1 SUPPLEMENTARY MATERIAL APPENDICES Appendix 1. Early
advertisement

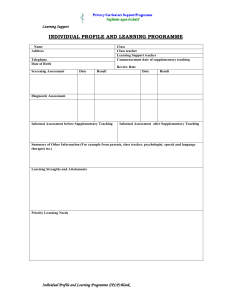
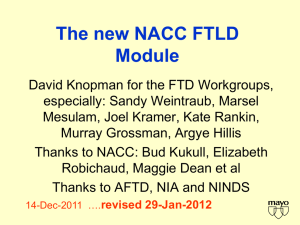
1 SUPPLEMENTARY MATERIAL APPENDICES Appendix 1. Early features SUPPLEMENTARY TABLE LEGENDS Supplementary Table 1. Cases by site Supplementary Table 2. 1998 Consensus criteria for bvFTD (Neary et al., 1998) Supplementary Table 3. First and last clinical diagnoses SUPPLEMENTARY FIGURE CAPTIONS Supplementary Figure 1: Sensitivity of bvFTD criteria by age of onset: (A) Sensitivity of FTDC and 1998 criteria (B) FTDC diagnostic features. Clear bars show percent of cases with early onset (before age 65), black bars show percent of cases with late onset (after 65); * p<.05. Supplementary Figure 2: 1998 criteria supportive features. Frequency is shown as percent of cases in the 1998 criteria sample (clear bars) or the common sample (black bars). 2 Appendix 1 To help establish the optimal duration for criteria involving “early” presentations (i.e., disinhibition, apathy, loss of empathy, perseverative behaviors), raters were asked to provide the timing of symptom onset when available. Table 1 shows symptom onset findings in patients who met criteria for Possible bvFTD and were ascertained for both FTDC and 1998 criteria (n=118). Symptom onset ratings were only available for a subset of these patients. Since FTDC criteria require the presence of 3 or more diagnostic features, a sample of patients with 3 or more symptom onset ratings (n=96) was used to determine the optimal temporal cutoff for fulfillment of Possible bvFTD. Please refer to the subsequent text for information on samples and criteria. Table 1: Symptom onset and temporal fulfillment of criteria for Possible bvFTD (n=118) Cumulative percent by time course (years from onset) Patients 0 yrs with onset 1 yr 2yrs 3yrs > 3yrs (onset) ratings Early disinhibition 92 65 87 93 98 100 Early apathy / inertia 98 70 90 95 97 100 Early loss of empathy 81 49 90 96 100 100 Early perseverative / compulsive 74 42 73 88 97 100 Meet criteria for Possible bvFTD 96 41 83 93 97 100 3 In this sample, “early” symptoms are present in 97-100% of patients within the first three years. Based on these limited observations, a cut-off of 3 years is suggested as a general guideline for the onset of these features. Prospective studies are needed to determine the optimal temporal cut-off for symptom onset and fulfillment of criteria. 4 Supplementary Table 1 Site # Patients Rotterdam 25 Johns Hopkins 23 Mayo 17 Western Ontario 17 UCSF 14 Sydney/Cambridge 14 UCL Institute of Neurology 13 UCSD 11 U Penn 10 UCLA 10 Sunnybrook 7 Northwestern 4 Harvard 4 Munich 3 Lille 2 VU Amsterdam 2 5 Supplementary Table 2 I. Core diagnostic features A. Insidious onset and gradual progression B. Early decline in social interpersonal conduct C. Early impairment in regulation of personal conduct D. Early emotional blunting E. Early loss of insight II. Supportive diagnostic features A. Behavioral disorder 1. Decline in personal hygiene and grooming 2. Mental rigidity and inflexibility 3. Distractibility and impersistence 4. Hyperorality and dietary changes 5. Perseverative and stereotyped behavior 6. Utilization behavior B. Speech and language 1. Altered speech output 2. Stereotypy of speech 3. Echolalia 4. Perseveration 5. Mutism C. Physical signs 6 1. Primitive reflexes 2. Incontinence 3. Akinesia, rigidity, and tremor 4. Low and labile blood pressure D. Investigations 1. Neuropsychology: significant impairment on frontal lobe tests in the absence of severe amnesia, aphasia, or perceptuospatial disorder 2. Electroencephalography: normal on conventional EEG despite clinically evident dementia 3. Brain imaging (structural and/or functional): predominant frontal and/or anterior temporal abnormality III. Supportive features (common to clinical syndromes of FTLD) A. Onset before 65: positive family history of similar disorder in first-degree relative B. Bulbar palsy, muscular weakness and wasting, fasciculations (associated motor neuron disease present in a minority of patients) IV. Diagnostic exclusion features (common to clinical syndromes of FTLD) A. Historical and clinical 1. Abrupt onset with ictal events 2. Head trauma related to onset 3. Early, severe amnesia 4. Spatial disorientation 7 5. Logoclonic, festinant speech with loss of train of thought 6. Myoclonus 7. Corticospinal weakness 8. Cerebellar ataxia 9. Choreoathetosis B. Investigations 1. Brain imaging: predominant postcentral structural or functional deficit, multifocal lesions on CT or MRI 2. Laboratory tests indicating brain involvement or inflammatory disorder such as MS, syphilis, AIDS and herpes simplex encephalitis V. Relative diagnostic exclusion features (common to clinical syndromes of FTLD) A. Typical history of chronic alcoholism B. Sustained hypertension C. History of vascular disease (e.g., angina, claudication) 8 Supplementary Table 3 First diagnosis Last diagnosis n n bvFTD 122 112 AD 26 18 FTD / ALS 13 27 Other 13 5 DLB 2 5 CBS 0 1 PNFA 0 2 PSP 0 2 SD 0 2 Don’t Know 0 2 9 ACKNOWLEDGEMENTS Work undertaken at UCLH/UCL received a proportion of funding from the UK Department of Health’s NIHR Biomedical Research Centres funding scheme. The UCL Dementia Research Centre is an Alzheimer’s Research UK Co-ordinating Centre and has also received equipment funded by Alzheimer’s Research UK. Drs. Fox and Rossor have received support from the NIHR and the MRC; Dr. Warren is supported by a Wellcome Senior Clinical Fellowship. Dr. Piguet is supported by a National Health and Medical Research Council Clinical Career Development Award fellowship (#510184). Dr. David Salmon is supported by NIH grant P50-AG05131. Dr. Black’s research is supported by the Canadian Institutes of Health Research (MT-13129).