End of Life Care Education
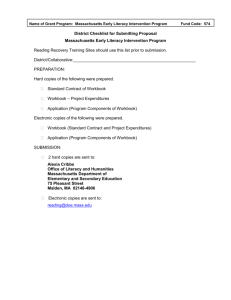
advertisement

Advance Care Planning WORKBOOK An Introductory Workbook for Health and Social Care Practitioners Supporting Individuals in End of Life Care Ref ACP.WB Level: Intermediate Last updated 14/12/10 Sue Ryder Care lorraine.dixon@suerydercare.org Name ………………………………….…………………………………………………… Job role …………………………………………………………………………………… Line Manager/Mentor …………………………….………………………………….... Date workbook started ………………………………………………………………… Date completed………………………………………………………………………..... Completion of this workbook will help provide evidence towards: Common Induction Standards End of Life National Occupational Standards Knowledge Set for End of Life Care To view or print the Advance Care Planning tool. ‘Planning for your Future Care’ used in Gloucestershire please visit http://www.gloucestershireccg.nhs.uk/?page_id=176 You will find the ACP document half way down in the right hand column. WORKING IN PARTNERSHIP WITH 2gether NHS Foundation Trust Cotswold Care Hospice Gloucestershire County Council Gloucestershire Hospitals NHS Foundation Trust Great Oaks Hospice NHS Gloucestershire Care Services Sue Ryder Hospice Important This resource was funded and written by members of the Gloucestershire End of Life Education group. Please be aware that materials will need to be reviewed and updated periodically (last update 01/2012). D:\106751367.doc 1 Introduction This workbook is one of two introductory Advance Care Planning learning resources. It is recommended you either complete this workbook OR attend one of the facilitated sessions being delivered across the county. Advance Care Planning is part of a series of facilitated sessions and workbooks designed to develop your skills and knowledge in supporting patients at End of Life. Target Audience All health and social care staff who frequently deal with end of life care as part of their role. Aims This workbook aims to develop your knowledge, skills and understanding of Advance Care Planning and your role as a health and social care practitioner in facilitating Advance Care Planning for patients in your care. Outcomes On completion of this workbook you will: Develop your knowledge and understanding of the concept of Advance Care Planning and its relevance to your own practice setting; Be aware of local resources to support patients in preparing for their future; Identify further learning needs that you may have as a practitioner to further develop your skills and knowledge in relation to Advance Care Planning. How to use this workbook The workbook provides information, guidance and opportunities for reflection to aid learning and understanding. The workbook is designed to be completed by you in your own time although enhanced learning is likely to be achieved when discussed with your mentor, peers and colleagues. It is recommended that you work through the workbook in a chronological order building in time to read every section carefully and spend sufficient time thinking about and completing each activity. It is recommended that you plan your study time carefully – you do not need to complete the workbook is just one session. Time required completing this workbook: 1-2 hours (This assumes that you have already gathered the resources identified in the reference list). Other related resources: it is recommended you consider the following additional End of Life Care workshops or workbooks: Raising Awareness Communicating with Confidence Supporting the bereaved Please contact Sue.goold@glos.nhs.uk for further information or the EoLC Calendar of Events on http://www.gloucestershireccg.nhs.uk/?page_id=176 D:\106751367.doc 2 What is Advance Care Planning? Advance care planning (ACP) is a voluntary process of discussion about future care between an individual and their care providers, irrespective of discipline. If the individual wishes, their family and friends may be included. It is recommended that with the individual’s agreement this discussion is documented, regularly reviewed, and communicated to key persons involved in their care. An ACP discussion might include: • the individual’s concerns and wishes, • their important values or personal goals for care, • their understanding about their illness and prognosis, • their preferences and wishes for types of care or treatment that may be beneficial in the future and the availability of these. Henry & Seymour (2008) ACP differs from more general forms of planning in that it is taken in the context of an anticipated deterioration in the individual’s condition with the attendant loss of capacity to make or communicate decisions (Killick et al. 2010). Activity Make a list to discuss with your mentor of potential challenges ACP might present for: - the patient - their family/carer - the professional. Make a note of the key challenges and how they might be managed. Challenges of ACP for the patient D:\106751367.doc Strategy to manage the challenge 3 Challenges of ACP for the family/carer Strategy to manage the challenge Challenges of ACP for the professional Strategy to manage the challenge D:\106751367.doc 4 Key Principles of Advance Care Planning Process National guidance published by the Department of Health and supported by the National Council for Palliative Care recommends the following key principles for ACP (Henry & Seymour, 2008). 1. The process is voluntary. No pressure should be brought to bear by the professional, the family or any organisation on the individual concerned to take part in ACP 2. ACP must be a patient centred dialogue over a period of time 3. The process of ACP is a reflection of society’s desire to respect personal autonomy. The content of any discussion should be determined by the individual concerned. The individual may not wish to confront future issues; this should be respected 4. All health and social care staff should be open to any discussion which may be instigated by an individual and know how to respond to their questions 5. Health and social care staff should instigate ACP only if in the context of a professional judgement that leads them to believe it is likely to benefit the care of the individual. The discussion should be introduced sensitively 6. Staff will require the appropriate training to enable them to communicate effectively and to understand the legal and ethical issues involved 7. Staff need to be aware when they have reached the limits of their knowledge and competence and know when and from whom to seek advice 8. Discussion should focus on the views of the individual, although they may wish to invite their carer or another close family member or friend to participate. Some families may have discussed their issues and would welcome an approach to share this discussion 9. Confidentiality should be respected in line with current good practice and professional guidance 10. Health and social care staff should be aware of and give a realistic account of the support, services and choices available in the particular circumstances. This should entail referral to an appropriate colleague or agency when necessary 11. The professional must have adequate knowledge of the benefits, harms and risks associated with treatment to enable the individual to make an informed decision 12. Choice in terms of place of care will influence treatment options, as certain treatments may not be available at home or in a care home, e.g. chemotherapy or intravenous therapy. Individuals may need to be admitted to hospital for symptom management, or may need to be admitted to a hospice or hospital, because support is not available at home 13. ACP requires that the individual has the capacity to understand, discuss options available and agree to what is then planned. Agreement should be documented www.opsi.gov.uk/acts/acts2005/20050009.htm 14. Should an individual wish to make a decision to refuse treatment (advance decision) they should be guided by a professional with appropriate knowledge and this should be documented according to the requirements of the MCA 2005 www.opsi.gov.uk/acts/acts2005/20050009.htm D:\106751367.doc 5 Reflect and make notes on each principle in relation to supporting individuals and their families in your own practice setting with ACP. The questions below each principle in italics are intended to prompt your reflection. Discuss your notes on completion of the activity with your mentor. 1. The process is voluntary. No pressure should be brought to bear by the professional, the family or any organisation on the individual concerned to take part in ACP As a practitioner how would you ensure that the process was voluntary and that no pressure was placed on those involved? 2. ACP must be a patient centred dialogue over a period of time How could you facilitate the dialogue to be patient centred? How could you ensure the accuracy of the ACP over a period of time? 3. The process of ACP is a reflection of society’s desire to respect personal autonomy. The content of any discussion should be determined by the individual concerned. The individual may not wish to confront future issues; this should be respected What strategies could you use to ensure the conversation about ACP is led by the individual? How would you recognise when an individual does not want to confront an issue? How might you manage this if family or carers have a differing view? D:\106751367.doc 6 4. All health and social care staff should be open to any discussion which may be instigated by an individual and know how to respond to their questions. What are your strengths and weaknesses in managing difficult conversations? How do you recognise your professional boundaries? If you recognise a limit in your knowledge or experience who might you refer the patient to for further support and discussion of their ACP? 5. Health and social care staff should instigate ACP only if in the context of a professional judgement that leads them to believe it is likely to benefit the care of the individual. The discussion should be introduced sensitively When would it be appropriate to instigate ACP? How can you as a practitioner determine ACP will be of benefit to the individual? How can a discussion be introduced sensitively? 6. Staff will require the appropriate training to enable them to communicate effectively and to understand the legal and ethical issues involved a) If you have completed a communication module you may choose to omit this part of the exercise, or reflect on your learning from the module and identify areas for further improvement of your communication skills. If you have not completed the communication learning resource use the NHS Knowledge And Skills Framework (NHS KSF) and The Development Review Process Appendix 2: Core dimension 1: communication NHS knowledge and skills framework – October 2004 to discuss with your mentor your communication skill and identify your strengths and areas that you feel less comfortable with. Make a plan to further develop your communication skills in relation to ACP. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/ dh_4107979.pdf b) To understand the legal and ethical issues related to ACP complete the section from page 9. 7. Staff need to be aware when they have reached the limits of their knowledge and competence and know when and from whom to seek advice a) How do you recognise when you have reached the limits of your knowledge and competence? b) If you are supporting a patient with ACP and felt you had reached the limits of your knowledge and competence who would you seek advice from and why? D:\106751367.doc 7 8. Discussion should focus on the views of the individual, although they may wish to invite their carer or another close family member or friend to participate. Some families may have discussed their issues and would welcome an approach to share this discussion How would you support the individual to include their carer or close family member to participate? What strategies would you use to ensure that they did not take over the discussion and the individual’s views were respected? 9. Confidentiality should be respected in line with current good practice and professional guidance As a healthcare practitioner you will be familiar with the expected good practice and professional guidance specific to your profession. Take this opportunity to revisit the guidance. Make notes and consider the guidance with respect to ACP. For medics go to: http://www.gmc-uk.org/guidance/ethical_guidance/confidentiality.asp For nurses and midwives go to: http://www.nmc-uk.org/Nurses-and-midwives/Advice-by-topic/A/Advice/Confidentiality/ 10. Health and social care staff should be aware of and give a realistic account of the support, services and choices available in the particular circumstances. This should entail referral to an appropriate colleague or agency when necessary Providing a realistic account of the support, services and choices available in particular circumstances, can be challenging for health and social care professionals. In considering Preferred Priorities for Care it is important to recognise that an individual’s wish might change over time. a) What safe guard would you put in place to ensure the document is current? b) See the following link below to the NHS Gloucestershire Advance Care Planning document' http://www.gloucestershireccg.nhs.uk/wp-content/uploads/2012/03/PLANNING-FORFUTURE-CARE-Print-version.pdf Read the document and familiarise yourself with the prompts for discussion and the documentation. Is an ACP a legal document? No! An ACP is not a legal document. It is an account of an individuals wishes, which can be used as a guide to inform carers and professionals of their preferred priorities of care. It can act as an aid to prompt communication around difficult issues. It can provide a written record of the individual’s wishes and care preferences to prompt further discussion or actions. D:\106751367.doc 8 If an individual wishes they can make decisions about any treatments that they will or won’t have by completing an Advance Decision (Living Will) this is a legally binding document which allows an individual to refuse certain treatments. The National Gold Standards Framework (2010) states there are two specific but overlapping areas within Advance Care Planning: 1) Advance Statement, which is a discussion of people's preferences, wishes and likely plans i.e. what they wish might happen to them. These are generally called Advance Statement/Statement of wishes. These are not legally binding, but are invaluable in determining planned provision of care. The process of discussing this can be seen as part of the solution in that it enables emotional 'catch up' and adaptation to the new reality and normalisation of life. Sensitive discussion of advance care planning can strengthen coping mechanisms and enable realistic planning. There is some evidence that it increases not decreases realistic hope. They reference their own Advance Statement included in the GSFCH programme. Other examples such as the Preferred Place of Care (PPC) document and the NHS Gloucestershire Advance Planning Document ‘Planning for Your Future Care’. 2) Advance Decision, is used to clarify refusal of treatment or what patients do NOT wish to happen, involves assessment of mental competency to make that decision at the time and when accurately formulated, can be legally binding. It also strengthens the role of the Lasting Power of Attorney to enable a nominated proxy person to make decisions about medical as well as social welfare. National Gold Standards Framework (2010) Visit the following Gold Standards Framework website for more information on Advance Decisions and Advance Statements. http://www.goldstandardsframework.nhs.uk/AdvanceCarePlanning Reflect and make notes on the last four principles in relation to supporting individuals and their families in your own practice setting with ACP. The questions below each principle in italics are intended to prompt your reflection. Discuss your notes on completion of the activity with your mentor. 11. The professional must have adequate knowledge of the benefits, harms and risks associated with treatment to enable the individual to make an informed decision Are you the appropriate person to enable an individual to make an informed decision? If your answer is YES how do you know you have adequate knowledge of the benefits, harms and risks associated with the decision? If NO who would you refer the patient to make an advance decision? D:\106751367.doc 9 12. Choice in terms of place of care will influence treatment options, as certain treatments may not be available at home or in a care home, e.g. chemotherapy or intravenous therapy. Individuals may need to be admitted to hospital for symptom management, or may need to be admitted to a hospice or hospital, because support is not available at home. What strategies would you adopt to ensure the individual has a realistic understanding of the nature of their illness and where specific treatments that might be required could be delivered? 13. ACP requires that the individual has the capacity to understand, discuss options available and agree to what is then planned. Agreement should be documented www.opsi.gov.uk/acts/acts2005/20050009.htm What processes are in place within your practice setting to ensure an individual has capacity to understand and discuss options available and agree to what is planned? 14. Should an individual wish to make a decision to refuse treatment (advance decision) they should be guided by a professional with appropriate knowledge and this should be documented according to the requirements of the MCA 2005 www.opsi.gov.uk/acts/acts2005/20050009.htm Who would be an appropriate professional for you to refer to and why? D:\106751367.doc 10 Mental Capacity Act (2005) The following principles apply for the purposes of this Act: A person must be assumed to have capacity unless it is established that he lacks capacity A person is not to be treated as unable to make a decision unless all practicable steps to help him to do so have been taken without success. A person is not to be treated as unable to make a decision merely because he makes an unwise decision. An act done, or decision made, under this Act for or on behalf of a person who lacks capacity must be done, or made, in his best interests. Before the act is done, or the decision is made, regard must be had to whether the purpose for which it is needed can be as effectively achieved in a way that is less restrictive of the person's rights and freedom of action. Mental Capacity Act (2005) http://www.legislation.gov.uk/ukpga/2005/9/contents The Mental Capacity Act 2005 covers the development of a new Lasting Power of Attorney (LPA), allowing an appointed person to make decisions about that person’s healthcare should that person loose capacity to do so for themselves. Wilson, Seymour & Perkins (2010) LPA’s can cover health and welfare decisions be registered at any time and MUST be registered before they are used attorney’s acting under an LPA have a legal duty to act in accordance with the principles set out in the Mental Capacity Code of Practice The Law Society (2010) Activity The flow chart on the next page summarises the process for Advance Care Planning. With your mentor reflect on what you have learnt about Advance Care Planning and make an action plan to further develop your knowledge and skills in this area that acknowledges your strengths and weaknesses. D:\106751367.doc 11 Department of Health (2008) D:\106751367.doc 12 Personal Experiences of ACP The End of Life Care Strategy encourages more open dialogue surrounding death and preparation for death. You may choose to work through the NHS Gloucestershire Advance Care Planning document yourself, and reflect on your personal experience. What did you find that was helpful in the document? What was difficult to complete? Did you discuss the document with anyone as you completed it? Reflect on the issues that this raised for you. If you feel comfortable to do so discuss the experience with your mentor D:\106751367.doc 13 Personal Reflections of learning To complete this workbook now spend some time reflecting on what you have learnt and how you will put this new learning into practice. Something I’ve learnt about myself whilst completing this workbook: The most helpful thing I’ve learnt whilst completing this workbook: The most important thing I’ve learnt whilst completing this workbook: One thing I’ll try to do differently at work as a result of what I’ve learnt? One skill or area I’d like to develop further in relation to supporting the bereaved: D:\106751367.doc 14 Support services & information Accessing further End of Life Care Education and resources in Gloucestershire Further learning and development needs will largely depend on role within your organisation. It is recommended you speak to your line manager in the first instance to find out about further opportunities. Local providers of End of Life and Palliative Care education include: Cotswold Care Hospice (01453 886868) www.cotswoldcare.org.uk Great Oaks Hospice (01594 811910) www.greatoakshospice.org.uk Sue Ryder Hospice (01242 230199) http://www.suerydercare.org/care_centres.php/16/sue_ryder_care_leckhampton_court_hospice Gloucestershire Care Services – Clinical skills training department (08456 598100) Gloucestershire County Council – for social care staff (01452 425063) Gloucestershire Hospitals NHS Trust, Specialist Palliative Care Team (01452 371022) 2gether NHS Trust – specialising in Mental Health and Learning Disabilities (01453 891254) End of Life e-learning modules for Health and Social Care Staff www.e-ELCA.org.uk D:\106751367.doc 15 References Department of Health (2004) The NHS Knowledge and Skills Framework (NHS KSF) and the Development Review Process, Appendix 2: Core dimension 1: Communication NHS knowledge and skills framework – October http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasse t/dh_4107979.pdf Henry, C. and Seymour (2008) Advance Care Planning: A guide for health and social care staff, Department of Health, accessed on 31/08/10 http://www.ncpc.org.uk/download/publications/AdvanceCarePlanning.pdf Killick, S., Pharaoh, A. and Randall, F. (2010) Advance care planning in care homes, Palliative Medicine, Vol 24, No 4, pp. 445-446. NHS Gloucestershire (2010) Advance Care Planning Document, accessed on 08/12/10 http://www.gloucestershireccg.nhs.uk/wp-content/uploads/2012/03/PLANNING-FOR-FUTURECARE-Print-version.pdf The Law Society (2010) Assessment of Mental Capacity, Capacity to consent to and refuse medical treatment and procedures., 3rd edition, Chapter 13, pp. 130-131 Wilson, E, Seymour, J. and Perkins, P. (2010) Working with the Mental Capacity Act: findings from specialist palliative care and neurological settings, Palliative Medicine, Vol 24, No 4, pp. 396-402. Possible further reading Davison, S. N. (2009) Advance care planning in patients with end-stage renal disease, Progress in Palliative Care, Vol 17, No 4, pp. 170-178. Goth, M., Gardiner, C., Small, N., Payne, S., Seamark., Barnes, S., Halpin, D. and Ruse, C. (2009) Barriers to advance care planning in chronic obstructive pulmonary disease, Palliative Medicine, Vol 23, No 7, pp. 642-648. Johnston, B. (2010) Reclaiming truly dignified care, International Journal of Palliative Nursing, Vol 16, No 7, p. 315. Kataoka-Yahiro, M., Conde, F., Wong, R., Page, V. and Peller, B. (2010) Advance care planning among Asian Americans and Native Hawaiians receiving haemodialysis, International Journal of Palliative Nursing, Vol 16, No 1, pp. 32-40. Newson, P. (2009) End-of-life care: making links with dementia care, Nursing and Residential Care, September, Vol 11, No 9, pp. 433-436. Newton, J., Clark, R. and Ahlquist, P. (2009) Evaluation of the introduction of an advanced care plan into multiple palliative care settings, International Journal of Palliative Nursing, Vol 15, No 11, pp. 554-561. Wiener, L., Ballard, E., Brennan, T.,Battles, H., Martinez, P. and Pao, M. (2009) How I Wish to be Remembered: The Use of an Advance Care Planning Document in Adolescent and Young Adult Populations, Journal of Palliative Medicine, March 3, pp. 2-10. D:\106751367.doc 16 Appendix 1 End of Life Education in Gloucestershire Evaluation Form Workbook Title: Date: What was the best feature of the workbook and why? How would you suggest changing/improving the workbook – if at all? Please indicate your response to the following questions by ticking the appropriate box. 1. Material of Content Strongly Agree Disagree Strongly N/A Agree Disagree The workbook was at an appropriate level for me. The workbook content was relevant to my working situation Comments: 2. Teaching and Presentation Strongly Agree Agree Disagree Strongly Disagree N/A The teaching methods were appropriate Comments: The workbook was well structured and organised D:\106751367.doc 17 Comments: 3. Learning and its Application Strongly Agree Disagree Strongly to work Agree Disagree I will be able to apply learning from the workbook List 3 actions you will be taking as a result of completing the workbook. N/A 4. Conclusion Overall, I would evaluate the workbook as: Comments: Poor Excellent Good Average Fair Would you recommend this workbook to a colleague? Yes No Any other comments: If you would like to receive further end of Life Care Education, please list what subject areas you would like to be covered. Thanks you for completing this evaluation. Please send any major comments to Kath Keogh at Leckhampton Court, Church Rd, Leckhampton, Cheltenham GL53 0QJ Otherwise please share with your manager. D:\106751367.doc 18