single point of access protocol - South West Yorkshire Partnership
advertisement

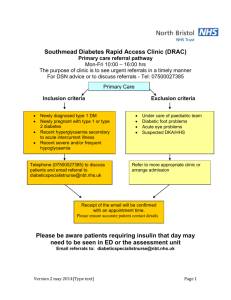
ACCESSING SECONDARY MENTAL HEALTH SERVICES IN CALDERDALE GUIDANCE FOR REFERRERS. 1 SINGLE POINT OF ACCESS (SPA) DIAGRAM 2 AIM AND PURPOSE OF SPA 3 GUIDELINES FOR REFERRERS 4 REFERRAL FORM 5 RANGE OF SPECIALIST MENTAL HEALTH SERVICES PROVIDED BY SWYPFT -1- 1 SINGLE POINT OF ACCESS DIAGRAM Referral SPA Admin 14 day response Urgent WAA/OPS Non-urgent OPS Non-urgent WAA 14 day response Daily Urgent MDT Assessment Daily meeting MDT Response 4 hours CMHT 2 CMHT 1 Memory 2 Memory 1 Point of First Assessment Care Home Liaison Team Acute Hospital Liaison Not approp. Signpost -2- O/P Appt Psych. Appt. Community 2 AIM AND PURPOSE OF SPA South West Yorkshire Partnership NHS Foundation Trust/Calderdale MBC Calderdale Single Point of Access (SPA) Protocol and guidelines The Single Point of Access (SPA) builds upon the existing concept in Older Peoples Services in Calderdale and aims to provide a streamlined service to individuals referred to secondary Mental Health Services. All referrals to secondary Mental Health services will be received and managed by the Single Point of Access. This approach has been developed following wide-ranging discussion with a cross-section of staff who will be involved in ensuring the success of the SPA. The concept has been accepted by Commissioners, Trust Board, Service User Groups, and Carers Groups. Purpose and benefits of SPA Equitability of access for individuals referred. Clarity for referrers. Improved response times for assessment and treatment. Consistency of response. Reduction of multiple assessments. Promoting understanding of resources. Standardised information for service users. Increased service quality and efficiency. Benefits identified accord with those identified regionally and nationally. The SPA will accept ownership of incoming referrals and will not pass enquiries or potential referrers to other departments within the Mental Health Service. Principles of SPA 1. The Single Point of Access will manage all referrals for access to secondary mental health care in Calderdale. 2. The service will operate 24 hours a day (every day of the year). 3. There will be a single phone number for referrers. 4. The referrer will have an opportunity to discuss a referral with a member of the multi-disciplinary SPA team. 5. Referrals will be managed within the Mental Health Service and a response will not be made to the referrer until a decision is made on acceptance for assessment. 6. Links will be maintained with all partners(Commissioning, Local Authority, Service User and Carers Dialogue Groups) -3- 7. Urgent referrals will be screened at the point of entry, and if accepted will be responded to in four hours. 8. Non-urgent referrals will be screened on a daily basis by a Designated Multi-Disciplinary Team which will rotate on a weekly basis. This team will make a decision on allocation for assessment. 9. Internal referrals will be managed within the Mental Health Service and will not be returned to the referrer for actioning. 10. External referrals received at other former referral points eg CMHT, will be sent directly to the SPA and not returned to the referrer to re-direct. Composition of the SPA team All referrals, whether by phone, Safe Haven Fax or letter, will be received by the SPA administrator with access to a SPA clinician as required. The admin worker will be responsible for entering initial demographic information on RIO. Designated Multi-Disciplinary Team The Designated Multi-Disciplinary Team will be responsible for screening all non-urgent referrals on a daily basis. The team will consist of Consultant Psychiatrist, Clinical Psychologist, Team Leader (or staff deputising for team members) and SPA admin. Team leaders/medics will be allocated on a weekly basis from the community teams. Service principles All urgent referrals accepted should be seen within four hours. All non-urgent referrals accepted should be seen within 14 days. A letter will be sent to the referrer informing them of the outcome of the daily MDT within 4 working days. Referrals will be reviewed on a monthly basis by the mental health management team. The SPA will be reviewed 3 months after commencement -4- 3 GUIDELINES FOR REFERRERS South West Yorkshire Partnership Foundation Trust/Calderdale MBC Referring individuals to secondary Mental Health Services in Calderdale To progress the development of secondary mental health services in Calderdale, a Single Point of Access (SPA) for all new referrals to Working Age Adults and Older People Services commenced on 2nd April 2012. The SPA will provide equitability of access for individuals through a clear pathway for referral agencies. This system will reduce the number of referral routes and provide a consistent response to referrers – effectively a “one-stop shop”. Single Point of Access The SPA will operate 24 hours a day every day of the year. All referrals both urgent and non-urgent will be received at the SPA and will be triaged to the appropriate service. Urgent referrals Urgent referrals will include Mental Health Act Assessments and police enquiries. Urgent referrals will be received by telephone or Safe Haven Fax. When accepted for assessment, urgent referrals will be seen within four hours. If not accepted for assessment, a discussion will take place with the referrer and advice will be given as to the best way of helping the service user. Non-urgent referrals It is requested that non-urgent referrals are made in writing or sent to Safe Haven Fax using the referral form. The referrals will be discussed daily (Monday to Friday) by a senior clinical team comprising Consultant, Psychologist, Team Leader and SPA clinicians. If accepted by the service, referrals will be allocated for initial assessment: o Initial assessment clinic - 14 days o Initial assessment Insight - 14 days o Initial assessment AOT – 14 days o Psychology - 14 days o Outpatient clinics – 14 days -5- If one of these options is not possible due to the individual’s disability, arrangements can be made for the person to be seen at home or other venue by arrangement. Please contact the SPA if you would like a discussion about the individual referred to us. Those referrals not accepted will be signposted to another service or returned to you with appropriate advice. A referral form is attached for your use. A letter will be sent to referrers advising of the outcome of the referral within 4 working days. A member of the SPA team may also contact you by phone to discuss the outcome. Single Point of Access (SPA) Phone 01422 222888 Safe Haven Fax Address 01422 222881 Willowdale The Dales Salterhebble Halifax HX3 0PW. -6- 4 REFERRAL FORM SINGLE POINT OF ACCESS TO SECONDARY MENTAL HEALTH SERVICES IN CALDERDALE REFERRAL FORM Date of referral………………………………………………………………………………………….. Referred by………………………………………………………………………………………………. Urgent (to be seen within 4 hours) Yes*/No* Routine (Assess within 14 days) Yes*/No* SERVICE USER DETAILS First Name: ……………………………… Last Name: ………………………… Address: ……………………………………………………………………………………. ………………………………………………………………………………………………… Postcode: …………………..................... Male / Female Date of Birth: ……………………………. Marital Status: ………………………… Tele No: ………………………………….. Mobile: …………………………………. (this number may be sued to send text reminder of appointment Lives with: ………………………………. (Please indicate which number they are happy to be contacted on) Is the patient able to telephone to make an appointment? Yes/No NHS No: ……………………………… Rio Number: ……………………(if known) Carer name: ………………………… Carer Contact Number………………..... Does the patient have hearing/visual impairment? Interpreter/Signer required? Yes/No Yes/No Preferred First Language…………………….. Is the client aware of this referral? Yes/No Ethnicity: …………………………......... Do you believe this to be a memory problem, if so please provide the results below? MMSE/AMT: Yes/No (please delete) Date……. MSU: Yes/No (please delete) Date………… Bloods: Yes/No (please delete) Date…………. ECG: Yes/No (Please delete) Date………… GP DETAILS Name: …………………………………. Surgery Address: ………………………………….. ………………………………………………………………………………………………………… ………………………..Postcode: ………………… Tel No: ……………………………………. -7- 1. SERVICE REQUESTED Psychological Interventions---------------------------------------WAA CMHT (Working Age Adults) -----------------------------OPS CMHT (Older people Services) ---------------------------Memory -----------------------------------------------------------------Liaison ------------------------------------------------------------------Insight -------------------------------------------------------------------REASON FOR REFERRAL (nature of the problem e.g. mood, behaviour, hallucinations, delusions etc including views of significant others) 2. CURRENT MENTAL HEALTH PRESENTATION (please give details of the onset and development, duration and severity of the problem including details on sleep, appetite, concentration, hallucinations, delusions, mood, behaviour etc) MMSE PHQ 9 and GAD 7 Scores……………Please include a copy of the questionnaires) 3. PREVIOUS MENTAL HEALTH HISTORY WITH DATES, INTERVENTIONS AND OUTCOMES (please include details of both psychiatric and psychological interventions including referral to IAPT/Oakdale service, CBT). 4. RELEVANT MEDICAL HISTORY – Physical Health Issues 5. CURRENT MEDICATION – including details of when prescribed, previously tried medications including dose and when prescribed. -8- 6. CURRENT CIRCUMSTANCES: (please include details of: social employment, housing, significant others, family issues, age of children, type of benefits. Had shared care guidelines been considered prior to referral to secondary services)? 7. FORENSIC HISTORY (including current policing involvement) 8. RISK ASSESSMENT: please provide as much information as possible Is the Client Historical Current Evidence of violence and aggression in what context and who is at risk? Yes* / No*/ Not known* Yes / No Inappropriate sexual behaviour, in what context and who is at risk? Yes* / No*/ Not known* Yes / No Substance Misuse? Yes* / No* / Not known* Yes / No Safeguarding Children/Adults issues? Yes* / No* / Not known Yes / No Expressing suicidal ideation? Nature, frequency, when last experienced, likelihood of acting on thoughts, plans/action, preventative measures? Yes* / No* / Not known Yes / No Drug Alcohol? -9- Details Frequency and amount? Evidence of SelfHarm: Nature and Frequency? Yes* / No* / Not known Yes / No Evidence of psychosis? Yes* / No* / Not known Yes / No Evidence of self neglect including wandering. Yes* / No* / Not known Yes / No Symptoms? Name: …………………………………… Profession: …………………………………… Signature: ……………………………… Date: ………………………………………….. Please include any additional information on a separate sheet. Please return this referral form either via post to: Calderdale SPA Office, Willowdale, The Dales, Calderdale Royal Hospital, Salterhebble, Halifax HX3 0PW Or phone Or Fax to 01422 222888 01422 222881 - 10 - 5. RANGE OF SPECIALIST MENTAL HEALTH SERVICES PROVIDED BY SWYPFT Services for adults of working age with moderate to severe mental health problems From 2nd April 2012, Calderdale’s community services (Working Age Adults) will be remodelled into two community teams. The roles and functions of the community mental health teams will merge with psychology and inclusion support (day services) to form one team. One of the specialist teams (Assertive Outreach Team or Insight, Early Intervention in Psychosis) will be based within each of the teams. Community Mental Health Teams Provide a community-based service for working-age adults who are experiencing moderate to severe mental health problems, including: Bipolar disorder Severe anxiety, depression or obsessive compulsive disorder where there may be risk and where there is an inability to use a cognitive behavioural psychological approach Schizophrenia which is symptomatic or in need of continued services in order to prevent relapse, and to maintain and improve functioning Emotional instability which is debilitating and where the individual is not able to engage in individual or group work offered by the psychological therapies department Dual Diagnosis provides a service for people who have complex mental health needs and who have co existing problematic substance misuse. Early Intervention in Psychosis Provides a person centred service for people aged 14-35 who are experiencing a psychotic illness for the first time, or who are experiencing prodromal symptoms of a psychotic disorder and therefore deemed having an at risk mental state. To support their treatment and recovery and maintain well being outside of the mainstream mental health system. - 11 - Assertive Outreach Team The Assertive Outreach Team is a specialist multi-disciplinary team, offering a comprehensive package of care which covers the holistic needs of a small but significant group of the most severely mentally ill population, who have a documented history of non-engagement with services, invariably noncompliance with medication, and have a significant history of risk behaviour in terms of risk to themselves or the public; this will also include exploitation by others and vulnerability to self neglect. The service aims to establish robust links with people in the community, offering intensive treatment and working towards a strengths model of care. We see people in their own homes or elsewhere in the community. When hospital admission is required we hope to facilitate this ourselves and offer regular in-reach to clients in hospital, whilst working collaboratively with the ward staff. The team works with a number of different agencies from the statutory sector and voluntary sector. We operate Monday-Friday 9-5, and offer a service to people between the ages of 18-65, taking into consideration the graduate policy. Calderdale Inclusion Support Service Calderdale Inclusion Support Services (CISS) provides individual and group work to promote social inclusion and vocational activity for adults 18-65. The service is provided utilizing mainstream activities and facilities in the Calderdale area Referrals are taken from CMHT for people on Standard CPA and CPA. The service uses the Recovery Star to assess and care plan with the service user. CISS team is made up of Occupational Therapists, Day Service Workers and Support Workers. The team deliver therapeutic interventions, for example, anxiety management, confidence building, activities that promote social inclusion and reduce social isolation. The Vocational team focus supporting people to retain employment and developing the skills for work. Secondary Care Specialist Adult Psychological Therapies Service The Services described are for adults who are in a position to engage in an active Psychological Therapy (age 18 upwards). APTS treat people who are experiencing SEVERE AND PERSISTENT NonPsychotic Mental Health Problems including: Depression Anxiety disorders PTSD Eating Disorder OCD Disorders arising from Sexual/Physical /Emotional Abuse in childhood. Pervasive Interpersonal Problems: Pervasive conflicts and difficulties in establishing and maintaining relationships (not marital/partnership breakdown suitable for RELATE). - 12 - Somatoform Disorders: Somatisation and body dysmorphic disorder. Complex Adjustment Disorders: complex and enduring grief reactions (persistent and not resolving with the passage of time). Personality Disorders: characteriological issues requiring specialist assessment and treatment. Severe and Complex Disorders involving co-morbidity where specialist assessment and consultation is required to provide a second opinion and/or where formulation will help to indicate appropriate intervention and/or management. SEVERE and COMPLEX is characterised by: Persistent episode. Recurrent episodes. Causing significant disruption in everyday functioning. Increased likelihood of significant risk, e.g. suicidal ideation but no active plans. Using self harm as a coping mechanism. Complex picture with co-morbidity. Not responsive to previous lower tiered interventions (such as psychoeducational groups, and up to 20 sessions of cognitive-behavioural therapy). Complicating underpinning personality based issues. The Psychological Therapies Lead (WAA) for the Calderdale Locality is Christine Marklow, The Dales Unit, The Calderdale Royal Hospital, Salterhebble, Halifax HX3 OPW. Telephone No. 01422 222733. ACUTE PATHWAY Assessment and Home Based Treatment (AHBT) The service provides assessment and short-term treatment to those services users aged 18 – 65 experiencing the onset or relapse of severe mental illness / disorder / distress where a breakdown in normal coping mechanisms or a change in circumstances necessitates a rapid, flexible and intensive approach. The service offers a rapid assessment within 4 hours and intensive home based treatment as an alternative to hospital admission. The Service is available 365 days a year between the hours of 08:00h and 23:00h; outside of these hours an in-reach assessment service is available to attend the A&E department at CRH. A referral for AHBT will usually be characterised by one or more of the following: Imminent risk of harm to self or others by a service user experiencing mental health problems. A mental health crisis likely to necessitate psychiatric inpatient admission. Acute onset of a suspected psychiatric illness. Risk of service users self neglect or exploitation of a service user with mental health problems. A person in A & E or a general medical ward thought to have a serious mental health illness. - 13 - Interventions offered are intended to: Provide a timely and effective response to metal health crisis and provide intensive home based treatment where this will meet the needs of those in crisis. Contribute toward a Gate-keeping role to inpatient services, signposting service users to appropriate services and facilitating/coordinating admission to hospital where necessary Reduce frequency and duration of hospital admissions. Facilitate the timely discharge from hospital of those service users requiring admission Promote recovery and prevent relapse. In-Patient Services Provide assessment and treatment for people whose mental health needs cannot safely be met in the community. Elmdale (Adults) – Dales Unit, Calderdale Royal Hospital, Halifax Beechdale ( Older People Service) – Dales Unit, Calderdale Royal Hospital, Halifax REHABILITATION PATHWAY Lyndhurst Lyndhurst is a mixed sex in patient unit for people with serious mental health problems who require assessment, treatment and rehabilitation back into the community. The service is based in the community providing 14 in-patient beds. Patients admitted to Lyndhurst have usually already been in hospital, on an acute ward or in a more secure hospital environment. Patients can be admitted informally or detained under the restrictions of the Mental Health Act; they will always be already on CPA at the point of referral. Referrals should be discussed with the manager and are managed via Residential Panel. Wells House Wells House is an 18 placement service with the ability to provide 12 residential beds and 6 places supporting people in their own homes. The service is delivered within a supported tenancy framework. Support from health and social care staff enables ongoing recovery and integration into community living. The service uses the outcome focused Recovery Wheel to assess and care plan and review individual needs. Referrals are managed via the Residential Panel. Wells House works closely with Lyndhurst to provide transition to independent community living. - 14 - SHARE Providing accommodation for people with mental health problems for either crisis support, respite or short term rehabilitation. Supporting the delivery of effective care plan as part of the CPA. The aim of the rehabilitation service is to provide short term accommodation for people leaving hospital that offers intensive support and structure to help deal with issues and problems that might otherwise prevent or hinder successful resettlement in the community. The aim of the respite service is to support people in maintaining as independent a lifestyle as possible whilst continuing to live in the community The aim of the crisis beds is to help service users or their carers to prevent or manage a crisis as an alternative to hospital admissions where home treatment is not indicated Referrals from Bed Management, Elmdale or Residential Panel. Share facilitates and supports community based treatment options such as Clozapine initiation and Out patient ECT. This is managed by the Assessment Home Based Treatment Team Union Housing Union Housing provides residential support to people experiencing long term mental health problems. The service promotes the recovery of mental health service users whose needs still cannot be wholly met by the range of acute, community and short-term residential services. The Scheme aims to offer accommodation and staff support, providing safe environments in which health and risk issues can be monitored and daily living skills/recreational & vocational activities/goals of increased independence can be identified, promoted and achieved in a collaborative manner. Referrals are by the Residential Panel. - 15 - Calderdale Older People Services Community Mental Health Teams Provide a community-based service for older adults who are experiencing moderate to severe mental health problems, including: Bipolar disorder Severe anxiety, depression or obsessive compulsive disorder where there may be risk and where there is an inability to use a cognitive behavioural psychological approach Schizophrenia which is symptomatic or in need of continued services in order to prevent relapse, and to maintain and improve functioning Emotional instability which is debilitating and where the individual is not able to engage in individual or group work offered by the psychological therapies department. First episode of psychosis Dementia which requires ongoing monitoring and support Care Home Liaison Team. The team supports older people with mental health problems who live in care homes in Calderdale. A typical user of the service would be an older person experiencing dementia or severe and enduring mental health issues. They may have difficulties with accepting help from care staff and behave in ways that care staff can find difficult to understand and manage. The team will assess individuals (nursing and dietetic staff) and help care staff develop plans of care. The team facilitates reviews of medication and liaises with primary care teams. The team will provide mental health nursing assessments for social workers and the PCT. The team will also provide ad hoc training and education sessions for care staff having facilitated over 100 staff in the past 12 months. The team is supported by medical staff from the older people’s mental health service. The team also carries out funded nursing care and continuing health care assessments for the PCT. Acute Hospital Liaison Team Works closely with the Calderdale and Huddersfield NHS Foundation Trust to ensure that the mental health needs of older people admitted to an acute hospital setting are recognised and met. The team cover both hospitals and participate in the Virtual ward and provide a Dementia matron service to all areas This document compiled by: Andrew Donato CPA/Risk Manager/Safeguarding Lead Irene Stephenson Support Services Manager 23rd September 2011 Updated by Janice Wootton Community Manager Mental Health 21/3/12 - 16 -