067_MLP_ENG
advertisement

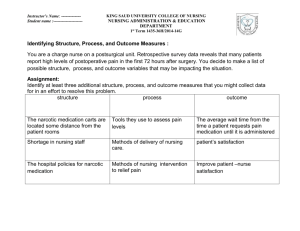
AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication Instructor Serial/Semester Location Start/Finish Time Date LESSON OBJECTIVE Performance: To gain an understanding of pain medications. Conditions: The student will be presented a powerpoint presentation by the instructor and will have all necessary references made available to him/her. Standard: 1. Given the five elements of the nursing care process and a simulated privileged provider’s order by correctly responding to written, oral, and experiential assessment measures . TEACHING POINTS 1. Identify the action, uses, side effects, nursing considerations for selected nonnarcotic analgesics. 2. Identify the action, uses, side effects, nursing assessment and patient teaching for selected narcotic analgesics. 3. Identify the action, uses, side effects, nursing assessment and patient teaching for selected narcotic antagonist. 4. 5. 6. 7. 8 9. 10. INSTRUCTIONAL STRATEGY Interactive Lecture Method: Instructor Media: Classroom Environment: OTHER LESSON SPECIFICATIONS Knowledge Lesson Type of Lesson: 1/50 Ratio: Resources: . End of Lesson Test: None Minutes Instructional Time: 138 Reference(s): ISBN 0-7817-3696-X Introductory Clinical Pharmacology, 7th Ed. 01 Jan 2004 LESSON PLAN APPROVAL Signature of Standards Officer Date AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication INTRODUCTION Allocated Time: Review: 5 Minutes You have had previous anatomy and physiology lectures in your combat medic training, this lecture will build upon prior instruction. Objective: To discuss/describe topics related to the nursing process. Importance: Nurses work in various health care settings so it is important to gain an understanding of this subject as it will apply to your clinical practice. Fit: Pain management is a primary concern for many patients you will care for as a nurse. Many diagnoses manifests with some form of pain or discomfort. Effective pain management can be directly related to quality of care, increased patient compliance with medical treatment, and a positive perception of care by the patient. Approach: You will be presented the subject in lecture format and will be tested using a written exam at a later date. Control Statement: If you have any questions during the lesson please feel free to ask. BODY 1. Teaching Point: Identify the action, uses, side effects, nursing considerations for selected nonnarcotic analgesics. Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Skill Lesson Learning Support: a. Non-narcotic Analgesics. (1) General information: (a) Group of drugs used to relieve pain without the possibility of physical dependency. (b) Also used as antipyretics (drugs that decrease body temperature) and anti-inflammatory drugs. (2) Examples: (a) Salicylates. (b) Nonsalicylates. (c) Nonsteroidal Anti-inflammatory Drugs (NSAIDs). b. Salicylates: 1 AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication (1) Action: (a) Relieve pain and inflammation by inhibiting prostaglandins. 1) Prostaglandins are fatty acid derivatives found in almost every tissue of the body and body fluid. 2) Release of prostaglandin is thought to increase the sensitivity of peripheral pain receptors. (b) Lower elevated body temperature by dilating peripheral blood vessels, which cools the body. (c) Aspirin also prolongs the bleeding time by inhibiting the aggregation (clumping) of platelets. (2) Examples: (a) Aspirin (Bayer, Ecotrin). (b) Magnesium salicylate (Extra Strength Doan's). (c) Sodium thiosalicylate (Rexolate). (3) Uses: (a) Relieve mild to moderate pain. (b) Reduction of elevated body temperature. (c) Treatment of inflammatory conditions. (d) Reduction of the risk of myocardial infarction in those with unstable angina-aspirin only. (e) Reduction of the risk of transient ischemic attacks in clients with a history of fibrin platelet emboli-aspirin only. (4) Side Effects: (a) Gastric upset, heartburn, nausea/vomiting, anorexia. (b) Gastrointestinal bleeding. (c) Salicylism (Salicylate toxicity): 1) Dizziness, tinnitus, impaired hearing. 2) Flushing, sweating. 3) Rapid breathing, tachycardia. 4) Mental confusion, drowsiness. 2 AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication 5) Respiratory depression and coma with large doses. c. Nonsalicylates: (1) Major drug classified as a nonsalicylate is acetaminophen. (2) Action: (a) Mechanism of action is not known. (b) Has analgesic and antipyretic activity, but no anti-inflammatory action. (3) Example: acetaminophen (Tylenol). (4) Uses: (a) Relieve of mild to moderate pain. (b) Reduction of elevated body temperature. (c) Used for its analgesia and anti-inflammatory properties in clients with aspirin allergies, bleeding disorders or on anti coagulation therapy. (5) Side Effects: (a) Adverse reactions usually occur with chronic use or when recommended dose is exceeded. (b) Skin eruptions, urticaria. (c) Hemolytic anemia, pancytopenia. (d) Hypoglycemia. (e) Hepatotoxicity, hepatic failure. (f) Acute acetaminophen toxicity- can occur with single dose. 1) Nausea/vomiting, confusion. 2) Liver tenderness, jaundice. 3) Hypotension, arrhythmias. 4) Acute hepatic and renal failure. d. Nonsteriodal Anti-inflammatory Drugs (NSAID): (1) Action: (a) Inhibit prostaglandin synthesis causing analgesic and anti-inflammatory activity. 3 AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication (b) Exact mechanism of action for NSAID antipyretic effect is unknown. (2) Examples: (a) Celecoxib (Celebrex). (b) Ibuprofen (Advil, Motrin, Nuprin). (c) Indomethacin (Indocin). (d) Ketorolac (Toradol). (e) Naproxen (Aleve, Naprosyn). (3) Uses: (a) NSAIDs have a wide variety of uses depending on the individual agent. (b) Relieve mild to moderate pain. (c) Reduction of elevated body temperature. (d) Treatment of inflammatory conditions. (4) Side Effects: (a) GI: Nausea/vomiting, diarrhea or constipation, epigastric pain, intestinal ulceration, stomatitis, jaundice. (b) CNS: Dizziness, anxiety, vertigo, drowsiness or insomnia, confusion, depression, psychic disturbances. (c) Cardiovascular: Congestive heart failure, blood pressure changes, cardiac arrhythmias. (d) Renal: Hematuria, cystitis, elevated BUN, polyuria, dysuria, acute renal failure. (e) Special senses: Visual disturbances, diplopia, photo phobia, tinnitus, taste changes,rhinitis. (f) Hematologic: Neutropenia, pancytopenia, aplastic anemia. (g) Skin: Rash, skin eruptions, Stevens-Johnson syndrome, ecchymosis. (h) Metabolic/endocrinologic: Decreased appetite, weight changes, glucose intolerance, flushing, sweating, menstrual disorders. (i) Other: Thirst, fever,chills, vaginitis. e. Nursing Assessment: 4 AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication (1) Non-narcotic Analgesics: (a) Assess type, onset and location of pain. (b) Examine the area of pain. (2) Salicylates: Give with food, milk or full glass of water to prevent GI upset. (3) Nonsalicylates (Acetaminophen): (a) Assess the overall health of the client and use of alcohol. Client with increase alcohol consumption and malnourished clients are at greater risk for hepatotoxicity. (b) May be taken with meals or on an empty stomach. Take with full glass of water. f. Patient Teaching: (1) Non-narcotic Analgesics: (a) Take medication exactly as prescribed. Do not increase or decrease the dose without advise from primary health care provider. (b) Take the drug with food or a full glass of water unless otherwise directed. If gastric upset occurs, take with food or milk. (c) Inform all health care providers of usage of the drug. (d) If pain persists more than 10 days or if fever persists more than 3 days, consult the primary health care provider. (2) Salicylates: (a) Reye's syndrome (a life threatening condition characterized by vomiting and lethargy progressing to coma) can occur in children and teenagers with influenza or chicken pox who take aspirin. (b) Salicylates often deteriorate more rapidly than other drugs. If there is a vinegar odor to the salicylate, discard the entire contents. Keep the container tightly closed. Salicylates deteriorate rapidly when exposed to air. (c) Do not take OTC medications that contain aspirin while taking salicylate. (d) If surgery or invasive dental procedure is anticipated, notify the primary health care provider or dentist. Salicylate may be discontinued 1 week before procedure related to possibility of postoperative bleeding. (3) Nonsalicylates: (a) In the case of arthritis, do not change from aspirin to acetaminophen without consulting the primary health care provider. Acetaminophen lacks the anti-inflammatory properties of aspirin. 5 AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication (b) Avoid the use of alcoholic beverages. (4) Nonsteriodal Anti-inflammatory Drugs: (a) Avoid the use of aspirin or other salicylate when taking an NSAID. (b) Drug may take several days to produce an effect (relief of pain and tenderness). (c) Use caution while driving or performing tasks that require alertness if drowsiness, dizziness or blurred vision occur. g. Older Adult Considerations: (1) Older clients are often prescribed these medications on long term basis for disease processes such as arthritis. This predisposes them for increased risk of gastrointestinal bleeding. (2) Caution the older client to take the medication with a full glass of water or with food to decrease the GI effects. (3) Nonsalicylates: Use acetaminophen cautiously in the older adult with liver damage. Knowledge Lesson: Question: Answer: Check on Learning In a knowledge lesson, pose questions to the class. Click here to enter the question. Click here to enter the answer. Skill Lesson: In a skill lesson, provide practice and watch students perform a skill. 2. Teaching Point: Identify the action, uses, side effects, nursing assessment and patient teaching for selected narcotic analgesics. Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Skill Lesson Learning Support: a. Narcotic Analgesics: are divided into two classes: (1) Narcotic analgesics obtained from raw opium: called opioids. (a) Examples: 1) Morphine 2) Codeine 6 AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication 3) Hydromorphone (Dilaudid) 4) Oxymorphone (Numorphan) 5) Oxycodone 6) Heroin (2) Synthetic narcotic analgesics. (a) Examples: 1) Butorphanol (Stadol) 2) Merperidine (Demerol) 3) Propoxyphene (Darvon) b. Action is a complex physiologic and pharmacologic process: (1) A neurotransmitter is released by the pain (opiate) receptors that allow the pain impulse to go to the brain where it is interpreted. (2) The enkephalins and endorphins attach to pain (opiate) receptor sites and prevent the release of the neurotransmitter that carries the pain impulse. (3) Narcotic agonists occupy the same opiate receptors as do the endokephalins and endorphins thereby reducing the sensation of pain. (4) Administration of a narcotic analgesic elevates the pain threshold and alters the client's perception of pain. (5) Sedation action of narcotics reduces the anxiety that accompanies pain thereby enhancing the analgesic activity of the drug. c. Uses: (1) Relief of pain. (2) Treatment of severe diarrhea and intestinal cramping. (3) Relief of severe, persistent cough (codeine). (4) Dsypnea associated with acute left ventricular failure and pulmonary edema (Morphine). (5) Preoperatively to lessen anxiety and sedate the client. This allows for use of less anesthesia and it is easier to maintain the client under anesthesia. (6) Detoxification and maintenance for the client addicted to narcotics (Methodone). 7 AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication d. Side Effects: (1) Major complication: Respiratory depression with a decrease in respiratory rate and depth. (2) Most frequent adverse reactions: Light-headedness, dizziness, sedation, constipation, anorexia, nausea/vomiting, sweating. (3) Other side effects: (a) CNS: Euphoria, pinpoint pupils, agitation, tremors, impairment of mental tasks. (b) GI: Dry mouth, biliary tract spasms. (c) Cardiovascular: Flushing of the face, tachy/bradycardia. (d) GU: Spasm of the ureters and bladder sphincter, urinary retention or hesitancy. (e) Physical dependency. e. Nursing Assessment: (1) Obtain nursing health history and physical, allergy history, past and present drug therapies. (2) Assess pain: Type, intensity, location. (3) Obtain vital signs. (4) PCA: Patient Controlled Analgesia: (a) Allows clients to administer their own pain medication by means of an IV pump. (b) Preset limits and controls prevent client from administering too much medication. (c) Assess client's understanding and ability to use the PCA method. f. Patient Teaching: (1) Explain the name of the medication, the purpose of the medication, how often it can be administered. (2) PCA: (a) Location of the control button that activates the administration of the medication. (b) Machine regulates the dose of the drug as well as the time interval between doses. (c) If the control button is used too soon after the last dose, the machine will not deliver the drug until the time has lapsed and the button is pushed again. (d) Pain relief should occur shortly after pushing the button. 8 AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication (3) General points: (a) Drug may cause drowsiness, dizziness and blurring of vision. Use caution when driving orperforming tasks requiring alertness. (b) Avoid the use of alcoholic beverages while taking this medication. Alcohol may intensify the action of the drug and cause extreme drowsiness or dizziness or even death. (c) Take drug as prescribed. Do not increase dosage unless advised by health care provider. (d) If GI upset occurs, take the medication with food. (e) Withhold the narcotic analgesic and contact the primary health care provider immediately if any of the following are present. 1) A significant decrease in respiratory rate or a rate of 10/min or below. 2) A significant increased or decrease in pulse rate, or a change in pulse quality. 3) A significant decrease in blood pressure (systolic or diastolic) or a systolic pressure below 100 mm hg. Knowledge Lesson: Question: Answer: Check on Learning In a knowledge lesson, pose questions to the class. Click here to enter the question. Click here to enter the answer. Skill Lesson: In a skill lesson, provide practice and watch students perform a skill. 3. Teaching Point: Identify the action, uses, side effects, nursing assessment and patient teaching for selected narcotic antagonist. Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Skill Lesson Learning Support: a. Action: (1) Antagonists are used to reverse the respiratory depression associated with the opiates. (a) Competes for opiate receptor sites. (b) If the client has received an opiate, the effects are reversed. 9 AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication (c) If the client has not received an opiate, the drug has no drug activity. (2) Examples: (a) Naloxone (Narcan) (b) Naltrexone (Depade) b. Uses: (1) Naloxone: (a) Complete or partial reversal of narcotic depression, including respiratory depression. (b) Capable of restoring respiratory function within 1-2 minutes after administration. (2) Naltrexone: (a) Used in the treatment of client dependent on opioids. (b) Blocks the euphoric effects experienced in opiate dependence. Note: Give Naltrexone with caution and only when necessary in patients receiving a narcotic for severe pain. Naloxone remove all the pain-relieving effects and may lead to withdraw symptoms or the return of pain. c. Side Effects: (1) Naloxone: Abrupt reversal of narcotic depression may result in: (a) Nausea/vomiting. (b) Sweating. (c) Tachycardia. (d) Increases blood pressure. (e) Tremors. (2) Naltrexone: (a) Anxiety, difficulty sleeping, dizziness, irritability, drowsiness, depression. (b) Abdominal cramps, nausea/vomiting. (c) Nasal congestion. (d) Joint and muscle pain, fatigue. 10 AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication d. Nursing Assessment: (1) Client receiving narcotic antagonist for respiratory depression: (a) Obtain vital signs. (b) Record the drug suspected of causing the over dosage. (c) Monitor the client for return of pain or respiratory depression. (2) Client receiving a narcotic antagonist for treatment of opoid dependency. (a) Obtain a complete drug history. (b) Complete a nursing history and physical. e. Patient Teaching: (1) Client taking naltrexone should be instructed to wear or carry identification. Narcotics administered to these clients will have no pain relieving effect. (2) Narcotic Analgesics: Older clients are especially prone to adverse reactions to these medications, particularly depression and confusion. Lower doses may be indicated. END OF LESSON TEST Allocated Time: Instructions: Test Questions or Performance Expected: Test Key: 0 Minutes CONCLUSION Allocated Time: Summary: 5 Minutes Review and re-emphasize the difficult Teaching Points below. 1. 2. 3. Closing Statement: 11 Identify the action, uses, side effects, nursing considerations for selected nonnarcotic analgesics. Identify the action, uses, side effects, nursing assessment and patient teaching for selected narcotic analgesics. Identify the action, uses, side effects, nursing assessment and patient teaching for selected narcotic antagonist. You will be presented the subject in lecture format and will be tested using a written exam at a later date. AFAMS Master Lesson Plan (MLP) Nursing Program Pain Medication Re-motivating Statement: 12 Pain management is a primary concern for many patients you will care for as a nurse. Many diagnoses manifests with some form of pain or discomfort. Effective pain management can be directly related to quality of care, increased patient compliance with medical treatment, and a positive perception of care by the patient.