bone tissue - WordPress.com
advertisement

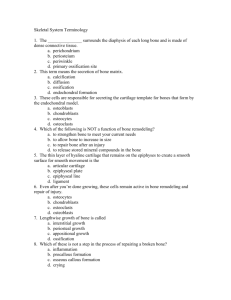
1 BONE TISSUE: Skeleton, cartilage, ligaments, connective tissue Ligaments Tendons Functions 1. Structural support framework 2. Protection 3. Movement 4. Blood cell production 5. Storage of minerals & lipids (electrolyte balance) a. Ca & phosphate ions b. Lipids 6. Leverage 7. Acid-base balance 8. Detoxification Contain: Osseous tissue, connective tissue, smooth muscle and neural tissue Mineralization or calcification Structure Types of osseous tissue: 1. Compact 2. Spongy bone General Features: Articular cartilage Epiphysis Diaphysis Nutrient foramina Epiphyseal plate/Line Periosteum- outer surface of the bone 1. Isolates bone from surrounding tissue 2. Provides route for nervous & blood supply 3. Participates in bone growth & repair Endosteum- lines bone marrow cavity 1. Active during growth and repair 2. Incomplete epithelial layer Classification of Bones: 1. 2. 3. 4. 5. 6. Long Short bone Flat bones Irregular Sesamoid Surface bones (wormian) Matrix & specialized cells 1. Cells a. Osteoprogenitor cells/Osteogenic cells- (mesenchymal) 2 b. Osteoblast (non mitotic) - Responsible for synthesis matrix compounds c. Osteocytes Lacunae Canaliculi d. Osteoclasts 2. Matrix - Collagen form frame work for mineral crystals Structural Differences: 1. Compact - Basic functional unit = osteon - Osteocytes in concentric layers around central canal (lamellae) 2. Spongy - No osteons - Concentric lamellar from trabeculae-plates that branch. Ex. forms an open network. 3. Bone marrow 1. Red marrow (hemopoeitic) 2. Yellow marrow 3. Gelatinous marrow BONE DEVELOPMENT Formation of bone = Ossification or osteogenesis 1. Intramembranous bone development from Mesenchymal cells without an intervening cartilage stage 2. Endochondralwithin cartilage or cartilaginous tissue Intramembranous Ossification Produces most of the flat bones of the skull and the clavicle Steps: Embryonic CT condenses into a sheet of soft tissue with a dense supply of capillaries The sheet enlarges and differentiates into osteogenic cells Some mesenchyme transforms into a network of soft trebeculae Osteogenic cells gather on the trabeculae, become osteoblasts and deposit osteoid tissue- soft bone tissue lacking minerals As trabeculae grow thicker, calcium phosphate is deposited in the matrix and some osteoblasts become trapped in lacunae. Once trapped, osteoblasts differentiate into osteocytes Some calcified trabeculae become permanent spongy bone Osteoclasts appear early on these trabeculae, reabsorbing and remodeling the bone creating a marrow space within the bone. Trabeculae at the surface of the bone continue to calcify until the spaces between them are filled in converting spongy bone to compact bone. Mesenchymal cells on the surface remains uncalcified but becomes increasingly fibrous and will eventually give rise to the periosteum of the bone. 3 Endochondral Ossification Produces bones including vertebrae, pelvic bones and bones of the limbs. Mesenchyme transforms into a hyaline cartilage model which eventually turns into bone. Multiplication of chondrocytes near the center of the model forming a primary ossification center. As lacunae enlarge, the matrix is reduced and the model weakens Some cells of the perichondrium become osteoblasts, producing a bony collar around the model The collar provides support and cuts off diffusion of the nutrients to the chondrocytes, becomes a sheath known as the periosteum. CT grows from the periosteum into cartilage penetrating and breaking down the lacunae transforming the primary ossification center into the primary marrow space. Osteogenic cells invade the model via CT buds, transform into osteoblasts and line the marrow space. The osteoblasts deposit osteoid tissue and then calcify it to form temporary network of trabeculae. As ossification progresses, osteoclasts breakdown the temp. trabeculae and enlarge the primary marrow space. The ends of thebone are still composed of hyaline cartilage. Development of the metaphysis Transitional zone exhibiting 5 zones of transformation form cartilage to bone. 1. Zone of reserve cartilage- Farthest from the marrow- resting 2. Zone of cell proliferation- Chondrocytes multiply and become arranged into longitudinal columns of flattened lacunae 3. Zone of hypertrophy- chondrocytes cease to divide and begin to hypertrophy ( Zones 3 & 2 piush zone 1 upward) 4. Zone of calcification- Minerals are deposited in the matrix between columns of lacunae and calcify the cartilage fro temp. support. 5. Zone of bone deposition- Within each column, the walls between lacunae breakdown and chondrocytes begin to die. Each channel is converted into a hollow channel which becomes invaded by blood vessels. Osteoclasts dissolve the calcified cartilage while osteoblasts line up along the channel walls depositing concentric lamellae of the matrix. Osteoblasts trapped in their own matrix become osteocytes and stop producing matrix. Around birth, secondary ossification centers begin to form around the epiphyses Chondrocytes enlarge, the walls of the matrix begin dissolving and chondrocytes die. Cartilage is eroded from the center of the epiphysis outward in all directions Thin trabeculae of the cartilage matrix are calcified into spongy bone. Hyaline cartilage persists as articular cartilage on the surface of bones and at the junction of the diaphysis and epiphysis= froming epiphyseal plate. Bone Growth and Remodeling Bones continue to grow and remodel themselves throughout life. Cartilage grows by 2 mechanisms 1. interstitial growth- adding more matrix internally (adds length) 2. appositional growth- adding more to the surface ( similar to intramembranous ossification) Achondroplastic Dwarfism PHYSIOLOGY OF OSSEUS TISSUE Mineral Depostition- crystallization process in which calcium and phosphate ions are taken from the blood plasma and deposited in bone tissue. Osteoblasts produce collagen fibers which become encrusted with minerals- calcium phosphate 4 The product of Calcium and phosphate must reach a certain level in the tissues for crystals (hydroxyapetite) to form, osteoblasts neutralize inhibitors allowing the salts to precipitate in the bone matrix. The first crystals act as “seed crystals”. Osseus tissue sometimes forms in the lungs, brain, eyes, muscle tendon, arteries= abnormal ossification= ectopic ossification Calculus- a calcified mass in soft organs. Mineral Resorption The process of dissolving bone Carried out by osteoclasts Hydrogen pumps in the ruffled border of the osteoclasts secrete hydrogen ions in the extracellular fluid and chloride ions follow by electrical attraction Space between the osteoclasts and bone become filled with HCL (pH=4) that dissolves the bone minerals Osteoclasts also secretes acid phosphatase that digests the collagen of the bone matrix. Calcium and Phosphate homeostasis Calcium Phosphate 99% of Calcium is in the bones 2 pools of Ca 1. hydroxyapetite 2. tissue fluid- exchangeable hypocalcemia- deficiency in blood calcium- leads to muscle tremors, spasms, or tetany- inability of muscles to relax normal blood calcium= 9.2-10.4 mg/dL 6mg/dL- carpopedal spasm 4mg/dL- laryngospasm hypercalcemia- excess of blood calcium 12mg/dL- depression of the nervous system, emotional disturbances, muscle weakness, sluggish reflexes and sometimes cardiac arrest. Calcium phosphate homeostasis is regulated by 3 hormones: calcitrol, calcitonin and parathyroid hormone. Calcitrol- Form of vitamin D produced by action of the skin, liver and kidneys Vitamin that raises blood calcium concentration 3 mechanisms: 1. increases absorption by the small iontestine 2. Increase calcium and phosphate reabsorption by the from the skeleton 3. Weakly promotes reabsorption of Ca+ by the kidneys. ALSO needed for bone deposistion otherwise leads to rickets in children and osteomalacia in adults. Calcitonin-Secreted by C cells of the thyroid gland Secreted when blood Ca levels are too high, loweres concentration by 2 mechanisms: 1. osteoclast inhibition 2. osteoblast stimulation Important role in children (osteoclasts are very active due to modeling) Very little effect on adults Parathyroid Hormone Raises blood Ca levels by 4 mechanisms: 1.stimulates secretion of osteoclast stimulating factor 2. promotes Ca reabsorption by the kidneys 3. promotes the final step of calcitrol synthesis 4. Inhibits collagen synthesis by osteoblasts, inhibiting bone deposition 5 Skeletal system 2 divisions 1. Appendicular 2. Axial – skull (22), thorax (25), vertebral column (26); form longitudinal axis of the body Function of Axial Skeleton 1. Creates framework that supports the organs of the dorsal & ventral cavity 2. Houses sense organs for taste, smell, hearing 3. Provides surface area for attaching muscle Cranium- 8 bones 1-frontal 2-temporal 1-occipital 2-paroetal 1-sphenoid 1-ethmoid Facial bones-14 bones 2-maxilla 2-palatine 2-nasal 2- inferior nasal conchae 2- zygomatic 2- lacrimal 1-vomer 1- mandible Nasal Complex Orbital complex Auditory ossicles Hyoid bone Vertebral column (26 bones): Functions - Column of support, bears weight of the head, neck, trunk; transferring it to appendicular skeleton Cervical- 7; c1-c7; C1=atlas, holds head; C2=axis; dens odontoid process forms pivot for rotation Thoracic – 12; T1-T12 Lumbar- 5; L1-L5 Sacral- originates as 5 bones Coccygeal- originates as 3-5 bones Ribs (12 Pairs): 1-7 are true ribs 8-12 are false ribs o 11-12 are floating ribs Sternum: 1. Manubrium 2. Body 3. Xyphoid 6 Appendicular skeleton - includes bones of the upper & lower limbs - supporting elements = girdles connect hem to the trunk - marking are attached sites for the muscles or opening for the nerve or blood vessels Pectoral girdle & upper limb: Pectoral girdle Upper limb Pelvis girdle & lower limb: - supports & protects lower viscera, reproductive organs - bears weight of body - locomotion consists of: paired or fused coxae ( coxae) pelvis - coxae of append. 7& sacrum & coccyx of axial skeleton each coxae - 3 parts ilium, ischium, pubis pelvis subdivided into: - false/greater pelvis blades & ilium - true/ lesser pelvis pubic bone, ischium, sacrum lower limbs: femur patella tibia fibula tarsal metatarsal phalanges ************Page 207; table 7-1; be able to differentiate male & female skeleton************* Articulation- joint, where two bones interact 3 functional categories of joints 1. synarthorsis 2. Amphiarthrosis 3. Diarthrosis Synarthrosis: a. suture b. Periodontal ligament c. Synostosis Amphiarthrosis: Maybe connected by collagen fibers in cartilage 1. syndismosis 2. symphysis 3. Diarthrosis - permits a wide range of movement - found at ends of long bones - articulation surfaces covered by cartilage - surround by a capsule- dense connective tissue 7 Synovial membrane line joint & produce Synovial fluid - provide lubrication - nourish the chondrocyte - act as shock absorber Accessory structures: 1. pads of cartilage or fats 2. ligaments 3. tendons 4. bursae Articular form & function: - Possible movement of bone at articulation 1. linear motion 2. angular motion 3. rotation joints classified on the number of axes they allow movement - monaxial - biaxial - triaxial types of movement: 1. gliding 2. angular motion - abduction - adduction - flexion - extension - hyperextension - circumduction Rotation – left & right - pronation - supination Special movements: - eversion/inversion (foot) - plantar flexion & dorsiflexion (foot) - lateral flexion - protraction/retraction - opposition - elevation/depression Structural classification of Synovial joints: - gliding joints - hinge joint - pivot joints - ellipsoidal - saddle joints - Ball & socket joint ***********read clinical briefs in chapter*************************** 8