Lesson 7
advertisement

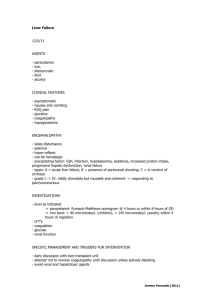
Lesson 7 Medications (drugs) Ex 1. Key-words: 1 used as over-the-counter analgesic (pain reliever) 2 antipyretic (fever reducer) 3 to be derived from coal tar 4 a nonsteroidal antiinflammatory drug 5 a major ingredient in numerous cold and flu remedies 6 severe pain (such as in advanced cancer) 7 The World Health Organization (WHO) 8 prolongation of bleeding time 9 a common household drug 10 redness, and swelling of the knee joint 11 a physician 12 to be available in a tablet, capsule, liquid suspension, suppository, intravenous, and intramuscular form. 13 adult dose 14 maximum daily dose 15 to be safe for children and infants 16 to be metabolised in the liver 17 viral illnesses 18 vomiting 19 salivation and discolouration of the tongue and gums 20 liver damage 1 используемый как внебиржевой болеутоляющий облегчитель), 2 жаропонижающий 3 быть полученными из битума 4 нестероидный антиподстрекательский препарат 5 главный компонент средств против многочисленных простуд и гриппа 6 сильные боли (как при раке) 7 Всемирная организация здравоохранения 8 продление кровотечения 9 общий домашний препарат 10 краснота и опухоль коленного сустава 11 врач 12 доступные в таблетках, капсулах, жидких суспензиях, свечах, внутривенных и внутримышечных формах. 13 взрослая доза 14 максимальная ежедневная доза 15, безопасно для детей и младенцев 16, усвоенный в печени 17 вирусные болезни 18 рвота 19 слюнотечение и discolouration языка и десен 20 повреждение печени Ex 2. Read and translate the following word-combinations: Glucuronidation, sulfation, sulfate conjugation, N-hydroxylation, rearrangement, GSH conjugation, the hepatic cytochrome P450 enzyme system metabolizm, significant alkylating metabolite, N-acetyl-p-benzo-quinone imine, sulfhydryl groups of glutathione, the toxic effects of paracetamol, unlike other common analgesics, little anti-inflammatory activity, affect blood coagulation, affect function of the kidneys, calcified kidneys, affect the closure of the fetal ductus arteriosus, viral illness. Ex 3. Read some information about “Drugs for the pain & consciousness”: For pain & consciousness (analgesic drugs) The main classes of painkillers are NSAIDs, opioids and various orphans such as paracetamol, tricyclic antidepressants and anticonvulsants. Text 15. Analgesic An analgesic (also known as a painkiller) is any member of the group of drugs used to relieve pain (achieve analgesia). The word analgesic derives from Greek an- ("without") and algos ("pain"). Analgesic drugs act in various ways on the peripheral and central nervous systems; they include paracetamol (para-acetylaminophenol, also known in the US as acetaminophen), the nonsteroidal anti-inflammatory drugs (NSAIDs) such as the salicylates, and opioid drugs such as morphine and opium. They are distinct from anesthetics, which reversibly eliminate sensation. In choosing analgesics, the severity and response to other medication determines the choice of agent; the WHO pain ladder, originally developed in cancer-related pain, is widely applied to find suitable drugs in a stepwise manner. The analgesic choice is also determined by the type of pain: for neuropathic pain, traditional analgesics are less effective, and there is often benefit from classes of drugs that are not normally considered analgesics, such as tricyclic antidepressants and anticonvulsants. The major classes: Paracetamol and NSAIDs The exact mechanism of action of paracetamol/acetaminophen is uncertain, but it appears to be acting centrally (in the brain rather than in nerve endings). Aspirin and the other non-steroidal anti-inflammatory drugs (NSAIDs) inhibit cyclooxygenases, leading to a decrease in prostaglandin production. This reduces pain and also inflammation (in contrast to paracetamol and the opioids). Paracetamol has few side effects and is regarded as safe, although intake above the recommended dose can lead to liver damage, which can be severe and life-threatening, and occasionally kidney damage. NSAIDs predispose to peptic ulcers, renal failure, allergic reactions, and occasionally hearing loss, and they can increase the risk of hemorrhage by affecting platelet function. The use of aspirin in children under 16 suffering from viral illness has been linked to Reye's syndrome, a rare but severe liver disorder. COX-2 inhibitors. These drugs have been derived from NSAIDs. The cyclooxygenase enzyme inhibited by NSAIDs was discovered to have at least 2 different versions: COX1 and COX2. Research suggested that most of the adverse effects of NSAIDs were mediated by blocking the COX1 (constitutive) enzyme, with the analgesic effects being mediated by the COX2 (inducible) enzyme. The COX2 inhibitors were thus developed to inhibit only the COX2 enzyme (traditional NSAIDs block both versions in general). These drugs (such as rofecoxib and celecoxib) are equally effective analgesics when compared with NSAIDs, but cause less gastrointestinal hemorrhage in particular. However, post-launch data indicated increased risk of cardiac and cerebrovascular events with these drugs; this is probably due to an imbalance in blood coagulation. Rofecoxib (marketed as Vioxx) was subsequently withdrawn from the market. The role for the remaining members of this class of drug is debated. Opiates and morphinomimetics. Morphine, the archetypal opioid, and various other substances (e.g. codeine, oxycodone, hydrocodone, dihydromorphine, pethidine) all exert a similar influence on the cerebral opioid receptor system. Tramadol and buprenorphine are thought to be partial agonists of the opioid receptors. Tramadol is structurally closer to venlafaxine than to codeine and delivers analgesia by not only delivering "opiate-like" effects (through mild agonism of the mu receptor) but also by acting as a weak but fast-acting serotonin and norepinephrine reuptake inhibitor. Dosing of all opioids may be limited by opioid toxicity (confusion, respiratory depression, myoclonic jerks and pinpoint pupils), seizures (tramadol), but there is no dose ceiling in patients who tolerate this. Opioids, while very effective analgesics, may have some unpleasant side-effects. Up to 1 in 3 patients starting morphine may experience nausea and vomiting (generally relieved by a short course of antiemetics). Pruritus (itching) may require switching to a different opioid. Constipation occurs in almost all patients on opioids, and laxatives (lactulose, macrogolcontaining or co-danthramer) are typically co-prescribed. When used appropriately, opioids and similar narcotic analgesics are otherwise safe and effective, however risks such as addiction and the body becoming used to the drug (tolerance) can occur. The effect of tolerance means that drug dosing may have to be increased if for a chronic disease. Flupirtine is a centrally acting K+ channel opener with weak NMDA antagonist properties. It is used in Europe for moderate to strong pain and migraine and its muscle relaxant properties. It has no anticholinergic properties and is believed be devoid of any activity on dopamine, serotonin or histamin receptors. It is not addictive and tolerance does not develop. Specific agents In patients with chronic or neuropathic pain, various other substances may have analgesic properties. Tricyclic antidepressants, especially amitriptyline, have been shown to improve pain in what appears to be a central manner. Nefopam is used in Europe for pain relief with concurrent opioids. The exact mechanism of carbamazepine, gabapentin and pregabalin is similarly unclear, but these anticonvulsants are used to treat neuropathic pain with differing degrees of success. Anticonvulsants are most commonly used for neuropathic pain as their mechanism of action tends to decrease the firing of specific nerve systems. Specific forms and uses Combinations Analgesics are frequently used in combination, such as the paracetamol and codeine preparations found in many non-prescription pain relievers. They can also be found in combination with vasoconstrictor drugs such as pseudoephedrine for sinus-related preparations, or with antihistamine drugs for allergy sufferers. While the use of paracetamol, as well as aspirin, ibuprofen, naproxen, and other NSAIDS concurrently with weak to mid-range opiates (up to about the hydrocodone level) has been said to show beneficial synergistic effects by combatting pain at multiple sites of action, several combination analgesic products have been shown to have little efficacy benefits when compared to similar doses of their individual components. These combination analgesics can often result in significant adverse events including accidental overdoses, most often due to confusion which arises from the multiple (and often non-acting) components of these combinations. Topical or systemic. Topical analgesia is generally recommended to avoid systemic side-effects. Painful joints, for example, may be treated with an ibuprofen- or diclofenaccontaining gel; capsaicin also is used topically. Lidocaine, an anesthetic, and steroids may be injected into painful joints for longer-term pain relief. Lidocaine is also used for painful mouth sores and to numb areas for dental work and minor medical procedures. Psychotropic agents. Tetrahydrocannabinol (THC) and some other cannabinoids, either from the Cannabis sativa plant or synthetic, have analgesic properties, although the use of cannabis derivatives is currently illegal in many countries. A recent study finds that inhaled cannabis is effective in alleviating neuropathy and pain resulting from e.g. spinal injury and multiple sclerosis.[6] Other psychotropic analgesic agents include ketamine (an NMDA receptor antagonist), clonidine and other α2-adrenoreceptor agonists, and mexiletine and other local anaesthetic analogues. Atypical and/or adjuvant analgesics. Orphenadrine, cyclobenzaprine, scopolamine, atropine, gabapentin, first-generation antidepressants and other drugs possessing anticholinergic and/or antispasmodic properties are used in many cases along with analgesics to potentiate centrally acting analgesics such as opioids when used against pain especially of neuropathic origin and to modulate the effects of many other types of analgesics by action in the parasympathetic nervous system. Dextromethorphan has been noted to slow the development of tolerance to opioids and exert additional analgesia by acting upon the NMDA receptors; some analgesics such as methadone and ketobemidone and perhaps piritramide have intrinsic NMDA action. High-alcohol liquor has been used in the past as an agent for dulling pain, due to the CNS depressant effects of ethyl alcohol, a notable example being the American Civil War. However, the ability of alcohol to "kill pain" may be inferior to many analgesics used today (e.g. morphine, codeine). As such, the idea of alcohol for analgesia is generally considered a primitive practice in virtually all industrialized countries today. The use of adjuvant analgesics is an important and growing part of the pain-control field and new discoveries are made practically every year. Many of these drugs combat the side effects of opioid analgesics, an added bonus. For example, antihistamines including orphenadrine combat the release of histamine caused by many opioids, methylphenidate, caffeine, ephedrine, dextroamphetamine, and cocaine work against heavy sedation and may elevate mood in distressed patients as do the antidepressants. A well-accepted benefit of THC to chronic pain patients on opioids is its superior anti-nauseant action. Text 16. Paracetamol Definition. Paracetamol or acetaminophen is a widely used over-the-counter analgesic (pain reliever) and antipyretic (fever reducer). Paracetamol is derived from coal tar, and is part of the class of drugs known as "aniline analgesics"; it is the only such drug still in use today. It is the active metabolite of phenacetin, once popular as an analgesic and antipyretic in its own right, but unlike phenacetin and its combinations, paracetamol is not considered to be carcinogenic at therapeutic doses. The words acetaminophen (used in the United States, Canada, Hong Kong, Iran, Colombia and other Latin American countries) and paracetamol (used elsewhere) both come from chemical names for the compound: para-acetylaminophenol and para-acetylaminophenol. In some contexts, it is simply abbreviated as APAP, for N-acetyl-para-aminophenol. There is confusion in terminology of paracetamol. It could be considered a nonsteroidal antiinflammatory drug (NSAID), but paracetamol has very little anti-inflammatory effect in many tissues. However, aspirin, paracetamol and other NSAIDs all act by the same mechanism (inhibition of prostaglandin (PG) synthesis) and all show varying levels of analgesic, antiinflammatory, antipyretic and antiplatelet actions. Indications. It is commonly used for the relief of headaches, and other minor aches and pains, and is a major ingredient in numerous cold and flu remedies. In combination with opioid analgesics, paracetamol could be used also in the management of more severe pain (such as in advanced cancer). The World Health Organization (WHO) recommends that paracetamol be given to children with fever higher than 38.5 °C (101.3 °F). Paracetamol is much more effective than aspirin, especially in patients where excessive gastric acid secretion or prolongation of bleeding time may be a concern. While paracetamol has analgesic and antipyretic properties comparable to those of aspirin, its anti-inflammatory effects are weak. Because paracetamol is well tolerated, available without a prescription, and lacks the gastric side effects of aspirin, it has in recent years increasingly become a common household drug. Acetaminophen is used for the relief of fevers, aches and pains associated with many parts of the body. Acetaminophen relieves pain in mild arthritis but has no effect on the underlying inflammation, redness, and swelling of the joint. If the pain is not due to inflammation, acetaminophen is as effective as aspirin. It is as effective as the non-steroidal antiinflammatory drug ibuprofen (Motrin) in relieving the pain of osteoarthritis of the knee. Unless directed by physician, acetaminophen should not be used for longer than 10 days. Structure and reactivity. Paracetamol consists of a benzene ring core, substituted by one hydroxyl group and the nitrogen atom of an amide group in the para pattern. The amide group is acetamide (ethanamide). It is an extensively conjugated system, as the lone pair on the hydroxyl oxygen, the benzene pi cloud, the nitrogen lone pair, the p orbital on the carbonyl carbon, and the lone pair on the carbonyl oxygen are all conjugated. The presence of two activating groups also make the benzene ring highly reactive toward electrophilic aromatic substitution. As the substituents are ortho, para-directing and para with respect to each other, all positions on the ring are more or less equally activated. The conjugation also greatly reduces the basicity of the oxygens and the nitrogen, while making the hydroxyl acidic through delocalisation of charge developed on the phenoxide anion. Synthesis. Compared with many other drugs, paracetamol is much easier to synthesize, because it lacks stereocenters. As a result, there is no need to design a stereo-selective synthesis. Industrial preparation of paracetamol usually proceeds from nitrobenzene. A one-step reductive acetamidation reaction can be mediated by thioacetate. Paracetamol may be easily prepared in the laboratory by nitrating phenol with sodium nitrate, separating the desired p-nitrophenol from the ortho- byproduct, and reducing the nitro group with sodium borohydride. The resultant p-aminophenol is then acetylated with acetic anhydride. In this reaction, phenol is strongly activating, thus the reaction only requires mild conditions: Reactions. p-Aminophenol may be obtained by the amide hydrolysis of paracetamol. pAminophenol prepared this way, and related to the commercially available Metol, has been used as a developer in photography by hobbyists. Available forms. Paracetamol is available in a tablet, capsule, liquid suspension, suppository, intravenous, and intramuscular form. The common adult dose is 500 mg to 1000 mg. The recommended maximum daily dose, for adults, is 4000 mg. In recommended doses, paracetamol generally is safe for children and infants, as well as for adults. Metabolism. Paracetamol is metabolised primarily in the liver, into non-toxic products. Three metabolic pathways are notable: Glucuronidation is believed to account for 40% to two-thirds of the metabolism of paracetamol. Sulfation (sulfate conjugation) may account for 20–40%. N-hydroxylation and rearrangement, then GSH conjugation, accounts for less than 15%. The hepatic cytochrome P450 enzyme system metabolizes paracetamol, forming a minor yet significant alkylating metabolite known as NAPQI (N-acetyl-p-benzo-quinone imine). NAPQI is then irreversibly conjugated with the sulfhydryl groups of glutathione. All three pathways yield final products that are inactive, non-toxic, and eventually excreted by the kidneys. In the third pathway, however, the intermediate product NAPQI is toxic. NAPQI is primarily responsible for the toxic effects of paracetamol; this constitutes an excellent example of toxication. Efficacy and side effects. Paracetamol, unlike other common analgesics such as aspirin and ibuprofen, has relatively little anti-inflammatory activity, so it is not considered to be a nonsteroidal anti-inflammatory drug (NSAID). In recommended doses, paracetamol does not irritate the lining of the stomach, affect blood coagulation as much as NSAIDs, or affect function of the kidneys. However, some studies have shown that high dose-usage (greater than 2,000 mg per day) does increase the risk of upper gastrointestinal complications such as stomach bleeding. The researchers found that heavy use of aspirin or paracetamol - defined as 300 grams a year (1 g per day on average) - was linked to a condition known as small, indented and calcified kidneys (SICK). Paracetamol is safe in pregnancy, and does not affect the closure of the fetal ductus arteriosus as NSAIDs can. Unlike aspirin, it is safe in children, as paracetamol is not associated with a risk of Reye's syndrome in children with viral illnesses. Effects on animals. Paracetamol is extremely toxic to cats. Cats lack the necessary glucuronyl transferase enzymes to safely break paracetamol down, and minute portions of a tablet may prove fatal. Initial symptoms include vomiting, salivation and discolouration of the tongue and gums, liver damage, death. Although paracetamol is believed to have no significant anti-inflammatory activity, it has been reported to be as effective as aspirin in the treatment of musculoskeletal pain in dogs. Paracetamol is also lethal to snakes. Ex 4. Speak about the use of paracetomol. What diaseases can it treat? Ex 5. Writing. Write the composition describing your favourite place of summer holidays. Follow this plan: 1. Identify the time and place 2. Convey actions with vivid verbs 3. Express your attitudes, feelings and emotions.