Theme - 4 First aid in Emergency InWEnt
advertisement

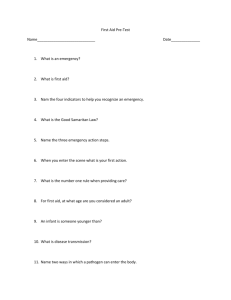
Theme - 4 First aid in Emergency For further information Contact: Disaster Management Institute Paryavaran Parisar, E-5, Arera Colony, PB No. 563, Bhopal-462 016 MP (India), Fon +91-755-2466715, 2461538, 2461348, Fax +91-755-2466653 dmi@dmibhopal.nic.i n www.dmibhopal.nic.in July 2010 5.03-0008-2010 InWEnt International Weiterbildung und Entwicklung gGmbH Capacity Building International, Germany Friedrich-Ebert-Allee 40 53113 Bonn Fon +49 228 4460-0 Fax +49 228 44601766 www.inwent.org Imprint MoEF Chief Editor Praveen Garg, IAS, Executive Director, DMI, Bhopal, India Editors Dr. Rakesh Dubey, Director, DMI, Bhopal, India Florian Bemmerlein-Lux, Sr. Advisor, InWEnt, Germany Support Sudheer Dwivedi, Dy. Director, DMI, Bhopal, India Dr. Asit Patra, Asstt. Director, DMI, Bhopal, India Neeraj Pandey, Content Manager, InWEnt India Amit Kumar Dadhich, Content Manager, InWEnt India Huda Khan, Content Manager, InWEnt India COOPERATIONREPUBL IC INDIA FEDERAL REPUBLICOF GERMANY Published under InWEnt International Weiterbildung und Entwicklung gGmbH Capacity Building International, Germany Division for Environment, Energy and Water Lützowufer 6-9, 10785 Berlin, Germany Dr. Christina Kamlage Phone +49 30 25487-117 christina.kamlage@inwent. org Steffi Mallinger Phone +49 30 25487-116 steffi.mallinger@inwent.or g Disaster Management Institute Paryavaran Parisar, E-5, Arera Colony, PB No. 563 Bhopal-462 016 MP (India), Fon +91-755-2466715, 2461538, 2461348, Fax +91-755-2466653 www.hrdp-iDRM.in GTZ ASEM Advisory Service in Environmental Management A-33, Gulmohar Park, New Delhi 110049 Fon +91-1126528840 Fax +91-1126537673 www.asemindia.com Disclaimer Though all care has been taken while researching and compiling the contents provided in this booklet. DMIInWEnt-gtz-ASEM accept no liability for its correctness. The reader is advised to confirm specifications and health hazards described in the booklet before taking any steps, suitability of action requires verifications through other sources also. Information provided here does not constitute an endorsement or recommendation. in ent GermanyCapacity Building Internationale InWEnt - Qualified to Shape the Future InWEnt-gtz-ASEM Capacity Development Programme for industrial Disaster Risk Management (iDRM) Edition 1, 2010 OF The Ministry of Environment & Forests (MoEF) is the nodal agency in the administrative structure of the Central Government for the planning, promotion, coordination and overseeing the implementation of India’s environmental and forestry policies and programmes. The Ministry also serves as the nodal agency in the country for the United Nations Environment Programme (UNEP), South Asia Co-operative Environment Programme (SACEP), International Centre for Integrated Mountain Development (ICIMOD) and for the follow-up of the United Nations Conference on Environment and Development (UNCED). The Ministry is also entrusted with issues relating to multilateral bodies such as the Commission on Sustainable Development (CSD), Global Environment Facility (GEF) and of regional bodies like Economic and Social Council for Asia and Pacific (ESCAP) and South Asian Association for Regional Co-operation (SAARC) on matters pertaining to the environment. COOPERATION REPUBLIC OF INDIA FEDERAL REPUBLICOF GERMANY InWEnt - Capacity Building International, Germany, is a non-profit organisation with worldwide operations dedicated to human resource development, advanced training, and dialogue. Our capacity building programmes are directed at experts and executives from politics, administration, the business community, and civil society. We are commissioned by the German federal government to assist with the implementation of the Millennium Development Goals of the United Nations. in addition, we provide the German business sector with support for public private partnership projects. Through exchange programmes, InWEnt also offers young people from Germany the opportunity to gain professional experience abroad. Detailed Information can be explored using our WEB sites: www.inwent.org gtz-ASEM The Advisory Services in Environmental Management (ASEM) Programme, is a joint programme of the German Technical Cooperation (GTZ) and the Indian Ministry of Environment and Forests (MoEF). The German Federal Ministry for Economic Cooperation and Development (BMZ) supports several environment related projects in India through GTZ. ASEM focuses on seven major thrust areas -Sustainable Industrial Development, Sustainable Urban Development, Sustainable Consumption and Consumer Protection, Sustainable Environmental Governance and the cross cutting areas. Climate Change and Human Resource Development. Public Private Partnership (PPP) project with Indian and German companies contribute towards identified project activities. Detailed Information can be explored using our WEB sites: www.asemindia.co m www.hrdp-net.in Disaster Management Institute (DMI) Bhopal The Disaster Management Institute (DMI) was set up in 1987 by the Government of Madhya Pradesh (GoMP) as an autonomous organization in the aftermath of the industrial disaster in Bhopal. Since inception, DMI has built vast experience in preparation of both On-site and Off-site Emergency Management Plans, Safety Audit, Risk Analysis and Risk Assessment, Hazard and Operability Studies (HAZOP), etc. The National Disaster Management Authority (NDMA) constituted under the chairmanship of the Prime Minister selected DMI as a member of the Core Group for preparation of the National Disaster Management Guidelines- Chemical Disaster. It is a matter of pride that NDMA has selected DMI for conducting Mock Exercises on chemical (industrial) Disaster Management at key industrial locations in the country. The Ministry of Environment and Forests, InWEnt and gtz-ASEM Germany have recognized DMI as a Nodal Training Institutes for capacity building in industrial Disaster Risk Management. www.HRDP-iDRM.in Contents It's an old saying that ”An Ounce of Prevention, is Worth a Pound of Cure”, especially in an emergency situation when seconds count. Here are a few selected first aid tips that may be useful in a disaster situation!! 1. Why it is needed -2 2. What is First aid -3 3. Principles of First aid -5 4. Emergency situations -7 Warning about the module This module is made to educate the readers who are involved in chemical emergency management. This module does not recommend any one to take first aid steps what have been discussed herewith unless he/she is trained first aid trainer or volunteer after having qualified training from either Red Cross or St. Johns ambulances or any other govt approved agency. 4.1. Respiration -7 4.2. Asphyxia -8 4.3. Poisoning - 15 4.4. Burns - 18 5 First aid kit - 22 6 Elements of training in First aid - 25 6.1. Teaching Methods - 25 6.2. Assessing the scene and the Victim(s) - 25 6.3. Responding to Life-Threatening Emergencies - 26 6.4. Responding to Non-Life-Threatening Emergencies - 27 7 Conclusion - 28 8. Glossary - 30 9. References - 31 1 1. Why it is needed First aid is emergency care provided for injury or sudden illness before emergency medical treatment is available. The first-aid provider in the workplace is someone who is trained in the delivery of initial medical emergency procedures, using a limited amount of equipment to perform a primary assessment and intervention while awaiting arrival of emergency medical service (EMS) personnel. A workplace first-aid program is part of a comprehensive safety and health management system that includes the following four essential elements: Management Leadership and Employee Involvement Worksite Analysis Hazard Prevention and Control Safety and Health Training The purpose of this module is to present a summary of the basic elements for a first-aid program at the workplace. Those elements include: Identifying and assessing the workplace risks that have potential to cause worker injury or illness. Designing and implementing a workplace first-aid programme that: -Aims to minimise the outcome of accidents or exposures -Complies with essential provisions of regulations -Includes sufficient quantities of appropriate and readily accessible first-aid supplies and first-aid equipment, such as bandages and automated external physical and medical support. -Assigns and trains first-aid providers, who receive first-aid training suitable to the specific workplace and receive periodic refresher courses on first-aid skills and knowledge. 2 -Instructs all workers about the first-aid programme, including what workers should do if a co-worker is injured or ill. Putting the policies and programme in writing is recommended to implement this and other programme elements. -Provides for scheduled evaluation and changing of the first-aid programme to keep the programme current and applicable to emerging risks in the workplace, including regular assessment of the adequacy of the first-aid training course. 2. What is First-aid First aid is the immediate care given to a person who is injured or ill. Sudden illness or injury can often cause irreversible damage or death to the victim unless proper care is initiated as soon as possible. First aid includes identifying a life-threatening condition, taking action to prevent further injury or death, reducing pain, and counteracting the effects of shock. Because life-threatening situations do occur, everyone should know how to provide emergency care until a victim can be treated or transported to a medical facility. First aid is not intended to replace care by a physician or surgeon. Its intent is to protect the victim until medical assistance can be obtained. The primary purpose of first aid is to: Care for life-threatening situations Protect the victim from further injury and complications Arrange transportation for the victim to a medical facility Make the victim as comfortable as possible to conserve strength Provide reassurance to the victim An accident can occur at any time or any place where hazardous chemicals are being used and the working conditions are not safe. If you are the first person to arrive and 3 see some accident, there are a few basic principles you should follow to protect yourself and the victim. The following steps are required immediately: 1. Survey the Scene. Before you help the victim, determine if the scene is safe. If anything dangerous is present, don't put your own life at risk to try and help the victim; you will be of no aid if you become a victim too. Summon help and wait for trained people to resolve the situation. If the scene is safe, try and determine what happened and how many victims there may be. Never move the victim unless an immediate, life threatening danger exists, such as a fire or the threat of a building collapse. 2. Primary Victim Survey. After ensuring the scene is safe, you can turn your attention to the victim. Begin by performing a primary survey to determine if the victim: A) is conscious B) has an open, unobstructed airway C) is breathing D) has a heartbeat E) is not bleeding severely To check for consciousness, gently tap the person and ask if they are okay. If there is no response, this in an indication that a possible life-threatening situation may exist. If the person is responsive and can talk or cry, this indicates they are conscious, breathing, have an unobstructed airway, and a pulse. If the victim is unconscious, kneel down next to the head and check for the ABC's: Airway, Breathing, and Circulation. To check the Airway (clear and maintain an open airway), Breathing (restore breathing), and Circulation (restore circulation), place your ear next to the victim's mouth and listen/feel for breath sounds while looking for a rise and fall of the chest. While doing this, check for a pulse by placing your fingers on the neck, just below the angle of the jaw, and feel for the pulse from the carotid artery. These three steps will determine if cardiopulmonary resuscitation (CPR)is needed. 4 3. Principles of First aid The Gurumantra (thumbrule) of First aid is opting the point wise followings: R is for Responsiveness which means that we have to check the following: Is the victim conscious? Touch their shoulder, ask if they are alright. Ask if they need help. If they say no, then proceed no further. If yes, or no response, then proceed to A breathing, they may need their head repositioned. If they are still not breathing they need rescue breathing, do not give unless you are trained, instead, find an adult. RAPABCH. To make it convenient we are C is for circulation If there is not a pulse, then this person needs CPR. The best place to check for a pulse is the carotid artery along the side of the neck along the windpipe. If you are not trained in CPR, then find someone who is. H is for hemorrhaging If the victim is bleeding, then provide the necessary care. If not, then begin a secondary assessment. A summary of the first aid can be briefed in Fig-1: A is for Activate Emergency Management Services (EMS), in India recently the 108 has started in jointly with health and police department. Please see what emergency management services number is available in your area. What are the four things you need to remember when making an EMS call? And therefore the following points are suggested: YES IS THE CASUALTY CONSCIOUS? Your name and contact number The emergency The location of the emergency condition of the victim Check the victim for responsiveness. If he do not respond or if he tells you that he need help, ask what need, to be contacted, when and where? Some very basic question and stay till EMS arrives to take care of victim NO 5 IS THE CASUALTY BREATHING? NO P is for Position IS THERE PULSE? Only re-position the victim if the victim is in further danger in their present location and / or there does not seem to be spinal injury and additional care requires moving them. NO DIAL FOR HELP. GIVE ARTIFICIAL RESPIRATION AND EXTERNAL MASSAGE ARRIVES. Explain when an injured person should and should not be moved? If there are suspected spinal injuries, do not move the victim (except when the victim is in a life threatening situation). Four Steps of Victim Assessment is important and it should be conducted by the use of the “ABCH” A is for airway and check to see if the airway is blocked by: Use your finger to sweep the mouth to remove any seen object. If this fails, then perform the Heimlich manoeuvre or abdominal thrusts. B is for breathing Look, listen and feel by watching the chest and placing your cheek a few inches above the mouth of the victim to sense any movement of air. If the victim is not 6 TILL CARDIAC HELP TREAT ANY INJURIES GET HELP IF NECESSARY YES IS THE CASUALTY BREATHING NOISILY? YES OPEN AND CLEAR AIRWAY NO YES TREAT ANY LIFE THREATENING INJURIES. PLACE CASUALTY IN RECOVERY POSITION AND CALL FOR HELP. GIVE BREATHS OF ARTIFICIAL RESPIRATION DIAL FOR HELP CONTINUE RESPIRATION ARRIVES Fig-1 TILL ARTIFICIAL HELP 7 4. Emergency situations Now in the following paragraphs some of the emergency situations are being discussed from first aid angle: 4.1 Respiration Respiration means breathing in and breathing out of air. It helps in supply of oxygen (of the air) to all parts of the body. Breathing contains three phases: Breathing in (inspiration). Breathing out (expiration). Pause. Respiratory system: Air passage. Lungs. Air passage: Air passage consists of nose, mouth, throat (pharynx), the windpipe (trachea), and the air tubes (bronchi). The bronchi divide in to minute branches (bronchioles), which end in the lung substance (alveoli). Lungs: Two in number. Situated on right & left sides of chest cavity. Made up of small sacs (alveoli). Covered by a membrane called pleura, which lines the inner wall of the chest cavity. Mechanism of respiration: Inspiration: -Diaphragm contracts and flattens. (this increases chest cavity, above downwards) -Ribs move upward and forward due to contraction of intercostals muscles. (this increases the chest cavity from and to back). -Due to this lungs expansion, volume of the lungs increases and pressure inside the lungs decreases. At a point when the pressure in lungs is less than the atmospheric pressure, air enters from atmosphere in to the lungs. Expiration: -Diaphragm relaxes and comes back to its original state. =Intercostal muscle relaxes and ribs also come back to the original state. -Lungs being elastic and spongy, it comes back to the original state. -Volume of lungs decreases and pressure in lungs increases. So air is pushed out. Exchange of gases: This occurs in capillaries surrounding the alveoli. Oxygen is absorbed by red blood corpuscles (RBC) and water vapour and carbon-dioxide is let out from the blood plasma into the alveoli, which is expelled during expiration. Respiratory centre: Lungs are supplied with nerves, which are connected to the respiratory centre in brain. This controls respiration. It determines the rate and depth of respiration. Respiratory rate: Average adult- 16 to 18 times (per minute). Children - 20 to 30 times (per minute). This varies during stress, exercise, injury, illness, etc. Heart rate will accordingly increase to carry the extra oxygen around the body. CLINICAL DEATH BIOLOGICAL DEATH - O MINUTES. BREATHING AND CIRCULATION STOPS. LETHAL BRAIN DAMAGE - 4 TO 6 MINUTES. - 10 MINUTES. BRAIN CELLS DIE. 4.2 Asphyxia Asphyxia is a condition where lungs do not get sufficient supply of air for breathing. Causes:affecting air passages. Spasm: Food, water, irritant gases (coal gas, exhaust fumes, smoke, etc.), sewage gas, gas in unused wells, etc., entering air passage, bronchial asthma. 8 Obstruction: Due to foreign body, falling back of tongue in case of unconscious patient, swelling of tissues of throat (scalding, burns, corrosives, etc.). Continue till normal breathing sets. Prevent damage to brain and other vital organs. Artificial respiration. External cardiac compression. Keep body warm by light blanket. Provide shelter. Compression: Strangulation, smothering, throttling. Affecting respiratory mechanism: Epilepsy, tetanus, rabies. Paralysis of chest wall, diaphragm (polio, poisoning, etc). Different kinds of asphyxia: Drowning: Water (any other liquid) enters in to air passage and clogs the lungs. Affecting respiratory centre: Morphine, sleeping tablets, electric shock, stroke, etc. Management: Drain the fluid from lungs. Give artificial respiration. Compression of chest: Fall on earth, wall, etc. Crushing against wall (stampede, etc). Lack of oxygen at higher altitude and lower atmospheric pressure. Acclimatisation (gradualascent is necessary). Treatment: Act quickly. Remove foreign bodies from throat and nose. Start artificial respiration (even while in water). Put the casualty face down and head to one side and arms stretched beyond his head. Infants or child can be held upside down for a short period. Raise middle part of the body with your hands round the belly. This will help in draining out water. Give artificial respiration till breathing becomes normal. Remove wet clothing. Keep body warm. If conscious, give hot drinks. Don't allow to sit. Shift to hospital as stretcher case. Signs and symptoms: First phase: Breathing rate increases. Short breathing. Swollen neck veins. Face, lips, nails, tongue, and toes turning blue (cyanosis). Fast and feeble pulse. Second phase: Semiconsciousness or unconsciousness. Froth in mouth and nostrils and Fits. Management: Remove the cause or remove the casualty from the cause. Ensure open airway. This enables air to reach the lungs. Open airway Support the nape of neck on your palm and press the head backwards. Press the angle of the jaw forward from behind. (this extends the head on the neck and lifts the tongue to clear off the airway). If airway is clear, the casualty gasps and starts to breathe. Give 3 or 4 inhalations by 'mouth-to-mouth method. Strangulation, hanging, throttling: Pressure from outside the air way and obstructs air way. Hanging: Suspension of body by a noose. It can also cause fracture in spine causing damage to spinal cord. Strangulation and throttling: Airway is blocked due to tight contraction or intentional squeezing of person's throat. 9 10 Management: Cut and remove the band contracting the throat, supporting the weight of the body in case of hanging (cut below the knot). 'ABC' of resuscitation. Put in recovery position after recovery. Shift to hospital. Choking: It is due to obstruction of windpipe. Common in children. Signs and symptoms: -General signs of asphyxia. -Unable to speak or breathe. -Gripping of throat. -Congestion of face and neck, etc. With prominent veins. Grasp your fist with the other hand. Pull both hands towards you with quick inward and upward thrust so that upper abdomen is compressed. Repeat 4 times if needed. In case of unconscious patient: -Lay the patient back with head in open airway position. -Kneel astride the patient's thigh. -Place heel of one hand in the centre of patient's upper abdomen and cover with other hand, with fingers clear of abdomen. -Press with both arms straight into the abdomen with quick inward and upward thrust. -Repeat if needed, for 4 times. In children: Make the child sit on your lap. Give abdominal thrust with one hand, with less pressure. Infant: -Place on firm surface. -Press the upper abdomen with two fingers, with less pressure. Management: Remove the obstruction. Shift to hospital. Treatment: Remove any visible obstruction by hooking out with your fingers. Encourage patient to cough. If not cleared, bend the casualty head lower than lungs. Slap between shoulder blades with the help of hands, four times. Check the mouth and remove the foreign body if dislodged. If not, perform abdominal thrust four times. Remove the foreign body, if dislodged. If not, repeat slapping, checking mouth & abdomen thrusts, till obstruction is removed. Swelling within throat: Due to drinking of very hot liquids, corrosive poisons and inflammation. Management: Give ice to suck or cold water sip. Give butter, olive oil and liquid paraffin, orally. Apply cloth wrung out of hot water, to the front of neck. Give artificial respiration if needed. Suffocation by smoke: Protect yourself by a towel or wet cloth over mouth and nose. Keep low and remove the casualty quickly. Give artificial respiration if breathing stops. In children: Hold upside down and smack on the back 2 or 3 times. If not successful lay the child prone with head hanging over the knee & give sharp smacks, between the shoulder blades. Induce vomiting by introducing two fingers into the throat. Abdominal thrust: Applying series of thrust to upper abdomen, to force air out of choking lungs. Stand or kneel behind the casualty. Put one arm around the patient's abdomen and clench your fist and place it with your thumb inwards in the centre of upper abdomen 11 Suffocation by poisonous gases: Carbon monoxide [CO] (lighter then air) -Ensure fresh air. -Opening doors and windows if there is no fire. -Before entering to rescue the patient, take deep breath and hold. -Crawl along the floor. -Remove to fresh air. -Loosen clothing. -Give artificial respiration. Carbon-dioxide [CO2](heavier then air) 12 In coal-mines, deep unused wells, sewages, other gases emitted from leaking refrigerators, LPG, etc. Continue artificial respiration till normal breathing resumes. Note: Artificial respiration can be given even if breathing is there, but not normal. Management: Same as above Bronchial asthma: Due to sudden contraction of air way, due to allergy, infection, anxiety. If heart also not working: Signs: Face will be pale or blue. Dilated pupils. Heart beat and pulse will be absent. Management: Reassure the patient to sit up and lean forward with a table or pillows to lean. Open windows for fresh air. Shift to hospital. Management: Lay casualty on back on a hard surface (bench, table, etc). Give a hit, with edge of your hand on the lower and left angle of the sternum. This usually stimulates the heart. If heart does not work, persist striking for 10-15 times, at the rate of 1 strike/second. If hear beat starts, then stop striking. Continue artificial respiration side by side. If heart does not function, start ECC. Artificial respiration: Best method - mouth to mouth or -Mouth to nose breathing. Other methods are: -Sylvester's method. -Holger nelson method. -Schafer's method. Mouth to mouth method: Place the casualty on his back. Hold the head tilted back. Take deep breath with your mouth wide open. Keep the casualty's nose pinched. Cover the mouth of casualty with your mouth smugly. (cover mouth with clean cloth if possible). Blow on to the lungs and watch chest raise. Withdraw your mouth and watch chest falling back. Repeat at the rate of 15 to 20 times per minute. Note: In case of small children, the open mouth should cover the mouth and nose and blow gently. Rate 18-22 per minute. If chest does not rise on blowing: Suspect obstruction. Ensure open air way. Remove any obstruction by thumping on back, etc. If mouth-to-mouth is not possible, use mouth to nose method, but mouth should be kept closed. 13 External Cardiac Compression (ECC): Note: - thumping the heart or ECC should not be done until the heart has stopped beating. Feel and mark the lower part of sternum. Place heel of hand, two fingerbreadth above the joint of rib margin and breastbone. Place heel of other hand over it. With arms straight, press sternum backward (about 4 to 5 cms. In adults) and release. Compression must be regular, smooth, not jerky or jabbing. Rate: Adults - above 60 per minute. Children (2 to 10 years) - above 80 to 90 but with one hand. Children (0 to 2 years) - 100 per minute only with finger. If two trained people are there: Person giving artificial respiration should be on right side, near the head and one giving ECC on the left, at the level of the middle of the chest. Give two inflation and check. If there is no heartbeat, give 5 compressions at rate of 80 compressions per minute. Give single inflation on the upstroke of every fifth compression. Continue till recovery. 14 Signs of effective treatment: Colour will become normal. Pupils will contract. Carotid pulse is felt. If only one trained person is available: Artificial respiration and ECC is done alternatively by shifting position. 15 compressions at the rate of 80 per minute, followed by two breaths of mouth-tomouth method. Check pulse after first minute and then every three minutes, till pulse is felt. Stop ECC, as soon as pulse is felt. Continue, mouth-to-mouth respiration till breathing becomes normal. Put in recovery position after the recovery. 4.3 Poisoning Poison: A poison is a substance that, if taken into the body in sufficient quantity, can cause temporary or permanent damage. Types of poisons: 1. Ingested poison: eating or drinking poisonous substances. (Rat poison, poisonous plants, etc.) 2. Absorbed poison: Absorbed through skin. (Insecticides) 3. Inhaled poison: Chemical vapours. (Sprays, cleaning fluids, etc.) Fumes from fire, stoves, exhausts, sewer gases, etc. 4. Injected poison: Insect bites. (Spiders, wasps, etc.), Snake bite, etc. 5. Drugs. Signs and symptoms: -Unconsciousness or altered behaviour. -Shortness of breath. -Cough. -Abnormal pulse. -Burning eyes, mouth, nose, throat, chest, etc. -Severe headache. -Nausea & vomiting. -Reddening of lips. (in carbon monoxide poisoning) Treatment: -Remove the patient from the spot. -Open airway. -CPR if needed. -Remove contaminated clothing, carefully. -Provide intensive First aid, if possible. -Shift to hospital. Acts as Corrosive or irritant. Suffocating agent displacing oxygen. symptoms Treatment: -Open airway. -Dilute poison with water or milk. -Induce vomiting with syrup ipecac, soap & water, etc. (except if patient is unconscious, ingested corrosives, gasoline products, etc.) -Ensure patient does not aspirate vomitus. -Give one tablespoon of powdered charcoal or white of egg. -Antidote, if known & available, can be given. -Transport to hospital in lateral recumbent position. Inhaled poison: Effects: Depends on the nature, concentration and how it enters the body. Signs, -Unusual odours of breath, on clothing or at the scene. (garlic smell rat poison) -Abnormal breathing. -Abnormal pulse. -Sweating. -Dilated or contracted pupils. -Excess salivation or foaming from the mouth. -Painful swallowing. -Distension, pain & tenderness of abdomen. -Nausea & vomiting. -Diarrhoea. -Convulsions. -Altered state of consciousness. and management: Ingested poison: Signs and symptoms -Burns and stains around the mouth. 16 15 Injected poison: Absorbed poison: Signs and symptoms: -Noticeable stings or bites. -Localised pain or itching or burning sensation. -Swelling or blistering at the site. -Weakness or collapse. -Abnormal pulse and breathing. -Headache. -Dizziness. -Nausea & vomiting. -Muscle cramps, chest tightening & joint -Excessive salivation, sweating, etc. -Anaphylactic shock. Signs and symptoms: -Skin reactions. -Itching. -Irritation of eyes. -Headache. -Increased relative skin temperature. -Anaphylactic shock. Treatment: -Remove the patient from the spot. -Brush off any dry material. -Wash the area with plenty of water and soap, if available. -Remove all contaminated clothing, shoes, jewellery, etc. -Shift to hospital. Treatment: -Treat for shock. -Scrap away bee or wasp stingers & veno -Place ice bag over the sting area. Points to be remembered while handling poisonous cases: Look for evidence. Get details from the patient or others. Retain any left over poison, bottle or any container, etc. This will help in identification. Retain the vomitus, stained clothing, dead snake, insects etc. This will help to identify the poison. While rescuing a person, take all safety precautions, before attempting. In snake bite: Signs and symptoms: -Noticeable bite on skin. -Pain & swelling over the bite area. -Rapid pulse & laboured breathing. -Progressive general weakness. -Vision problems.(dim or blurred) -Nausea or vomiting. -Convulsions. -Drowsiness or unconsciousness. -Bleeding (in viper bites) 4.4 Burns Burns are caused by extremes of temperature (hot or cold), chemicals or radiation. Types of Burns: Treatment: -Keep patient calm. -Clean the area with soap & water. -Treat for shock. -Remove constrictive items on the bitten extremities. -Immobilise bitten extremities. -Keep bite area at the level or at a lower level from the heart. -Apply constrictive band above and below the wound. -Avoid cutting over the wound and shift to hospital. 1.Dry burns: Caused by dry heat, like fire, flame, hot metal, high tension electric current, lightening, friction, etc. 2.Scalds: Caused by moist heat like boiling water, steam, oil, hot tar, etc. 3.Cold Burns: Caused by metals in freezing condition, liquid oxygen, liquid nitrogen, etc. 17 18 4.Chemical Burns: Caused by strong acids like Sulphuric Acid, Nitric Acid, etc., strong Alkalis like Caustic Soda, Potash, Quick Lime, etc. 5.Electrical Burns: Caused by high tension electric current. 6.Radiation Burns: Caused by exposure to Sun, X-Rays, and radiation after Nuclear explosion, etc. Second Degree Burn Classification of Burns: First degree (Superficial Burns) -Skin reddening seen. Second degree (Intermediate Burns) -Blister formation is seen. Third degree (Deep Burns) -Destruction of deeper tissues and scaring seen. Severity of Burns: This is judged by the area of burns rather than the degree of burns. Superficial burns affecting larger area is more dangerous than third degree burns affecting a smaller area. Area of burns is judged by “rule of nines”. Burns are considered to be critical, when: -Area of second degree burns is > 30 %. -There is third degree burns of face, groin, hand, feet or major joints. -Third Degree Burns > 10 %. -It is associated with other complications affecting respiration, etc. The photos as shown below and in next page show the types of burns. First, second and third degree burns need to be reviewed in the chemical (industrial) emergency before any type of medical treatment. Victims should be decontaminated first. Third Degree Burn Complications due to burns: Damage to tissues. Scars & disfigurement seen later. Loss of plasma, resulting in decrease in blood volume. Shock. Respiratory problems. Sepsis. Death. Dangers due to fire How to help a person whose clothes have caught fire? Put out flames using water or whatever means available. Water is best since it quenches the flames & also cools the burnt area so that the damage is minimised. Don't allow the person to run about. Hold a wet rug in front of you, while approaching. Lay him down & wrap tightly with a cloth so as to smother the flames. If the clothes in front have caught fire, lay him on his back & vice versa, till suitable material is brought to smother the flame. First Degree Burn 19 20 How to rescue a person from fire? Clean air will be at ground level. So crawl along the floor to pull out the person. Tie a wet kerchief round your face, to prevent inhalation of smoke. Act quickly. Don't open the windows. Management: In minor cases: Pour cold water. If water is not available, use any cold harmless liquid like milk, etc. Remove any material of constrictive in nature, like rings, watches, belts, shoes, etc. Apply clean dressing. Don't break blisters or remove any loose skins. Don't apply any ointments. Don't apply adhesive dressings. In Severe Cases: Lay casualty down. Pour water. Protect the burnt area from contact with the ground. Gently remove any rings, watches, etc. Carefully remove any clothing soaked in boiling liquid. Cover the injured area with sterile dressing and secure. Don't remove anything that is sticking to the burnt area. Don't break blisters. Don't apply ointments, Immobilise badly burnt limbs. Give oral rehydration fluids, if person is conscious. If unconscious, open airway & check breathing. Complete “ABC” of resuscitation and then put in recovery position. Shift to hospital. Burns in the mouth and throat: (Usually Chemical Burns or Scalds) Swelling of mouth, tongue, throat, etc. Can cause airway obstruction. So treat accordingly. Sun burns: Remove to shady cool place & bathe with cool water. Cover with sterile dressing. Treat for general effects of over heating. Shift to hospital. Prevention of burns: Stoves should be kept at a higher level. Avoid free hanging clothes. Avoid using clothes made of nylon or similar fibres, which can catch fire quickly. Better use cotton. Never open Fire unattended in hazardous area. Restrict entry of local ignition sources in hazardous area. Never keep combustible material near to open or direct flame or sources of heat. Keep Inflammable materials safe. 5. First aid kit Tips for making First aid kit Container To keep all first aid items in one common container. Gauze Pads -To cover wounds and prevent infection. Roll Bandage -To stabilize strains and sprains and cover wounds. Triangular Bandage -To cover wounds and prevent infection . Bandages -To stop minor bleeding and prevent infection. Adhesive Tape -To secure bandages to wounds. Antibacterial Ointment -To prevent infection on small cuts. Calamine Lotion -To prevent itching. Soap -To clean minor wounds and cuts and to prevent infection. Latex Gloves -To protect the rescuer from infection and blood pathogens. Bandage Scissors -To cut gauze and bandages. Tweezers -To pull splinters. Moleskin -To protect blisters and prevent infection. Antiseptic lotion - To prevent infections. Analgesic - Pain killer Anti-inflamatory - pyretic/ painkiller Chemical burns: Wash the chemical with large quantities of water. Ensure that the washings does not flow over normal areas. Cut out and remove contaminated clothing. Treat as for burns. Burns of eye: Wash immediately with cold water. Ensure washing do not flow over other eye. Caution the patient against rubbing the eye. Shift to hospital. 21 22 Establish where extra items are kept to restock the kit. Make up an inventory list. One copy with the kit, one copy with the troop. Show everyone the kit, what is in it, and how to find/use the contents. Define clear responsibility for maintaining the kit. What should be in first aid kit We recommend the following items must be in kit essentially: Coban - Also called selfadhering bandage. Carry the 1/2 inch size and one larger size like 2 or 3 inch. Once applied it keeps most dirt out, is flexible, and will stay on if wet. Very useful for use in the outdoors. Wound wash - How about a small bottle of contact lens saline solution? It is near sterile and can be used to wash a cut or rinse the eye. It should be placed in a visible location near the centre of the activities and clearly signposted. Everyone should be aware of its location. Steps to make a first aid kit The following points need to be addressed before making a first aid kit: Identify how kit will be used and where it will be kept (determines size and type of container). Analyse what type of injuries are expected (determines what to carry). Select and obtain the bag, box, or container for the kit. Obtain the contents, repackage them if necessary, and pack the kit. 2 3 Gloves - Carry medium and large size, which should fit just about everyone. Replace them periodically if they age and break down. Antibiotic Carry the triple antibiotic type. Band Aids Have both small and large sizes. Check them periodically, as they will age and become unusable. Gauze Pads You can purchase the "semi-sterile" type that come in bulk packages. Transfer them to plastic bags to put in the kit. 4x4 inch and 2x2 inch are useful sizes. Ace Bandages Also called elastic bandages. You may need the 3 inch size for wrists and the 6 inch size for larger joints. Triangular Bandages - They can be used as slings, dressing, and ties for splints Scissors - Obtain an inexpensive pair of small medical scissors. It cuts bandages, ties, tape, clothing, whatever. Very useful to have. Mouth Barrier Device - We recommend a pocket mask type…the one that comes in a hard plastic case. Small splints - A few wooden tongue depressors or popsicle sticks work as finger splints, scrapes, or as a tongue depressor. Side cutters (pliers) - If you are active with fishing activities this is needed to cut fish hooks. 24 2 5 Thermometer - Good to know just how high the fever is. Aspirin - You can carry this in the kits for cardiac issues. Ibuprofen - Used for ailments such as joint and muscle pain, etc. Chap stick - Dehydration can lead to cracked lips. Throat Lozenges - Helpful for a sore throat. Antacid - Helps with some of that camp cooking or for stomach illness or disorder. Sanitiser - In the field a quick way to wash up before and after treatment. Soap - J and J shampoo mixed with water works well to clean cuts. Small soap bars are available in the travel section. 6. Elements of Training in first aid 6.1 Teaching methods Training programmes should incorporate the following principles: Having appropriate first-aid supplies and equipment available; Exposing trainees to acute injury and illness settings as well as to the appropriate response through the use of visual aids; Including a course information resource for reference both during and after training; Allowing enough time for emphasis on commonly occurring situations; Emphasising skills training and confidence-building over classroom lectures; Emphasising quick response to first-aid situations. 6.2 Assessing the scene and the victim(s) The training programme should include instruction on the following: Assessing the scene for safety, number of injured, and nature of the event; Assessing the toxic potential of the environment and the need for respiratory protection; Establishing the presence of a confined space and the need for respiratory protection and specialised training to perform a rescue; Prioritising care when there are several injured; Assessing each victim for responsiveness, airway patency (blockage), breathing, circulation, and medical alert tags; Taking a victim's history at the scene, including determining the mechanism of injury; Performing a logical head-to-toe check for injuries; Stressing the need to continuously monitor the victim; Emphasising early activation of EMS; Indications for and methods of safely moving and rescuing victims; Repositioning ill/injured victims to prevent further injury. 6.3 Responding to Life-Threatening Emergencies The training program should be designed or adapted for the specific worksite and may include first-aid instruction on the following: Establishing responsiveness; Establishing and maintaining an open and clear airway; Performing rescue breathing; Treating airway obstruction in a conscious victim; Performing CPR; Using an AED; Recognising the signs and symptoms of shock and providing first aid for shock due to illness or injury; Assessing and treating a victim who has an unexplained change in level of consciousness or sudden illness; Controlling bleeding with direct pressure; Poisoning; Recognising asphyxiation and the danger of entering a confined space without appropriate respiratory protection. Additional training is required if first-aid personnel will assist in the rescue from the confined space. Responding to Medical Emergencies -Chest pain; -Stroke; -Breathing problems; -Anaphylactic reaction; 26 7. Conclusion -Hypoglycemia in diabetics taking insulin; -Seizures; -Pregnancy complications; -Abdominal injury; -Reduced level of consciousness; -Impaled object. 6.4 Responding to Non-Life-Threatening Emergencies The training programme should be designed for the specific worksite and include firstaid instruction for the management of the following: Wounds -Assessment and first aid for wounds including abrasions, cuts, lacerations, punctures, avulsions, amputations and crush injuries; -Principles of wound care, including infection precautions; -Principles of body substance isolation, universal precautions and use of personal protective equipment. Burns -Assessing the severity of a burn; -Recognising whether a burn is thermal, electrical, or chemical and the appropriate first aid; -Reviewing corrosive chemicals at a specific worksite, along with appropriate first aid. Temperature Extremes -Exposure to cold, including frostbite and hypothermia; -Exposure to heat, including heat cramps, heat exhaustion and heat stroke. Musculoskeletal Injuries -Fractures; -Sprains, strains, contusions and cramps; -Head, neck, back and spinal injuries; -Appropriate handling of amputated body parts. Eye injuries -First aid for eye injuries; -First aid for chemical burns. Mouth and Teeth Injuries -Oral injuries; lip and tongue injuries; broken and missing teeth; -The importance of preventing aspiration of blood and/or teeth. Bites and Stings -Human and animal bites; -Bites and stings from insects; instruction in first-aid treatment of anaphylactic shock. Many deaths and impact of injuries can be prevented with First Aid if causalities are treated immediately. First aid is the initial care given to an injured person. Mostly, this timely care prior to the arrival of the medical help means the difference between life and death. It must start immediately when the injury or illness occurs and continue until medical help arrives or the casualty recovers. The basic aims of first aid are: To save life To protect the casualty from getting more harm To reduce pain and Priorities of Casualty Treatment Priorities of Casualty Treatment Asphyxia Cardiac Arrest Severe Haemorrhage (Bleeding) Other Injuries/Illnesses Shock Immediate Requirement Critical four minutes One of the most common causes of an accidental death is due to loss of oxygen supply. This is mostly caused by a blocked airway. Normally it takes less than four minutes for a blocked airway to cause death. The 'golden hour' In emergency medicine, the golden hour is the first 60 minutes after the occurrence of a major multisystem trauma. It is widely believed that the victim's chances of survival are greatest if he or she receives definitive care within the first hour. First aid is the first step to save a victim. The first aid steps can be summarised again as in next Fig-2. Training should be imparted by qualified trainers only and repeated in regular intervals. 28 27 8. Glossary DANGER Consequence: Outcome or impact of an event. RESPONSE Event: Occurrence of a particular set of circumstances. Air Yes Manage bleeding, shock they Breathing and other injuries First aid: Is an attempted to a ill person to provide health care immediately after sudden health problems. Frequency: A measure of the number of occurrences per unit of time. AIRWAY Roll to side, supporting head and neck. Clear airway Hazard: A source of potential harm or a situation with a potential to cause loss. Health Loss: Any negative consequence or adverse effect on human health. Health Risk: The chance of something happening that will have an impact upon the huma health. BREATHING Looks, listen and Feel DANGER Health treatment: Process of selection and implementation of measures to modify risk. Place in lateral Yes position, monitor ABCs, treat other injuries Likelihood: A general description of probability or frequency. Roll onto back, supporting head and neek, 5 full breaths in 10 seconds CIRCULATION Yes Do they have a pulse? Commence Ear (not breathing, pulse present) No Commence CPR (not breathing, no pulse) Fig-2 29 30 9. References Notes 1. Best Practices Guide: Fundamentals of a Workplace First-Aid Programmes, U.S. Department of Labor Occupational Safety and Health Administration OSHA 331706N 2006. 2. Best Practices Guide: Fundamentals of a Workplace First-Aid Programmes, Indian Red Cross Society. 3. www.hrdp-idrm.in 31 32