MICROBIOLOGICAL ANALYSIS OF THE AIR
advertisement

MICROBIOLOGICAL ANALYSIS OF
THE AIR.
Diploma: Environmental Protection, Year 3
Module: E318
Lecturer: Dr. Michael Broaders.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 1
READING LIST FOR AIR MICROBIOLOGY
See website. http://www.itsligo.ie/staff/mabroaders for more reference
material
Environmental Microbiology. 2000. Maier, R.A, Pepper, I.L & Gerba, C.P.
Academic Press.
C.H.Collins & AJ. Beale. 1992. Safety in Industrial Microbiology and
Biotechnology. Butterworth Heinemann. Isbn 0 7506 1105 7
660.6
Harriet A. Burge Bioaerosols.1995. CRC Press Inc. 0-87371-724-4.
..................613.5
Christopher S. Cox & Christopher M. Wathes. 1995. Bioaerosols Handbook.
CRC Press Inc. 1-87371-615-9 .............576.190961
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 2
RULES, REGULATIONS AND CODE OF CONDUCT FOR SAFETY IN THE
MICROBIOLOGY LABORATORY
APROPRIATE PROTECTIVE CLOTHING MUST
BE WORN IN THE
LABORATORY AT ALL TIMES.
SAFETY GLASSES TO BE WORN AT ALL TIMES.
(LABORATORY COATS MUST BE WORN AT ALL TIMES AND MUST BE
CLEAN AND FREE OF GRAFFITTI.)
BEHAVIOUR IN THE LABORATORY MUST BE APPROPRIATE TO REFLECT
SAFETY STANDARDS. (Performance and behaviour in the laboratory are taken into
account for CA marks.)
EATING, DRINKING AND SMOKING ARE NOT PERMITTED IN THE
LABORATORY.
HANDS MUST BE WASHED WITH SOAP ON ENTERING THE LABORATORY
AND AT ALL TIMES LEAVING THE LABORATORY.
BENCH TOPS MUST BE SWABBED WITH DISINFECTANT AT THE START
AND END OF EACH CLASS. (ETHANOL IS PROVIDED)
WASTE DISPOSAL BAGS ARE PROVIDED FOR PETRI DISHES AND OTHER
DISPOSABLES WHICH REQUIRE AUTOCLAVING.
WASTE DISPOSAL BINS ARE PROVIDED FOR WASTE PAPER .
DISCARD JARS ON THE BENCH TOPS CONTAINING DISINFECTANT ARE
PROVIDED FOR DISPOSAL OF GLASS SLIDES AND USED PIPETTES AND
PIPETTE TIPS
SINKS MUST NOT BE USED FOR WASTE DISPOSAL.
HANDLE ALL CULTURES AS IF POTENTIALLY PATHOGENIC (i.e
DANGEROUS DISEASE CAUSING ORGANISMS).
HANDLE ALL MATERIAL I.E, WATER FROM RIVERS/LAKES etc., SOIL,
SLUDGES AND MATERIALS FROM OTHER SOURCES AS CONTAINING
POTENTIAL PATHOGENS.
DO NOT LICK LABELS, PENCILS, FINGERS etc.
TRY TO PREVENT RUBBING YOUR EYES AND LIPS, BE AWARE OF THE
POSSIBILITY OF CONTAMINATION AT ALL TIMES.
THINK ASEPTIC TECHNIQUE AT ALL TIMES
IN CASE OF ACCIDENT (BREAKAGES, SPILLAGES etc.) INFORM THE
LECTURER IMMEDIATELY.
ALWAYS LEAVE THE LABORATORY CLEAN AND TIDY FOR YOUR NEXT
CLASS. Clean bench top of stains and put away microscopes, hot plates etc.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 3
Objectives
You should be able to:
prepare instruments for recovery of viable bioaerosol from the
air in occupied habitats
determine the materials required and prepare and sterilise all
materials for use with the instruments
operate the instruments, incubate the plates and record the
results
present the results in an acceptable format and be able to
analyse and manipulate the data to interpret the result
draw conclusions about the extent of contamination and the
use of the instruments in air analysis
Compare and contrast the use of instruments used in air
analysis
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 4
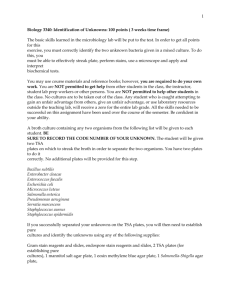
MICROBIOLOGICAL ANALYSIS OF THE AIR.
In this series of practicals you will sample the air in the Laboratory to
determine its microbial content.
The instruments and methods used in the analysis are as follows:1. Casella Slit–to–agar sampler (impactor) ;
2. Anderson Two Stage Sampler (impactor) ;
3. Millipore Liquid Impingement (as a demonstration only);
4. All Glass Liquid Impingement;
5. Hawksley Air Sampler (Filtration);
6. Biotest Centrifugal Air Sampler;
7. Surface Air Sampler (impactor) ;
8. Settle Plates (Passive)
From using these methods you will:a) compare the microbial loading of the atmosphere at each location in
terms of the total number of microorganisms per m3 of air i.e. the
total number of bacteria plus the total number of yeasts and
moulds.
It is desirable to present a breakdown of the microbial
populations
i.e. what are the percentages of bacteria and yeasts
and moulds present at each location.
What proportion of the microorganisms are
respirable, by using the Anderson sampler,
Also, of the bacterial population, what proportion are
Gram positive or Gram negative or rods or cocci.
By using selective media determine the proportion of
Staphylococci and Streptococci,
Identify the microorganisms (both bacteria and fungi)
as far as possible
b) compare the sampling efficiency of each device at each location. i.e.
compare the amount of bacteria and fungi collected at each location by
each device.
Present the results in proper manner using Tables, Graphs, Barcharts.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 5
MATERIALS AND PROCEDURES.
Casella Slit–to–Agar Sampler
Large Petri dishes (14.5 cm) are filled with agar medium to within 5 mm.
of the top of the dish, (approx. 200ml) and allowed to dry.
TSA is used to collect total bacteria.
Saboraud Dextrose Agar to select for yeasts and moulds.
Sucrose peptone nitrate agar for Actinomycetes.
Malt Agar (supplemented with either Triton N101 (500 mg/l) or Rose Bengal (50
mg/l) and the antibiotics penicillin (20 units/ml) and streptomycin (40 units/ml)) may
also be used.
Agar plates are incubated at the appropriate temperatures to allow the
microorganisms to develop.
Follow the procedure carefully as in the notes below.
The sampler works by drawing
air through one or more of the
narrow slits (1mm width)
positioned 0.2 cm above the
surface of the agar plate. While
the air is being drawn through the
machine, the plate is rotated
through 360° so that the
microorganisms are distributed
over the surface.
Both the volume of air per minute drawn through the machine and the
total time for the rotation of the plate, are variable and this data is used
to determine the volume of air passed through the sampler.
The total volume of air per plate can be varied from 87.5 litres to 3,500
litres. (Table 1).
For routine use 175 l/min for a 2 min. sampling time should be used.
(Total: 350 litres air sampled)
The volume of air passing through the sampler can be altered by blanking
off one or more slits and by adjusting the vacuum reading accordingly.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 6
If only one slit is used, the needle on the dial should be adjusted to the
first thin line. If two slits are used the needle should be adjusted to the
second thin line. If three slits are used the needle should be adjusted to
the third thin line. (Fig.2).
Preliminary checks.
Before commencing sampling, the slits and tube above should be cleaned
by swabbing over the slit faces and around the tube with 70% iso-propyl
alcohol. Do not steam sterilise.
Sampling procedure
1. After checking that switch 'A' is off, connect the vacuum pump to the
sampler and plug in the mains.
2. Check that you are using the correct number of slits, according to the
volume of air to be sampled (Table 1)
3. Turn on switch 'A', put switch 'B' into the "down" position. Adjust the
vacuum to the correct mark on the gauge. Turn off switch 'A', and put
switch 'B' up.
4. Unclamp the slit box and lower the turn-table with the control knob.
5. Turn the turn-table so that that the indicator is at zero. Place the agar
plate centrally on the table.
6. Replace the slit box.
7. Turn on mains switch 'A'.
8. Raise the turn-table with the control knob until the neon light glows.
9. Select speed with switch 'C'.
10. Put switch 'B' in "down" position until the turn-table is past 30° and
then return to "up" position.
11. When the cycle has finished, turn off mains switch 'A', lower turntable, remove slit box and plate.
12. Incubate plate at the appropriate temperature
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 7
13. Repeat the above procedure for each sample location.
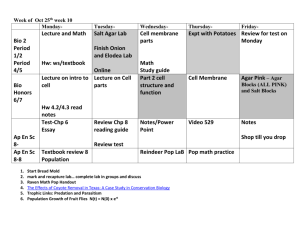
Table 1.
No. of slits
Flow/min (litres)
Time of one cycle
in min.
Volume sampled
(litres)
1
175
2
350
3
525
4
700
0.5
2
5
0.5
2
5
0.5
2
5
0.5
2
5
87.5
350
875
175
700
1750
262.5
1050
2625
350
1400
3500
Fig. 1 Slits from Casella Sampler
Figure 2. Front panel of Casella Sampler.
Switch A
Switch B
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 8
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 9
Anderson Two stage Viable Sampler.
The sampler collects 95% of
particles above 0.8 µm.
The sampler separates viable
particles into size ranges, with a
50% cut off diameter of Stage 1
at 8.0 µm.
The pump maintains a flow rate
of 28.3 litres/min.
Each stage contains 200 tapered
orifices.
The diameter of the stage 1
orifices is 1.5 mm and 0.4 mm on
the second stage.
Use plates of TSA (Total Bacteria),
Malt Agar, (Yeasts/moulds)
Mannitol salt (Staphylococci)
Mitis salivarius (Streptococci)
Plates should contain 25 ml of agar.
The sampler requires two plates, one for each stage.
Label one plate for upper chamber and one for lower chamber.
Sample for four minutes.
Record the volume of air sampled.
Incubate plates at the appropriate temperature, i.e 25C for yeasts and
moulds and 35C for all bacteria.
Count all colonies after incubation from both plates to determine number
of microorganisms in the air sampled.
Calculate number of CFU's per m3 of air.
(Add all microorganisms from upper and lower plate)
Calculate the percentage of particles on each stage and represent as
respirable particles from stage 2 (lower) and nonrespirable particles from
stage 1 (upper).
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 10
Impingement
Airborne Microorganisms may be collected without significant loss of
viability by impingement in a sterile buffered broth.
Millipore Impingement Apparatus,
vacuum pump, limiting orifice and impingement fluid, membrane filters,
Recovery agars, TSA, Sabaroud Dextrose Agar
IMPINGEMENT FLUID.
In 1l of distilled water dissolve:
2g powdered gelatin,
4g Na2HPO4,
37g Brain Heart Infusion broth,
0.1ml octyl alcohol.
Mix the ingredients in a flask and boil for 15 min. Use 50 ml of
impingement fluid in the filter funnel.
Prepare the apparatus according to the instructions.
Note the use of critical orifices to regulate flow rate.
Record flow rate and time.
After sampling the air, the impingement fluid may be drawn off and
filtered through a membrane for culturing and counting or diluted serially
and plate counted.
In this case use the vacuum to draw the fluid through the membrane to
collect microorganisms onto the membrane. Remove the filter aseptically
and place onto a TSA plate for total bacteria. Repeat the process and this
time place the membrane onto a plate of Sabaroud Dextrose agar for
yeasts and moulds.
Incubate at the appropriate temperature.
Note the volume of air sampled from the duration and rate of sampling.
Report on the number of microorganisms collected from the various
locations.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 11
All Glass Liquid Impingement. (AGI)
Air is drawn through the
impinger at 12.5 litres per minute
with a vacuum pump. The
capillary tubing in the sampler
determines the flow rate.
30 ml sterile impingement fluid
is aseptically added to the lower
section of the impinger.
Be sure the tip of the impinger is
covered by liquid.
After the sampling period (note
the sampling time and volume of
air), turn off the vacuum pump.
Sample for 30 mins.
If foaming in the sampler occurs add a drop of n Octyl alcohol.
Ensure evaporation does not reduce the volume below the capillary
tip.
Analysis of sample.
Collect the impingement fluid in a sterile measuring cylinder, wash the
walls of the impinger with a small volume of sterile diluent and make the
volume up to 50 mls.
Carry out serial dilution in Ringers and recover total bacteria and yeasts
and moulds by plate count using the same agar media as before.
Selective media can be used to recover Staphylococci, Streptococci or
other specialized microorganisms.
Alternatively,
Collect the impingement fluid in a sterile measuring cylinder, wash the
walls of the impinger with a small volume of sterile diluent and make the
volume up to 50 mls.
Pass all the sample through a sterile membrane filtration unit. Remove the
filter aseptically and place onto a TSA plate for total bacteria. Repeat the
process and this time place the membrane onto a plate of Sabaroud
Dextrose agar for yeasts and moulds.
Incubate at the appropriate temperature.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 12
Hawksley Air Sampler.
This sampler collects particles in the air directly onto the surface of a
membrane held in a membrane holder attached to a vacuum pump.
The vacuum pump is set to collect between 10-30 litres of air per minute.
The actual rate of sampling is largely determined by the level of
contamination of the air to be sampled. Heavily contaminated air can
only be sampled for a short duration, otherwise the membrane becomes
overcrowded, however prolonged sampling tends to desiccate the delicate
microorganisms on the membrane.
Set up the sampling device as described.
Care is needed to place the membrane in the filter holder aseptically.
Note and record the rate of air sampling and the duration of the
sampling and record the total volume of air sampled.
Recover the cells on the membranes by transferring to suitable recovery
media i.e. total bacteria use TSA, yeasts and moulds use Sabaroud
Dextrose agar. Incubate at the appropriate temperature.
Report on the number of microorganisms collected from the various
locations.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 13
Biotest Centrifugal Air Sampler.
Calibrate and sterilise the impeller head.
Swab using 70% iso propyl alcohol and allow to evaporate. Do not
autoclave. Do not heat in the oven.
Use the bacterial strips for collecting bacteria and the correct agar strip
for yeasts and moulds.
Make sure not to touch the agar in the agar strips with your fingers.
Insert the agar strip with the agar facing the impeller blades while holding
the edge of the strip. Insert fully.
Sample time is normally set for 4 mins.
After the impeller comes to rest, carefully remove the strip, making sure
not to touch the agar with your fingers.
Return the strip to the cover agar side facing into the cavity. Tape to
prevent drying out, label and incubate at the appropriate temperature.
Report on the number of microorganisms collected from the various
locations.
Sampling Volume.
Because of the design of the instrument not all the particles in the air
sampled are impacted onto the agar strips. The volume of air sampled is
280 l/min but the separation volume for particles 4 µm diameter is 40
l/min. Therefore for a 4 min sampling period the amount of air sampled
is 160 litres.
The detected number of organisms per unit of air volume can be
calculated as follows:CFU/m3 = Colonies on the agar strip x 25
Sampling time (mins)
Principle of operation
The Biotest RCS Air Sampler works on the impaction principle. The function of the Air
Sampler is to collect airborne microorganisms quantitatively onto a culture medium. The
air under examination is sucked into the sampler from a distance of at least 40 cm by
means of the impeller.
The air enters the impeller drum concentrically and in a conical form, is set in rotation,
and the particles contained in the air are impacted by centrifugal force onto a plastic strip
containing a culture medium. The air then leaves the drum in a spiral form around the
outside of the cone of air entering the sampler. After the sample has been taken, the agar
strips are incubated and the colonies counted. The sampler has an average rotational
speed of 4096 rpm with an accuracy of + 2%. The separation volume is 40 litres per
minute.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 14
Volume characteristics
Due to its principle of operation and the geometric properties of the impeller drum the
RCS Air Sampler has special volume characteristics. It is therefore necessary to
differentiate between the total volume sampled (= Sampling Volume) and the volume
relevant for separating the particles ( = Separation Volume). The Separation Volume
per time unit is the basis for calculating the number of organisms per air volume.
1 Sampling Volume The air which is to be examined enters the instrument head
concentrically with a diameter of 2a and at velocity Cax. Here it is picked up by the
impeller blade, deflected through 180° and routed to flow past a strip filled with a nutrient
medium. The air is expelled via an annular gap with width b. The total sampling volume
(V) can be determined by point-by-point measuring of the velocity and angle of flow over
the radius r and subsequent mathematical evaluation. This sampling volume is 280 l/min
at a speed of rotation of 4096 rpm. This sampling volume is a parameter for calculating
the volume of air that is relevant to separation of the particles.
2. Separation Volume By virtue of the high centrifugal force, the particles in the rotating
ring of air are forced outwards and impacted onto the surface of the nutrient medium.
However, this separation takes place only from one part of the sampling volume. It is
possible to determine the separation volume mathematically. In doing so, a major
parameter for separation is the height of the instrument head. This height (Imin) can be
calculated for the separation of all particles contained in the total sampling volume. The
basis for this is the resolution of a differential equation which describes the spiral flight
path of the particles under the influence of the air flow velocity, the direction of flow and
the centrifugal force that arises.
For a relevant particle diameter of 4 µm, this produces a height of 14 cm.
However, since instead of 14 cm, only 2 cm are available in the instrument head as the
separating height, separation is not effected from the whole sampling volume but from
only 1/7 of this.
Thus the separation volume for the instrument is 40 l per minute.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 15
SAS Surface Air Sampler.
This instrument is designed for use with the regular Contact plates,
(RODAC) containing agar suitable for recovery of various
microorganisms.
The sampler has two sampling heads which can be used simultaneously.
It is possible to use the same agar to give two replicate samples or you
may use two different agars.
In this case we will use duplicate contact plates containing TSA for total
bacteria, Mannitol Salt for presumptive Staphylococcus and Sabaroud
Dextrose for yeasts and moulds.
Instructions for SAS
Open covers and place Contact plates into holders without lids.
1. Replace perforated cover.
2. Switch ON button
3. Allow display to reach SELECT HEAD & DATE
4. Press ENTER
5. HEAD LEFT is displayed.
6. Press up arrow and select HEAD LEFT + RIGHT
7. Press enter
8. START FOR 500 may be displayed.
9. If so then press START otherwise
10.Press down arrow
11.Select Standard Mode
12.Press ENTER
13.Std Prog 500 may be displayed
14.Select Volume of air using up/down buttons for 500l
15.Press ENTER
16.START.
The instrument samples 500l air. Remove contact agar plates, cover with
their lids, label and incubate at the appropriate temperature.
Report CFU’s per m3 air sampled in your location.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 16
Settle Plates.
A variety of agar media can be used to sample the air for the microbial
load using this technique. You will prepare plates of agar medium
suitable for the growth of the following microorganisms:
total bacteria;
total fungi, (yeasts and
moulds
staphylococci
Oral streptococci
Actinomycetes
TSA
Sabaroud Dextrose Agar or
Malt Agar acidified, (2ml lactic
acid (10%) per 100ml agar
a) Mannitol salt
b) Mitis salivarius
Act medium
Actinomycetes medium has the following ingredients:
Sucrose 30.0, peptone 5.0, KNO3 2.0 (or NaNO3 3.0), K2HPO4 1.0, KCl 0.5,
MgSO4.7H2O 0.5,Yeast Ext. 2.0, FeSO4.7H2O, Agar 15.0, all g/L. pH 7.3
Check with the manufacturers manual on the expected characteristics of
the organisms appearing on the plates.
Open the agar dishes on the benches in your location and leave the agar
surface exposed for the 10, 20, 40 and 80 mins. Carry out the exposure in
triplicate for each time period.
After 10 mins close one set of agar plates and proceed until all the
sampling periods have expired.
The plates are incubated at appropriate temperatures and total colonies
counted.
The results are presented in table and graph form to show the number of
colonies deposited per settlement area per unit of time.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 17
Surfaces Analysis
The bacteriological quality of surfaces can be assessed by using agar
contact plates (RODAC plates) or by using a swabbing technique.
Contact plates.
Contact plates are poured using the molten agar supplied.
TSA, Mannitol salt, McConkey agar and Sabaroud Dextrose agar.
13 ml of molten agar is carefully poured into the agar plate and allowed
to set.
The agar plates are used to take an imprint of the surface under
examination, incubated @ the appropriate temperature and examined.
Report your results.
Swabs
Templates outlining an area of 5 cm2 are first sterilized.
The template is placed into position and the area within the template is
washed with a sterile cotton wool swab moistened with some sterile
diluent.
The swab is broken off into the diluent.
A dry swab is now used to wash the area within the template and is also
placed into the diluent.
The diluent is shaken for 3 minutes.
A 1/10 dilution is carried out and the number of microorganisms is
determined by the pour plate method using TSA.
Plates are incubated @ 32C for 48 hrs.
After incubation examine the plates and record your results.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 18
Presentation Of Results From Sampling Devices at your location.
1. Compare the collection efficiency of each of the devices for
bacteria (CFU/m3),
2. Compare the collection efficiency of each of the devices for
yeasts/moulds (CFU/m3),
3. Total microorganisms, i.e. total bacteria plus total yeasts/moulds
(CFU/m3),
4. From the Anderson Sampler results present the % respirable and %
nonrespirable for
a) Bacteria
b) Yeasts and moulds
c) Total microorganisms
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 19
Casella Flow rate: 175l/min
Sample 1
0.5 min
Sample 2
2.0 min
CFU/plate
Vol air litres
CFU/m3
Mean CFU/m3
Anderson two Stage Sampler
Flow Rate: 28.3l/min for 4 mins sample time
Vol of air =
Bacteria
Mannitol
Fermenters
CFU Upper
plate
CFU Lower
plate
Total CFU
CFU/m3
Hawksley Filter Sampler 20 l /min
CFU/plate
Bacteria
Sample 1
1 min
Sample 2
4 mins
Mitis
Salivarius
Mannitol
Fermenters
Vol of air =
CFU/m3
Vol of air =
CFU/m3
Mean
CFU/m3
Biotest Sampler
SAS
Impinger
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 20
Microbial Loading at your location
Devices
Total
microorganisms
CFU/m3
Total Bacteria Total
CFU/m3: (%)
yeasts/moulds
CFU/m3 : (%)
Total
(%)
Bacteria Total yeas
(%)
Casella STA
Anderson
SAS
Biotest
Hawksley
Impinger
Anderson Sampler Results
At your Location
CFU/m3
Total Bacteria
Total
Yeasts/moulds
Total
microorganisms
Mannitol Salts
% Respirable
% non Respirable
Presumptive Staphylococcus
Mitis Salivarius
Oral Streptococci
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 21
Settle Plate Table
Total Bacteria by Settle plate on TSA in Microbiology Laboratory
10 mins
30 mins
60 mins
120 mins
CFU/plate
CFU/plate
CFU/plate
Mean CFU
Mannitol Fermenting Bacteria by Settle plate on Mannitol Salt in
Microbiology Laboratory
10 mins
30 mins
60 mins
120 mins
CFU/plate
CFU/plate
CFU/plate
Mean CFU
Yeast & Moulds by Settle plate on Sab Dex in Microbiology Laboratory
10 mins
30 mins
60 mins
120 mins
CFU/plate
CFU/plate
CFU/plate
Mean CFU
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 22
Further Analysis Of The Microbial Populations Recovered From The
Atmosphere.
Bacteria:
Carry out Gram stains from colonies on representative plates from your
analysis and determine the
% Gram positive to % Gram negative bacteria on the plates.
And also the ratio of rods to cocci.
These results can be presented in the form of a pie chart.
***********************************************************
Confirmation of Staphylococcus aureus and Streptococcus spp.
Pick suspect Staph. colonies from the Mannitol Salt agar plates and
transfer onto TSA, Blood Agar, Dnase, and Baird Parker agar, using
spot inoculation.
Include a positive control in the centre of each plate.
Incubate @ 37C for 48 hrs.
Likewise, spot Blood agar and TSA with suspect colonies from
Mitis Salivarius agar and incubate @ 37C for 72 hrs.
After incubation examine the colonies on each agar medium and
compare the colonies characteristics to the positive control for
Staphylococcus aureus.
Table showing colony morphologies of suspect Staphylococcus aureus
Blood Agar for Dnase (+/_)
haemolysis
(+/_)
Baird
Parker
(describe)
TSA for Cell
&
colony
morphology
Control
Staphylococcus
aureus
Suspect
colony 2
Suspect
colony 3
Suspect
colony 4
Conclusion: From the results in the table indicate whether the suspect is
Staphylococcus aureus or otherwise.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 23
Staphylococci and micrococci are frequently isolated. Distinguishing between the two
groups is important. Some Staphylococci are known to be pathogens; some are
doubtful or opportunist pathogens; others, and micrococci, appear to be harmless but
are useful indicators of pollution. Staphylococci are fermentative capable of producing
acid from glucose anaerobically; micrococci are oxidative and produce acid from
glucose only in the presence of oxygen.
Identification
They are Gram-positive, oxidase negative, catalase positive, fermentative cocci
arranged in clusters.
Colonies of staphylococci and micrococci are golden brown, white, yellow or pink,
opaque, domed 1-3 mm in diameter after 24 hr. on Blood agar and are usually easily
emulsified. There may be -haemolysis on blood agar. (clear haemolysed zone in
which all the red cells have been destroyed)
On Baird-Parker medium after 24 hr., Staphylococcus aureus gives black, shiny,
convex colonies, 1-1.5 mm in diameter; there is a narrow white margin and the
colonies are surrounded by a zone of clearing 2-5 mm in diameter. This clearing may
be evident only at 36 h.
Other staphylococci, micrococci, some enterococci, coryneforms and enterobacteria
may grow and may produce black colonies but do not produce the clear zone.
Some strains of S. epidermidis have a wide opaque zone surrounded by a narrow clear
zone. Any grey or white colonies can be ignored. Most other organisms are inhibited.
Examine Gram-stained films. Do coagulase and DNase tests on Gram-positive cocci
growing in clusters. This is a short cut: strains positive by both tests are probably S.
aureus.
Coagulase test
Possession of the enzyme coagulase which coagulates plasma is an almost exclusive
property of S. aureus. There are two ways of performing this test:
(l) Slide coagulase test Emulsify one or two colonies in a drop of water on a slide. If
no clumping occurs in 10-20 s dip a straight wire into human or rabbit plasma
(EDTA) and stir the bacterial suspension with it. S. aureus agglutinates, causing
visible clumping in 10 s.
Use water instead of saline because some staphylococci are salt sensitive,
particularly if they have been cultured in salt media. Avoid excess (e.g. a loopful)
of plasma as this may give false positives. Check the plasma with a known
coagulase positive staphylococcus.
(2) Tube test Do this (a) to confirm the slide test, (b) if the slide test is negative. Add
0.2 ml of plasma to 0.8 ml of nutrient (not glucose) broth in a small tube.
Inoculate with the suspected staphylococcus and incubate at 37°C in a waterbath. Examine at 3 h and if negative leave overnight at room temperature and
examine again. Include known positive and negative controls. It is advisable
to use EDTA plasma (available commercially) or oxalate or heparin plasma.
Check Gram films of all tube coagulase positive organisms.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 24
S. aureus produces a clot, gelling either the whole contents of the tube or forming a
loose web of fibrin. Longer incubation may result in disappearance of the clot due to
digestion (fibrinolysis).
The slide test detects 'bound' coagulase ('clumping factor'), which acts on fibrinogen
directly; the tube test detects 'free' coagulase, which acts on fibrinogen in conjunction
with other factors in the plasma.
Either or both coagulases may be present .
DNase test
Inoculate DNase agar plates with a loop so that the growth is in plaques about 1 cm
in diameter. Incubate at 37°C overnight. Flood the plate with 1 M hydrochloric acid.
Clearing around the colonies indicates DNase activity. The hydrochloric acid reacts
with unchanged deoxyribonucleic acid to give a cloudy precipitate.
The API Staph system is useful if identification to species is required.
Staphylococcus aureus
This species is coagulase and DNase positive, forms acid from lactose, maltose
and mannitol, reduces nitrate, hydrolyses urea and reduces methylene blue. It is
usually phosphatase positive but does not grow on ammonium phosphate agar.
Some strains are haemolytic on horse blood agar but the zone of haemolysis is
relatively small compared with the diameter of the colony (differing from the
haemolytic streptococcus).
S. aureus is usually identified by either the coagulase or the DNase test. False-positive
coagulase tests are possible with enterococci.
S. aureus is a common cause of pyogenic infections and food poisoning. Staphylococci
are disseminated by common domestic and ward activities such as bedmaking,
dressing or undressing. They are present in the nose, on the skin and in the hair of a
large proportion of the population.
Micrococcus
These are Gram-positive, oxidase negative, catalase positive cocci that differ from the
staphylococci in that they utilise glucose oxidatively or do not produce enough acid to
change the colour of the indicator in the medium. They are common saprophytes of air,
water and soil and are often found in foods.
Streptococcus
Gram-positive cocci that always divide in the same plane, forming pairs or chains; the
individual cells may be oval or lanceolate. They are Gram-positive, nonsporing, nonmotile and some are capsulated. Most strains are aerobic. The catalase test is negative.
Isolation
Plate on blood agar and trypticase yeast extract cystine agar or mitis salivarius agar.
Air
For -haemolytic streptococci, use crystal violet agar containing 1:500 000 crystal violet
with slit samplers. For evidence of vitiation use mitis salivarius agar.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 25
Identification of streptococci
Colonies on blood agar are usually small, 1-2 mm in diameter and convex with an entire
edge. The whole colony can sometimes be pushed along the surface of the medium.
Colonies may be 'glossy', 'matt' or 'mucoid'. Growth in broth is often granular, with a
deposit at the bottom of the tube.
The primary classification is made on the basis of alteration of haemolysis on horse
blood agar.
-Haemolytic or 'viridans' streptococci produce a small, greenish zone around the
colonies. This is best observed on chocolate blood agar.
' (Alpha prime)-haemolytic streptococci are surrounded by an area of haemolysis which
superficially resembles that of -haemolytic streptococci (below) but with a hazy outline
and unaltered red blood cells within the haemolysed area.
-Haemolytic streptococci give small colonies surrounded by a much larger, clear
haemolysed zone in which all the red cells have been destroyed.
Some streptococci show no haemolysis.
Haemolysis on blood agar is only a rough guide to pathogenicity. The -haemolytic
streptococci include those strains which are pathogenic for humans and animals but the
type of haemolysis may depend on conditions of incubation and the medium used as a
base for the blood agar.
Streptococcal antigens
Species and strains of streptococci are usually identified by their serological group and
type. There are 15 Lancefield groups characterised by a series of carbohydrate antigens
contained in the cell wall.
The API 20 Strep and Rapid ID Strep systems are useful for identifying streptococci.
Group A
These are -haemolytic, are the so-called haemolytic streptococci of scarlet fever,
tonsillitis, puerperal sepsis and other infections of humans, and are known as S. pyogenes.
Some strains are capsulated and form large (3-mm) colonies like water drops on the
surface of the medium.
S. salivarius
These are commensals in the human upper respiratory tract and are therefore useful
indicators in air hygiene and ventilation investigations. The colonies are large and mucoid
on media containing 5% sucrose.
Aerccoccus
These are Gram-positive, oxidase negative, fermentative cocci that are usually in clusters,
pairs, tetrads or short chains.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 26
Classification of fungi.
The fungi are divided into two divisions:
1. Myxomycota (slime moulds)
2. Eumycota (true fungi).
Our interest is with the true fungi or Eumycota.
Two basic growth forms:
(i) unicellular or yeast form which reproduces by simple budding. Colonies
usually moist or mucoid.
(ii) filamentous or mould form which reproduces by spores or conidia.
Colonies are usually velvety or cottony in appearance.
Examination of the fungal colony under the microscope reveals a
filamentous structure.
The filaments that make up the colony are known as hyphae and the mass of
hyphae form the mycelium or the body of the fungus.
There are two kinds of hyphae, non-septate (coenocytic) and septate. The
septa divide the hyphae into compartments but not into cells.
Subdivisions of Eumycota:
1. Mastigomycotina - one class only: oomycetes- typically aquatic fungi containing
580 species, non-septate hyphae.
2. Zygomycotina - one class only: zygomycetes- rapidly growing,
predominantly saprophytic fungi containing 665 species, non-septate hyphae.
Medically important genera include Absidia, Basidiobolus, Conidiobolus, Mucor,
Rhizopus.
3. Ascomycotina - classes no longer recognized: mostly terrestial
saprophytes and parasites of plants containing 28,650 species, septate hyphae, sexual
spores produced within asci.
Medically important genera include Allescheria, Aspergillus, Blastomyces, Geotrichum,
Microsporum, Piedraia, Trichophyton.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 27
4. Basidiomycotina - four classes: hymenomycetes (mushrooms)
gasteromycetes (puff balls) uredimomycetes (rusts) ustilaginomycetes (smuts) terrestial saprophytes and parasites of plants containing 16,000 species, septate hyphae,
sexual spores produced externally on basidia.
Medically important genera include the poisonous mushrooms and
Cryptococcus.
5. Deuteromycotina - a subdivision created for the "fungi imperfecti" i.e. no sexual
forms detected. Two classes: coelomycetes (produce conidia in sac-like structures)
hyphomycetes (conidia produced without sac-like structures). Contains 17,000 species,
septate hyphae. Most of the medically important fungi are included in the "fungi
imperfecti" including Candida, Cladosporum Coccidioides, Epidermophyton, Fonsecaea,
Madurella, Malassezia, Microsporum, Sporothrix, Trichosporon.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 28
Two groups of fungi are significant for air pollution:
The systemic mycoses (causing pulmonary infection from air-borne
conidia). Blastomyces, Coccidiomyces, Histoplasma, Paracoccidioides.
The opportunistic systemic mycoses (fungi of low virulence which can
invade immuno-compromised hosts). Absidia, Aspergillus, Candida,
Cryptococcus, Geotrichum, Mucor, Rhodotorula, Rhizopus, Torulopsis.
Contaminating fungi:
The more common contaminating fungi are also opportunistic pathogens
e.g. Absidia, Aspergillus, Mucor, Penicillium, Rhizopus, Rhodotorula,
Scopulariopsis.
Contaminating fungi may have very small pathogenic risk, other than
allergic reactions, but some of them are of great importance to food and
agricultural mycologists.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 29
Culture media for fungi:
Mycological media should inhibit bacterial growth so that the slower
growing fungi can develop. The traditional way to do this is to use low
pH media e.g.
Sabouraud Dextrose Agar and
Potato Dextrose Agar at pH 5.6,
Malt Extract Agar at pH 5.4 and
Wort Agar at pH 4.8.
Although these media are still widely used, it is accepted that low pH
levels can suppress the growth of stressed fungal cells. The pH can be
raised to neutrality, if antibiotics are added to suppress the growth of
bacteria e.g.
Oxytetracycline-Glucose-Yeast Extract Agar (OGYE Agar)
Dermasel Agar Base with Dermasel Selective Supplement SR75.
An alternative to selective media is elective media (or enrichment culture)
i.e. a formulation which allows only those organisms to grow which can
utilise the growth factors provided. Czapek-Dox Agar, a synthetic
medium in which sodium nitrate is the sole source of nitrogen, is a popular
example of an elective fungal medium.
A second problem with mycological media is the tendency of rapidly
growing fungal colonies to spread and overwhelm neighbouring colonies
of slower-growing organisms.
The incorporation of ox-bile or preferably rosebengal inhibits spreading.
Rose-Bengal/ Chloramphenicol Agar combines inhibition of spreading
and bacterial growth. Rose-Bengal is not quite effective enough to control
spreading of very rapidly growing fungi, such as Rhizopus and Mucor
species.
Dichloran can be added to assist rosebengal.
Dichloran-Rose Bengal-Chloramphenicol Agar (DRBC Agar with
chloramphenicol) is a good example of this type of medium.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 30
Methods for Microscopic examination of filamentous fungi
a) Using a sharp blade remove a sliver of colony with the reproductive
the structures intact. Transfer the material to a clean slide and stain
with Lactophenol cotton blue. (may need to wash away excess
spores with Ethanol)
b) Look for and note the presence or absence of septae within the
filaments.
c) Draw the typical reproductive structures carrying the spores
(conidia or sporangia) and the shape and arrangement of the spores.
Alternatively use Sellotape for lifting fungal material directly from the
colony and place onto a slide with a drop of stain and examine as above.
Mounting media for yeasts/moulds:
Lactic acid with /without aniline blue dye [0.1% in Lactic Acid),
Shear’s Mounting Fluid, (3g Kacetate; 150ml Water; 60ml glycerin; 90ml ethOH (95%)]
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 31
Use low powers of the microscope x100 and x200, x400.
Septa
(P/A)
Reproductive structure
Draw spores
Colony 1
Colony 2
Colony 3
Colony 4
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 32
Examination of yeasts (unicellular)
a) Note the colony morphology on the agar plate, i.e. colour and texture.
b) Prepare a simple stain on a slide using Methylene Blue, cover with a cover slip
and examine under the microscope.
c) Note the shape and size of the cells. Measure at least 10 cells.
Colony
morphology Cell shape Mean
(colour and texture)
Cell size (m)
Colony 1
Colony 2
Colony 3
Colony 4
Calibration of microscope and determination of yeast cell size.
Using a eyepiece graticule and a stage micrometer it is possible to calibrate your
microscope to measure size of particles and structures under the microscope.
Insert the eyepiece graticule at the field stop of the eyepiece lens as directed.
Centre the micrometer under the microscope and focus.
Calibrate the eyepiece at:
low power (x100)
medium power (x400)
high power (x1000)
The eyepiece has a rule with 100 subdivisions.
The stage micrometer is ruled to 1mm, subdivide into 100 by 0.01mm.
Line up the stage micrometer superimposed under the eyepiece graticule to the left side of
the micrometer, and measure the length of the eyepiece graticule under each
magnification.
Line up as carefully as possible.
Measure the greatest length possible.
Note your results below.
Magnification
Eyepiece units Corresponding
Length of
Micrometer units 1 Eyepiece unit
low power (x100)
medium power (x400)
high power (x1000)
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 33
Fungal infections are normally only a superficial nuisance (e.g.
Ringworm), but a few fungi can cause serious systemic disease, usually
entering via the lung in the form of spores, the outcome depends on the
degree and type of immune response, and may range from an unnoticed
respiratory event to rapid fatal dissemination or a violent hypersensitivity
reaction. (Type 3: Extrinsic Allergic Alveolitis)
The severe respiratory difficulties associated with Farmer's Lung occur
within 6-8 hours of exposure to the dust from mouldy hay. People are found
to be sensitised to thermophilic actinomycetes which grow in the mould hay.
Inhalation of the spores into the lungs introduces antigen into the lungs and a
complex-mediated hypersensitivity reaction occurs.
Extrinsic Allergic Alveolitis Caused By Inhaled Spores.
SOURCE
OF
DUST
Mouldy Hay
THE DISEASE
Farmer's Lung
Air-conditioning systems
Hypersensitivity
pneumonitis
Bagasse
Bagassosis
Redwood sawdust
Sequoiosis
Malting barley
Maltworker's Lung
Maple bark
Cheese
Maple bark pneumonitis
Cheese washer's Lung
ORGANISM
Micropolyspora faeni
Thermoactinomyces
vulgaris
Micropolyspora faeni
Thermoactinomyces
vulgaris
Thermoactinomyces
sacchari
Aureobasidium pullulans
Graphium sp.
Aspergillus clavatus
Aspergillus fumigatus
Cryptostroma corticale
Penicillium caesi
Fungi And Actinomycetes Associated With Respiratory Infections.
Disease
Cryptococcosis
blastomycosis
blastomycosis
Source
Pigeon droppings
soil
soil
Coccidiodmycosis
Histoplasmosis
Sporotrichosis
Adiaspiromycosis
soil
chicken, bat droppings
Straw, sphagnum moss
Nests of field mice
Organism
Cryptococcus neoformans
Blastomyces dermatitidis
Paracoccidiodes
brasiliensis
Coccidioides immitis
Histoplasma capsulatum
Sporothrix schenckii
Emmonsia crescens
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 34
Bacterial Infections Which May Be Acquired By Inhalation.
Disease
Organism
Pulmonary tuberculosis
Mycobacterium tuberculosis
Pulmonary anthrax
Bacillus anthracis
Staphylococcal respiratory
Staphylococcus sp.
infections
Streptococcal respiratory
Streptococcus pyogenes
infections
Pneumococcal pneumonia
Diploccus pneumonia
Nocardiosis
Actinomadura asteroides
Q fever
Coxiella burnetii
Whooping cough
Bordetella pertussis
Diphtheria
Corynebacterium diphtheria
Sinusitis, bronchitis
Haemophilus influenza
Primary atypical pneumonia
Mycoplasma pneumoniae
Pneumonic plague
Yersinia pestis
Legionnaires Disease
Legionella pneumophila
***********************************************************
Examples of Fungi
Rhizopus
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 35
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 36
Helminthosporium.
Cladosporium.
Phialophora
Paecilomyces.
.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 37
Analysis of Surfaces for Microbial Contamination
Two common ways of assessing the Microbiological quality of working surfaces are
by using RODAC contact plates and by swabbing.
Contact plates.
13 ml of molten agar is carefully poured into the agar plate and allowed to set.
The agar plates are used to take an imprint of the surface under examination,
incubated @ the appropriate temperature and examined.
Report your results as CFU/cm2.
Materials:
TSA contact plates are used for Total Bacteria. (Incubate @ 37ºC/48 hrs.)
Mannitol Salt contact plates are used for presumptive Staphylococci. (Incubate @
37ºC/48 hrs.)
Sabaroud Dextrose agar contact plates are used for yeasts and moulds. (Incubate @
25ºC/4-5 days)
Swabs
Templates outlining an area of 5 cm2 are first sterilized.
The template is placed into position and the area within the template is washed with a
sterile cotton wool swab moistened with some sterile diluent.
The swab is broken off into the diluent.
A dry swab is now used to wash the area within the template and is also place into the
diluent.
The diluent is shaken for 3 minutes.
A 1/10 dilution is carried out and the number of microorganisms is determined by the
pour plate method using TSA.
Plates are incubated @ 32C for 48 hrs.
After incubation examine the plates and record your results.
Present as CFU/cm2.
Air Pollution Microbiology Dr Michael Broaders, IT, Sligo
Page 38