Cardio_feb24hypertension

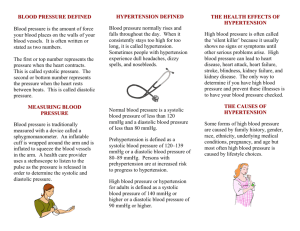
Hypertension
A condition of chronically elevated blood pressure . (Normally defined as a systolic pressure of 140 and/or a diastolic of 90 or above) ( on one more visit within 2 weeks)
The above is used to demonstrate that either excessive fluid or a decrease in the diameter of the vessels may contribute to hypertension.
Left ventricle (myocardial hypertrophy)
Blood pressure
Measures the relationship between cardiac output and the total peripheral resistance
Arterial blood pressure depends on the normal pumping of the heart, the elasticity and resistance of the blood vessels.
Blood pressure rises during left ventricle contraction (highest at systole), falls when heart relaxes (lowest pressure at diastole)
Systolic pressure – indicates greatest pressure in the arterial wall during ventricular contraction. (As blood is ejected from the left ventricle it stretches the blood vessel wall and causes aortic pressure to rise.) ( if the aorta is rigid it cannot accommodate the blood ejected into it)
Influenced by the amount of blood ejected and the elasticity of the blood vessel walls ( systolic pressure increases if the volume of blood increases or blood vessel walls have increased rigidity.)
Diastolic pressure – the resting pressure in the arterial wall. (rises if there is an increase in vascular resistance) (the basis of usuing relaxation massage as a treatment for hypertension to decrease s.n.s. firing which normally causes vasoconstriction)
Influenced by elasticity of arterial walls, the total peripheral resistance and aortic valvular competence
( causes a decrease in diastolic because blood flows back into left ventricle through the regurgative aortic valve)
Pulse pressure – difference between systolic and diastolic. Gives an understanding how well the heart is working. The normal in a resting situation is 35 – 45.
(eg. Normal BP is 120/80; 120 – 80 = 40)
Mean arterial pressure – average pressure in the systemic circulation
- Diastolic pressure + 1/3 rd of pulse pressure
- Main indicator of tissue perfusion ( determines tissue blood flow)
- Normal healthy range is 83 – 93
Blood pressure = CO (cardiac output)
X
TPR (total peripheral resistance)
- TPR = the resistance of all blood vessels downstream of the aorta
- the sum of all elements that resist the flow of blood
Or stated another way:
Blood pressure = SV (stroke volume) X HR (heart rate) X TPR
SV (~ 70 to 80 ml/min) X HR (~ 70 beats/min) = ~4900 ml/min therefore it takes about 1 min for a drop of blood to circumnavigate the body.
Total peripheral resistance is determiend by: Blood vessel diameter (S.N.S &/or blockage), blood viscosity, total blood volume
Cardiac Output indicates the hearts strength as a pump, heart rate and rhythm, venous return.
Measuring Blood Pressure
Cuff pressure is elevated above the clients exprected systolic pressure (usually over 160 mm Hg). This causes collapse of the artery being measured. As cuff pressure is released, a point is reached when the artery becomes open enough for blood to pass through (at the peak of systole) and you will hear ‘tapping’ sounds in your stethascope.
These sounds are known as ‘Korotkoff sounds’; sounds made by blood rushing through compressed but slightly opened vessels.
Korotkoff sounds ‘disappear’ when cuff pressure reaches and becomes less than diastolic pressure. Now, the artery is no longer compressed, and blood flow no longer exerts a perssure against the cuff, eliciting sound.
Systolic pressure is largely determined by stroke volume
Diastolic pressure is largely determined by the health of arteries and arterioles
Venous return
Influenced by the autonomic nervous system – stroke volume decreases as heart rate increases
High sympathetic N.S. – lower S.V.
High parasympathetic – higher S.V. Determinants of stroke volume
Chamber capacity (the amount of blood ejected from each
Strength of heart wall ventricle during each heartbeat)
Sympathetic – increases heart rate
Parasympathetic – decreases heart rate
Tissue need Determinants of heart rate
Changes in venous return (beats/min)
Elasticity of arteries
Arteriolar tone – controlled by H.R.?
Degree of sympathetic N.S. activation Determinants of T.P.R.
To arteriole smooth muscle (the total resistance of all blood
Local tissue chemistry via feed back loop vessels downstream of the aorta)
Blood viscosity
Massage Therapy Influences
Increases venous return
Affect autonomic nervous system, decreases sympathetic nervous response
May increase strength of heart wall in weakened heart ( improves strength and health of heart by allowing more time for perfusion of heart during diastole )
Decreases heart rate
Affects tissue need
Arteriole tone? (same as second?)
Local tissue chemistry (neutralizes pH levels)
Increased parasympathetic response
Decreases blood viscosity (increases fluid return from tissue. Which in turn increase blood plasma and lowers red blood cell concentration - hemodilution
Suggestions :
Place heat (thermaphore) on back (may have to modify or contraindicate depending on extent of CCHF and/or other CV complications)
Start with drainage work on legs
Progress proximally?Start at feet for relaxation then work prox/distal/prox.
Heart rate rises during the first 20 min of treatment (this is normal). If not enough work is done to decrease T.P.R. the heart rate will start to increase as the work load on the heart increases
Heart rate Hypertensive client (if T.P.R is not decreased)
Normal client
0 15 30 45 60 time in minutes
Primary Hypertension (A.K.A. benign, essential)
90 % of hypertensive population
Typical diastolic between 95 – 115
Causes – typically unknown
Common theories:
Overly sensitive sympathetic N.S.
Overly sensitive Renin – angiotensin response
(kidneys react to pressure drop and release hormones that cause systemic vasoconstriction)
Inheritance
Secondary Hypertension
10 % of hypertensive population
Diastolic tends to be higher than in primary
Causes:
-
-
-
-
-
Secondary to known cause
Atherosclerosis
Kidney disease
Liver disease
Respiratory disease
Thyroid and other endocrine disorders
Diabetes
Eclampsia
Primary Hypertension
Morbidity:
60 % die of chronic heart failure
30 % die of cerebral hemorrhage
10 % die of renal failure
Secondary Hypertension
Morbidity
50 % die of renal failure
Rest is equally chronic congestive heart failure and cerebral hemorrhage
Risk factors
Age ( increased rigidity of blood vessels when aging)
Race – increases with African Americans
Alcohol consumption > 3 drinks per day
Stress ( increased s.n.s firing)
? Salt intake? (May not cause hypertension but increases water retention)
Hormonal changes
(women’s blood pressure tends to be lower but after menopause the difference equals out)
(Cardiovascular fitness/exercise level)
Problems/Complications of having hypertension
Increased stress on heart due to/leading to chronic congestive heart failure
Increased stress on kidneys – renal failure
Increased stress on liver – failure of organ
Increased stress on lungs – failure of organ
Increased risk of arteriole rupture (A.K.A. hemorrhagic infarction, often in the brain {i.e. stroke})
Blood vessel damage o High correlation with atherosclerosis o Hyalinization
Addition of more squamous epithelial cells/layers to re-inforce the tissue.
Problems occur with decreased diffusion/transfer across capillary wall, thus increasing the T.P.R {total peripheral resistance}
Decreased elasticity of arteriole walls due to chronic distension o Onion skinning
ONION
SKINNING
Inner wall of blood vessel { lumen } becomes damaged and repairs with scar tissue due to the force of the pressure
Recurrent scar tissue formation following recurrent pressure induced blood vessel wall trauma
Problems with decreased diffusion/transfer
Decreased elasticity of arteriole walls
Decreased tissue health generally
Decreased perfusion, (edema compromises perfusion and drainage)