Assessment of Bowel Elimination
advertisement

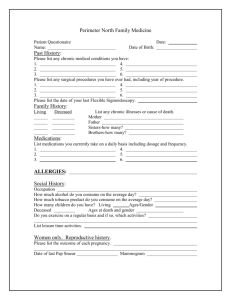
BallaratHealthServices CLINICAL PRACTICE GUIDELINES (NURSING) Number: EQuIP Number: TO : All Staff SUBJECT : Assessment of Bowel Elimination Date Effective: Reg. Authority: Date Revised: Date for next review: Review Responsibility: Scope: Executive Director, Nursing Services Nursing Practice Committee DESIRED OUTCOME / OBJECTIVE: 1. There is timely identification of those at risk of developing bowel elimination problems. 2. Where a bowel problem exists, appropriate, thorough and prompt assessment is provided 3. The assessment is clearly documented 4. Management and treatment is appropriate and contemporary and based on a thorough assessment POLICY Individual bowel management programs are consistent with contemporary practice in the area, implemented and reviewed at regular intervals. Treatment and management of any bowel condition is based on a thorough individual assessment and the rationale for treatment and management are clearly documented. KEY CONCEPTS Defining a normal bowel pattern It is not necessary for people to open their bowels every day. While it is true that some people do have daily bowel actions, most people don’t. It is considered normal for a person to open their bowels anywhere from 3 times per day through to 3 times per week (Heaton et al, 1992). It is more important for a person to have a regular, relaxed and easy bowel motion than it is for them to go every day. When defining normal bowel patterns, a number of factors need to be considered as well as bowel motion frequency. A normal bowel motions should be: regular and within the normal frequency range (ie 3x/day to 3x/week) soft but formed, not hard or sloppy easy to pass without straining or pain followed by a feeling of having emptied the bowel properly For definitions of constipation, diarrhoea, feacal incontinence see the associated BHS protocols. ASSESSMENT Routine screening of bowel patterns On admission, all patients/residents will have their bowel elimination needs screened by the bowel elimination questions on the nursing admission/assessment form relevant to the unit. This screening should include: details of normal bowel habit when bowels were last opened currently used management (eg. any laxatives (prescribed and unprescribed) or special foods usually taken to promote regularity) presence of past/current bowel problems Bowel pattern during the admission should then be recorded on the daily observation form or on the daily bowel record if this is the routine practice in the unit. Assessment of a specific bowel problem If there are concerns about a person’s bowel status or a problem is identified a more thorough assessment is required. A specific assessment of bowel function should be initiated if: 1. a person is thought to be at significant risk of developing a bowel problem 2. a bowel problem has been reported or noted 3. when the person’s bowel status deteriorates or changes suspiciously 4. a person on a bowel management/prevention plan needs periodic review (ie. in residential care) The assessment should be commenced as soon as possible following the identification of the problem and completed within 7 – 14 days. A Bowel Elimination Assessment will include: 1. The BHS Bowel Elimination Assessment form (MR/209.2) which assists in collecting all the data required for a nursing bowel assessment including: a history of bowel elimination pattern – including continence status a history of relevant general conditions that may impact on bowel status a review of medications that may impact on bowel status an review of nutritional status in relation to bowel elimination 2. The BHS Bowel Elimination Observation Chart (MR/550.0) which includes observations of: frequency and timing of bowel motions consistency (or form) of stools (using the Bristol Stool Form Scale – Heaton et al, 1994) amount or size of stools presence of straining, pain etc associated with a bowel motion presence of abnormalities in the stool such as blood, mucous, fat or undigested food 3. A physical examination may be conducted and appropriately documented by an RN Div 1 or medical staff which may include: examination of the abdomen (palpation and auscultation) for as signs such as abdominal tenderness, a mass and decreased bowel sounds perineal inspection, looking for abnormalities such as evidence of soiling, rectal prolapse, peri-anal scaring, a gaping anus or perineal descent or haemorrhoids a rectal examination to determine amount and type of faeces in the rectum, the presence of any rectal mass and the state of anal sphincter tone Length of time for bowel observation & charting The best amount of time for assessment bowel charting has not yet been established by research. However, the length of stay and the type of unit to which the person is admitted will clearly influence the amount of charting that is possible. The purpose of the observation also will influence the time it is maintained. 1. for initial observation Acute Care observe and chart for 3 days up to one week or as required by medical staff Sub-acute or Residential Care it is preferable to observe and chart for assessment of a bowel problem for a week or as directed by medical or specialist nursing staff. 2. for monitoring during implementation of the treatment and management strategies maintain the bowel observation chart to observe the effectiveness of these strategies once the goals of treatment/management have been reached (ie the management is working), recording the frequency of bowel actions on daily observation charts or on a daily bowel sheet as per the unit’s policy is adequate Suggestions to help with assessment: 1. Involve the patient or resident in their own bowel charting if possible and appropriate eg. by giving them an illustrated stool form chart so they can observe their own bowel motions 2. Maintain a detailed chart only as long as required 3. In residential care units, limit the number of people being assessed to one or two per unit at a time to minimize staff workload and reduce the risk of confusion TREATMENT AND MANAGEMENT A decision regarding the type of bowel elimination problem is made following thorough assessment. An individual management plan is based on this assessment in consultation with medical staff and with the person as appropriate. The plan of care is documented as per the unit’s protocol. See BHS management protocols/guidelines for the specific bowel elimination problems of constipation (no. #), diarrhoea (no. #), faecal incontinence (no. #). EVALUATION The management program is to be evaluated to determine if the nursing interventions are achieving the goals of care. For a routine evaluation such as required in residential care (12 monthly), a Bowel Elimination Observation Chart (MR/550.0) is to be completed for at least 3 days and preferably a week while the management plan is in place. If the person’s bowel pattern is demonstrated to be satisfactory and continues to meet the care plan goals, no further assessment is required. However, the Bowel Elimination Assessment form (MR/209.2) will need to be repeated if the evaluation bowel chart demonstrates a problem, or if a problem is identified by either the person or the staff between routine evaluation. REFERENCES: Heaton, K.M., Radvan, J., Cripps, H., Mountford, R.A., Braddon, F.E.M., Hughes, A.O., 1992, “ Defecation frequency and timing, and stool form in the general population: a prospective study”, Gut, 33, 818-824 Heaton, K.M., O'Donnell, L.J.D. 1994, “An Office Guide to Whole-Gut Transit Time: Patient's Recollection of their Stool Form”, Journal of Clinical Gastroenterology, 19(1), 28-30