Violent_Patient_Policy
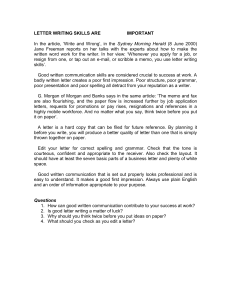
advertisement
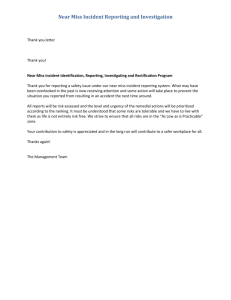
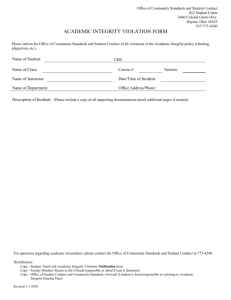
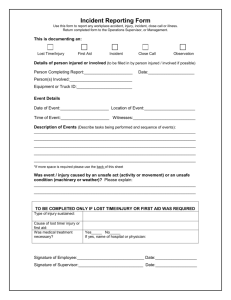
Violent and Aggressive Patient Policy Dr A. Lyon & Partners September 2011 Document Control Page Title of document Violent and Aggressive Patient Policy Author’s name Anne Grundy Author’s job title Practice Manager Doc. Status Final Signed off by Anne Grundy Original Publication Date August 2011 Last Reviewed July 2013 Next review date 2014 Distribution General Practice Consultation History Version 0.1 0.2 0.3 0.4 Date Consultation May 2010 Practice Manager/Partners Meeting September 2011 6th October 2011 Practice Manager/Partners/Reception Meeting July 2013 Revised by Practice Manager Reception Meeting 1.0 Introduction The NHS has a zero tolerance policy of all violence and aggression. This policy is for the protection of all NHS staff, but also for the protection of other patients, their families, visitors, etc. In order to ensure that this zero tolerance approach is adhered to, it is essential to have robust policies and procedures in place. In General Practice, this will need to cover a variety of situations in which incidents could occur. 2.0 Aims and Objectives The aims and objectives of this policy are as follows: To ensure adequate processes are in place for the protection of staff and patients To ensure staff are fully aware of their responsibilities when dealing with violent or aggressive patients To ensure that staff are fully aware of their rights when they have to deal with such incidents 3.0 Aggressive Patient What is an aggressive patient? This is a patient (or relative) who exhibits one or more of the following patterns of behaviour: Verbally abusive, offensive or intimidating in their behaviour towards staff Threatening physical violence Making excessive demands and/or maintaining certain expectations and failing to accept that these are unreasonable (e.g. wanting an immediate appointment and becoming aggressive when this is not possible) insisting that a member of staff is dismissed insisting that treatment is carried out on demand constantly requesting a different GP demands to see a particular member of staff/clinician 4.0 Dealing with an Aggressive Patient Patients can become aggressive for a variety of reasons, and it is always advisable to try to calm down the situation as early as possible, as this may prevent an incident. 4.1 An Aggressive Incident If the patient does become aggressive, then the following process should be followed: If they continue with their aggressive behaviour, then tell them that they will not be dealt with until they calm down. Remain calm and clear and keep repeating that the behaviour is unacceptable. Insist that you are trying to help, but cannot do so until they calm down. In the interests of safety, it is best to stay accompanied by another member of staff. Staff should never isolate themselves with a potentially violent patient. Get a more senior member of staff to speak to the patient, again keeping calm and stressing that you are trying to help. Following the incident, the main points should be recorded on a significant events form All incidents of violent and aggressive behaviour should be reported to the Practice Manager 4.2 Repeated Incidents If there are repeated incidents from a particular patient, then the practice should write to the patient warning them that no other incidents will be tolerated, and the patient will be removed from the list if this happens again. (See app 1 for sample letter) Note that it is important to carry out this action once it has been written down. If the patient continues with this behaviour, even after the written warning, then they should be removed from the list for the sake of staff and other patients. 5.0 Violent Patients Dealing with a violent patient requires a much more immediate response. As soon as a patient turns violent, then immediate action must be taken, as follows: Lock the reception door If the aggressive behaviour continues and a panic alarm is available, then press this immediately If the patient is in the consulting room with a clinician, then the correct procedure should implemented (see app 2) Phone the police. Once violence occurs, it becomes a crime. If there are other patients in the vicinity, then there is a duty to protect them. If possible remove other patients in the vicinity to another part of the waiting area or another room away from the situation. Following an incident of violence, the practice should hold a significant event meeting to decide if the patient should be removed from the list. If the patient is to be removed from the list, then the practice should now follow the procedure for the removal of patients. 6.0 Removal of Patient from Practice List When it becomes necessary to remove the patient from the practice list, for reasons of violent or aggressive behaviour, then a specific process should be followed. (See info 4 Policy on removing Patients from the Practice List). Under schedule 6 of the NHS (GMS Contracts) Regulations (2004), the PCT would be required to remove a patient from the GP practice list if it is informed by the practice that the patient has committed an act of violence against anyone present on the practice premises, or at any place where the services were provided to the patient, or that the patient has behaved in such a way that any person has feared for his/her safety. It is essential in all cases that the incident has been reported to the police, prior to the application to the PCT to remove the patient from the list. (See appendix 4 for an extract of the GP Contract) 7.0 Following an Incident Every incident of violence or aggression should be recorded in a log specifically used for this purpose. This log should contain the following information: Patient ID (eg NHS number) Time and date of incident Nature of incident – particularly the trigger point (eg not able to get appointment) Perspective of staff member dealing with the incident, Names and statement of any witnesses Record of any actions taken 8.0 Staff Support The member of staff who was subjected to the violence or aggression will need support, even though they may not recognise this fact immediately. The way this support is handled can often make the difference to the way the staff member is able to deal with what has happened, with minimal adverse effects. The following process should take place as soon as possible after the incident: The Practice Manager should have a one-to-one discussion with the staff member, in private and as informally as possible (if the Practice Manager is the person affected, then a GP or Practice Nurse should do this) The staff member should be encouraged talk about the incident from their perspective, and encouraged to write it down (this is the best time to complete the incident log) Ask the staff member what support they feel they need to help them deal with the situation If the staff member feels they need counselling, then provide this as soon as possible, either within the practice if there is a trained counsellor, or by referral to the appropriate service If the person affected is not employed by the practice (e.g a Health Trainer) then inform their line manager immediately after the incident 9.0 When a Violent Patient Joins the Practice Because of the length of time it takes for patient notes to come from LaSCA, it is possible that a new patient could join the practice, and only after several weeks would you discover that they have been violent in a previous practice. In the event of this happening, it is advisable to write to the patient, to notify them that you are aware of the previous incident, and that if there is any instance of violence or aggression within your own practice, then the patient would be removed from the list. (see app 3) 10.0 Governance Arrangements This policy will be approved by the Practice Manager. The Practice Manager will be responsible for notifying all staff of the process, ensuring all staff has up to date copies of the document and that the staff are following the processes documented within. This policy will be reviewed 2 years from the date of publication Appendix 1 Dr Alison L Lyon MB. CH.B. M.R.C.G.P. FPA Dr C J Earnshaw MB. CH.B.D[OBST] RCOG Dr R L Swann MB. CH.B Dr Eve Haworth MB. CH.B DCH DRCOG M.R.C.G.P. Tel: Dr F Thagia MB.CH. B DRCOG M.R.C.G.P 1st Floor, Lever Chambers Centre for Health Ashburner Street, Bolton BL1 1SQ Tel: 01204 462630 Fax: 01204 462636 Dr A. Lyon & Partners Our Ref: ALL/AMG/STW Date: In Confidence To: Dear On your visit to the surgery on ...................., you were ..................................................... We feel we must inform you that this behaviour is unacceptable. It is our responsibility to point out to you that we have a zero tolerance policy across the NHS for patients who are abusive and/or violent to staff. At Dr Lyon & Partners we take this policy very seriously, and would not hesitate to remove patients from the list who do not abide by this policy. We are happy for you to remain with the practice, but insist that you abide by the above mentioned policy in all your dealings with the practice. We hope you understand that should such poor behaviour occur again, we will have no alternative other than to exercise our right to remove you from our List Yours sincerely, Dr. A. Lyon & Partners Dr Lyon & Partners Telephone: 462630 Web:www.boltondoctors.co.uk Please look us up at www.nhschoices.net Appendix 2 Dealing with a violent or aggressive patient if the patient is in the consulting room with a clinician requires a much more immediate response. As soon as a patient turns violent, then the correct procedure should implemented and immediate action must be taken, as follows: If possible the Clinician should proceed to the door of the consulting room as request assistance from reception staff. If unable to get to the door, press the panic button immediately A member of staff must immediately respond to the clinic room to provide assistance Another member of staff should call security to aid the removal of the patient from the premises Phone the police. Once violence occurs, it becomes a crime. If there are other patients in the vicinity, then there is a duty to protect them. If possible remove other patients in the vicinity to another part of the waiting area or another room away from the situation. Following an incident of violence, the practice should hold a significant event meeting to decide if the patient should be removed from the list. If the patient is to be removed from the list, then the practice should now follow the procedure for the removal of patients. Following the incident, the main points should be recorded on a significant events form All incidents of violent and aggressive behaviour should be reported to the Practice Manager Appendix 3 Dr Alison L Lyon MB. CH.B. M.R.C.G.P. FPA Dr C J Earnshaw MB. CH.B.D[OBST] RCOG Dr R L Swann MB. CH.B Dr Eve Haworth MB. CH.B DCH DRCOG M.R.C.G.P. Tel: Dr F Thagia MB.CH. B DRCOG M.R.C.G.P 1st Floor, Lever Chambers Centre for Health Ashburner Street, Bolton BL1 1SQ Tel: 01204 462630 Fax: 01204 462636 Dr A. Lyon & Partners ALL/AMG/STW Date …………………………… In Confidence To: ………………………………… …………………………………….. Dear Thank you for registering with Dr A. Lyon & Partners We are now in receipt of your full medical records. We note, from these records, that you have a history of abusive and/or violent behaviour at your previous practice. It is my responsibility to point out to you that we have a zero tolerance policy across the NHS for patients who are abusive and/or violent to staff. At Dr Lyon & Partners we take this policy very seriously, and would not hesitate to remove patients from the list who do not abide by this policy. We are happy for you to remain with the practice, but insist that you abide by the above mentioned policy in all your dealings with the practice. If you wish to discuss this matter further, then please do not hesitate to contact me. Yours sincerely Anne Grundy Practice Manager Practice Manager – Anne Grundy AMSPAR[DIP] Member of Institute Healthcare Management (MIHM) Direct Tel: 01204 462644 E.mail: anne.grundy@nhs.net Web. www.boltondoctors.co.uk Appendix 4 Removals from the list of patients who are violent 202. Where the Contractor wishes a patient to be removed from its list of patients with immediate effect on the grounds that: 202.1. the patient has committed an act of violence against any of the persons specified in clause 203 or behaved in such a way that any such person has feared for his safety; and 202.2. it has reported the incident to the police, the Contractor shall notify the PCT in accordance with clause 204. 203. The persons referred to in clause 202 are: 203.1. if the Contract is with an individual medical practitioner, that individual; 203.2. if the Contract is with a partnership, a partner in that partnership; 203.3. if the Contract is with a company, a legal and beneficial owner of shares in that company; 203.4. a member of the Contractor’s staff; 203.5. a person employed or engaged by the Contractor to perform or assist in the performance of services under the Contract; or 203.6. any other person present on the practice premises or in the place where services were provided to the patient under the Contract. 204. Notification under clause 202 may be given by any means including telephone or fax but if not given in writing shall subsequently be confirmed in writing within seven days (and for this purpose a faxed notification is not a written one). 205. The PCT shall acknowledge in writing receipt of a request from the Contractor under clause 202. 206. A removal requested in accordance with clause 202 shall take effect at the time the Contractor makes the telephone call to the PCT, or sends or delivers the notification to the PCT. 207. Where, pursuant to clauses 202 to 206, the Contractor has notified the PCT that it wishes to have a patient removed from its list of patients, it shall inform the patient concerned unless: 207.1. it is not reasonably practicable for it to do so; or 207.2. it has reasonable grounds for believing that to do so would be harmful to the physical or mental health of the patient or would put at risk the safety of one or more of the persons specified in clause 203. 208. Where the PCT has removed a patient from the Contractor’s list of patients in accordance with clause 206 it shall give written notice of the removal to that patient. 209. Where a patient is removed from the Contractor’s list of patients in accordance with clauses 202 to 208, the Contractor shall record in the patient’s medical records that the patient has been removed under this paragraph and the circumstances leading to his removal. GP Safehaven (Violent Patient) Scheme Risk Assessment CLIENT NAME DATE DATE OF BIRTH____________ NHS NO___________________ ADDRESS_____________________________________________________________________ Information sources available/accessed in completing Risk Assessment (tick all sources used and state whom) Patient Case notes Carer/relative Other Specify Specify Reason for referral onto the scheme. Name of present GP Contact Number of referring person Reason for referral Name of person making referral Section 1: Suicide. a) Does the professional consider the individual at risk of suicide? Yes/No b) Is there a history of suicide attempts? Yes/No Section 2: Self Harm. a) Does the professional consider the individual at risk of intentional self-harm? Yes/No b) Is there a history of intentional self-harm? Yes/No Section 3: Harm to others. a) Does the professional consider the individual at risk of harming others? Yes/No b) Is there a history of harm to others? Yes/No c) If yes please provide more information Section 4; Substance Misuse. a) Is there evidence of substance misuse? Yes/No b) Is there a history of substance misuse? Yes/No c) Does the professional feel the level of misuse warrants concern for the safety of the individual or others? Yes/No d) If yes to ( c ) please explain further: Section 5: Social circumstances. a) Does the professional feel any of the social circumstances or medical conditions warrant concerns for the individual’s safety? Yes/No b) Have any social circumstances or medical conditions led to deterioration in the past? Yes/No Section 6: Neglect. a) Does the professional consider the individual is at risk of neglect by self or others? Yes/No b) Is there a history of neglect (emotional, physical, mental)? Yes/No Section 7: Treatment related indicators. a) Does the professional consider the individual is at risk of not complying with treatments/services? Yes/No b) Is there a history of not complying with treatment/services? Yes/No Section 8: Risk to staff. a) Does the professional consider that there are any risks involved in the individuals care? Yes/No b) Is there a history of risk to staff? Yes/No Please provide any further relevant information Reviewed By____________________________ Completed by Designation Date Primary Care Support Services (Preston Office) Incident Report Form Please use this form for the removal of a patient following a violent incident towards a GP, a member of staff or a patient. The incident must be reported to the police and the police incident log number must be stated on this form. Without this number, immediate removal is not possible under the regulations for violent patient removal. Practitioner’s name: Practice address: Practice contact number: Patient’s name: Patient’s NHS number: Date of birth: Patient’s address: Date of incident: Time of incident: Police incident log number: Location of incident: (Patient’s address/Surgery etc) Date obtained: Type of incident (please tick the appropriate box) Non physical violence i.e. intimidation, abuse, threats etc Physical Violence Vandalism to: Aggravated Physical Violence e.g. use of weapons Premises Vehicle Approximate cost of damage (optional): £ Assault to: (please tick the appropriate box) GP/Dentist Verbal Staff Verbal Other Patient(s) Verbal Physical Physical Physical Please supply brief details of the incident GP signature (actual signature must be provided): ****E-mail completed form to: lasca.registrations@nhs.net or fax to 01772 221447**** Info 4 Dr A Lyon & Partners Policy on Removing Patients from the Practice List REVISED September 2011 Dr A. Lyon & Partners POLICY ON REMOVING PATIENTS FROM PRACTICE LIST PURPOSE The surgery aims to provide the best possible health care for its patients. However there may be circumstances when it would be considered reasonable, or in the best interests of the patient, to remove patients from the list. The purpose of this policy, therefore, is to define the practice guidelines for when it is reasonable to remove a patient from the practice list and to ensure that any concerns about removing patients from the list are dealt with fairly. SITUATIONS WHICH JUSTIFY REMOVAL VIOLENCE DISTANCE EMBARKATION DEATH FAILURE TO ATTEND PRE-BOOKED APPOINTMENTS IRRETRIEVABLE BREAKDOWN OF THE DOCTOR-PATIENT RELATIONSHIP UNDELIVERED MAIL CRIME & DECEPTION DEFINED AS VIOLENCE DEFINED AS When a patient:Is physically violent or threatening towards a doctor, practice staff or other patients on the practice premises. Causes physical damage to practice premises or other patient’s property Gives verbal abuse or makes threats towards the doctor, practice staff or other patients Gives racist abuse, orally or physically Is violent or uses or condones threatening behaviour to doctors [or some other members of the primary health care team] while visiting the patient’s home. Such behaviour may involve the patient, a relative, a household member, or pets [such as unchained dogs]. Where a patient: Fraudulently obtains drugs for non-medical reasons Deliberately lies to the doctor or other member of the primary health care team [e.g. by giving a false name or false medical history] in order to obtain any service or benefit by deception Attempts to use the doctor or conceal or aid any criminal activity Steals from practice premises /2 Policy on removing patients from practice list cont… DISTANCE DEFINED AS Where a patient has moved out of the designated practice area and has failed to register with another GP EMBARKATION DEFINED AS Where a patient has moved abroad for a period of 3 months or more FAILURE TO ATTEND PRE-BOOKED APPOINTMENTS DEFINED AS Where a patient fails to attend pre-booked appointments on a number of occasions during a given period IRRETRIEVABLE BREAKDOWN OF THE DOCTOR-PATIENT RELATIONSHIP DEFINED AS Where a patients behaviour falls outside of that which is normally considered reasonable and leads to an irretrievable breakdown of the doctor-patient relationship UNDELIVERED MAIL IS DEFINDED AS Letters returned to the practice by royal mail or occupant from the address which mail has been sent but the addressee is no longer resident. PROCEDURE FOR REMOVAL VIOLENCE/CRIME AND DECEPTION Any incident involving violence, crime or deception will be reported to the practice manager who will complete an incident report and bring to the attention of the practice partners Each individual case will be discussed at a practice meeting and a majority agreement will be reached Following agreement, the practice manager will write to the patient and explain the reasons for removal DISTANCE On notification that the patient is no longer living within the practice boundary, the patient is usually informed verbally that they will require to register at a new surgery in their area. The change of address is completed on Vision and the Health Authority notified to deduct the patient. EMBARKATION On notification that the patient has moved abroad the patient will be removed from the practice list within 3 months of that notification FAILURE TO ATTEND PRE-BOOKED APPOINTMENTS If a patient fails to attend 2 pre-booked appointment on more than one occasion in the last year, a warning letter will be sent to the patient, advising them that a further occurrence could risk removal from the practice. If the patient fails to attend another appointment, the matter will be discussed at a Practice Meeting and a majority agreement will be reached as to whether the patient will be removed from the practice list. Following agreement, the practice manager will write to the patient and explain the reasons for removal. GUIDELINES ON REMOVING PATIENTS DUE TO IRRETRIEVABLE BREAKDOWN OF THE DOCTOR-PATIENT RELATIONSHIP Occasionally patients persistently act inconsiderately and their behaviour falls outside that which is normally considered to be reasonable. In such circumstances the practice may consider there to be a complete breakdown in the doctor-patient relationship. Steps taken within the practice All appropriate members of the practice will be informed about the problem The patient and possible reasons for their behaviour [i.e. disagreeableness, cultural differences, mental illness, personality disorder] will be discussed at a Practice Meeting Steps to be taken with the patient The practice will inform the patient, either personally or in writing, that there is a problem, explain the nature of the problem to the patient obtain the patient’s perspective and interpretation of the situation. If necessary the practice will obtain the advice of a Medical Defence Society . If discussion fails to resolve the problem, the practice may suggest that another GP within the practice might better fit with the patient’s needs and expectations Removing the patient when necessary The practice will inform LASCA in writing of the decision (See appendix A) Inform that patient in writing of the decision and the reason for removal from the list (see Appendix B) Explain to the patient that he/she will not be left without a GP Give the patient information on how to begin the process of registering with another GP FAMILY MEMBERS The decision to remove family members/extended family members of the patient removed may be made if necessary. The practice will write to the family/patients concerned explaining the reason for removal and allowing them 4 weeks to re-register with another practice rather than removing them from the list immediately RESPONSIBILITY for implementing and monitoring the policy will rest with the Practice Partners/Practice Manager The Partners at the surgery re-affirm their commitment to do everything possible to protect staff, patients and visitors from unacceptable behaviour and their zero tolerance of any incident that causes hurt, alarm, damage or distress. Appendix A Dr Alison L Lyon MB. CH.B. M.R.C.G.P. FPA Dr C J Earnshaw MB. CH.B.D[OBST] RCOG Dr R L Swann MB. CH.B Dr Eve Haworth MB. CH.B DCH DRCOG M.R.C.G.P. Tel: Dr F Thagia MB.CH. B DRCOG M.R.C.G.P 1st Floor, Lever Chambers Centre for Health Ashburner Street, Bolton BL1 1SQ Tel: 01204 462630 Fax: 01204 462636 Dr A. Lyon & Partners Date: Patient Data Department Lancashire & South Cumbria Agency (LaSCA) 3 Caxton Road Fulwood Preston PR2 9ZZ Dear Colleagues, Please remove the patient’s detailed below from our List with immediate effect due to________________________________________________________________. Name Address Date of birth Yours sincerely, Dr Alison Lyon Dr Richard Swann Dr Christopher Earnshaw Dr Eve Haworth Dr Ferjana Thagia Medical Secretary – Sharon Telephone 462630 Ext: 7050 – Fax 462636 Email: sharon.wilmot@nhs.net Web:www.boltondoctors.co.uk Please look us up at www.nhschoices.net NHS Number Appendix B Dr Alison L Lyon MB. CH.B. M.R.C.G.P. FPA Dr C J Earnshaw MB. CH.B.D[OBST] RCOG Dr R L Swann MB. CH.B Dr Eve Haworth MB. CH.B DCH DRCOG M.R.C.G.P. Tel: Dr F Thagia MB.CH. B DRCOG M.R.C.G.P 1st Floor, Lever Chambers Centre for Health Ashburner Street, Bolton BL1 1SQ Tel: 01204 462630 Fax: 01204 462636 Dr A. Lyon & Partners Our Ref: Date: In Confidence To: Dear Unfortunately due to events which have taken place recently at the surgery, namely your aggressive manner and inappropriate behaviour i.e. _____________________________, leading to the irrevocable breakdown of communication and breach of trust between yourself and the Practice, we feel we have no alternative other than to remove you from our List and ask you to find another doctor. You have been issued with enough medication until you register with a new Gp. The Health Authority will contact you about finding another Practice to register with. The Health Authority Patient Services Department can be contacted on 01772 221 444. Yours sincerely, Dr Alison Lyon Dr Richard Swann Dr Christopher Earnshaw Dr Eve Haworth Dr Ferjana Thagia Dr Lyon & Partners Telephone: 462630 Web:www.boltondoctors.co.uk Please look us up at www.nhschoices.net