File
advertisement

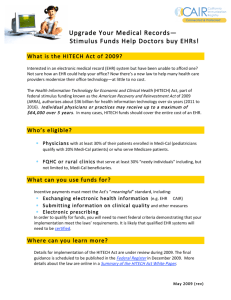
EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE EHR: Advantages – Weaknesses / Threats - Future Leslie LaStofka, Matt Reid, Terry Davis: MMI 401-DL 55 Northwestern University June 3, 2011 1 EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 2 Abstract Electronic health record systems are a key part of the next generation in health care. To help highlight the pros and cons with such an integral part of the health system we have used a modified SWOT analysis approach to investigate the advantages, weaknesses, future and threats to EHR systems. We have found that EHR systems can improve the quality of care and safety of patients while also providing cost savings and improved productivity. However, the cost of implementation along with the potential workflow disruptions can pose a burden to physician practices that are not equipped with sufficient IT personnel or training. Patients are also weary for the security of their personal medical information stored in EHR systems. With the influx of data entered into EHR systems, the secondary use opportunities are just starting to become apparent to the public and private sectors for both business opportunities and public health initiatives. Advantages of the Electronic Health Record The electronic health record (EHR) offers significant advantages when compared to the traditional paper medical record. The key advantages of an EHR can be categorized into the following general areas: 1. Improved quality of care and patient safety 2. Improved productivity, financial effectiveness and cost savings 3. Improved end-user job satisfaction 4. Improved patient satisfaction 5. Improved ability to meet regulatory agency requirements Improved quality of care and patient safety, the most important of the advantages, can be achieved with an EHR as attested to through numerous studies. Kaiser Permanente has determined the following through the implementation of KP HealthConnect: EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 3 “Benefits of the System KP HealthConnect's built-in treatment guidelines are helping the organization improve the management of common/chronic conditions such as diabetes and hypertension. Kaiser Permanente is also enhancing patient care by increasing the accessibility of the patient medical record. Doctors and caregivers have data at their fingertips to identify what treatments and protocols work best. Industry studies show that paper medical records are unavailable up to 30 percent of the time for patient office visits and are almost never available for patient care in an emergency room. Kaiser Permanente's electronic health record is available when and where it is needed. Having electronic health information that is integrated into Kaiser Permanente's services helps the organization's doctors care for its patients in ways never experienced before. With a patients' lifetime health record at their fingertips, doctors and other clinicians are improving care and services. In addition, because KP HealthConnect includes more comprehensive patient information, it is helping caregivers address multiple problems or the provision of multiple services in a single visit, reducing the need for additional follow-up appointments. And Kaiser Permanente's new online features found at kp.org (secure e-mail to your doctor's office) have brought members unprecedented access to Kaiser Permanente care. Over time, it is expected these changes will bring measurable improvements to the quality, patient safety and service experienced by Kaiser Permanente members each and every day.” (Kaiser Permanente HealthConnect™: Transforming Medical Care and Service, (2007, February 15) Retrieved from http://xnet.kp.org/newscenter/ehr/2007/021507kphealthconnect.html. May 9, 2011) With an EHR, clinical and demographic patient information can be accessed quickly and by multiple end-users simultaneously at the point-of-care. Critical clinical decisions rely on a patient’s medical history and previous treatment which is documented within the medical record. If providers are hindered from having access to this information when needed, patient safety and quality of care can EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 4 be compromised. In the paper medical record world, there may be a delay in locating a previous admission or perhaps key documents such as dictation, lab, pathology or radiology results have not yet been filed within the medical record. With the EHR, the documents are either created directly within the application or received via a real-time interface from other source systems that collect the information. This allows care providers to reference key clinical information while treating the patient as well as conference with other providers who can see the same information from a remote location. In addition, with an optimally configured health information exchange process, a patient’s health care information can be immediately available across the continuum of care, in a longitudinal format, to ensure that the treating professional has global access to all clinical information before rendering a care decision. This type of efficient exchange is not available in the paper record world which can impact the quality of care delivered and safety of the patient. It also eliminates the need to order duplicate diagnostics tests when either the results cannot be located or the ordering physician is unaware that the test has already been completed. Another key set of factors that improve the quality of care and patient safety is computerized provider order entry (CPOE), medication management and access to decision support tools, such as the latest medical literature regarding a condition as well as best practices that are believed to contribute to improved quality of care. In addition, EHRs promote evidence-based medicine that allows the availability of vast amounts of clinical information for research which can quicken the knowledge level related to effective clinical practices. CPOE assists greatly in medication error reduction and cost-savings through use of standardized order sets and other electronic controls. As noted in Health Affairs, “CPOE could eliminate 200,000 adverse drug events and save about $1 billion per year if installed in all hospitals.” (R. Hillestad, et al. Health Affairs). Also, medication EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 5 management “expert knowledge” or EHR “intelligence” tools provide immediate “alerts” to ordering providers if there is any counter-indication to the use of a particular medication or combination of medications when considering the patient’s medical diagnoses. The alerts are also designed to flag abnormal diagnostic test results and other critical information that the care provider needs to make the best care decision. Having prompt knowledge of this kind of information allows the appropriate remediation to take place quickly which improves care and reduces the possibility of adverse outcomes. With the paper medical record, these kinds of benefits cannot be achieved. The legibility of entries, a long-standing and significant problem with paper medical records, is no longer an issue with the EHR. This, in and of itself, has been proven to reduce medication errors in particular. “Medication errors are among the leading causes of preventable errors, with a reported inpatient incidence of 5.7% (Kaushal, Bates, Landrigan, et al., 2001). Bates reports that preventable medication errors cost approximately $5,000 per event, with a projected annual cost of $2.8 million dollars for a 700-bed hospital (Bates, Spell, Dullen, et al., 1997). In To Err Is Human, the Institute of Medicine stated that the highest priority for healthcare organizations is medication safety (2000, pg. 27). Medication errors are frequently the result of illegibile physician orders. A large healthcare system in the southeastern United States conducted a study on medication safety and discovered the following as related to the legibility of physician orders: “Legibility of physicians' medication orders did not meet expectations in any of the hospital units. The percentages by unit were as follows: 13% legibility in the NICU, 53% in ICU, and 28% in telemetry. One medical surgical unit had 80% legibility, and the remaining medical surgical units ranged between 50% and 60%.” (Ettel, D. et al) EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 6 Improved productivity and financial effectiveness is another advantage the EHR affords the organization. Records can be accessed instantaneously without requiring staff to identify, retrieve, and refile hard copy charts. In addition, the cost to store an EHR is no where near the cost to maintain on-site and off-site storage areas for the paper medical records. The thoroughness and accuracy of ICD-9-CM and CPT code assignment is often times much improved because of the availability and timeliness of more comprehensive diagnostic information from the complete care team. A more thorough and accurate set of code assignments may lead to a higher level of reimbursement. Eliminating the legibility issue is also a key promoter of improved productivity and financial effectiveness. In addition, billing staff can immediately retrieve the clinical documents required for billing which enhances staff productivity as well as the efficient production of bills for quicker payment by third party payers. Many studies have demonstrated the financial benefits of EHRs as reflected in Virtual Medical Worlds article entitled “Value Measurement and Return On investment for EHRs” “To-date benefits of health information technology have been quantified and documented in a number of areas, e.g. Electronic Health Records (EHR) and Health Information Exchange (HIE) solutions. These benefits have been estimated at a global level, but there are some documented case studies that show benefits achieved by specific organizations. The following points highlight some global level benefits that have been observed in the United States: Health Information Exchange & Interoperability o Reduction in redundant tests, reduction in delays and cost associated with paperbased ordering and reporting would result in $31.8 billion benefits per year o Savings from avoided tests and improved efficiencies - $26.2 billion per year o Medium-size hospital would accrue $1.3 million benefits per year with improved efficiency in transactions with providers, ancillaries, payers and pharmacies Benefits of Health Information Technology - A recent GAO Study focusing showed: EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE o 7 40 percent decrease in radiology tests resulting in $1 million in savings among the pilot group; o Reduction in staff with automation of manual processes resulting in savings of over $700,000; o Savings of $4 million in automated claims processing without manual intervention. The actual benefits can be summarized as follows: EHR Systems o It is estimated that over 5 years, EHR benefits will be $86,400 per provider and the benefits will be accrued by several stakeholders such as physician practices, ancillary services, pharmacies and most importantly patients o Ohio State University Health System reduced the time for getting medication to patients by 65 percent from 5.28 hours to 1.51 hours. They also reduced Radiology turnaround from 7.37 hours to 4.21 hours o Maimonides Medical Center reported 30.4 percent reduction in average length of stay from 7.26 to 5.05 days. They also realized organizational efficiencies by preventing duplicate ancillary tests o Heritage Behavioral Health experienced 70 percent reduction in cost of clinical documentation with EHR o University of Illinois at Chicago Medical Center gained significant benefits in reallocation of nursing time from manual documentation to direct care - estimated to be $1.2 million e-Prescriptions o Many errors occur because of handwritten prescriptions that can be easily misunderstood and can result in adverse drug events or complications. More than 3 billion prescriptions are written annually and according to an eHI report, medication errors account for 1 out 131 ambulatory care deaths and many deaths in acute care are also attributed to medication error. o Studies indicate that the national savings from universal adoption could be as high as $27 billion annually Computerized Provider Order Entry (CPOE) EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE o 8 The Center for Information Technology Leadership (CITL) estimates that implementing advanced ambulatory CPOE systems would eliminate over 2 million drug events per year; avoid nearly 13 million physician visits, 190,000 admissions and over 130,000 life-threatening adverse drug events per year and save $44 billion per year. o Brigham and Women's Hospital in Boston reported 55 percent reduction in serious medication errors and 17 percent reduction in preventable Adverse Drug Events (ADE) - average cost of an ADE was $2,595, resulting in projected savings of $480,000 per year. They estimated net savings from $5 million to $10 million per year. o Maimonides Medical Center in New York realized 55 percent decrease in medication discrepancies and 58 percent reduction in problem medication orders. They also eliminated pharmacy transcription errors. o Children's Hospital of Pittsburg has eradicated handwriting transcription errors completely and cut harmful medication errors by 75 percent.” (Value Measurement and Return on Investment for EHRs. Retrieved fromhttp://www.hoise.com/vmw/06/articles/vmw/LV- VM-08-06-19.html May 11, 2011) Lastly, the time spent charting by health care professionals is reduced due to the efficiency of drop-down menus, document templates that support box check-marks, and other electronic documentation tools, including spell-check. Of note, the following results were cited in the Journal of the American Pediatrics – 2010: "Children at intervention sites were more likely to have had a visit during the study period in which their ADHD was assessed. The ADHD template was used at 32% of visits at which patients were scheduled specifically for ADHD assessment, and its use was associated with improved documentation of symptoms, treatment effectiveness, and treatment adverse effects." (Journal of the American Pediatrics – 2010). EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 9 A reduction in transcription costs can also be realized since the EHR supports the use of direct-entry templates that contain clinical information that would be dictated in the paper medical record world. Lastly, in the physician office, all of the previously mentioned benefits can be realized as well as improved efficiency when re-filling prescriptions and communicating with the pharmacy. Improved end-user job satisfaction is evident when using an EHR because of the eliminating and/or reduction of tedious tasks such as loose filing of documents and the copying of paper documents for release of information requests. Information within an EHR, when properly organized during initial design sessions, is much easier and quicker to locate. In response to a request for information, the EHR content may be transmitted to a secure server or burned to a CD. In addition and as previously cited, the record can be accessed by multiple users at one time so there is no longer the need to wait for the single hard-copy record to be available. In light of the number of uses involving the medical record, including patient care, peer review, quality management studies, basic processing for deficiencies and coding, medical information release, research studies, internal and external agency auditing, this is a great advantage. Patients are also more satisfied with the use of an EHR. When properly configured, they can have direct access to their medical record and personal health record (PHR) through a patient portal or other similar mechanism. There is a much improved method of delivering patient education materials that pertain to their specific conditions and necessary patient/physician follow-up. There is an improved overall continuity of care due to the availability of their clinical information to their physicians in various healthcare delivery settings. No longer does the patient have to retrieve a hard-copy of their medical record from a provider in order to present to the next physician he/she is scheduled to see. Lastly, EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 10 hospitals and physician offices that have an EHR tend to run more efficiently and cost-effectively which leads to enhanced satisfaction for the patient. “"Patients are very amazed, especially ones that go over to urgent care and they say, "Oh, you already have my records?' On the flip side, if they go in to see the doctor, the doctor already knows the patient went in to urgent care. For the doctor to know that real-time is very impressive to patients." — Beth Lopez, RN Manager, Kaiser Permanente Southern California "I know that when I see a member, the chart is available...I can see all the pertinent information, write my notes, order labs and medications, and feel secure that the next provider who sees this member will have all this information as well." — Nancy Goler, MD, The Permanente Medical Group, Kaiser Permanente Northern California "KP HealthConnect is my lifeline. Everything is on it from my schedule to my patients to my phone calls to patient history. I don't know how I survived with the paper chart." — Linda Ramirez, medical assistant, Kaiser Permanente Northwest” (News Release—Kaiser Permanente Makes Major Gains in Online Medicine: Retrieved from http://xnet.kp.org/newscenter/ehr/2007/021507kphealthconnect.html. May 9, 2011) The EHR also assists the healthcare delivery system in adhering to external regulatory agency requirements. In the realm of privacy and data security, the EHR is designed in a manner that demonstrates high level information security through implementation reliable and industry standardized IT controls. The privacy of the information can be assured through the required use of unique logons and passwords by authorized individuals who must attest, in some environments, to their reason for accessing the electronic record. In addition, end-user access logs are maintaining within the EHR system that tracks the date and time an individual viewed or modified the record, and from what location. This is extremely critical data to have should there be a suspected breach of confidential patient information. This is not functionality that is available with the paper medical record. EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 11 External agencies such as state reviewers and the Joint Commission applaud hospitals that have implementation an integrated EHR for all of the reasons as previously stated as well as due to the fact it simplifies the process of reviewing charts for them. Last, but not least, it is only through an EHR under Health Care Reform that meaningful use can be demonstrated and qualifications met to receive incentive payments from the governmental agencies. The federal government has recognized the advantages of the EHR for all stakeholders in the healthcare delivery system in the United States. As a consequence, they have promoted its implementation and effective use by setting into policy the American Recovery and Reinvestment Act and its various financial incentives. WEAKNESSES and THREATS With the passage of the American Recovery and Reinvestment Act of 2009, as much as $50 billion will be made available to physicians and hospitals for the implementation of EHR through the year 2014 (Abraham, 2010). While on the surface it might appear that it is a “slam-dunk” for physicians and hospitals to “install EHR and get a check”, the implementation of EHR is much more involved than simply installing one’s favorite (or not so favorite) software package from Microsoft. Abraham (2010) looked at the barriers to implementing EHR through the lens of a “Strengths, Weaknesses, Opportunities and Threats” (SWOT) analysis. He listed the weaknesses and threats as: cost of implementation, penalties for missing implementation deadlines (i.e., “meaningful use”), initial infrastructure burdens, potential data security breaches, potential-workflow disruptions, and education/training requirements. Before investigating each of the weaknesses and threats, it is worthwhile to look at the latest figures on EHR adoption rates. In January of this year, the Office of the National Coordinator for Health Information Technology (ONCHIT) published numbers indicating that 81% of the hospitals EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 12 and 41% of office-based physicians will be in a position to receive ““meaningful use”” payments (Lewis). In October 2010, the marketing research firm of SK&A provided a breakdown of the adoption rates for office-based physicians. For primary care physicians, positive adoption rates were positively correlated with the size of the practice: 1 physician (28.5%), 2 physicians (36.8%), 3-5 physicians (42.7%), 6-10 physicians (54.4%), 11-25 physicians (65.2%), 26+ physicians (71.0%). Adoption rates were also positively correlated with the ownership structure of the practice: hospital owned (54.9%), non-hospital owned (37.1%), health system owned (61.2%), non-health system owned (36.8%). The “chief complaint” of the small/independent practices was the financial challenge of implementing EHR technology (Pamela Lewis Dolan). Cost of Implementation Given that “cost” is topmost on the minds of office-based physicians, we begin our discussion of weakness and threats with the cost of implementation. Reming, Culler, McCorkle, Becker, & Ballard (2011) reviewed the implementation of EHR in 26 primary care physician practices in north Texas and found that a five-physician practice can expect initial software/hardware/labor costs of $162,000 ($32,409/physician) through the first 60 days after launch and $85,500 ($17,100/physician) in maintenance expenses during the first year. While these numbers were found to be in line with studies conducted in New York and Massachusetts, they are somewhat different than those published by CDW Healthcare (2011). In 2010, CDW Healthcare surveyed 200 physician group practices that were not using EHR technology. They developed a cost model for a “typical group practice” based upon: 1.) suggested information technology (I/T) solutions from the “communi.T.com” website, 2.) practice information from the University of Virginia, the Medical Group Management Association (MGMA) and the EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 13 American Congress of Healthcare Executives, and 3.) cost benchmarks from their own customer implementations. Based upon the cost model, they calculated initial software/hardware/labor costs of $19,000/physician, with ongoing maintenance expenses of $30,000/physician. But unlike the north Texas study, they calculated that in the initial year of implementation, each physician would lose $101,000 due to lost productivity (Caraher & LaVanway). A 2005 benchmark survey of 3,300 physician practices conducted by the MGMA and the University of Minnesota (UofM) found that the average EHR implementation cost was $32,606/physician (consistent with the north Texas study) and that the ongoing maintenance expenses were $14,124/physician. These figures do not take into account the fact that on average, implementations overran the vendor’s initial estimate by 24.8%. As with the CDW study, an attempt was made to quantify the financial impact of lost productivity. The MGMA and UofM estimated that manual data entry slowed doctors down by 15%, resulting in a 30% decrease in take-home pay (Steele). Gans, Kralewski, Hammons, & Dowd (2005) reported a 10% decrease in take-home pay but they reached their figure by amortizing the initial ($33,000/physician) and maintenance ($18,000/physician) costs over a 5-year period with a cost-of-capital of 8%. So what does this mean for the small and/or independently owned practice? Because of the tax codes, capital expenditures are funded out of the physician’s income. Couple this with the fact that most of these practices have limited access to investment capital and the projected 10-30% decrease in take home pay could put some practices in financial peril. The end result is an increased likelihood that these practices will limit their adoption of EHR technologies (Gans, Kralewski, Hammons, & Dowd). EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 14 Penalties for Missing Implementation Deadlines But this should beg the question “what about the penalties that will be imposed for failing to demonstrate ‘meaningful use’”? Aren’t physicians incented to implement EHR so as to avoid the penalties? In 2010, the Physician’s Reciprocal Insurers conducted a survey of 500 physicians concerning EHR implementation and the penalties that will be imposed for failing to demonstrate “meaningful use”. They found that while 85% of the physicians were aware of the financial incentives for implementing the systems, more than 35% did not know that they faced government-assessed financial penalties for not complying…However, those penalties do not seem to be having the intended effect, as more than 65% of the physicians who were unaware of the financial penalties said this would not cause them to implement EMR. (John, September, 2010). In June, 2009, physicians at the AMA Annual Meeting vocalized their opposition to the penalties for failure to demonstrate “meaningful use”. They passed a resolution asking for the AMA to petition the government to rescind the penalties on the grounds that it violates the AMA’s “payfor-performance” policy. They further argued that it penalizes those physicians who cannot afford the upfront costs. David McKalip, MD, a neurosurgeon from Florida voiced a common sentiment of the meeting’s attendees. “My financial calculations say it’s cheaper for me to take the penalty than to put the system in, and that’s what I’m going to do”. (Berry) According to the American Academy of Family Physicians (AAFP), the aforementioned physicians make a good case for simply paying the penalties. Per the AAFP, the average physician practice grosses $500,000 in revenue and does $100,000 in Medicare business. With the penalties starting at 1% in 2015 and rising to 5% in 2019, the average practice is looking at penalties in the range of $1,000-$5,000 (John, October, 2010). EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 15 Avalere Health LLC (2009) compared EHR costs against both the incentives that are being offered and the penalties that will be assessed. Using AHRQ’s 2005 estimates for initial ($35,000/physician) and maintenance ($18,000/physician) costs, it was determined that individual and/or small group practices will spend up to $124,000 for the years 2011-2015 yet only be eligible to receive $44,000 in incentive payments. Based upon AHRQ’s estimates, the average physician sees eight Medicare patients/day at a cost of $85/patient, resulting in $170,000 in annual Medicare revenues. With the annual penalties rising from 1% to 5% of Medicare revenues, the average physician will face $25,500 in penalties over the 5-year period. Totaling the loss of the incentive payments and the penalties and subtracting them from the cost of implementation will put the physician $54,400 ahead by simply doing nothing. Based upon this math, some physicians will simply pay the penalty rather than implement EHR. (Konig, Rosenfeld, Rubin, & Weier) I/T Infrastructure Burdens Contributing to the $32,000-$35,000/physician for an initial EHR implementation is the cost associated with the I/T infrastructure. Walk into most physicians’ offices today and the odds are pretty good that you will find PCs that perform mostly administrative tasks (e.g., word processing, scheduling, registration, record keeping, etc.). This usage pattern has not dictated the need for a robust I/T infrastructure. However with the implementation of EHR, the increased usage of information technology will strain most of the currently installed infrastructures. Most of these I/T infrastructures consist of: 1.) uneven wireless coverage, 2.) networks with insufficient bandwidth, and 3.) inadequate levels of redundancy and backup (Staren). Most EHR systems rely on wireless networks as they expect the physician to make use of mobile technology, bringing technology to the “point of care”. Uneven or spotty network coverage is problematic for the EHR system since most do not gracefully recover from intermittent network EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 16 outages. Unfortunately, most wireless networks are plagued by: disruptions caused by moving from one access point to another; connectivity drops caused by insufficient bandwidth for the number of users; coverage “dead spots”; and a mix-and-match of protocols (i.e., 803.11b, 803.11g, 803.11n) that cause performance problems (Staren). Unless an installation is in a single site, the installation will most likely rely on a wide-area or metropolitan network that shares bandwidth with other users (Staren). Given the increased demands that EHR will place on the network (e.g., transmission of images, additional access points) coupled with the unknown usage by the other users of the network, the uneven and/or poor performance of the network will lead to user dissatisfaction with the EHR. But even if the installation runs its own network, care must be taken to properly size the network for the increased demands. Michael Silver, VP of Imaging Services for Sg2, relates a story about a visit that he paid to a hospital that had purchased new digital radiography equipment. The purchase was justified based upon the cost savings over traditional film and the speed of transmitting the images over the network. When asked what the hospital had done to create a network capable of efficiently shuttling gigabyte-sized files throughout the hospital, the answer, Silver says in amazement, was ‘Nothing.’ ‘They acquired digital radiography equipment at about three times the price of standard X-ray equipment, but they didn’t have a network to send the images on,’ he says (Joch). Two forms of redundancy must be in place for EHR: equipment and application/data. When the network is used for only a few administrative PCs, equipment redundancy is not that critical. But when EHR causes the network to become the life-line of the practice, equipment redundancy is a must. Alternate means must be in place to ensure that physicians can continue to practice regardless EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 17 of a system outage. When paper was the medium for storing patient information, a backup was usually stored on microfiche. Once the medium becomes electronic, a more sophisticated, off-site strategy must be deployed. And of course, regardless of how it is implemented, physicians must be able to have access to the information wherever and/or however it is stored (Staren). CareGroup Healthcare System, Boston, thought redundant equipment was protecting the organization from widespread disasters until a network outage in 2002 shut down electronic operations for more than three days. ‘That showed us that unless you have a bulletproof infrastructure, it’s pretty hard to have a completely paperless and electronic hospital because no one can get to the labs, the digital radiography, or electronic medical records,’ says CareGroup CIO John Halamka (Joch). Since 1998, the “Most Wired” survey of hospitals and health systems has been sponsored by the American Hospital Association. The survey assesses I/T implementation in four areas: 1.) infrastructure; 2.) business and administrative management; 3.) clinical quality and safety (inpatient/outpatient hospital); and 4.) care continuum (ambulatory/physician/community) (Kling). Based upon the 2007 “Most Wired” (NOTE: 2010 survey results are available for $395, which is beyond the budget of this writer) survey, respondents were asked to indicate how long it would take them to restore their clinical systems after a total loss of those systems. 33% of the “most wired” could restore within 4 hours and 55% could restore within 1 day. Only 5% of the “least wired” could restore within 4 hours and 27% could restore within 1 day (Solovy). Potential Data Security Breaches A 2005 survey conducted by the California HealthCare Foundation found that 67% of the respondents listed privacy and security as their biggest concerns about EHR. When illnesses were factored into the equation, an even greater percentage of respondents indicated their concern. In fact, EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 18 12.5% of the respondents indicated that they had taken actions to conceal their medical condition. Unfortunately, those actions may have had adverse effects on their healthcare. Those actions included: avoiding trips to the doctor, asking physicians to falsify diagnoses, paying physicians to “non-report” a medical condition to insurance companies, and forgoing medical tests (Terry & Francis). It is therefore incumbent upon the I/T infrastructure to ensure that patient information is secure and that privacy rights are adhered to. Unfortunately, not all I/T infrastructures are up to the task. In 2006, the Privacy Rights Clearinghouse recorded 27 breaches of health information security that affected more than 900,000 patients. Nine of those “breaches involved EHR systems, with the causes being attributed to flaws in software, criminal theft, and hacking.” (Layman) In November, 2007, hackers stole HIV and hepatitis information from a Canadian health agency computer (“Electronic medical records: The pros and cons”). Finjan Software, a leading software security firm, has noticed increased interest on the part of cybercriminals to obtain healthcare records. Cybercriminals infect PCs with malware, hijack the data, and then send the data to unprotected remote servers. Once search engines index those servers, any user of “Google” who enters the correct search term will have access to the records. One incident involved a server located in Malaysia that had “log-in information to a U.S. healthcare organization that manages hospitals and medical clinics”. With this data, the hackers could potentially make false insurance claims because they would have access to patient medical histories and records (Kirk). In 2007, Atlanta-based security firm SecureWorks noticed a 85% increase in cyber attacks against its healthcare clients. Cyber attacks rose from 11,146/healthcare client day in the first half of 2007 to 20,630 per day in the second half of the year. Based upon their analysis, hackers target EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 19 members of preferred medical plans with the intent of selling that information to criminals who specialize in counterfeit documents. Those documents are usually sold to illegal immigrants. But cyber attacks are not the only concern. At Tenet Healthcare, a former employee in the finance department pled guilty to stealing patient information. In Sarasota, Fl., an office cleaner at HealthSouth Ridgelake Hospital ordered credit cards in the names of patients whose information he had stolen. And in hospitals in Minnesota, California and Pennsylvania, laptops containing patient information have been lost and/or stolen (Messmer). With more patient information being gathered, managed, stored and transmitted via EHR systems, the potential for adverse outcomes from lost and/or stolen data is a reality that must be dealt with. Potential-Workflow Disruptions The National Institute for Health Care Management (NIHCM) offers the following definition of “workflow”: Workflow refers to how a practice organizes its staff and resources to conduct defined tasks to produce outcomes. An important part of workflow is the interactions among staff as they fulfill their tasks using available resources. Also critical is how information is (or is not) exchanged. (Lee & Shartzer) The tasks that a practice performs can be divided into Administrative (i.e., schedule appointments; document patient information; retrieve and store patient medical records; process billing and claims; communication) and Clinical (i.e., medical treatment (triage); record patient history; examine and assess patients; develop treatment plans; provide patient education; prescribe medication; order procedures and lab test; clinical follow-up with patients). (Bowens, Frye, & Jones) Studies indicate that physicians are concerned about disruptions to their practice’s workflow and productivity. This is especially true in primary care practices which typically operate with thin EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 20 margins and can little afford any drop in productivity (Rowley). In 2010, the “HIMSS EHR Usability Taskforce – User Pain Points Workgroup” study reported that workflow was the #1 “pain point” across all seventeen EHR modules/components that were studied (Ribitzky, Sterling, & Bradley). Common to the studies are the following areas of concern: incorporating the EHR system into the practice; navigating the various templates, forms and screens; having to input data while trying to maintain face-to-face communication with the patient; learning to manage the many alerts, especially the false-positives (Bowens, Frye, & Jones). In December of 2010, the University of California-Davis published the results of a study that investigated the impact of an EHR system (i.e., PracticeConnect which is based on Epic) on physician productivity. The study was limited to ambulatory care practices (i.e., internal medicine, family medicine and pediatricians). Based upon input from over 100 physicians, they found that internal medicine specialties (which include more procedure-oriented practices) adjusted to the new technology and experienced slight increases in productivity. However, family medicine and pediatrics (which is more evaluation-and-management intensive) experienced a 25-30% drop in productivity, which lasted about a month before slowly rising to near pre-EHR levels by 6 months. (Rowley) From their findings, they concluded that “one-size” does not fit all. A procedural system such as Epic might work well for procedural practices (e.g., internal medicine), but it does not work well for those practices that are more interactive and cognitive (e.g., family medicine and pediatrics). “Such tools have not yet fully matured, even in very-expensive installations of ‘mature’ EHR products.” (Rowley) EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 21 Education/Training Requirements A recent survey conducted by MGMA of 4,588 physician practices reported that 53.2% of the respondents admitted to either “mildly” or “severely” underestimating the amount of training required for implementing an EHR system (Monegain). One of the explanations for this underestimation might be a lack of understanding of the complexity of the system. In other words, the system was not as easy to learn and use as the salesman promised. However, alternative theories might shed some light on such a large percentage of underestimation. In some cases, physicians are not forthcoming in admitting that they need to be trained because they are fearful of having to learn new technologies. In other cases, they fear the loss of stature in the eyes of their subordinates if they appear to be computer illiterate. (Gelmon & Droppers, 2008) And then there is “’the Lake Wobegon effect’ (the belief by a particular group that all of its members are above average in parameters such as looks and intelligence)” (Jenkins). Often times this hubris is nurtured by the salesman who convinces the project sponsors and leaders that the system is so intuitive that it can practically run itself. Given the premium on everyone’s time, the natural tendency is to reduce the “suggested” training time, sometimes by as much as 50%. Unfortunately, once the system is up and running and the training starts, it is to everyone’s chagrin when they realize that they did not allot enough time and budget for training. And it is even more embarrassing if the amount of training that is actually required exceeds the salesman’s “recommendation” (Jenkins). Regardless of the reason for underestimating the amount of training, the success of the EHR implementation hinges on an adequately trained user population. After 35 years in the I/T field, this author has learned a valuable rule of thumb for estimating projects. Whatever the initial estimate “feels like”…double it. EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 22 Future As previously mentioned, the benefits to incorporating an electronic health record system in a medical organization, both ambulatory and inpatient, can provide improvements in productivity and quality of care. However, with the increasing implementation of EHRs due to the Health Information Technology for Economic and Clinical Health (HITECH) Act and reimbursements through the Centers for Medicare and Medicaid Services (CMS), there is an ever growing amount of patient data being accumulated that can provide secondary opportunities for non-direct care use. In a white paper by The Journal of the American Medical Informatics Association (JAMIA), Charles Safran et al. (2007) stated that, “Secondary use of health data can enhance health care experiences for individuals, expand knowledge about disease and appropriate treatments, strengthen understanding about effectiveness and efficiency of health care systems, support public health and security goals, and aid businesses in meeting customers’ needs.” Secondary use can be defined as “non-direct care use of PHI including but not limited to analysis, research, quality/safety measurement, public health, payment, provider certification or accreditation, and marketing and other business including strictly commercial activities.” (Safran et al., 2007) Collected personal health information (PHI) can provide value to both public and private organizations and industries. In the realm of research and analysis, EHRs can provide a unique opportunity to improve the “conduct of practice-based clinical research.” (Khoury, Rich, Randhawa, Teutsch & Niederhuber, 2009) Primarily, before the expansion of EHRs data was collected through organized studies entailing limited cohorts that may not provide adequate representation of different patient populations and could lead to a lack of generalizability. (Khoury et al., 2009) With the advent of the EHR and clinical data warehousing, large aggregated data sets can be analyzed, provided the EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 23 information is collected in clinical registries where completeness, consistency and accuracy are maintained. These registries require “both the collection of clinical and laboratory information at a patient encounter and a database to record this information. Thus, a standardized protocol is required, which is administered to all patients at the encounter, and is then entered into the database. Information can subsequently be obtained from the database and analyzed using a statistical package.” (Gladman & Menter, 2005) In an AMIA study done in 2010, clinical data obtained from the data warehouse at the Columbia University Medical Center in New York City was used to analyze the mortality of pancreatic cancer patients. The data was collected through the use of an EHR between the years of 1999 and 2009 and contained 3068 patients who had been diagnosed with pancreatic cancer. The focus of this study was to view the leading data quality issues that arise from not properly maintaining a clinical registry. Inaccuracies were discovered reflected by “poor granularity of the diagnosis terms or disease classification codes and inadequate or non-standardized documentation of disease status or treatment details.” (Botsis, Hartvigsen, Chen & Chunhua, 2010) Inconsistencies also occurred due to the variation in EHR data sources. For instance, chemotherapy regimens were sometimes recorded in the clinical notes and not the drug registry. Also, some diagnoses reported as chronic were captured in the clinical notes as acute. These “uncoordinated or redundant data entries into different data sources in EHR could not only cause information discrepancies but also form big barriers to selecting reliable data sources for secondary use of EHR data.” (Botsis et al., 2010) Although issues were discovered in the utilization of EHRs, in this case, the primary lack in data quality centered on user initiated actions and not the failing of the overall system. “Information incompleteness due to poor documentation could be attributed to both patients and healthcare EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 24 providers who did not report or document critical information, e.g. family history or personal habits.” (Botsis et al., 2010) The main consensus of the study reported that the secondary use of EHR data could improve quality in clinical analytics as overall improvements in data warehousing matured. (Botsis et al., 2010) Various national establishments are promoting public sector efforts in the use of secondary EHR data. Both the centers for the American Health Information Community (AHIC) and the Nationwide Health Information Network (NHIN) are developing networks that can support “safe, equitable, efficient, effective, and patient-centered health care” through the adoption and sharing of EHR data. (Safran et al., 2007) To facilitate this, the need for secure and federated information sharing will require a health information exchange (HIE) model broadly connecting EHR data. Utilizing this approach will provide advantages on two fronts. First, no one entity will completely own patient data drawing a distinction between data tenure and data access. Second, attempts to study population-based environmental and genetic illnesses can be sidelined by patient relocation and changes in family structure such as marriage or divorce. (Safran et al., 2007) Leveraging the inherent connected structure of an HIE, patient demographic information can more closely be tracked and updated provided a national patient identification system is in place. Allowing for the interconnection of desperate EHR data provides development in applications that can address public issues such as emergency preparedness, pandemic outbreaks and other public health imperatives. The AMIA under contract to the Office of the National Coordinator for Health Information Technology (ONC) “presents a vision for an ongoing cycle of data collection, research, and new knowledge generation to strengthen clinical decision support.” (Safran et al., 2007) To help foster these initiatives an upsurge in activity has been placed on the adoption of personal health records (PHR) throughout the health care community. (Tang, Ash, Bates, Overhage & Sands, 2006) The EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 25 benefits for individuals, providers and payers using PHRs continue to evolve with technology. Although the focus on patient-driven health care has been the major focus of PHRs, it will take the providers with their robust EHR systems and payers providing purchasing incentives to their clients to formalize PHR utility. All three groups pose to gain from the added incorporation between EHRs and PHRs through data sharing, decision support and chronic disease management. The same benefits can be realized with their participation with EHRs in secondary usage opportunities. To provide any advantages, PHRs need to be interconnected with a provider or accountable care organization’s EHR. The hybrid PHR-EHR system approach would allow enhanced data collection by providing patients the ability to inject pre or post-visit data otherwise not captured by the EHR. “In some cases, patients may add supplemental information that may or may not subsequently be incorporated into the provider's EHR. Some hybrid PHR systems can connect to various health care data sources to acquire and transmit data.” (Tang et al., 2006) Not only can this data be use for the betterment of the patient but, with permission, could be added to a larger data warehouse adding richness in public and private research. Public health initiatives include the management of chronic care by both the physician and the individual. The chronic care model developed by the MacColl Institute highlights both selfmanagement and decision support to improve outcomes. (MacColl, 2011) For the physician, decision support is provided by in-house or on-line databases routed through their EHR. However, for the patient “health care management tools are a relatively new form of PHR facilitators that may appeal to consumers.” (Tang et al., 2006) By providing medication information, knowledge resources and directed decision support, patients can become more engaged in their health care improving functional outcomes and medication adherence. (Tang et al., 2006) Expanding on the health care experience of individuals, PHR-EHR systems provide secondary use opportunities in both the EHR: ADVANTAGES – WEAKNESSES / THREATS - FUTURE 26 education and management of chronic diseases lifting some of the burden on an already overtaxed health care system. EHR: ADVANTAGES – WEAKNESS/THREATS - FUTURE References Abraham, S. (2010). Technological trends in health care: Electronic health record. The Health Care Manager, 29(4), 318-323. Benefits of EMR or EHR Over Paper Charts; Retrieved May 2011 from http://www.emrandhipaa.com/benefits-of-emr-or-ehr-over-paper-charts/ Berry, E. (2009, June 29). AMA meeting: Doctors object to penalties for avoiding EHRs. Retrieved from http://www.ama-assn.org/amednews/2009/06/29/prsd0629.htm Botsis, T., Gartvigsen, G., Chen, F., Weng, C. (2010). Secondary Use of EHR: Data Quality Issues and Informatics Opportunities. AMIA Summits Transl Sci Proc. 1-5. Retrieved May 2011 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3041534/?tool=pubmed Bowens, F. M., Frye, P. A., & Jones, W. A. (Fall 2010). Health information technology: Integration of clinical workflow into meaningful use of electronic health records. Retrieved from http://www.ncbi.nlm.nih.gov.ezproxy.galter.northwestern.edu/pmc/articles/PMC2966355 /pdf/phim0007-0001d.pdf Caraher, K., & LaVanway, A. H. (2010, December 13). Physician practice EHR price tag. Retrieved from http://mikemeikle.files.wordpress.com/2011/01/cdw-healthcarephysician-practice-ehr-price-tag.pdf Center for Health IT: Potential Benefits of an EHR. Retrieved May 2011 from http://www.centerforhit.org/online/chit/home/cmelearn/tutorials/ehrcourses/ehr101/benefits.html 27 EHR: ADVANTAGES – WEAKNESS/THREATS - FUTURE References Co John Patrick T., MD, MPHa, Sarah A. Johnson, BAb, Eric G. Poon, MD, MPHc, Julie Fiskio, BSc, Sowmya R. Rao, PhDd, Jeanne Van Cleave, MDa, James M. Perrin, MDa, Timothy G. Ferris, MD, MPHa,b Electronic Health Record Decision Support and Quality of Care for Children With ADHD Published online July 19, 2010 Electronic medical records: the pros and cons. (2009, March 1). Retrieved from http://healthworldnet.com/Articles/print/?C=6238 Gans, D., Kralewski, J., Hammons, T., & Dowd, B. (2005, October). Medical groups’ adoption of electronic health records and information systems. Retrieved from http://content.healthaffairs.org.ezproxy.galter.northwestern.edu/content/24/5/1323.full.pd f Gelmon, S. B., & Droppers, O. (2008). Community health centers and electronic health records: Issues, challenges, and opportunities. Retrieved from http://nwhf.org/images/files/Electronic_Medical_Record_Handbook.pdf Hillestad Richard, James Bigelow, Anthony Bower, Federico Girosi, Robin Meili, Richard Scoville and Roger Taylor Health Affairs, 24, no. 5 (2005): 1103-1117 doi: 10.1377/hlthaff.24.5.1103 Retrieved from http://content.healthaffairs.org/content/24/5/1103.full Kaiser Permanente HealthConnect: Transforming Medical Care and Service, (2007, February 15) Retrieved May 2011from http://xnet.kp.org/newscenter/ehr/2007/021507kphealthconnect.html. 28 EHR: ADVANTAGES – WEAKNESS/THREATS - FUTURE References Khoury, M. J., Rich, E., Randhawa, G., Teutsch, S., Niederhuber, J. (2009, October). Comparative effectiveness research and genomic medicine: An evolving partnership for 21st century medicine. Genetics in Medicine. 11(10), 707-711. Retrieved May 2011 from http://journals.lww.com/geneticsinmedicine/Fulltext/2009/10000/Comparative_effectiven ess_research_and_genomic.3.aspx?WT.mc_id=HPxADx20100319xMP MacColl Institute. (2011) The Chronic Care Model. Retrieved May 2011 from http://www.improvingchroniccare.org/index.php?p=The_Chronic_Care_Model&s=2 Menter, A., Gladman, D. D. (2005) Introduction / overview on clinical registries. Ann Rheum Dis. 64(2) Retrieved May 2011 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1766879/pdf/v064pii101.pdf PEDIATRICS Vol. 126 No. 2 August 2010, pp. 239-246 (doi:10.1542/peds.2009-0710) Retrieved May 2011 from http://pediatrics.aappublications.org/cgi/content/abstract/126/2/239 Practice Fusion: The Best Care for Your Patients. Retrieved May 2011 from http://www.practicefusion.com/pages/quality_of_care.html Safran, C., Bloomrosen, M., Hammond, E. W., Labkoff, S., Markel-Fox, S., Tang, P. C., Detmer, D. E. (2007, February). Toward a National Framework for the Secondary Use of Health Data: An American Medical Informatics Association White Paper. Journal of the American Medical Informatics Assoication. 14(1). Retrieved May 2011 from https://www.amia.org/files/shared/establishing_the_framework.pdf 29 EHR: ADVANTAGES – WEAKNESS/THREATS - FUTURE References Tang, P. C., Ash, J. S., Bates, D. W., Overhage, J. M., Sands, D. Z. (2006, March). Personal Health Records: Definitions, Benefits, and Strategies for Overcoming Barriers to Adoption. Journal of the American Medical Informatics Association. 13(2), 121-126. Retrieved May 2011 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1447551 Value Measurement and Return on Investment for EHRs. Retrieved May 2011 from http://www.hoise.com/vmw/06/articles/vmw/LV- VM-08-06-19.html 30