Appendix of Forms
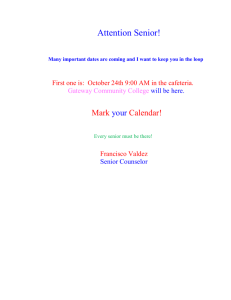
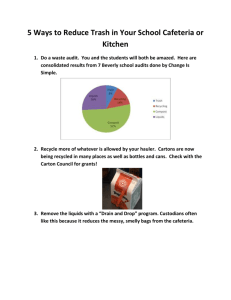
advertisement

Section 7 Appendix of Forms IRS FORMS CONTAINED IN THIS SECTION ARE SAMPLES ONLY. For current forms, go to: www.irs.gov © 2006 MHM Resources, Inc. 7-1 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-2 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-3 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-4 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-5 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-6 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-7 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-8 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-9 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-10 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-11 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-12 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-13 Section 125 Cafeteria Plan Administrators Training Date Contact Name Company Address 1 Address 2 City/State/Zip RE: Individual Health Insurance Plans in a Cafeteria Plan Dear [Contact Name]: Due to recent changes in the law, a question has arisen as to the advisability of allowing an "other health insurance premium" conversion option as part of an Internal Revenue Code (IRC) Section 125 plan (cafeteria plan). According to Revenue Ruling 61-146, and an informal opinion by the Office of IRS Chief Counsel, this is a permissible practice. However, several issues must be considered in determining the advisability of allowing such an option. When a salary reduction contribution is made through an IRC §125 plan, the contribution, in effect, becomes an employer contribution. Thus, for many purposes, the individual policy becomes an employer-sponsored plan subject to laws and regulations such as: COBRA HIPAA, including the certification requirements ERISA, including reporting and disclosure requirements Medicare secondary payor rules Nondiscrimination rules under Title VII of the Civil Rights Act In addition, many state group health insurance laws define such arrangements as employer sponsored plans subject to the group health insurance mandates. Many insurance carriers are unwilling to issue individual policies that are brought under the group insurance laws in this manner. For the aforestated reasons, we discourage the practice of allowing "other health insurance premiums" to be a permitted salary reduction option through an IRC §125 plan. If you intend to continue or commence such a practice, we recommend that you notify the carrier of the individual health insurance plan and consult with your legal counsel. If you have any questions, please contact [Name and Phone Number]. © 2006 MHM Resources, Inc. 7-14 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-15 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-16 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-17 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-18 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-19 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-20 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-21 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-22 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-23 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-24 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-25 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-26 Section 125 Cafeteria Plan Administrators Training Pre-Qualification Worksheet Employer Characteristics and Considerations Flexible Benefits Plans Yes No Has the employer had a POP-Kit or other premium conversion plan installed for at least 12 months? Does the employer have at least ten employees who have annual unreimbursed medical and/or dependent care expenses that average $1,200 per participant? Does the employer have a computerized payroll system? Does the current medical insurance plan have a “high” deductible? The current medical insurance plan does not cover all vision, dental or orthodontia expenses Is the employee turnover low? Do some of the employees have young dependents? If all or most of the above questions can be answered “Yes,” this employer may be a likely candidate for a Flexible Benefit Plan. © 2006 MHM Resources, Inc. 7-27 Section 125 Cafeteria Plan Administrators Training Employee Benefits Survey Name________ _______________________________ (Please print) Group Insurance 1. 2. Circle One Do you currently pay an insurance premium for one of the following through a payroll deduction? • Health insurance Yes No • Group-term life insurance Yes No • Disability insurance Yes No • Dental insurance Yes No If so, approximately how much are these premiums annually? $_____________ Medical Expenses 1. Do you or a member of your family incur medical expenses which are not reimbursed by insurance? Yes No Examples: • Annual medical exams • Prescription drugs • Dental cleaning • Eyeglasses • Orthodontia 2. • Insurance deductible If so, approximately how much are these expenses annually? $_____________ Dependent Care 1. 2. 3. If you are married, does your spouse work or attend school on a full-time basis? Yes No N/A If you are not married, do you have a child or other dependent living in your home? Yes No N/A If the answer to numbers 1 or 2 above is “yes,” do you have a child (under age 13) or other dependent (spouse or other family member) living in your home which requires daycare or other similar expenses? Yes No Examples: • Day care center • Baby-sitter • Housekeeper 4. If the answer to number 3 is “yes,” approximately how much are these expenses annually? © 2006 MHM Resources, Inc. 7-28 $_______________ Section 125 Cafeteria Plan Administrators Training Feasibility Study Internal Revenue Code Section 125 Flexible Compensation Plans. Feasibility Study for Cafeteria Plan. Report of participation and employer estimated savings. Medical Care Reimbursement Annualized Number Elections of Employees $ _______ Dependent Child Care Group Hospital Insurance Group Term Life Insurance Total redirection $ Employer savings FICA 1 @ 7.65% $ ______ Worker’s compensation and unemployment Total savings $ Employer costs Annual base fee — printing costs $_______ Form 5500 preparation administration fee Annualized $_______ One time set up — $650.00 Amortized over two years Total costs $_______ Annual net savings (cost). Set up cost amortized. Initial net savings (cost). Set up not amortized. $ Total savings of all employees $_______ © 2006 MHM Resources, Inc. 7-29 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-30 Section 125 Cafeteria Plan Administrators Training Client Engagement Manager • • • • • • • • • • • • • • • • • • • • • • • • Interview with client to fill out Client Checklist and design Plan Document and Summary Plan Description. Conduct initial discrimination tests. Establish a contact at client’s office that participants will be working with for all questions about the Plan. Provide client with worksheets to determine key employees [IRC 416(i)(1)(A)], highly compensated employees [IRC 414(q)] and those making under $25,000 in annual compensation Distribute general information about the Cafeteria Plan to all employees. Pickup key employee, highly compensated employee and total compensation worksheets. Meet with payroll personnel to discuss salary redirection and reimbursements as they apply to individual paychecks. Enrollment — Group or individual meetings to explain Cafeteria Plan and answer any questions. Advise those with dependent care expenses of childcare credit. Distribute Summary Plan Descriptions to participants within 120 days after plan is adopted. Distribute Summary Plan Descriptions to new employees within 90 days after they become participants. Collect election forms directly from participants or have employer assemble and forward to you. Return short verification letter to each participant restating their annual and per paycheck election for each portion of the Plan. Determine total nontaxable benefits provided to all employees, key employees and highly compensated employees based on annual elections. Test for discrimination (25% Concentration Test for all benefits, 55% Average Benefits Test, and 25% Owners Test for the dependent care portion of the Plan). Test for discrimination at the beginning of the Plan based on annual election amounts and at least quarterly thereafter based on year-to-date contributions. Keep accurate records throughout the Plan Year for changes of family status, terminations, and new employees. Keep your client and participants informed of account balances through company statements and individual employee statements. Reconcile to client’s year-to-date records quarterly. Two months before the Plan year end — inform employees of account balances including year-to-date contributions, claims, and disbursements plus a reminder of their annual election amount, the amount they need to request by Plan year end, the number of grace days allowed after the Plan year end, and their risk of forfeiture. Thirty days prior to Plan year end — send individual reelection forms showing last year’s elections and stating any changes that will take place in the new Plan year. Enrollment — Group or individual meetings to explain Cafeteria Plan and answer any questions. Advise those with dependent care expenses of childcare credit. By January 31 of every year — furnish participants in dependent care portion of Plan with W-2 showing total benefits provided for their taxable year through the Cafeteria Plan. Plan year end plus grace days expiration — test for discrimination based on total disbursements from the Plan and send final reports to advise client and participants of any forfeitures or pre-funded amounts. Complete Form 5500. All required forms and schedules are due by the last day of the 7th month after the plan year-ends. If needed, File Form 5558 “Application for Extension of Time To File Certain Employee Plan Returns” to obtain an extension of time for 2 ½ months. (Suspended for Fringe Benefit Plans.) Final Discrimination Testing - test for discrimination at the end of the Plan based on total disbursement amounts. © 2006 MHM Resources, Inc. 7-31 Section 125 Cafeteria Plan Administrators Training Flexible Spending Account Plan Application 1.Legal Name of Company Sponsoring Plan ______________________________________ 2. Business Entity Type: C Corp. Sole Proprietorship Partnership Not-For-Profit Government Entity or church S Corp. Limited Liability Company 3. Principal Business Activity _______________________________________________ 4. Federal Employer Identification Number (Must be 9 digits): __ __ -- __ __ __ __ __ __ __ 5. Contact Person _________________________________ Title __________________________________________ 6. Street Address (No PO Boxes): ____________________________________________ City, State, Zip: _________________________________________________ 7. Phone Number Fax Number E-mail Address 8. Effective Date – This FSA plan will be: ( ) A new plan effective as of (date) _______________________ ( ) An amendment and restatement is effective as of (date) ____________________ (1) This amendment and restatement is effective as of (date) ______________________ (2) State the effective date of the original plan (date) ___________________ (3) State the plan number (consult your last Form 5500 and/or plan document for this number assigned to your plan) ________ 9. Plan Year – The first plan year for the FSA will be: A 12-consecutive-month period beginning (date) ___________ and ending (date) __________________ A short plan year beginning (date) ____________________and ending (date) ____________________ 10. Employer’s Principal Office – This FSA plan shall be governed under the laws of the: State of ____________________________ Commonwealth of __________________________ 11. All employees are eligible for the FSA Plan: Except: Employees not eligible under Employers group medical plan Part-time Employees expected to work less than ___ hours per week Commissioned Employees Union Employees Other (type & attach) 12. All employees can enter the FSA Plan: Same as Employer’s group medical plan _____ days after date of hire 13. Benefits – The benefits selected below shall be included in the FSA Plan: Medical expenses not covered by insurance and © 2006 MHM Resources, Inc. 7-32 Section 125 Cafeteria Plan Administrators Training annual maximum per participant shall be $_____________ (typical limits are between $1,500 and $2,600 annually) Adult and child daycare expenses Health and other insurance (select coverages below): __Health Insurance Premiums __Disability insurance** __Critical Illness Insurance __Dental Insurance __Vision Care Insurance __ Accidental Death/Dismemberment __Group-term Life Insurance* __Cancer Insurance __Other Insurance (specify) _____ *Group-term life insurance up to $50,000 coverage **If disability insurance is paid for on a pretax basis, any benefits received are taxable to the employee Note: Insurance products with a return-of-premium feature cannot be paid for on a pretax basis. Individual Health and Disability Insurance 14. Contributions – The contributions for the FSA Plan will be: Employee (salary reduction) contributions only Employer contributions only Both salary redirection and Employer contributions $ ________annually per Participant $_____Employer contributions convertible to cash 15. Legal names(s) of affiliated company(ies) that will be covered by this plan: (provide names, tax ID numbers and full addresses on attachment) 16. Total number of employees ___________ 17. Pay cycles – Payroll is provided (weekly, semi-monthly, monthly, etc.) _________________________ Deductions to begin ________________________________ Payroll is prepared: __In house __Out sourced (specify payroll company): ___________________________________________ Pricing Information 18. Fee for a New Plan setup or restatement. Call for quote 19. Fee for Participant Services. $__ per month/participant. Client is billed by Admin. Co. each month. 20. Fee for Annual Plan Compliance. $__ per month is billed by Administrative Company Shipping Instructions 21. Shipping method (FSA setup kit is shipped within 2 business days): Date Received Date Application Signed Client Number Full Administration Plan Doc/5500 Only Accounting Use Set-up Fee Monthly Charge per participant Annual Fee Lead Source (Company Name) Relationship Manager (Agent Name) EZ POP Agent Bonus Commission Schedule Anticipated First Billing Month Additional Notes If Individual Health and Disability Insurance marked – send advice letter. © 2006 MHM Resources, Inc. 7-33 Section 125 Cafeteria Plan Administrators Training March 9, 2016 Dear One of the services we provide for your Flexible Benefit Plan is discrimination testing. In order to perform the discrimination testing; please complete the enclosed questionnaires identifying the Key and Highly Compensated employees for your plan year 2001. One of the discrimination tests is performed on all qualified benefits that are part of your Flexible Benefit Plan. Although we track the amounts contributed to the flexible spending accounts (Health Care Reimbursement and Dependent Care), we need the following information for the insurance premium portion of the plan. Total dollar amount of salary redirections for the insurance benefits that are part of your Plan. for the Key Employees: $ ___________ for all other employees $___________ - Please provide this information for these premiums for the Month of June Provide the total number of employees eligible to participate in the Dependent Care Portion of your plan. _____________________. This should be every employee that is eligible for your Section 125 Cafeteria Plan. Once we have received this information, we will perform the tests and advise if your Flexible Benefit Plan has failed the discrimination testing. No notice will be returned if your Plan is found to be nondiscriminatory. Please return the information to our office as soon as possible. If you have any questions, please feel free to contact me. My telephone number is. Sincerely, © 2006 MHM Resources, Inc. 7-34 Section 125 Cafeteria Plan Administrators Training IRC Section 125 — Cafeteria Plan Highly Compensated Employees — IRC 414(q) ______________________________________________ (Company Name) Plan Year Ended ________________ List all employees who fit into one or more of the following categories. An employee may be classified as highly compensated on the basis of more than one category. When listing highly compensated employees, list each employee only once. 1. List all employees with more than 5% ownership during the prior or current plan year. ______________________________ ______________________________ ______________________________ ______________________________ 2. List all employees who are a spouse or relative (within the meaning of IRC Section 318) of any individual listed in number 1 above. 3. ______________________________ ______________________________ ______________________________ ______________________________ List the employees earning more than $95,000 (2005) (indexed) in the prior plan year.* ______________________________ ______________________________ ______________________________ ______________________________ * An employer may elect to treat as highly compensated under the $95,000 compensation test only those employees who are also in the top-paid 20% group. © 2006 MHM Resources, Inc. 7-35 Section 125 Cafeteria Plan Administrators Training IRC Section 125 — Cafeteria Plan Key Employees — IRC 416(i)(1)(A) __________________________________ (Company Name) Plan Year Ended __________________ List all employees who, at any time during the current plan year, fit into one or more of the following four categories. An employee may be classified as a key employee on the basis of more than one category. When listing key employees, list each employee in each category. 1. 2. 3 Officers* with annual compensation greater than $140,000 (indexed)]: _________________________________ _________________________________ _________________________________ _________________________________ Employees with more than 5% ownership: ________ __________________________________ _________________________________ _________________________________ _________________________________ _________________________________ _________________________________ _________________________________ Employees with more than 1% ownership and annual compensation greater than $150,000: _________________________________ _________________________________ *The determination as to whether an employee is an officer should be made on all the facts and circumstances. Generally the term “officer” means an administrative executive. According to regulations under 414(q), an officer includes the president, vice-presidents, general manager, treasurer, secretary, and comptroller of a corporation and any other person who performs duties corresponding to those normally performed by persons occupying those positions. So, for example, all of the employees of a bank who have the title of vice-president or assistant vice-president are not necessarily officers unless they have the authority of an officer. Similarly, an employee who has the authority but not the title would be considered an officer. Sole proprietorships, partnerships, and associations, among other unincorporated entities, may have officer for this purpose. No more than 50 employees shall be treated as officers. If there are less than 50 employees who are treated as officers, no more than the greater of 1) three employees or 2) 10% of all employees will be treated as officers. © 2006 MHM Resources, Inc. 7-36 Section 125 Cafeteria Plan Administrators Training IRC SECTION 105 (h) Medical Expense Reimbursement Plans Percentage Test A plan is not discriminatory as to eligibility if it satisfies one of the following percentage tests. The medical expense reimbursement plan benefits: A. 70% or more of all employees. or B. 80% or more of all the employees who are eligible to benefit under the plan if 70% or more of all employees are eligible to benefit under the plan. 1. Total employees __________ 2. Total inelgible (see line 6, Excluded Employees Form) __________ 3. Employees eligible under the plan (subtract (1) from (2)) __________ 4. Employees excluded from benefiting __________ 5. Employees eligible to benefit (subtract 4 from 3) __________ 6. Number of employees participating in plan __________ 7. Percent of eligible nonexcluded employees who participate (divide (6) by (3)). If > 70% stop. Do not complete the remainder of this form. __________ Complete (8) only if (7) is less than 70% and complete (9) only if (8) is 70% or more: 8. 9. Percent of nonexcluded employees who are eligible to participate (divide (5) by (3)) __________ Percent of eligible employees who are participating (divide (6) by (5)) __________ Conclusion: If line (7) is > 70%, the plan has satisfied requirement A above. If line (8) is > 70% and line (9) is 80% or more, the plan has satisfied requirement B above. © 2006 MHM Resources, Inc. 7-37 Section 125 Cafeteria Plan Administrators Training IRC Section 105(h) Medical Expense Reimbursement Plans Benefits Available Test Answer the following questions. YES NO 1. Are any benefits under the plan available only to highly compensated individuals? If yes, this plan is discriminatory. Highly compensated individuals must include excess benefits in gross income. 2. Are all benefits available for the dependents of highly compensated individuals also available on the same basis for dependents of all other employees who are participants? If no, the plan is discriminatory. Highly compensated individuals must include excess benefits in gross income. 3. Is the plan’s maximum limit for the amount of reimbursement which may be paid to a participant for any single benefit, or combination of benefits based on: A. Percent of compensation? B. Participant’s age? C. Years of service? If yes to A, B, or C this plan is discriminatory. Highly compensated individuals must include excess benefits in gross income. 7 4. 5. Is the plan’s maximum limit for the amount of reimbursement, uniform to all participants and for all dependents of employees who are participants?* If no, this plan is discriminatory. Highly compensated individuals must include excess benefits in gross income. Are waiting period uniform to all participants? © 2006 MHM Resources, Inc. If no, this plan may be discriminatory. Highly compensated individuals must include excess benefits in gross income. 7-38 Section 125 Cafeteria Plan Administrators Training Nondiscriminatory Classification Test Reg. Section 410(b) ____________________________________ (Company Name) Plan Year Ended ____________________ Total Highly Nonhighly Employees Compensated Compensated 1. Total employees ___________ ___________ __________ 2. Employees ineligible under the plan ___________ ___________ __________ 3. Total eligible employees (Subtract line 2 from line 1) _______ (A) ________ 4. Total employees excluded from benefiting ________ (B) ___________ ___________ _________ 5. Total employees eligible to benefit (Subtract line 4 from line 3) ___________ ___________ 6. Concentration of nonhighly compensated employees ________ (C) _________ % (Divide Nonhighly compensated (B) by Total Employees (A)) 7. Safe Harbor percentage _________ % 8. Unsafe Harbor percentage _________ % 9. Percentage of nonexcluded, nonhighly compensated employees eligible to benefit under the plan. (Divide Nonhighly Compensated (C) by Nonhighly Compensated (B)) _________ % Conclusion: If line 9 is less than line 7, then it fails the Nondiscriminatory Classification Test. © 2006 MHM Resources, Inc. 7-39 Section 125 Cafeteria Plan Administrators Training Nondiscriminatory Classification Test Reg. Section 410(b) © 2006 MHM Resources, Inc. NHCE Concentration Percentage Safe Harbor Percentage Unsafe Harbor Percentage 0-60% 61% 62% 63% 64% 65% 66% 67% 68% 69% 70% 71% 72% 73% 74% 75% 76% 77% 78% 79% 80% 81% 82% 83% 84% 85% 86% 87% 88% 89% 90% 91% 92% 93% 94% 95% 96% 97% 98% 99% 50.00% 49.25% 48.50% 47.75% 47.00% 46.25% 45.50% 44.75% 44.00% 43.25% 42.50% 41.75% 41.00% 40.25% 39.50% 38.75% 38.00% 37.25% 36.50% 35.75% 35.00% 34.25% 33.50% 32.75% 32.00% 31.25% 30.50% 29.75% 29.00% 28.25% 27.50% 26.75% 26.00% 25.25% 24.50% 23.75% 23.00% 22.25% 21.50% 20.75% 40.00% 39.25% 38.50% 37.75% 37.00% 36.25% 35.50% 34.75% 34.00% 33.25% 32.50% 31.75% 31.00% 30.25% 29.50% 28.75% 28.00% 27.25% 26.50% 25.75% 25.00% 24.25% 23.50% 22.75% 22.00% 21.25% 20.50% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 7-40 Section 125 Cafeteria Plan Administrators Training Indexed Figures The indexed compensation levels for determining who is a highly compensated employee or a key employee are as follows. TYPE OF EMPLOYEE BASE YEAR 1987 2005 2006 2007 Highly Compensated Employee $75,000 $ 95,000 $100,000 $100,000 Top Paid Group of 20% $50,000 $95,000 $100,000 $100,000 Key Employee, Officer $45,000 $135,000 $140,000 $145,000 © 2006 MHM Resources, Inc. 7-41 Section 125 Cafeteria Plan Administrators Training IRC Section 129 — Dependent Care Assistance Plan 55% Average Benefits Test IRC 129(d)(8) (Applies to plan years beginning after December 31, 1989) __________________________________ (Company Name) Plan Year Ended _______________ STEP 1 Nontaxable benefits paid to highly compensated employees ________________ (A) Number of highly compensated employees ________________ (B) _____ Average benefits paid to highly compensated employees (A/B) (C) STEP 2 Nontaxable benefits paid to nonhighly compensated employees ________________ (D) Number of nonhighly compensated employees _________________ (E) Average benefits paid to nonhighly compensated employees (D/E) ______ (F) STEP 3 ______ Average benefits paid to highly compensated employees (A/B) (C) Ratio X 55% ______ Average benefit threshold for nonhighly compensated employee Conclusion: ______ (G) If (F) is less than (G), then all amounts paid to the highly compensated employees under IRC Section 129 are taxable. NOTE: When applying this test, in the case of any benefits provided through a salary redirection agreement, the employer may disregard all employees whose compensation falls below any specified amount that is less than $25,000, all employees who have not attained age 21 and completed 1 year of service, and employees covered by a collective bargaining agreement. CAUTION: Some people have interpreted this test to include all eligible employees in the denominator. Others believe that only employees electing dependent care assistance are to be included in the denominator. The IRS has not issued any regulations regarding the exact method of computing the Average Benefits Test but seems to favor using all eligible employees. © 2006 MHM Resources, Inc. 7-42 Section 125 Cafeteria Plan Administrators Training IRC Section 129 — Dependent Care Assistance Plan 25% Concentration Test for Principal Shareholders or Owners — IRC 129(d)(4) _________________________________________________ (Company Name) Plan Year Ended_____________________________ Nontaxable benefits paid to principal shareholders or owners _____ (A) Nontaxable benefits paid to all participants Total benefits paid (B) Percentage of benefits paid to principal shareholders or owners (A/ B)% ______(C) Conclusion: If (C) is greater than 25%, all amounts paid to highly compensated participants under IRC Section 129 are taxable. © 2006 MHM Resources, Inc. 7-43 Section 125 Cafeteria Plan Administrators Training IRC Section 137 — Adoption Assistance Plan 5% Concentration Test for Principal Shareholders or Owners — IRC 137(a)(3) __________________________________ (Company Name) Plan Year Ended _______________ Nontaxable benefits paid to principal shareholders or owners (A) Nontaxable benefits paid to all participants _______ Total benefits paid (B) Percentage of benefits paid to principal shareholders or owners (A : B) % (C) Conclusion: If (C) is greater than 5%, all amounts paid to shareholders and owners under IRC Section 137 are taxable. © 2006 MHM Resources, Inc. 7-44 Section 125 Cafeteria Plan Administrators Training IRC Section 125 — Cafeteria Plan 25% Concentration IRC 125(b)(2) __________________________________________ (Company Name) Plan Year Ended_____________________________ Total nontaxable benefits paid to all participants who are key employees __________(A) Total nontaxable benefits paid to all other participants ____________ Total nontaxable benefits paid _____________(B) Percent of nontaxable benefits paid to participants who are key employees (A / B) ____________% (C) Conclusion: If (C) is greater than 25%, participants who are key employees will include in income any “nontaxable benefits” received for the plan year. © 2006 MHM Resources, Inc. 7-45 Section 125 Cafeteria Plan Administrators Training Discrimination Tests Guide for Cafeteria Plans (2006) “Haves” Name 1. Percentage Test or 2. Classification Test (410(b)) HC HC 3. Benefits Available Test HC 4. Discriminatory in Operation HC Exclude 1 2 3 4 5 Definition §105 Calculation 5 highest pd officers Owns more >10% stock Apply 318 Highest pd 25% of all eligibles Consequences 70% / 80% Test 1HC$ X (HC$/Total$) Excess Reimbursement Excess Reimbursement 1HC$ - Max limit for NHCs Excess Benefits 1HC$ - Max limit for NHCs Excess Benefits § 125 1. Eligibility HC 2. Contributions and Benefits HC 3. 25% Concentration Test Key 1. Contributions and Benefits HC 2. Classification Test (410(b)) HC 3. 55% Average Benefits Test HC 4. 25% Concentration Test (5% Owner’s Test) An officer Owns >5% stock An HCE Apply 152 Officer & >$140,000(I) >5% ownership >1% ownrshp & $150,000 Apply 318 (416(i)) § 129 6 7 8 4 5 9 401(b) Limit 3 YOS Participate 1st day HC Taxed Facts and Circumstances HC Taxed Key$ / Total$ = ≤25% .333 X Nonkey = Key$ limit >5% owner prior/current Apply 318 >$95,000 prior year (414(q)) “5% owner” Keys Taxed After end of plan year, total $ taxable Can adjust during year Everyone can elect same benefits HC Taxed HC Taxed >5% Owner Apply 1563 HC$/HCs eligible = A NHC$/NHCs eligible = B B/A must be ≥ 55% HC Taxed “5%Owner”$/Total$ ≤ 25% HC Taxed §137 1. Classification Test (410 (b)) 2. 5% Concentration Test HC 414(q) “Shareholders” or “Owners” Indexed figures Highly Compensated Employee Top Paid Group of 20% Key Employee, Officer Base Year 1987 $75,000 $50,000 $45,000 1. Employees with less than 3 YOS 2. Employees not attained age 25 3, Part-time or seasonal who work less than 35 hrs 4, Union 5. Nonresident aliens with no US income 6. Not completed 6 MOS 7. Work less than 17 ½ hrs 8. Work not more than 6 mos per year 9. Under age 21 © 2006 MHM Resources, Inc. 4 HC Taxed >”5%”$/Total$ ≤ 5% >5%Owner Spouse or Dependent of above 2002 2003 2004 2005 $90,000 $90,000 $90,000 $95,000 $90,000 $90,000 $90,000 $95,000 $130,000 $130,000 $130,000 $135,000 2006 $100,000 $100,000 $140,000 2007 $100,000 Look back year $100,000 Look back year $145,000 Current 318: Spouse, children, grandchildren, or parents 152: Spouse and dependents 7-46 Section 125 Cafeteria Plan Administrators Training “5%” Taxed SECTION 125 CAFETERIA PLAN CHANGE IN STATUS/TERMINATION ELECTION FORM Complete this form when a change in status has occurred which affects your Cafeteria Plan election. All changes must be due to and consistent with the change in status. Company Name Effective Date of Change Employee Name Social Security Number Employee Address Phone Number If Terminating, Date of Last Deduction As a participant in the Cafeteria Plan, I am entitled to revoke my prior benefits election and enter into a new election in the event of certain changes in status. I understand that the change in my benefits election must be due to and consistent with the change in status and that the change must be acceptable under the Regulations issued by the Department of Treasury. I certify that I have incurred the following change in status: Change in Marital Status Change in legal marital status including marriage, death of the spouse, divorce, legal separation or annulment. Change in Number of Tax dependents Change in the number of tax dependents including birth, adoption, placement for adoption or death of a dependent. Changes in Spouse or Dependent’s Eligibility Under an Employer’s Plan Change in dependent status in satisfying or ceasing to satisfy the eligibility requirements of the plan, such as attainment of limiting age or student status or change in marital status. Judgment, decree or order including the imposition of a Qualified Medical Child Support Order Gain or loss of Medicaid or Medicare entitlement Entitlement to COBRA. Special requirements relating to the Family and Medical Leave Act (FMLA) Change in Employment Status That Changes Eligibility Status Change of employment status, such as termination or commencement of employment by the employee, spouse or dependent. Change in work schedule, such as a reduction or increase in hours of employment by the employee, spouse or dependent, including a switch between part-time and full-time, a strike or lockout, a change in worksite, or commencement or return from an unpaid leave of absence. Change in eligibility due to change in residency of the employee, spouse or dependent. Change in Cost or Coverage (applicable for health insurance and dependent care assistance account elections only) Significant cost increase in your or your dependent’s coverage Significant curtailment of your or your dependent’s coverage Addition or elimination of benefit package option under your or your dependent’s employer’s plan Change in coverage or open enrollment of spouse or dependent under other employer’s plan provided that the employee, spouse or dependent elects coverage under the dependent’s plan. Dependent care provider is replaced by another. Please change my election(s) as follows: Premium Savings Account Change insurance premiums to $________ per pay period. Health Care Expense Account Change my annual election for my Health Care Expense Account from $_______ to $ _______. My new per pay period election will be $ ________ effective with the ____________ ______ payroll. Dependent Care Assistance Program Change my annual election for my Dependent Care Assistance Program from $ _______ to $ ________. My new per pay period election will be $ ________ effective with the ___________ _____ payroll. ____________________ Employee Signature _________________________ Date Accepted and agreed to by: ____________________ Company Representative © 2006 MHM Resources, Inc. _________________________ Date 7-47 Section 125 Cafeteria Plan Administrators Training Certificate of Section 125 Medical Reimbursement Coverage **IMPORTANT – This certificate provides evidence of your prior coverage under a Section 125 Medical Reimbursement Plan. You may need to furnish this certificate if you become eligible under a group health plan that excludes coverage for certain medical conditions that you have before you enroll. This certificate may need to be provided if medical advice, diagnosis, care, or treatment was recommended or received for the condition within a sixmonth period to your enrollment in the new plan. If you become covered under another group health plan, check with the plan administrator to see if you need to provide this certificate. You may also need this certificate to buy, for yourself or your family, an insurance policy that does not exclude coverage for medical conditions that are present before you enroll. 1. Date of this Certificate: 2. Name of group health plan: 3. Name of participant: 4. Identification number of participant: 5. Name of any dependents to whom this certificate applies: 6. Name, address, and telephone number of plan administrator or issuer responsible for providing this certificate: 7. For further information, contact: 8. If the individual(s) identified in line 3 and line 5 has at least 18 months of creditable coverage (disregarding periods of coverage before a 63-day break), check here and skip questions 9 and 10. 9. Date waiting period or affiliation period (if any) began: 10. Date coverage began: 11. Date coverage ended: Note: (check if coverage is continuing as of date of this certificate). Separate Certificates will be furnished if information is not identical for the participant and each Beneficiary. (Company name) © 2006 MHM Resources, Inc. 7-48 Section 125 Cafeteria Plan Administrators Training Employee COBRA Notice/Election Date: SSN: Name: Address: City: State, Zip: This is to inform you that even though you can no longer be covered under our Unreimbursed Medical Expense reimbursement plan, as of, / / , you may continue your benefits under the plan beyond this date for the remainder of the plan year, provided you have a balance in your account (contributions are more than claims paid) at the time of your qualifying event. If any dependents of yours were covered under the plan, you may also continue their benefits. You have 60 days from the date of this notice to notify us of your election. If you elect this option, the benefits will be continued until: the end of the plan year following you become a covered employee under any group health plan that has not limitations or exclusions with respect to any preexisting conditions / / ; that you (or your dependent) may have; you or your dependent(s) become entitled to Medicare. If you become entitled to Medicare, the continuation coverage period for your dependent(s) begins on the date on which you became entitled to Medicare (or, if applicable, the date of an earlier qualifying event) and extends until the end of the plan year. you fail to pay the monthly charge for this coverage on time; or our Unreimbursed Medical Expense reimbursement plan is no longer in force; whichever is earliest. Before termination of employment, you elected $ of annual health care reimbursement benefits, for which you were contributing $ per pay period through a payroll deduction. You, and each of your dependents separately, have the right to continue the full amount of the annual benefit by continuing to pay for this coverage. If you elect to continue coverage a single monthly payment of $ will be required, and will cover you and your dependents. However, if you do not elect to continue the coverage but your spouse or dependent(s) do, this monthly amount must be paid by each individual in your family who chooses to continue coverage under the plan. The initial premium payment will be for the coverage period from the date coverage as an employee terminates to 60 days from the date of this notice. We must receive your first payment within 45 days of the date you sign this election form. ________________________________ © 2006 MHM Resources, Inc. 7-49 Section 125 Cafeteria Plan Administrators Training (Company Name) MEDICAL EXPENSE REIMBURSEMENT ACCOUNT Employee COBRA Notice/Election DATE: ________________ SSN: ________________ NAME: _________________________________ ADDRESS: ______________________________ CITY: __________________________________ STATE, ZIP______________________________ This is to inform you that even though you can no longer be covered under our Unreimbursed Medical Expense reimbursement plan, as of _______________, ________, you may continue your benefits under the plan beyond this date for the remainder of the plan year provided you have a balance in your account (contributions are more than claims paid) at the time of your qualifying event. If any dependents of yours were covered under the plan, you may also continue their benefits. You have 60 days from the date of this notice to notify us of your election. If you elect this option, the benefits will be continued until: the end of the plan year following ________, ________ ; you become a covered employee under any group health plan that has no limitations or exclusions with respect to any preexisting conditions that you (or your dependent) may have; you or your dependent(s) become entitled to Medicare. If you become entitled to Medicare, the continuation coverage period for your dependent(s) begins on the date on which you became entitled to Medicare (or, if applicable, the date of an earlier qualifying event) and extends until the end of the plan year; you fail to pay the monthly charge for this coverage on time; or our Unreimbursed Medical Expense reimbursement plan is no longer in force; whichever event is earliest. Before termination of employment, you had elected $ _______ of annual health care reimbursement benefits, for which you were contributing $ _________ per pay period through a payroll deduction. You, and each of your dependents separately, have the right to continue the full amount of the annual benefit by continuing to pay for this coverage. If you elect to continue coverage a single monthly payment of $ _______ will be required, and will cover you and your dependents. However, if you do not elect to continue the coverage but your spouse or dependent(s) do, this monthly amount must be paid by each individual in your family who chooses to continues to be covered under the plan. The initial premium payment will be for the coverage period from the date coverage as an employee terminates to 60 days from the date of this notice. We must receive your first payment within 45 days of the date you sign this election form. © 2006 MHM Resources, Inc. 7-50 Section 125 Cafeteria Plan Administrators Training If your first payment, or any subsequent monthly payment, is not received on time, you will lose your option to continue coverage. You have a 30 day grace period in which to pay premiums due. Please complete the bottom portion of this notice. Keep a copy for your records and return the original copy to: _____________________ _____________________ _____________________ _____________________ I wish to continue my employee benefits under your Medical Expense Reimbursement plan for myself and my spouse and dependent(s) Yes No The following family members wish to continue individual coverage under your Medical Expense Reimbursement plan: Spouse/Dependent Name Monthly Amount _____________________ _________ _____________________ _________ _____________________ _________ _____________________ _________ My first payment is enclosed Yes No I will make my first payment within 45 days Yes No Signature Date IMPORTANT In order that your coverage may continue, we must receive: 1. A completed copy of this notice by 2. Your first payment within 45 days following the date you sign this form. © 2006 MHM Resources, Inc. , 7-51 . Section 125 Cafeteria Plan Administrators Training March 9, 2016 «contact_name» «company_name» «address1» «address2» «city», «state» «zip» «phone» As part of the compliance services we perform for your Flexible Benefits Plan we annually request information to complete your discrimination testing and IRS Form 5500 filing. On April 4, 2002, the IRS announced that it has suspended the requirement to file annual information returns (Schedule F attached to Form 5500) for fringe benefit (Section 125 Cafeteria Plan) programs. Note, however, that cafeteria plans must still satisfy annual reporting requirements (IRS Form 5500) for component plans that are subject to ERISA (such your health FSA, medical reimbursement plan), unless an applicable exception applies. In order to determine if your plan is still required to file a Form 5500 and to accurately complete the discrimination testing for your plan, please complete the information below. 1. Total number of employees ELIGIBLE to participate in your plan as of: January 1, 2002 1. _____________ Employees Eligible 2. Total dollar amount of salary redirections for the insurance benefits that are part of your Plan. for the Key Employees: 2.a. $ ___________ for all other employees: b. $___________ - Please provide this information for these premiums for the month of January. Once we have received this information, we will perform the discrimination tests and advise you of the results. We will also complete the IRS Form 5500 should it be required. Please FAX (816-968-2050) or mail this letter to the attention of the Compliance Coordinator at MHM. If you need assistance with completing the questions, please call the compliance at 800-950-0105. You may also e-mail your responses or send questions to our e-mail: Flexhelp@mhmbiz.com. © 2006 MHM Resources, Inc. 7-52 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-53 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-54 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-55 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-56 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-57 Section 125 Cafeteria Plan Administrators Training Simplified line-by-line instructions for 2006 Form 5500 hand print version filed for a welfare benefit plan within a Cafeteria Plan. Use these instructions for an HRA or a health FSA plan that has more than 100 participants. Complete the Form 5500 with the “2006” printed in the upper right corner for a plan year that began in 2006, including the signature block. Part I -- Enter the plan year beginning and ending date if 1) this is a fiscal plan year, or 2) the plan has not been in effect for 12 months. Plan year beginning _________ Plan year end ________ Part I,A -- Check the box which indicates the type of plan entity: (1) Multiemployer plan a. A plan is a multi-employer plan if:(1) more than one employer is required to contribute, (2) the plan is maintained pursuant to one or more collective bargaining agreements, and (3) an election under Code section 414(f)(5) and ERISA section 3(37)(E) has not been made. (2) Single-employer plan (Other than a multiple-employer plan) a. A single-employer plan is an employee benefit plan maintained by one employer or one employee organization. Most employers will select “Single-employer plan. (3) Multiple-employer plan a. A multiple-employer plan is a plan that is maintained by more than one employer and is not one of the plans already described. Do NOT check this box if the employers maintaining the plan are members of the same controlled group. (4) DFE (specify) NOTE: A "controlled group" is generally considered one employer for Form 5500 purposes, and would usually check “Single-employer plan.” Part I,B-- Check the box(es) which indicates: (1) first return filed for this plan (2) already filed for this plan year submitting an amended return (3) plan no longer exists, and this is the final return a. Do NOT mark final return/report here if you are reporting participants and/or assets at the end of the plan year. (4) return is being filed for a plan of less than 12 months Part I,C -- Check this box if the benefits paid are subject to the collective bargaining process (even if only some of the employees covered by the plan are members of a collective bargaining unit.) Part I,D -- Check this box if an extension of time was filed. Attach a photocopy of the completed and signed Form 5558, “Application for Extension of Time to File Certain Employee Plan Returns,” you filed. © 2006 MHM Resources, Inc. 7-58 Section 125 Cafeteria Plan Administrators Training Part II,1a -- Enter the formal name of the plan. Part II,1b -- Enter the three-digit number assigned to the plan. All welfare or fringe benefit plan numbers start at 501 Part II,1c -- Enter the date the plan first became effective. Type name of individual signing as plan administrator Type name of individual signing as employer or plan sponsor Part II,2a -- Enter the name and address of the sponsor. This would be the employer's name if this return is for a singleemployer plan. Part II,2b -- Enter the nine-digit Employer ID number assigned to the plan sponsor. Part II,2c -- Enter the sponsor's phone number. Part II,2d -- Enter the six-digit business code that best describes the nature of the employer's business. (See the code listing provided in the CPMS Supplement) Part II,3a -- Enter the name and address of the plan administrator. Usually the administrator is the sponsor even if someone else is doing the bookkeeping. If that is the case enter "Same". Part II,3b -- Enter the administrator's EIN. Leave blank if 3a is "Same". Part II,3c -- Enter phone number of administrator. Leave blank if 3a is "Same". Part II,4 -- If name and/or EIN of the plan sponsor is different than last return 4a Enter the sponsor's name from the last return/report 4b Sponsor's EIN from the last return/report 4c Plan number from the last return/report Part II,5a -- (Optional) Enter the name and address of the preparer of this Form 5500 5b -- (Optional) Enter the EIN of the preparer 5c -- (Optional) Enter the phone number of the preparer Part II, 6 –- Enter the total number of participates in the health FSA portion of the cafeteria plan as of the first day of the plan year. Part II,7a –- Enter the total number of participates in the heath FSA portion of the cafeteria plan as of the end of the plan year. Enter 0 (zero) if you marked Line B of Part I as a final return/report. © 2006 MHM Resources, Inc. 7-59 Section 125 Cafeteria Plan Administrators Training 7b –- Enter the number of retired or separated participants receiving benefits as of the end of the plan year. Enter 0 (zero) if you marked Line B of Part I as a final return/report. 7c –- Enter the number of other retired or separated participants entitled to future benefits. Enter 0 (zero) if you marked Line B of Part I as a final return/report. 7d –- Enter total of lines 7a, 7b and 7c and proceed to line 8. Enter 0 (zero) if you marked Line B of Part I as a final return/report. Part II,8b -– Check this box to indicate you are filing this form for a welfare benefit plan AND enter the Characteristic Code of 4A to indicate you are filing for a health plan that is other than dental or vision) Part II,9a –- Check all boxes that apply to indicate the funding and benefit and 9b arrangements used during the plan year. Generally the funding and benefit arrangements for a Section 125 Cafeteria Plan are “General assets of the sponsor.” Check your plan document for specific funding and benefit arrangements. . General Processing Tips If the current year Form 5500 is not available before the due date of a short plan year return/report, use the latest Form 5500 available and enter the dates the short plan year began and ended in Part I. A separate Form 5500, with box A(2) checked, must be filed by each employer participating in a plan or program of benefits in which the funds attributable to each employer are available to pay benefits only for that employer’s employees, even if the plan is maintained by a controlled group. EFAST Processing Tips Paper forms must be obtained from the IRS or printed using software from an EFAST approved software developer. Original forms are preferable. Photocopies may be rejected or cause correspondence requiring additional information. All information should be in the specific fields or boxes provided on the forms and schedules. Information entered outside of the fields or boxes may not be processed. Do not use felt tip pens or other writing instruments that can cause signatures or data to bleed through to the other side of the paper. One-sided documents should have not markings on the blank side. Paper should be clean without glue or other sticky substances. Do not staple the forms. Use binder clips or other fasteners that do not perforate the paper. Do not submit extraneous material or information, such as arrows used to indicate where to sign, notes between preparers of the report, notations on the form, e.g., “DOL copy,” etc. Do not submit unnecessary or blank schedules. Except for certain Schedule SSA filings specifically permitted by the instructions, schedules should be submitted only with a Form 5500 or in response to correspondence from the Pension and Welfare Benefits Administration (PWBA) regarding the processing of your return/report. Manual entries on the machine print forms are not permitted. Submit all schedules (including the correct number of schedules) for which a box is checked on Form 5500, Part II, line 10. Do not attach or send any payments to EFAST. As of July 1, 2001, all Forms 5500 (including 1998 and prior year Forms 5500, 5500-C/R, and 5500-EZ) must be filed with the EBSA. © 2006 MHM Resources, Inc. 7-60 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-61 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-62 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-63 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-64 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-65 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-66 Section 125 Cafeteria Plan Administrators Training Employee/Participant Flexible Benefit Plan — Authorization for Direct Deposit of Reimbursement Claims Employee/Participant Name: ____________________________ Employee SSN __________________ Company Name: ______________________________________ I hereby authorize MHM Business Services, Inc. to initiate credit entries to my: checking account or savings account indicated below and the depository named below (Depository) to credit the same to such account. **An actual voided check must be attached** Staple voided check here This form will be not be processed without a voided check Account Number: ________________________________________________ ______________ Depository (Financial Institution): _________________________ City:______________________________________________ ___ Branch:____________________ State :________________________ Bank ACH Transit Routing Number ________________________________________________ This authority will remain in full force and effect until MHM Business Services, Inc. has received written notification from me of its termination in such time and in such manner as to afford MHM Business Services a reasonable opportunity to act on it. Signature _________________________________________ Date ______________________ Fax or mail to: 1-555-555-1212 Company Name Company Address © 2006 MHM Resources, Inc. 7-67 Section 125 Cafeteria Plan Administrators Training Worksheet for Estimating Medical Expenses Not Paid by Insurance: Name: ________________________________________________ 1. Recurring Expenses a. b. c. d. e. f. g. h. 2. Vision or hearing care (hearing aids, contacts, eyeglasses, etc.) ................................................................. $ Medicine and drugs excluding vitamins (prescribed by a doctor) ...................................................... Contraceptives (birth control pills) ..................................... Dental expense not paid by insurance (cleaning, check-ups, braces, root canals, extractions, etc.) ................ Blood work.......................................................................... b. c. d. e. f. g. h. i. j. k. l. m. 194.00 _____________ 80.00 _____________ Physical exams .................................................................... 150.00 Child birth ........................................................................... _____________ Hospitalization, dental, disability, or cancer insurance paid by you other than what is deducted from your paycheck ... _____________ i. Other medical treatments .................................................... Nonrecurring expenses a. 150.00 Wheelchairs for the disabled and extra automobile costs to accommodate wheelchair ....................................... Special instructions for the deaf or blind ............................ Special plumbing fixtures for the handicapped .................. Inclinator for stairs after heart attack .................................. Fluoride equipment for home water supply ........................ Special food and beverage costs as prescribed by doctor ... Transportation to receive healthcare (10 cents per mile) .... Oxygen equipment .............................................................. Health institution fees for physical or mental illness .......... Psychiatric therapy, psychologist treatments ...................... Therapeutic care for drug and alcohol addiction ................ Nonpermanent air-conditioning devices and operating costs if prescribed by doctor ............................... Other medical expenses ...................................................... Total Expense Estimate for the Year .............................................. (add 1a. - 1i. plus 2a. - 2m.) © 2006 MHM Resources, Inc. 7-68 50.00 _____________ _____________ _____________ _____________ _____________ _____________ _____________ _____________ _____________ _____________ _____________ _____________ _____________ 624.00 Section 125 Cafeteria Plan Administrators Training Flexible Benefit (Cafeteria Plan) Tax-Saving Survey For: Bill Crystal Date: 12/15/07 The purpose of this survey is to collect the information needed to determine your tax savings, if any, by participating in the proposed Plan. A detailed analysis will be returned to you based on this information. Some questions require estimation. When in doubt, be conservative. This information is taken in confidence and will not be distributed or used for any other reason. Employee General Information: A. B. C. D. E. F. G. H. I. J. K. L. M. Payroll system identification number 789-65-4123 Name (First, Initial, Last) Bill Crystal_________________________________________ Address line 1 4321 North 123rd Street________________________________________ Address line 2 _________________________________________________________________________ City – State Mission , KS_____________________________________ Zip 66221 -______________ ____________________________________________________ Social security number 789 65 _________ 4123 _________ Phone (optional)________________________________________________________________________ Date of birth 11-1-83 (required to estimate S.S. benefits) Pay checks per year (52, 48, 26, 24, 12) 26__________________________________________ Number of dependents 1_________________________________________________________ Department Production_________________________________________________________ Filing status Married, filing jointly__________________________________________________ (S-Single, M-Married joint, M-Married separate, H-Head of Household) . Employee Income and Expense Information: From your paycheck stub, please enter the amounts for 1 pay period, not year-to-date. Gross wages ................................................................................................................. $ 1,000.00 1. Federal taxes ......................................................................................................... 145.30 2. State, local, and other taxes ................................................................................. 47.40 3. Other pretax deductions (i.e. 402K)........................................................................ ______________ 4. Other taxable deductions ........................................................................................ ______________ 5. Group-term insurance ............................................................................................. 1.50 6. Group hospital insurance ........................................................................................ 115.00 O. Total deductions (Add lines 1 through 6) ...................................................................... 309.20 P. Pay check amount (Line N minus line O) .................................................................... $ 690.80 Estimated benefit plan elections per paycheck: Q. Medical Care Expenses ................................................................................................ $ 24.00 R. Dependent Care ........................................................................................................... $ 120.00 N © 2006 MHM Resources, Inc. 7-69 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-70 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-71 Section 125 Cafeteria Plan Administrators Training UPDATED CHARTS ARE LOCATED AT: http://www.mhmresources.com/er_dccvsfsa.htm Dependent Care Credit vs. Dependent Care FSA Calendar Year 2003 2004 Tax Rates - Married, filing Joint 2 Eligible Dependents $6,000 $6,000 Daycare expense AGI credit Flex Tax Flex Best But Tax Tax Tax credit Tax Over not over credit % Savings savings* $1,000 savings* Diff. Option $0 $14,300 35% $2,100 $883 $350 $1,233 ($868) Credit $14,300 $15,000 35% $2,100 $1,133 $350 $1,483 ($618) Credit $15,000 $17,000 34% $2,040 $1,133 $340 $1,473 ($568) Credit $17,000 $19,000 33% $1,980 $1,133 $330 $1,463 ($518) Credit $19,000 $21,000 32% $1,920 $1,133 $320 $1,453 ($468) Credit $21,000 $23,000 31% $1,860 $1,133 $310 $1,443 ($418) Credit $23,000 $25,000 30% $1,800 $1,133 $300 $1,433 ($368) Credit $25,000 $27,000 29% $1,740 $1,133 $290 $1,423 ($318) Credit $27,000 $29,000 28% $1,680 $1,133 $280 $1,413 ($268) Credit $29,000 $31,000 27% $1,620 $1,133 $270 $1,403 ($218) Credit $31,000 $33,000 26% $1,560 $1,133 $260 $1,393 ($168) Credit $33,000 $35,000 25% $1,500 $1,133 $250 $1,383 ($118) Credit $35,000 $37,000 24% $1,440 $1,133 $240 $1,373 ($68) Credit $38,050 $39,000 23% $1,380 $1,133 $230 $1,363 ($18) Credit $39,000 $41,000 22% $1,320 $1,133 $220 $1,353 $33 Flex $41,000 $43,000 21% $1,260 $1,133 $210 $1,343 $83 Flex $43,000 $58,100 20% $1,200 $1,133 $200 $1,333 $133 Flex $58,100 $87,900 20% $1,200 $1,633 $200 $1,833 $633 Flex $87,900 $117,250 20% $1,200 $1,323 $200 $1,523 $323 Flex $117,250 $178,650 20% $1,200 $1,473 $200 $1,673 $473 Flex *125 Tax Savings percentage applied to $5,000 © 2006 MHM Resources, Inc. 7-73 Section 125 Cafeteria Plan Administrators Training 1 Eligible Dependent $3,000 $3,000 Daycare expense AGI 125 Tax But Tax Tax Tax credit Over not over credit % credit savings* $0 $0 $14,300 35% $1,050 $530 $0 $14,300 $15,000 35% $1,050 $680 $15,000 $17,000 34% $1,020 $17,000 $19,000 33% $19,000 $21,000 $21,000 Best Diff. Option $530 ($521) Credit $0 $680 ($371) Credit $680 $0 $680 ($341) Credit $990 $680 $0 $680 ($311) Credit 32% $960 $680 $0 $680 ($281) Credit $23,000 31% $930 $680 $0 $680 ($251) Credit $23,000 $25,000 30% $900 $680 $0 $680 ($221) Credit $25,000 $27,000 29% $870 $680 $0 $680 ($191) Credit $27,000 $29,000 28% $840 $680 $0 $680 ($161) Credit $29,000 $31,000 27% $810 $680 $0 $680 ($131) Credit $31,000 $33,000 26% $780 $680 $0 $680 ($101) Credit $33,000 $35,000 25% $750 $680 $0 $680 ($71) Credit $35,000 $37,000 24% $720 $680 $0 $680 ($41) Credit $38,050 $39,000 23% $690 $680 $0 $680 ($11) Credit $39,000 $41,000 22% $660 $980 $0 $980 $320 Flex $41,000 $43,000 21% $630 $980 $0 $980 $350 Flex $43,000 $58,100 20% $600 $980 $0 $980 $380 Flex $58,100 $87,900 20% $600 $980 $0 $980 $380 Flex $87,900 $117,250 20% $600 $794 $0 $794 $194 Flex $117,250 $178,650 20% $600 $884 $0 $884 $284 Flex © 2006 MHM Resources, Inc. 7-74 Section 125 Cafeteria Plan Administrators Training 1 Eligible Dependent $5,000 $5,000 Daycare expense AGI 125 Tax But Tax Tax Tax credit Over not over credit % credit savings* $0 $0 $14,300 35% $1,050 $883 $0 $14,300 $15,000 35% $1,050 $1,133 $15,000 $17,000 34% $1,020 $17,000 $19,000 33% $19,000 $21,000 $21,000 Best Diff. Option $883 ($168) Credit $0 $1,133 $83 Flex $1,133 $0 $1,133 $113 Flex $990 $1,133 $0 $1,133 $143 Flex 32% $960 $1,133 $0 $1,133 $173 Flex $23,000 31% $930 $1,133 $0 $1,133 $203 Flex $23,000 $25,000 30% $900 $1,133 $0 $1,133 $233 Flex $25,000 $27,000 29% $870 $1,133 $0 $1,133 $263 Flex $27,000 $29,000 28% $840 $1,133 $0 $1,133 $293 Flex $29,000 $31,000 27% $810 $1,133 $0 $1,133 $323 Flex $31,000 $33,000 26% $780 $1,133 $0 $1,133 $353 Flex $33,000 $35,000 25% $750 $1,133 $0 $1,133 $383 Flex $35,000 $37,000 24% $720 $1,133 $0 $1,133 $413 Flex $38,050 $39,000 23% $690 $1,133 $0 $1,133 $443 Flex $39,000 $41,000 22% $660 $1,633 $0 $1,633 $973 Flex $41,000 $43,000 21% $630 $1,633 $0 $1,633 $1,003 Flex $43,000 $58,100 20% $600 $1,633 $0 $1,633 $1,033 Flex $58,100 $87,900 20% $600 $1,633 $0 $1,633 $1,033 Flex $87,900 $117,250 20% $600 $1,323 $0 $1,323 $723 Flex $117,250 $178,650 20% $600 $1,473 $0 $1,473 $873 Flex Note: State and local tax savings were not taken into consideration. State and local taxes vary in percentages and dependent care credit availability © 2006 MHM Resources, Inc. 7-75 Section 125 Cafeteria Plan Administrators Training Dependent Care Credit vs. Dependent Care FSA Calendar Year 2003 2003 Tax Rates - Single, Head of Household 2 Eligible Dependents Daycare $6,000.00 Daycare expense expenses AGI Credit Flex Tax Flex Best But Tax Tax Tax credit Tax Over not over credit % Savings Savings* $1,000 Savings* Diff. Option $0 $10,200 35% $2,100.00 $883 $350 $1,233 ($868) Credit $10,200 $15,000 35% $2,100.00 $1,133 $350 $1,483 ($618) Credit $15,000 $17,000 34% $2,040.00 $1,133 $340 $1,473 ($568) Credit $17,000 $19,000 33% $1,980.00 $1,133 $330 $1,463 ($518) Credit $19,000 $21,000 32% $1,920.00 $1,133 $320 $1,453 ($468) Credit $21,000 $23,000 31% $1,860.00 $1,133 $310 $1,443 ($418) Credit $23,000 $25,000 30% $1,800.00 $1,133 $300 $1,433 ($368) Credit $25,000 $27,000 29% $1,740.00 $1,133 $290 $1,423 ($318) Credit $27,000 $29,000 28% $1,680.00 $1,133 $280 $1,413 ($268) Credit $29,000 $31,000 27% $1,620.00 $1,133 $270 $1,403 ($218) Credit $31,000 $33,000 26% $1,560.00 $1,133 $260 $1,393 ($168) Credit $33,000 $35,000 25% $1,500.00 $1,133 $250 $1,383 ($118) Credit $35,000 $37,000 24% $1,440.00 $1,133 $240 $1,373 ($68) Credit $37,000 $38,900 23% $1,380.00 $1,133 $230 $1,363 ($18) Credit $38,900 $39,000 23% $1,380.00 $1,633 $230 $1,863 $483 Flex $39,000 $41,000 22% $1,320.00 $1,633 $220 $1,853 $533 Flex $41,000 $43,000 21% $1,260.00 $1,633 $210 $1,843 $583 Flex $43,000 $87,900 20% $1,200.00 $1,633 $200 $1,833 $633 Flex $87,900 $105,500 20% $1,200.00 $1,323 $200 $1,523 $323 Flex $105,500 $162,700 20% $1,200.00 $1,473 $200 $1,673 $473 Flex *Flex percentage applied to $5,000 and $1,000 to Credit © 2006 MHM Resources, Inc. 7-76 Section 125 Cafeteria Plan Administrators Training 1 Eligible Dependent Daycare $3,000.00 Daycare expense expenses AGI 125 Tax But Tax Tax Tax credit Over not over credit % credit savings* $0 $0 $10,200 35% $1,050.00 $530 $0 $10,200 $15,000 35% $1,050.00 $680 $15,000 $17,000 34% $1,020.00 $17,000 $19,000 33% $19,000 $21,000 $21,000 Best Diff. Option $530 ($521) Credit $0 $680 ($371) Credit $680 $0 $680 ($341) Credit $990.00 $680 $0 $680 ($311) Credit 32% $960.00 $680 $0 $680 ($281) Credit $23,000 31% $930.00 $680 $0 $680 ($251) Credit $23,000 $25,000 30% $900.00 $680 $0 $680 ($221) Credit $25,000 $27,000 29% $870.00 $680 $0 $680 ($191) Credit $27,000 $29,000 28% $840.00 $680 $0 $680 ($161) Credit $29,000 $31,000 27% $810.00 $680 $0 $680 ($131) Credit $31,000 $33,000 26% $780.00 $680 $0 $680 ($101) Credit $33,000 $35,000 25% $750.00 $680 $0 $680 ($71) Credit $35,000 $37,000 24% $720.00 $680 $0 $680 ($41) Credit $37,000 $38,900 23% $690.00 $680 $0 $680 ($11) Credit $38,900 $39,000 23% $690.00 $980 $0 $980 $290 Flex $39,000 $41,000 22% $660.00 $980 $0 $980 $320 Flex $41,000 $43,000 21% $630.00 $980 $0 $980 $350 Flex $43,000 $87,900 20% $600.00 $980 $0 $980 $380 Flex $87,900 $105,500 20% $600.00 $794 $0 $794 $194 Flex $105,500 $162,700 20% $600.00 $884 $0 $884 $284 Flex © 2006 MHM Resources, Inc. 7-77 Section 125 Cafeteria Plan Administrators Training 1 Eligible Dependent Daycare $5,000.00 Daycare expense expenses AGI Flex Tax But Tax Tax Tax credit Over not over credit % credit savings* $0 $0 $10,200 35% $1,050.00 $883 $0 $10,200 $15,000 35% $1,050.00 $1,133 $15,000 $17,000 34% $1,020.00 $17,000 $19,000 33% $19,000 $21,000 $21,000 Best Diff. Option $883 ($168) Credit $0 $1,133 $83 Flex $1,133 $0 $1,133 $113 Flex $990.00 $1,133 $0 $1,133 $143 Flex 32% $960.00 $1,133 $0 $1,133 $173 Flex $23,000 31% $930.00 $1,133 $0 $1,133 $203 Flex $23,000 $25,000 30% $900.00 $1,133 $0 $1,133 $233 Flex $25,000 $27,000 29% $870.00 $1,133 $0 $1,133 $263 Flex $27,000 $29,000 28% $840.00 $1,133 $0 $1,133 $293 Flex $29,000 $31,000 27% $810.00 $1,133 $0 $1,133 $323 Flex $31,000 $33,000 26% $780.00 $1,133 $0 $1,133 $353 Flex $33,000 $35,000 25% $750.00 $1,133 $0 $1,133 $383 Flex $35,000 $37,000 24% $720.00 $1,133 $0 $1,133 $413 Flex $37,000 $38,900 23% $690.00 $1,133 $0 $1,133 $443 Flex $38,900 $39,000 23% $690.00 $1,633 $0 $1,633 $943 Flex $39,000 $41,000 22% $660.00 $1,633 $0 $1,633 $973 Flex $41,000 $43,000 21% $630.00 $1,633 $0 $1,633 $1,003 Flex $43,000 $87,900 20% $600.00 $1,633 $0 $1,633 $1,033 Flex $87,900 $105,500 20% $600.00 $1,323 $0 $1,323 $723 Flex $105,500 $162,700 20% $600.00 $1,473 $0 $1,473 $873 Flex Note: State and local tax savings were not taken into consideration. State and local taxes vary in percentages and dependent care credit availability © 2006 MHM Resources, Inc. 7-78 Section 125 Cafeteria Plan Administrators Training Employer Claim For Reimbursement Sample Report Company Name Billy Crystal ____________________________________ Social Security # _____ 444-66-3377 Employee # __________________ Dependent Care Expense Claims Name of Dependents Period Covered From Bill Jr. Name, Address and Taxpayer Identification Number of Provider of Service Amount Incurred To 9/1/07 9/30/07 Wilma Simpson 190.00 234-56-7890 TOTAL DEPENDENT CARE EXPENSE CLAIM 190.00 *NOTE: The total amount claimed under the Plan for any coverage period must not exceed the lesser of your earned income for the plan year or the earned income of your spouse. (If your spouse is either a full-time student or is incapable of taking care of himself or herself, then he or she is deemed to have monthly earnings of $200 if there is one (1) child or dependent, and $400 if there are two (2) or more.) No payment may be made under the Plan if the service provider is your dependent for federal income tax purposes, or is your child or stepchild and is under age 19. Unreimbursed Medical Expense Claims Date Expense Incurred Name of Service Provider Expense Description Person for Whom Expense Incurred Net Amount 9/14/07 Children’s Clinic Office Visit Bill Jr. 35.00 9/14/06 K-Mart Prescription Bill Jr. 10.00 7/9/07 Dr. Glass Contacts Bill Sr. TOTAL MEDICAL CARE EXPENSE CLAIM 250.00 295.00 285.00 READ CAREFULLY The undersigned participant in the Plan certifies that all expenses for which reimbursement or payment is claimed by submission of this form were incurred during a period while the undersigned was covered under the Company’s Flexible Spending Plan with respect to such expenses and that the medical expenses have not been reimbursed or are not reimbursable under any other health plan coverage. The undersigned fully understands that he or she alone is fully responsible for the sufficiency, accuracy, and veracity of all information relating to this claim which is provided by the undersigned, and that unless an expense for which payment or reimbursement is claimed is a proper expense under the Plan, the undersigned may be liable for payment of all related taxes including federal, state, or city income tax on amounts paid from the Plan which relate to such expense. Billy Crystal ___________________________________________ Employee’s Signature © 2006 MHM Resources, Inc. 11/22/07 _________________________________________________ Date 7-79 Section 125 Cafeteria Plan Administrators Training Guide to Allowable Medical Expenses Reimbursed through an IRC Section 125 Cafeteria Plan 1. Date Expense Incurred a. Services were rendered during employer’s cafeteria plan year b. Services were rendered during the participant’s eligible period of coverage 2. Whose medical expenses can you include? a. Participant b. Spouse c. Dependents i. A person that lived with participant for the entire year as a member of participant’s household or is related to participant. ii. Person was a U.S. citizen or resident, or a resident of Canada or Mexico for some part of the calendar yea in which participant’s tax year began. iii. Participant provided over half of that person’s total support for the calendar year. iv. Adopted child 1. Child qualified as participant’s dependent when the medical services were provided. v. Child of divorced or separated parents 1. If either parent can claim a child as a dependent under the rules for divorced or separated parents, each parent can include the medical expenses he or she pays for the child even if an exemption for the child is claimed by the other parent. vi. Support claimed under a multiple support agreement 1. If participant is considered to have provided more than half of a person’s support under such an agreement, the participant can claim medical expenses for that person. 3. Medical Definitions a. Amounts paid for the diagnosis, cure, mitigation, treatment or prevention of disease, or for the purpose of affecting any structure or function of the body. b. Transportation for and essential to medical care c. Legally obtained drugs or biologicals that require the prescription of a physician or is proved to be medically necessary for use by individual d. Cosmetic surgery or other similar procedure to treat a deformity relating to congenital abnormality, a personal injury, or disfiguring disease. i. Procedure promotes the proper function of the body e. Excess Cost f. Capital expense item for medical care i. Permanently improve property ii. Only expenses in excess of the increase in the value of the related property iii. Operation or maintenance expenses of a qualifying medical capital asset © 2006 MHM Resources, Inc. 7-80 Section 125 Cafeteria Plan Administrators Training 4. Primary Purpose Test a. Was the expense incurred at the direction or suggestion of a physician? b. Did the treatment bear directly on the physical condition in question? c. Did the treatment have a direct or proximate therapeutic relation to the bodily condition so as to justify a reasonable belief that it would produce the desired results? d. Was the treatment proximate in time to the onset or recurrence of the disease or condition so as to make the treatment specific to the condition rather than for general physical improvement? 5. “But For” Test a. Would the medical expense have been incurred “but for” the disease or illness? 6. Reasonableness Test a. Is the medical expense reasonable? b. Is the expenditure for other than personal, living, and family expenses? 7. Factual Determination Test a. Based on the facts and circumstances, was the medical expense incurred to prevent or alleviate a medical condition? © 2006 MHM Resources, Inc. 7-81 Section 125 Cafeteria Plan Administrators Training 8. © 2006 MHM Resources, Inc. 7-82 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-83 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-84 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-85 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-86 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-87 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-88 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-89 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-90 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-91 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-92 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-93 Section 125 Cafeteria Plan Administrators Training ^TodaysDate ^EmpName ^EmpAddress1 ^EmpAddress2 ^EmpCity, ^EmpState ^EmpZip We recently received the following Claim for Reimbursement: Account Type: Claim Description: Claim Amount: Service Start Date: Service End Date: ^Benefit ^ClaimDesc ^Amount ^StartDate ^EndDate The amount of ^RejAmount cannot be approved for payment because of the following reason(s): Any Additional expenses listed on this claim form have been processed. Refer to your Summary Plan Description for your additional rights and obligations concerning the claims denial process. Please return your corrected claim form, if applicable, at your earliest convenience. Do not resubmit the additional expenses on this claim form that we have processed. If you have any questions, please contact our Claims Processing Service Center at 1-800555-1212 or via e-mail at help@TPA.com Thank You Third Party Administrator © 2006 MHM Resources, Inc. 7-94 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-95 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-96 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-97 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-98 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-99 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-100 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-101 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-102 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-103 Section 125 Cafeteria Plan Administrators Training Over-The-Counter Drugs Can Now Be Reimbursed Through Health FSAs! For years, receiving guidance on cafeteria plans was like trying to get money from a distant relative. Now, Section 125 cafeteria plans are the IRS’ new, best friend, and the IRS has arrived at the door with their bags packed and ready for a lengthy stay. This is the first in a series of articles concerning the far-reaching effects of IRS Revenue Ruling 2003-102 making certain over-the-counter (OTC) medications eligible for reimbursement through FSAs. The second article will be a discussion of how the Revenue Ruling affects employees. It will ask the questions you will face from participants and provide factual, real-life answers. Article three will deal with debit cards – How should the smart agent, broker, or Third Party Administrator (TPA) be educating employees about the use of debit cards? You might be surprised at the consequences this new Revenue Ruling has on employees and their debit card habits. Background Several events have prompted the IRS’ renewed interest in FSAs. Rising health costs, consumer demands, prescription drugs becoming over-the-counter, and it didn’t hurt that federal employees made their first-time elections into FSAs this last summer. The following quotes were included in the IRS-Newswire e-mail announcing the Revenue Ruling: “Flexible Spending Accounts are an important tool in helping people meet their health care costs,” stated Treasury Secretary John Snow. “Since many prescription drugs have moved to the OTC market, this action today makes paying for them a little bit easier to swallow.” “Flexible Spending Accounts were established under the tax code to provide incentives for better health care,” said IRS Commissioner Mark W. Everson. “This action is a sensible expansion and simplification of the program consistent with existing law.” New Rules From The IRS The example to establish the facts for this ruling is very simple. The employer sponsors a health flexible spending arrangement (Health FSA) and a participant in the employer’s plan makes certain purchases at a pharmacy. The purchases include an antacid, an allergy medicine, a pain reliever, and a cold medicine. The participant also purchases vitamins. At this point in the ruling, it is made clear that these purchases could have been for the use of the participant, or the participant’s spouse or dependents. It is also stated that the purchases were incurred during the current Health FSA plan year. The Revenue Ruling concludes that: “There is no requirement in § 105(b) that the expense be allowed as a deduction for medical care under § 213(a) or that only medicines or drugs that require a physician’s prescription be taken into account.” Therefore, the antacid, allergy medicine, pain reliever, and cold medicine claims may be reimbursed from a Health FSA. However the purchase of dietary supplements, like vitamins, would not be an eligible expense because they are merely beneficial to the general health of the participant or the participant’s spouse or dependents. What Are OTC Medications? The Revenue Ruling expressly points out common purchases for pain relievers and allergy medicine. But what about creams or lotions used to alleviate arthritis pain or the itching from poison ivy? If the cream or lotion is an expenditure for medical care – to cure or treat a disease, the expense should be allowed as an eligible medical expense to be reimbursed through an employer’s Health FSA. © 2006 MHM Resources, Inc. 7-104 Section 125 Cafeteria Plan Administrators Training Claims Adjudication What can Third Party Administrators (TPAs) use as their guide? It’s as easy as reading the description on the box for an OTC medications rule. For instance, if the box reads, “Relieves the cough and stuffy nose associated with a cold or allergy,” it would pass the test. Generally a dietary supplement like vitamin E carries no such claim. But what about the recommendation from the doctor to take a specified dose of vitamin E for relief from psoriasis? With a doctor’s letter stating the medial condition, specified time period, and “prescription” for a dietary supplement – a TPA could be confident with accepting this type of expense as eligible to be reimbursed from a Health FSA. TPAs may find there are certain medications that could be considered medically necessary in some conditions, but for general health in other instances (i.e., weight-loss products). For an individual with an underlying disease or who is obese, the weight-loss product would be medically necessary. However, if the individual just wants to drop 10 pounds before the high school reunion, the same weight-loss product would be considered a personal use item. The same reasoning would apply for OTC nicotine gum and patches. When claims for these types of items are turned in, the TPA should ask for a doctor’s letter to determine medical necessity. Claritin - When Can You Accept The Receipts? The Revenue Ruling did not reveal a specific date for implementation. However, it did state that the sample employee “submits substantiated claims for all of these expenses, which have been incurred during the current plan year, …” TPAs should reasonably be able to pay for eligible OTC medications that were incurred during the participant’s current plan year. In spite of the effect this Revenue Ruling has on the amount and type of expenses that can be reimbursed through a Health FSA, an employee cannot change an annual election without a valid change in status. These change in status rules are outlined in the final IRS Regulations Section 1.125-4. Check The Plan Document Before reimbursing any “unusual” items, check the employer’s plan document. The employer’s Health FSA or Health Reimbursement Arrangement (HRA) plan might contain language that would prohibit introducing OTC drug reimbursement. Look for the plan document and Summary Plan Description (SPD) to reference IRC Section 213(d) as the guidance for eligible medical expenses. Will Debit Card Swipes Be Paperless? The news that OTC medications can be reimbursed from your Health FSA isn’t all good. If a debit card is used to pay for both OTC drugs and prescription co-pays, most TPAs will require that participants submit receipts for verification or force the employee to repay the swipe. Why? Because the total amount on a single card receipt (for two or more items) cannot be electronically substantiated under the new IRS Revenue Ruling 2002-43. According to the IRS, a card swipe will only be paperless if it is (1) an exact co-payment amount, (2) a verified recurring expense, or (3) the vendor provides additional information to the plan administrator at the point of sale. This is a very narrow window to hit since OTC drugs will rarely fall into any of these three categories. For example, a card swiped at the pharmacy for a $10 co-pay could be adjudicated electronically by matching it with the participant’s health plan co-pay. And, when a card swipe is “electronically adjudicated,” the employee will not be required to submit a paper receipt to the TPA. On the other hand, if the participant pays for a bottle of aspirin along with his drug co-pay, electronic adjudication will be impossible. That’s because the total on the card receipt cannot be matched with his $10 co-pay. In both cases, the card swipe should work and the vendor will get paid. But, in this case, the IRS requires that a paper receipt be provided to the TPA for verification purposes. Let’s look at an example of how typical debit card use is likely to change. Joe goes to the pharmacy to pick up a prescription. He also purchases cough medicine for his daughter and an antacid for his wife. He presents all the purchases to the pharmacist, along with his Health FSA debit card, which processes © 2006 MHM Resources, Inc. 7-105 Section 125 Cafeteria Plan Administrators Training everything on one card swipe. According to Revenue Ruling 2003-43 on debit cards, the swipe would work at this merchant because pharmacies are considered a qualified vendor. In other words, the card swipe would work at the checkout counter so the pharmacy gets paid. However, the swipe could not be electronically adjudicated by the TPA because it does not match Joe’s pharmacy co-payment amount, nor is it a recurring expense. In this scenario, the TPA would notify Joe that further information is needed for this transaction, and copies of receipts must be submitted. Information from the receipts must be reviewed by the TPA, and the participant will be released of further obligation. But what if Joe had merely swiped his card only for the prescription co-pay? The card will work at the checkout counter. This claim could be electronically adjudicated, and no further information would be requested. Joe would then turn in a paper claim for the OTC items. Eventually, Joe will adjust his purchasing habits and swipe his debit card only once for all eligible medical expenses. He can then turn in a single receipt verification form to cover all the items on the swipe. After all, he knows he will need to respond to the inevitable request from the TPA to fax his receipts for confirmation. In this case, the biggest advantage to Joe is that by swiping the debit card, the pharmacy got paid. And Joe didn’t have to reach into his pocket to pay and wait for a reimbursement. More Work For The TPA? Not necessarily. However, the TPA will need a system built to automatically generate requests for additional information, an Internet claims entry arrangement, and electronic processing of Internet claims. The TPA’s system must have a fully automated method of retrieving improper payments made from the plan, and seeking restitution from the employee, employer, and automatically shutting off debit card privileges. © 2006 MHM Resources, Inc. 7-106 Section 125 Cafeteria Plan Administrators Training New law establishes Health Savings Accounts. Cafeteria Plan Comparison Table Flex Tech Links Free Newsletter 125Plan.com The Medicare Bill just signed by President Bush contained great news. Added at the very end of this lengthy legislation was a valuable new benefit. It's a healthcare reimbursement account that rolls forward, is portable, and can be offered through a Section 125 Cafeteria Plan. Participants must be covered by a high-deductible health insurance product, but the rest of the rules are easy and simple to live with. The newly coined Health Savings Account (HSA) is a carbon copy of the existing Archer Medical Savings Account (MSA) with two huge exceptions. First, employers of any size can set up a plan; and secondly, contributions may be made through the employer's cafeteria plan. Add a new benefit to any cafeteria plan Employers that already offer high-deductible health coverage, or are thinking about a higher-deductible product will want an HSA for their employees. HSAs reimburse all the same eligible expenses as a Health Flexible Spending Account, but without the fear of leaving money behind when the plan year ends or the participant changes jobs. Although an earlier version of this bill contained language that would allow FSA participants to carry forward $500 in unused funds, the HSA offers unlimited funds to be accrued every year. Just think of the jump in participation levels to the cafeteria plan when employees are offered this great new benefit. "Use it or lose it" can finally be dropped from everyone's vocabulary. Now let's get into the nuts and bolts of Health Savings Accounts. Health Savings Account (HSA) An HSA is an individual IRA type account that is established by an eligible individual in order to pay for qualified medical expenses. The participant owns the account. That means the HSA remains with the account beneficiary when changing jobs or health insurance coverage. In addition, unlike MSAs, both employers and employees can contribute to the account during the same calendar year. Who can establish an HSA? An individual under the age of 65 covered by a high-deductible health plan as of the 1st day of any month, and An individual not covered by any other health plan, which provides the same coverage as the high-deductible health plan. The account beneficiary may be covered by "permitted insurance" products and insurance that provides accident, disability, dental © 2006 MHM Resources, Inc. 7-107 Section 125 Cafeteria Plan Administrators Training care, vision care, or long-term care. "Permitted insurance" includes Worker's Compensation, tort liabilities, insurance coverage for ownership or use of property, other such similar liabilities, insurance for a specific disease or illness, or insurance that pays a fixed amount per day for hospitalization. What is a high-deductible product? Not less than $1,000 for single coverage with an out-of-pocket total not to exceed $5,000. Not less than $2,000 for family coverage with an out-of-pocket total not to exceed $10,000. Preventative care services are not subject to the deductible. Policies with out-of-network dollar requirements are not taken into consideration when determining the deductible or the out-of-pocket maximums. Contributions For single coverage, the lesser of the health plan deductible or up to a maximum of $2,600. For family coverage, the lesser of the health plan deductible or up to a maximum of $5,150. Individuals age 55-65 can make additional pre-tax "catch-up" contributions of $500 for 2004. This amount is increased until it reaches $1,000 in 2009 and thereafter. Amounts are doubled if the account beneficiary is married and both spouses are over 55 years of age. Contributions accumulate tax-free. HSA contributions must be coordinated with MSA contributions. The contribution limitations are decreased by any contributions to an MSA and/or employer contributions to the HSA. Employer contributions must be "comparable" (nondiscriminatory) in order to be excludible from the employee's income. A penalty tax is applied to employers who fail to make employee contributions in a nondiscriminatory manner. © 2006 MHM Resources, Inc. 7-108 Section 125 Cafeteria Plan Administrators Training Comparable for similarly situated employees means, comparable as to percentage or dollar amount. There are also special rules for employers who make contributions to Archer MSAs and Health Savings Accounts during the calendar year. Medicare eligible individuals may not make contributions to an HSA. The participant and their employer may make contributions to one HSA in the same calendar year. The employer will report employer contributions to the plan on the employee's W-2, and certain reporting requirements may be required of carriers. For example, insurance carriers may be asked to supply a comprehensive list of all individuals and/or families covered by a highdeductible health insurance product. More information about the type and timing of these reports will be released by the proper federal department later. Eligible reimbursements Health insurance may not be purchased from the HSA, except for COBRA continuation premiums or for health insurance coverage while an individual is receiving unemployment compensation. Long-term care insurance premiums may be paid from the account and at the individual's retirement age, any health insurance premiums, other than a Medicare supplemental policy made be paid with HSA funds. Payments from an HSA may be made on a tax-free basis for qualified medical expenses. These expenses include medical care for the account beneficiary, and their spouse and dependents. Medical care is defined in section 213(d). This does not include the clause that the expenses also be deductible for income tax purposes. So, over-the-counter drugs may be reimbursed from an HSA on a tax-free basis. Rollovers can be accepted into an HSA account from the account beneficiary's MSA account, or another HSA account. Rollover amounts transferred from one account to another must be completed within 60 days, and cannot occur more than once per year. If money is used for anything other than eligible medical expenses, the account beneficiary will have to pay normal taxes plus a 10% penalty of other monies drawn from the account. There is an exception for disability, death, or retirement where the penalty will not apply. Confused between HSA, FSA, HRA, or MSA? Check our Handy Comparison Chart Need help in sorting out all the flexible benefit choices? To assist you and your clients in choosing the account that's right for them, we've developed a side-by-side comparison chart. This chart emphasizes the different features for all flexible accounts. Also attached is an additional benefit comparison chart. MHM Resources Inc. 888-946-3539 © 2006 MHM Resources, Inc. 7-109 Section 125 Cafeteria Plan Administrators Training We respect your online privacy. If you feel you have received this e-mail in error, or do not wish to receive any further mailings, click here. Copyright 2003 MHM Resources Inc. The information contained in this e-mail is not intended to be legal, accounting, or other professional advice. We assume no liability whatsoever in connection with its use, nor are these comments directed to specific situations. © 2006 MHM Resources, Inc. 7-110 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-111 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-112 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-113 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-114 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-115 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-116 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-117 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-118 Section 125 Cafeteria Plan Administrators Training © 2006 MHM Resources, Inc. 7-119 Section 125 Cafeteria Plan Administrators Training