File - Wk 1-2
advertisement

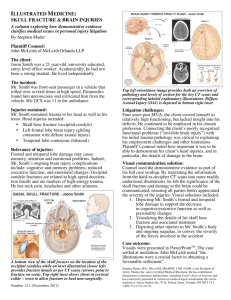
Learning Objectives Wk 12 – Head Injuries Applied Anatomy of Head Injuries Understand and explain the concepts & associated principles, functional & clinical applications of: 1. The mechanism, diagnosis and effects of extradural haemorrhage. An extradural hemorrhage can be described as bleeding between the inside of the skull and the outer covering of the brain (called the "dura"). This type of hemorrhage is typically caused by a fracture of the skull which can cause the rupturing of a blood vessel, usually an artery. This rupture will cause blood to bleed into the space between the dura matter and the skull (bone). The blood in this space will build and continuously deliver more pressure onto the brain considering that the skull is a closed compartment. This extra pressure can lead to numerous neurological symptoms and eventually death if a serious injury is not treated properly. The diagnosis of an extradural hemorrhage is usually based on a history, neurological examination and a CT scan. A patient with this hemorrhage can present with headaches, deteriorating states of consciousness, focal neurological signs (depends on which part of the brain is affected – see bottom) and a change in vital signs. Symptoms can occur within hours of a head injury with a ‘lucid interval’ of no signs between the symptom onset and the initial head injury. The extradural hemorrhage can often occur in children and adolescents because their membrane covering (of the brain) is not as firmly attached to the skull as in older people. 2. The layers (of the scalp and skull) traversed by a ‘burr-hole’ in the temporal region. Trepanation (also known as trepanning, trephination, trephining or ‘burr hole’) is a form of surgery in which a hole is drilled or scraped into the skull, thus exposing the dura mater in order to treat health problems related to intracranial diseases, though in the modern era it is used only to treat epidural (aka. extradural) and subdural hematomas. The layers of the scalp and skull traversed by a burr-hole include: skin & superficial fascia deep (temporal) fascia & pericranium outer table of compact bone diploe (spongy bone) inner table of compact bone extradural space 3. How fractures of the base of the skull may leak CSF from: the nose; the ear. A basal skull fracture is a fracture of the base of the skull, typically involving the temporal bone, occipital bone, sphenoid bone, and/or ethmoid bone. A fracture in any of these areas can cause a tear in the protective membranous layers of the brain. With regards to cerebrospinal fluid (CSF) leaks in the nose, these caused by fractures in the anterior cranial fossa that may cause the tearing of the basal dura resulting in a fistula (abnormal connection) between the cranial cavity and the frontal, ethmoid or sphenoid sinuses. This is known as CSF Rinorrhea cause for emergency as it may result in bacterial meningitis. Prophylactic antibiotics will always be required for cases such as these. CSF Otorrhea is another type of CSF leak that affects the ears. This type of leak often occurs from fractures of the skull base involving the petrous temporal bone. A fracture of the temporal bone is particularly at risk of causing a fistula through the tegmen tympani through the middle ear. Blood and CSF will leak through the perforate tympanic membrane (aka ear drum). 4. Why fractures of the body of the mandible are usually ‘compound’. The mandible is in the shaped in a semi-circle. While a blow to the mandible can yield a single isolated fracture, trauma will more frequently lead to multiple sites of fractures. For example, trauma to the side usually yields an ipsilateral body fracture and a contralateral subcondylar fracture. A classic severe blow to the symphysis produces a symphyseal fracture and bilateral subcondylar fractures. Due to their nature, these fractures will frequently become displaced and end up tearing and lacerating the tissues of the mouth. As a result, fractures of the mandible will frequently become compound fractures. Note: Compound fracture: A fracture in which the bone is sticking through the skin. Also called an “open fracture”. 5. Why scalp lacerations tend to gape and bleed profusely. Lacerations of the scalp can gape and bleed profusely because of its structural and functional nature. The scalp has a blood supply provided by 5 pairs of arteries; supratrochlear artery and the supraorbital artery which stem from the internal carotid artery; as well as the the superficial temporal artery, the occipital artery and the posterior auricular artery all of which come from the external carotid artery. These arteries freely anastamose into the second layer of the scalp and provide quite a rich blood supply. While arteries usually contract when cut in an attempt to prevent bleeding, the arteries in the scalp cannot contract due to the density of the connective tissue layer present within the scalp known as the superficial fascia. The superficial fascia is a fibrofatty layer that connects skin to the underlying aponeurosis of the occipitofrontalis muscle and provides a passageway for nerves and blood vessels. Blood vessels are attached to this fibrous connective tissue. If the vessels are cut, this attachment prevents vasospasm, which could lead to profuse bleeding after injury. Scalp lacerations also tend to gape open particularly in the coronal plane (across from left to right or vice versa) because the muscle in front (frontalis) and to the back (occipitalis) of the scalp tends to pull the laceration open. 6. The layers repaired in a suture of a scalp laceration. The layers of the scalp which repaired during suturing include: Loose Areolar Tissue – the layer immediately above the pericranium (periosteum of the skull bone) which contains the major blood vessels of the scalp. Aponeurosis – also referred to as the epicranial aponeurosis (or galea aponeurotica), is a dense layer of fibrous tissue which runs from the frontalis muscle back to the occipitalis muscle. Connective Tissue – a thin layer of fat and fibrous tissue just underneath the skin. These layers are repaired in that order (mnemonic: “LAC”) or from the inside out during the suturing of a scalp laceration. 7. The significance of emissary veins as potential avenues of intracranial spread of face and scalp infections. Emissary veins are veins that drain blood from the external veins of the skull into the dural venous sinuses. Through this route, they connect the intracranial venous system with the extracranial (face and scalp) veins. These veins however are valveless and thus blood can flow either way on these veins. As a result of this, infections can spread through the emissary veins in either way, hence scalp and facial infections can spread into the brain. Focal Neurological Signs – not a learning objective, included just for people who are interested Frontal lobe signs Frontal lobe signs usually involve the motor system, and may include many special types of deficit, depending on which part of the frontal lobe is affected: unsteadiness in walking muscular rigidity, resistance to passive movements of the limbs (hypertonia) paralysis of a limb (monoparesis) or a larger area on one side of the body (hemiparesis) paralysis head and eye movements inability to express oneself linguistically, described as an expressive aphasia (Broca's aphasia) focal seizures which can spread to adjacent areas (Jacksonian seizure) grand mal or tonic-clonic seizures changes in personality such as disinhibition, inappropriate jocularity, rage without provocation; or loss of initiative and concern, apathy, akinetic mutism, general retardation "frontal release" signs, i.e. reappearance of primitive reflexes such as the snout reflex, the grasp reflex, and the palmar-mental reflex unilateral loss of smell (anosmia) Parietal lobe signs Parietal lobe signs usually involve somatic sensation, and may include: impairment of tactile sensation impairment of proprioception, i.e. postural sensation and sensation of passive movement sensory and visual neglect syndromes, i.e. inability to pay attention to things in certain parts of the person's sensory or spatial environment. This can be as extreme as denial of a limb. loss of ability to read, write or calculate (dyslexia, dysgraphia, dyscalculia) loss of ability to find a defined place (geographical agnosia) loss of ability to identify objects based on touch (astereognosia.) Temporal lobe signs Temporal lobe signs usually involve auditory sensation and memory, and may include: deafness without damage to the structures of the ear, described as cortical deafness tinnitus, auditory hallucinations loss of ability to comprehend music or language, described as a sensory aphasia (Wernicke's aphasia) amnesia, memory loss (affecting either long- or short-term memory or both) other memory disturbances such as deja vu complex, multimodal hallucinations complex partial seizures (temporal lobe epilepsy) Occipital lobe signs Occipital lobe signs usually involve visual sensation, and may include: total loss of vision (cortical blindness) loss of vision with denial of the loss (Anton's syndrome) loss of vision on one side of the visual field of both eyes (homonymous hemianopsia) visual agnosias, i.e. inability to recognize familiar objects, colors, or faces visual illusions such as micropsia (objects appear smaller) and macropsia (objects appear larger) visual hallucinations, displaying elementary forms, such as zig-zags and flashes, in one half of the visual field only for each eye. (In contrast, temporal lobe visual hallucinations display complex forms, and fill the entire visual field.) Cerebellar signs Cerebellar signs usually involve balance and coordination, and may include: unsteady and clumsy motion of the limbs or torso (ataxia) inability to coordinate fine motor activities (intention tremor), e.g. "past-pointing" (pointing beyond the finger in the finger-nose test) inability to perform rapid alternating movements (dysdiadochokinesis), e.g. inability to rapidly flip the hands involuntary left-right eye movements (nystagmus) Brainstem signs Brainstem signs can involve a host of specific sensory and motor abnormalities, depending on which fiber tracts and cranial nerve nuclei are affected. Spinal cord signs Spinal cord signs generally involve unilateral paralysis with contralateral loss of pain sensation