Module 5: Activities of Daily Living/Immobility
advertisement
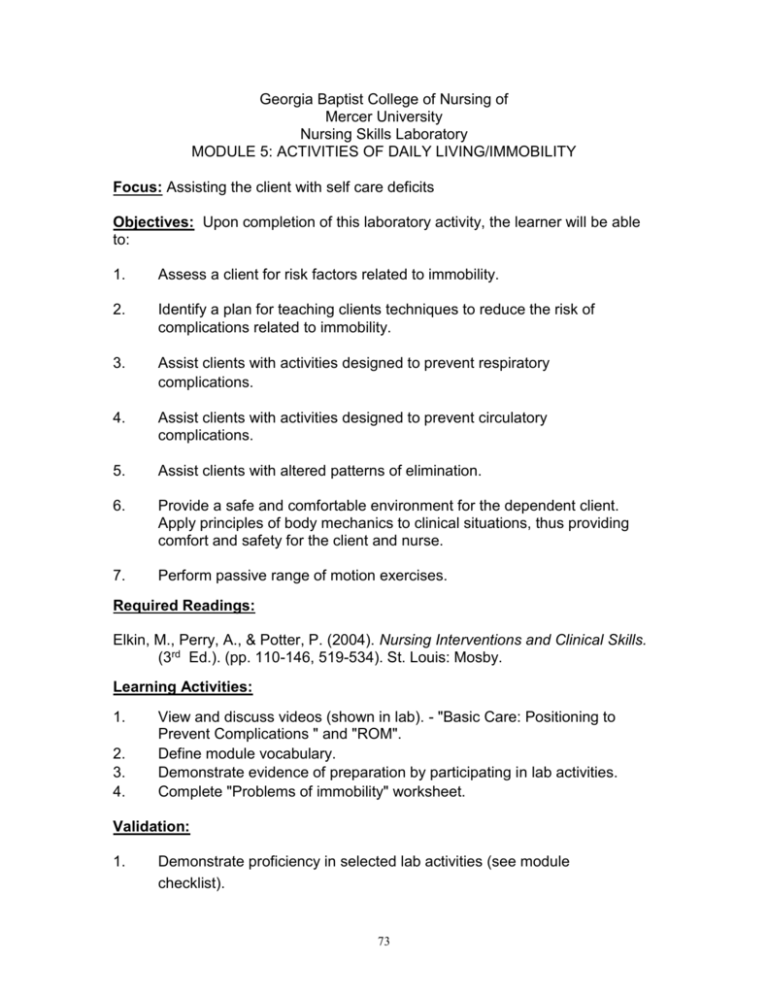
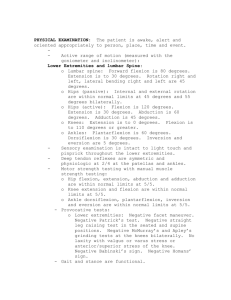
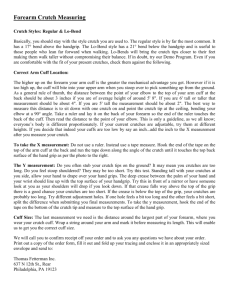
Georgia Baptist College of Nursing of Mercer University Nursing Skills Laboratory MODULE 5: ACTIVITIES OF DAILY LIVING/IMMOBILITY Focus: Assisting the client with self care deficits Objectives: Upon completion of this laboratory activity, the learner will be able to: 1. Assess a client for risk factors related to immobility. 2. Identify a plan for teaching clients techniques to reduce the risk of complications related to immobility. 3. Assist clients with activities designed to prevent respiratory complications. 4. Assist clients with activities designed to prevent circulatory complications. 5. Assist clients with altered patterns of elimination. 6. Provide a safe and comfortable environment for the dependent client. Apply principles of body mechanics to clinical situations, thus providing comfort and safety for the client and nurse. 7. Perform passive range of motion exercises. Required Readings: Elkin, M., Perry, A., & Potter, P. (2004). Nursing Interventions and Clinical Skills. (3rd Ed.). (pp. 110-146, 519-534). St. Louis: Mosby. Learning Activities: 1. 2. 3. 4. View and discuss videos (shown in lab). - "Basic Care: Positioning to Prevent Complications " and "ROM". Define module vocabulary. Demonstrate evidence of preparation by participating in lab activities. Complete "Problems of immobility" worksheet. Validation: 1. Demonstrate proficiency in selected lab activities (see module checklist). 73 2. 3. 4. Use correct body mechanics for nurse and client. Maintain your client's comfort, safety, and privacy. State scientific rationale for each action. Clinical Application: 1. 2. 3. Provide safe, thorough, and effective care for the pre- and postoperative client, clients with mobility needs. Initiate interventions designed to prevent complications related to the surgical experience or immobility. Consult with your clinical faculty for opportunities. 7/039SEB/FK; Rev. 04/04/FK; 02/05/FK 74 MODULE 5: ACTIVITIES OF DAILY LIVING, IMMOBILITY Vocabulary: Activities of Daily Living Directions: Define each word in the space provided. 1. Aspiration pneumonia: 2. Atelectasis: 3. Decompression: 4. Hypoventilaiton: 5. Hypovolemia: 6. Hypoxia: 7. Paralytic ileus: 8. Postoperative: 11/95/GH;6/98/GH Revised 11/01/SEB; Rev. 11/03/SEB 75 MODULE 5 PROBLEMS OF IMMOBILITY Body System Problems Assessment Revised 11/01/SEB 76 Nursing Care Positioning to Prevent Complications Immoblilization can produce complications 1. Respiratory System A. Decreased lung expansion B. Decreased gas exchange C. Secretions accumulate D. Pneumonia 2. Musculoskeletal System A. Decreases muscle tone B. Atrophy C. Contractures D. Deformity 3. Circulatory System A. Venous stasis B. Edema C. Phlebitis D. Clot formation (embolus) 4. Nervous System A. Pain B. Neuritis 5. Integumentary System A. Decubitus 6. Gastrointestinal System A. Decreases appetite B. Poor nutrition C. Constipation Prevent complications via 1. Change position every two hours 2. Ask client to assist 3. Place on a ‘turn schedule’ 4. Keep client in good alignment Supine positioning 1. Neutral alignment 2. Supportive aids 3. Increase circulation 4. Susceptible areas to pressureA. Ear B. Scapula C. Elbow D. Hip E. Sacrum F. Knees G. Ankles 77 5. 6. H. Heels Perform ROM Provide dry, wrinkle-free bed Before repositioning 1. Consider sequence of position 2. Consider related medical disease 3. Get supportive aids 4. Explain procedure to client 5. Provide privacy 6. Use proper body mechanics 7. Assess skin integrity 8. Provide skin care 9. Align trunk 10. Perform ROM 11. Be sure bed is clean and dry Four Positions : 1. Supine 2. Fowler’s 3. Side-lying/Lateral 4. Prone SupineReposition up in bed Use trochanter rolls at thigh and hip Use supportive aids Prevent footdrop, plantar flexion, contractures Fowler’sReposition up in bed Head of bed (HOB) up 45 degrees Support weak extremities Use supportive aids Prevent foot drop Check proper alignment Low Fowler’s-approximately 30 degrees Semi-Fowler’s-approximately 45 degrees High Fowler’s-approximately 90 degrees LateralSlide client over to one side with the draw sheet Place support pillow at back and axillary area Check proper alignment Support upper arm 78 Alternate LateralUse if client has difficulty with lateral Sim’s- (semi-prone) Position between lateral and prone positions PronePosition client over to side of bed and lower in bed Place in side lying position Roll to center of bed Support with pillow Be sure toes are off the end of mattress Assess client tolerance REMEMBER SAFETY Position with draw sheet Document tolerance, skin condition, skin care Dev. 09/01/SEB Rev. 02/05/FK 79 ASSISTIVE DEVICES 1. Canes A. Standard B. T- handle C. Quad 2. Crutches A. Axillary B. Lofstrand (handgrip and forearm band) 3. Walker A. Standard B. Foldable C. Wheels Terms Weight bearing Partial weight bearing No weight bearing REMEMBER SAFETY Review health status Assess V/S Assess level of orientation Assess ROM Assess environment Assess level of understanding Cane Assisted Ambulation 1. Used with partial weight bearing 2. Assess balance, strength, and confidence 3. Usually used unilaterally 4. Instruct client to hold cane on uninvolved side. The cane and weaker leg work together while ambulating Allow 15-30 degrees elbow flexion with the cane 5. Move cane forward 6-10 inches, while keeping weight on both legs 6. Move affected leg forward so it is even with the cane 7. Bring the unaffected leg past the cane 8. Move affected leg even with the unaffected leg 9. Repeat steps Do not use words like good or bad; instead, use involved/uninvolved affected/unaffected, right/left 80 Crutch Assisted Ambulation What disorders necessitate the use of crutches? REMEMBER SAFETY Assess arm and shoulder strength Assess balance Assess endurance Proper measurement is important Standing measurements: Two or three fingers should fit between the top of the crutch and the axilla and/or Crutch pads should be 1 1/2- 2 inches below axilla Rubber tips on crutch should reach 4 - 6 inches to side of client's feet (Handgrip) Elbow should be flexed 15-30 degrees AMBULATION 4 point gait 1. Begin with feet comfortably apart and crutches 6 inches in front and 6 inches to side of each foot. (Be sure body is in alignment) [tripod position] 2. Keeping feet together, move right crutch forward 4-6 inches 3. (Crutch and foot move in opposition) Move left foot forward to be equal level with left cane 4. Move left crutch forward 4-6 inches 5. (Crutch and foot move in opposition) Move right foot forward to be equal level with right crutch 6. Repeat 3 point gait 1. Begin in tripod position (above) 2. Bring both crutches and affected leg forward 3. Move unaffected leg forward 4. Repeat 2 point gait 1. Begin in tripod position (above) 2. (Crutch and foot move together in opposition) Move left crutch and right foot forward (together) 3. Move right crutch and left foot forward (together) 4. Repeat 81 Swing-to gait 1. Move both crutches forward 2. Lift and swing legs to crutches 3. Repeat Swing-through gait 1. Move both crutches forward 2. Lift and swing legs through and past the crutches 3. Repeat Walker Assisted Ambulation 1. Position- Upper bar of walker is slightly below client's waist. Elbows are flexed 15-30 degrees (with hands on hand grips) 2. Lift walker and move forward 6-8 inches. Step forward. Follow-through with opposite foot. (If one side is affected, step forward with affected leg first) 3. Repeat Outcomes: 1. Client will correctly demonstrate use of the assistive device 2. Client ambulates without injury 3. No significant change(s) in V/S are noted Documentation A:ambdevices.901 Dev.9/01/SEB Rev. 02/05/FK 82 Range of Motion Objectives of Range of Motion 1. Improve or maintain a) joint function and b) muscle tone and strength 2. Promote circulation 3. Counteract effects of prolonged bedrest or immobilization 4. Prevent contracture formation 5. Increase endurance 6 Develop coordination 7. Prepare for ambulation and activity Definition Range of Motion- Extent of movement of which a joint is normally capable Types of Range of Motion (ROM) 1. Active Range of Motion (AROM) 2. Active Assistive Range of Motion (AAROM) 3. Passive Range of Motion (PROM) Contracture- Strength- EnduranceTypes of movement of a synovial joint: 1. Pivot joint 2. Ball and socket joint 3. Hinge 4. Condyloid joint 5. Saddle joint 6 Gliding joint Joint Movement 1. Flexion 2. Extension 3. Hyperextension 4. Rotation- Internal and External 5. Circumduction 6 Opposition 7. Pronation 8. Supination 9. Adduction 83 10. 11. 12. 13. 14. Abduction Eversion Inversion Dorsiflexion Plantar flexion Guidelines for ROM 1. Wash hands 2. Explain/teach 3. Use proper body mechanics 4. Provide privacy 5. ROM- Support joint and limb 6 Move smoothly, slowly, rhythmically 7. Move to resistance (not pain) 8. Return joint to neutral alignment 9. Perform 2-3 times per day 10. Assess client 11. Document Suggested order for performing ROM 1. Wash hands 2. Explain ROM 3. Raise bed (body mechanics) 4. Position client close to side of bed 5. Neck- flexion, extension, rotation, hyperextension 6. Shoulder- flexion, extension, hyperextension, abduction, adduction external rotation, internal rotation, circumduction 7. Elbow- flexion, extension 8. Forearm- supination, pronation 9. Wrist- flexion, extension, hyperextension, radial deviation, ulnar deviation 10. Hands/fingers- flexion, extension, hyperextension, abduction, adduction Thumb- flexion, extension, abduction, adduction, opposition 11. Hip-flexion, -extension, abduction, adduction, external rotation, internal rotation, circumduction, hyperextension 12. Knee- flexion, extension 13. Ankle- dorsiflexion, plantar flexion 14. Foot- inversion, eversion 15. Toes- flexion, extension, abduction, adduction 16. Documentation 17. Nursing diagnosis- Impaired Mobility A: ROMvideo Dev. 9/01/SEB 84 85 Georgia Baptist College of Nursing of Mercer University Nursing Skills Laboratory MODULE 5: ACTIVITY OF DAILY LIVING/IMMOBILITY ACTIVITY WORKSHEET Directions: Participate in the following activities. Check or initial when completed. Have faculty sign or initial in the space provided when you have completed all activities. 1. Practice and critique 2 or more crutch-walking gaits. 2. Assist client with visual deficit to ambulate. 3. Practice ambulation with a walker. 4. Practice mobility using a wheelchair. 5. Perform coughing and deep breathing exercises including abdominal breathing and incentive spirometer. 6. Perform leg exercises/ROM on partner. 7. View and handle sequential compression device/plexipulse. 8. Apply TED hose to lab partner. 9. Change client's gown with "IV" in place. 10. Apply "Depends" (brief) to manikin. 11. View manikin display with various tubes & drains. Name & describe management of each tube/drain. 12. I feel I have mastered the content of this module and am able to apply in the clinical setting. 13. I need more practice/instruction. Faculty Date Rev. 04/04/FK 86