Document
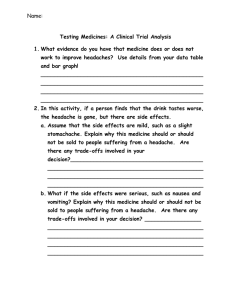
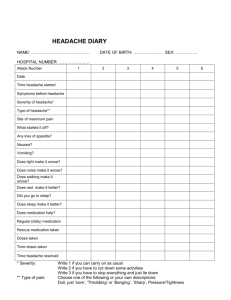
advertisement

神經內科標準病歷範本 I. Cerebral vascular accident Present Illness: A man aged 62 had sudden left arm and leg weakness and slurred speech. Except for untreated hypertension, his medical history was unremarkable. He is a smoker with a 45 pack-year smoking history. On arrival at the emergency department 1 hour 15 minutes after the symptom onset, he reported no headache or vomiting. His blood pressure was 180/100 mm Hg; his pulse, 76 beats/min and regular. Neurologic examination examined dysarthria, a left homonymous hemianopia, severe left-sided weakness; bilateral palpation, no left sided body response (left tactile extinction). Ⅱ. Seizure Present Illness: This man aged 70 had 2-year R’t cerebral infarction with mild left hemiparesis but lived independently. His wife witnessed that he had left arm seizures after four-limb convulsions for about 2 minutes with upward gaze, trismus and grimacing with cyanosis. After the seizing, he effortfully breathed and was unresponseive to others’ voice until the ambulance arrived in about 8 minutes. Ⅲ. Foot drop Present Illness: A 35-year-old man without systemic diseases visited our neurologic clinic because the intermittent right lower leg tonic posture, following clonic twitching 1 minute, occurred several times since September 2001. Resultanltly, the right leg weakness lasted for several minutes. One week prior to an outpatient clinic relentless right foot weakness was observed. The neurologic examination evinced intact mentality, cranial nerves and sensory 1 function. The four-limb muscle strength was normal except right ankle dorsiflexion weakness which was Medical Research Council-rated 4. The deep tendon reflex, representing the ankle jerk, was symmetric; bilateral plantar flexion, perceived by eliciting the plantar reflex. He could walk over to the right on his tiptoes but not on his heels. Ⅳ. Diplopia and blurred vision Present Illness: This man aged 54 years and of blurred vision, dizziness, and visual defects two months before admission experienced double vision, headache, and photophobia one month later despite our neurologic outpatient department-prescribed medications. The patient was neurologically indicated impaired left visual acuity, left conjunctival chemosis, left eyelid swelling, left eye proptosis, and complete oculomotor palsy, and left trochlear and abducens nerves. His pupils exposed isocoria. The visual fields were full. The sensation was slightly trimmed in the left trigeminal nerve ophthalmic branch. The left corneal response was marred, consistent with a left trigeminal nerve abnormality. There were no: facial palsy; hearing impairment; tinnitus; dysphagia; uvula and tongue deviation. Ⅴ. Headache Present Illness: A 32-year-old woman without migraine or other chronic headache history until two weeks prior to the admission accounted nausea- and vomiting- accompanied intermittent severe throbbing headache in her bilateral occipito-temporal regions, beside the headache intensity often increasing upon awakening, bending forward or abdominal straining. There was no photophobia, phonophobia, tinnitus, monocular or 2 binocular visual loss, dilopia, fever, orthostatic edema, neck stiffness, arthralgia, or ataxia or other focal neurologic symptom. This patient took regular medication and had no relevant medical history except danazol 600 mg taken daily for endometriosis 6 months ago and most notably discontinued 20 days prior to admission. Ⅵ. Progressive dysarthria and dysphagia Present Illness: The 47-year-old non-diabetic of nasopharyngeal carcinoma (NPC) 20 years ago received complete cobalt radiotherapy and experienced no recurrence. About 6 months prior to admission, the persistent deep-seated headache over the right frontotemporal and maxillary regions happened; so did subsequently progressive dysarthria and dysphagia. The serial examinations by otolaryngologists averred a thickened posterior pharyngeal wall; The biopsy, only chronic inflammation. No culture was acquired at that time. One week prior to admission, the left hemiparesis suddenly started. On the examination, he was alert and reported a distressing headache. The blood pressure and body temperature were normal. The multiple cranial nerve lesions were manifested. There were right eye ptosis and miosis. His dysarthric speech was with a nasal tone. His dysphagia was severe; naso-gastric tube, for feeding. A plain protuberant posterior pharyngeal wall was perceived. The right side gag reflexes were spoiled and the right posterior tongue sensation was lost. The tongue deviated to the right when extended. No external auditory canal granulation tissue was avowed. Ⅶ. Motor neuron disease Present Illness: This computer-programming engineer aged 37 years denied any systemic disease 3 or previous regular medications. He noted intermittent face and bilateral arms twitching in recent 3 years and an insidious onset leg weakness exacerbated in recent one year causing difficulty climbing stairs. Occasionally, he also felt both posterior thigh numbness and prolonged speaking-stimulated nasal tones. These symptoms did not occur at a particular timing or show a diurnal change. They developed insidiously but appeared aggravated increasingly, so he came to our hospital for check up. Ⅷ. CNS infection Present Illness: The Taiwanese man aged 30 who studied in Berlin, Germany and had five day fever and generalized weakness visited our infectious disease clinic. Laboratory data (complete blood count with differential and chemical analysis) and urinalysis were within normal limits, and so was chest X-ray. He was admitted to the infectious disease ward next day. Ceftriaxone, broad-spectrum coverage for suspected salmonellosis, was started. Fever (peak, roughly 38.5°C) with dizziness, vomiting, and neck stiffness waxed and waned during the initial hospital days. Ⅸ. Diabetic cranial neuropathies Present Illness: A woman aged 56 years suffered acute onset left eye ptosis and binocular double vision. Her past DM for five years without known hypertension or hyperlipidemia was notable. Meanwhile, she ingested antihyperglycemic agents and had fasting sugar from 100 to 250 mg/dl. Over the past two years the two transient facial palsy episodes occurred bilaterally, respectively. Additionally, she was once hospitalized for right eye similar ptosis events two months prior to this admission. Paresis over the right medial rectus, superior rectus, and inferior rectus, and equivocally reduced 4 pinprick sensation over the right ophthalmic nerve were recorded. The right oculomotor nerve palsy was diagnosed, which completely resolved one month later. Ⅹ. Unilateral Paresthesia Present Illness: A non-vegetarian aged 74 years with past significant hypertension and diabetes mellitus presented with acute onset right face, arm and leg numbness and tingling. The unilateral paresthesia persisted one day before medical consultation sought. On admission, she was alert and oriented and without fever, meningismus, headache, or head injury signs. Blood pressure was 154/86 mmHg. Neurological examination and basic laboratory test results were unremarkable. 5