Ultrasound of the Gastrointestinal Track and Pancreas
advertisement

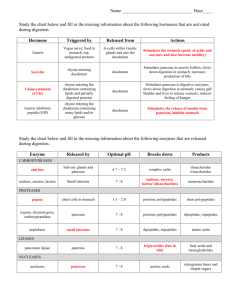
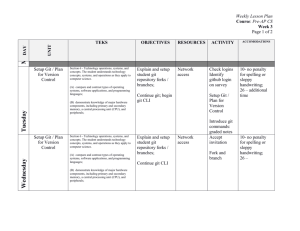
Ultrasound of the Gastrointestinal Track And Pancreas Alain Giroux, DVM, MSc, DACVR Introduction Ultrasound evaluation of the gastro-intestinal tract (GIt) is often underestimated in its value. Very useful and diagnostic information can be obtained with careful scanning. Evaluation of the Git is often forgotten since in most case it contains gas, which causes acoustic shadowing artifacts, and with the exception of the stomach and colon, the intestines are well spread throughout the abdomen. Evaluation of the pancreas is a more difficult task because if normal, it is not well seen, without a high frequency transducer. The following is a review of the anatomy, which is crucial for complete evaluation of the abdomen and will describe the appearance of common disease processes. Anatomy of the GIt The stomach easy to identified (Fig. 1GIT). It is oriented perpendicular to the spine and just caudal to the liver. The different portions of the stomach are not demarcated by specific ultrasound characteristics. However a general idea of the structure affected can be given. The caudal esophagus enters the stomach thru the cardia. The fundus of the stomach is located on the left side of the abdomen and is more dorsal than the pylorus. The body of the stomach connects the fundus and pylorus. The pylorus is located on the right of the mid line in dogs and near the midline in cats. The pylorus empties in the proximal transverse duodenum. The duodenum has a proximal portion (perpendicular the spine), which terminates at the cranial duodenal flexure where the descending portion starts. The descending duodenum runs paralleled to the spine on the right side in dogs, and close to the mid-line in cats. The descending duodenum can be found, in most cases, lateral and ventral to the right kidney in dogs, and in frequently, it is the only bowel located lateral to the kidney. As the duodenum reaches the level of the right kidney, it becomes medial to the caudal pole of the right kidney and continues to the caudal flexure before forming a short ascending segment. In cats, the descending duodenum generally runs medial to the right kidney in its entirety. It is often just slightly dorsal t the ascending colon. In ideal conditions, the entire canine duodenum can be followed ultrasonographically from the stomach to its junction with the jejunum. The colon (Fig. 2.GIT) has three portions that can be identified: ascending, transverse and descending portion. It can be difficult to follow the colon when it does not contain fecal material and gas. The transverse colon may be the easiest to see as it runs parallel and caudal to the stomach. The descending colon is normally medial to the left kidney and can be on the right or left side of the urinary bladder as it enters the pelvic canal. In general, it is dorsal and on the left side of the urinary bladder. The pancreas (Fig .1.GIT) is divided in right limb, body and left limb. Again the different portions are not demarcated with ultrasound but their location can give a general idea of the portion affected. The right limb of the pancreas lines the medio-dorsal aspect of the duodenum. It often extends along the entire descending duodenum length. The body of the pancreas is medial, caudal and dorsal to the cranial flexure of the duodenum, and is sometime easier to identify by scanning the ventral aspect of the extrahepatic portal vein. The left limb of the pancreas is located in the caudo-dorsal aspect of the stomach and perpendicular to the spine. It is located in between the stomach and colon. In some cases the left limb of the pancreas extends to the left side where it is in close contact with the cranial aspect spleen. 1 Figure 1.GIT: Stomach, Duodenum And Pancreas Anatomy: Ventral View Adapted from Miller’s anatomy of the dogs, 1967, second edition. Pancreas: Body (B) Right limb (RL) Left Limb (LL) Figure 2.GIT: Anatomy of the Colon Colon: Ascending (AC) Transverse (TC) Descending (DC) 2 Ultrasound Git Anatomy: The stomach normally has a round appearance with shadowing artifact when the transducer is oriented sagitally. Its dorsal aspect may not be seen if it contains gas or ingesta but will be visualized if the gastric lumen contains fluid or is empty. The pylorus can be visualized as it connects to the proximal duodenum. The duodenum (in dogs) is identified by obtaining a transverse view of the right kidney and scanning the lateral aspect of the kidney. It can be follow cranially and caudally. Its most proximal portion can be difficult to see. The duodenum can also be seen with a sagittal orientation and by fanning lateral to the right kidney. The duodenum is often more prominent when compared to the rest of the small bowel due to the slightly thicker wall (mostly thicker mucosa). The rest of the small bowel is seen throughout the abdomen. The colon is identified by its consistent gas filled appearance. Here are the criteria for evaluation of the stomach and intestine: 1-Thicknes and symmetry of each wall 2-Integrity of the layers 3-Luminal content and size (subjective) 4-Motility 5-Orientation and location 6-Shape and contour 7-Integrity of nearby lymph nodes The thickness of the stomach and intestines vary from species and location. Table 1.GIT describes the measurements used for evaluation. The thickness of one wall should not include the lumen, and should be measured from the inner margin of the mucosa to the outer margin of the serosa. A description of how to measured the wall is presented in figure 3.GIT. It is important to measure the walls of multiple GI structures in patients with clinical signs associated with the Git. Table 1.GIT: Normal Thickness of the Git in Dogs and Cats: Figure 3.GITt: Measurements of the Git Layers Dog: Stomach: less than 5mm Duodenum: less than 5mm Jejunum, ileum and colon: less than 4 mm Cat: Stomach: less than 4mm Duodenum: often less than 4mm Jejunum, ileum and colon: often less than 3 mm 3 Git Ultrasound Identification: The stomach and small bowel layers are fairly easy to identify. Each wall as four layers and the lumen is considered a fifth layer. The colonic wall layers can only be well seen in ideal condition. The ultrasonographic appearance of the Git layers are described in table 1.GIT and are identified in the figure 4.GIT and figure 5.GIT. It is important to try to identify the layers in diseased bowel since neoplastic processes, especially carcinoma and lymphoma, will have poor visualizations of the layers. Table 2.GIT: The Git Wall Layers and Respective Echogenicity From inner layers to outer layers: Mucus\lumen content Echogenecity: Hyperechoic unless only fluid (hypoechoic) Mucosa Hypoechoic Sub-mucosa Hyperechoic Muscularis Hypoechoic Serosa Hyperechoic Figure 3.GIT: Intestinal Layers: Sagital View Figure 4.GIT: Intestinal Layers: Transverse View 4 Git Ultrasound Identification: The luminal contents can be difficult to characterize. However, with experience, ultrasound can become a great tool to identify foreign bodies, or mostly the obstruction they cause. However, in regards to their direct visualization, intra-luminal foreign bodies can have similar appearance to focal gas accumulation. Obstruction especially due to cancer, or intussusceptions can be diagnosed with ultrasound by the appearance of the walls and of the lumen. The normal size of the lumen is more difficult to define and is partially subjective. The dilatation of the suspicious intestinal segment should be compared with the size of other segments and should prompt evaluation for obstructive disease and lymph node enlargement. The motility of the stomach and small bowel can be evaluated in perfect condition when patient is fairly still. The gastric peristaltism is normally 3 to 5 contractions per minutes. Disease affecting the stomach and small bowel may increase or decreased the peristaltism. If a patient is quite stressed, or if sedatives are utilized, the peristaltism can be decreased. The orientation and location of the Git can be altered by nearby abnormal structure such as splenic and hepatic enlargement. The shape and contour of the intestines can be affected by direct or indirect disease. It can appear corrugated and tortuous. For example, in pancreatitis involving the right limb of the pancreas, the duodenum may have an accordion appearance due to focal inflammation The normal pancreas is isoechoic to the mesenteric fat and cannot be seen unless high a frequency transducer is utilized. However, its location, as described in the anatomy review, should be evaluated for potential disease. The pancreatic duct can be seen frequently in cats and on some occasions in dogs, it is reported to be less than 2 mm in diameter when normal. Here are some criteria’s of evaluation for the pancreas: 1-Parenchymal echogenicity and contour. 2-Surrounding mesentery echogenicity 3-Fluid in the peritoneum 4-Integrity of the pancreatic duct and vessels. 5-Integrity of the biliary system 5 Abnormal Git: Abnormal stomach and intestine are often noted by changed in wall thickness and lumen size and content. For example, seeing fluid in the colon is indicative of abnormal function, possibly from a specific disease. With neoplastic process, the layers of the bowel are often not identified, and the thickness of the wall is asymmetrical. In diffuse inflammatory process, the walls may be only slightly thickened and the layers still can be seen. Lymphoma can cause diffused thickening with partial layers visualization. The pancreas can have a hypoechoic appearance in acute pancreatitis. The surrounding mesentery may be hyperechoic and fluid may be seen, due to focal peritonitis The stomach and duodenum, and sometimes the ascending and transverse colon may be thickened or have and irregular shape (corrugation) due to focal inflammation. In more chronic pancreatic disease, the pancreas may be hyperechoic to the mesentery or more often slightly hypoechoic, without mesentery change in echogenicity. Pancreatic cancer often has a nodular appearance with mixed echogenicity and absence of pain on transducer pressure Here is a list and some ultrasounds images of the most common diseases Abnormal Stomach Figure 5.GIT: Gastric Ulcer -Benin\Inflammatory Disease: -Pyloric hypertrophy -Gastritis (Fig. 6a and 6b.GIT) -Leiomyoma -Autoimmune -Ulcers (Fig. 5.GIT) -Neoplastic Infiltrate: Lymphosarcoma Adenocarcinoma Leiomyosarcoma Mast cell tumor Other uncommon neoplasms Metastatic neoplasms Abnormal -Infectious: -Viral, parasital bacterial gastritis Figure 6a.GIT: Focal Fundic Gastritis: Transverse View Figure 6b.GIT: Focal Gastritis: Normal Portion for Comparison: Transverse View 6 Figure 7.GIT: Small Intestine Lymphoma Abnormal Small and Large Intestine: -Benin\Inflammatory Disease: -Enteritis -Leiomyoma -Autoimmune;IBD (Fig. 8.GIT) -Lymphangiectasia -Ulcers -Neoplastic Infiltrate: -Lymphosarcoma (Fig.7.GIT) -Adenocarcinoma (Fig 9, 10, 11.GIT) -Leiomyosarcoma -Other uncommon neoplasms -Metastatic neoplasms -Infectious: -Viral, parasital, bacterial enteritis -Chronic non-active lesion (Fig. 13.GIT) -Cyst Figure 8.GIT: IBG: Sagital View Figure 9.GIT: Carcinoma and Lymph Node Enlargement 7 Figure 10.GIT: SI Carcinoma: Transverse View Figure 11.GIT: SI Carcinoma: Transverse View Abnormal Pancreas: -Benin Disease: -Neoplastic Infiltrate: -Adenocarcinoma (Fig. 14.GIT) -Insulinoma -Other uncommon neoplasms -Metastatic neoplasms -Infectious\Inflammatory: -Acute pancreatitis (Fig. 12.GIT) -Sub-acute pancreatitis -Abscess -Cyst Figure 12.GIT: Acute Pancreatitis 8 Figure 13 GIT: Chronic Active Pancreatitis: Right Limb Transverse View Figure 14 GIT: Pancreatic Carcinoma: Right Limb Sagital View 9
![[#MODULES-1201] spec helper cannot check out git branches](http://s3.studylib.net/store/data/008555300_1-880f0225968435214e13ca807252de3e-300x300.png)