Gastrointestinal Motility – Part I

GI #12
Tuesday 2/18 2:00pm
Dr. Gwirtz
Kevin Stancoven for Kara Starnes
Page 1 of 6
Submitted for review
Gastrointestinal Motility – Part I
Response of gut smooth muscle to NE: NE binds to alpha & beta-receptors. Alpha-receptors cause IP3 to form, which opens Ca 2+ channels in sarcoplasmic reticulum & releases Ca 2+ , which causes muscle contraction. Beta-receptors generates intracellular cAMP, which cause the SR to take up Ca 2+ & causes
Ca 2+ pump to pump calcium out of cell, which causes muscle relaxtion. Predominant receptor in gut is beta-2 receptor.
Objectives o Describe the basic patterns of GI motility: peristalsis, segmentation, & sphincter tone o Describe swallowing & the motor behavior of the lower esophageal sphincter o
Explain the process of mixing of stomach contents o Describe the control of stomach emptying o Explain the movement of material in the small & large intestines o Describe the interdigestive migrating motor complex o
Describe the defecation reflex o Explain disorders of the esophagus: dysphagia, achalasia, esophageal spasm, & heartburn o Describe the motor disorders of constipation, diarrhea, & gas o Explain the vomiting reflex
Time a meal spends in the GI tract o Mouth to LES – 9 seconds o Digestion in the stomach – 3-5 hours
Mixes with gastric secretions & ground into small particles o
Time to move through the pyloric sphincter – 1-5 minutes o Time spent in small intestines – 4-5 hours
Digestion & absorption o In proximal colon – 6-7 hours o
In transverse colon – 9-10 hours
Spends most of the time in the o In distal colon – 12-24 hours
Type of motility in the GI tract colon o Peristalsis
Contractile ring which is proceeded by receptive relaxation
Relaxation in front of chyme & contraction behind it
Moves material slowly down the GI tract
Reflex mediated by myenteric nerves. Myenteric nerves lead to weak contraction & reinforced by parasympathetic nerves.
Peristalsis reflex
Stimulus o Distention of the gut o Irritation of the epithelial lining
Complex pattern which requires coordination by the myenteric nervous system
Moves chyme analward (oral cavity towards anus) o Law of the gut
Location: pharynx, esophagus, stomach, intestines, colon, & bile ducts o
Mixing movements
Local constrictive contractions occurring every few cm in the gut wall
Decreases particle size of food, increases surface area available for digestion by enzymes and for absorption
Mixes with secretions & exposes to enzymes
Local constrictive contractions of the gut wall
Does not necessarily require myenteric nerves for coordination – not a reflex
Attributed to activity of circular muscle layer
Varies in rate from 12 (duodenum) to 3 (stomach) per minute in different parts of the gut
Keeps gut contents thoroughly mixed at all times o Tonic contractions – at sphincters
Tonic contractions with intermittent relaxation of sphincters
Serves to regulate the movement of luminal contents
Sphincters are rings of smooth muscle that remain in a continuous state of contraction, which produces a high pressure zone in the lumen
Neurotransmitter constantly released to allow continuous Ca 2+ entry into cell
Separates 2 specialized compartments along the GI tract
Location of GI sphincters
Upper esophageal sphincter o Skeletal muscle
Lower esophageal sphincter o
Smooth muscle
Gastroduodenal (pyloric) sphincter o Smooth muscle o Between stomach & duodenum
Ileocecal sphincter o Smooth muscle o Between ileum & large intestines
Internal anal sphincter o
Smooth muscle
External anal sphincter o Skeletal muscle
Sphincter of Oddi o Smooth muscle
You have control over sphincter with skeletal muscle
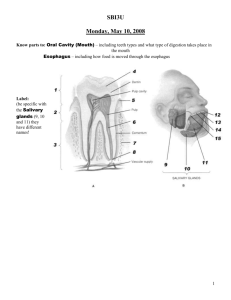
Chewing reflex – mastication o
Initiated by presence of food in mouth o Can be carried out voluntarily, but is more frequently a reflex behavior
There is a specific part of brainstem that control chewing o Requires parasympathetic nerves & myenteric plexus: central reflex o
Controlled by signals from touch & pressure receptors in the mouth, stretch receptors in the muscles & joints o Aids in digestion of food by increasing the surface area available for enzymes to act o
Mixes food with saliva & makes easier to swallow
Alpha-amylase begins starch digestion
Swallowing reflex o Stages:
Voluntary stage
Initiates swallowing reflex
Tongue pushes bolus of food back into pharynx, which stimulates nerve endings around pharynx
Can start or stop at will – involves motor neuron activation of skeletal muscle o You can control this part of swallowing
Pharyngeal stage
Involuntary
Controlled by brainstem swallowing center
Initiated by stimulation of swallowing receptors in pharynx
Results in the passage of food through pharynx into esophagus by pharyngeal muscle contraction
Inhibition of respiratory center o
Very brief – not noticeable o Swallowing center located next to respiratory center in brainstem
Trachea & nasopharynx closed by glottis – to prevent aspiration
Esophageal stage
Involuntary
Promotes passage of food from pharynx to stomach
Primary peristalsis o Initiated by swallowing reflex o Wave of contraction preceded & followed by wave of relaxation o
9 seconds in length o 1 wave carries food from pharynx to stomach o This can still occur when you stand on your head
Secondary peristalsis o Initiated by irritation or distention of o Repeated peristalsis waves o Example: food getting stuck in esophagus
Receptive relaxation of stomach
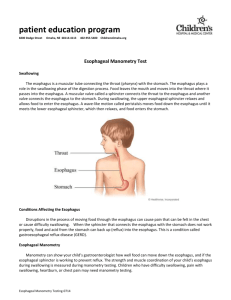
Figures: o Food being chewed & tongue pushes back toward pharynx o Beginning of swallowing reflex, upper esophageal sphincter is relaxed so food can move through o Sphincter closed & contraction pushes bolus down esophagus o Receptive relaxation of LES & stomach so food moves completely into stomach
Primary peristalsis o
Continuation of the peristaltic wave that begins in the pharynx & spreads into the esophagus during the pharyngeal stage of swallowing o Passes from pharynx to the stomach in 5-10 seconds o Mediated by vagal nerves & myenteric plexus
Vagal nerves must be intact for swallowing reflex to occur normally
Pressures during a swallow o Patient swallows balloon connected to manometer (to measure pressures) o Tracings on right show normal pressure in a swallow
Pressure at rest is at zero in pharynx & esophagus
High pressure (30 mm HG) recorded UES & LES at rest
Get receptive relaxation at sphincters & stomach before bolus reaches sphincters & stomach o
Peristalsis causes an increase in pressure as the bolus is moved down the esophagus o Swallowing disorders cause abnormal pressure readings
Secondary peristalsis o Stimulus is distension of smooth muscle wall of the esophagus, which may result if the primary peristaltic wave fails to move all of the food into the stomach o Initiated by intrinsic neural circuits in the myenteric plexus o Mediated by myenteric & reinforced by vagal nerve fibers
LES – lower esophageal sphincter o
Thoracic cavity is at a negative pressure – so it keeps the esophagus open o Abdominal cavity is at a positive pressure – so it collapses the esophagus
LES is in the abdominal cavity (below diaphragm) o Functional sphincter due to position below the level of the diaphragm
Not anatomical – doesn’t have smooth muscle rings
o Tonically constricted o
Receptive relaxation of LES & stomach during swallowing o Prevents reflux of stomach contents (acid) into esophagus
Factors increasing LES tone – increase muscle contraction o Chemical
Muscarinic agents, alpha-receptor agonists
ACh, cholenergic medications o Hormonal
Gastrin (released during digestion in stomach), motilin (released between meals, controls motility in GI tract between meals), NPY (co-released with ACh) o Other
Protein meal (amino acids causes gastrin secretion)
Antacids & alkali agents
Factors decreasing LES tone – promote gastric reflux (GERD) o Purinergic (ATP-type neurotransmitters), beta-agonists o CCK, secretin, VIP, glucagon, histamine (H
2
receptors), nitric oxide, progesterone
(pregnancy) o
Fats, carbohydrates, chocolate, cola drinks, peppermint o Anticholinergics, nitrates, nicotine, alcohol, caffeine o Increased abdominal pressure
Advanced pregnancy, bending, squatting, heavy lifting, constrictive clothing, obesity o Hiatal hernia
Esophageal hiatus (larger hole or weakening in diaphragm) causes LES to move into thoracic cavity – sphincter opens easier
Disorders of the esophagus o Skeletal muscle – interfere with swallowing
Myasthenia gravis, dystrophies, polio o Dysphagia
Diffuse esophageal spasm – prolonged contraction of lower esophagus
Achalasia – spasms of LES o GERD – gastroesophageal reflux
Pregnancy
Hiatal hernia
Deep anesthesia
Delayed gastric emptying
Pressure figures o
1 st one has normal pressures in the esophagus with swallowing o 2 nd figure is a representation of a patient with diffuse esophageal spasm
Motility disorder due to problems with myenteric nerve plexus
Get high pressure contractions occurring at multiple places along esophagus at the same time
UES & LES still functioning normally
Scans show a normal esophagus & one from a patient with diffuse esophageal spasm
This is a painful condition, pain radiates to neck & shoulder
Mimics angina o 3 rd figure is achalasia
Degeneration of myenteric plexus – fail to have peristalsis contractions in esophagus
Affects primarily LES – LES fails to relax
Food accumulates in the body of the esophagus
Next pictures shows a enlarged esophagus o Patients are in pain, discomfort & may aspirate food o Get esophagitis or esophageal cancer
GERD mechanism
o Table in power points o
Lists 4 different mechanisms of GERD & contributing factors o Read over & learn
Ascites – increased vascular pressure causes backup in liver & increases liver pressure (portal hypertension). Liver weeps fluid & fluid accumulates in abdominal cavity
Case study: GERD o F.J. is 44-year-old female with complaint of chest pain. She describes it as burning & pressure in middle of her chest. It radiates up into her neck & gets worse after eating o Possible causes of her GERD & their mechanisms
Decreased tone of LES – pregnancy,
Dietary
Obesity
Hiatal hernia
Good history & physical is needed to identify exact cause of GERD
Treatment depends on cause of GERD
Diet will help, sleep with head elevated, don’t eat before going to sleep
Anatomy of the stomach o Fundus – superior part o Body – primarily made of secretory glands
Pacemaker zone – interstitial cells of Cajal
Set slow wave rate (3 per minute) o Pyloric & antrum – inferior part
Enters in duodenum
Muscle thickness increases
Contractions push food back into body of stomach until food is small enough to escape through pyloric sphincter
Chyme needs to be 1-2 mm in diameter & be a liquid consistency in order to be squirted through pyloric sphincter
Stomach only empties when pressure is higher in antrum than the pressure in duodenum
Functions of the stomach o
Store large quantities of food – can hold 2 liters (normally)
When stomach if filled with food, intragastric pressure stays the same because smooth muscle relaxes as volume increases
If you loose vagus nerve, as you fill the stomach, pressure will increase o
Mix food with gastric secretions until it forms a semi-fluid mixture called chyme o
Slow emptying of the chyme into the small intestines at a rate suitable for proper digestion & absorption o Dilutes or concentrates fluids so they are the same concentration as the body fluids before reaching the intestines
Makes chyme isoosmotic (relative to plasma) o Forms intrinsic factor which is necessary for vitamin B
Receptive relaxation of the stomach
12
absorption o
Ability of the stomach to accommodate a large volume meal with only a small increase in intraluminal pressure o Vagal fibers innervate intrinsic nerves to cause receptive relaxation via a neurotransmitter
(VIP or NO) o
Vagotomy (vagus nerve is severed or removed) greatly diminishes receptive relaxation
Motility in the stomach o Slow waves – 3 per minute
Basic electrical rhythm
Interstitial cells of Cajal
Spontaneous fluctuations of membrane potential o Mixing wave
Weak contractions which move toward antrum of stomach
Mix food with gastric secretions
You make about 2 liters of gastric secretions a day o Peristaltic constriction rings
Force antral contents under pressure towards pylorus
Emptying of the stomach o
Promoted by intense peristaltic contractions of the stomach antrum o Opposed by varying degrees of resistance (constriction) to the passage of chyme through o
Begins 30-60 minutes after eating
Complete within 4-4 ½ hours after eating (depending on meal)
Fatty meal – stays longer in stomach
Liquid meal – passes through stomach quickly
Figure the pyloric sphincter
Influenced by nervous & humoral signals from the stomach & duodenum o Graphic showing different contractions of stomach o Also shows stomach emptying