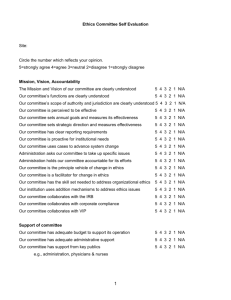
CECP Ethics Paragraphs
advertisement

Clinical Ethics Credentialing Project Center for Ethics and Law in Medicine at Montefiore Medical Center Meeting the Challenges of Clinical Ethics Consultation National Working Group Meeting November 10-11, 2008 Table of Contents Welcome Letter from Nancy Dubler ……………………………………………… 3 Meeting Agenda …………………………………………………………………… 5 Working Group Meeting Attendee List …………………………………………… 7 CECP Participant List …………………………………………………………….. 9 Section I: PowerPoint Presentations……………………………………………….. 11 #1 – Meeting the Challenges of Clinical Ethics Consultation …………….. 12 Slides by Nancy Dubler & Allen Keller; Presentation by Nancy Dubler #2 – CECP Background and Implementation …………………………….. 22 Slides & Presentation by Deborah Swiderski, Allen Keller, & Asher Aladjem #3 – Evaluation of the Clinical Ethics Credentialing Project …………….. 31 Slides by Mayris Webber & Sharon Lawrence; Presentation by Mayris Webber Section II: Sample Original Chart Notes from CECP Participants ………………. Sample Chart Note #1 …………………………………………………….. Sample Chart Note #2 …………………………………………………….. Sample Chart Note #3 …………………………………………………….. 45 46 48 50 Section III: Redacted Chart Notes from Montefiore Medical Center …………….. 52 Chart Note #1 – Patient AB ……………………………………………….. 53 Chart Note #2 – Patient CD ……………………………………………….. 55 Chart Note #3 – Patient EF ……………………………………………….. 58 Chart Note #4 – Patient GH ………………………………………………. 61 Section IV: CECP Background Documents ……………………………………… Document A – A Model for an Institutional Clinical Ethics Consultation Service ……………………………………… Document B – The Context of Clinical Ethics Consultation ……………... Document C – How to Write a Bioethics Chart Note …………………….. 64 65 77 87 Section V: CECP Tools …………………………………………………………… 94 CECP QI Form ……………………………………………………………. 95 QI Scoring System ………………………………………………………… 99 Institutional Survey ……………………………………………………….. 101 Initial Self-Efficacy Scale …………………………………………………. 103 End-of-Year Survey ………………………………………………………. 105 Final Self-Efficacy Scale ………………………………………………….. 106 ASBH Interview Guide ……………………………………………………. 107 Montefiore Credentialing Application Forms …………………………….. 110 Educational Paragraphs ……………………………………………………. 116 2 October 29, 2008 Dear Working Group Participants, First, my sincere and great thanks for coming to join us for this meeting. I realize that you are all woefully busy and one more trip to anywhere, even wonderful New York City, is low on your list of priorities. But you are all busy because you are all recognized experts in your field and that is precisely why we wanted, and needed, you to join us for this discussion. And, make no mistake, it is a discussion even though the first day is rather chock-a-block with presentations. We have determined nothing in advance. We have not written “the article”. We have lots of findings, lots of suggestions and lots of questions. We count on all of you to help us move forward to some products that will be helpful to the practices of Clinical Ethics Consultation. Here is the pitch. Many of us have toiled in the fields of bioethics consultation for many decades, making gains, experiencing setbacks, expecting standards, talking to each other, awaiting a national discussion of guidelines. Yes there have been scholarly books and articles [to which many of you have contributed] but no emerging consensus on what this creature— Clinical Ethics Consultation--looks like, how it walks, talks and leaves its image on a case—to overburden a metaphor. So, here is one opportunity for such a discussion. What emerges from our discussions will not be the ultimate word on practice and product--that will need to await further developments, perhaps some sort of certification. Our goal is to gather experienced, thoughtful and articulate professionals whose aim is to make a contribution, and set them loose on reacting, responding and critiquing our experience in the Clinical Ethics Credentialing Project. Please note that we have enclosed materials, in both CD ROM and hard copy, to facilitate the work we will be doing together. The materials include: copies of PowerPoints for presentations on Day 1, which will be devoted to the theoretical and practical background of the project; CECP Tools, the actual instruments and documents used in the CECP training; sample chart notes from CECP participants, to give you a flavor of the work generated by project participants; sample chart notes from Montefiore Medical Center; and CECP background documents, which we hope to discuss in depth with you on Day 2 Now some details: The Beacon Hotel is where the Dublers put up out-of-town guests who spill over the room in our small Manhattan apartment. It has many benefits—a small kitchenette is one—and proximity to Fairway--NYC’s best greengrocer--is the other. And, for academic projects like ours, it is affordable. So, for Sunday night, if you are tired, go across to Fairway for food, wine is at the corner of 74th and enjoy. If you are in the mood to go out, I suggest: Nikkos—corner 76th and Broadway—looks junky but has great food, Greek and broiled fish are specialties; Ruby Foos—corner 75th and Broadway—Asian fusion; Nice Matin—79th and Amsterdam—really good food a bit upscale from the others; Haru—82nd and Amsterdam—good Japanese—also a bit fusion. 3 Transportation to Cardozo Law School: Taxi—self explanatory. Bus—corner of Broadway and 72nd is the Number 5 Limited that scoots you down Broadway to 5th Avenue and 13th Street and gives a great tour of the city. Note that for the bus you will need a Metrocard that is available in the atrium of the Subway station at 72nd street. Between 8 and 9 the buses run every 6 minutes and take about 45 to get there. Subway—corner of 72nd and Broadway is the #2 and 3 express that gets you to 14th Street in three stops and is really quick—much quicker than taxi or bus if you are running late. Short walk to the law school—two blocks downtown and two east from 7th Ave to 5th Ave. VERY IMPORTANT: PLEASE KEEP ALL RECEIPTS—EVEN THE SMALL ONES. THE REIMBURSING AUTHORITIES REQUIRE ALL ORIGINGAL RECEIPTS. For those of you now accustomed to the more forgiving rules on reimbursement [for over $50 or $75 used by most institutions] THESE DO NOT APPLY TO MONTEFIORE’S DEPARTMENT OF FAMILY AND SOCIAL MEDICINE. KEEP ALL ORIGINAL RECEIPTS FOR SUBMISSION. Continental breakfast is at Cardozo from 8:30 am on Monday November 10 and we will begin at 9am. Dinner Monday evening is at the Blue Water Grill that is rated by Zagats as one of the 20 best restaurants in NYC. [I skimp on hotel but not on food]. The meeting will end at 5:30 pm and dinner is at 6 pm so that the tired among us can return to the hotel in time to crash. My home number is 212-362-3649 and I can be reached over the weekend, or indeed at any time. So, safe trip in and again thank you so much for joining us in this adventure. Nancy 4 CECP Working Group Agenda Day 1: 8:30 am – 9:00 9:00 – 10:00 10:00 – 11:00 11:00 – 11:15 11:15 – 12:30 pm 12:30 – 1:30 1:30 – 3:15 3:15 – 3:30 3:30 – 5:00 Breakfast Introduction to the meeting (Nancy Neveloff Dubler, LLB) Clinical Ethics Consultation: How it looks to the Institution (Gary Kalkut, MD – Senior VP and Medical Director, MMC) Coffee Break Introductions Lunch CECP Background and Implementation (Deborah Swiderski, MD; Allen Keller, MD; Asher Aladjem, MD) Coffee Break Evaluation of the CECP Training Program (Mayris Webber, DrPH) Day 2: 8:30 am – 9:00 Breakfast 9:00 – 10:00 Consensus Statement 10:00 – 12:00 pm Review of Documents Topics for review, discussion, and consideration for Consensus Statement A. Elements of a Clinical Ethics Consultation (CEC) Service 1. Clear indications for a consultation 2. Regular process for convening care providers 3. A typed note in the chart 4. A standard form for writing the Clinical Ethics Consultation note in the chart 5. Conception of Bioethics as one voice in a complex institutional system— Collaborative Bioethics 6. A Robust Quality Improvement process 7. A Peer Review Process 8. Credentialing and Privileging B. How to write a Bioethics Chart Note: C. The Context of Clinical Ethics Consultation? 1. How did Clinical Ethics Consultation evolve? 2. Are Guidelines and Standards needed to structure these services? 3. How is Clinical Ethics Consultation both similar to and different from other expert medical consultation? 4. What is Clinical Ethics Consultation [CEC]? 5. When is a clinical ethics consultation appropriate? 6. What skills are needed for clinical ethics consultation? 7. What is General Bioethics Consultation? 8. What skills are needed for general bioethics consultation? 9. What is an appropriate trigger for ethics consultation? 5 10. Does there always need to be a meeting for a CEC to occur? 11. How should an ethics consultation be triggered? 12. Who should be able to request a consultation? 13. How could the consultant structure the Clinical Ethics Consultation? 14. Who pays for this elaborate process and how can it be accomplished without financial support? 15. Is it critical that there be a note in the chart? 16. What can be done if the administration or the office of legal counsel objects to a written chart note? 17. Must the chart note be typed? 18. How should chart notes be used, protected and communicated? 19. Some final thoughts on diction, structure and perspective of the chart note and of the CEC 12:00 – 1:00 1:00 – 3:00 6 Lunch Continued Discussion CECP Working Group Meeting Attendees Asher Aladjem, MD Bellevue Hospital NYU School of Medicine Asher.aladjem@med.nyu.edu 212-562-2526 Adrienne Asch, PhD Yeshiva University asch@yu.edu 212-960-0834 Edward J. Bergman, JD University of Pennsylvania ejb@gear3.net 609-921-1502 Robert Arnold, MD University of Pittsburgh drpalliative@gmail.com 412-692-4834 Mark Aulisio, PhD Case Western Reserve University Mark.aulisio@case.edu 216-778-8497 Kenneth Berkowitz, MD Veterans Administration Kenneth.berkowitz@va.gov 212-686-7500 x3989 Montefiore/Einstein Center for Bioethics Kate Ettinger, JD Mural Institute ettinger@jhu.edu 415-861-1280 ndubler@montefiore.org 212-362-3649 Joseph Fins, MD Nancy Dubler, LL.B. Senior Associate New York Weill-Cornell Medical Center Margot Eves, JD Cleveland Clinic jjfins@med.cornell.edu 212-746-4246 Fellowship in Advanced Bioethics mmeves@gmail.com 216-445-1286 (office) 917-701-6646 (cell) Joel Frader, MD Allen Keller, MD Bellevue Hospital NYU School of Medicine Ask45@aol.com 212-994-7169 Northwestern University Medical School JEFrader@childrensmemorial.org 773-880-8361 Sharon Lawrence Montefiore Medical Center slawrenc@montefiore.org 718-920-4094 Hannah Lipmann, MD Montefiore Medical Center hlipmann@montefiore.org Lisa Lehmann, MD Harvard Medical School Llehmann1@partner.org 617-820-8682 Bernard Lo, MD University of California, San Francisco Bernie@medicine.ucsf.edu 415-476-5370 7 Mary Majumder, JD, PhD Baylor College majumder@bcm.edu 713-798-3511 Tia Powell, MD Montefiore Medical Center tpowell@montefiore.org 718-920-6226 Ramanathan Raju, MD NYC Health and Hospitals Corporation rajur@nychhc.org 212-788-3339 Lynn Richmond, NP Montefiore Medical Center lrichmon@montefiore.org 718-920-7052 Salvatore Russo Lawrence Schneiderman, MD University of California, San Diego ljs@ucsd.edu 858-534-4206 NYC Health and Hospitals Corporation Salvatore.russo@nychhc.org 212-788-3300 Jeffrey Spike, PhD Florida State University Tallahassee Medical Center Jeffrey.spike@med.fsu.edu 850-645-1540 Deborah Swiderski, MD Montefiore Medical Center Albert Einstein College of Medicine dswiders@montefiore.org 718-920-2818 8 Daniel Sulmasey, OFM, MD, PhD St. Vincent Catholic Medical Centers Daniel_sulmasey@nymc.edu 212-604-8280 Anita Tarzian, PhD, RN University of Maryland atarzian@law.umaryland.edu 410-706-4457 Mayris Webber, DrPH Montefiore Medical Center Albert Einstein College of Medicine mwebber@montefiore.org 718-999-2665 CECP Participants David Alfandre Nessa Coyle Mount Sinai Med. Center, non-HHC Memorial Sloan-Kettering Cancer Center, nonHHC Ife Ayodele Metropolitan Hospital, HHC Karen David Metropolitan Hospital, HHC Patricia Banks Coney Island Hospital, HHC Anca Dinescu Mount Sinai Med Center, non-HHC Andy Benejam Lincoln Hospital, HHC Maureen Eisner Westchester Med. Center, non-HHC Shirley Berenstein AHRC NYC, non-HHC Steven Field NYU Hospital Center, non-HHC Kenneth Berkowitz VA Med Center (Observer) Simon Fink NY Hospital-Queens, non-HHC Jeffrey Brensilver Soundshore Med. Center, non-HHC Barbara Flax Elmhurst Hospital, HHC Catherine Cahill Montefiore Medical Center, non-HHC Cornelia Fleming Sound Shore Med. Center, non-HHC Deborah Cappell North Central Bronx Hospital, HHC Michael Gage Hudson Valley Hospital Center, non-HHC Linnea Capps Harlem Hospital, HHC Claudene George Montefiore Medical Center, non-HHC Mary Caram Harlem Hospital, HHC Patricia Murray Given Staten Island Univ. Hospital, non-HHC Sandra Chaiken Jacobi/ North Central Bronx, HHC Douglas Green Hospital for Special Surgery, non-HHC Maggy Chalvire Woodhull Medical Center, HHC Shelley Henderson Lawrence Hospital, non-HHC Barbara Chanko VA Med Center (Observer) Barrie Huberman Lenox Hill Hospital, non-HHC Ilene Cohen Bellevue Hospital, HHC Jeanne Kerwin Overlook Hospital, non-HHC 9 Scott Klein Nicole Pearlstein Maimonides Medical Center, non-HHC Queens Hospital, HHC Stephanie Levy Susan Pincus St. Michael’s Medical Center, non-HHC AHRC NYC, non-HHC C. Ronald MacKenzie Daniel Pomerantz Hospital for Special Surgery, non-HHC Sound Shore Med. Center, non-HHC Christine Malmgreen Robin Rait Hudson Valley Hospital Center, non-HHC St. Barnabus Hospital, non-HHC May Mamiya Ellen Rosman Vassar Brothers Med. Center, non-HHC AHRC NYC, non-HHC Isaac Mann Susan Sanelli Metropolitan Hospital, HHC Queens Hospital, HHC Franca Martino-Starvaggi Naalla Schreiber Montefiore Medical Center, non-HHC Montefiore Medical Center, non-HHC Jeff Matican Haseen Sharma-Cooper Englewood Hospital, non-HHC North Central Bronx Hospital, HHC H. Hugh Maynard-Reid Rita Sherman Woodhull Medical Center, HHC Woodhull Medical Center, HHC Mary McCabe Pavel Shulman Memorial Sloan-Kettering Cancer Center, nonHHC Coney Island Hospital, HHC Sheldon Stachel Carol Mutnick Woodhull Medical Center, HHC NY Hospital-Queens, non-HHC Jan St. Hill David Nassef North Central Bronx Hospital, HHC Pitney Bowes (Observer) Naomi Tamerin Helayne Neri Cherin No hospital affiliation, non-HHC Coney Island Hospital, HHC Gregory Todd Elizabeth Nilson Maimonides Med. Center, non-HHC Weill Cornell Medical College, non-HHC Vanessa Young Lawrence Noble Harlem Hospital, HHC Elmhurst Hospital, HHC James Zisfein Brent Pawlecki Pitney Bowes (Observer) 10 Lincoln Hospital, HHC Section I PowerPoint Presentations 11 Presentations #1: Nancy Dubler 1 ___________________________________ ___________________________________ Meeting the Challenges of Clinical Ethics Consultation National Working Group November 10-11, 2008 ___________________________________ ___________________________________ ___________________________________ Nancy Neveloff Dubler LL.B. Senior Associate Montefiore-Einstein Center for Bioethics Montefiore Medical Center, Bronx, NY Professor Emerita the Albert Einstein College of Medicine ___________________________________ ___________________________________ 1 2 ___________________________________ History of Bioethics at Montefiore Medical Center ___________________________________ • 1978—Retrospective Review • 1980-1992—Prospective Consultation: neutral space • 1992—Mediation Training: skills • 1996—JCAHO Standard on Ethics capacity • 1994—Certificate Program in Bioethics and Medical Humanities: trained 250 professionals • 2000—Fellowship in Clinical Ethics: [failure] • 2007—Credentialing and Privileging Fellowship Training ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 2 3 ___________________________________ Role of JCAHO ___________________________________ … significant growth in clinical ethics consultation services has been spurred mainly by the demands of JCAHO accreditation, which states that: The goal of the ethics, rights, and responsibilities function is to improve care, treatment, services, and outcomes by recognizing and respecting the rights of each client and by conducting business in an ethical manner. [i] [i] CAMBHC Update 2, September 2006, R1-1. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 3 12 4 ___________________________________ Value Preferences Determined ___________________________________ • • • • • • Personal Narratives Religious Commitments Ethnicity Level of Education Health Care Disparities Experience with the United States Health Care System • Quality of Illness [AIDS] ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 4 5 ___________________________________ What is a Bioethics Consultation? ___________________________________ General Ethics Consultation [GEC]: • expert discussion of the content and history of ___________________________________ bioethics concepts including: ___________________________________ – bases in the law and in the scholarly medical and philosophical commentary – the shared principles and practices of American medicine and law ___________________________________ Clinical Ethics Consultation [CEC]: • facilitation of the process of discussion and decision ___________________________________ making; • mediation of conflict between and among the staff or ___________________________________ between staff and patient or family 5 6 ___________________________________ Major Domains of Ethics Consultation • • • • • • • • ___________________________________ shared decision making with patients ethical practices in end-of-life care patient privacy and confidentiality professionalism in patient care ethical practices in resource allocation ethical practices in business and management ethical practices in the everyday workplace, and ethical practices in research. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ [ASBH-draft May 2008] 6 13 7 ___________________________________ ___________________________________ ___________________________________ Quality Improvement in Clinical Ethics Consultation 1978-2006 ___________________________________ ___________________________________ ___________________________________ ___________________________________ 7 8 ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 8 9 ___________________________________ Quality Improvement in Clinical Ethics Consultation ___________________________________ ___________________________________ 2004: Notes Typed in the Chart ___________________________________ ___________________________________ 2006: Expert Outside Review 2008: QI process on all chart notes for 2007 ___________________________________ ___________________________________ 9 14 10 ___________________________________ Quality Improvement in Clinical Ethics Consultation ___________________________________ Report to the Montefiore Quality Council: 2006 • Were appropriate people involved in consultation? • Do consultations reflect legal and ethical principles governing contemporary bioethics? • Is the process of consultation clear? • Does the process of consultation conform to Bioethics Mediation Model? • Was there conflict? • Was the conflict resolved? • Was there a description of the consensus reached, or was the disagreement ongoing? ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 10 11 ___________________________________ Results ___________________________________ • Reviewers’ responses indicated that: “A strong feature is the clear distinction between legal and ethical principles”. • “Often disagreements are resolved by understanding the patient’s or family’s view and the reasons they do not agree with the healthcare team’s recommendations”. • “When consensus was reached, it was clearly described in the note, usually with practical suggestions for application”. • “When disagreements continued, the note generally clarified the nature of the disagreement and the positions of the parties”. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 11 12 ___________________________________ Suggested Opportunities for Improvement: ___________________________________ • A more structured consultation note to ensure that all important information is included; • Greater consistency in the reports; • Reports should indicate the need for addressing recurring systems issues; • More attention to communication in bioethics disputes; • Use more open-ended questions; • Empathic comments; • “I wish …” statements; ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 12 15 13 ___________________________________ Suggested Opportunities for Improvement: ___________________________________ • Development of the electronic medical record; • Shared central drive files; • Regular meetings with the Medical Director’s Office and the Clinical Ethics Consultation service. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 13 14 ___________________________________ Electronic Medical Record ___________________________________ Need to be credentialed and privileged Epiphany: Dr. Gary Kalkut Leading to: ___________________________________ ___________________________________ – Process: for Credentialing and Privileging – Product: Proposal: Standards for Clinical Ethics Consultation: – Program: MMC Training Program ___________________________________ ___________________________________ ___________________________________ 14 15 History of CECP Clinical Ethics Credentialing Project Fox, E, Myers, S, Pearlman, R, Ethics Consultation in U.S. Hospitals: A National Survey, AJOB, February 2007. Study reveals that clinical ethics consultation: • currently available in 81% of all general hospitals and 100% of hospitals over 400 beds. • only 41% of consultants had formal supervised training in ethics consultation; • 65% made recommendations and 6% never did; • 22% of Ethics Consultation Services performed no consultations in the previous year and; • 90% performed fewer than 25; • only 4% of consultations were evaluated by anyone outside of the process. 15 16 ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 16 ___________________________________ Critical Fox Findings ___________________________________ • 29,000 individuals devoted more than 314,000 hours to perform over 36,000 consultations/year ___________________________________ ___________________________________ – Who are they? – Do hospitals know what they are doing? – How and when are they intervening – How do they document their intervention? – Does anyone review these consultations for quality? ___________________________________ ___________________________________ ___________________________________ 16 17 ___________________________________ The Value of Clinical Ethics Consultations ___________________________________ • A clinical ethics consultant may bring breadth and resonance to difficult situations: ___________________________________ – Trained in the language, substance and theory of bioethics and the law – Knowledgeable of the literature and history of medicine – Trained in conflict resolution/mediation ___________________________________ • A clinical ethics consultant can address ethical issues and conflicts free from the constraints of medical power and prior family dynamics. ___________________________________ ___________________________________ ___________________________________ 17 18 ___________________________________ The Danger of Clinical Ethics Consultation ___________________________________ • Potential for inadequately trained medical/hospital staff to impose their own values on patients and families, under the guise of accepted bioethical principles • Individual and family interests/rights may be readily violated • A poorly trained clinical ethics consultant can exacerbate discord, further obfuscate the issues and make difficult situations worse. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 18 17 19 ___________________________________ Proposal Submitted ___________________________________ Standards for Clinical Ethics Consultation: Credentialing and Privileging Consultants and Creating a Model for Continuous Quality Improvement ___________________________________ ___________________________________ ___________________________________ Submitted by ___________________________________ Montefiore Medical Center (MMC) and New York City Health and Hospitals Corporation (HHC) ___________________________________ 19 20 ___________________________________ Funders • • • • ___________________________________ United Hospital Fund New York Community Trusts Silverman Family Fund HHC Foundation ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 20 21 ___________________________________ Aims 1 and 2 ___________________________________ 1. Designing a process to credential and privilege clinical ethics consultants; ___________________________________ ___________________________________ 2. Creating a one-year training program in clinical ethics consultation: ___________________________________ – One group for HHC staff and another group for MMC and other hospital staff – Participants qualify for credentialing based on status as graduates of the Certificate Program in Bioethics and Medical Humanities or comparable education 21 18 ___________________________________ ___________________________________ 22 ___________________________________ Aims 3 and 4 ___________________________________ 3. Developing a QI tool for clinical ethics consultation that: ___________________________________ – Permits the collection of quantitative and qualitative data – Employs an on-going peer review of consultation notes – Integrates the findings of this process into: • the hospital’s overall QI structure ___________________________________ ___________________________________ • the practice of the consultation services • the individual’s biannual privileging assessment ___________________________________ 4. Convening a working group of nationally recognized experts in bioethics and clinical ethics consultation to: – Advise core staff during the development of this project – Convene one two-day meeting to examine the components of the proposed Credentialing, Privileging and QI Process ___________________________________ 22 23 ___________________________________ Products of the Grant ___________________________________ ___________________________________ 1) A credentialing tool including: -suggested scoring system and guidelines for applicant references -suggested standards for the biannual re-privileging process required by JCAHO ___________________________________ 2) Recommendations for the design of a one-year training program 3) A library of educational, analytic paragraphs for use in clinical ethics chart notes; 4) A QI tool for assessing the quality of clinical ethics consultations 5) Recommendations from an expert panel on standards for credentialing and privileging clinical ethics consultants. ___________________________________ ___________________________________ ___________________________________ 23 24 ___________________________________ The “Paragraphs” DECISION-MAKING CAPACITY Determining whether a patient has the capacity to make medical decisions is often a key ingredient of a clinical ethics consultation. Decisional capacity is not a legal determination (this is called “competence”) but a clinical one that can be made by any member of the health care team who is familiar with the patient and has interacted with him or her over a more or less extended period of time. Capacity refers to the patient’s ability to perform a set of cognitive tasks, including: • Understanding and processing information about diagnosis, prognosis, and treatment options; • Weighing the relative benefits, burdens, and risks of the therapeutic options; • Applying a set of values to the analysis; • Arriving at a decision that is consistent over time; • Communicating the decision. Having capacity enables an individual to make decisions; it does not obligate him or her to do so, and in fact a person with decisional capacity may waive the right to make decisions or confer this right on others. 24 ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 19 25 ___________________________________ MONTEFIORE MEDICAL CENTER DELINEATION OF CLINICAL PRIVILEGES CLINICAL ETHICS CONSULTATION ___________________________________ ___________________________________ Clinical Ethics Consultation is the intervention by a trained bioethics professional that: • responds to the request from any member of medical care team, patient or family member for a bioethics consultation; • gathers the clinical care team and other consultants to discuss the case; • involves the patient or family with a select number of the health care team to maximize options and seek consensus; • employs discussion of bioethical principles and practices, facilitation and mediation to reach a consensus about a plan of care going forward; • documents the process and substance of the consultation in the medical record. ___________________________________ ___________________________________ ___________________________________ ___________________________________ 25 26 ___________________________________ Criteria for Granting of Privileges (check all that apply) ___________________________________ Completion of Certificate Program in Bioethics and Medical Humanities or comparable academic program. _ Completion of Montefiore’s Fellowship Training Program in Clinical Ethics Consultation or comparable experience. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 26 27 ___________________________________ Criteria for Reappointment of Privilege ___________________________________ ___________________________________ • Completion of requisite number of Clinical Ethics Consultations • Participation in the Bioethics Committee Journal Club (Attendance Certificate Attached) • Indication of site-specific privileges, where appropriate. 27 20 ___________________________________ ___________________________________ ___________________________________ ___________________________________ 28 ___________________________________ Elements of a Clinical Ethics Consultation Service (CECS) : ___________________________________ 1. Clear indications for a consultation; 2. Regular process for convening care providers; 3. A standard form for writing the Clinical Ethics Consultation note in the chart; 4. A typed note in the chart; 5. Conception of Bioethics as one voice in a complex institutional system— Collaborative Bioethics; ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 28 29 ___________________________________ Elements continued: ___________________________________ 6. A Robust Quality Improvement process; 7. A Peer Review Process; 8. Credentialing and Privileging. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 29 30 ___________________________________ Goals for this Meeting • • • • • • • • • ___________________________________ Review Discuss Assess Think Project Strategize Decide if Standards are Needed Select Standards Determine Process for Dissemination ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 30 21 Presentation #2: Deborah Swiderski, Allen Keller, and Asher Aladjem 1 ___________________________________ ___________________________________ ___________________________________ CECP Background and Implementation ___________________________________ ___________________________________ Site PIs Deborah Swiderski, MD Allen Keller, MD John Corser, MD Asher Aladjem, MD ___________________________________ ___________________________________ 1 2 ___________________________________ Background 1. ___________________________________ Although the ASBH has developed a set of capacities that an ethics consultant should possess, there are no agreed-upon standards for how an individual could or should prepare to become a clinical ethics consultant ___________________________________ 2. There is no agreed-upon standard for either the process or the documentation of bioethics consultation ___________________________________ 3. Very few institutions have a process in place for evaluating bioethics consultations ___________________________________ ___________________________________ ___________________________________ 2 3 ___________________________________ CECP Aims 1. 2. 3. 4. ___________________________________ To design a process to credential and privilege clinical ethics consultants To create a one-year training program in clinical ethics consultation who qualify as credentialed To develop a QI tool employing on-going peer review of consultation notes, with integration of the findings of this process into the practice of the consultation service, the individual’s biannual privileging assessment, and the hospital’s overall QI structure. To assemble a working group of national experts in bioethics and clinical ethics consultation ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 3 22 4 ___________________________________ Pilot at Montefiore Medical Center 2006-2007 ___________________________________ • 4 physicians who had completed Certificate Program met monthly with the Division of Bioethics • Goal 1: to refine the QI tool by applying it to existing chart notes • Goal 2: to scrutinize the structure and content of consult notes. • Goal 3: To train these individuals to become consultants through an apprenticeship model ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 4 5 ___________________________________ What did we learn during the pilot? 1. ___________________________________ ___________________________________ Consultants felt the quality of their notes improved with imposed structure 2. ___________________________________ The “dreaded” QI tool applied to notes is an acceptable proxy for consultation process 3. ___________________________________ Group discussion of notes using QI tool provided a forum ___________________________________ for peer review of consult process 4. “Educational paragraphs” were needed for ethical teaching ___________________________________ points commonly used in consultation notes 5 6 ___________________________________ Non-HHC Participants ___________________________________ • 20 institutions, varied in size, structure and governance • 35 participants ___________________________________ ___________________________________ ___________________________________ • No shared institutional commitment to CECP mission ___________________________________ • Wide spectrum of bioethics practice across institutions ___________________________________ 6 23 7 ___________________________________ CECP Phase I ___________________________________ Training program would run from September, 2007 through June, 2008 ___________________________________ Core faculty: ___________________________________ • Principal Investigator • Site Leaders from Montefiore and HHC • Epidemiologist/Evaluator • Ethics Scholar ___________________________________ ___________________________________ ___________________________________ 7 8 ___________________________________ Recruitment ___________________________________ 1. PI was principal recruiter ___________________________________ 2. Certificate Program graduates were main pool of ___________________________________ recruits (Certificate to serve as necessary credential to enter project) ___________________________________ 3. Additional participants recruited by word of mouth 4. Entry “test” for those who had not completed Certificate Program ___________________________________ ___________________________________ 5. Participants to submit original consultation note before formal process began 8 9 ___________________________________ Plan for Training Process ___________________________________ 1. Monthly 3-hour meetings of participants and faculty 2. Participants would submit notes from their practices throughout the year 3. Participant notes would be reviewed using QI tool ___________________________________ 4. Work in dyads or triads to analyze notes and report back to entire group ___________________________________ 5. Group discussion of notes and process of using QI tool, moderated by PI First session to analyze note written by PI, to familiarize group with process ___________________________________ ___________________________________ 9 24 ___________________________________ 10 ___________________________________ Additional aspects of training ___________________________________ ___________________________________ 1. Participants expected to learn to use educational paragraphs in their notes ___________________________________ ___________________________________ 2. Online journal club: key to future credentialing efforts ___________________________________ ___________________________________ 10 11 ___________________________________ Actual Experience ___________________________________ ___________________________________ • Less than half of participants produced an ___________________________________ original note prior to start of pilot • Many never required to write notes in their ___________________________________ practice ___________________________________ • Many insecure about quality of notes if they did write them ___________________________________ 11 12 ___________________________________ Turbulence and Tumult ___________________________________ • First 2 meetings spent trying to apply QI tool to a faculty note • Much expressed dissatisfaction with, and resistance to, the QI tool • Difficult meetings • Different starting points; experience, comfort levels, and skill sets • Participants asked for a standardized experience from which to generate a note: in-class role plays were adopted as a method to provide this • PI developed a document “How to Write a Bioethics Chart Note” ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 12 25 13 ___________________________________ Moving Forward ___________________________________ • Cases/role plays had been developed for training in the ___________________________________ certificate program ___________________________________ • Role plays were “run” by PI and site PIs, who would periodically stop action, discuss, offer observations, ___________________________________ suggestions, entertain questions (mediation training “fish bowl”) ___________________________________ • Became clear that this was an excellent and desired vehicle to learn “how to do a consult” ___________________________________ • PI developed a document “The Context of Clinical Ethics Consultation” 13 14 ___________________________________ Finally! ___________________________________ • Participants notes on role plays were discussed in class, using QI tool ___________________________________ ___________________________________ • Very productive sessions • Gradually, participants brought in their own notes ___________________________________ • Discussion of notes, using QI tool as framework for analysis, allowed discussion of actual consult process ___________________________________ ___________________________________ 14 15 ___________________________________ CECP Qualitative Outcomes at non-HHC Facilities • • • • ___________________________________ Identified need for ongoing peer-review Enthusiasm for role-play methodology Ultimately embraced use of QI tool Educational paragraphs regarded as critical ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 15 26 16 ___________________________________ Next Steps ___________________________________ • Varied progress at different institutions ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 16 17 ___________________________________ HHC Project Background ___________________________________ • The New York City Health and Hospitals Corporation (HHC) is the largest public hospital system in the U.S. and serves 1.3 million New Yorkers-nearly 400,000 who are uninsured. ___________________________________ • ___________________________________ HHC provides services at 11 acute care hospitals, 4 skilled nursing facilities, 6 large diagnostic and treatment centers and more than 80 community based clinics located throughout the 5 Boroughs of NYC. . ___________________________________ ___________________________________ ___________________________________ • HHC also provides home health services in New York City. 17 18 ___________________________________ HHC Mission ___________________________________ • To extend equally to all New Yorkers, regardless of their ability to pay, comprehensive health services of the highest quality in an atmosphere of humane care, dignity and respect; • To promote and protect, as both innovator and advocate, the health, welfare and safety of the people of the City of New York; • To join with other health workers and with communities in a partnership which will enable each of our institutions to promote and protect health in its fullest sense -- the total physical, mental and social well-being of the people. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 18 27 19 ___________________________________ Ethics Consultations at HHC Prior to CECP (Strengths) ___________________________________ • Shared mission • Each HHC hospital has an ethics committee generally serving 3 roles: ___________________________________ ___________________________________ – Policy development – Education – Ethics Consultation • Committees are multi-disciplinary • Many Committee members are graduates of the Montefiore Ethics Certificate Course. (HHC provides funding for this) • Strong linkages with Hospital Risk Mgmt. Depts. and with HHC Central Office • HHC Consortium of Ethics Committee Chairs meeting regularly for several years • Annual Ethics Symposium for hospital committee members ___________________________________ ___________________________________ ___________________________________ 19 20 ___________________________________ Ethics Consultations at HHC prior to CECP (Challenges) ___________________________________ • Variability in number, experience, and availability of ethics committee members and consultants. • Variability in ethics-related policies between different hospitals • Underdeveloped infrastructure for Committee functioning and evaluation • Committee work, including consultation, is added responsibility for individuals with already busy schedules ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 20 21 ___________________________________ CECP at HHC: Carpe Diem! ___________________________________ • Need for trained, credentialed ethics consultants • Strong support from HHC Leadership • External funding • Opportunity for implementing a replicable ethics consultation model that can be adapted and evaluated ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 21 28 22 ___________________________________ HHC CECP Implementation ___________________________________ • 25 participants from 10 HHC facilities • Strong group identity • Variability in experience, ability and confidence to conduct consultations • Initial resistance to applying the QI tool ___________________________________ ___________________________________ ___________________________________ – “Is the note a good proxy for the consult”? – “When will we learn how to do a bioethics consult?” ___________________________________ • Untimely death of Dr. John Corser, beloved leader, colleague and friend ___________________________________ 22 23 ___________________________________ CECP Outcomes at HHC ___________________________________ • Forum and network developed for sharing knowledge and experience • Strengthened skills in conducting consultations and writing notes • Progress in disseminating and implementing model throughout HHC • Commitment from HHC leadership for providing needed support for ethics Committees and Consultation Services ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 23 24 HHC CLINICAL ETHICS CONSULTANT CREDENTIALING AND PRIVILEGING KEY POINTS • Both Physicians and Non-Physicians are eligible for credentialing and privileging as clinical ethics consultants at all HHC Facilities. • Physicians are initially credentialed through their Facility’s Medical Board. Re-credentialing every two years is through the Medical Board as well. • Nurses, Nurse Practitioners, Physician’s Assistants, and midwives are initially credentialed through their Facility’s Medical Board. Recredentialing every two years through their Facility’s Human Resources Department. • HHC staff other than those listed above, (eg. Social Workers, Attorneys, PhD’s in philosophy) are credentialed and re-credentialed through their facility’s Human Resources Department. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ • Chairs of Ethics Committees are responsible for evaluating and approving individuals for credentialing prior to being referred to the medical board or Human Resources. 24 29 25 ___________________________________ HHC CLINICAL ETHICS CONSULTANT CREDENTIALING AND PRIVILEGING KEY POINTS ___________________________________ • Criteria for Ethics Committee Chairs to evaluate and approve individuals for credentialing include: – – – – Completion of Advanced Bioethics Training Committee Chairs have discretion to appoint individuals they deem qualified. Individuals requesting credentialing/re-credentialing as a Clinical Ethics Consultant must read and submit in writing a brief critique (1 page) of 10 bioethics related articles in scholarly journals each year. (The CECP Bioethics server will post these articles.) • Prior to Initial Credentialing/Privileging, Clinical Ethics Consultation candidates shall be observed conducting at least one ethics consultation • The chart notes of the credentialed Clinical Ethics Consultants will be reviewed every year and approved by Quality Improvement process. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ • Peer review will determine, by review of the chart notes, that the process of clinical ethics consultation engaged in by the Clinical Ethics Consultant meets the improved standard of the institution. 25 26 ___________________________________ Next steps ___________________________________ • Continue regular group meetings • Secure protected time, funding, and resources for ethics consultations • Complete development of HHC ethics consultation website • Finalize and standardize policy for ethics consultations and credentialing throughout HHC • Strengthen relationships with individual palliative care teams and HHC-wide initiative • Collect further data • Disseminate Model 26 30 ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ Presentation #3: Mayris Webber 1 ___________________________________ ___________________________________ Evaluation of the Clinical Ethics Credentialing Project (CECP) ___________________________________ ___________________________________ Mayris P. Webber CECP Epidemiologist/Evaluator Associate Professor Epidemiology & Population Health and Sharon Lawrence CECP Research Assistant ___________________________________ ___________________________________ ___________________________________ 1 2 ___________________________________ Logic Model for Program Evaluation INPUTS: ___________________________________ ___________________________________ What did we start with? ACTIVITIES: What did we do to effect a change? ___________________________________ OUTPUTS: ___________________________________ What were short-term outcomes? OUTCOMES: What were the long term outcomes? ___________________________________ INPUTS ACTIVITIES OR PROCESSES OUTPUTS OUTCOMES ___________________________________ 2 3 ___________________________________ Logic Model for Program Evaluation Inputs Activities Short-term Goals Long-term Goals Core Staff - Faculty w/ range of expertise including clinical ethics consultation (CEC), mentoring and evaluation Core Staff - Identify & recruit trainees - Stipulate training elements - Develop template for CEC: chart notes, QI, educational paragraphs - Set up trainee database and tracking system - Identify & recruit expert panel members Core Staff - Produce tool for credentialing to present to expert panel - Produce revised elements of training for privileging - Produce revised template for ethics consultations - Produce revised QI standards for chart notes - Convene expert panel Core Staff - Endorsement CEC standards by expert panel - Dissemination of project tools by presentations at meetings and publications Trainees - Attend monthly case reviews - Perform at least 3 consultations - Participate in hospital ethics committees - Complete baseline surveys Trainees - Complete all trainee program activities - Demonstrate competence via peer review of 3 consults and competence in reviewing consults of other trainees Institutions - Allow trainees time to attend sessions Institutions - Trainee hospitals take concrete steps to credential and privilege clinical ethicists Trainees - Motivation to learn or improve CEC skills - Demographic - Ethics training & experience - Professional discipline - Protected time Institutions - Willingness to support CEC - # Beds & patient mix - Ethics service - Experienced mentors ___________________________________ ___________________________________ ___________________________________ Trainees - Become highly skilled practicing clinical ethicists who elevate the field - Become mentors to others - Provide leadership in local & national professional organizations - Publish widely ___________________________________ ___________________________________ Institutions - Incorporate national standards for CEC in hospitals ___________________________________ 3 31 4 ___________________________________ Inputs ___________________________________ What did we start with? ___________________________________ ___________________________________ – Kinds of institutions represented? – Who were the trainees? – Range of clinical ethics experience? – What is the clinical ethics consultation (CEC) practice environment? ___________________________________ ___________________________________ ___________________________________ 4 5 ___________________________________ Inputs: Institutional Characteristics HHC Hospitals (N=10) All acute care/public facilities ___________________________________ Institution Characteristics ___________________________________ # of Beds 100 - 200 0 200-300 3 300-400 4 >400 3 400-500 1 500-700 1 800+ 1 ___________________________________ ___________________________________ ___________________________________ Type of Hospital Voluntary 0 Private 0 Public 10 ___________________________________ Type of Care Acute 10 Chronic 0 5 6 ___________________________________ Inputs: Institutional Characteristics Non-HHC Hospitals (N=17) ___________________________________ Institution Characteristics ___________________________________ # of Beds 100 - 200 2 200-300 1 300-400 2 >400 8 ___________________________________ 400-500 2 500-700 4 900- 1200 2 ___________________________________ Voluntary 7 ___________________________________ Private 8 Public 2 Type of Hospital ___________________________________ Type of Care Acute 8 Chronic 4 6 32 7 ___________________________________ Inputs: Who were the trainees? ___________________________________ ___________________________________ Description: HHC Non-HHC # of Trainees* 24 29 % Female 70 78 % Completed certificate program 85 78 ___________________________________ ___________________________________ ___________________________________ *The number of trainees refers to the people that submitted at least ___________________________________ one written assignment, whether a role play assignment or an actual note. 7 8 ___________________________________ Inputs: Who were the trainees? Highest Degree HHC N=20 Non HHC N=27 MD or Dental 35% 44% MSW / social work 20% 11% Chaplain Training 10% 0% Law 0% 4% Nursing 10% 19% Psychology 10% 4% MA/MS 10% 19% Other 5% 0% ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 8 9 ___________________________________ Inputs: What was the range of clinical ethics experience? ___________________________________ ___________________________________ Bioethics Work: HHC Non HHC Median # of yrs doing bioethics (range) 5.5 (1-35) 9 (1-25) Median hrs/mo doing bioethics (range) 4.5 (1-25) 7 (3-120) ___________________________________ ___________________________________ ___________________________________ ___________________________________ 9 33 10 ___________________________________ Inputs: CEC Practice environment Institutional support: HHC N=19 Non HHC N=26 Protected time/salary 11% 35% Institutional acknowledgment/recognition 68% 69% Conference attendance 53% 50% Other 5% 15% Journal club 5% 12% Topic presentations 58% 54% Grand rounds 47% 46% Inter-institutional Network 11% 42% Other 16% 27% ___________________________________ ___________________________________ ___________________________________ ___________________________________ Other incentives: ___________________________________ ___________________________________ 10 11 ___________________________________ Inputs: CEC Practice environment Question: HHC N=19 ___________________________________ Non HHC N=26 Respondents with an Ethics Committee 100% 96% Median longevity of committee (range) 15 yrs (5-26) 14.5 yrs (1-25) Voluntary appt to committee? 74% 77% Mandatory appt to committee? 11% 0% Both voluntary and mandatory appt? 0% 4% Regularly scheduled meetings? 58% 65% Ad hoc meetings? 26% 4% Both regularly scheduled and ad hoc meetings? 16% 15% Monthly meetings 26% 65% Quarterly meetings 26% 8% Yearly meetings 11% 4% ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 11 12 ___________________________________ Logic Model for Program Evaluation Inputs Activities Core Staff - Faculty w/ range of expertise including clinical ethics consultation (CEC), mentoring and evaluation Core Staff - Identify & recruit trainees - Stipulate training elements - Develop template for CEC: chart notes, QI, educational paragraphs - Set up trainee database and tracking system - Identify & recruit expert panel members Trainees - Motivation to learn or improve CEC skills - Demographic - Ethics training & experience - Professional discipline - Protected time Institutions - Willingness to support CEC - # Beds & patient mix - Ethics service - Experienced mentors ___________________________________ ___________________________________ ___________________________________ ___________________________________ Trainees - Attend monthly case reviews - Perform at least 3 consultations - Participate in hospital ethics committees - Complete baseline surveys ___________________________________ ___________________________________ Institutions - Allow trainees time to attend sessions 12 34 13 ___________________________________ Activities: Components of Training Program ___________________________________ Monthly 3 hour sessions (8 total) Early sessions focused on critique of faculty and trainee notes (QI tool) Back-to-basics “how to write a clinical ethics chart note” Led to in-class role plays & discussion Written assignments: up to 4 original notes and 3 role plays ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 13 14 ___________________________________ Logic Model for Program Evaluation Inputs Activities Core Staff - Faculty w/ range of expertise including clinical ethics consultation (CEC), mentoring and evaluation Core Staff - Identify & recruit trainees - Stipulate training elements - Develop template for CEC: chart notes, QI, educational paragraphs - Set up trainee database and tracking system - Identify & recruit expert panel members Core Staff - Produce tool for credentialing to present to expert panel - Produce revised elements of training for privileging - Produce revised template for ethics consultations - Produce revised QI standards for chart notes - Convene expert panel Trainees - Attend monthly case reviews - Perform at least 3 consultations - Participate in hospital ethics committees - Complete baseline surveys Trainees - Complete all trainee program activities - Demonstrate competence via peer review of 3 consults and competence in reviewing consults of other trainees Institutions - Allow trainees time to attend sessions Institutions - Trainee hospitals take concrete steps to credential and privilege clinical ethicists Trainees - Motivation to learn or improve CEC skills - Demographic - Ethics training & experience - Professional discipline - Protected time Institutions - Willingness to support CEC - # Beds & patient mix - Ethics service - Experienced mentors ___________________________________ Short-term Goals ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 14 15 ___________________________________ Short-term Goals ___________________________________ Did training program activities result in measurable differences? ___________________________________ ___________________________________ # 1 Quality of the CEC notes overall and in specific sections (compare scores of initial to later chart notes using QI tool) # 2 Way that CEC is practiced in the institutions (compare before and after in end of yr survey) # 3 Trainees sense of competence (compare self-efficacy scores of first to last class) ___________________________________ ___________________________________ ___________________________________ 15 35 16 ___________________________________ QI Tool ___________________________________ Arose from earlier recommendation of reviewers for uniform structure of notes during previous QI of MMC notes ___________________________________ Created distinct sections to reflect core areas of quality consultation. ___________________________________ – Key metrics include: - inclusion of key players in consult process - face-to-face meeting with team and patient - chart note documents, educates, recommends Most heavily weighted sections (ethics) account for 1/3 of total score ___________________________________ ___________________________________ ___________________________________ 16 17 ___________________________________ QI Tool ___________________________________ 8 Sections A-H: ___________________________________ A. Participants (14 pts.) Who was involved in the consult: doc, family, patient? B. Ethically relevant medical and social history (10 pts). C. Consult implementation (10 pts.) Is it clear whether the focus of the consult was conflict mediation or clarification of ethical principles; were there joint meetings? ___________________________________ ___________________________________ ___________________________________ ___________________________________ 17 18 ___________________________________ QI Tool ___________________________________ D. Ethical Problem (10 pts.) Has the consultant correctly identified the key ethical issue(s)? E. Ethical Analysis (20 pts.) “meat” of the consult note; was relevant bioethical knowledge integrated into note and were educational goals met? 18 36 ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 19 ___________________________________ QI Tool ___________________________________ F. Process (14 pts.) Does the note give clear description of dynamic of discussion? G. Recommendations (10 pts.) Was consensus achieved and were recommendations clear? H. Style (10 pts.) Was appropriate language used throughout? ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 19 20 ___________________________________ QI Tool ___________________________________ The goal of this project is to influence the quality of the clinical consultation, but we can only assess the completeness and clarity of the chart note. The score should reflect how much relevant information is included in the clinical ethics note. The “yes/most” > 85% of the information in this section is in the note; < 85% - 25% “some/part”; <25% scored as “no/none”. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 20 21 ___________________________________ Quality of the Notes: Scoring with the QI Tool ___________________________________ Scoring system using points per section was our crude way of quantifying change over time in quality of notes Step 1: Notes were scored by evaluation team leader using the QI tool and assessments reviewed with site PIs. Step 2: Additional notes were independently scored by team members. Step 3: All notes for analyses were scored by one team member using final versions of QI tool and scoring system. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 21 37 22 ___________________________________ Goal 1: Mean QI Scores Over Time (N=85) ___________________________________ ___________________________________ 0.9 ___________________________________ 0.8 0.7 Score 0.6 0.5 HHC 0.4 nonHHC ___________________________________ 0.3 ___________________________________ 0.2 0.1 ___________________________________ 0 1st note 2nd note 3rd note 4th note 22 23 ___________________________________ Goal 1: Mean Ethical Analysis Scores Over Time ___________________________________ ___________________________________ 0.8 ___________________________________ 0.7 0.6 Score 0.5 ___________________________________ HHC 0.4 nonHHC 0.3 ___________________________________ 0.2 0.1 ___________________________________ 0 1st note 2nd note 3rd note 4th note 23 24 ___________________________________ Goal 1: Mean Recommendation Scores Over Time ___________________________________ ___________________________________ 1.2 ___________________________________ 1 Score 0.8 ___________________________________ HHC 0.6 nonHHC 0.4 ___________________________________ 0.2 ___________________________________ 0 1st note 2nd note 3rd note 4th note 24 38 25 ___________________________________ Goal 1: Mean Participant Scores Over Time ___________________________________ Score ___________________________________ 0.9 0.8 0.7 0.6 0.5 0.4 ___________________________________ ___________________________________ HHC nonHHC 0.3 0.2 0.1 0 ___________________________________ 1st note 2nd note 3rd note ___________________________________ 4th note 25 26 ___________________________________ Goal 1: Mean History Scores Over Time ___________________________________ ___________________________________ 1.05 ___________________________________ 1 Score 0.95 ___________________________________ HHC nonHHC 0.9 ___________________________________ 0.85 ___________________________________ 0.8 1st note 2nd note 3rd note 4th note 26 27 ___________________________________ Mean Difference between First and Last CEC by Section (N=33) QI Tool Mean change SD A. Participants +0.11 0.23 0.01 B. History +0.06 0.20 0.09 C. Implementation +0.01 0.20 0.78 D. Ethical problem +0.05 0.22 0.20 E. Ethical analysis +0.27 0.44 0.001 F. B/C process +0.08 0.31 0.15 G.Recommendation +0.12 0.25 0.01 H. Style +0.02 0.10 0.26 Overall score +0.11 0.16 0.0004 ___________________________________ ___________________________________ Pvalue ___________________________________ ___________________________________ ___________________________________ ___________________________________ 27 39 28 ___________________________________ Multivariate Models Predicting Positive Change in QI Score ___________________________________ Variables independently related to improvement in overall QI score: non-HHC affiliation, female, MD training. Years performing CEC, number of assignments submitted, attendance, and self-efficacy scores were not related to change in QI score. ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 28 29 ___________________________________ Goal 1: Mean Scores of Chart Notes ___________________________________ The previous analyses examined original notes by date of the consult and grouped them as note 1, 2, 3 or 4 per person, separately for HHC and nonHHC. All first notes were analyzed together but they may have reflected different calendar time periods. An alternate analysis was carried out1 using calendar time (month/quarter) and had similar results. 1 ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ Kate Ettinger, JD 29 30 ___________________________________ Analyses By Calendar Time Time Period Pre-9/07 9/01-1/08 1/08-4/08 4/08 – end Mean (sd) .58 (.13) .62 (.12) .78 (.13) .80 (.12) ___________________________________ ___________________________________ Number notes 21 15 17 28 ___________________________________ ___________________________________ ___________________________________ There is a statistically significant increase in mean scores over time P <.001 30 40 ___________________________________ 31 ___________________________________ Caveats ___________________________________ Only 58% (14/24) HHC trainees submitted >1 original note compared with 83% non-HHC (24/29; p=.05). ___________________________________ Those who did NOT submit any notes were: slightly more likely to be male and had lower first role play scores (75% vs. 81%; NS). ___________________________________ This means that our results may have been conservative because it is generally assumed to be easier to show improvement in persons who start with lower scores. ___________________________________ ___________________________________ ___________________________________ 31 32 ___________________________________ Goal 2: Change the way CEC is practiced ___________________________________ ___________________________________ Percent Do you track the # of bioethics consults? 100 90 80 70 60 50 40 30 20 10 0 ___________________________________ ___________________________________ ___________________________________ HHC Before HHC After nonHHC Before nonHHC After ___________________________________ P=.02 and P=.003 for HHC and non-HHC, respectively. P values assume intended change occurs. Bars represent responses of “often”. The red caps represent % who intend to start performing the action in question. ___________________________________ Goal 2: Change the way CEC is practiced ___________________________________ ___________________________________ Is there a handwritten chart note? Percent 33 32 100 90 80 70 60 50 40 30 20 10 0 ___________________________________ ___________________________________ HHC Before HHC After nonHHC Before ___________________________________ nonHHC After ___________________________________ P=NS for HHC and non-HHC. Bars represent responses of “often”. The red caps represent % who intend to start performing the action in question. 33 41 34 ___________________________________ Goal 2: Change the way CEC is practiced ___________________________________ ___________________________________ Percent Is there a typed chart note? 100 90 80 70 60 50 40 30 20 10 0 ___________________________________ ___________________________________ ___________________________________ HHC Before HHC After nonHHC Before nonHHC After ___________________________________ P=.02 and P=.01 for HHC and non-HHC, respectively. P values assume intended change occurs. Bars represent responses of “often”. The red caps represent % who intend to start performing the action in question. 35 34 ___________________________________ Goal 2: Change the way CEC is practiced ___________________________________ ___________________________________ Percent Is the note put in the medical chart? 100 90 80 70 60 50 40 30 20 10 0 ___________________________________ ___________________________________ HHC Before HHC After nonHHC Before ___________________________________ nonHHC After ___________________________________ P=NS for HHC and P=.04 for non-HHC, respectively. P values assume Intended change occurs. Bars represent responses of “often”. The red caps represent % who intend to start performing the action in question. 35 36 ___________________________________ Goal 2: Change the way CEC is practiced ___________________________________ ___________________________________ Percent Is the re any ov e rsight or pe e r re v ie w of chart note s? 100 90 80 70 60 50 40 30 20 10 0 ___________________________________ ___________________________________ HHC Before HHC After nonHHC Before ___________________________________ nonHHC After ___________________________________ P=.02 and P=.002 for HHC and non-HHC, respectively. P values assume intended change occurs. Bars represent responses of “often”. The red caps represent % who intend to start performing the action in question. 36 42 37 ___________________________________ Goal 3: Change trainees sense of competence or “Self-efficacy” ___________________________________ Self-efficacy is the belief, whether or not accurate, that one has the power to produce a desired effect. ___________________________________ We adapted widely validated self efficacy measure: - 10 questions assessed work in role as clinical ethics consultant: ___________________________________ “In my role as a clinical ethics consultant, I can solve most problems if I invest the necessary effort.” ___________________________________ – Choices were 1 = Not at all true; 2 = Hardly true; 3 = Moderately true; and 4 = Exactly true. ___________________________________ - Possible scores range 10-40. ___________________________________ – No change (mean 21.5 during first class to 21.8 at last class). Ref: Ralf Schwarzer & Matthias Jerusalem, 1993 37 38 ___________________________________ Conclusions ___________________________________ This training model probably is effective in: ___________________________________ – Improving quality and completeness of CEC notes. – Promoting change in CEC practices. – However, no evidence that self-efficacy improves within this time frame. – Do not know how long changes last and if intended changes in practice take place. ___________________________________ ___________________________________ ___________________________________ ___________________________________ 38 39 ___________________________________ Sustainability Challenges ___________________________________ Peer review and support on regular basis ___________________________________ Trainees stated that discussion of the note offered a window into the actual process of the consult Peer discussions were highly valued ___________________________________ ___________________________________ Institution – protected time /salary – Recognition? – JCAHO – billable service? ___________________________________ ___________________________________ 39 43 40 ___________________________________ Logic Model for Program Evaluation Inputs Activities Short-term Goals Long-term Goals Core Staff - Faculty w/ range of expertise including clinical ethics consultation (CEC), mentoring and evaluation Core Staff - Identify & recruit trainees - Stipulate training elements - Develop template for CEC: chart notes, QI, educational paragraphs - Set up trainee database and tracking system - Identify & recruit expert panel members Core Staff - Produce tool for credentialing to present to expert panel - Produce revised elements of training for privileging - Produce revised template for ethics consultations - Produce revised QI standards for chart notes - Convene expert panel Core Staff - Endorsement CEC standards by expert panel - Dissemination of project tools by presentations at meetings and publications Trainees - Attend monthly case reviews - Perform at least 3 consultations - Participate in hospital ethics committees - Complete baseline surveys Trainees - Complete all trainee program activities - Demonstrate competence via peer review of 3 consults and competence in reviewing consults of other trainees Institutions - Allow trainees time to attend sessions Institutions - Trainee hospitals take concrete steps to credential and privilege clinical ethicists Trainees - Motivation to learn or improve CEC skills - Demographic - Ethics training & experience - Professional discipline - Protected time Institutions - Willingness to support CEC - # Beds & patient mix - Ethics service - Experienced mentors ___________________________________ ___________________________________ ___________________________________ Trainees - Become highly skilled practicing clinical ethicists who elevate the field - Become mentors to others - Provide leadership in local & national professional organizations - Publish widely ___________________________________ ___________________________________ Institutions - Incorporate national standards for CEC in hospitals ___________________________________ 40 41 ___________________________________ Long term outcomes ___________________________________ Dissemination of project results through peer reviewed articles? Endorsement of standards and training program by expert panel? Incorporation by hospitals of CEC into routine credentialing and privileging apparatus? ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ 41 44 Section II Sample Original Chart Notes from CECP Participants 45 Sample Chart Note 1: Bioethics Note on Consult by XY Patient Name: MS MR#: 000000 Primary Diagnosis: Small Cell Adenocarcinoma with metastases to the liver and bones, including vertebrae, COPD, Hypertension, Schizophrenia. DOB: --/--/---Date of admission: 1/29/08 Date and time of Consult: 2/15/08 at 10am, Pt evaluated on 2/15/08 at 4pm. Unit: -Reason for Consult: Refusal of Palliative Radiation Therapy. Reviewed the chart, spoke with pt's social worker and met with the pt in his room on --. Consult called by Dr B of the Palliative Care Team. Medical Hx: This is a 65 yr old African American male who was admitted with a dx of COPD, Hypertension and Schizophrenia, who was subsequently diagnosed with having Non Small cell Adenocarcinoma with metastases to the Liver, Bone, including his vertebrae -T11, 12 and L1. He presented with back pain. Neurology found him to have lower extremity hypotonia, arefflexia and an absent rectal tone, all suggestive of cord compression. Radiologic studies have not found any extension of the mets into the spinal canal. He also carries a diagnosis of Schizophrenia and has had multiple psychiatric admissions for this. He is currently psychiatrically at his baseline which is pleasant and cooperative but with delusions about the Mafia being responsible for his pain and wanting money from him. He also believes that a 'Negro Doctor" would be able to cure him. He is on psychiatric medications. Social Hx: Living at X Adult Home for about 14 years and is liked there. He attends a Day Program at --. No known family. 1 sister died and the Adult Home staff has not been able to reach the other sister for about 6 months now. Pt says he would like to have contact with his sister but did not have her phone number but knew her address. Consultation: A brief psychiatric assessment was done initially. He was able to discuss his psychiatric condition but not in any great depth. He was delusional about the Mafia and about a Negro doctor curing him but he was able to agree it was unlikely a Negro doctor would cure cancer and he also agreed that the cancer was probably causing the pain and not the Mafia but he was convinced they wanted his money. He also endorsed auditory hallucinations telling him these things but he said he always heard these voices and they did not bother him. His medical condition was then discussed and he understood he had Cancer. This writer then explained what the reason for the radiation treatment was, that is to prevent the cancer compressing his spinal cord and possibly paralyzing him. He said he did not want to be paralyzed and wanted the treatment. It was explained to him that the treatment would not cure the cancer and he expressed understanding. He wanted to know if the cancer could be cured and his poor prognosis was discussed with him. He appeared sad but took it in stoically. Pastoral counseling was offered but he declined, saying he was not religious. He did say he would be happy if we could reach his sister. Ethical problem: Autonomy and the right to choose in a patient with a chronic psychiatric illness vs withholding palliative radiation treatment, possibly leading to further nerve damage: As it turns out, this patient agreed to the treatment and he appeared to understand the benefits 46 and limitations of this treatment. Based on this assessment, he did have decisional capacity despite his ongoing psychiatric symptoms. However, decisional capacity can only be issue and time specific and his decisional capacity has changed over the course of this admission and may change again. Recommendations: 1) Since he is now agreeing to the palliative radiation treatment, this can proceed, if indicated. 2) Social Worker to attempt to contact his sister to provide support to him. 3) Provide adequate pain relief. 47 Sample Chart Note 2: CONFIDENTIAL Ethics Committee Case Consultation November 2007 Attendance: Noted in CCP E. C. MR #000 I. Reason for Consultation: The meeting was held at the request of Mrs. C. regarding consideration of a feeding tube for her husband. The meeting was scheduled to accommodate the needs of one of the resident’s daughters who is having difficulty with a previous decision not to insert a feeding tube. However, this daughter stated she had an emergency and could not attend. Mrs. C. was the only family member present. None of their nine adult children attended. II. Clinical Background: The resident’s primary physician was not present at the meeting. The medical history was reviewed by the Medical Director. In summary, the resident is an 86 year-old man who has resided at this facility for the past two years. He was admitted following a hospitalization for a BKA secondary to DM. He has a history of dementia which has continued to advance over the years. He is now in the advanced stages of dementia and a swallowing evaluation determined that he retains food in is mouth and no longer remembers how to swallow. He continues to lose weight. III. Resident’s Wishes: The resident has been determined to lack the capacity to participate in decisions regarding his care and did not appoint a HCP. A previous ethics consult was held in February 2007 regarding artificial nutrition and hydration. At that meeting, Mrs. C. described conversations she had with her husband over the years regarding this topic and end-of-life considerations and how he did not want a feeding tube. It was determined that Mrs. C. had presented clear and convincing evidence of the resident’s wishes and a recommendation was made that his wishes be respected and a feeding tube not be considered. IV. Ethical Issues/Discussion: After an introduction of those present, the intent of the meeting was clarified: to determine the resident’s wishes regarding a feeding tube at this time. Mrs. C. has lost two of her brothers in the last three weeks and is grieving and very tearful. All present acknowledged this burden and offered condolences. The resident’s medical condition and prognosis were reviewed by the Medical Director. It is clear that his dementia has progressed and is irreversible. Mrs. C. stated that she understood these facts. She said that he is still able to recognize her and, although extremely weak, tries to call her by name. She said that when she asked him if he were hungry, he indicated that he was. She said that she wants what is best for her husband. The contents of the February ethics consultation were reviewed and Mrs. C. acknowledged the accuracy of 48 them. She said that she is concerned for the children, particularly for the one daughter who wants her father to have a feeding tube. She asked what could be done for her husband if he did not have a feeding tube. At the previous meeting she had indicated that he would accept IV nutrition and he is currently receiving IV therapy. A hospice evaluation has been initiated and the benefits of the hospice service were explained. The services of the facility’s palliative care nurse practitioner would also be available. The goal of all care will be the resident’s comfort. We asked if it would be helpful to schedule a meeting with the concerned daughter to explore her concerns and provide education regarding nutrition in light of end-stage dementia and ways in which comfort can be provided. She said that this would be of benefit. The social worker will arrange the meeting. V. Ethics Consultation Recommendations: The committee recommends that: (1) the previously documented wishes of the resident (February 2007 ethics consult) continue to be honored and a feeding tube not be considered; (2) Hospice services be arranged; (3) a meeting be scheduled with the resident’s concerned daughter and any other family members who might want to participate. Present: Mrs. C. Resident’s wife R. B. MD, Medical Director J. R, DON P. C., Nursing Care Coordinator A.T. Social Worker M. L. Dietician D. P. MD, Co-chair Ethics Committee C. F. RN, Co-chair, Ethics Committee D. B. NP, member, Ethics Committee 49 Sample Chart Note 3: Medical Ethics Consultation/Ethics Committee Meeting March 2008 NP MR #0000000 Room -Reason for Consult: Patient is a 30 Y/0 man with H/O Seizure Disorder non-compliant with medications who continues to operate a motor vehicle. Consult called by Neurology Attending. Chart was reviewed. The Medical Attending, Resident and Intern, were interviewed prior to interview with patient. The following history was obtained: This is a 30 Y/0 man with history of ethanol abuse, pancreatitis, and seizure disorder secondary to arteriovenous malformation of the brain. The patient presented to the ED with back and abdominal pain described as 10 out of 10 in scale and constant since 3/4/08. He stated the pain started in his back and radiated to his abdomen. Since he gave history of seizure disorder and told the medical staff that he stopped taking Dilantin 3 months ago because it made him dizzy, medical resident called a Neurology Consult who in turn called Ethics Consult. According to the patient his first seizure occurred in South America 3 years ago. He had a second seizure which occurred in New York City in September 2005. The patient presented to this hospital at that time and CT scan revealed left parietal lobe AVM. He was transferred to another hospital for neurosurgical evaluation, subsequently discharged and given telephone number to follow up at another Manhattan Hospital for more specialized treatment. Due to insurance issues he could not be seen at the Manhattan hospital, nor did he follow up with his PCP at the HIP center. However, he continued to take the Dilantin on and off until 3 months ago when he decided to stop it because it made him dizzy. The patient claims to not have had any more seizures after the one in September 2005. His seizures are described as loss of vision, blackout and falling to the ground. Both times associated with tongue biting. The patient has significant ethanol abuse and claims to drink primarily on weekends (about 1 pint of Vodka) and smokes heavily while drinking. He claims he used to drink daily before that. He works (in his own business) as a welder on construction sites and often times at heights. He is married, lives with his wife and 2 children. Physical Examination was unremarkable except for some mild abdominal pain on palpation. MMSE score was 29/30. CT scan of the brain revealed a large left parietal AVM which was also confirmed by MRI. MRI revealed Left parietal AVM from the MCA territory draining into the superior saggittal sinus. Discussion : There seemed to be an element of refusal of treatment in this case which can directly adversely affect the health and well-being of the public. For these reasons we discussed that the patient might not understand the nature of the treatment that is being proposed and it’s potential risks and benefits, or may have certain fears relating to the treatment that can be addressed, or may have a treatable depression. Therefore, special attention should be given to the adequacy of the information given and the quality of the explanation, possible language or cultural barriers to understanding, and the patient’s capacity and of the consequences of the foregoing treatment 50 The importance of medication compliance was discussed with this patient. (due to dizziness from Dilantin he was prescribed Keppra for seizures). We discussed his alcohol abuse, and the fact that he is employed as a Welder ( often welding at heights at construction sites) is extremely dangerous in light of his seizure disorder. We also discussed New York driver licensing laws and that the New York State licensing regulations require that a person with epilepsy not have experienced a loss of consciousness within the previous 12 month period. We explained to him that a person who has experienced a loss of consciousness during this period may be licensed at the discretion of the Motor Vehicles Commissioner if 1) it was due solely to a physician-directed change in the medication and the physician submits a statement to that effect or 2) the person submits a physician’s statement confirming his/her knowledge of all such incidents and recommending licensing despite the medical history because in his/her opinion the condition will not interfere with the safe operation of a vehicle[D.M.V. Reg. 9.3]. We discussed how dangerous this could be and also mentioned his children and his driving them around. We explained to him that there is no statutory provision requiring physicians to report patients who have been treated for or diagnosed with epilepsy however the physician can report can report at any time a condition that can affect the driving skills of a patient, the DMV can suspend the driver license. We also asked if there were other means of transportation, including his wife and /or public transportation. We stressed follow up with his PCP at the HIP center to obtain referral to a Neurosurgeon for further work up and treatment. A follow up appointment was made for him to be seen in the Neurology out-patient clinic 2 weeks after discharge. He agreed we could call his wife and also tell her all we discussed. The wife was contacted and informed of the above. After Ethics Committee meeting of March 13, 2008 (see attendance sheet for list of attendees) it was determined that if the patient did not keep the Neurology Clinic appointment nor does he follow-up with the HIP center we will try to contact him either at his home or through his wife and we will file a Physician’s Request for Driver Review (form DS-6) from the DMV. 51 Section III Redacted Chart Notes from Montefiore Medical Center 52 Chart Note 1: Telephone Consultation 2007 Physician: Dr. X [telephone call to discuss troubling situation] Beeper: 914-000-0000 Pt: AB MR# 000000 Issue: Refusal of feeding tube by the wife of the patient Summary of medical situation: AB is a patient in his early 70s who suffered a stroke in the early 1990s. Since that time he has had some residual deficits including some stiffness and difficulty in ambulation for which he has used a cane and some decreased renal function. However he has lived at home and been ambulatory and generally pleasant during his doctor visits. Dr. X has cared for him for approximately a year and a half. About 4 months ago he was admitted to XX Nursing Home with a marked personality disorder and a refusal to eat and drink. In the last three months there have been three admissions to Hospital W. Each was prompted by his refusal to eat, drink and to take his medicines. At each admission liaison psychiatry stated that the cause of the event was a toxic-metabolic trigger, which, on each admission, was never found. The patient was metabolically chaotic at each admission, was given a full medical and neurological work up, and, when no identified cause was found, was returned to the nursing home where the pattern was repeated. On his prior admission Dr. X stated that it was essential that a feeding tube be provided for the patient before the he was returned to the nursing home. The wife agreed and then withdrew her agreement before discharge. The patient returned to Hospital W a month later. On this admission Dr. X’s partner stated to the wife that he would not care for the patient unless a feeding tube was placed, thus contradicting his partner. Social and family situation: This case is colored by the relationship of the patient to his wife. This is a middle class family, well educated and seemingly savvy to the economic consequences of medical decisions. The wife states that she cannot care for the patient at home with a feeding tube and she cannot pay for him in long-term care. For her the ping-pong to the hospital and then to post-hospital LT care seems economically the best solution. There appear to be assets; no specifics are known about origin or amount. Dr. X states that the wife has indicated that she has received legal counsel. There has been no consistent social worker involved in the case as each admission has been to a different floor. The wife states that she cannot support him in a nursing home and that she is afraid of loosing her house. This may, or may not be a realistic fear. My last encounter with Medicaid NH payment indicated that the home may receive a lien against future sales…this may be out-of-date information. There is no question, however, that assets in the name of the patient or a pension to his person, would both need to be spent down before Medicaid would assume the obligation of nursing home payment. 53 Ethical Analysis: This may be a patient who is being abandoned to the needs of a family member rather than having his medical and social needs addressed by the health care system. It cannot be in the patient’s long term health care interest to have a metabolism that is bounced by lack of food, fluid and medication every few months and must be dragged back to normal only to fall yet again. Unless this patient is a palliative care patient—likely a hard position to sustain as a few months ago he was ambulatory, “charming” and quite interactive--his present course may be counter to his long-term health interests. His best interest may not be served by permitting his wife—who appears to have conflicting interests—to remain as the unchallenged decision-maker in this case. As far as Dr. X knows his wife is not the patient’s legal health care proxy. We are turning to her for her permission to place a feeding tube as that is, by convention, how decisions are made for patients who cannot make decisions for themselves. But, this decision seems counter to the best interest of the patient and cannot be made, unchallenged, by the wife, who is so clearly motivated by her own notions of self-interest. Even if she were the legal health care proxy her decision, that appears, at least at this distance and with this information, so at odds with the interests of her husband would need, ethically, to be challenged by the system. This is also a very difficult case to manage as the wife will not answer telephone calls and will not arrange for meetings at the hospital. There are also some adult children who have not been willing to be involved. Recommendation: I stated to Dr. X yesterday that this case was not yet ripe for an ethics consultation but that after all of the tests were run, yet again, and the patient was metabolically stable, we should convene the wife, adult children and the patient, if able, for a mediation. I now think, upon reflection, that this is not correct—or not entirely so. This is a mixed model case, both an ethics mediation, but more importantly, a complex case/hospital policy matter. This is a matter of “false choices” for a family member. It is not possible to care for this patient without a feeding tube then, the argument is, that it must be placed and, I would argue, should be placed, as soon as possible, if it is medically indicated. The wife should be “told” not asked about placement of a feeding tube. This in itself is not only a bioethics decision but a hospital policy decision. I think that this case requires a rather immediate intervention of Bioethics, through the intervention of an Ad Hoc Bioethics Committee meeting, followed by a report of the committee to the OMD in order to identify and address the best interests of this patient. This has been discussed with the patient’s physician who agreed and who requested that this consultation note be written and placed in the chart of the patient. Clinical Ethics Consultant 54 Chart Note 2: Patient: MR#: Date: Time: Place: Present: CD [referred to as “Robert” in note] 00000000 2007 1pm Small room off of the MICU Patient’s mother, his uncle, three nieces, his sister, Dr. X, MICU attending E, nurse for the patient, SW, Palliative Care, Clinical EthicsConsultant, Bioethics Ethically Relevant medical history: This is a 54 year old patient who was admitted from home on …07 for shortness of breath, uncontrolled diabetes and renal failure. He experienced a cardiac arrest in the ED and in the over 20 minutes before he was resuscitated he suffered irreversible anoxic brain damage. He was transferred to the MICU because of “uncertain” prognosis. His family had requested that his ventilator be turned off and as a result of that request a bioethics consultation was called. Subsequent to a discussion with the staff a meeting was held with the family. Discussion with the family: The bioethics consultant began the meeting by asking each of the family and the staff to introduce him or herself. After those introductions she asked CD’s Mom, “Tell me about Robert.” “”Ah”, she said, “he was a bad boy”. She related how, after Robert had been diagnosed with diabetes about 10 years ago, he finished the initial course of treatment and then never returned to the doctor again for additional prescriptions. Shortly after that diagnosis he returned to live with his mother. He had been a bus dispatcher for the transit authority but about 6 years ago his one good eye began to go blind—likely a combination of cataracts and whatever vascular changes accompanied his untreated diabetes. He did go to the ophthalmologist but when surgery for the eye was suggested he rejected it and became blind. He lost his job and gradually, according to his Mom, descended into isolation and depression. Old friends called him and he never returned the calls. When he finally could not breath, before his admission, his Mom begged him to let her call an ambulance—he refused. Only on his collapse did she call 911. The patient’s three nieces related that the patient was a father figure to them. Their parents had divorced when they were little and their uncle CD took them to their proms and to those special times that called for a father. They wept and said that, despite their great sadness, they were ready for him to die. All of the family agreed that CD would never want to live like this. I asked the family if there had been other members of their family who had ever been in intensive care on life-supports. They answered, no. They were very clear that Robert had always rejected medical care, had refused medical interventions and would be horrified by his present state. He would not want this they all agreed. 55 The night before this consultation the family members had met with their parish priest and discussed this decision with him. The priest had been clear that if this was extraordinary care, that is if it were overly burdensome, that it would not be morally required by the church. He made the distinction for the family between ordinary and extraordinary care. The first is morally mandatory and the second is not. The family recalled that when the Terrie Schiavo case was in the news, the patient commented that removing her feeding tube was not permitted by the church, and he did not approve, while turning off any of her machines, if there had been any, would have been fine. The family discussed with the priest that the choice was having Robert die now or letting him go back and forth to a nursing home until he got an infection that finally ended his life. They do not want that for him and they stated that he would not want that for himself. The bioethics consultant explained that this was a difficult decision that would have to be reviewed by different members of the administration of the hospital. They family stated that they were surprised as they had expected to have the ventilator removed this afternoon. When it was clear that that would not be possible, they asked that the decision be made a soon as possible. Dr. X explained that even after the ventilator was removed it might be many days before the patient died, as there was still some ability of his body to breath without mechanical support. The SW addressed the regrets of the Mom that she had not been stronger and stated that in the face of this clear opposition of the patient to any sort of medical intervention, they had all done their best. The SW explained that the patient would be moved to a palliative care bed and that hospice would be contacted to provide extra support for the family. Ethical Analysis: This is a patient with no possible prognosis for any meaningful recovery. The anoxic damage to his brain makes any recovery impossible. He was a person who never accepted medical care and the notion that this would be forced on him now is ethically obnoxious to his family on his behalf. His refusal of care has been consistent over the years of his illness and over the years of his growing disability. This is a patient who has given every indication that he would not ever accept any intervention, including the ambulance when he was having trouble breathing, that involved him in medical care. He has clearly rejected all medical interventions at each stage of his illness. This last rejection, of life-sustaining technology, is merely the extension of his clear pattern of decisions when he was decisionally capable. Patients are asked to undergo burdensome interventions when there is any likelihood of recovery. Most patients, not all, agree to these interventions in pursuit of greater health and longer life. However, this patient has an invariable pattern of refusing all medical interventions, no matter how insignificant their burden. His refusal of care, when he was capable, was absolute. He sought no care and accepted no care. His state of refusal was consistent and without variance. Those were in situations where benefit was likely. Here any meaningful benefit is impossible as the anoxic damage is severe and irreversible. Any intervention at this point would merely extend the process of recurrent illness, recurrent hospitalizations, and eventual death. Recommendation: 56 This is a loving family that is in total agreement. The medical team agreed also that there is no further care that can restore him to a prior level of health and functioning. The clear wishes of this patient, when he was capable, was to avoid and abstain from any intertwining with the health care system. These clear wishes should be followed now that he is incapacitated. The family has asked be told when the ventilator will be removed. They indicated that they wanted to be there when this was done and that if he lingered, that they wanted to be called before he died. xxx Bioethics x-0000 57 Chart Note 3: Bioethics Consultation Patient: EF, MR#: xxxxx Date: 2008 Time: 1 pm Place SICU This consultation was requested by Dr. XX attending Critical Care physician in the SICU, at the request of the patient’s daughter, Ms. F. The Clinical Ethics Consultant, Dr. XX and Dr. YY, the patient’s surgeon and the patient’s daughter all met to discuss the case. There is an estranged son of the patient who has chosen not to be involved in her care. Relevant medical and social history: A visit to the bed of the patient revealed a patient, without capacity, tied to many tubes, obtunded and ventilator dependent. In response to the question--“Tell me about Mama”--the patient daughter recounted a woman, now 81, who had been vibrant, in charge, committed to helping others, stubborn, independent and outgoing. She had survived the death of her husband, and the virtual disappearance of her son, and gone on with charm and courage. She had entered the S Home some years ago and lived independently there. She was committed to helping others and ran the volunteer coffee and book program for many of the residents. She was involved in the community, sold coffee in the coffee shop for the residents, read voraciously and corresponded with her favorite authors. It is difficult to imagine that the silent woman in the bed, whose hands are swollen and blue, could be the woman described. Most importantly, for this discussion, she had made her wishes clear when her husband died that she wanted “no extreme measures” when she reached the end of her life. She also commented to her daughter, in response to the question—“If you can’t talk to me should I just manage your pain?—“Yes”. Even in the context of past prior expressed wishes and preferences for care, prognosis matters. As Dr. XX explained, gently when the patient’s daughter was there and bluntly when she had stepped away for a moment, this patient is in the process of dying. She is in multi-system failure and will not recover. She has had a promising and then difficult course. She came in, with back pain and a very high blood pressure, and was diagnosed with a thrombosed abdominal aneurism. However while awaiting surgery she appears to have tried to get out of bed to reach the bathroom and fell. This led to Dr. YY performing an extra-anatomical by pass graft to reestablish circulation to the lower extremities. This was successful but was followed by escalating renal insufficiency, a cardiac arrest, cardiogenic shock and liver failure. As described by Dr. XX, this patient is actively dying. Process of consultation and ethical issues: 58 This consultation was largely a discussion among the daughter of the patient and the physicians about the future care of the patient. There were two options: continued aggressive management of the patient’s many and increasing medical problems or acceptance of the sad fact of her decline and subsequent management to ensure her comfort and not prolong the process of dying. The choice between these two options involves not only medical expertise but also the values of the care providers and of the patient—as expressed by her daughter. Patients, family members and physicians come to individual cases with previously developed values and commitments. In this case the options were couched as a choice between “doing everything for a long as possible” and recognizing the overwhelming decline in the patient’s biologic capacity and need of the daughter to recognize and respect what she understands to be her mother’s clearly expressed prior wishes for “no extreme measures”. Often times the distance between positions can be narrowed by discussion over time and by the implementation of incremental measures and plans that will, gradually, demonstrate the wisdom of one course over another. This is made difficult by the existence of rather absolute values regarding the existence of options. If the only acceptable option is to continue aggressive care then, when disagreement exists about prognosis and prior expressed values, the only possible outcome is an “agreement to disagree”. This was the outcome of this discussion. It was agreed that it would be unfair to insist that the wishes of the patient be ignored because of conflicting values of a care provider; but those very strong values physician values would not be changed by the discussion. Ethical Analysis: This is a very difficult case because of the status of the patient, her precipitous decline in the face of successful surgery, her clear wishes expressed to her daughter and conflicting very strongly held value commitments of the care providers. In the development of modern medical ethics these clashes of values were explored and scholarly commentaries created that acknowledge the overwhelming scientific expertise of the physicians and yet credit the value preferences of patients, as expressed by them or by family members on their behalf. If a clash should occur, especially in the light of a dismal prognosis, then it is the values of the patient that determine the care plan. This conclusion, of scholars and the courts, recognizes that the skills of medicine provide an offer of help that can be accepted or declined by the patient based on religious commitments, idiosyncratic personal history [here the fact of watching the death of her husband] personality and a notion of individual good. This tip to patient values, a trump card, in no way diminishes the skill and expertise of the physician but recognizes that the patient is the expert on his or her life narrative, its course and conclusions. In this particular case the daughter of the patient was fulsome in her praise for the care her Mom had received and especially for the surgery. She stated that if her Mom’s case was different she would be “throwing rose petals” at the surgeon and gladly accepting all of his advice for care. But in the face of decline she felt that she most honor her Mom’s wishes for how she would want to die. 59 It is argued by many that once the patient is no longer able to recover that the distress of the family is one, if not the prime, focus of care providers. This daughter feels acutely her obligation to follow her Mom’s prior wishes about her care when she is dying. To prevent the daughter from acting as she feels is her obligation is to burden her with a feeling of her failure to act with fealty and loyalty to her Mom who she clearly loves and admires. Recommendations: A patient who has expressed wishes in regard to end-of-life care has the right to have those wishes respected. The process of respect does not nullify the obligation of the physicians to act in the best interest of the patient if “best interest” and prior expressed wishes conflict. However, in the case of a patient who is actively dying, the obligation to intervene weights less heavily than the obligation to respect patient values. Dr. YY agreed to speak with Drs. S and B who have known this patient for many years. If they are comfortable with the discussion, Dr. XX will recognize that this patient is in the process of dying and will not take actions to extend the process. Bioethics Consultant X-0000 60 Chart Note 4: Clinical Ethics Consultation Patient: GH MR# 000000 Location of consultation: Hospital 6B. The patient was interviewed in his hospital room. Discussion followed in the nurses work room on the unit. Participants: AB, MD internist and attending of record, CD, MD consult liaison psychiatry attending, EF, MD psychiatry resident, GH, Ethics, IJ, Ethics, KL MD Ethics. Presenting Problem: A clinical ethics consultation was requested because the patient, who does not have the capacity to do so, is refusing recommended medical care. Relevant Medical History: Mr. GH is a 57 year old man, who lives in XX Care Center nursing home. He has lived there for about 5 years. He has a history of psychiatric illness, homelessness, and substance abuse. Additional medical history includes diabetes and hypertension. Prior to living in the nursing home, he did not seek regular medical care. In the nursing home, his diabetes in managed with insulin, but poorly controlled. He is treated with antipsychotic medications in doses used for the treatment of schizophrenia. Mr. GH was admitted to the hospital in March. In the nursing home he was described as being found pulseless, received CPR, and was revived. Throughout the hospitalization, he has been clinically stable, without evidence of heart attack. He has intermittently refused blood draws. As part of the work up for a possible syncopal spell or cardiac arrest, a chest CT with contrast was done to rule out pulmonary embolus. There was no PE, but a spiculated lung nodule was found, highly suspicious for lung cancer. To further evaluate his cardiac status, the cardiology team has recommended cardiac catheterization. To further evaluate the lung nodule, the pulmonary team has recommended a bronchoscopy and biopsy of the nodule. Mr. GH has refused both tests. Psychosocial history: Mr. GH states he has parents in the South as well as a brother and sister there. He has provided no contact information. The nursing home records have no contact information for friends or family. Process: We first interviewed Mr. GH in his hospital room. He knows that he is in the hospital because he passed out and that there might have been something wrong with his heart or lungs. He remembered having the CT scan and did remember that it had showed something that might be cancer in the lung. He knew that more tests would be needed. He does not wholly believe that there is a tumor in the lung, stating a few times “I never had that before.” I told him again about the bronchoscopy that would be necessary to definitively diagnose cancer and he said a few times, “I don’t want that.” When asked why, he said, “I never had that before.” He seemed upset by giving a piece of his body in the form of a biopsy. He said “there must be a better way to do that.” When asked if he would want to know if he had cancer, he did not answer directly or definitively. I asked if his brother and sister were people he would confide in about this kind of medical problem. He said yes, and that they would tell him to have the tests, but that he didn’t want to. He stated his plan is to go home to the nursing home and come back to the hospital if he 61 gets sick. He declined an offer to view the CT scan to see the tumor. I explained that the bronchoscopy was needed to try to see if he had cancer, and that if he had cancer, it could kill him, and that his doctors wanted to prevent that. He does not believe that he could have cancer or die from it. When asked what he is giving up by not having the recommended tests, he said he was not giving up anything. He does not understand that at the point he develops symptoms it could be too late to cure. When offered the option of trying the test, but stopping if he didn’t like it, he said no, he didn’t want to start. Ethical Analysis: Mr. GH is a man who does not understand the nature of the medical problem he is facing. He does not understand the risks and benefits of the plan for work up his doctors have recommended. He does not have the capacity to provide informed refusal. He has nobody that can act on his behalf as a surrogate decision maker. His prior pattern is to avoid medical care. He has a hernia causing an enlarged scrotum that he has never allowed to be fixed. Here he has consistently stated that he does not want to go invasive procedures, but tolerated a noninvasive test. This consistency over time in his refusal of medical care could be viewed as adding up to a statement of who he is. Honoring these consistently stated preferences may be in the patient’s best interest. However, he does not understand that his life could be saved by proceeding now. He should not be allowed to choose a potentially harmful plan of care if he does not understand the harm. He has told the care team that he likes his life in the nursing home and he has given no indication he is ready to die. Additionally, Mr. GH did not indicate that he would not want to know if he had cancer. He did leave also a door open when he said, ”there must be a better way to do that,” which I took to mean that he might be willing to undergo further noninvasive tests that did not involve taking tissue. Options: The team considered the following options: 1. Proceeding with bronchoscopy with administrative consent. However, the patient would need to provide assent to even begin the procedure or be sedated at the very outset. Advantages – a definitive diagnosis could be made according to the recommended care plan, which may allow a definitive treatment, ie. surgery to be done. Disadvantages – going against the patient’s stated wishes, uncertain that Mr. GH would go along with follow up care (blood draws, etc.) which might be required to minimize the risks of bronchoscopy/surgery. Even more invasive procedures would be required to fully realize advantages. 2. Discharge the patient to the nursing home without further workup and revisit when/if Mr. GH agrees to invasive tests or develops symptoms. Advantages: honoring Mr. GH’s stated wishes. Disadvantages: missed opportunity to provide for Mr. GH care that optimizes his chance of healthy survival. Because it has been difficult to contact the MD at the nursing home, continuity of care is not ensured. A plan for treatment/palliation of symptoms when they arise would need to be in place. 3. Pursue further noninvasive tests if would add additional information, such as a PET scan to evaluate for metastatic disease and a stress test to evaluate for high risk coronary artery disease. The presence of either might alter the plan of care. Advantages: Because Mr. GH has a history of getting used to things and allowing them more over time (insulin, medication), this plan may get more information for him and give some time for him to understand he may have cancer and assent to the work up. Medical conditions (mets, severe CAD) that would decrease his chance of having a favorable outcome with surgery 62 or chemo could be uncovered and added to the risk/benefit analysis. There in not a small possibility that Mr. GH could have a cancer that is curable by surgery and that he could medically tolerate that surgery well. Disadvantages: continued hospitalization. Mr. GH prefers to go home. Recommendations: The team recommends option 3. as an interim plan. More information is needed to comfortably pursue either 1. or 2. and further time and workup may provide it. Additionally, more information will be sought from the staff and administration at the XX Health Care Center nursing home. Pursuing this sort of interim plan requires that the care team and ethics team agree to reconvene when more information is available to reweigh the risks and benefits of further invasive procedures for Mr. GH A follow up meeting will take place. YY Ethics 63 Section IV CECP Background Documents 64 Document A: A Model for An Institutional Clinical Ethics Consultation Service: I. Introduction: Clinical Ethics Consultation [CEC] has developed over the last three decades in many different forms in various hospitals and medical centers. The structure and process of individual institutional services vary by setting, by the skill, training and experience of the ethics consultant and by the support, or lack thereof, from the sponsoring institution. Scholars have offered taxonomies of the components of the process; consultants have described patient and family interactions; experts have analyzed the principles supporting the outcomes. As is often the case with a new area of intellectual and clinical endeavor there is no general agreement on how services should be structured, offered to patients, providers and family members, supervised, evaluated and supported. The Joint Commission on the Accreditation of Hospital Organizations [JCAHO] has been instrumental in placing ethics on the agenda of hospitals and other health care institutions by requiring that they have the capacity to address ethical issues. However, by its silence on standards and quality, it has encouraged institutions to draft existing medical, administrative and nursing staff to engage in these efforts without adequate attention to compensation for time and effort and without sufficient concern about adequate preparedness. A clinical service with integrity demands and deserves clear standards for operation, policies that are integrated into institutional practice, compensation for practitioners and a commitment to quality. JCAHO requires none of these. Clinical Ethics Consultation many assume to be the intervention of a skilled professional to bring resolution to a classical ethics dilemma—the beneficent obligation of the physician to do good verses the desire of a patient to exercise his or her autonomy. However experience indicates that CEC can be required in broad categories of issues that fall well beyond the classical statement of the “bioethics dilemma”—a clash of relevant principles. The messiness of the reasons for requesting CEC reflect the fact that patients and families are generally unable to articulate discomfort in bioethical terms—although there is always some bioethical “hook” on which to hang the request for consultation--but will indicate the same by behaviors and disagreements that cause the displacement of care as the focus of the medical team. The realities can include, among others issues, conflict between and among care providers or providers, patient or family; questions about ethical interpretation or analysis; questions about institutional ethics policies; uncertainty about the ethically appropriate plans of care; or questions about whether the voice of the patient has been adequately sought or attended to in the process of choosing a direction for care. 65 A case raises issues that are appropriate for clinical ethics consultation when there are: a. the need for an explanation of principles and practices; b. a clash of values; c. the need to facilitate communication; d. conflicts about the allocation of decision-authority; or e. the shared desire for the management of conflict that can be addressed by mediation . The American Society of Bioethics and Humanities cites the following eight categories as topics for ethics consultation: • shared decision making with patients • ethical practices in end-of-life care • patient privacy and confidentiality • professionalism in patient care • ethical practices in resource allocation • ethical practices in business and management • ethical practices in the everyday workplace, and • ethical practices in research. The first four are considered to be clinical ethics issues and the last are mainly organizational ethics issues. Both sorts of issues are often triggered in CEC. The proliferation in clinical ethics consultation services, has been spurred by the demands of accreditation but supported, in addition, by the public and professional perceptions of increasing value conflicts in medicine. In a post-Schiavo universe, with continuing disagreement over contraception—let alone abortion-- the value divisions in American society are clear. Many of these opposing views collide in the medical setting, especially in end-of-life care discussions and decisions. This perceived need for ethics consultation presents opportunities and dangers. The opportunities are obvious. A skilled professional, trained in the language and substance of bioethics and the law with a broad based acquaintanceship with the literature and history of medicine, should bring additional breadth and resonance to conflicted discussions. And these are conflicted discussions and decisions—if all are in agreement and if no conflict exists no one calls for a CEC. The call for consultation means that there is a barrier to a consensus care plan. The call for bioethics consultation is a call for help in solving a problem If the person called to address the conflict is trained in mediation the stalled dynamics of planning may be set free from the structural constraints presented by the medical power structure and prior dysfunctional family patterns. If, however, the opportunity for CEC becomes the avenue for inadequately trained medical or other hospital staff imposing their own values on patients and families, under the guise of applying bioethical and legal principles, then what poses as the good of bioethics consultation may actually emerge as a process for subjugating individual and family interests and even violating individual rights. 66 One reason that CEC has not advanced further is that hospitals have not been convinced that this is a valuable service and one that should be supported financially. A two-pronged approach should be useful: first develop a service that is subject to evaluation and quality improvement and, second, make clear that hospitals need to credential and privilege those engaging in the service, thus making them accountable and responsible. Bioethics professionals should receive a high level of scrutiny regarding past education and experience and present ability. One way of accomplishing this goal, as no national accrediting body or standards for accreditation presently exist, is for hospitals to own the process, examine these individuals, make judgments about their credentials, gather references from their past, and think clearly about their authority and responsibility going forward as they are privileged to intervene and to document their intervention in the medical chart. This document suggests a set of standards for health care institutions for instituting, evaluating and normalizing a Clinical Ethics Consultation service. These standards and their accompanying explanations may not be entirely correct or sufficiently comprehensive. This suggested structure is meant to begin and not to end this discussion. MMC has experience with these components but other institutions may have different and equally relevant models to offer. Discussions of policy and practice unrelated to individual cases are part of what the profession of bioethics does as a matter of course in many forums. This document is related solely to the practice of Clinical Ethics Consultation (CEC) which is that prospective intervention, with staff, patient and family, that seeks to clarify the issues, identify the conflicting values and forge a shared solution that meets the professional commitments of the staff and the values, history, emotional needs of the patient and the family members given the present medical realities--and likely medical future--of the patient. II. Elements of a Clinical Ethics Consultation (CEC) Service: 1. Clear indications for a consultation: A request for CEC is a call for help. No one calls for a consultation when the care team, patient and family are all comfortable with the process of care, the decisions that have been made and course that is planned. But there are different sorts of dilemmas that either fit, or not, into the mode of CEC. Some interventions are best suited to questions about hospital policy and practice…the questions that can be addressed by multiple choice solutions; for example: Do you need two physicians to agree to a DNR Order for a patient without a surrogate? Is it possible to remove a patient from a ventilator without a Palliative Care Consultation? What is the process for a patient without capacity who is refusing a discharge plan? These sorts of questions constitute many of the basic interventions of CEC in that they offer clarification, usually only to care providers, in order to facilitate discussions with the patient and family. It is for this reasons that clinical ethics consultants must be totally familiar with the policies and procedures of the institution in which they work. 67 However, most clinical ethics questions cannot be solved by reference to hospital policy or to state law or regulation. Most are about misunderstandings, disagreements and disputes that address the care of a specific patient at a moment in time when diagnosis, prognosis and outcome are uncertain. [See How to conduct a Clinical Ethics Consultation and How to Write a Bioethics Chart Note for accompanying guides to this essay] Some cases are complicated, demand attention, take up care provider time and energy and are not really appropriate for CEC. It is important to identify these at the outset so that they don’t deflect energy from more appropriate cases for CEC. The trained bioethics consultant may be of some support in these discussions, as she understands the setting and the issues, but cannot really provide the services and expertise that these cases demand. We have labeled these: “Complex Cases”. These sorts of cases are uncomfortable for providers, patients and family because the services that are available and affordable don’t meet the needs of the patient or have been rejected by the patient and the family. These discussions, usually in the context of discharge planning, raise issues of provider and institutional responsibility, possible liability, assumption of financial burden and likely reimbursement. They rarely raise “ethical issues” but for the ever-present theme of the right of cognitively diminished elderly patients to assume risk. Complex cases also address patient and family behaviors that respond to the shifting notion of the patient as consumer. Consumers get to demand the services that they want; patients get to choose from among the range of medically acceptable options. The patient and the consumer are not ethically and practically fungible entities. Behaviors that are appropriate to the former are not always ethically acceptable for the latter. Some of the elements of these complex cases may raise ethical issues, but the forum is a broad spectrum administrative team that thinks about the funding and reimbursement of medical services and about how to set boundaries for behaviors that are disruptive and counter-productive in the institution. [See Complex Case Scenarios for descriptions of cases] 2. Regular process for convening care providers: Medical centers, and all health care institutions, are under increasing regulatory and financial stress. There is a press for sufficient time to accomplish all of the tasks that excellent patient care requires and, in addition, to reflect thoughtfully on the process. Providers are constrained by scarce resources, lack of adequate staff, diminished reimbursement, burgeoning regulation and emerging new federal and state measurements for quality. It is always difficult to convene another meeting in the middle of the day to discuss a difficult and contentious set of issues involving multiple providers, family members and the patient. 68 Yet an initial meeting among all of the care providers is a necessary first step in the consultation process [see Bioethics Mediation pages x-y]; this meeting permits all of the care providers to hear and challenge each other before presenting an agreed upon medical statement of diagnosis and prognosis, or emphasizing the lack of agreement, to the patient or family members. It may surface tensions among members of the care team, between the nursing staff and the physicians or between sub-specialty services. There are often hierarchical disagreements between senior and junior members of the staff that are hard to air in usual circumstances. All of these have some play in a meeting with a mediator set to highlight uncertainty but defuse tensions. Often this meeting is the first time that the various members of the team and the consultants have ever sat together to discuss this patient’s diagnosis and prognosis. It often leads the discussion of the “pieces of the elephant” to resolve into a discussion of the entire animal—in this case the patient. Disagreements among staff that are communicated to family members are a frequent reasons for conflict between family members and the care team. The family, unsure and anxious, searches for authority and thus conflicting voices undermine trust and engender worry and concern. The care team meeting is often useful in ferreting out these disagreements, resolving them, or providing the basis for explaining to the family that there is a range of agreement and some uncertainty regarding the diagnosis, prognosis and possibilities for treatment. One way to approach disagreement and uncertainty is to acknowledge both and explain the origins to the patient and the family. Family members rarely understand the nature of medical reasoning, the place of data and evidence and the combination of these into a medical “fact”. The term “fact” seems to non-medical patients and family members to have the ring of scientific objectivity. What most do not understand is that what is a medical fact and how it is interpreted is a matter of selection and interpretation. Indeed, a postmodern definition of a medical fact might label it as --“a contested notion, reflecting assumptions about who has the right and authority to define what counts as a fact.” For all of these reasons a meeting is absolutely essential to really understanding what is happening medically with the patient, which is a necessary precondition to discussing what is relevant ethically. 3. A typed note in the chart: A typed note in the chart is a method for communicating among the care providers for all aspects of the care of the patient. It is a legal record of what has occurred and the intellectual depository of discussion and deliberation about the options for care and the reasons that certain paths were chosen over others. As such the patient’s chart is never an appropriate occasion for invective and denunciation. The language must always be formal and respectful. Yet it is an appropriate location for a chart note that details events, discussions, options, ethical analysis and recommendations. 69 It is the process at MMC for copies of the chart note to sent, by e-mail, to all of the staff who participated in the consultation [please note that different institutions have interpretations of HIPAA that may or not permit this sort of communication] . This practice serves three purposes: first it alerts members of the staff to how their statements were heard and interpreted by the CEC; second, it helps to insure that the chart note is actually faithful to the statements and arguments that were made--one more step in the practice of transparency; and, third, it provides concrete reinforcement of the process and permits the participants in the conference to review how the issues discussed were relayed to the naïve chart reader, that is the newly arriving staff shift. There are some institutions that continue to maintain a policy that bars CEC notes from the patient’s chart. Most are relying on some risk-management decision that these notes are somehow more dangerous to the institution than other sorts of patient care notes. Certainly a clinical ethics chart note that is disrespectful, and waived the flags of misconduct could well be a concern to the institution. But an institution that has selected the bioethics consultant and is aware of her practice in regard to chart notes should be comfortable that the note will thoughtfully reflect the players, their interests, the bioethics analysis and the recommendation. None of this would be possible without a typed note in the chart. No sane person is going to struggle through multiple pages of hand written scribbles of intricate ethical analyses. Nor should they. It is expected that a note should be crafted, reviewed by the author and edited, checked for accuracy and readability before it is placed in the chart. 4. A standard form for writing the Clinical Ethics Consultation note in the chart: The chart note must tell the “story”, identify the characters, present the plot, identify the medical options and measure the ethical weight of each option, clarify the issues in the case, discuss and reference the ethical literature and make clear recommendations. The chart note is evidence of the transparent and collaborative nature of the ethics process. A chart note that is readable—which means typed--reflects the narratives of the parties presents a clear sense of process and offers a clear analysis ethical issues and a snap shot of the dynamic of the consultation. In addition it is the vehicle, always, for teaching. By discussing the concepts of bioethics that undergird consultation practice [See sample Chart Note Paragraphs] these chart notes, properly redacted, are the building blocks for a clinical ethics curriculum for departments and divisions within the health care institution. They are also available for administrative review, and review by the Bioethics Committee, the Quality Improvement process and as material for research. The CECP has developed a clear set of guidelines for “How to Write a Clinical Ethics Chart Note”. It closely tracks the Quality Improvement tool that was developed to 70 evaluate the consultations. The theory of the QI tool as an effective instrument for change was based on the experience at MMC in having chart notes evaluated and using the responses of expert reviewers to improve the service. This process can only work if the chart notes are sufficiently rich and robust in their presentation and analysis. 5. Conception of Bioethics as one voice in a complex institutional system— Collaborative Bioethics: Bioethics is one of the players in complex institutional systems that include others and especially the Office of the Medical Director [or the highest medical authority], the Office of Risk Management and the Office of Legal Counsel. Sometimes it even involves the CEO of the institution as issues of organizational ethics approach strategic planning and financial management decisions. All of these offices and the professionals that manage them have different, important and equally valid perspectives and none will dominate at all times. Because the Clinical Ethics Consultation voice comes with the title of “ethics” [morality, righteousness, virtue] does not mean that it will always prevail when possibly conflicting institutional interests are at stake. It is a very important voice but only one voice, Both American law and American bioethics are committed to foundation principles and both adhere to a similar mode of analysis. But the task of Legal Counsel, and of an Office of Risk Management, is to keep the organization safely within the law and to prevent later liability. The task of bioethics is to identify and pursue the interests and rights of patients and providers. These appear to be similar goals and largely they are. However, given the state of the law, and the litigious nature of American society, they may occasionally diverge. Many of the cases that arise in the context of CEC will involve behaviors and issues that may well raise legal and risk management concerns. The task of the Office of Legal counsel is to oversee the compliance of the health care institution with the legally applicable statutes, regulations and state and federal case law that apply to the institution. The relevant rules often comprise a difficult set of stipulated behaviorconstraining dictates that may seem arbitrary and even wrong to those whose focus is not on what rules exist but what rules should exist to further the interests of patients and providers. There is some basic tension between a rule based system, that of the law, and a normative system such as bioethics. The tension is not always visible and not always relevant but is always hovering over various discussions and interactions. An office of Risk Management has a different set of tasks. It must evaluate events in the institution and decide which ones generate concern about future liability. Those cases must be addressed differently from cases that do not generate liability. So, for example, a case in which the family is threatening to sue is in the bailiwick of risk management and is probably not a good case for CEC. Too many factors extraneous to the consultation are sure to affect the process and the result. 71 The only productive route for approaching the multiplicity of tasks and perspectives in any organization is to respect difference and create a respectful and transparent process. In the model envisioned in this document, a chart note that might raise issues for the Office of Legal counsel or the Office of Risk-management would be sent to them in order to alert them to what might be differences in perspective and tasks. Clinical Ethics Consultation facilitates a forum and a process for the clinical team, the various medical consultants, other experts in the institution and occasional outside consultants such as members of the child abuse team or a case worker from Adult Protective Services. The consultations serve as a central meeting ground for all of the voices that comprise the variously discordant or complimentary notes for the chorus of care. The bioethics team in its clinical ethics consultation work must also develop procedures that facilitate collaboration and leave room for disagreement. Appeal to a higher medical and corporate authority is always appropriate. The ethical issues are one but only one set of issues that a manager of a health care institution must accommodate. 6. A Robust Quality Improvement process: The issue of how to evaluate the effectiveness of CEC has long plagued the field. Many suggested that only a hands-on viewing could accomplish the goal of determining effectiveness and quality. However, it is difficult to actually view most consultations and, even if this were possible, to agree on outcome measures. At MMC we had, for many years, sent follow-up questions to the staff involved: Was the consultation effective? Did it help to resolve the dilemma? The response of the house staff was uniformly positive; 95% regularly stated that it was helpful in resolving the dilemma. However, these rather primitive reviews, indicating high marks for the CEC did not mean that it was a quality intervention, merely, we suspected, that it made the staff participants feel heard and supported. In 2004 the Division of Bioethics began typing its chart notes and placing these typed notes in the chart. It also shared the notes with the staff participants in the consultations and used the notes as the basis for referral to an administrative authority for resolution when the consultation failed to resolve fulminate conflict. The existence of this data base permitted us to examine the content of the ethics consultations in detail. In 2006 the Office of the Medical Director, at MMC was given 10 names, by the CEC team, of national experts who might be engaged as outside reviewers for the recently developed typed chart note system at the medical center. Two reviewers responded and contributed comments on approximately 100 chart notes that were generated in 2005. The reviewers were given the following questions to address in the course of their review: • Were appropriate people involved in consultation? 72 • • • • • • Do consultations reflect legal and ethical principles governing contemporary bioethics? Is the process of consultation clear? Does the process of consultation conform to Bioethics Mediation Model? Was there conflict? Was the conflict resolved? Was there a description of the consensus reached, or was the disagreement ongoing? Reviewers’ Responses indicated that: ”A strong feature is the clear distinction between legal and ethical principles”. ”Often disagreements are resolved by understanding the patient’s or family’s view and the reasons they do not agree with the healthcare team’s recommendations”. ”When consensus was reached, it was clearly described in the note, usually with practical suggestions for application”. ”When disagreements continued, the note generally clarified the nature of the disagreement and the positions of the parties”. The reviewers suggested as opportunities for improvement: • A more structured consultation note to ensure that all important information is included; Provide greater consistency in the reports; Consult reports should indicate the need for addressing recurring systems issues; • More attention to communication in bioethics disputes; • Use more open-ended questions; • Empathic comments; “I wish …” statements; For planned/ongoing actions they suggested: Development of the electronic medical record; Shared central drive files; Regular meetings with the Office of the Medical Director and the Clinical Ethics Consultation service. Question Addressed by Reviewer % of Cases “Yes” Were appropriate people involved in consultation? 73% Do consultations reflect legal and ethical principles governing contemporary bioethics? 88% Is the process of consultation clear? 78% Does the process of consultation conform to Bioethics Mediation Model? 70% 73 Was there conflict? 81% Was the conflict resolved? 50% Was there a description of the consensus reached, or was the disagreement ongoing? 80% Suggestions of one reviewer [excerpted] “As indicated, these notes demonstrate that the Bioethics Consultation Service provides very skilled consultations on cases that pose difficult ethical dilemmas. Generally the consultation helps resolve disputes. Nonetheless, there is always room for improvement, and in the spirit of quality improvement, I offer the following suggestions: 1. Consider a structured consultation note: The mediation process suggests a number of steps that are useful in carrying out bioethics consultations. A structured consultation note, like a clinical care pathway, helps to assure that the desired procedures are carried out in each case. The standardized physician’s admitting note, while restricting the collection of certain types of information, does assure that crucial information about current medication, allergies, etc are gathered in each case. Important information that was missing from some notes included: Who is present at the consultation? Summary of medical situation. Next steps. 2. Give additional attention to systems issues: Current thinking on quality improvement emphasizes that undesired outcomes in particular cases often result from systems problems rather than shortcomings of individuals involved in the case. Several cases identified systematic problems that need to be addressed in order to prevent similar problems in the future. 3. Give more attention to communication in bioethics disputes: Written notes can never capture the nuances and dynamics of the discussions with patients, proxies, and families. Nonetheless, some hints in the notes suggest that the consultation service may want to examine in more detail the specific phrases they use and consider alternatives that are suggested in the literature. Some consultations do not take advantage of opportunities to explore the emotions of the key stakeholders, particularly when the family disagrees with the health care team. To be sure, the Bioethics Consultation Service appropriately puts great importance on clarifying the ethical and legal issues. However, once the consultation moves into the subsequent phases of gathering information and problem solving, more emphasis on exploring emotions and building a relationship with the family may help In summary, the notes I reviewed demonstrate that the Bioethics Consultation Service carries out extremely high-quality consultations on complex, difficult cases. It provides a valuable and important service that is of great value to the physicians and nurses providing clinical care, to the 74 institution, and most of all to the patients and families who are facing such difficult situations.” All of the suggestions made by reviewers were implemented in the MMC process to very positive effect. This experience was key in convincing the institution that a robust QI process could be based on a review and analysis of chart notes. This experience was further strengthened by the experience of CECP [Clinical Ethics Credentialing Project is 2007-2008]. As the two study groups gained experience they were able to dissect the chart notes of participants and penetrate to the process and substance as the basis for critique and suggestions for change and improvement. 7. A Peer Review Process. A QI process is essential to CEC but, in addition, there should be a regular process for consultants to review each other’s cases. This is relatively easy to accomplish if there is a program such as the CECP or if there are more than one consultant at an institution. In the event that neither exists the Clinical Ethics Consultant to seek some peer review supervision structure similar to that created by therapists and various other counseling professionals. 8. Credentialing and Privileging. Quality improvement is mandatory in all of medicine. It is not optional in bioethics consultation. Modern American medicine no longer functions as totally independent sub-specialties. That system for providing care, a vestige of the independent agent idea of medical practice, has been modified by a combination of sub-specialty cooperation and by the patient safety movement. Bioethics consultation should not be exempt from these developments. As it moves into the main stream it must be judged by mainstream technologies. Bioethics consultation and bioethics consultants must be subjected to the same level of scrutiny, credentialing and privileging as other members of the medical staff who see patients, and write notes in the chart. It would be easier to take this next step were there clear standards for accrediting these intervenors but even without this platform the obligation of hospitals to ensure quality mandates that they accept responsibility for this function that affects the lives of patients and providers. In order to be credentialed as a clinical ethics consultant by a health care organization, an individual must satisfy a number of criteria. A. Participation in a formal training program. For credentialing, clinical ethics consultants should successfully complete a substantial, formal program in medical ethics. Any such program should emphasize the development of core competencies in the following areas. 75 Knowledge: Consultants should know (a) the central concepts, principles, and theories of bioethics, as well as (b) common bioethical issues and the dominant approaches in the field to them. Knowledge of (c) relevant health law and (d) of relevant codes of professional ethics is also required. Interpersonal Skills: Consultants should have proficiency in the techniques of dispute resolution and mediation in order to be able to resolve disagreements that arise in the clinical context. The training program should be rigorous and should teach both the background theory needed for clinical ethics consultation and the practical skills required for successful consultation work. Significant feedback from senior teachers and mentors should be part of the program. One model for such a training program is the Certificate Program in Bioethics and the Medical Humanities, run by the Division of Bioethics at Montefiore Medical Center, and staffed by experienced faculty from philosophy, law, history, and medicine. This is an eight month long program that meets weekly for three hours. There are two retreats, one at the start of the program, emphasizing different disciplinary perspectives from which to examine issues in health care, a second at the start of the second half of the course, emphasizing the practice of clinical ethics mediation. Students are expected to do a considerable amount of reading and to write three papers. The latter receive extensive comments from the faculty. Programs that meet the formal training requirement must be on an advanced level. They must be comparable to the Certificate Program in terms of rigor, scope of coverage, faculty-student interaction, and skill development. B. Completion of an Apprenticeship Clinical ethics consultants must complete a one-year apprenticeship, similar to a clinical fellowship for medical specialties like oncology and critical care. The apprenticeship should consist of the following elements: Participation as an observer in clinical ethics consultants performed by experienced consultants. Attendance at a monthly multi-disciplinary chart review meeting, to debrief past and ongoing cases that raise ethical issues. Successful completion and documentation of three consultations as lead consultant, under the supervision of experienced mentors. C. Verification of Qualifications Educational background, participation in a formal training program, and completion of an apprenticeship, must be verified by appropriate documentation. With respect to both the training program and the apprenticeship, the candidate’s teachers/mentors must provide written evaluations of his or her performance and fitness to do clinical ethic consultations. 76 Document B: The Context of Clinical Ethics Consultation How did Clinical Ethics Consultation evolve? Modern bioethics is a field that has developed out of the scholarship and practice of medicine and the allied medical professions, and the disciplines of philosophy, religion, the humanities and law. Increasingly it incorporates the skills of alternative dispute resolution. Its origins lie in the long-standing oaths and ethical commitments of medicine. Discussions about the ethics of medicine were focused by the confrontation with Nazi research abuses after World War II and by the subsequent exposure of research wrongs in the United States in the 1970s. Ethical dilemmas multiplied with confrontations with the development of new medical technologies, and new pharmaceutical interventions in the later half of the 20th Century. Before the 1950s--before antibiotics, modern surgery, anti-retroviral therapy and anti-psychotic drugs--there were few choices for patients to address in medical practice. Medicine could always comfort, sometimes diagnose but rarely cure. In the mid-20th Century all changed. There were choices to be made and the questions arose: who should make these choices, based on what principles, under what set of governing standards and with what notions of review? The answers to these questions, in the first phase of modern bioethics, focused on the doctorpatient relationship, the mechanisms for sharing information and process of informed consent. This was largely a scholarly discussion engaging all of the relevant voices whose discourse was reflected in professional journals, and legal opinions. Bioethics was then largely an academic discipline existing in scholarly university departments and bioethics centers with small inroads into the medical arena. Clinical ethics consultation has been developing as a separate field since the late 1970s despite its deeply embedded origins in medicine. With the Karen Ann Quinlan case in New Jersey in 1976, the American legal system entered the discussion and has, since then, been essential in setting standards and raising public awareness of new medical developments that produced qualitatively different confrontations between and among the governing principles of medical care. Modern bioethical scholarship has explored the evolution of technology, legal opinions on these developments and societal reactions to these abilities to extend organ function and enhance quantity, if not quality, of life. All of these developments raise new issues and these issues, interact with older obligations and prior commitments to require new analyses. Clinical ethics consultation occurs at the intersection of the abstract development of the issues and the concrete needs of one patient and family system in the context of the institution caring for the patient in the limitations of the American health care system. In 1986 JCAHO added a standard requiring hospitals and nursing homes to have the capacity to address bioethical issues. This demand has lead to the growth of Bioethics Committees and to the development of clinical ethics consultation capacity within those committees. Sometimes it has lead to the creation of Clinical Ethics Consultation services either within or outside of the 77 committees. This capacity for Clinical Ethics Consultation addresses retrospective analysis of cases or, increasingly, intervenes in cases as they develop in order to affect the outcome. Clinical Ethics Consultation also evolved in response to calls for help in resolving difficult conflicts between and among medical care providers, patients and family members. It is no secret in a post Terrie Schiavo universe that the United States is divided in regard to the assumptions about and the values that should animate medical care. Clinical ethics consultation helps to bridge these gaps. Are guidelines and standards needed to structure these services? Prospective Clinical Ethics Consultation is that arena of bioethics that most directly touches patients and families in the medical setting. By intervening in difficult and conflicted cases [take it as a given that no one calls for a clinical ethics consultation if the care is proceeding smoothly and family and care providers are all comfortable] the clinical ethicist engages in an intervention that may affect the course and conduct of care. As such it should be well-thought out and carefully structured to provide a framework of principles and practices that have been carefully developed and tested and, in addition, vetted and approved by the institution. There needs to be a clear notion of what this discipline is, how it is practiced, organized and supervised and how it functions within its particular institution. Why is this the case? Scholarly articles are important and frame the terms of discussion; they are not unimportant. But institutions that deliver health care and that use bioethics consultation as one of the clinical services have different and greater moral obligations than scholars. They must ensure that fairness, justice, respect for patients and families in their cultural setting and sensitivity to providers all animate their clinical services and especially their clinical ethics services. In order to provide a clear systems basis for clinical ethics practice the elements of that practice must be embedded in and approved by the highest medical and corporate leaders. These authorities must approve of the style of practice, the form of the chart note, the transparency of the system and agree how the practice will be evaluated and improved. Quality improvement and accountability are features of bioethics consultation as they are facets of any clinical medical specialty. How is Clinical Ethics Consultation both similar to and different from other expert medical consultation? Bioethics is not a stand-alone process within a health care institution. It must be integrated into the fabric of care delivery. Clinical Ethics Consultation is a clinical consultation service, as any other and yet qualitatively different. How it functions must be negotiated and determined in a set of conversations with administrators and clinical service chiefs. A bioethics consultation is like other medical consultations in that it is requested by a member of the care team to fill a void in expertise and experience that is not possessed, in general, by the 78 health care team. But it is also distinct from expert medical consultation and this difference must be noted at the core of the operation, respected and honored. General medical consultation calls on the expertise of the consultant, in neurology or gastroenterology, or infectious disease, for example, to offer focused advice in her area on a specific question of treatment for a particular patient. That advice needs to be weighed and evaluated by the attending physician in light of the overall condition of the patient and the concurrent and possibly conflicting advice of other consultants. It is the responsibility of the attending physician, and the responsible health care team to gather all of the advice and expert opinion and create a coherent health care plan that meets the medical complexity, hypothetical prognosis and immediate and possible future medical needs of the patient. It is common for the attending physician and the team to reject the advice of one or more consultants as a constituent part of the health care plan. Experts look at only one aspect of the patient and reflect only that venue. The team has the responsibility for the patient as a whole. Bioethics consultation has a different valence from other consultations in medicine. It is qualitatively different to write, “this is the problem with the kidneys/vascular structure” and, this is the “ethical problem/dilemma” and the “ethical solution”. The first reflects scientific judgment and expertise; the second implies moral superiority—a noteworthy and significant difference. This is why we would suggest that the chart note never state that this is the “ethical solution”. [see “How to Write a Bioethics Chart Note” section on Recommendations] However, even if the discussion has been dispassionate and analytical and the chart note is clear in its analysis of options, it is still a bioethics consultation. The common understandings of ethical include “principled, correct, moral, right, fair, decent, just and proper”. It is, therefore, greatly more difficult to reject the recommendation of the Clinical Ethics Consultation than it is to reject the organ specific advice of the renal specialist. This is one, but only one, of the reasons that clinical ethics consultation is different from other medical consultations. Another is that this sort of consultation takes into account materials, such as values and social history, that are more subject to interpretation and nuance than generally considered medical data, including medical tests and scans. This consultation process address values, personal history, religious commitments, and the basic constructs of power and authority that infuse medicine and medical institutions. Disparities of power, in and of themselves would demand a process for arriving at a recommendation that is collaborative, open, transparent and fair. Taken all together these differences require a process that contains all of the noted elements and one which, in addition, strives to redress power differentials. A Bioethics Chart Note carries more weight than other notes. It denotes not just expertise but approval and opprobrium. It is not just a suggestion; it is a suggestion that is infused with the cadence of right and wrong. As such it must be approached with the care and dignity that issues of propriety demand. The nature of the process of a bioethics intervention provides an additional reason for an open and collaborative process. America is a multi-religious, multi-cultural, multi-political society. It is also a society that clearly provides less adequate access to care to the poor, citizens of color 79 and undocumented persons and reflects differential levels of care and disparities of care with these populations. Unequal treatment of patients is a moral burden for the health care system to bear. Doubly important therefore that bioethics consultants, committed to fairness and justice, be aware of health care disparities and alert to patient and family with suspicions of the system or imbued with values and beliefs that may be opposed to or discordant with the dominant assumptions and practices of modern medicine. That is why collaboration, at the very least, and mediation, in areas of greatest conflict are critical to the clinical ethics consultation process. Collaboration and mediation are the major tools to prevent the values of the power elite, reflected in the assumptions and practice of much of modern medicine, from overwhelming the less articulate but often conflicting values and views of patients and family members. Medicine is a science and also an art. Part of the artistry of medicine is the willingness to conceive of the “goods” of medicine as offerings to those who can benefit rather than as platforms for the obligation of the patient to accept what is offered. It is a principled basis of ethical practice that “adult patients who have the capacity to make health care decision have the right to consent to or to refuse care.” But, in actual practice, the pressure to accept what medicine has to offer is often overwhelming. It is the task of the clinical ethics consultant to inquire into all of the crevices of communication, in light of the guidance provided by the patient and the family, and to help to fashion a solution that meets competing and conflicting perspectives. What is Clinical Ethics Consultation [CEC]? Clinical Ethics Consultation is an intervention by a person trained in the principles and practice of bioethics, learned about the history and literature of medicine, schooled in the practice of dispute resolution and the techniques of mediation that assists hospital/health care staff previously involved in an individual case in order to: Identify and distinguish the medical, social and ethical issues; Determine that there is a conflict of values or ethical principles; Establish who are the family and who are the medical stake-holders and their convergent and possibly competing interests; Explore conflict if it exists and attempt to disaggregate its component parts; Clarify ethical issues and indicate when the analysis is unclear or conflicted; Recognize related and relevant legal matters; Specify the best interest of the patient; Indicate how that best interest might be met; Initiate management, or resolution, of conflict and explore how the conflict might be contained in the future Suggest possible future action in this case and a plan for follow-up; Recommend possible consideration of institutional policy change. When is a clinical ethics consultation appropriate? Clinical ethics consultation is appropriate whenever a member of the medical staff, a patient or a family member have: 80 Questions about the values, ethical principles and law that might surround a case; Questions about whether the interests of the stakeholders have been adequately explored and supported [patient, family, staff]; Questions about the rights and interests of the patient and the family Questions about the legal duties and obligation of the care providers; Questions about the shifting diagnosis and prognosis and how they may affect care? What skills are needed for clinical ethics consultation? A clinical ethics consultant needs a deep and wide grounding in the field of bioethics and specific skills in dispute resolution and mediation. But clinical ethics consultation cannot proceed in an intellectual vacuum. It must have the resonance of prior and surrounding discussions to ensure that it can be located fairly and justly in the context of the individual case. The clinical ethics consultant must be aware of the history of discrimination against the mentally ill and the persons with disabilities in order to be alert to the possibility in an individual case. Knowledge of past situations, arguments and analysis provide the frame for understanding and intervening in the present. In addition, many requests for consultation are actually requests for help in resolving conflict. In order to resolve conflict the CEC needs some skills. The most basic skills that can be acquired involve skills of mediation. Other techniques of dispute resolution are also supportive of shared outcomes but mediation skills are the most immediately supportive of the needs of medical resolution. [Please see Competencies for Bioethics Consultation ASBH for a full discussion of the capacities of the CEC] What is General Bioethics Consultation? Bioethics consultation may not be related to a specific case and may be addressed to specific issues, principles and practices in bioethics. The advice and explanation should be informed by history, scholarship in medicine, law and bioethics, should be specific and accompanied, whenever possible, by suggestions for more detailed investigation. Bioethics consultation may also be directed to investigation and fact finding as a precursor to the development of new policy for the administration or institution. It may then be tasked with the construction of new policy that meets standards in the field and fits the administrative, structural and cultural needs of the institution. What skills are needed for general bioethics consultation? The same depth of knowledge is needed for bioethics consultation but, in addition, the consultant needs to be comfortable with techniques of research and writing. Bioethics consultation requires that the consultant be able to organize a comment or report that is current and reflects the latest in legal and ethical scholarship. 81 What is an appropriate trigger for ethics consultation? The request for general bioethics consultation or clinical ethics consultation may be triggered by: Uncertainty about moral or legal norms of care; Discomfort with the dynamic or developing outcome in a particular care; Awareness of incipient, actual or escalating conflict between and among care providers, patient and family members; Perception that a previously uninvolved professional might unlodge a conceptual or procedural roadblock in thinking about or acting in a particular case. An active CEC service should encourage a wide net for initial requests for consultation. It then has the option, after a brief investigation of: 1. answering a brief and focused question, 2. referring the case for greater exploration to an allied service such as legal affairs, risk-management or palliative care; 3. requesting more information to facilitate a CEC; 4. establishing who will be at a consultation of care providers and where it should take place; 5. establishing whether the patient, or what family members, will be available after the care provider meeting to meet with the staff. Does there always need to be a meeting for a CEC to occur? This is a contentious issue and is controlled more by the realities of care and practice than by the theoretical needs of the intervention. In theory a meeting is always essential. Actually two meetings are really essential. First is a meeting of care team. In the dynamic of meeting together care providers confront their own biases, conceptions and misconceptions, disagreements with other providers, recent changes in the status of the patient and different lenses of the various subspecialties that deal with a patient in the complex world of modern medicine. There is a clarifying and cleansing character to a meeting among all of the care providers who challenge each other to explain and justify their positions. This can be, and often is, a crucial moment in identifying and resolving conflict. A bioethics consultation with a trained facilitator may surface power differentials that have clouded the discussions. However, the “best is the enemy of the good” and it is sometimes not possible to convene a meeting. This is the reality. There is a dynamic of a meeting, however, that can never be replaced by a series of single conversations. How should an ethics consultation be triggered? There should be one telephone number or a beeper to which all staff members, physicians, nurses, social workers, medical students and house staff have access and which is the number to reach for consultation. This number should also be available to patients and family although at some institutions it is given out by “customer services” or another department that is responsible for responding [within federally specified guidelines] to patient and family complaints. 82 Who should be able to request a consultation? Bioethics consultation should be available to any member of the staff including physicians, nurses, social workers and medical students. Most requests for CEC come from house staff officers who are asked by their attending physicians to initiate the consultation. Whereas most requests for consultation must arise with the attending physician, CEC like palliative care and AIDS consultation must be available whether the attending physician agrees or not. However, some arise without attending physician involvement and these consultations take on a slightly different aura. If the attending physician was not involved in the request then the first call should be to this physician to alert her to the request. Principles of diplomacy should guide the consultant’s approach. The attending physician should be informed of the request for consultation and assured that the consultation request follows the policy of the institution to trigger a CEC in all cases that exhibit the characteristics of this case. Protecting the requestor then may assume somewhat of the aspect of protecting a whistle blower—it is a political task for the consultant. Here again professionals of good will and broad education can differ. As noted above, we argue that the gold standard, for bioethics consultations whose presenting issue includes conflict is below: [see Bioethics Mediation; a Guide to Shaping Shared Solutions by Nancy Neveloff Dubler and Carol B Liebman, United Hospital Fund, New York, New York, 2004]: Is all CEC dispute resolution? No, obviously not. The areas of expertise noted above are as much substantive as process skills—both matter. Requests for help in matters of bioethics never fit exactly with previous cases. But both the substance and the process must be mastered if the goal is to have an effective intervention. Knowing that patients, family members and physicians all have rights and interests constitutes the platform; knowing what those rights are frames the intellectual building; knowing how those rights have been developed and critiqued provides the specificity of design; and, being able to comprehend how those rights are affected by the particulars of the case at hand comprises the unique individual character of the entire structure. Then how to deal with the edifice in its setting requires different skills—a long but perhaps instructive metaphor. How could the consultant structure the Clinical Ethics Consultation? What follows are the stages of mediation from the Dubler and Liebman volume. These stages are an amalgam of bioethics consultation experience and mediation experience of the authors that incorporates the relevant literature. It is one model but one that has been tested and appears to be useful. The stages are: 1. Assessment and preparation: Assessing the situation Receiving the consultation request Evaluating the nature of the dispute 83 Gathering information about the medical facts Establishing the decision history of the case Meeting with the care team Meeting the patient and family Assessing the time constraints Identifying areas of uncertainty and gathering more pre-mediation information Preparing for the mediation identifying the decision maker(s) and determining whether the patient is decisionally capable Determining who should be at the table Determining what additional supports are necessary Discussing the decision-making process with a decisionally capable patient Identifying family members and friends who may seek to participate in decisions Arranging a location for the mediation 2. Beginning the mediation Introductions The mediators opening statement/the mediators role/the process/goals/disclosure/ground rules/confidentiality/ final points/questions 3. Eliciting the medical facts 4. Gathering information Inviting statements by participants Identifying issues, interests and feelings Educating the staff, patient and family about the relevant legal and ethical principles Developing a working hypothesis 5. Problem solving Managing discussion Developing options Shaping solutions Helping parties make choices 6. Resolution Mediator’s role when agreement is reached Mediator’s role when there is no agreement Mediator’s role when another session is required What constitutes a successful outcome in Bioethics mediation Closing the session Documenting the decision in the patient’s chart 7. Follow-up Ensuring that the agreed-upon resolution is implemented Following –up with family and staff to see whether support for the family is needed 84 Debriefing medical staff on medical, ethical and policy issues Highlighting the hospital policy issues Who pays for this elaborate process and how can it be accomplished without financial support? To be effective Clinical Ethics Consultation must be seen as an essential clinical service which like all others must be supported by the budget of the institution. But a number of elements are combining that are likely to determine, in the future, the this must be a compensated service. One of them is this project, the Clinical Ethics Credentialing Project, which will credential and privilege this activity in a series of medical centers. Another is the JCAHO insistence on credentialing and importance of this process in the accreditation of hospital organizations. Finally is the QI process that this project presents that is time consuming but ethically, practically and strategically critical in moving to the professionalization of the field and its inevitable compensation. Is it critical that there be a note in the chart? Here the answer is still somewhat controversial but clearly, yes. A bioethics consultation is a major intervention that will likely change the course of what happens. Bioethics consultations are hardly ever called for frivolous reasons. People request help because they need help, or think that they do. What happens in a CEC is a substantial event. It will affect how providers, family members and the patient think about and analyze what is happening, in the present, and how they contemplate what will ultimately happen, in the future. As such it is a part of the clinical narrative and must be reflected in the patient’s clinical chart. What can be done if the administration or the office of legal counsel objects to a written chart note? This matter needs to be confronted directly. One of the guidelines about written CEC chart notes is that they must declare from the outset and remain faithful to the notion that they are about the ethics of a situation. This is an ethical analysis not in any way a legal opinion. An ethical analysis presents the principles on which it is based, describes the dynamics, provides alternative analyses and uses the teaching paragraphs to reference the discussion. It is a part of the clinical process and belongs in the clinical chart. It is neither secret nor dangerous and its omission leaves key elements of decision process obscured. Must the chart note be typed? Again this is a subject of some disagreement but if the chart note is to be used for directing the process of care and for purposes of education it must be typed. No one reads a long multiple paged hand written note. Also, a typed note is prerequisite for a QI process and for saving notes in a format that can be assessed later for origin of consultation and use of the service. The notes are a rich basis for institutional self-analysis and policy development. How should chart notes be used, protected and communicated? 85 This question is answered as much by institutional culture and technology as by theory. At Montefiore Medical Center [MMC] there is a shared institutional I-drive to which all of the bioethics consultants have access. On that drive are shared documents, e.g. the QI form and the scoring system, and a yearly file with monthly slots. Every consultation note is filed in this system and all of the consultants have access. This ensures, by providing a stable searchable base, that any consultant can determine instantly whether or not this patient’s care has been the subject of a prior consultation, whether on a prior admission or on this present admission. [Once the chart notes are a part of the electronic medical record--a process under engagement--this need will be somewhat ameliorated.] In addition, at MMC, a copy of the chart note is sent to all of the staff members who were present at the discussion via the closed and protected institutional system. Finally, the note is used as the basis for communication in two other situations: first, if the ethics consultation is counter to the peculiarities of New York State end-of-life law and second, if there may be administrative consequences that follow from the consultation. If there appears to be some tension between the dictates of ethical analysis and the arcane holdings of NY state law that discrepancy is highlighted—not in the note itself—but in a transmitting e-mail to the relevant administrative persons. The first, second and third rules of bioethics consultation are “transparency” at least among colleagues and staff. The chart note is also an excellent vehicle for arranging a transfer of authority if mediation and negotiation fail to reach a solution that is acceptable to all involved. Sometimes a bioethics consultation fails to reach a shared solution and the institution must then assume authority and use its administrative structure to devise and enforce an outcome. In such an event the chart note is an important history of the decision thus far. None of this communication can be facilitated by a hand written chart note. Indeed, given the increasing aegis of the electronic medical record it may not even be feasible in the future. Some final thoughts on diction, structure and perspective of the chart note and of the CEC. A chart note must be true to the facts and as objective as possible. It should eschew all pejorative and negative references to members of the care team, family or patient. It should strive to be non-subjective, with a tonality that is respectful. It should be concise but still be an embellished section of the patient narrative. It must always teach about the case and highlight the principles and analysis that is relevant. Clinical ethics consultation is important in the individual case and critical to forming the intellectual shared perspective of the institution. It is how the principles and practices of bioethics get built into the intellectual fabric of the institution. By addressing each case respectfully and carefully, and by documenting that intervention and analysis in the chart, departments and divisions in the medical center acquire case material to review and teach each year with new housestaff, medical students and attending physicians. Good chart notes are the basis for grand rounds, case conferences and ethics curricula that speak in a language and tell the tales that physicians can hear and assimilate. 86 Document C: How to Write a Bioethics Chart Note: A. Introduction: A Bioethics Chart Note tells a story. It tells the reader, and reinforces for the participants, what happened, how it happened, who the players are—patient, family, providers--what their interests are and how the options for care are ethically developed and supported. Clearly much of the perspective presented in this memorandum has been honed over the years in discussions among the MMC staff and in collaboration with Rita Charon, the master of “narrative ethics”. The bioethics chart note has a plot, and perhaps a subplot. It has intertwining characters some of whom have interacted before and have a history together and some of whom are new to the setting and the issues. How the players perceive the situation and their threatened rights or interests will determine, to some part, how they play out their roles. The chart note author is also a character in the unfolding narrative; she, too, has a role and interests. Her interest is largely in reaching a consensus that encompasses, to the degree possible, all of the clashing, colliding and conforming values and interests of the other parties. She is the mediator of all of the past and collected history, the present clashes of perspective, needs, wants and desires. It is through her eyes, and in her voice, that the chart notes takes form. That voice should reflect the reality, as far as it can be determined, of the meetings and interaction. When it is the voice of the “bioethics consultant”, that, too, must be clear. Much of this perspective is not new. It is the documentation of the process set forth in Bioethics Mediation, A Guide to Shaping Shared Solutions, by Dubler and Liebman. It reflects the skills that we all learned from Carol Liebman about framing, stroking, shouldering responsibility, amplifying voices, supporting positions and maximizing options. This document will not repeat all of that wisdom. This is the last step in the clinical ethics consultation experience: how to pass on the a sense of the process and product in a way that is helpful and guiding for the staff that must continue with the patient, the family and each other. It is also critical to keep in mind that the chart note is a legal document. It is part of the legally discoverable record of the care of the patient in the institution which can be introduced as evidence if the care is ever challenged in a court case. As such the clinical ethics consultant should not offer an opinion in regard to what the law is. That is not the object, the goal or the appropriate stance of the ethics note. The note should be clear about ethical knowledge, ethical principles, ethical perspectives and the weight of different modes of analysis and different ethical exercises in balancing the benefits and burdens of care in the context of the life of the patient. The Clinical Ethics Chart note is just that: it is about ethics. It is about value contexts and value conflicts. It is about mediation and ethical positioning. It is not about what the law is and what the law would demand or permit in the circumstance presented. This reluctance to state the law is in direct confrontation with the knowledge that clinical ethics consultants must have about what the law is in their jurisdiction. But, in the allocation of 87 authority in major modern medical centers there is almost always an office of legal affairs that has the responsibility and authority to state what the law is or is not in the space of the medical center. These staff are, rightfully, guardians of their powers. There are also offices of riskmanagement which have the responsibility for assessing risk and determining hospital actions in matters of risk. A clinical ethics consultant needs to be aware of the boundaries of ethics consultation and respect these other institutional voices. The chart note must reflect these divisions of authority and power if it is to have its own sphere of influence. A clinical ethics consultation note is just that: an identification and analysis of ethical issues and opinions. It is not a legal or risk management memorandum. If the chart note is typed, however, it can be an excellent vehicle for transmitting an ethical analysis of the situation and the options to these other offices. In the MMC model we are committed to a totally transparent process in regard to these other related, allied and coordinate players in the institution. If there is a case that may be of concern to the office of legal counsel or the office of risk management, the chart note will be e-mailed to those offices, but only after it is written and placed in the chart. However do note, Bioethics Mediation [page x] that there are some situations that may not be appropriate for bioethics intervention at all: cases that involve very hostile family members or patients who are threatening to sue; cases in which a suit has already been instituted; or some special circumstance such as, in New York State, certain wards of the state who are living in group homes, as long-term mentally ill or congenitally retarded persons, and decisions about whose care is regulated by special sets of state rules In these cases there may be a request for Clinical Ethics Consultation from the office of legal affairs or the office of risk management but that would be a special matter to be coordinated with these offices. The CEC chart note has a special place in the medical record. It has an obligation to adhere to standards in the profession. It must be knowledgeable, readable, clear, directive and respectful throughout to patients, family members and the staff. It should lead by example. It should state the narrative, explain the ethical issues, outline the options and state the conclusion, recommendations and future plans. Equally as important, it should educate the reader about the area of ethical knowledge that was involved in the consultation. The Bioethics Chart note is a part of a process of Bioethics Consultation Model at any health care institution. On the next page please find the elements of that model: B. The Chart Note: [Note: Before sitting down to write a chart note review the QI form. It is designed as a quick guide to directing a CEC and as a guide for designing the chart note. It can not replace the depth of knowledge in Bioethics Mediation but can be a quick refresher as a consultation begins. It is always the place to state when the char note is in formation. If all of the points on the QI form have been addressed in the process of the consultations and documented clearly in the note, it will be rated as a quality intervention.] As you can see from the above Institution Bioethics Consultation Model, bioethics consultation is not a “stand-alone” statue; it is not an isolated object. It is part of the fabric of delivering 88 clinical care to the patient in the context of the family. It is clinical service that clarifies and explains ethical options and the benefits and burdens of these options to the patient, family a members of the medical team. It then communicates these discussions through a chart note that is placed in the patient’s chart and sent, if the culture of the institution permits, to the participating medical staff. The Template: The chart note is based on the following template: Introductory material: [Note: These are the data that you should be keeping to have a searchable data base that permits gathering aggregate data on the sorts of consultation called over the year, by whom, on what issues. It is the basic data that the person getting the call, or carrying the beeper, should collect. It is also the heading for an electronic medical record.] Patient’s name, MR# ____________________________________________________ Primary diagnosis_______________________________________________________ Patient’s DOB_________________Date of hospital admission___________________ Name & position of person who called consult _______________________________ Unit (service/ICU)__________________ Name of PCP_________________________ Time and date of consult request___________________________________________ Stated reason for consult_________________________________________________ A. Time and place of the consultation: [See QI Form section A. Participants] [Note: these paragraphs locate the discussion. They, in effect, set the stage, cramped or spacious, orderly or somewhat chaotic. They may describe a meeting in an empty room in the MICU with staff sitting on beds and on the windowsill. The conditions of the consultation and the participants emerge here.] Persons present at the consultation including title [housestaff, patient’s attending, social worker for the patient etc.], place of the consultation [in the conference room behind the nurses station]. This descriptive section should explain which staff members were there and which were not and why. If the patient’s attending physician was not there—was she contacted, refused, was present by phone? Were all of the care providers who have been involved in the case and who are necessary to understand the history and the future possible courses of medical intervention present? [Note: the chart note should never be part of a” chart war” or other hostile interaction. If the attending physician was clear that she would never attend this sort of event, which almost never is the case, then it should be noted that the attending physician was aware of the meeting and could not attend, either by conference call or in person.] 89 If the patient is able to participate has she been interviewed and if not has she been seen? Respect for patients requires, in this model, that the patient be encountered as part of the process. A CEC should never write a chart note, or even convene a discussion about a patient’s care without having encountered the patient. Sometimes that means trying to rouse the patient and failing to do so. The attempt is what matters. What was the initial arc of discussion with the care providers? What issues were raised, what disagreements surfaced and what possible resolutions suggested? B.1.Relevant medical history: [See QI Form Section B. Relevant history] [Note: this is a more difficult section to write than one might think. For non-medical staff it must be clear to them what the sentinel medical issues are that correlate with the ethical questions. For new consultants who are not medically trained it is best to ask questions, clarify, restate and, in the case of very, very complex medical situations, prepare a draft that can be reviewed by a medical person before placing this section in the chart note.] Was the medical history of the patient clear? Were sufficient facts provided so that the reader had a sense of the course and development of the illness or condition? Was it clear that there were, or were not, additional medical consultations that needed to be scheduled or facts that needed to be clarified? Were all at the meeting satisfied that the medical facts explained the present status and possible future options for the patient? B.2. Relevant social and family history: [See QI Form Section B. Relevant history] [Note: This is a difficult section to construct as the complexity of families is one of the givens of modern bioethical and literary life: “Happy families are all alike; every unhappy family is unhappy in its own way.” Leo Tolstoy, Anna Karenina, Chapter 1, Line 1, The issue for bioethics consultation is where to draw the line. A clinical ethics consultant is not a therapist, although some of the same skill may be required, not a short story writer, although some of the same skills may be required and not a criminal investigator, although some of the same skills may be required. A CEConsultation is an attempt to delve sufficiently deeply into the dynamic of the family so as to better understand the patient and the choices that the patient may have in terms of medical options. It is also critical to explore some family dynamics when it is one, or many, of the family members who are making the decision for a patient who can no longer decide for herself. Even when there is a legally appointed proxy or health care agent, the agent is balancing many imponderable factors in her decision: what did the patient actually say, when capacitated; what short of person was—is—the patient? What sort of decision can the proxy live with, going forward into the future? What decision can the family, who will go on with the proxy, tolerate and accommodate? These are the currents that may surround a discussion with the proxy.] Was the history of the patient and the family explored in the chart note? 90 C. Conduct of the consultation/mediation: [See QI Form Section C. Consult implementation] It is the commitment of the MMC Consultation Service that most calls for bioethics consultation are actually calls for some sort of dispute resolution, whether between staff or among family, patient and staff. The experience of the MMC service is reflected in “Bioethics Mediation”. This brief document is not designed to replace “Bioethics Mediation”. That volume is necessary to understand the dynamics of bioethics consultation that are documented in the chart note. [Note: this section should reflect the progress and process of the various meetings, telephone calls and other relevant interactions. It is quite helpful, if the chart note contains brief quotation. These sorts of “textured” language give authenticity to the discussion. The note should attempt to capture the tone of the conversations and the voice of the patient, especially if the patient is not any longer able to participate in the discussion. What does the CEC, want to capture from the feeling, tenor, emotion, information and dynamic of the meeting. What will be helpful in directing the readers’ attention to the relevant ethical issues and how they should be resolved?] D. Ethical Problem: [See QI Form Section D. Ethical Problem] This section should attempt to describe the ethical problems that are encountered in the consultation and, if possible, assign them to categories. [Note: we are particularly not looking for the identification of principles; autonomy, beneficence, non-maleficence and justice. These are perfectly good mid-level ethical principles that animate much of the philosophical discussion in foundation bioethics. But it will not help the staff to note that a problem is solved be a de-ontological or consequentialist analysis. Nor it is helpful, in and of itself, to identify the ethical issues involved. Autonomy may be the platform for the discussion, but it needs more elaboration to be ethically useful to the staff, patient, family and chart note reader. What this section of the note should do is to address the sorts of categories of bioethical problems that have been elucidated in bioethics and legal literature. How would we, as CEC, explain the contours of the problem, both in the discussion, where teaching is always appropriate, and in the chart note where the same holds true. The “paragraphs” in the back-up materials are particularly useful in constructing the chart note. As you become familiar with the list in Section D of the QI Form, it will become increasingly easy to structure the discussion and to create the chart note.] E. Ethical Analysis: [See QI Form Section E. Ethical Analysis] This is a central feature of the CEC chart note. This section of the note calls on all of the training as a clinical ethics consultant. The “paragraphs” will be very useful in t his regard as they can provide a road map for the analysis. Ethical knowledge is what qualifies the CEConsultant for the role that she plays. [Note: this does not need to be an extensive section but it needs to be clear. See models of chart notes attached] F. Process: [See QI Form Section F. Process] 91 This section follows closely on the ethical analysis section and describes the process of dissection and disaggregation of issues, discussion and consensus building. Or, it describes unmanageable conflict that can’t be ameliorated by the consultation process. [Note: this section, as with section D. Ethical Problems, gives you specific guidance on how to write the note in questions 1-10. If the note addresses all of the questions outlined it will give a clear sense of the process of the meeting.] This section really describes the discussions that took place among the staff and between staff member, patient and family. There can almost never be too much description. The more that the dynamic of the conversation is relayed, developed and the nuances highlighted, the better the reader understands what happened. Things happen in discussions as they happen in interventions, and the CEC is an intervention. If there were shifting positions and evolving arguments they will contribute to ultimate understanding of how the decision turned out and why. G. Recommendations: [See QI Form Section G. Recommendations] This is an extremely important and very complex section to create. First of all, this is not a medical note that will suggest a medical intervention. Although it may be the case that in order to effectuate the ethical recommendations some medical follow-up will be needed. This is a recommendation that should emerge from the case discussion and analysis of the chart note and must “sound” in ethics and not just in medicine. The recommendation might read: This is a difficult case of a medically complex patient, with COPD and a below the knee amputation whose ability to remain at home and be safe is in question. However, despite some deficits, with the support of her son, all concluded that it was worth the attempt at one more discharge to home. Neither the patient nor her son wants her discharged to a nursing home. The patient has sufficient capacity to assess her situation and to opt for some level of risk in her setting to meet her needs for independence and autonomy. This is an example of “supported autonomy” which depends, on large measure on the ongoing involvement and caring interventions of her son. However, as these remain in place, it seems not to endanger the patient more than her capacity to assume risk would support. This would be more helpful than the recommendation that was actually written in the case: There is no reason at the present time to push for nursing home placement. Neither the patient nor her son wants it and we have a discharge plan that may work. We have K’s cooperation. The big question is how the patient will respond. The suggested recommendation is also far better than the sorts often seen that state: Psychiatry should assess her capacity one more time. The pulmonary service should be asked to assess the oxygen machine in the home to determine whether or not it is working at peak capacity. Home care should assess her for services. All of the above might be embedded in the note but they do not constitute the Recommendation of the Clinical Ethics Consultation. Ethics should beget ethics. 92 H. Style: [See QI form Section H. Style] This section relates to the “diction” of the chart note. Diction is not a common word, but, nonetheless, a useful one. Is the language precise, careful, respectful, non-judgmental? Is slang used when more medical, ethical or sociological language would be more helpful? Are abbreviations used when a more complete appellation would be more helpful? Are all derogatory terms avoided? Does it help the analysis to label a patient as a LOLFOF—a little old lady found on floor? Does the chart note model the sort of language and presentation that should be the goal for medical communication? 93 Section V CECP Tools 94 CECP QI Form: CLINICAL ETHICS CONSULTATION LOG Patient’s name: ______________________________________________________ MR#: _____________________ Patient’s DOB: ___________________________ Primary diagnosis: ___________________________________________________ Date of hospital admission: ____________ Date ICU admission: _____________ Name/position of person who called consult: ______________________________ Unit (service/ICU): ____________ Name of PCP: ______________________ Time and date of consult request: _______________________________________ Stated reason for consult: ______________________________________________ ____________________________________________________________________ 95 CLINICAL ETHICS CONSULTATION CHART REVIEW FORM Date of consultation__________Name of consultant____________________________ Question A. Participants 1. Was it clear who requested the consultation? (specify in comment field) 2. If it was not the attending physician, was s/he informed in person or by telephone? 3. Were important care providers involved? 4. Was the patient cognitively able to participate? 5. Was there a face-to-face patient visit? 6. Were important family stakeholders involved? 7. Is it clear who is making decisions on the patient’s behalf? (specify in comment field) B. Relevant history 1. Ethically relevant medical history? 2. Ethically relevant social history? C. Consult implementation 1. Was the consult largely mediation, that is dispute resolution among care providers, family or patient? 2. Was the consult largely consultation, that is clarification and analysis of relevant ethical principles and practices? 3. Were there meetings/discussions with care providers only? 4. Were there meetings/discussions with family only? 5. Was there a joint meeting/discussion with care providers and family(or patient/proxy)? 96 Yes/ Most Some/ Part No NA1 Comment Question Yes/ Most Some/ Part No NA1 Comment D. Ethical problem 1. Was the ethical/mediation issue(s) well identified? 2. Which of the following issues most apply (indicate “yes” to all that apply; optional: rank 1-3 in importance) Allocation of scarce resources Benefit burden analysis in care options Best interest of the patient Confidentiality Cultural values and treatment Decision specific capacity Doctrine of double effect End of life balance of acute and palliative care interventions Failure of the medical team to assume “responsibility” for difficult medical choices Informed consent Justice in the context of American medicine Medical ‘futility’ Patient autonomy Prior directives and delegation of authority Proposing ‘false choices’ to pts and family Refusal of care Religious values and treatment Setting boundaries for care Special pediatric issues: best interest for neonates, children and adolescents best interest Substituted judgment Truth telling Withdrawing and withholding treatment Other (describe) 97 Question Yes/ Most Some/ Part No NA1 Comment E. Ethical Analysis 1. Was relevant bioethical knowledge integrated into the note? 2. Was the chart note sufficient for educational purposes? F. Process 1. Does the note give a clear description of the dynamic of the discussion? 2. Was the voice of the patient clear? 3. Were the voices of the family stakeholders clear? 4. Were the positions of the care providers clear? 5. If there was disagreement among health care team members, was consensus achieved? 6. If there was disagreement among family members, was consensus achieved? 7. If there was disagreement among health team and family members (or patient/proxy), was consensus achieved? G. Recommendations 1. If consensus was achieved: Were the recommendations clear? 2. If consensus was not achieved: Was it clear what should happen next? H. Style 1. Appropriate medical language used throughout? 2. Neutral language used throughout? Name of person reviewing this chart note_____________________________________ 98 Notes on Using the QI Tool and Scoring System for the Chart Note The goal of this project is to influence the quality of the clinical consultation, but we can only assess the completeness and clarity of the chart note. The score should reflect how much relevant information is included in the clinical ethics note. Of equal importance, “relevant information” also means that the consultant has noted missing/unavailable information. If all questions are applicable to the note, there are 98 possible points (denominator). For a “NA” (not applicable) variable, the maximum number of points for this question are subtracted from the denominator so the note is not penalized. The “yes/most” column should be used if at least 85% of the information you deem important in this section is in the note. Less then 85% should get points as “some/part” unless there is very little information (<25%) which should get scored as “no/none”. If you use the “not applicable” (NA) option, explain why in comment field. But the comment field should be used for any comment, not only to explain “NA”. Suggested Scoring System Each section (A-H) of the Chart Review Form has been assigned a maximum number of points according to its relative importance in a clinical ethics chart note (in parens). We have drafted guidelines about how each section should be scored. While we expect some subjectivity, we are striving for general consistency between reviewers. A. Participants (0 - 14) The note should be clear about how which individuals [beyond the consultant(s)] were involved in the clinical consult, and whether important people participated. 2 points for each “yes” Q.1-3, 5-7. 1 for “some/part” 0 for “no”. Q 4 which gets 2 points for a “yes/most”, “some/part”, or “no” answer. For Q5, if a face-to-face patient visit is not stated, then the answer should be “no”. This does not depend on patient’s cognitive status. If “NA” is appropriate (as in q.6, if patient has no family) 2 points will be subtracted from the note’s denominator. B. Relevant history (0-10) The relevant history (medical and social) should state what is and what is not known (i.e., what needs to be clarified and what can’t be further clarified even when relevant). 5 points each for “yes/most” 3 for “some/part” 0 for “no” C. Consult implementation (0-10) Either Q1 or Q2 should be “yes/most” so that it is clear whether the focus of the consult was conflict mediation or clarification of ethical principles. If Q1 is “yes/most” and Q2 is “some/part” or “no”, give 4 points for the correct combination; similarly if Q1 is “some/part” or “no” and Q2 is “yes/some”, give 4 points for the combination. In some instances Q1 and Q2 could both be “yes/most” and receive full credit (4 points). Q 3-5 2 points each for “yes/most” 1 for “some/part” 0 for “no” 99 D. Ethical Problem (0 - 10) The note should be clear about the primary ethical issue (s) raised by this case. This question can be understood as has the consultant correctly and clearly identified the key ethical issue(s)? Q. 1 gets 5 points if the central ethical issue is well defined and fleshed out. Otherwise, it gets partial credit of 3 points. If ‘no’ is appropriate, it gets 0 points. For Q. 2, because the number of identified issues will be different in different cases, Q. 2 gets full credit of 5 points if at least 1 issue is clearly and correctly identified. There is no partial credit. “NA” is not appropriate for this section. E. Ethical Analysis (0-20) Q. 1-2 10 points each for “yes/most” 5 for “some/part” 0 for “no” “NA” is not appropriate for this section This section is the “meat” of the consult note. For full credit evaluate whether educational goals have been met by considering if the ethical principle(s) raised by the case were clearly and correctly identified and if the discussion appropriately linked these principles to the case. This section should include the use of educational paragraphs, and you must assess whether these paragraphs were correctly chosen and adapted for the particulars of this note. F. Process (0-14) Q. 1-4 2 points each for “yes/most” 1 for “some/part” 0 for “no” Q 5-7 Same as 1-4 except “NA” might be appropriate if there was no disagreement; points deducted from denominator for appropriate use of “NA:” Q5-7 should get 2 points for “yes/most”, “some/part”, and “no”, because achieving consensus is beyond the mediator’s control. G. Recommendations (0-10) Q. 1 or 2 10 points for “yes/most” (10 points for Q.1 means “yes/most” to both bullets) 5 for “some/part” 0 for “no” H. Style (0-10) Q. 1-2 5 points each for “yes/most” 3 for “some/part” 0 for “no” 100 CECP Institutional Survey One goal of the Clinical Ethics Consultation Project is to understand how bioethics consultations actually take place within institutions, and to help institutions standardize that process to improve quality. Please take a moment to answer the following questions about your institution, its current process for addressing bioethical issues and your role in that process. We will re-visit these questions later in the project. NAME OF TRAINEE ____________________________________________________ SETTING Name of Institution: ___________________________________________________ Description (check all that apply): Private/public/voluntary __ Acute/Chronic care ___ Academic Medical Center ___ Hospital Consortium ___ Ambulatory network ___ Other ______________________________________________________ # Beds ______ STRUCTURE FOR BIOETHICS Ethics Committee Yes ___ No ___ If “Yes”: How long has Ethics Committee existed? ________________________________ Who sits on the Committee (department, discipline, gender) _________________ How many members are on the Committee? ______________________________ Is there a defined tenure for members? __________________________________ Is appointment voluntary or mandatory? (circle) How is Chair chosen? _______________________________________________ Is Chair paid? Yes No Don’t Know (circle) Who sets agenda? __________________________________________________ How often does Committee meet? _____________________________________ Are meetings regularly scheduled or ad hoc? (circle) To whom does Committee report? _____________________________________ What is the relationship of the Committee to Risk Management? _____________ Other comments: ___________________________________________________ 101 Page two Bioethics Consultation Service Yes ___ No ____ If “Yes”: How long has the service existed? _____________________________________ Who staffs the service (department, discipline, gender) _____________________ How many consultants are there? ______________________________________ What is relationship of Consultation Service to Ethics Committee? ____________ Number of consults done in the last 12 months ____________________________ Number of consults done by you in the last 12 months ______________________ Other comments: ___________________________________________________ If “No”: What mechanism is in place to respond to clinical ethical problems? PROCESS Describe the process by which consults are done, from beginning to end. How are consults generated? __________________________________________ How is it determined who will respond? _________________________________ Is a chart note generated? _____________________________________________ Is there any oversight or review of the process and/or the note? _______________ SUPPORT FOR CLINICAL ETHICS WORK Check all that apply: ___ Protected time/salary support ___ Institutional recognition/acknowledgement ___ Conference attendance ___ Other (describe) CME Are there any educational activities in bioethics supported by your institution (check all that apply)? ___ Journal Club ___ Topic Presentations ___ Grand Rounds ___ Inter-institutional Network ___ Other (describe) ___No support 102 Trainee Characteristics and Initial Self-Efficacy Scale A. Personal Information 1. Name ___________________________________________ 2. Sex __________________ 3. Race/ethnicity __________________________ 4. Highest educational level (include professional degrees)_________________ 5. Current (or most recent) work ______________________________________ Characteristics of your work in bioethics 6. Describe the nature of your clinical ethics work___________________ _________________________________________________________ 7. During an average month, how many hours of your time are spent doing clinical ethics work?_______________________________ 8. How long has this work been a part of your job? ___________________ 9. What formal training in bioethics did you participate in? __________________________________________________________ __________________________________________________________ __________________________________________________________ B. The General Self-Efficacy Scale 1,2 In my role as a bioethicist or clinical ethicist, I believe that… (circle only one choice per statement) 1. I can always manage to solve difficult problems if I try hard enough. Not at all true 1 Hardly true 2 Moderately true 3 Exactly true 4 2. If someone opposes me, I can find the means and ways to get what I want. Not at all true 1 Hardly true 2 Moderately true 3 Exactly true 4 103 3. It is easy for me to stick to my aims and accomplish my goals. Not at all true 1 Hardly true 2 Moderately true Exactly true 3 4 4. I am confident that I could deal efficiently with unexpected events. Not at all true 1 Hardly true 2 Moderately true 3 Exactly true 4 5. Thanks to my resourcefulness, I know how to handle unforeseen situations. Not at all true 1 Hardly true 2 Moderately true 3 Exactly true 4 6. I can solve most problems if I invest the necessary effort. Not at all true 1 Hardly true 2 Moderately true 3 Exactly true 4 7. I can remain calm when facing difficulties because I can rely on my coping abilities. Not at all true 1 Hardly true 2 Moderately true 3 Exactly true 4 8. When I am confronted with a problem, I can usually find several solutions. Not at all true 1 Hardly true 2 Moderately true 3 Exactly true 4 9. If I am in trouble, I can usually think of a solution. Not at all true 1 Hardly true 2 Moderately true 3 Exactly true 4 10. I can usually handle whatever comes my way. Not at all true 1 Hardly true 2 Moderately true 3 Exactly true 4 1. Schwarzer R, Jerusalem, M. Generalized Self-Efficacy scale. In Weinman J, Wright S, Johnston M. Measures in health psychology: A user’s portfolio. Causal and control beliefs. Windsor, UK. NFER-Nelson. 1995: 35-37. 2. Schwarzer R, Fuchs R. Self-efficacy and health behaviors. In Conner M, Norman P (Eds.), Predicting health behavior: Research and practice with social cognition models. Buckingham, UK: Open University Press. 1996:163-196. 104 End of Year Survey NAME OF TRAINEE ____________________________________________________ Please fill in the chart below to help us understand whether you were able to incorporate any changes at your institution based on CECP training. If you have additional comments for any of the variables listed below, please add them on the back of the page. Variable Track # b/c Before CECP (Circle one) Rarely/Sometimes/Often Track who performed b/c Hand-written chart note Typed chart note Rarely/Sometimes/Often Note put in medical chart Face-to-face meeting w/ care team Face-to-face patient meeting Rarely/Sometimes/Often Rarely/Sometimes/Often Rarely/Sometimes/Often Rarely/Sometimes/Often Since CECP (Circle one) Rarely/Sometimes/Often/ Intend to start/started Rarely/Sometimes/Often/ Intend to start/started Rarely/Sometimes/Often/ Intend to start/started Rarely/Sometimes/Often/ Intend to start/started Rarely/Sometimes/Often/ Intend to start/started Rarely/Sometimes/Often/ Intend to start/started Rarely/Sometimes/Often Rarely/Sometimes/Often/ Intend to start/started Face-to-face Rarely/Sometimes/Often family meeting Any oversight/peer Rarely/Sometimes/Often review of b/c Rarely/Sometimes/Often/ Intend to start/started Rarely/Sometimes/Often/ Intend to start/started QI process for b/c Rarely/Sometimes/Often QI process for b/c note Rarely/Sometimes/Often Rarely/Sometimes/Often/ Intend to start/started Rarely/Sometimes/Often/ Intend to start/started Has your consult service changed in any (other) concrete way since you started the CECP? If yes, please explain: ______________________________________________________________________________ ______________________________________________________________________________ ____________________________________________________________ Number of consults done by the consult service since the start of the CECP ___________ Number of consults done by you since the start of the CECP _______________________ 105 FINAL SELF-EFFICACY In my role as a bioethicist or clinical ethicist, I believe that… (circle only one choice per statement) 1. I can always manage to solve difficult problems if I try hard enough. Not at all true Hardly true Moderately true 1 2 3 Exactly true 4 2. If someone opposes me, I can find the means and ways to get what I want. Not at all true Hardly true Moderately true Exactly true 1 2 3 4 3. It is easy for me to stick to my aims and accomplish my goals. Not at all true Hardly true Moderately true Exactly true 1 2 3 4 4. I am confident that I could deal efficiently with unexpected events. Not at all true Hardly true Moderately true 1 2 3 Exactly true 4 5. Thanks to my resourcefulness, I know how to handle unforeseen situations. Not at all true Hardly true Moderately true Exactly true 1 2 3 4 6. I can solve most problems if I invest the necessary effort. Not at all true Hardly true Moderately true 1 2 3 Exactly true 4 7. I can remain calm when facing difficulties because I can rely on my coping abilities. Not at all true Hardly true Moderately true Exactly true 1 2 3 4 8. When I am confronted with a problem, I can usually find several solutions. Not at all true Hardly true Moderately true Exactly true 1 2 3 4 9. If I am in trouble, I can usually think of a solution. Not at all true Hardly true Moderately true 1 2 3 Exactly true 4 10. I can usually handle whatever comes my way. Not at all true Hardly true Moderately true 1 2 3 Exactly true 4 106 ASBH Interview Guide Personal Information: Name? Gender? M/F Race/Ethnicity? Year of birth? A. Institution Demographics: What is the name of the institution where you work? Where is it located (City, State)? Is this location urban/rural/suburban? Is it a private/public/voluntary institution? Does it provide acute/chronic care? Is it a(n): Academic medical center? Community hospital? Hospital consortium? Ambulatory network? Other? (nursing home/rehab center/hospice/etc.) How many beds does it have? In the last year (2007) did you personally perform any clinical ethics consultation at this institution? Y/N In the last year (2007) did you personally perform any clinical ethics consultation at another health care facility? Y/N o What was that facility? If “No” to having performed clinical ethics consultations in the last year (2007): Ok – we have just a few more questions for you… Does your institution have a bioethics committee? If yes, in the last year has the committee performed any clinical ethics consultations? Please describe the process. o How is a consult initiated? o Who is involved? o To whom does this clinical ethics (committee?) report? o Is a note written in the chart? by whom? o Is there any QI function that reviews the notes? o Is there any training in Clinical Ethics Consultation? Are there any requirements (what kind of requirements?) for who is involved in the consultation? Would you be willing to send us a resume? Many thanks for your time. Would you like us to send you a final report when we have completed it? If yes, at what email address? 107 If “Yes” to having performed clinical ethics consultations in the last year (2007): The next questions ask about the structure of clinical ethics consultation[CEC] at your institution. B. Bioethics Structure: 1. General structure: What is your title in the institution (if you work at more than 1 institution, what is your title at the institution where you spend the most time)? Is there a policy in your institution governing clinical ethics consultation? Is the CEC performed by the Bioethics Committee as a whole, or in some sub-structure? How were you appointed to the clinical ethics consultation service? By whom [title] were you appointed? 2. Ethics committee: Are you a member of the institution’s bioethics committee? (If no, skip to #3; if yes, continue.) What is your title within the institution’s bioethics committee? Who appointed you to the bioethics committee? How long have you served on the bioethics committee? In your institution, is the bioethics committee responsible for the clinical ethics consultation? To whom do you report when you do clinical ethics consultations? How many consultations did the committee do in total in 2007? How many consultations did you do in 2007? 3. Characteristics of clinical ethics consultation: How many professionals engage in clinical ethics consultation in your institution? Are written notes generated for the consultations? If so, who writes the note? If so, where are they placed? (e.g. medical chart) If not in medical chart, where are they held? o If not in medical chart, who has access to the written consult notes? Does your institution use electronic medical records? o If so, are clinical ethics consultation notes entered in the electronic medical record? Is there a quality improvement process for the clinical ethics consultations and/or notes? If yes, please describe it. Who reviews the work of the clinical ethics consultation service? Are you on salary at your institution? Are you compensated in any way for your clinical ethics consultation work (percent effort, comp time, etc)? 108 How long have you been a practicing clinical ethics consultation? During an average week, how many hours do you spend on clinical ethics consultation work? Would you be willing to send us a resume? Many thanks for your time. Would you like us to send you a final report when we have completed it? If yes, at what email address? 109 MONTEFIORE MEDICAL CENTER DELINEATION OF CLINICAL PRIVILEGES CLINICAL ETHICS CONSULTATION Clinical Ethics Consultation is the intervention by a trained bioethics professional that: 1. responds to the request from any member of medical care team, patient or family member for a bioethics consultation; 2. gathers the clinical care team and other consultants to discuss the case; 3. involves the patient or family with a select number of the health care team to maximize options and seek consensus; 4. employs discussion of bioethical principles and practices, facilitation and mediation to reach a consensus about a plan of care going forward; 5. documents the process and substance of the consultation in the medical record Name (Please print) Name of Department (and specialty) MANDATORY: List Each Practice Site Location Location/s of Practice Ambulatory Site _ Inpatient Site _______organization-wide (Attach additional sheets, if necessary, to list all practice site locations) Criteria for Granting of Privileges (check all that apply) Completion of Certificate Program in Bioethics and Medical Humanities or comparable academic program. ______ Completion of Montefiore’s Fellowship Training Program in Clinical Ethics Consultation or comparable experience. Criteria for Reappointment of Privilege Completion of requisite number of Clinical Ethics Consultations, participation in the Bioethics Committee Journal Club (Attendance Certificate Attached) Mandatory: Indicate site-specific privileges, where appropriate. Privileges Requested Clinical Ethics Consultations 110 Yes No Privilege Approved Privilege Denied Practice Site Specific Comments Signature of Applicant Date Signature of Division Director Date Signature of Chairperson Date Model Forms For Credentialing FORM #1 TO: I, ____________________________ hereby authorize ___________________________, Name of Applicant Name of Institution its staff, or representative to provide the Medical Center any and all information requested below, whether such information is favorable or unfavorable, and I hereby release from any and all liability the above named hospital and/or person for any and all acts performed in fulfilling this request, provided that such acts are performed in good faith and without malice. I understand that completed forms must be returned directly to the Medical Center and if returned to me will not be accepted for verification purposes. Applicant’s Signature ______________________ Social Security# _____-_____-_____ The above-named allied provider has applied for clinical privileges as a clinical ethics consultant at the Medical Center and advised us that she/he completed clinical ethics education at your institution. Please indicate below the education completed in your institution and return this form directly to: Verifications returned to the applicant will not be accepted. Type of Educational Program: ______________________________________________ Year Entered: _______ Year of Graduation: _______ Degree/Certificate: ____________ I attest that the foregoing information is true and correct. _____________________________ __________________________ Signature Date _____________________________ __________________________ Print Name Telephone # _____________________________ Title 111 FORM #2 APPLICATION FOR CREDENTIALING AS A CLINICAL ETHICS CONSULTANT AT THE MEDICAL CENTER AND VERFICATION OF PROFESSIONAL TRAINING TO: DATE: I, ____________________________ hereby authorize ___________________________, Name of Applicant Name of Institution its staff, or representative to provide to the Medical Center any and all information requested below, whether such information is favorable or unfavorable, and I hereby release from any and all liability the above named hospital and/or person for any and all acts performed in fulfilling this request, provided that such acts are performed in good faith and without malice. I understand that completed forms must be returned directly to the Medical Center and if returned to me will not be accepted for verification purposes. Applicant’s Signature ______________________ Social Security# _____-_____-_____ The above-named allied provider has applied for clinical privileges as a clinical ethics consultant at the Medical Center and advised us that she/he completed clinical ethics education at your institution. Please indicate below the education completed in your institution and return this form directly to: Verifications returned to the applicant will not be accepted. Type of Training: __________________________ Dates: From _________ To _____________ Type of Training: __________________________ Dates: From _________ To _____________ Type of Training: __________________________ Dates: From _________ To _____________ I attest that the foregoing information is true and correct. _____________________________ __________________________ Signature Date _____________________________ __________________________ Print Name Telephone # _____________________________ Title 112 FORM #3 APPLICATION FOR CREDENTIALING AS A CLINICAL ETHICS CONSULTANT MALPRACTICE CLAIMS HISTORY To: Policy #: _____________________ I, ______________________________ hereby authorize ______________________________, Name of Applicant Name of Malpractice Insurance Carrier its staff, or representative to provide to the Medical Center any and all information requested below, whether such information is favorable or unfavorable, and I hereby release from any and all liability the above named hospital and/or person for any and all acts performed in fulfilling this request, provided that such acts are performed in good faith and without malice. I understand that completed forms must be returned directly to the Medical Center and if returned to me will not be accepted for verification purposes. Applicant’s Signature ________________________ Social Security# ______-______-______ MALPRACTICE CARRIER: Please complete the lower portion of this form and return to: 1. 2. 3. 4. Has the professional liability insurance of the person listed above been denied, suspended or revoked or changed in any way in the last ten years? Have any professional liability suits been filed against the person listed above in the last ten years? Have any judgments or settlements been made against the person listed above in professional liability cases in the last ten years? Are there any suits filed which are presently pending? Yes No □ □ □ □ □ □ □ □ If the answer to any of the above questions is “YES”, please provide details including dates and a brief summary of the claim(s) or incidents on a separate sheet. This information will be used for credentialing purposes only and kept confidential. _____________________________ __________________________ Signature Date _____________________________ __________________________ Print Name Telephone # _____________________________ Title 113 FORM #4 MEDICAL CENTER APPLICATION FOR PRIVILEGING AS A CLINICAL ETHICS CONSULTANT CONFIDENTIAL PROFESSIONAL REFERENCE EVALUATION TO: DATE: APPLICANT: _____________________________ DEPARTMENT: _________________ The above-named Professional has applied for clinical privileges as a clinical ethics consultant at the Medical Center. Please complete this form and return it directly to: I. RELATIONSHIP OF REFERENCE TO APPLICANT 1. Your title or position at the time of observation: ______________________________ 2. Dates of observation: ______ / _____ / ______ to ______ / _____ / ______ II. APPLICANT’S PROFESSIONAL KNOWLEDGE, SKILLS AND ATTITUDE 1. Are there any clinical areas or issues which you would be concerned about allowing the applicant to do clinical ethics consultants on if she/he were in practice with you? No □ Yes □ If Yes, please explain: 2. Have you ever observed or been informed of any physical, mental, health, drug, alcohol dependence or other problems which the applicant has that have or could potentially impair his/her ability to do ethics consultations in a reasonably sensitive and skillful manner? No □ Yes □ If Yes, please explain: 3. To the best of your knowledge, has the applicant’s clinical privileges as a clinical ethics consultant, hospital staff membership or any aspect thereof, or other professional status ever been denied, challenged, investigated, suspended, revoked, modified, restricted, placed on probation, or voluntarily surrendered under investigation, or do you have knowledge of any such actions are pending? No □ Yes □ If Yes, please explain: 4. Do you know of any malpractice actions or professional medical misconduct proceedings instituted or in process in your state or any other state involving the applicant? No 114 □ Yes □ If Yes, please explain: 5. Please rate the following: Bioethical knowledge Clinical ethics judgment Use of assistance when needed Availability and thoroughness in performing consultations Medical record timeliness, clarity, and completeness Participation in committees, etc Verbal and written fluency in English Rapport with medical staff, patients, and families Ability to work/communicate with others Excellent Good Fair Poor Unknown □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ III. SUMMARY 1. My general recommendation concerning the applicant is: Recommended without reservation Recommend Not Recommend □ □ □ 2. Please use this section for any additional comments, information, or recommendations which you believe would be relevant to our decision to grant staff membership and clinical privileges. _____________________________ __________________________ Signature Date _____________________________ __________________________ Print Name Telephone # _____________________________ Title 115 CECP Ethics Paragraphs ADVANCE DIRECTIVES All patients who are capable of making decision have the right to execute an advance directive to ensure that their wishes will be followed if they become incapacitated. Advance directives may be oral or written. There are basically of two types: Living Wills and Proxy or Health Care Agent Appointments. A Living will is a document that explains what the patient would want in the future if she could no longer discuss the decision and provide contemporaneous informed consent. Living wills are value neutral and could be used to prospectively request or refuse care. Most living wills, however, are structured to refuse interventions like surgery, ventilators and antibiotics. Health care proxy appointments give the person appointed general ability to make decisions for the patient based on the standards of what the patient has said she would want [explicit directive], what one could surmise she would want from her behavior and pattern of life [substituted judgment] and absent both of these what is in her best interest. Health care proxy appointments are generally more flexible and more responsive to the nuances of medical conditions than are living wills. Proxy appointments permit the team with the proxy to begin an intervention, to assess its success and then to continue or withdraw it as the condition of the patient requires. Living wills are less flexible and tend not to reflect the nuance of patient wishes: “I do not want a ventilator” does not generally mean that the patient would not want a few days of supported breathing if the result is likely to be effective and then would let the patient continue unassisted. Living Wills tend to make absolute rather than nuanced statements, and as such are less appropriate to the art of medicine. ALLOCATION OF SCARCE RESOURCES A condition of scarcity occurs when demand exceeds supply, and medical examples include intensive care resources and transplantable organs. An important distinction is between scarce and expensive resources. Ventricular devices are currently extremely expensive resources, but they are widely available. By contrast, hearts for transplant are expensive as well as scarce. Scarce resources are generally also expensive; but the converse does not hold. Another distinction is between natural scarcity and created or artificial scarcity. For example, ICU beds are an expensive resource that is made into a scarce resource by an organizational decision limiting the number of beds. If the institutional budget permitted ICU expansion, more beds could be made available. In contrast, solid organs, such as hearts, are from the outset a scarce resource because of their finite supply and the scarcity cannot be eliminated entirely. When the scarcity is a created or artificial one, an appropriate question to ask is what it would take to eliminate the scarcity and at what cost to other programs meeting other needs. Sometimes, because the cost would be ethically prohibitive, the scarcity must be accepted as the least bad arrangement. Scarce resources are those that cannot meet the needs of all who could benefit from them, and therefore some way of setting priorities among them must be devised. Since not everyone who could benefit can receive the resource, some will have to go without, and this may mean some 116 will have to die. Because of the stakes involved, decisions regarding allocation of scarce resources must be based on sound medical and ethical criteria. Ethically, a system of allocating scarce resources must be both fair and designed to benefit the greatest number of patients. In the case of ICU care, priorities are established and patients with a greater likelihood of benefiting from ICU care are given preference over those who are less likely to benefit from care in that setting. Generally accepted medical criteria exclude patients who won’t benefit from critical care because it would be physiologically futile, or they are in PVS or brain dead. Criteria that are considered ethically unacceptable include ability to pay and social worth. ASSENT AND CONSENT Effective informed consent provides ethical as well as legal authorization for the physician to treat. Consent contrasts with assent. The latter, a notion with particular relevance in pediatrics, reflects the patient’s agreement with a treatment plan, rather than authorization of it. Only when the conditions of informational disclosure, understanding, and voluntariness have been met in the context of decisional capacity can the patient’s consent or refusal be considered truly informed. Though young children cannot provide truly informed consent to treatment, they can, depending on the circumstances, assent to it, at least in the sense that they do not actively oppose it. Assent in this context is important since it facilitates treatment that is deemed to be in the child’s best interest. It may be difficult it not practically impossible to treat a child who is unwilling to cooperate with the plan of care. As the child matures and becomes an adult, he may be able not merely to assent but to provide legally and ethically valid consent. Among incapacitated adults, assent also has value. Though an adult patient may lack the capacity to consent to dialysis, for example, long-term treatment is likely to be unsustainable if the patient persists in actively opposing it. BEST INTEREST STANDARD Frequently treatment decisions must be made for patients who lack capacity and cannot decide for themselves. These may be persons who were formerly but are no longer capable of making decisions or individuals, like newborns or severely retarded, who never had the opportunity to form values or preferences. The standards for health care decisions for patients who lack capacity give preference to the patient’s voice as the central and most widely accepted source of authority. In some cases, the decision maker may rely on the prior stated wishes of the patient or, if these are not known or were never articulated, the inferred wishes of the patient. But when neither is possible, the decision maker must rely on a best interest standard. This standard requires an objective assessment of the relative burdens of benefits of available treatment options. Since this standard is employed when there is no knowledge of a particular patient’s prior wishes or inferred wishes, it is primarily an impersonal standard. In the absence of such particularized knowledge, the best interest standard considers what would be most likely to benefit or promote the well-being of a hypothetical reasonable patient in the same circumstances as those of the patient. Any additional information specific to the particular patient being treated might also contribute to an assessment of what is in his or her best interest. 117 In assessing best interest, both the outcome and the probability of achieving this outcome for different treatment options should be considered. In the clinical setting, the best interest standard would consider mitigating pain and suffering, prolonging life, restoring and enhancing comfort, and maximizing the potential for independent functioning. In all cases where this standard is invoked, best interest should be determined as far as possible from the perspective of the patient, not that of the decision maker. A life that may be unacceptable to the decision maker may be acceptable to the patient, and it is the latter standpoint that should be adopted. BRAIN DEATH AND REASONABLE ACCOMMODATION According to traditional criteria of death, death is the irreversible cessation of heartbeat and respiration. However, with the advent of heart transplants in the late 1960s, it became necessary to supplement this with a neurological definition that permitted the timely retrieval of usable organs for transplantation. The first well-accepted definition of brain death was the product of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death, which issued its report in 1968. The committee defined brain death as the irreversible cessation of total brain function. The Uniform Determination of Death Act, adopted in 1980 by the National Conference of Commissioners on Uniform State Laws, expanded the definition of death to include both cessation of circulatory and respiratory function and brain death. Brain death should not be confused with other neurological conditions, such as permanent vegetative state or minimally conscious state. Though the nature of death has been a question with which philosophers and theologians have wrestled for millennia, there is widespread consensus that, medically speaking, a brain dead patient is dead, period. The qualifier “brain” can be confusing to families because it suggests that only one organ (!) of the patient is dead, so many clinicians prefer not to use the expression “brain dead” but simply “dead.” Patients who are brain dead might have their organs maintained on a ventilator for some period of time, awaiting organ retrieval, and families often have difficulty accepting that the patient is truly dead when looking at a body that is warm, healthy-colored, has a heartbeat, and appears to be breathing. It only adds to the family’s confusion to say that the patient is brain dead but “is being kept alive” on a breathing machine, and such language should be avoided. Because the definition of death raises deep ethical, religious, and philosophical issues, some patients and families, for example, some Orthodox Jews and Muslims, reject defining brain death as death. Their religious and ethical convictions should be respected to the extent of making an effort at reasonable accommodation. Reasonable accommodation includes, for example, continuing ventilation, nutrition and hydration, and/or medications for some short, specified period of time. It does not mean that the now dead individual should continue to be treated as a patient. In particular, the resources provided by ICU care are scarce and should be allocated to those who can benefit from them the most. Since brain dead patients can no longer benefit in any way from care, they should not remain in the ICU. CONFIDENTIALITY 118 Confidentiality is one of the bedrock ethical principles in health care. The principle of confidentiality has a number of bases. First, respect for persons underlies patients’ right to control who has access to their health care information and requires that medical records and communications in the clinical setting be protected from unwarranted disclosure. Control of this information can be seen as a form of self-determination. Second, the effectiveness of the clinical relationship and the resulting quality of the health care that is provided depend on an atmosphere of trust between the patient and the physician, and this trust is facilitated by confidentiality. Without assurance of confidentiality, patients may be reluctant to provide all relevant information about their medical condition. Third, confidentiality protects patients from unauthorized disclosure of information that, if made public, may be personally embarrassing or damaging to them. The principle of confidentiality governs other relations as well, including priest-penitent and lawyer-client, and various protections for the confidentiality of these relationships are established in the law. In recognition of the fact that most health care today is provided by teams of medical professionals, and consonant with the requirements of HIPPA, the principle of confidentiality does not preclude the free exchange of patient information within the team caring for the patient. In other ways as well, changes in health care delivery have altered the contours of the principle of confidentiality, allowing legal and government bureaucracies and third party payers access to personal medical information. The principle of confidentiality is not absolute. There are three exceptions: first, when the patient poses an imminent risk of serious harm to him or herself; second, when the patient poses an imminent threat of serious harm to identifiable others (as argued in the famous 1976 case of Tarasoff v. Regents of the University of California); third, when the patient poses an imminent threat of serious harm to society at large (the so-called public health exception, as in cases of reporting infectious diseases). CONSCIENTIOUS OBJECTION Conscientious objection refers to a situation in which a physician or other caregiver opts out of participating in a plan of care or providing a particular medical service on moral or religious grounds. Most hospitals have policies permitting conscientious objection, as long as certain other conditions are met. Common examples include objection to honoring the decision of a patient or surrogate to forgo life-sustaining treatment or to institute a do-not-resuscitate order, and objection to assisting with or performing an abortion. The grounding in religious or moral principles is definitional of conscientious objection. Thus, objection to participating in withdrawal of life support because it reminds one of an unpleasant experience from one’s past does not count as conscientious objection, however much we may sympathize with the clinician’s reluctance. Similarly, treatment that the physician believes is detrimental to the patient’s best interest is not the same as treatment to which a physician has a conscientious objection. The rationale for honoring conscientious objection is that it respects and preserves the clinician’s personal integrity. One’s moral and religious convictions represent what one stands for on a deep 119 level, and they constitute one’s identity as a responsible individual accountable for one’s actions. To violate them is to do damage to one’s moral and religious identity; and to bar an individual from engaging in conscientious objection is to put him or her in the position either of resigning or violating his or her conscience. It is unfair to health professionals to put them in this position. At the same time, there are certain conditions that must be satisfied if conscientious objection is to be permitted. First, the clinician who conscientiously objects must notify the patient or surrogate, as well as his/her supervisor or superior, that his/her religious or moral convictions prevent participation. Second, the objecting clinician must make reasonable efforts to find another non-objecting clinician to take his/her place and to arrange transfer of the patient to that physician. Continuity of care should be maintained as far as possible and non-abandonment remains an important ethical obligation. Third, if transfer of the patient cannot be arranged, the objecting health professional may have to provide the requested service, depending on the seriousness of the patient’s medical condition and prognosis with or without the intervention. CONSENT TO AND REFUSAL OF TREATMENT The flip side of a capable patient’s right to consent to proposed treatment is the right to refuse proposed treatment. It is an established principle of law and ethics that capable patients have the right to refuse any proposed medical treatment, even if its likely consequence is his or her death. Respecting the patient’s refusal, like seeking the patient’s consent, is an aspect of honoring the patient’s right to autonomy. Refusal of recommended treatment should initiate a discussion about the reasons for the refusal. The patient might not understand the nature of the treatment that is being proposed and its potential risks and benefits; or may have certain fears relating to the treatment that can be addressed; or may have a treatable depression. Because of their profound implications, refusals of life-sustaining treatment in particular should receive heightened scrutiny. In general, in the case of treatment refusal, special attention should be given to the adequacy of the information presented and the quality of the explanation, possible language or cultural barriers to understanding, and the patient’s capacity and appreciation of the consequences of forgoing treatment. DEALING WITH THE ADOLESCENT PATIENT Adolescence is a developmental stage that falls between childhood and adulthood and that shares properties of each. By the age of 14, the normal child demonstrates a capacity to reason, including the ability to understand the causes and effects of illness, that is both as good and as flawed as it will be in adulthood. However, the capacity to reason is not the only ingredient of decisional capacity and adolescent capacity may be deficient in other respects. Other factors include: personal values, biological and emotional maturity, life experience, and appreciation of the long-term consequences of one’s actions. Moreover, the capacity of adolescents to make autonomous decisions is enormously variable because it is tied to the development of a sense of identity and to the adoption of a more or less stable set of values. As the adolescent matures, she acquires an increasing ability to assume control of and responsibility for her own decisions, and 120 correspondingly, a greater weight should be given to her values and wishes. All of these factors make ethical decision making for adolescents very complex. Adolescent decisions are typically the product of less experience and more volatile emotions than adult decisions, and more so than with adults, the decisions of adolescents reflect immature self-image, unrealistic appraisal of risks and consequences, and susceptibility to peer pressure. However, there are some adolescents, especially older ones or those who have lived with chronic illness for much of their lives, whose decision making capacities are not impaired in these ways. While the law makes categorical distinctions between adults and minors based on somewhat rigid and arbitrary standards, ethically a more individualized assessment of adolescent decisional capacity is required. The factors to be considered include the adolescent’s emotional maturity, her ability to solve problems and consider alternatives, and her experience with illness and loss. DECISION-MAKING CAPACITY Determining whether a patient has the capacity to make medical decisions is often a key ingredient of a clinical ethics consultation. Decisional capacity is not a legal determination (this is called “competence”) but a clinical one that can be made by any member of the health care team who is familiar with the patient and has interacted with him or her over a more or less extended period of time. Capacity refers to the patient’s ability to perform a set of cognitive tasks, including: o Understanding and processing information about diagnosis, prognosis, and treatment options; o Weighing the relative benefits, burdens, and risks of the therapeutic options; o Applying a set of values to the analysis; o Arriving at a decision that is consistent over time; o Communicating the decision. Having capacity enables an individual to make decisions; it does not obligate him or her to do so, and in fact a person with decisional capacity may waive the right to make decisions or confer this right on others. It is an established principle of law and ethics that adults who have the capacity to make their own medical decisions should be able to do so. Not to give them the opportunity to make their own decisions is a violation of their right to autonomy. Decisional capacity is decision-specific, that is, it varies according to the complexity and seriousness of the decision at hand: more complex and more weighty decisions require a greater degree of decisional capacity than less complex and less serious ones. The appointment of a health care agent, for example, requires only a fairly low level of decisional capacity, whereas deciding whether to have a complicated surgical procedure requires considerably more. In addition, decisional capacity is not always clear-cut or necessarily constant. In some cases, there may be no definite answer to whether the patient has the capacity to make a particular decision. And depending on their age, cognitive abilities, clinical condition, and treatment regimen, patients may exhibit fluctuating capacity. For example, elderly patients often exhibit greater alertness, clearer reasoning, and better communication earlier in the day. Drug interactions can also cause a temporary loss of capacity. 121 DECISIONS ABOUT ARTIFICIAL HYDRATION AND NUTRITION The issue of withdrawing artificial hydration and nutrition frequently arises for patients who have permanently loss consciousness; it is also considered for patients who are irreversibly and terminally ill and do not tolerate the procedure well. Ethical concerns about forgoing artificial hydration and nutrition often take the form of worries that we will be “starving” the patient if he or she is not fed or hydrated. However, existing medical opinion suggests that patients who have permanently lost consciousness do not experience pain or discomfort following the withdrawal of artificial hydration and nutrition. Less information is available about the experience of patients in the end stage of the dying process, but available information here too suggests that these patients appear to experience little, if any, discomfort when routine comfort measures are provided. In fact, provision of artificial hydration and nutrition can in some instances actually increase the patient’s discomfort and cause numerous complications, including pulmonary edema, nausea, and mental confusion. Ethical debate about artificial hydration and nutrition has centered on whether these measures should be distinguished from other treatments on medical or clinical grounds. On one side, some argue that artificial hydration and nutrition constitute “basic care” rather than medical treatment, hence that artificial hydration and nutrition should almost always be provided. Also, some commentators argue that forgoing artificial hydration and nutrition intentionally causes death unlike, say, the forgoing of ventilatory support, and is tantamount to killing. On the other side of the debate are those who argue that artificial hydration and nutrition should not be distinguished from other medical treatments. They are not universal needs for all persons, but interventions in response to an underlying disease and condition. In addition, it has been argued that forgoing artificial hydration and nutrition is crucially different from intentional and active killing. The view that artificial hydration and nutrition are not to be distinguished from other medical treatments is reflected in statements by the AMA’s Council on Ethical and Judicial Affairs and recent court decisions. DECISION-MAKING IN THE NEONTATAL INTENSIVE CARE UNIT Decision making in the NICU involves three parties, caregivers and parents, and the state as well in its role as parens patriae or protector of the vulnerable. In this setting, parents have a great deal of authority to make decisions on behalf of their newborns, including, in some circumstances, the right to terminate life-sustaining care. Our society’s deference to parental decisions rests on respect for family integrity, the presumption that parents act in their child’s best interests, and the need to have a designated authority to make such decisions. Specifically, three ethical rules of thumb guide decision making in the NICU: 1. If the parents are making decisions that are medically indicated and clearly in their child’s best interest, their decision should be supported; 2. If the parents are making decisions that are not medically indicated and not in the child’s best interest, their decision should be resisted; 3. If it is unclear whether the parents’ decision is in the child’s best interest, or if there is legitimate disagreement about this, the parents’ decision should be respected. 122 Conceptions of benefit and harm may be defined differently by caregivers and parents, creating conflicts in the NICU over how or even whether to treat their sick newborns. These conflicts may reflect different conceptions of what constitutes an acceptable quality of life for the child. In addition, the fact of prognostic uncertainty complicates decision making. Often conflicts between parents and caregivers can be resolved as the child’s condition and prognosis become clearer, parents are given time to absorb bad news, and they receive the emotional support of the team. Part of this emotional support is dispelling the notion that they are “monsters” because they have decided to terminate life-support for their critically ill newborn. DEMANDING FAMILIES Health professionals sometimes find themselves confronting families that they describe as “demanding,” “difficult,” or “unreasonable.” It is important for good patient care to uncover and deal with the source of these problems. Families may demand treatments that are judged to be therapeutically inappropriate or otherwise not indicated, such as dialysis for a patient who is actively dying, or refuse treatments that are clearly medically indicated, such as a life-saving blood transfusion for a young child. Another possibility is that families will try to micromanage care for their loved ones. However, while family members often provide consent for recommended treatment, there are ethical limits to what they may demand or refuse, and these limits are set by existing standards of care. Though members of the health care team may feel intimidated by demanding families, there is no ethical obligation to provide treatment simply because the family wants it. Boundaries also have to be set by the health care team to prevent intrusive and obstructive interference by family members in the care their loved ones receive. Demands for treatment should trigger a discussion with families that explores their understanding of the patient’s medical condition and prognosis, the specifics of their demands, and their hopes and expectations for the patient. A mediation approach, which seeks to level the playing field and provides a forum for all interested parties to voice their concerns and raise questions, is often helpful in these circumstances. Families may demand that “everything” be done without having an understanding of what “everything” encompasses or that everything reasonable and medically indicated is already being done. Carefully probing their concerns may reveal fears and misconceptions that can be addressed. In the end, however, if no consensus can be reached between family and caregivers, it is the ethical obligation of health professionals to practice good medicine. DNR ORDERS New York State has a do-not-resuscitate law that authorizes patients with capacity to provide consent to a DNR order. The consent must be informed, that is, caregivers are required to inform the patient about his/her condition, the risks and benefits of CPR, and the consequences of a DNR order. For patients who lack capacity, and who have not appointed a health care agent, a duly authorized surrogate may consent on his/her behalf, but only if the patient meets one of the following medical conditions: (a) the patient has a terminal condition; (b) the patient is permanently unconscious; (c) resuscitation would be medically futile; (d) resuscitation would impose an extraordinary burden on the patient in light of the patient’s medical condition and the 123 expected outcome of resuscitation for the patient. The surrogate who has legal authority to consent to a DNR order for a patient who has not appointed a health care agent is a person in the highest category on the following list who is available, willing, and competent to decide about CPR: 1. A guardian 2. Spouse 3. Son or daughter 18 years or older 4. A parent 5. Brother or sister 18 years or older 6. A close friend. If the patient has appointed a health care agent, the agent may make all health care decisions the patient can make, including decisions to discontinue life-sustaining treatment such as CPR. A health care agent can generally decide about all treatment; a surrogate under the DNR law, however, can only decide about CPR. In addition, if there is a health care agent, he/she takes priority over a surrogate in deciding about CPR. A DNR order on grounds of medical futility can only be entered if the physician determines, to the best of his/her medical judgment, that CPR would be unsuccessful in resuscitating the patient or that the patient would arrest again in a short period of time before death occurs. The physician must discuss the order with the patient, agent, or surrogate, if possible, but does require his/her consent. The judgment of futility must be confirmed by a second physician. If the family of the patient objects to a DNR order on grounds of futility, mediation may help resolve the conflict. If mediation is unsuccessful, a DNR will normally not be entered. THE DOCTRINE OF DOUBLE EFFECT The doctrine of double effect was formulated in response to the recognition that an act may have both a good and a bad effect. According to this doctrine, the permissibility of an action depends largely on whether the bad effect is intended, or merely foreseen and permitted to happen. In addition, it must also be the case that the act is not wrong in itself; the good effect is the result of the intentional act, not the result of the bad or harmful effect; and the benefits of the good effect outweigh the foreseen but unintended bad effect. The doctrine of double effect has been used to support adequate palliation, especially at the end of life. The doctrine recognizes that, while the administration of sufficient opioids to manage pain at the end of life may risk depressing respirations enough to hasten death, the clinical and ethical mandate to relieve suffering is paramount. The physician’s purpose is not to kill but, rather, to alleviate pain, although he foresees that death is possible, perhaps even likely. Also, giving drugs to relieve pain is not wrong in itself, and the good effect – the relief of pain – is produced directly by the administration of the drug not by the patient’s death. Finally, when a patient is terminally ill and suffering, the desirability of relieving pain sufficiently compensates for the shortening of his or her life. The doctrine of double effect is recognized as a valid ethical principle by professional medical associations as well as state and federal courts of law, including the Supreme Court in the 1997 physician-assisted suicide cases. However, the doctrine also has its critics. They argue that the 124 doctrine is often difficult to apply because it not always easy to know whether a result is intended or merely foreseen or whether it is brought about by means of the bad effect (e.g. the patient’s death) or the morally neutral action (e.g. administration of pain killers). Whatever the final verdict about the difficulty of its application, the doctrine is an important part of the practice of end-of-life care, and it would be unwise to abandon it. To do so would risk equating pain relief that has the effect of causing death with pain medication administered in order to cause death, and this would have a detrimental impact on the quality of patient care near the end of life. DO NOT RESUSCITATE AND DO NOT INTUBATE Do not resuscitate (DNR) is a specific order stating that CPR shall not be initiated in the event there is a cardiac or respiratory arrest. It does not refer to situations in which there is respiratory distress but no arrest. A capable patient has the right to consent to DNR and, depending on her clinical condition and prognosis, should be given the opportunity to consent to it. (In rare cases involving the so-called therapeutic exception, discussion of DNR with the patient may be illadvised.) If the patient is not capable of providing consent, or has not in the past indicated her wishes regarding resuscitation, others may be legally empowered to consent to a DNR order on her behalf. In New York State, there is a law authorizing specific others to consent to DNR, including health care agents, parents, spouses, siblings, and close friends. Surrogates may consent to DNR for a patient only if one of the following four medical conditions is met: (a) the patient is terminally ill or (b) permanently unconscious; (c) resuscitation would be medically futile (see paragraphs on “Medical Futility”); or (d) resuscitation would be inhumane, given the extraordinary burdens it would impose on the patient. DNR should not be confused with DNT – i.e. do not treat. Nor is it, by itself, a reason not to admit the patient to an intensive care unit, if it is felt that she could benefit from the services provided there. DNR orders are normally suspended in the OR, where an acute reversible process directly related to the surgery itself, and not to the patient’s underlying disease process, may require intubation. Resuscitation typically includes intubation and, depending on the patient’s clinical picture, this may be temporary or of indefinite duration. It may be in response to a cardiac or respiratory arrest, or in response to respiratory distress. DNR orders only cover the former situations. However, capable patients, their health care agents, or other appropriate surrogates, may refuse intubation in distress situations as well. FALSE CHOICES The suggestion is sometimes made that the full disclosure necessary for informed consent requires that the physician offer all possible treatment options for consideration to patients and families. However, this is an incorrect interpretation of what informed consent requires, because there are some care decisions that do not require and should not impose the burden of patient or family consent. These are cases of false choice in which patients and families are asked to reject interventions that have no clinical indication and which can provide no real benefit. Presenting patients and families with false choices actually diminishes rather than enhances the exercise of 125 their autonomy and abdicates the professional’s responsibility to exercise clinical judgment and guide patients and families in ways that make clinical sense. When reversal of or improvement in the patient’s condition is no longer possible, it is inappropriate for physicians to present care options in a way that suggests otherwise. Interventions that are physiologically futile (see Medical futility) or outside the standards of medical practice should not be proposed. When specific treatments, such as dialysis, antibiotics, or vasopressors, are no longer effective, it is disingenuous to patients and families to present them as if they were real options, and unfair to burden them with a choice that is not theirs to make. This is not an instance of medical paternalism that disempowers patients and families. Rather, it involves physicians assuming responsibility for making the judgments that only physicians can make and leaving patients and families with choices that fall within the realm of the medically possible. In this way, physicians support rather than usurp the genuine health decision making authority of patients and families. INFORMED CONSENT Informed consent is a process of communication between physician and patient characterized by mutual participation, respect for the autonomy of the patient, and shared decision making. Informed consent is not a perfunctory discussion or a signature on a document. The legal doctrine of informed consent, out of which the ethical principle developed, was initially based on the law of battery, holding that any unconsented-to touching consistuted an unlawful act. The signal case establishing the principle of informed consent in medicine was Canterbury v. Spence, 464 F.2d 772 (D.C. 1969), which held that the physician is obligated to provide sufficient information about a procedure’s risk so that a reasonable patient can make an informed decision. All health care procedures and treatments require the informed consent of the patient or an authorized representative. Informed consent has a number of requirements. There are disclosure requirements: the physician must disclose information about the proposed diagnostic or therapeutic intervention, the purpose of the intervention, the consequences of nontreatment and alternatives to the proposed intervention; and the physician should make a recommendation about how the patient might consider the benefits and burdens of the intervention. There is also a requirement that the consent be voluntary, that it not be coerced, or forced, or unduly influenced. However, this does not preclude providing recommendation and support to the patient. Independent decision making is not the same as isolated decision making. There are a number of exceptions to the consent requirement: emergency care; the so-called therapeutic exception in which disclosure of information is reasonably believed to present a substantial risk of immediate, direct, and significant harm to the patient; and waiver of consent by the patient. MEDIATION 126 Mediation is an extremely useful procedural technique for identifying, responding to and resolving conflicts that arise in the course of patient care, between and among patients, families, and health care providers. • It is a private, voluntary, informal process in which an impartial third person facilitates a negotiation between people in conflict and assists them to find solutions that meet their interests and needs. • The mediator works with the parties, helping them identify their goals and priorities, generate and explore options, and exchange information that may be necessary in formulating a solution. • Mediators are optimists. In health care settings, • Bioethics mediation combines the clinical substance and perspective of bioethics consultation with the tools of the mediation process, using the techniques of mediation and dispute resolution in order to: – identify the parties to the conflict (although disagreements between family and care providers are common, most conflicts have more than two sides); – understand the stated (presented) and latent interests of the participants; – level the playing field to minimize disparities of power, knowledge, skill, and experience (to the degree possible) that separate medical professional, patient, and family; – help the parties define their interests; – help maximize options for a resolution of the conflict; • One of the greatest advantages of using the mediation process in bioethics disputes is its flexibility. The general structure of mediation can be adapted and altered to fit the needs of the participants. But the starting point is always the same: respect for the patient, the family, and the care providers and an impartial stance regarding what should be the outcome in any particular case. • In bioethics mediation, the process is a key part of the product There are limitations of mediation, however: • Parties to a mediation must want to reach agreement, and sometimes they don’t. • In some cases, the patient or family members may not have the emotional strength to take responsibility for facing difficult facts or making hard choices. They may need to have some decisions made for them. MEDICAL FUTILITY The term “medically futile” is commonly used quite broadly and loosely to describe treatments that are felt not to benefit the patient because he or she has a very poor prognosis. For example, dialysis for a patient with terminal cancer may be said to be medically futile. However, the term “futile” should be used with great care and may in fact be unhelpful to the process of resolving conflicts in patient care. Some physicians use “futile” narrowly, considering treatments futile if they would be physiologically ineffective or would fail to postpone death, for any significant 127 period of time. New York State’s DNR law uses “futile” in this sense, to refer to resuscitation efforts that would be ineffective or, while effective, would not forestall death for more than a very short period of time. Some physicians adopt a broader understanding of the term, to refer to treatment that cannot improve the patient’s prognosis, comfort, well-being, or general state of health. Following this approach, a treatment might be seen as futile if it does not offer what the physician considers to be an acceptable quality of life. Debates about medical futility are not just about labels. How we define futility has important practical consequences for how conflicts in patient care are addressed and resolved. Underlying different definitions of futility are different assumptions about the balance that should be struck between the authority of patients and families, on the one hand, and the authority of physicians, on the other. The term “futility” commonly functions as a trump card, permitting the physician to discontinue or not initiate treatment, and it is appropriately used in this way in when it has a narrow physiological sense. Physicians currently have no duty to provide treatment that is futile in the narrow sense, even if patients and/or families request it. But it is not appropriately used as a unilateral physician trump card when it reflects judgments about acceptable quality of life, or broader notions of patient well-being. In general, the term “futile” should be avoided except in the very narrow circumstances of physiological futility. The danger of using too expansive a notion of medical futility is that it will pre-empt communication and conversation between the physician and the patient/family regarding difficult matters, such as withdrawal or withholding of life-sustaining treatment. PALLIATIVE CARE Providing comfort, especially at the end of life, is not a new concept or a departure from the traditional responsibilities of the caring professions. However, its importance has been overshadowed by the tremendous advances medicine has made in recent years in curing disease and forestalling death. The discipline of palliative care has successfully cast the light once again on the notion that relieving pain and suffering is central to the complete and authentic practice of medicine. Its defining philosophy is that cure and comfort are consistent objectives that may assume greater or lesser prominence, depending on the patient’s condition, prognosis, wishes, and values. When the potential exists for significant improvement, the plan of care tends to emphasize aggressive curative measures, supplemented by comfort measures. As the likelihood of cure fades and the patient approaches the end of life, the goal of care ought to shift and aggressive palliation becomes the primary focus. Aggressive palliation refers to the provision of therapeutic interventions, including narcotic medications and surgery, to relieve pain and manage other symptoms effectively. When curative measures are no longer possible, the message to patients and families should not be, “There is nothing more we can do,” but, rather, “There is a great deal we can do to keep the patient comfortable and allow for a dignified death.” The relief of pain is both a professional obligation and a moral imperative, clinically as well as ethically mandated. Before the advent of palliative care as a medical subspeciality, it was frequently noted that patients’ pain was often not adequately appreciated or managed and that many patients died in pain. With greater understanding of pain, how to assess and treat it, and an 128 enhanced appreciation of the importance of this long-overlooked aspect of patient care, this situation has begun to change in significant ways. RELIGIOUS OBJECTIONS TO TREATMENT There is a broad based consensus in our society that adults who have the capacity to make their own decisions have the right to consent to and refuse medical treatment, even if that refusal leads to their death. This right is endorsed in the bioethics literature as well as by federal and state courts of law, including the famous New Jersey case, In re Quinlan (1976), the first right-to-die case to achieve national prominence, and the U.S. Supreme Court decision in Cruzan v. Director, Missouri Department of Health in 1990. The right to refuse unwanted treatment is not predicated on any specific reasons that the patient has for refusing. As long as the decision can be construed as a more or less rational or reasonable one, the obligation to respect it applies. In particular, the refusal of treatment may be based on religious objections, such as the objection of a Jehovah’s Witness to receiving blood transfusions. A person’s religious faith embodies some of his most cherished values and deepest commitments, and respecting them is part of respecting patient autonomy. The right to refuse treatment based on one’s own religious convictions does not include the right to refuse treatment for one’s child, especially life-saving treatment, based on those convictions. Ethically, parents may martyr themselves to their religion, but not their children who are too young to have their own autonomously adopted religious beliefs. Further, most states do not allow individuals who have a religious objection to brain death to reject this definition of death (the only exception is New Jersey). What is called for in such cases is “reasonable accommodation,” and this does not include giving patients and their families the right to define death as they choose. Finally, the rights of physicians may impose some constraints on the exercise of religious choice by patients. For example, some anesthesiologists may refuse to participate in surgery on Jehovah’s Witness patients, if they cannot use blood as needed. SHARING THE BURDEN OF RESPONSIBILITY It is sometimes assumed that respect for patient autonomy means providing patients and families with full information about available treatment options, their risks and benefits, and then stepping back and allowing them to make their own decision. However, in most cases, such a view of patient autonomy amounts to “truth-dumping.” It overlooks the very real vulnerabilities that are part of the experience of illness and disability, and the need of patients and families for professional guidance in making sound health care decisions. Patients and families depend on professional guidance in making care decisions, and depriving them of the benefit of clinical judgment, advice, and support, and relying solely on the provision of full information, can be seen as a form of abandonment. Instead, physicians should be encouraged to clearly recommend what they believe to be the most appropriate therapeutic course and to discuss with patients and families their reasons for recommending it. Advice, recommendation, and guidance are often avoided out of the fear that they amount to the imposition of unjustified physician paternalism. But unjustified paternalism means violating another person’s right to freedom of choice, whereas advice and guidance can actually augment 129 freedom of choice rather than curtail it. Recommending should not be confused with imposing; assisting the exercise of autonomy should not be confused with usurping the exercise of autonomy. When physicians share the burden of decision making with patients and families and take some responsibility for guiding them in ways that make best clinical sense, they actually enhance the capacity of patients and families to make autonomous decisions. SIGNOUT AGAINST MEDICAL ADVICE Patients who choose to leave the hospital prematurely and against the advice of their physician represent a common and challenging dilemma. These patients who signout against medical advice are at risk because they have a higher rate of readmission. Finding a balance between attempting to protect patients from making “unwise” medical decisions and permitting patients to fully exercise their autonomy is challenging. This issue is particularly important because patients facing illness are in a higher-risk state both medically and emotionally. Physicians relying too heavily on their patients right to self-determination without a careful and thorough evaluation of their decisions, may be abandoning the patient when they are particularly vulnerable. Framed in terms of ethical principles, this problem is characterized by the tension between beneficence for patients and respecting patient’s autonomy. The patients “unwise” medical decision is a limited description in these types of dilemmas, because it assumes the priority of health concerns over all others. Indeed, health and longevity is only one of many values patient’s routinely consider in making decisions about their life. Using a non-judgmental approach to understanding a patients decisions can collect clearer patient information about their motivations to leave the hospital prior to an appropriate discharge. Better information about the patients motivating behavior allows physicians to target their counseling more appropriately and potentially negotiate a discharge to a more medically appropriate time. For example, when the clinician is able to determine that the patient wants to leave the hospital because she feels pressure to return promptly to work, he can attempt to reduce that burden by focusing on that issue (advocating on the patients behalf to her employer), rather than the conflict over discharge between doctor and patient. Ensuring informed consent can maximize the possibility that patients who choose to sign out against medical advice are receiving the best possible care. An informed decision means that patients have arrived at their decision by consultation with their provider, not under duress or coercion, and by understanding and appreciating the risks, benefits and alternatives of the decision at hand. Part of this process requires a capacity evaluation about the patient’s decision to discharge themselves from the hospital. A formal decisional capacity evaluation includes the following: Does the patient understand and appreciate the diagnosis, prognosis, likelihood of risks and benefits, and the treatment alternatives? Can the patient make and communicate a choice? And can the patient articulate a reason for the refusal that is consistent with her values? Many advocate the use of a “sliding scale” of capacity assessment, in that the greater the risk due to the patients refusal, the more certain the clinician should be that the patient has decisional capacity. For example, patients may have capacity to refuse a blood draw, but not to refuse a life saving blood transfusion. 130 SUBSTITUTED JUDGMENT The standards of proxy decision making for incapacitated patients place particular emphasis on respecting the wishes and values of the patient when he or she had capacity. Often, however, the prior wishes of the patient are not known, or were never expressed, and then proxies should consider whether a substituted judgment standard can be applied to the case at hand. A term originally borrowed from the law, a substituted judgment is a decision by others based on the formerly capacitated patient’s inferred wishes. The question to ask here is, “Knowing what you know about this patient’s values, behavior, and decision history, what do you think she would decide in this situation?” It may also be helpful to pose the question this way: “Suppose that the patient were sitting here now, capable of making decisions, listening to this conversation and knowing his medical condition and prognosis. What do you think he would tell us to do for him?” Since patients often do not give much thought to what they would or would not want if they became critically or terminally ill, or they do not discuss these matters with others, substituted judgment is frequently a more useful approach to decision making for incapacitated patients. Persons who know the patient well and are familiar with his values and beliefs, such as close friends or family members, are in the best position to make substituted judgments. It is particularly important in discussions with them to stress that, as far as possible, they should try to make decisions based on what they believe the patient would want, not what they would want for the patient. THERAPEUTIC EXCEPTION Informed consent, including disclosure of information, is generally a requirement of ethical patient care. However, the requirement is not absolute and without exception. In very rare circumstances, physicians may believe that the disclosure of information about diagnoses or prognoses will cause clinically unstable patients to suffer immediate, direct, and significant harm. In these cases, potentially harmful information may be withheld from patients, even if the patient is judged to otherwise have the capacity to make medical decisions. The rationale for the exception is that disclosure of information is designed to support and facilitate autonomous decision making. When disclosure of information is likely to result in immediate, direct, and significant harm, autonomous decision making is not enhanced but threatened. Even if information is justifiably withheld on therapeutic exception grounds, once the patient’s clinical condition permits disclosure, the disclosure must take place. The therapeutic exception is not a license to withhold information indefinitely, regardless of any change in the patient’s medical condition. Further, withholding information on grounds of therapeutic exception must be based on strong evidence that the patient will or is likely to suffer harm from the disclosure. Conjecture that the patient may suffer harm, or that it may be significant, is not ethically sufficient, given the strong presumption in favor of truth-telling and informed consent. In this connection, it is particularly important for clinicians to determine whether withholding information is really for the benefit of the patient, or their own comfort or the comfort of the family. Breaking bad news is difficult, and it is understandable that clinicians may be reluctant to do so or may defer to a family’s request that their loved one not be informed. However, this 131 cannot serve to justify withholding clinical information from an otherwise capacitated patient. To preserve the basis of trust in the doctor-patient relationship, information should be withheld from capacitated patients only in the narrowly described circumstances of the therapeutic exception. TRUTH-TELLING Collaborative decision making and informed consent depend on the reasonable disclosure of necessary or material medical information. Patients and their authorized surrogates are ethically and legally entitled to information that enables them to understand the likely course of the medical condition, evaluate the therapeutic options, and make choices consistent with the patient’s goals and values. The ethical basis of the principle of truth-telling is two-fold. First, disclosure reflects respect for the patient’s right of self-determination. Patients or their surrogates cannot make autonomous decisions if they are denied information relevant to those decisions. Second, patients are normally the best judges of what is in their best interest, and they may not be able to protect those interests if material information is withheld from them. The principle of truth-telling does not permit physicians and other health professionals to bludgeon the patient with the truth. Truth must normally be told, but it should be told when the patient is ready to hear it and in a manner that the patient is able to assimilate. If a patient has clearly indicated that he or she is not ready to receive the truth, the truth is not required, at least for the time being. Also, the truth may be withheld if disclosing it would cause immediate, direct, and significant harm, although this will occur only rarely. Withholding truth is not the same as lying, however, and lying is more difficult to justify ethically. Bad news is always difficult to hear, but sadness at such times is normal and should not be used as an excuse for withholding information. Indeed, truth-telling can be therapeutic, in that it dispels the complicity of silence that often surrounds discussion of such matters. There are cultural differences with respect to truth telling. In some cultural groups, truth telling to the patient is not a moral requirement and may even be frowned upon. In these circumstances, clinicians should ask the patient how much he or she wants to know about his or her medical condition, how much he or she wants to be involved in decision making about his or her care, and if there is someone else he or she would prefer making decisions. WITHDRAWING VS. WITHHOLDING TREATMENT Health care professionals often distinguish between withdrawing and withholding treatment and, as a result, are sometimes willing to honor decisions by patients or families not to start treatment, but will not allow them to refuse treatment once it has begun. Studies have shown that for clinicians there is a significant emotional difference between withholding and withdrawing treatment: in general, withdrawing is felt to be more emotionally difficult. This may due in part to the belief that withholding treatment is an omission whereas withdrawing treatment is a positive action and hence more culpable. Some regard withholding as “letting nature take its course” and withdrawing as “killing.” Over the past decades, however, a consensus has emerged that there is no moral distinction between withholding and withdrawing treatment. Whether treatment is stopped or never 132 initiated, all relevant moral factors are the same, including the health professional’s duty to respect the patient’s wishes, the consequences, the intentions, the cause of death, and the potential for abuse. Indeed, if there is any distinction to be drawn at all between withdrawing and withholding, it may favor the former, for withdrawal may occur after a therapy has been tried and found ineffective or unacceptable to the patient. The law also does not distinguish between withholding and withdrawing treatment. When one is legally permissible, so is the other. It is important to understand that withholding and withdrawing treatment are morally and legally equivalent, for this may facilitate good patient care. If withholding is believed to be morally or legally permissible, but withdrawing is believed to not be, then physicians may elect not to start treatment and patients may suffer. 133