot project… (Also), the health and developmental status of children improved.’ 49 (Osofsky, et al. 2007:273) In addition there was a reduction of depressive symptoms in the caregivers along with a measured and reported improvement in the parent-child relationship. But a lot of effort went into these achievements, as should be expected for high risk families, and it was estimated that behind every hour of treatment were another ten spent on efforts to engage the family. The Parent Infant Psychotherapy (PIP) clinic at the Anna Freud Centre has a therapeutic focus on the parent-infant relationship as observed in the mutually influencing interactions in the sessions. (Baradon, et al. 2005) Here too, video feedback is an essential part of the process. One aim of parent-infant psychotherapy is to interrupt the generational continuity of unhelpful patterns of parenting and, ay the same time, to encourage the establishment of a secure attachment relationship for the child. A research project at the Anna Freud Centre, in a pilot study, evaluated outcomes using a range of psychometric tools. The majority of parents felt that their child’s development had been better than expected. Little more than 10-15% had significant concerns about the child at follow up. Less than one in twenty experienced a worsening. On both intellectual and motor development, as measured with the Bayley assessment of development, referred families had infants seven points behind the average. By six months they were indistinguishable from the average, and this improvement had increased slightly at follow-up. Another, final, example of a well-researched, intervention for parents and infants is the technique of “Watch, Wait and Wonder” used in the Toronto Infant-Parent Program. In this form of infant-parent psychotherapy the parent is encouraged to be 50 more directly involved with their child by engaging in playful interaction that follows the lead of the child. The parent is then invited to explore the feelings and thoughts that were evoked by what he or she observed and experienced in the preceding play session. This mode of treatment also appears to be a positive experience with good outcomes for mothers struggling with borderline personality disorder (Newman and Stevenson, 2008). Allowing the child to be spontaneous can be hard for a parent haunted by “ghosts in the nursery”, especially when these are revenants of past abuse; and a defensive infant, who is more used to complying to the pattern of available caregiving in order to extract the maximum available sense of felt-security, can be equally stumped. The research project set out to compare the effects of traditional infant-parent psychotherapy (PPT) with Wait, Watch and Wonder. A broad range of outcome measures was applied before and after treatment, and again on follow-up six months later. The majority of children referred to this service were insecurely attached. Both forms of treatment were delivered by highly trained clinicians. It was found that by the end of the intervention the Wait, Watch and Wonder method was associated with a more pronounced move towards secure attachment. The infants in this group also: “exhibited a greater capacity to regulate their emotions with a concomitant increase in cognitive ability.” (Cohen, et al., 1999:445) Their mothers: “reported more satisfaction with parenting than mothers in the PPT group and lower levels of depression at the end of treatment.” (ibid) Both forms of treatment showed similar positive gains. “They were associated with a reduction of presenting problems, improvement in the quality of the mother-child relationship, and reduction in parenting stress.” (ibid) However, at the six-month follow-up the two groups were similar on all measures. The Wait, Watch and Wonder group had retained its positive gains while the group receiving parent-infant psychotherapy had ‘caught up’. It was 51 concluded that both approaches are helpful, but the effects of Wait, Watch and Wonder came about more quickly. Wait, Watch and Wonder, with its dual emphasis on positive interaction and insight, is a hybrid of behavioural (i.e. interaction guidance) and psychodynamic approaches. Although not made explicit, this procedure too plainly targets and enhances parental reflective function with an emotionally containing setting. As with the other treatment modalities that have been mentioned, this technique could easily be offered in any CAMHS setting provided there were suitably qualified staff, since, again theoretically, the age–range for clients begins at zero. But there is an important caveat to be considered, since may would argue that infant mental health work does not naturally belong in the same stable as the interventions (and facilities) for older children and their families. This is not just a matter of site, access, noise- and intimidation-level, or the lack of suitably trained clinicians with relevant backgrounds. As Barrows (2000:19) argues, it is: “only within the context of a service that is dedicated to Infant Mental Health that (the) focus on the parent-infant relationship is likely to be sustained, and to feature as the prime focus of any therapy.” A consideration of the wide range of risk-factors that must be addressed makes it clear that a multi-disciplinary team is essential, since the caregiver-infant relationship will be influenced by seemingly distal pressures. Sometimes babies and toddlers are living in such adverse circumstances that they need to be moved to a new set of caregivers as quickly as possible. The relationship with the parent may be distorted beyond repair by an accumulation of risk factors. (Balbernie, 2002) As well as a treatment modality, the knowledge-base of infant 52 mental health offers us the understanding needed for speedy assessment and recommendation as to the course of action that will be in the baby’s best interest. The most radical and effective treatment for an infant is a new family. It is has been accepted for years that the longer after six months an adoption is finalised the greater the risk of later problems in relationships. (Singer, Brodzinsky, Ramsay, Steer and Waters, 1985) An Infant mental Health team in Baton Rouge, on the outskirts of New Orleans, is a pioneering example of how applied knowledge in this field enables a comparatively rapid assessment of caregiving to be carried out for very young children referred to the Child Protection Service. This project is funded by the courts and has a proven track record. It uses a range of specialised assessment methods, once again making careful use of video technology. (Larrieu and Zeanah, 2004) The purpose of this service is to provide the courts with an assessment that will be used as part of the decision-making process as to whether or not a child will be freed for adoption. A similar child population is served by an Attachment Clinic in Montreal which consults to the Youth Protection Service on issues related to permanency planning for very young children in foster care. (Gauthier, Fortin and Jeliu, 2004) They pay special attention to how the child has been affected by the original separation from biological parents and their response to the possibility that they might return after a long period with foster parents. The infant mental health specialist (a discrete profession in America) needs to call upon a wide range of skills and strategies that together: “contribute to the parent’s understanding of the infant, the awakening or repair of the early developing attachment relationship, and the parent’s capacity to nurture and protect a young child.” (Weatherston, 2000:6) This means strengthening relationships, whether 53 between parent and child, therapist and parent, or within the boundaries of the infant mental health service. Starting from the fundamental premise that all parents want to do the best they can for their babies, the infant mental health team builds on strengths in order to remove obstacles to a natural state of affairs. Parents, unsurprisingly, may not appreciate other know-it-alls thinking they need “training”, indeed, such an attitude: “may send a message of presumed incompetence, which might undermine a mother’s or father’s self-confidence and contribute inadvertently to less effective performance.” (Shonkoff & Phillips, 2000:371) Infant mental health specialists may be experts, but they relate to parents on the basis of partnership, not power, modelling the relationships they wish to promote. Conclusion. There is a growing body of evidence that demonstrates how early, targeted and strength-based interventions focussing on relationships can bring about positive changes in the emotional environment of vulnerable babies. As summarised by Professor Fonagy (1998:132) in an overview of the field: “early preventative interventions have the potential to improve in the short term the child’s health and welfare (including better nutrition, physical health, fewer feeding problems, lowbirth-weight babies, accident and emergency room visits, and reduced potential for maltreatment), while the parents can also expect to benefit in significant ways (including educational and work opportunities, better use of services, improved social support, enhanced self-efficacy as parents and improved relationships with their child 54 and partner). In the long term, children may further benefit in critical ways behaviourally (less aggression, distractibility, delinquency), educationally (better attitudes to school, higher achievement) and in terms of social functioning and attitudes (increased prosocial attitudes), while the parents can benefit in terms of employment, education and mental well-being.” To complement the evidence of clinical impact, longitudinal research, both psychological and neurological, has confirmed the vital importance of the early attachment relationship for future development. “The time of greatest influence, for good or ill, is when the brain is new. If we want to help the next generation we should be working with their parents while they are babies now” (Balbernie, 2001:253). This is simply a technical confirmation of what every parent has always known, although they may not have time to think about it until they are grandparents. It is something that somehow gets avoided when the implications have to be turned into policy or command resources. Who really doubts that: “The childhood shows the man, as morning shows the day.”? (Milton, 1671:Paradise Regained) If the first two years of life are cradled within secure attachment then the growing child feels good about him or herself, can appreciate the feelings of others and see their point of view, is able to take full advantage of education and has inherent psychological resiliency to fall back upon in times of stress. At the other end of the spectrum, the infant with disorganised attachment, who has often suffered abuse or neglect, will become the child who cannot trust relationships, who has no empathy for people or respect for social rules, who disrupts, attacks and tries to dominate what may be on offer in both the family and school, and who might well be seriously 55 vulnerable to later mental health problems. And furthermore, most importantly, these patterns of behaviour stand a good chance of being passed on to the next generation as the attachment experiences of infancy cut the template for the caregiving behaviours of adulthood. “By failing to understand the cumulative effects of the poisons assaulting our babies in the form of abuse, neglect, and toxic substances, we are participating in our own destruction.” (Karr-Morse & Wiley, 1997:12) Early intervention within the remit of an infant mental health service is an effective way of beginning to break the cycle of insecure attachment as it takes advantage of both the neurological plasticity of the baby and the fluid dynamics of a family in the process of adapting to a new member. Leave it too late and both the structure of the brain and family interactions become increasingly established and consequently harder to change. ***** Robin Balbernie. Child Psychotherapist. (robin.balbernie@glos.nhs.uk) (09/05/09). References. Adam, K. S., Sheldon-Keller, A. E., & West, M. (1996) Attachment organization and history of suicidal behavior in clinical adolescents. Journal of Consulting Psychology. 64, (2), 264-272. 56 Ainsworth, M. D., Blehar, M. C., Waters, E. & Walls, S. (1978) Patterns of attachment: A psychological study of the Strange Situation. Hillsdale, N. J.: Erlbaum. Allen, J. P., Houser, S. T., & Barman-Spurrell, E. (1996) Attachment theory as a framework for understanding sequelae of severe adolescent psychopathology: An 11year follow-up study. Journal of Clinical and Consulting Psychology. 64, 254-263. Allen, J. P., Moore, C. M. & Kupermine, G. P. (1997) Developmental approaches to understanding adolescent deviance. pp 548-567 in: Luthar, S. S. & Burack, J. A. (Eds) (1997) Developmental Psychopathology: Perspectives on Adjustment, Risk and Disorder. New York: Cambridge University Press. Bakermans-Kranenburg, M. J., van Ijzendoorn, M. H. & and Juffer, F. (2005) Disorganized infant attachment and preventative interventions: A review and metaanalysis. Infant Mental Health Journal. Vol. 26, (3), 191-216. Balbernie, R. (2001) Circuits and circumstances: the neurobiological consequences of early relationship experiences and how they shape later behaviour. Journal of Child Psychotherapy. Vol. 27, (3), 237-255. Balbernie, R. (2002) An infant in context: Multiple risks and a relationship. 57 Infant Mental Health Journal. 23, (3), 329-341. Balint, M. (1968) The Basic Fault. London: Tavistock Publications. Baradon, T., Broughton, C., Gibbs, I., James, J., Joyce, A. & Woodhead, J. (2005) The Practice of Psychoanalytic Parent Infant Psychotherapy: Claiming the Baby. London: Routledge. Baradon, T., Fonagy, P., Bland, K., Lenard, K. & Sleed, M. (2008) New Beginnings – an experience based programme addressing the attachment relationships between mothers and their babies in prisons. Journal of Child Psychotherapy. 34, (2), 240-258. Barlow, J., Davis, H., McIntosh, E., Jarrett, P., Mockford, C. & Stewert-Brown, S. (2007) Role of home visiting in improving parenting and health in families at risk of abuse and neglect: results of a multicentre randomised control trial and economic evaluation. Archives of Disease in Childhood, 92, 229-233. Barnard, K.E. (1998) Developing, implementing, and documenting interventions with parents and young children. Zero to Three. 18, (4), 23-29 58 Barnett, W. S. (2000) Economics of early childhood intervention. pp589-610 in: Shonkoff, J. P. & Meisals, S. J. (Eds) (2000) Handbook of Early Childhood Intervention. Cambridge: Cambridge University Press. Barrows, P. (2000) Making the case for dedicated infant mental health services. Psychoanalytic Psychotherapy. 14, (2), 111-128 Beebe, B. (2003) Brief mother-infant treatment: psychoanalytically informed video feedback. Infant Mental Health Journal. Vol. 24, (1), 24-52 Benoit, D., Madigan, S., Lecce, S., Shea, B., & Goldberg, S. (2001) Atypical maternal behaviour toward feeding-disordered infants before and after intervention. Infant Mental Health Journal. 22, (6), 611-626. Berlin, L. J., O’Neil, C. R., & Brooks-Gunn, J. (1998) What makes early intervention programs work? The program, its participants, and their interaction. Zero to Three. 18, (4), 4-15 van den Boom, D. (1995) Do first-year intervention effects endure? Follow-up study during toddlerhood of a sample of Dutch irritable infants. Child Development. 66, 1789-1816. 59 Brooks- Gunn, J., Leventhal, T., & Duncan, G. J. (2000) Why poverty matters for young children: Implications for policy. pp 89-131 in: Osofsky, J. D. & Fitzgerald, H. E. (Eds) (2000) WAIMH Handbook of Infant Mental Health. Vol. 3: Parenting and Child Care. New York: John Wiley & Sons. Campbell, F. A., & Ramey, C. T. (1994) Effects of early intervention on intellectual and academic achievement: A follow-up study of children from low-income families. Child Development. 65, 684-698. Campbell, F. A., & Ramey, C. T. (1995) Cognitive and high-school outcomes for high-risk African-American students at middle adolescence: Positive effects of early intervention. American Educational Research Journal. 32, (4), 743-772. Carlson,E. A. (1998) A prospective longitudinal study of attachment disorganization/disorientation. Child Development. 69, 1107-1129. Cassidy, J. (1988) Child mother attachment and the self in six year olds. Child Development. 59, 124-134 Cicchetti, D., Toth, S. L., & Rogosch, F. A. (1999) The efficacy of toddler-parent psychotherapy to increase attachment security in offspring of depressed mothers. Attachment & Human Development. 1, (1), 34-66. 60 Cohen, N. J., Muir, E., Parker, C. J., Brown, M., Lojkasek, M., Muir, R., & Barwick, M. (1999) Watch, Wait and Wonder: Testing the effectiveness of a new approach to mother-infant psychotherapy. Infant Mental Health Journal. 20, (4), 429-451. Cooper, G., Hoffman, K., Powell, B. & Marvin, R. (2005) The circle of security intervention: Differential diagnosis and differential treatment. pp. 127-151 in: Berlin, L. J., Ziv, Y., Amaya-Jackson, L. & Greenberg, M. T. (Eds) (2005) Enhancing Early Attachments. New York: The Guilford Press. Culp, A. M., Culp, R. E., Blankemeyer, M. & Passmark, L. (1998) Parent education home visitation program: adolescent and nonadolescent mother comparison after six months of intervention. Infant Mental Health Journal. 19, (2), 111-123. Culp, A. M., Culp, R. E., Hechtner-Galvin, T., Howell, C. S., Saathoff-Wells, T. & Marr, P. (2004) First-time mothers in home visitation services utilizing child development specialists. Infant Mental Health Journal. 25, (1), 1-15. Cummings, E. M., & Davies, P. T. (1994) Maternal depression and child development. Journal of Child Psychology and Psychiatry. 35, (1), 73-112. 61 Davis, H. (2009) The Family Partnership Model.) pp 63- 76 in: Barlow, J. & Svanberg, P. O. (Eds.) (2009) Keeping The Baby In Mind: Infant Mental Health in Practice. London: Routledge. Davis, H., Day, c. & Bidmead, C. (2002) The Parent Adviser Training Manual. London: Harcourt Assessment. Douglas, H. & Ginty, M. (2001) The Solihull Approach: changes in health visiting practice. Community practitioner. 74, (6), 222-224. Douglas, H. & Rheeston, M. (2009) The Solihull Approach: An integrative model across agencies. pp 29- 38 in: Barlow, J. & Svanberg, P. O. (Eds.) (2009) Keeping The Baby In Mind: Infant Mental Health in Practice. London: Routledge. Dozier, M., Stovell, K. C. & Jacobvitz, D. (1999) Attachment and psychopathology in adulthood. pp. 497-519 in: Cassidy, J. & Shaver, P. R. (Eds) (1999) Handbook of Attachment. New York: The Guilford Press. 62 Dozier, M., Stovell-McClough, K. C., & Albus, K. E. (2008) Attachment and psychopathology in adulthood. pp.718-744 in: Cassidy, J. & Shaver, P. R. (Eds) (2008) Handbook of Attachment. New York: The Guilford press. Eckenrode, J., Ganzel, B., Henderson, C. R., Smith, E., Olds, D. L., Powers, J., Cole, R., & Sidora, K. (2000) Preventing child abuse and neglect with a program of nurse home visitation. Journal of the American Medical Association. 284, (11), 1385-1391. Emde, R. N. (2001) Infant mental health challenges for Early Head Start: Understanding context and overcoming avoidance. Zero to Three. 22, (1), 21-24 Farren, D. C. (2000) Another decade of intervention for children who are low income or disabled: What do we know now? pp. 510-548 in: Shonkoff, J. P. & Meisals, S. J. (Eds) (2000) Handbook of Early Childhood Intervention. Cambridge: Cambridge University Press. Felitti, V. S., Anda, R. F., Nordenburg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss M. P., & Marks, J. S. (1998) Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine. 14, (4), 245-247. 63 Fitzgerald, H. E., Puttler, L. I., Mun, E. Y., & Zucker, R. A. (2000) Prenatal and postnatal exposure to parental alcohol use and abuse. pp. 123-159 in: Osofsky, J. D. & Fitzgerald, H. E. (Eds) (2000) WAIMH Handbook of Infant Mental Health. Vol. 4. Infant Mental Health in Groups at High Risk. New York: John Wiley & Sons. Fonagy, P. (1998) Prevention, the appropriate target of infant psychotherapy. Infant Mental Health Journal. 19, (2), 124-150. Fonagy, P. & Higgitt, A. (2000) An attachment theory perspective on early influences on development and social inequalities in health. pp. 521-578 in: Osofsky, J. D. & Fitzgerald, H. E. (Eds) (2000) WAIMH Handbook of Infant Mental Health, Vol. 4: Infant Mental Health in Groups at High Risk. New York: John Wiley & Sons. Fonagy, P., Steele, H., Steele, M., Moran, G. S. and Higgitt, A. C. (1991) The Capacity for Understanding Mental States: The Reflective Self in Parent and Child and its Significance for Security of Attachment. Infant Mental Health Journal. 12, (3), 201-218. Fonagy, P., Target, M., Steele, M., Steele, H., Leigh, T., Levinson, A., & Kennedy, R. (1997) Morality, disruptive behaviour, borderline personality disorder, crime, and their relation to security of attachment. pp. 223-274 in: Atkinson, L. & Zucker, K. J. (Eds) (1997) Attachment and Psychopathology. New York: The Guilford Press. 64 Fonagy, P., Steele, M., Steele, H., Leigh, T., Kennedy, R., Mattoon, G., & Target, M. (1995) Attachment, the reflective self, and borderline states. pp. 233-278 in: Goldberg, S., Muir, R., & Kerr, J. (Eds) (1995) Attachment Theory: Social, Developmental, and Clinical Perspectives. Hillsdale, N. J.: The Analytic Press. Free, F., Alechina, I., & Zahn-Waxler, C. (1996) Affective language between depressed mothers and their children: The potential impact of psychotherapy. Journal of the American Acadamy of Child & Adolescent Psychiatry. 35, (6), 783790. Friedli, L. & Parsonage, M. (2007) Building an economic case for mental health promotion: part1. Journal of Public Heath. Vol. 6, (3), 14-23 Gauthier, Y., Fortin, G. & Jeliu, G. (2004) Clinical application of attachment theory in permanency planning for children in foster care: The importance of continuity of care. Infant Mental Health Journal. 25, (4), 379-396. Glaser, D. (2000) Child abuse and neglect and the brain – a review. Journal of Child Psychology and Psychiatry, 41, (1), 97-116. Goldberg, S. (2000) Attachment and Development. London: Arnold. 65 Green, J., Stanley, C. and Peters, S. (2007) Disorganized attachment representations and atypical parenting in young school age children with externalising disorder. Attachment & Human Development, 9, (3), 207-222. Greenberg, M. T., De Klyer, M., Speltz, M. L. & Endriga, M. C. (1997) The role of attachment processes in externalizing psychopathology in young children. pp. 196222 in: Atkinson, L. & Zucker, K. J. (Eds) (1997) Attachment and Psychopathology. New York: The Guilford Press. Grienenberger, J., Kelly, K., and Slade, A. (2005) Maternal reflective functioning, mother-infant affective communication, and infant attachment: Exploring the link between mental states and observed caregiving behaviour in the intergenerational transmission of attachment. Attachment & Human Development, 7, (3), 299-311. Grossmann, K. E., Grossmann, K., & Zimmermann, P. (1999) A wider view of attachment and exploration: Stability and change during the years of immaturity. pp. 760-786 in : Cassidy, J. & Shaver, P. R. (Eds) (1999) Handbook of Attachment: Theory, Research, and Clinical Applications. New York: The Guilford Press. Halpern, R. (1993) Poverty in infant development. pp. 73-86 in: Zeanah, C. H. (Ed) (1993) Handbook of Infant Mental Health. New York: The Guilford Press. 66 Harris, W. M., Lieberman, A. F., & Marans, S. (2007) In the best interests of society. Journal of Child Psychology and Psychiatry, 48, 3 / 4, 392-411. Heinicke, C. M., Fineman, N. R., Ruth, G., Recchia, S. L., Guthrie, D., & Rodning, C. (1999) Relationship-based intervention with at-risk mothers: Outcome in the first year of life. Infant Mental Health Journal. 20, (4), 349-374. Heinicke, C. M., Fineman, N. R., Ponce, V. A., & Guthrie, D. (2001) Relationshipbased intervention with at-risk mothers: Outcome in the second year of life. Infant Mental Health Journal. 22, (4), 431-462. Jacobsen, T., Edelstein,W., & Hofmann, V. (1994) A longitudinal study of the relation between representations of attachment in childhood and cognitive functioning in childhood and adolescence. Developmental Psychology. 30, 112-124. Juffer, F., Bakermans-Kranenburg, M. J. & van IJzendoorn, M. H. (Eds) (2007) Promoting Positive Parenting: An Attachment-Based Intervention. London: Lawrence Erlbaum Associates. Karen, R. (1994) Becoming Attached: First Relationships and How They Shape Our Capacity to Love. Oxford: Oxford University Press. 67 Karlsson, K. & Skagerberg, A. (1999) Experience from the floor of attachment and relationship building. The Signal. 7, (2), 1-7 Karr-Morse, R. & Wiley, M. S. (1997) Ghosts From the Nursery: Tracing the Roots of Violence. New York: The Atlantic Monthly Press. Kobak, R., Little, M., Race, E., & Acosta, M. C. (2001) Attachment disruptions in seriously emotionally disturbed children: Implications for treatment. Attachment & Human Development. 3, (2), 243-258. Landy, S. (2000) Assessing the risks and strengths of infants and families in community-based programs. pp 335-375 in: Osofsky, J. D. & Fitzgerald, H. E. (Eds) (2000) WAIMH Handbook of Infant Mental Health. Vol. 2: Early Intervention, Evaluation, and Assessment. New York: John Wiley & Sons. Larrieu, J. A. and Zeanah, C. H. (2004) Treating parent-infant relationships in the context of maltreatment: An integrated systems approach. pp. 243-264 in: Sameroff, A. J., McDonough, S. C. & Rosenblum, K. L. (Eds) (2004) Treating Parent-Infant Relationship Problems: Strategies for Intervention. New York: The Guilford Press. 68 Lieberman, A. F., Diaz, M. A. & Van Horn, P (2009) Safer beginnings: Perinatal child-parent psychotherapy for newborns and mothers exposed to domestic violence. Zero to Three, 29, (5), 17-22. Lieberman, A. F., Ippen, C. G. & Van Horn, P. (2006) Child-parent psychotherapy: 6month follow-up of a randomised controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 45, (8), 913918. Lieberman, A. F. & Pawl, J. H. (1993) Infant-parent psychotherapy. pp 427-442 in: Zeanah, C. H. (Ed) (1993) Handbook of Infant Mental Health. New York: The Guilford Press. Lieberman, A. F., Van Horn, P. & Ippen, C. G. (2005) Towards evidence-based treatment: Child-parent psychotherapy with preschoolers exposed to marital violence. Journal of the American Academy of Child and Adolescent Psychiatry, 44, (12), 1241-1248) Lieberman, A. F. & Van Horn, P. (2008) Psychotherapy With Infants and Young Children. New York: The Guildford Press. Liotti, G. (1999) Disorganization of attachment as a model for understanding dissociative psychopathology. pp 291-317 in: Solomon, J. & George, C. (Eds) (1999) Attachment Disoganization. New York: The Guilford Press. 69 Lyons-Ruth, K. (2008) Contributions of the mother-infant relationship to dissociative, borderline, and conduct symptoms in young adulthood. Infant Mental Health Journal. 29, (3), 203-218. Lyons-Ruth, K. & Jacobvitz, D. (1999) Attachment disorganization: Unresolved loss, relational violence, and lapses in behavioural and attentional strategies. pp520-554 in: Cassidy, J. & Shaver, P. R. (Eds) (1999) Handbook of Attachment: Theory, Research, and Clinical Applications. New York: The Guilford Press. MacLeod, J. & Nelson, C. (2000) Programs for the promotion of family wellness and the prevention of child maltreatment: A meta-analytic review. Child Abuse and Neglect. 24, (9), 1127-1149 Madigan, S., Hawkins, e., Goldberg, S. & Benoit, D. (2006) Reduction of disrupted caregiver behaviour using modified interaction guidance. Infant Mental Health Journal. 27, (5), 509-527. Mayers, H. A., Hagar-Budny, M. and Buckner, E. B. (2008) The Chances for Children teen parent-infant project: results of a pilot intervention for teen mothers and their infants in inner city high-schools. Infant Mental Health Journal, 29, (4), 320-342, Melhuish, E., Belsky, J. & Barnes, J. (2010) Evaluation and value of Sure Start. Archives of Disease in Childhood, 95, 159-161. (available from adc.bmj.com) 70 McDonough, S. (1993) Interaction guidance: Understanding and treating early infantcaregiver relationship disturbances. pp 414-426 in: Zeanah, C. H. (Ed) (1993) Handbook of Infant Mental Health. New York: The Guilford Press. McDonough, S. (2004) Interaction guidance: promoting and nurturing the caregiving relationship. pp. 79-96 in: Sameroff, A. J., McDonough, S. C. & Rosenblum, K. L. (Eds) (2004) Treating Parent–Infant Relationship Problems: Strategies for Intervention. New York: The Guilford Press. Milford, R., Kleve, l., Lea, J. and Greenwood, R. (2006) A Pilot Evaluation of the Solihull Approach. Community practitioner, 79, (11), 358-362. Moss, E., Rousseau, D., Parent, s., St-Laurent, D., & Saintonge, J. (1998) Correlates of attachment at school age: Maternal reported stress, mother-child interaction and behaviour problems. Child Development. 69, 1390-1405. Moss, E., St-Laurent, D., & Parent, S. (1999) Disorganized attachment and developmental risk at school age. pp. 160-186 in: Solomon, J. & George, C. (Eds) (1999) Attachment Disorganization. New York: The Guilford Press. 71 Motz, M., Leslie, M. & DeMarchi, G. (2007) Breaking the Cycle: Using a Relational Approach to Address the Impact of Maternal Substance Abuse on Regulation and Attachment in Children. Zero to Three, 27, (4), 19-25. Murray, L. (1997) Postpartum depression and child development. Psychological Medecine. 27, 253-260. Murray, L., Sinclair, D., Cooper, P., Ducournau, P., & Turner, P. (1999) The socioemotional development of 5-year old children of postnatally depressed mothers. Journal of Child Psychology and Psychiatry. 40, (8), 1259-1271. New Economics Foundation. (2009) Backing the Future. Downloaded 03/05/2010 from: www.neweconomics.org/publications/backing-future Newman, L. & Stevenson, C. (2008) Issues in infant-parent psychotherapy for mothers with borderline personality disorder. Clinical Child Psychology and Psychiatry, 13, (4), 505-514. Olds, D. L. (2006) The nurse-family partnership: an evidence-based preventive intervention. Infant Mental health Journal, Vol. 27, (1), 5-25. 72 Olds, D. L., Eckenrode, J. J., Henderson, C. R., Kitzman, H., Powers, J., Cole, R., Sidora, P., Morris, L. M., Pettitt, L. M., & Luckey, D. (1997) Long-term effects of home visitation on maternal life course and child abuse and neglect: Fiveteen year follow-up of a randomized trial. Journal of the American Medical Association. 278, (8), 637-643. Olds, D. L., Henderson, C. R., Kitzman, H. J., Eckenrode, J. J., Cole, R. E., & Tatelbaum, R. C. (1999) Prenatal and infancy home visitation by nurses: Recent findings. The Future of Children. 9, (1), 44-65. Oppenheim, D. Goldsmith, D. & Koren-Karie, N. (2004) Maternal insightfulness and preschoolers’ emotion and behaviour problems: Reciprocal influences in a therapeutic preschool program. Infant Mental Health Journal. 25, (4), 352-367. Osofsky, J. D., Kronenberg, M., Hammer, J. h., Lederman, C., Katz, L., Adams, S., Graham, M. & Hogan, A. (2007) The development and evaluation of the intervention model for the Florida Infant Mental Health Pilot Program. Infant Mental Health Journal. 28, (3), 258-280. Osofsky, J. D. & Thompson, M. D. (2000) Adaptive and maladaptive parenting: Perspectives on risk and protective factors. pp 54-75 in: Shonkoff, J. P. & Meisals, S. J. (Eds) (2000) Handbook of Early Childhood Intervention. Cambridge: Cambridge University Press. 73 Paris, R., Spielman, E. & Bolton, R. E. (2009) Mother-infant psychotherapy: Examining the therapeutic process of change. Infant Mental Health Journal. 30, (3), 301-319. Powell, C. & Grantham-McGregor, S. (1998) Home visiting of varying frequency and child development. Pediatrics. 84, 157-164. Puckering, C. (2004) Mellow Parenting: An intensive intervention to change relationships. The Signal. 12, (1), 1-5. Puckering, C. (2009) Mellow Babies: Mellow Parenting with parents of infants. pp 155-163 in: Barlow, J. & Svanberg, P. O. (Eds.) (2009) Keeping The Baby In Mind: Infant Mental Health in Practice. London: Routledge. Ramey, C. T., Bryant, D. M., Wasik, B. H., Sparling, J. J., Fendt, K. H., & La Vange, L. M. (1992) Infant health and development program for low birth weight, premature infants: Program elements, family participation, and child intelligence. Pediatrics. 89, 454-465. 74 Read, J., Fink, P. J., Rudegeair, T., Felitti, V. & Whitfield, C. L. (2008) Child maltreatment and psychosis: A return to a genuinely integrated bio-social model. Clinical Schizophrenia & Related Psychosis, 2, (3), 217-225. Robert-Tissot, C., Cramer, B., Stern, D. S., Serpa, S. R., Bachmann, J. P., PalacioEspasa, F., Knauer, D., De Muralt, M., Bernay, C., & Mendiguren, G. (1996) Outcome evaluation in brief mother-infant psychotherapies: Report on 75 cases. Infant Mental Health Journal. 17, (2), 97-114. Roisman, G. I., Collins, W. A., Sroufe, L. A., & Egeland, B. (2005) Predictors of young adults’ representations of and behaviour in their current romantic relationship: Prospective tests of the prototype hypothesis. Attachment & Human Development. 7, (2), 105-121. Rosenblum, K. L., McDonough, S. C., Sameroff, A. J. and Muzic, M. (2008) Reflection in thought and action: Maternal parenting reflectivity predicts mindminded comments and interactive behavior. Infant Mental Health Journal, 29, (4), 362-376. Rosenstein, D. S. & Horowitz, H. A. (1996) Adolescent attachment and psychopathology. Journal of Consulting and Clinical Psychology, 64, 244-253. 75 Rowe, A. (2009) Perinatal home visiting: Implementing the Nurse-Family Partnership in England. pp 114-127 in: Barlow, J. & Svanberg, P. O. (Eds.) (2009) Keeping The Baby In Mind: Infant Mental Health in Practice. London: Routledge. Sameroff, A. (2000) Ecological perspectives on developmental risk. pp. 1-33 in: Osofsky, J. D. & Fitzgerald, H. E. (Eds) (2000) WAIMH Handbook of Infant Mental Health, Vol. 4: Infant Mental Health in Groups at High Risk. New York: John Wiley & Sons. Schechter, D. S. (2004) How post-traumatic stress affects mothers’ perceptions of their babies: A brief video feedback intervention makes a difference. Zero to Three. Vol. 24, (3), 43-49. Schechter, D. S., Myers, M. M., Brunelli, S. A., Coates, S. W., Zeanah, C. H., Davies, M., Grienenberger, J. F., Marshall, R. D., McCaw, J. E., Trabka, K. A. & Liebowitz, M. R. (2006) Traumatized mothers can change their minds about their toddlers: understanding how a novel use of videofeedback supports positive change of maternal attributions. Infant Mental Health Journal, 27, (5), 429-447. Schore, A.N. (1994) Affect Regulation and the Origin of the Self: The Neurobiology of Emotional Development. New Jersey: Erlbaum. Schore, A. N. (2001a) Effects of a secure attachment relationship on right brain development, affect regulation, and infant mental health. 76 Infant Mental Health Journal. 22, (1-2), 7-66. Schore, A. N. (2001b) The effects of early relational trauma on right brain development, affect regulation, and infant mental health. Infant Mental Health Journal. 22, (1-2), 201-269. Scott, Knapp, Henderson & Maughan (2001) Financial costs of social exclusion: Follow up study of antisocial children into adulthood. BMJ, 323, 7306:191 Shaw, D. S., Owens, E. B., Vondra, J. I., Keenan, K., & Winslow, E. B. (1996) Early risk factors and pathways in the development of early disruptive behaviour problems. Development and Psychopathology, 8, 679-699. Shonkoff, J. P. & Phillips, D. A. (Eds) (2000) From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington D. C.: National Academy Press. Siegal, D. J. (1999) The Developing Mind: Towards a Neurobiology of Interpersonal Experience. New York: The Guilford Press. Simpson, J. A. (1999) Attachment theory in modern evolutionary perspective. pp 115140 in: Cassidy, J. & Shaver, P. R. (Eds) (1999) Handbook of Attachment: Theory, Research, and Clinical Applications. 77 Sinclair, A. (2007) 0-5:How Small Children Make a Big Difference. Provocation Series, Vol. 3, (1) (Available online, www.theworkfoundation.com ) London: The Work Foundation. Sinclair, D. & Murray, L. (1998) The effect of postnatal depression on children’s adjustment to school. British Journal of Psychiatry. 172, 58-63. Singer, L. M., Brodzinsky, D. M., Ramsay, D., Steer, M. & Waters, E. (1985) Mother-infant attachment in adoptive families. Child Development, 56, 1543-1551. Slade, A., Grienenberger,J., Bernbach, E., Levy, D. & Locker, A. (2005) Maternal reflective functioning, attachment, and the transmission gap: A preliminary study. Attachment & Human Development. 7, (3), 283-298. Slade, A., Sandler, L. S., & Mayes, L. C. (2005) Minding the baby: Enhancing parental reflective functioning in a nursing/mental health home visiting program. pp. 152-177 in: Berlin, L. J., Ziv, Y., Amaya-Jackson, L. & Greenberg, M. T. (Eds) (2005) Enhancing Early Attachments. New York: The Guilford Press. Solchany, J. E. & Barnard, K. E. (2001) Is mom’s mind on her baby? Infant mental health in Early Head Start. Zero to Three. 22, (1), 39-47. 78 Speltz, M. L., Greenberg, M. T., & De Klyen, M. (1990) Attachment in preschoolers with disruptive behaviour: A comparison of clinic-referred and nonproblem children. Development and Psychopathology. 2, 31-46. Sroufe, L. A., Egeland, B., Carlson, E. A., & Collins, W. A. (2005) The Development of the Person: The Minnasota Study of Risk and Adaptation From Birth to Adulthood. New York: The Guilford Press. Svanberg, P. O. G. (2005) Promoting attachment security in primary prevention using video-feedback: The Sunderland Infant Programme. Infant Mental Health Journal. Submitted. Svanberg, P. O. (2009) Promoting a secure attachment through early screening and interventions. pp 100-114 in: Barlow, J. & Svanberg, P. O. (Eds.) (2009) Keeping The Baby In Mind: Infant Mental Health in Practice. London: Routledge. Thompson, R. A. (1999) Early attachment and later development. pp 265-286 in: Cassidy, J. & Shaver, P. R. (Eds) (1999) Handbook of Attachment: Theory, Research, and Clinical Applications. New York: The Guilford Press. Vaughan, S. C. (1997) The Talking Cure: The Science Behind Psychotherapy. New York: C. P. Putnam’s Sons. 79 Velderman, M. K., Bakermans-Kranenburg, M. J., Juffer, F. & Van Ijzendoorn, M. H. (2006) Preventing preschool externalizing behavior problems through video-feedback intervention in infancy. Infant Mental Health Journal, 27, (5), 466-493) Verschueren, K. (2001) Narratives in attachment research. Biennial meeting of the European Society of Developmental Psychology; Uppsala. Verschueren, K. & Marcoen, A. (1999) Representation of self and socioemotional competence in kindergartners: Differential and combined effects of attachment to mother and to father. Child Development. 70, 183-201. Warren, S. L., Huston, L., Egeland, B., & Sroufe, L. A. (1997) Child and adolescent anxiety disorders and early attachment. Journal of the American Academy of Child and Adolescent Psychiatry. 36, 637-644. Weatherston, D. J. (2000) The infant mental health specialist. Zero to Three. 21, (2), 3-10. Weinfield, N. S., Whaley, G. J. J., & Egeland, B. (2004) Continuity, discontinuity, and coherence in attachment from infancy to late adolescence: Sequelae of organization and disorganization. Attachment & Human Development. Vol.6, (1), 73-97. 80 Wood, M. J., Lee, S. S., & Lipper, E. G. (2000) Failure-to thrive is associated with disorganized infant-mother attachment and unresolved maternal attachment. Infant Mental Health Journal. 21, (6), 428-442. Velderman, M. K., Bakermans-Kranenburg, M. J., Juffer, F., Van Ijzendoorn, M. H., Mangelsdorf, S. C. & Zevalkink, J. (2006) Preventing preschool externalizing problems through video-feedback intervention in infancy. Infant Mental Health Journal, 27, (5), 466-493. Vik, K. & Braten, S. (2009) Video interaction guidance inviting transcendence of postpartum depressed mothers’ self-centred state and holding behavior. Infant Mental health Journal, 30, (3), 287-300. Zeanah, C. H., Boris, N. W., & Larrieu, J. A. (1997) Infant development and developmental risk: A review of the past ten years. Journal of the American Academy of Child and Adolescent Psychiatry. 32, 165-178. de Zulueta, F. (1993) From Pain to Violence: The Traumatic Roots of Destructiveness. London: Whurr Publications. 81