Services for Adult Survivors of Childhood Sexual
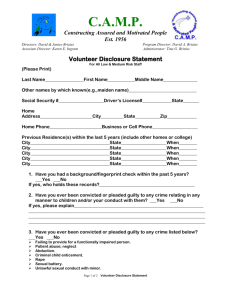
advertisement

The Report of the Scottish Executive Short-Life Working Group on the care needs of people who have survived childhood sexual abuse Services for Adult Survivors of Childhood Sexual Abuse Contents Executive Summary Recommendations 1. 2. 3. 4. 5. 6. 7. Introduction Purpose of this Report Policy Context Review of the Literature in Terms of the Prevalence of CSA and the Health and Social Consequences of CSA Models of Service for the Care and Treatment of Adult Survivors of Childhood Sexual Abuse Awareness Raising and Training Conclusion and Recommendations Appendix A – SLWG Membership and Remit Appendix B – Survivor Testimonies Appendix C – Attendance List from 28th April conference 1 Services for Adult Survivors of Childhood Sexual Abuse Executive Summary 1. This report highlights the enormity of the challenge in meeting the needs of survivors more effectively. But, as has been pointed out by the Cross Party Working Group (CPG), this is not a new population. Survivors are already receiving services from health and social care agencies in particular but, in most cases they are not receiving an integrated and coordinated service that responds to the complex needs of the whole person. 2. Childhood sexual abuse (CSA) is increasingly recognised as a major cause of morbidity and mortality. Two recent World Health Organisation (WHO) reports – World Report on Violence and Health (2002) and World Health Report 2002 (2002) – acknowledge that CSA is common in both females (20%) and males (5-10%). CSA is even more prevalent in specific populations including substance abusers, the homeless and psychiatric inpatients. 3. CSA is underreported with 10-17% reporting the abuse to child protection services and less than 1% of cases documented in health records. The consequences of CSA include mental health problems (including suicide and eating disorders), physical illness, and behavioural and social problems. The increased cost to hospital services of managing the health consequences of CSA for women in Scotland is estimated to be £30-60 million per annum. 4. There is no clear responsibility for identifying or supporting adult survivors of CSA within primary health or mental health services at present. 5. The voluntary sector has considerable expertise in helping adult survivors of CSA and currently provides the only substantial data collection. With adequate support and funding the voluntary sector could provide a vital function for the statutory sector. Currently this remains far from the case. 6. A significant problem for survivors of sexual abuse is that CSA is not widely recognised as a major contributing factor to a range of seriously disabling behaviours such as self-harm and substance abuse. It is therefore unsurprising that the emphasis in practice is largely placed upon treating the symptoms and minimising harm rather than supporting service users to explore aspects of their sexual abuse history which are problematic for them, and develop strategies for coping positively with daily life. 7. Survivors report that the people who help them do not come from any one professional background or use a particular therapeutic approach. They do not necessarily have high professional status. The majority have not attended specific training courses on child sexual abuse, although they had gathered expertise in other ways. Rather, they were secure and firm about boundaries, but related with warmth and kindness. They were informed and aware about the main effects of CSA trauma and had examined their own personal issues around working with sexual abuse. They worked non-hierarchically, consulting respectfully with survivors about what their main needs were and what their service could offer. They neither hid behind confidentiality nor broke it insensitively. 2 8. Given the complexity and diversity of issues arising from CSA it is essential that a range of services is developed. Survivors and professional workers have identified services models that are beneficial. These include a 24-hour telephone helpline, a crisis house, counselling, groupwork (both self-help and facilitated therapeutic work), respite and services that are able to work with and stick with people who present with challenging behaviours. 9. There is a need for more public awareness of the issues around childhood sexual abuse and how to protect children from perpetrators. There is also a need for people to know where to get help as survivors or as potential perpetrators. 10. Staff also need awareness raising about the common effects of CSA trauma, the relevance of CSA to their particular client group and their feelings about working with CSA. This training would be especially useful for anyone who works in an environment where there are likely to be many clients with a history of CSA. This includes psychiatric units, prisons, special hospitals, primary care, children's home/secure units, accident and emergency departments, self-harm projects, drug and alcohol projects, reproductive health, eating disorder projects, counselling projects, schools for emotional/behavioural problems, homelessness work. 11. For the vast majority of adult survivors, a more humane, open and empathetic service response is all that is required. This sounds simple and could be if the quality of services was assessed on these criteria. 12. From a policy perspective, it is essential that adult survivors work is integrated into existing areas of activity, rather than spawning a whole new infrastructure and sub-specialisation. There are also important links to be made with mental health policy. 13. The impact of childhood sexual abuse on a variety of health conditions is poorly understood, but given its prevalence, more thought is needed on its impact in clinical practice. For example, thought is needed on the possible impact this has on certain investigative procedures. 14. There is national and local work that is required to meet the needs of survivors more effectively. Obtaining better baseline data from both specialist and also mainstream services is a priority. 3 Recommendations 1. The Scottish Executive should incorporate the issue of adult survivors of childhood sexual abuse into policy developments around child protection, domestic abuse and mental health services. This policy work should cover prevention, treatment, support and recovery from the effects of childhood sexual abuse. 2. There needs to be a broad-based awareness campaign that challenges current public and professional attitudes. The campaign should make the links between childhood abuse and adult mental health problems. It is suggested that adult survivors are involved in the development of the campaign and that links are made to See Me the national campaign tackling stigma and discrimination. There is also a role for NHS Health Scotland in counteracting the secrecy associated with sexual abuse. 3. There needs to be a training strategy that puts childhood abuse on the curricula for basic training in nursing, medicine, social work and criminal justice (including police). For postgraduate training, we recommend the issues for adult survivors are integrated with training for child protection, domestic abuse and patient communication. 4. NHS Quality Improvement Scotland needs to develop national standards for the care of adult survivors of childhood sexual abuse who are cared for in mental health services. These standards would incorporate the need for a gender-sensitive approach to providing services. Survivors themselves should be involved in developing these. 5. A needs assessment should be undertaken of the prison population with particular attention to those on remand and with short sentences. 6. Medical and nursing bodies should review relevant areas of clinical practice and develop guidelines for undertaking sensitive examinations in adult survivors of sexual abuse. Involving survivors themselves in this work would be critical to its success. 7. NHS Health Scotland should encourage self-help tools, for instance through the marketing of Breathing Space, the national helpline as a source of help for adult survivors. The Justice and Education Departments of the Scottish Executive should develop materials for use in schools, communities and the web. Uptake should be evaluated to assess its impact. 8. Local commissioners need to urgently develop services to support adult survivors in line with best practice. This means supporting non-statutory services where they exist, ensuring they are put on a more secure financial footing, and evaluating good practice models. It also means dedicating resources towards and improving the quality of care in existing mainstream services in recognition of the strong association between CSA and significant mental health problems, reflecting the needs of survivors. More specialist services to provide support and treatment for survivors at the severe end of the spectrum are needed. There is also a need to join up approaches around services for children affected by sexual abuse and adult services in this area. Progress on implementing local service change should be monitored through the NHS Performance Assessment and Accountability Framework, and the Community Planning/Health Improvement process. 4 9. Better data collection about survivors is needed in addiction services, primary care, mental health, GUM, obstetrics and gynaecology, and Accident and Emergency. This will help to improve our understanding of the extent of the health needs of survivors. 10. It is recommended that there should be support for a network of researchers, practitioners and survivors with an interest in improving the care and treatment of adult survivors. 5 Services for Adult Survivors of Childhood Sexual Abuse 1. Introduction 1.1. This report originates from the work of the Scottish Parliament’s Cross Party Group (CPG) on Survivors of Childhood Sexual Abuse, and from Sarah Nelson’s Beyond Trauma: Mental Health Care Needs of Women Survivors of Childhood Sexual Abuse research report which highlighted service failings. Since its launch in 2001, the CPG group has held parliamentary debates, undertaken research and encouraged a broad cross-governmental approach to the issue. In response to their concerns, the Minister for Health and Community Care, Malcolm Chisholm set up a Short-Life Working Group on the Care Needs of People who are Survivors of Childhood Sexual Abuse (CSA). This report is the result of the work of the Short-Life Working Group to date. Its remit and membership is set out in Appendix 1. 1.2. The group commissioned a literature review and took evidence from a range of professionals and services. It met with the Scottish Parliament’s CPG and wherever possible has taken on board many of that Group’s concerns. This report takes into account all of this information and the discussions that flowed from them. It marks a stage in a bigger process of bringing attention to this complex issue and finding effective ways of dealing with it. 1.3. The group took this report to a wider range of people working in many different agencies and areas of Scotland and has changed the report to reflect this input. Two survivors talked about their experiences of service responses at this meeting. Their testimonies are attached in an appendix along with a list of participants at the wider event. 1.4. It was accepted by the group that whilst the scientific evidence-base for effective interventions was relatively limited, this was no reason for inaction. The group took the view that other forms of knowledge were also important, not least the view of survivors themselves. 1.5. This report is structured into 7 main chapters. Chapter 2 sets out the purpose. Chapter 3 covers the broad policy context and background. Chapter 4 summarises an extensive review of the literature in terms of the prevalence of CSA and the health and social consequences of CSA. Chapter 5 looks at models of care currently being advocated for mental health services and examines their effectiveness for this client group. The chapter goes on to explore the need for models in other services and agencies. Chapter 6 covers the wide range of training issues related to this client group. Chapter 7 draws some conclusions and makes some recommendations on taking this work further. 6 2. Purpose of Report 2.1. This report highlights the enormity of the challenge in meeting the needs of survivors more effectively. But, as has been pointed out by the Cross Party Working Group, this is not a new population. Survivors are already receiving services from health and social care agencies in particular but, in most cases they are not receiving an integrated and coordinated service that responds to the complex needs of the whole person. 2.2. However, this issue is of crucial/urgent importance. In the words of James Mercy from the Center for Disease Control in Atlanta, Georgia, ‘Imagine a childhood disease that affects one in five girls and one in seven boys before they reach 18; a disease that can cause dramatic mood swings, erratic behaviour, and even severe conduct disorders among those exposed; a disease that breeds distrust of adults and undermines the possibility of experiencing normal sexual relationships; a disease that can have profound implications for an individuals future health by increasing the risk of problems such a substance abuse, sexually transmitted diseases, and suicidal behaviour; a disease that replicates itself by causing some of its victims to expose future generations to its debilitating effects. Imagine what we would do as a society if such a disease existed. We would spare no expense. We would invest heavily in basic and applied research. We would devise systems to identify those affected and provide services to treat them. We would develop and broadly implement prevention campaign’s to protect our children. Wouldn’t we?’ 2.3. One of the main findings from our discussions was the level of stigma associated with this problem. Society’s uneasiness and reluctance to engage with this topic is a reflection of the secrecy that occurs within the family of origin similar to domestic abuse or other trauma occurring within the ‘sanctity’ of home. It is difficult to talk about this issue because: As a society, we are far from comfortable in talking about sex. Under-age sex is deemed particularly problematic to talk about. Where there is sexual abuse, there is often secrecy, denial and collusion, which again makes it difficult to talk about in an open way. There can also be threats of violence if any disclosures are made and these threats can remain powerful even when the child becomes an adult. Staff working with survivors are fearful of being perceived as abusive or re-traumatising when asking questions. Partly this is related to a need for the staff to gain confidence in working with this material. It is also an expression of the dynamics that are recognised in working with this group. The survivor, basing their expectation of contact on their early traumatic relationships can unconsciously re-enact these causing the interviewer to variously feel abusive or caring, idealised or denigrated with the survivor occupying the opposite role. Understanding this is central to working in a helpful therapeutic way. 2.4. However, so long as adults decline to provide the space for such matters to be discussed openly in a safe manner, children remain vulnerable to abuse and survivors struggle to articulate their experiences in ways that promote their recovery and healing. 7 2.5. The scale of the challenge is clear. We suggest a response that both strengthens existing good work in this area and enhances the capacity of the whole system of public services (statutory and voluntary) to rise to this challenge in partnership. There are already a number of national initiatives which can be built on with survivors needs in mind. We also need to ensure local strategy makes these links and provides a firm basis for local work. 8 3. Policy Context 3.1. Childhood sexual abuse is increasingly recognised as a major cause of morbidity and mortality. Two recent World Health Organisation (WHO) reports – World Report on Violence and Health (2002) and World Health Report 2002 (2002) – acknowledge that CSA is common in both females (20%) and males (5-10%). This chapter deals largely with health and social policy, whilst recognising there are other areas of work, for example in criminal justice policy that are relevant. 3.2. The main effects of childhood sexual abuse in adulthood are psychological, although the behavioural, social and physical consequences are no less important. As a result, mental health policy has the biggest impact on the development of appropriate services. Yet until recently, the major policy documents in this area have paid little attention specifically to the needs of adult survivors as is illustrated below. 3.3. Mental health policy in Scotland is set out in a number of key documents. The Framework for Mental Health Services in Scotland (1997) sets out the structures and design of services predominantly for people with severe and enduring illness. Working Together for a Healthier Scotland (1999) raises the importance of mental health promotion as a key component to public health strategy. Our National Health (2000) provides further impetus in this area with the development of a national programme for mental health and wellbeing. It also adds in the need for better services in primary care for people with mild to moderate mental health problems. More recently, the Mental Health (Care and Treatment) (Scotland) Act (2003) has been passed, emphasising the need for improved care and treatment services locally. However, despite evidence that points to significant mental health problems experienced by survivors, these documents rarely mention survivors’ needs. 3.4. Mind the Gaps – Meeting the Needs of People with Co-occurring Substance Misuse and Mental Health Problems (2003) makes a valuable contribution to current thinking on how best to respond to complex care needs, particularly so as survivors often appear in such services. It recommends the ‘earlier detection of abusive experiences, by facilitating disclosure and acceptable intervention’, the need for ‘staff trained to develop skills and confidence necessary to identify and understand clients with co-occurring problems’. 3.5. There is wide recognition for the impact of sexual abuse in children’s policy in Scotland. Recent work in the area of child protection began before devolution with Protecting Children – A Shared Responsibility (1998). For Scotland’s Children (2001) calls for more integrated working across all services. It’s Everyone’s Job to Make Sure I’m Alright (2002) puts a focus specifically on agencies involved in child protection, and growing concerns about internet abuse and child prostitution emphasise the need for continued vigilance. Links have been made between child protection and domestic abuse, but until now, there has been little recognition of the links between child protection and adult survivors of childhood sexual abuse. For example, links are not currently made in child protection documents between the needs and welfare of adult survivors, and the needs of abused children, nor between domestic violence and CSA; nor are the strengths and knowledge which survivors may have to offer acknowledged. 3.6 Recognising the links between the needs of child and adult survivors is important, both to help spread awareness and knowledge, and to provide recognition that for some survivors abusive experiences can be a life-long burden. For example, the experiences of survivors of sexual abuse in institutional care settings can be so painful and unhappy that their ability to trust 9 others has been shattered, and their feelings of anger, guilt and self-worth can inhibit how they build and maintain relationships. Despite this, survivors often have great resilience, and it is not uncommon for partners, relations and family networks to be unaware of past abuse and, even for those that do know, can result in relationships which are strained, placing significant pressures on family members to remain supportive. These are sensitivities that need to be taken into account when working with survivors, and their families, and in how services should be configured to best meet needs in the short, and longer, term. 3.6. The Scottish Needs Assessment Programme (SNAP) Report on Child and Adolescent Mental Health (2003) points out the connections between family circumstances (including abuse) and mental health problems. In many instances, mothers disclose their own experience of abuse after it has happened to their child. Clearly there are links to be made between this work on child and adolescent mental health and the service response for adult survivors. 3.7. Despite the evidence in the literature, there is even less recognition of the effects of childhood sexual abuse on adults in other services. These include substance misuse, criminal justice, gynaecology, maternity and primary care services. 3.8. The Department of Health Strategy for Women’s Mental Health Services points out that this under-recognition and lack of understanding of behavioural and physical consequences of sexual abuse in childhood can lead to a re-traumatisation of survivors by the services ostensibly there to help. 3.9. The National Programme for Improving Mental Health and Wellbeing (2003) offers some signs of the shift in thinking that is required to help adult survivors. One key aim of this programme is to reduce stigma and discrimination among people with mental health problems. Adult survivors and service providers have many concerns around the stigma and discrimination they experience, which again puts survivors at risk of re-traumatisation. A further key aim is to reduce suicide and self-harm with more details of this set out in Choose Life: A National Strategy for Suicide Reduction in Scotland (2002). Adult survivors are at higher risk of selfharm and people diagnosed with personality disorder (many of whom are adult survivors of CSA) account for about 15% of all suicides. Another key aim of the programme is to encourage a culture of hope and recovery. This is essential for survivors of childhood sexual abuse and is exemplified by the few specialist non-statutory services who work with this client group. 10 4. Review of the Literature in Terms of the Prevalence of CSA and the Health and Social Consequences of CSA 4.1. Definition 4.1.1. Definitions of CSA vary between studies, which makes comparison between studies difficult. For the purpose of this work the following definition has been used: ‘Any child may be deemed to have been sexually abused when any person(s), by design or neglect, exploits the child, directly or indirectly, in any activity intended to lead to the sexual arousal or other forms of gratification of that person or any other person(s) including organised networks. This definition holds whether or not there has been genital contact and whether or not the child is said to have initiated, or consented to, the behaviour’1. While this is a broad definition of CSA, there is evidence that adverse outcomes can result from all types of CSA. 4.2. Prevalence in the general population 4.2.1. Childhood sexual abuse is common. Historically, however, the prevalence of CSA in the UK has been underestimated at 12% for females and 8%2 for males. Comparing the estimate for females with international studies shows that this estimate is at the lower end of the range (736%). The World Health Organisation (WHO) puts the prevalence of CSA at 20-25% for women3. Using the equivalent WHO estimate and findings from the international literature, a prevalence of 5-10% is the best estimate for men. 4.3. Prevalence in other populations 4.3.1. Some populations are at higher risk of CSA, and the adverse effects of CSA, than the general population. Studies of these populations have followed a number of different study designs, and are of varying quality. The effect of study design is best illustrated by looking at the estimates from uncontrolled studies of substance abuse services and gynaecology clinics which reported the prevalence of CSA in women as 90%. These estimates from uncontrolled studies have therefore not been quoted in Table 1. The range of prevalence for these populations is useful for planning services. Population Psychiatric inpatients4: Homeless5: Substance abuse6-10: GUM clinics11: General practice12: Students (non-contact CSA)13: Students (contact CSA)13: Prevalence by gender 13-70% (F) 38-50% (F); 32% (M) 37-51% (F); 24% (M) 37% (gay and bisexual M) 20% (F) 54-59% (F); 27% (M) 21% (F); 7% (M) Table 1. 4.4. Severity 4.4.1. More severe outcomes can be predicted if the CSA is frequent and prolonged, involves penetration and/or is perpetrated by somebody who is known by the abused – such as a family member. Nonetheless, adverse outcomes can also occur following less severe abuse14. The prevalence of more severe abuse is more difficult to estimate with certainty. However one well designed Australian study of the general female population provides a useful breakdown into 11 severity of abuse15: 32% described some form of CSA, 25% reported CSA involving physical contact, 20% reported abuse involving contact with the victim’s or perpetrator’s genitals, and 6% involved actual penetration. A UK survey of young people (16-24 year olds) conducted by the NSPCC found a prevalence of non-contact CSA of 21% for females and 11% for males, and a prevalence of contact CSA of 16% for females and 7% for males16. 4.5. Routine data 4.5.1. Health service data does not provide an accurate estimate of prevalence of childhood sexual abuse (CSA) either overall or within high risk populations. Between 1999-2002, for the whole of Scotland, only 13 hospital discharge records coded for child abuse, none of which was for CSA (Scottish Morbidity Records – Information and Statistics Division). In Scotland for 2000-01 the prevalence of sexual abuse using GP spotter data was 0.01% for males and females under the age of 18 (Continuous Morbidity Recording – Information and Statistics Division). Only 10-17% survivors report CSA to child protection services 17-19. Clearly these figures reflect inaccuracies in reporting. Open Secret a voluntary organisation covering Clackmannanshire, Falkirk and Stirling recorded 254 referrals (42 males and 212 females) to their service in 2003. 217 of these referrals were survivors seeking support specifically relating to consequences of childhood abuse. 4.5.2. In Dundee, a sectorised psychodynamic psychotherapy service accepted referrals outside catchment for adults with a history of childhood sexual abuse and recorded 578 referrals over a 6 year period between 1996 and 2002. 183 men were referred, 84 of these men had a history of childhood sexual abuse which was the precipitant for the referral, and 99 men were referred for psychotherapy who did not report a history of CSA. Of the 395 women referred, 175 had a history of childhood sexual abuse and were referred specifically for difficulties relating to this, and 220 women were referred for psychotherapy who did not report a history of CSA. All these patients completed self report questionnaires (SCL90) which are currently being analysed. 4.5.3. The above is an example of the serious under collection of statistics vital to designing services in this much needed area. 4.6. Outcomes in adult survivors of CSA 4.6.1. Adverse effects of CSA are common and serious and include psychiatric, physical health and social problems. There is not, however, a common outcome or syndrome that results from CSA. One model for understanding the interrelation between exposures and outcomes following CSA is proposed below. This model acknowledges the links between different forms of childhood abuse. While this work does not explore the relationship between CSA and other forms of trauma, including childhood physical abuse (CPA), childhood neglect or domestic violence, it is clear that there are important similarities between these types of trauma. 12 4.7. Risk and resilience factors 4.7.1. Well-designed studies of risk factors for CSA are rare, partly due to CSA not being reported until many years after the abuse, meaning it is difficult to measure the exposures being studied. Nonetheless some insights are available from the literature. Finhelhor (1986) reports on a range of risk factors, including gender, girls > boys, age at onset, step-father families. Parental substance misuse, including alcohol misuse, places the child at increased risk of CSA20 and child abuse in general21. An impaired relationship between the primary caregiver and child is a potent risk factor for CSA22-24. Uncontrolled studies suggest that self-blame, denial or avoidance are associated with an adverse outcome25. Furthermore, if a mother has suffered CSA or disruption of care in her own childhood, her child is more likely to have behavioural problems if she/he experiences CSA21. Finhelhor does state however that lower socio-economic class does not increase risk, it is equal across classes. 4.7.2. Such data inevitably reflects the history of research into this complex issue. What is clear however is that responsibility for CSA lies with the abuser first and foremost; it is the abuser that presents the risk, and like other sex crimes there is no way of predicting in advance who will abuse. Risks are widespread because abusers are widespread, and children most at risk are those who have already been abused and exploited, because abusers pick them out. 4.7.3. Some factors have been shown to be protective for adult survivors of CSA. In contrast to the studies of self blame mentioned above, blame of others appears to be protective26. The social support of mother and child is an important protective influence. Social support from a primary caregiver, for example a non-offending mother, is related to a better prognosis27. ‘Connectedness’ acts as a protective factor for homeless people28. In a Canadian study of 384 adults who had experienced CSA, CPA and emotional abuse, the input of a ‘very helpful professional’ or service provider was found to increase self esteem and family functioning29. We must not forget, however, that the most important protective factor of all is prevention. 13 4.8. Adverse outcomes 4.8.1. Outcomes have been divided into three main groups: mental, physical health and social. The effects of CSA can be grouped into short-term14 and long-term30. The short-term effects often occur during the period of abuse and are difficult to study. Long-term effects typically occur in adolescence and adulthood and there is more agreement between studies. The longterm adverse outcomes were reviewed by Beitchman30 (1992). More recent evidence has been used to supplement the findings of that review. 4.8.2. Neurobiology research into the developmental and integrative aspects of the central nervous system describes changes occurring in the brain of adults who were sexually abused in childhood Bremner et al65 (2003). Numerous studies using scanning techniques have reported the negative impact on parts of the brain responsible for learning, memory and processing emotions. This scientific underpinning is essential to help us understand the mechanism of early childhood trauma and more research is needed to allow this information to become clinically relevant to aid the successful treatment of survivors. 4.8.3. While some of these studies were of variable quality, the list below demonstrates the range of problems that CSA has been linked with. In each of these areas further targeted research is required. 4.9. Mental health outcomes 4.9.1. There is good evidence for an association between CSA and the following mental health problems: Anxiety31, low self-esteem15;32, Borderline Personality Disorder, Bulimia15;33, Depression15, Post Traumatic Stress Disorder (PTSD)19;34-36 and suicide26;37;38. Some of these studies provide interesting additional information – adult survivors of CSA were almost twice as likely as the general population to be depressed8, and the experience of more severe or earlier abuse were associated with a greater risk and severity of PTSD34 and suicidal behaviour26. 4.9.2. Survivors of CSA experience a wide range of mental health problems. One study suggests that 74% of mental illness in survivors of CSA is directly attributable to CSA39. The World Health Report 2002 stated that 5-8% of self-inflected injuries, depression and alcohol, 33% of PTSD in women and 21% of PTSD in males can be attributed to CSA3. 4.9.3. Links are being made between treatment resistant depression and a history of childhood sexual abuse. Treatment resistance is well recognised and takes a considerable toll on the individual, their use of services and the practitioners treating them. It is suggested that these patients require psychological therapies as well as pharmacotherapy. For example, Nemeroff et al64 (2003) in Atlanta looked at 681 patients with chronic forms of major depression. They concluded that psychotherapy may be an essential element in the treatment of patients with chronic forms of major depression and a history of childhood trauma. 4.10. Physical health outcomes 4.10.1. There is evidence of a link between CSA and physical health problems in adult life including gastrointestinal problems, headache, obesity, pelvic pain40, premenstrual syndrome, pseudo-seizures, psychosomatic symptoms41-43, sexual disturbance15 and sexually transmitted disease44-46. 14 4.11. Social outcomes 4.11.1. Survivors of CSA have frequently experienced other adverse social circumstances in childhood. This can make evidence on social outcomes difficult to interpret. There is however evidence linking CSA with lower educational attainment47, family and relationship difficulties4750 , earlier and unsafe sexual practice15;22;51;52, some aspects of criminal behaviour53-55, substance misuse15;56;57, and revictimisation12;22;58. 4.11.2. The evidence linking CSA and future criminal behaviour is less clear than for childhood physical abuse, particularly for females53. Survivors in one US study had higher rates of ‘sexually acting out’ and runaway behaviour54. Another US study concluded that in comparison to childhood physical abuse and neglect, CSA did not appear to uniquely increase an individual’s risk for later delinquent or adult criminal behaviour, including arrests for sex crimes and alcohol. There was, however, no control group in this study55. 4.12. Use of health services 4.12.1. Adult survivors’ use of health services can be estimated from international studies. A French study estimated that between 56-80% of female survivors of CSA experience health problems in adulthood as a consequence of CSA59. Using the estimate of prevalence of CSA in women of 20-25%, it can be estimated that 10-20% of the general adult female population experience health problems as a consequence of CSA. 4.12.2. A study of 1,200 women randomly selected from a health maintenance organisation (HMO) in the USA showed that, compared to women with no history of maltreatment, women who had experienced CSA had median annual health costs ($1,606) that were $245 (18%) higher than women who had not suffered childhood trauma ($1,361). CSA had a greater effect on the use of hospital services than woman who had experienced other forms of childhood trauma who had median annual health costs $97 (7%) higher than women who had not suffered childhood trauma. Women who experienced CSA also had lower perceptions of their overall health, made greater use of primary care and had more emergency admissions60. 4.12.3. Using the estimate of excess health care costs of $245 (about £150), and the estimate that 10-20% of the general adult female population have health problems related to CSA, it can be estimated that the increased cost to hospital services in the NHS in Scotland of managing the health consequences of CSA in adult women is between £30-60 million each year. 4.13. Services for adult survivors of CSA 4.13.1 UK studies provide some insight into current services for adult survivors of CSA. 80% of medical and nursing professionals in primary care believe that CSA can result in significant health care problems, and 67% would like specific training for CSA. However, only 3-6% believe that adult patients should be screened routinely for CSA61. A study of staff in 47 addiction agencies in Scotland suggested that practitioners in these clinics believe that they are unequal to the task of working with clients who have been sexually abused6. In a study of services for male survivors of CSA, the majority of mental health professionals questioned rarely inquired about CSA in male patients and two-thirds of staff had not received specific training in the assessment/treatment of CSA10. A study in Edinburgh explored views of survivors and service providers (statutory and non-statutory) in mental health – the most striking finding of the report was the lack of consensus between sectors and within psychiatric services about the best way to help survivors of CSA62. 15 4.13.2 A health needs assessment of adult survivors in Fife surveyed service users and service providers (statutory and non-statutory)63. The health needs assessment showed that most survivors do not access statutory or non-statutory services. Using the estimate that 20-25% women have experienced CSA, 14,000-28,000 women in Fife would be expected to experience complications of CSA over their lifetime. The estimated number of male and female survivors accessing voluntary services over one year was 1,200. Statutory services could not provide an equivalent estimate, and there was a wide variation in the proportion of inpatients identified as survivors in different acute psychiatric units. One unit estimated that 20% of patients were survivors of CSA while another identified only seven survivors in the previous year. Existing data from the voluntary sector may therefore provide the best idea of current service use by survivors. Non-statutory and statutory service providers identified that survivors approached services for many reasons, the most frequent were: mental ill health (76%), self-harm (71%), alcohol (58%), domestic violence (36%), homelessness (25%), abuse of another family member (23%), sexual assault (20%), and physical ill health (17%). 16 5. Models of Service for the Care and Treatment of Adult Survivors of Childhood Sexual Abuse 5.1. A significant problem for survivors of sexual abuse is that CSA is not widely recognised as a major contributing factor to a range of seriously disabling behaviours such as self-harm and substance abuse. It is therefore unsurprising that the emphasis in practice is largely placed upon treating the symptoms and minimising harm rather than supporting service users to explore aspects of their sexual abuse history which are problematic for them, and develop strategies for coping positively with daily life. 5.2. Most service providers are working under considerable time pressures and stress. As a consequence, they can often be reluctant to address possible underlying causes of physical, psychological or behavioural problems. A serious concern about broaching the issue of a sexual abuse history with service users or starting working on trauma issues is evident in both voluntary and statutory mainstream services. Many staff in these services do not feel sufficiently confident in their skills or supported enough emotionally to be able to ask questions that might ‘open a can of worms’. Often staff are worried that they will not only do more harm than good but that there are also few specialist services available to refer service users on to if appropriate. 5.3. This problem is compounded by the difficulty many survivors have about trusting professionals enough to share their stories. Disclosure is not a one off event but a process which requires a trusting relationship built up over time. (It is important to stress that not everyone who has experienced abuse wishes to engage in further exploration or treatment and they should not feel that if they don’t they are avoiding something). 5.4. Male survivors of childhood sexual abuse experience many of the same feelings and issues as female survivors. There are however particular issues that are unique to male survivors: Society has difficulty in recognising the fact that men can be and are sexually abused. Young males are generally brought up to believe that they are ‘the stronger sex’, ‘the protector’ and so the concept of being a victim is extremely difficult to accept. Being unable to prevent the sexual abuse can be perceived by many male survivors as a loss of their ‘manhood’. Sexual abuse can cause heterosexual men to experience great anxiety about their sexual identity due to the mistaken belief that only gay men are sexually abused. There is an incorrect, but nevertheless widely held, view that men who have experienced abuse will go on to abuse children. Issues such as these can make it very difficult for men to feel safe about going to statutory services for help. 5.5. Although this report primarily addresses the needs of those who have experienced sexual abuse in childhood, the impact sexual abuse has on particularly vulnerable groups within society should not be overlooked. Older people, those from ethnic minorities, and people with physical and learning disabilities, can and do find themselves targeted by abusers, who may be relatives, close friends or carers. Exploitation of a trusting relationship is often very difficult for a survivor to cope with, let alone report, and may be compounded by some impaired capacity. Each vulnerable group present with particular needs and require flexible and tailored responses, 17 but which can nonetheless be delivered within a framework of better integrated services for survivors. 5.6. Moreover, problems continue in health and social care sectors, and in criminal justice services, in responding to sexual abuse allegations, and in prosecuting perpetrators because of perceived difficulties in the credibility and reliability of the victim. The House of Commons’ Health Committee Report on Elder Abuse (2003-04) highlights such service failings and has called for significant improvements to respond to victims’ needs. In responding to the SWSI and Mental Welfare Commission reports into the care of Miss X case in the Scottish Borders, the Scottish Executive has also accepted the need for added protections for vulnerable adults. 5.7. What qualities do survivors value? 5.7.1. What, however, was of prime importance were the particular qualities staff had. Sarah Nelson highlights these qualities in her report: 5.7.2. ‘Survivors described a small minority of staff from statutory, voluntary and independent sectors as tremendously helpful, or even life-changing. They were catalysts to the survivors making major improvements to their lives – for instance stopping drinking, having children returned from care, returning to university, making satisfactory personal relationships, returning to work, or freeing themselves from a lifetime of depressive illness. The characteristics of these staff, as described by survivors, were strikingly similar across the sectors – an impression confirmed when it was possible for the researchers to meet and interview them. They were secure and firm about boundaries, but related with warmth and kindness. They were informed and aware about the main effects of CSA trauma, or keen to become so, and had examined their own personal issues around working with sexual abuse. They worked non-hierarchically, consulting respectfully with survivors about what their main needs were and what their service could offer – trying to reach joint decisions about whether the service would be helpful, or about the work they would do together. They allowed survivors to talk about their abuse history whenever they wished, but did not pressurise them into doing so. They were skilful, flexible, imaginative and eclectic, sometimes ‘breaking the rules’ of their service in the client’s interest. They neither hid behind confidentiality nor broke it insensitively, consulting with the client about what information ought to be shared, and what need not be. They did not fear to persist in asking tactfully if a client had experienced childhood sexual abuse trauma, and they had the courage to stay with clients through distressing, frightening symptoms or behaviour. They were prepared to work consistently over a period of time: although brief contacts had sometimes proved a dramatic catalyst to survivors changing their lives. However They did not come from any one professional background or therapeutic approach and did not necessarily have high professional status, ranging from volunteer counsellor or project worker to staff nurse, social worker or consultant psychiatrist. A majority had not attended specific training courses on child sexual abuse, although they had gathered expertise in other ways. 18 5.8. Not all had support or supervision, although all thought these were essential.’ (Nelson, Beyond Trauma, (2001) p. 116) Service models 5.8.1. The issue of access to appropriate services is important for both service users and service providers. 5.8.2. Survivors need to be sensitively supported to explore their sexual abuse history at a pace appropriate to them by staff who feel confident and who can offer safe, helpful responses to disclosure. It is usually non-specialist frontline services, dealing with issues like substance misuse, homelessness or distressed behaviour, that survivors approach first for help, or to which they are referred for ‘presenting problems’. Very often however, these staff do not feel equipped to deal with the subject of childhood sexual abuse. Recipients of disclosure should be trained to avoid panic and possible unnecessary referral to specialist services, especially since many survivors do not wish constantly to be ‘referred on’. This raises training issues which are picked up in more detail in the next chapter. 5.8.3. There are currently a limited number of discrete specialist services for survivors, the majority of which are provided by the voluntary sector. It is more common that projects cover other issues (e.g. rape, domestic violence) than they are discrete services. In this chapter, we give a few examples of both types of project, in the statutory and voluntary sectors. A more detailed list is available from the Register of Services for Scotland on Violence and Abuse, published by the Women’s Support Project, Glasgow (currently being updated for 2004). 5.9. Examples in the voluntary sector 5.9.1. The Open Secret project in Falkirk offers individual counselling and a range of support and self-help groups to adult survivors of sexual abuse (16 plus). In Kirkcaldy, the Kingdom Abuse Survivors Project (KASP) offers a similar wide range of services; both these projects work with women and men. KASP offers one-to-one support, information and advice and a range of groupwork to survivors and their families, and includes a specific mental health post. 5.9.2. In Dundee, the Eighteen and Under project offers a range of support services(face-toface and telephone) and information to young people under the age of 18 who have experienced sexual, physical or emotional abuse, including ritual and satanic abuse. Based in Airdrie, the Moira Anderson Foundation offers services, information and support to survivors, families and others affected by sexual abuse from across Scotland. It also runs a safe house. 5.9.3. In Glasgow, Men Against Sexual Abuse (MASA) offers telephone support and one-toone support, while in Dundee, M Line offers telephone support, groupwork and one-to-one support for males. In Glasgow, Say Women offers accommodation and follow-on support to young women who have survived sexual abuse. The Rape and Abuse Line in Dingwall gives telephone support and one-to-one support to both women and men. Health in Mind, Edinburgh provides dedicated services of counselling, groupwork and one-to-one support to survivors. The majority of voluntary sector projects also offer training to a wide range of agencies. 5.9.4. In some voluntary sector projects, sexual abuse work is prominent but other issues including other sexual violence, domestic violence or prostitution are also covered. Such projects include the Women’s Support Project in Glasgow, Edinburgh Women’s Rape and Sexual Abuse Centre, and the Scottish network of Rape Crisis Centres. 19 5.9.5. The Central Scotland Rape Crisis Centre in Stirling works on the principle of not concentrating on the particular abuse but in raising the self-esteem and worth of survivors to help them make sense of how their experience has/is affecting their lives, while respecting their rights as individuals and empowering them to make their own choices as to what is best for them in their life. The South West Rape Crisis & Sexual Abuse Centre offers face-to-face counselling, an outreach service, and run a refuge. 5.9.6 Breathing Space, currently covering the West of Scotland, is a freephone service for people with depression or low mood. Wounded Wings, Edinburgh is a support project for selfharming people, many of whom are abuse survivors. 5.9.7 Stop it Now is a UK-wide project that provides telephone advice to people at risk of perpetrating abuse on children, their friends and relatives. They have been able to encourage people to go to the police rather than wait to be caught. 5.10. Examples in the statutory sector 5.10.1. In the statutory sector some psychiatric hospitals or units run special programmes to help survivors address issues arising from their abuse. For instance nurse-led, modified Cognitive Behavioural Therapy (CBT) programmes and longer-term work with complex trauma are available at St John’s Hospital Livingston, while longer-term nurse-led work with complex trauma is available at Cambridge Street Day Hospital in Edinburgh. Most psychotherapy departments receive a significant proportion of referrals with a history of childhood sexual abuse and will offer individual and group outpatient psychotherapy as appropriate. These services are not seen as being specific to CSA but are in response to the demand of the clinical population and might benefit from more coordinated contact with other agencies to facilitate an integrated programme of intervention addressing complex needs. 5.10.2. Other statutory projects feature sexual abuse prominently but also cover a wider range of issues. For instance the Eva Project in Coatbridge, a health initiative, covers all areas of male violence against women and offers a range of services including information and advice, counselling, and advocacy. The Centre for Women’s Health in Glasgow, another health initiative, offers one-to-one and group support, drop-in and library facilities, among other services. The sexual abuse service run by the Psychotherapy staff based at the Lansdowne Clinic in Glasgow offers therapy and counselling to survivors, and support to counsellors themselves. Breakthrough for Women in Glasgow, a social work initiative, provides support, counselling and information, includes counsellors with a range of ethnic minority languages and covers rape, sexual abuse and abuse through prostitution. The Sexual Abuse/Sexual Assault Clinic based at Stobhill Hospital in Glasgow has been providing a multi-disciplinary therapy service to women and men for 10 years. This includes an innovative dual-problems clinic for people with substance misuse and history of sexual abuse/assault. They also provide consultancy and training support to staff. 5.10.3. Despite their statutory basis, some of these services do not receive dedicated funding, sometimes relying on underspends to continue operating. This creates real uncertainty for staff, and inhibits forward planning. Some NHS boards offer, or are in process of establishing, multidisciplinary teams who do specialist work with people with complex trauma symptoms (e.g. heavy substance misuse, suicidal and self-harming behaviour). Many of these are sexual abuse survivors. One example is Ayrshire & Arran NHS Board which has a residential unit and care programmes run by teams that include psychiatrists, community psychiatric nurses, occupational therapists and social workers. 20 5.10.4. Evidence for different types of psychological interventions is currently being collected and analysed for a Cochrane Review. 5.10.5. Current victim support services do not adequately support adult survivors. This is because very few survivors take legal action. Those that do, and are referred to victim support services, find they are referred onto survivor support agencies. 5.11. Particular issues for the voluntary sector 5.11.1. The precarious state of voluntary sector funding means that very few projects have the security of consistent long-term funding and the majority spend a significant amount of staff time engaged in fundraising activities. Very short-term funding brings with it difficulties in staff recruitment and forward planning. In particular, despite the considerable cost benefits for health services when voluntary sector projects work successfully to reduce trauma in high health service users, it is rare for NHS boards to provide any kind of regular funding for such projects. In research for Health in Mind’s needs assessment of services for male survivors questionnaire (forthcoming) evidence showed that the most popular choice by statutory services for referring on clients was ‘the voluntary sector’. 5.11.2. A point highlighted in the Scottish Parliament’s Cross-Party Working Group on Survivors of Childhood Sexual Abuse – Survey of Support Services is that time-limited funding does not recognise the fact that child sexual abuse is not limited to any timescale and that it is frustrating that projects are continually required to be ‘innovative’ in order to attract funding. This ‘innovation requirement’ effectively discriminates against established agencies concentrating on improving practice and evolving naturally. It is stressed that core funding is vital in circumstances where a project is proving itself to be meeting needs so that it can continue in a more certain climate. Only two out of the 48 agencies surveyed had the reassurance of long-term funding and only 23 agencies had levels of funding that enabled proper salaries to be paid to staff. 5.11.3. The voluntary sector projects are staffed by people who bring to their posts a wide range of experience, qualifications and professional expertise. A significant number have health, social work or counselling and psychotherapy qualifications and experience and yet the sector is too often seen by statutory services as ‘insufficiently trained, reliable or qualified’ (F. Biggam, Clinical Psychology Services for Individuals who have experienced Childhood Sexual Abuse or Adult Sexual Assault in the Greater Glasgow Locality , S. Nelson, Beyond Trauma). This kind of thinking can inhibit the development of joined-up responsive services for survivors. 5.12. Developing integrated services 5.12.1. Given the complexity and diversity of issues arising from CSA it is essential that a range of services is developed for survivors. These can be provided by the voluntary, statutory sector and private sector and should promote the principle of inter-agency working. 5.12.2. The Beyond Trauma report highlighted a number of service models that were identified by both survivors and professional workers as being extremely beneficial. These included a 24hour telephone helpline, a crisis house, counselling, groupwork (both self-help and facilitated therapeutic work), respite and services that are able to work with and stick with people who present with challenging behaviours. 21 5.12.3. Alison Richardson in her presentation at the Mind the Gaps conference presented a model that illustrates how this integrated approach might look. Grades of Care 5. Highly Specialised 4. Specialised 3. Generic and Specialist 2. Generic Services 1. Community and Social Response 5.12.4. She highlighted the following necessary key features of service provision: Early intervention, avoiding inappropriate referrals to expensive specialist services; Social education and employment elements; Person centred interventions, not ones based on existing service availability; Advocacy; Positive expectations emphasised to clients and providers. 5.12.5. These models of care are similar to that proposed by the NHS Mental Health Framework document in the delivery of psychological therapies. Underpinning this framework is an acceptance of multi-disciplinary working and needs appropriate access to a tiered model of intervention. The services can range from information and education in the community to tertiary referral service specifically addressing severe and enduring aspects of the sequelae of CSA. 22 6. Awareness Raising and Training 6.1. This chapter outlines the issues around the need to raise awareness and provide training. It makes some proposals for the content of training programmes. 6.2. Service providers have real issues in terms of their perceived capacity to deal with this issue. In one study of addiction services across Scotland, practitioners stated that they were unequal to the task of working with clients who have been sexually abused. Similar conclusions were made in another London study of males attending alcohol addiction services. In another UK study, primary care professionals (general practitioners, practice nurses and health visitors) were asked about women survivors of CSA and domestic violence. While over 80% believed that CSA can result in significant health care issues, only 3-6% believed that adult patients should be routinely screened for CSA. 67% of professionals would have liked specific training for CSA. 6.3. ‘More training is needed’ has become a catchphrase in reports. Policy makers and funders are so used to reading it that some may be quite dismissive if they read it again. However, raising awareness of this issue and providing a substantial, accessible training programme is central to improving services in Scotland. Staff and volunteers who work with adult survivors through medical and mental health agencies, social work, criminal justice system, and many community-based projects need to feel comfortable and confident about doing so. The public too needs a better understanding of the issues, if we are to encourage abusers as well as survivors to seek help. 6.4. A number of studies (e.g. Read & Fraser 1998a, Read & Fraser 1998b, Goater & Meehan 1997) have shown widespread and persistent failure to inquire about a CSA history in psychiatric settings. This is so even when such a protocol is in place and despite the high probability that these patients or clients have such a history. Nelson (2001) found staff discomfort about working with the CSA issue was a significant barrier to support services being available, at both assessment and treatment stages, to survivors in mental distress. In children services, there are particular difficulties arising from abuse in residential settings. A child may have already lost parents and, if the person to whom they have been entrusted abuses them, then the child has few escapes, and often no extended family to contact. 6.5. Among reasons for failing to address issues of care and support for survivors of CSA trauma are listed below. It can be a very difficult issue to address personally for various reasons, so people often avoid it. Staff lack training or confidence to discuss CSA with survivors, or to handle a disclosure, and don’t know what action to take; so again try to avoid the issue. Many staff believe encouraging survivors to talk about their trauma will automatically make them feel worse, or believe they must work with survivors for a very long time to avoid this. Some agencies working with vulnerable, distressed or ‘troublesome’ people don’t see any need for training because they don’t see the relevance of CSA to their own work – yet many clients have a CSA history. Sometimes they deny a training need because a remit has been set ‘from above’ which is assumed to exclude CSA problems (e.g. mental health staff told to concentrate on ‘severe and enduring mental illness’). 23 6.6. These reasons relate to a need for the staff to gain confidence in working with this material. It is also an expression of the psychodynamics that are recognised in working with this group. The survivor, basing their expectation of contact on their early traumatic relationships can unconsciously re-enact these causing the interviewer to variously feel abusive or caring, idealised or denigrated with the survivor occupying the opposite role. Understanding this is central to working in a helpful therapeutic way. 6.7. Training programmes over a range of disciplines is important to break down these barriers. Awareness-raising and discussion, rather than detailed and complex learning modules or guidelines are the priorities for frontline staff in non-specialist mental health agencies. 6.8. Awareness raising 6.8.1. There is a need for more public awareness of the issues around childhood sexual abuse and how to protect children from perpetrators. There is also a need for people to know where to get help as survivors or as potential perpetrators. 6.8.2. For staff, awareness raising should include: Relating common effects of CSA trauma; Discussing relevance of CSA to their particular client group; Addressing staff feelings about working with CSA; Dealing with disclosure and tactful inquiry; Exploring what survivors most value in professionals. 6.8.3. This training would be especially useful for anyone who works in an environment where there are going to be a lot of clients with a history of CSA. This includes psychiatric units, prisons, special hospitals, primary care, children's home/secure units, Accident and Emergency departments, self-harm projects, drug and alcohol projects, reproductive health, eating disorder projects, counselling projects, schools for emotional/behavioural problems, homelessness work etc. 6.8.4. Outcomes from such training would include: Staff hear and handle a disclosure without panic, with far more confidence and refer people on if necessary; Staff feel able to ask sensitively if client had a CSA history and if he/she felt any particular problems had resulted from it; Staff are able to give more appropriate care, support and referral; Staff record data, enabling sounder research on prevalence. 6.8.5. The Scottish Executive has recently funded Health in Mind in Edinburgh to investigate training issues. In particular, the project aims to establish what the more useful basic and specialist training courses are for this (staff who work with sexual abuse survivors) wide range of staff. A training review group will be set up to study the implications of this report, explore existing innovative models of training and report within one year. The project also aims to ensure that staff in all agencies that are in regular working contact with sexual abuse survivors undergo whatever ‘basic sexual abuse awareness and information’ course is proposed by this review group. This should particularly aim to build self-confidence, develop safe, sensitive means of exploring a sexual abuse history, and encourage safe, helpful responses to disclosure. 24 6.8.6. This is an important development and should complement and expand the measures suggested in this chapter once it is completed. 6.9. Training for medium-term and/or time-limited work. 6.9.1. Examples of this include structured group programmes, or individual counselling, for CSA survivors who seek help – from a variety of disciplines, agencies and theoretical approaches, e.g. person centred CBT. 6.9.2. This training would be particularly helpful for people doing support work in mental health and social work and prison teams, health visitors, counsellors, phone helpline staff or volunteers, organisations working against sexual violence, and many other settings. 6.9.3. Examples of this type of support and training are found in Open Secret, Health in Mind and many other non-statutory services who provide support and counselling to adult survivors. 6.9.4. Outcomes would include: More confidence in mental health and social work teams or workplace that the issue can be tackled ‘above board’; Reduction of multiple referrals to other agencies and services; Avoidance of situation where one CPN, nurse, social worker or other team member becoming overworked because of their willingness to take on survivors of sexual abuse with more people trained at this level, staff with basic awareness training know there is someone they can recommend to their clients for further work. 6.10. Training in long term support and specialist work with complex trauma 6.10.1. The client group in this case is the smaller number of survivors with extensive psychological and behavioural problems. There are a range of approaches e.g. psychoanalytic, CBT, person centred, dialectical behaviour therapy, eye movement resensitisation and reprocessing, that can provide therapy to these severely affected survivors. Work may last several years. Only a small minority of staff will wish to take on this stressful and difficult work and will need strong support in the work setting. 6.10.2. Examples where this level of training and support exists include Psychotherapy Departments in Glasgow, Edinburgh, Dundee and Aberdeen, at the Sexual Abuse/Assualt clinic at Stobhill, at St. John’s Hospital Livingston, the Cambridge Street Day Hospital, Edinburgh, and some of the Eighteen and Under’s specialised work in Edinburgh on organised satanic abuse. (see sections 5.8 and 5.9 above for more detail). 6.11. Outcomes from training in at this level include: Appropriate referral for specialist care and treatment; Appropriate care and support for people who had previously been ‘written-off’ as the most intractable, troublesome and ‘personality-disordered’ clients; Staff may be a particularly valuable source of training, consultation and insight. 25 7. Conclusions and Recommendations 7.1. This brief report can only be a starting point for more wide-range discussions around the issues it raises in all areas of public life. However, it is possible to draw some interim conclusions from the work so far and propose some recommendations. 7.2. A policy framework 7.2.1. From a policy perspective, it is essential that adult survivors work is integrated into existing areas of activity, rather than spawning a whole new infrastructure and subspecialisation. Sexual abuse in childhood is a social and cultural phenomenon with potentially damaging effects. It requires above all, a recognition that it happens and that its impact can be lifelong, and not only in childhood, where existing policy focuses. Provision of help and support to children at the time abuse happens will always remain important, but more can be done to recognise and plan for continuing need in later life. To achieve the broad-based shifts in policy required for such a difficult yet common problem requires that it is integrated with policy development and practice around child protection and domestic abuse. 7.2.2. There are also important links to be made with mental health policy. Psychological services should be responding explicitly to the needs of adult survivors. This could be brought out in the psychological services addition to the national framework for mental health services. Services need to consider CSA survivors at all levels of service provision. This should become an aspect of performance management of mental health services. Recommendation 1 The Scottish Executive should incorporate the issue of adult survivors of childhood sexual abuse into policy developments around child protection, domestic abuse and mental health services. This policy work should cover prevention, treatment, support and recovery from the effects of childhood sexual abuse. 7.3. Need for awareness raising 7.3.1. Current work on developing better responses to the needs of adult survivors is hampered by the lack of awareness of the stigma and discrimination that these people feel. Survivors of childhood sexual abuse are not responsible for what happened to them – the perpetrators are. Yet often they feel they carry the guilt of the abuse themselves. A more positive climate of discussion, honesty and safe space for letting go of these feelings would be very helpful. There are strong links here with the See Me campaign. Survivors themselves would be interested in developing programmes to reduce stigma in this area. Recommendation 2 There needs to be a broad-based awareness campaign that challenges current public and professional attitudes. The campaign should make the links between childhood abuse and adult mental health problems. It is suggested that adult survivors are involved in the development of the campaign and that links are made to See Me the national campaign tackling stigma and discrimination. There is also a role for NHS Health Scotland in counteracting the secrecy associated with sexual abuse. 26 7.4. Training for staff 7.4.1. A key target audience for awareness raising are staff in frontline services. Much has been achieved around the issues of child protection and domestic abuse in Scotland. A similar effort is now needed to raise people’s awareness and ability to deal with disclosure by adults of abuse that they experienced as children. As models of care develop, further training is required for specific groups of staff to take on the counselling and support role required. 7.4.2. We need to be mindful of what survivors say about the staff who have been able to help them and involve survivors in training. Much of this training need not be additional. Instead, existing programmes for example on communication skills for doctors and nurses and for family care courses could include CSA issues as areas for improving skills. NHS Education Scotland and equivalent social work and criminal justice training bodies should incorporate these training needs into their programmes. 7.4.3. Also where there are training programmes for vulnerable groups, the issue of sexual abuse in childhood can be integrated. For example, in STRADA training for staff work with people who misuse drugs. Recommendation 3 There needs to be a training strategy that puts childhood abuse on the curricula for basic training in nursing, medicine, social work and criminal justice (including police). For post-graduate training, we recommend the issues for adult survivors are integrated with training for child protection, domestic abuse and patient communication. 7.5. A Quality Issue 7.5.1. For the vast majority of adult survivors, a more humane, open and empathetic service response is all that is required. This sounds simple and could be if the quality of services was assessed on these criteria. For survivors accessing support services, there is scope to incorporate these features into quality assurance with survivors themselves helping in the design of systems and their monitoring. Above all is the necessity to avoid re-traumatisation by services. It is also necessary to recognise the impact of abuse on the partners of survivors. These earlier experiences can present problems within relationships, and services should be capable of meeting such need. 7.5.2. Commissioners of mental health services should also recognise the need for gendersensitive services for adult survivors. For example, currently many services are available only for women survivors, yet an estimated 5-10% of men are also affected. Although most mental health services are compliant with single sex accommodation standards, wards are usually mixed which may not be the best environment for survivors. Recommendation 4 NHS Quality Improvement Scotland needs to develop national standards for the care of adult survivors of childhood sexual abuse who are cared for in mental health services. These standards would incorporate the need for a gender-sensitive approach to providing services. Survivors themselves should be involved in developing these. 27 7.6. A Criminal justice issue 7.6.1. As the literature review in Chapter 4 shows, survivors may come into contact with criminal justice services because their abuse experience has led to inappropriate behavioural responses (and are often associated with substance misuse problems). At present, little is known about the extent of this problem within the criminal justice system in Scotland, particularly those on remand and on short sentences (less than 6 months) in prison. Recommendation 5 A needs assessment should be undertaken of the prison population with particular attention to those on remand and with short sentences. 7.7. A medical and nursing issue 7.7.1. The impact of childhood sexual abuse on a variety of health conditions is poorly understood, but given its prevalence, more thought is needed on its impact in clinical practice. For example, thought is needed on the possible impact this has on certain investigative procedures. The Royal College of Obstetrics and Gynaecology have produced guidelines on cervical screening that include mention of vulnerable groups such as adult survivors. Recommendation 6 Medical and nursing bodies should review relevant areas of clinical practice and develop guidelines for undertaking sensitive examinations in adult survivors of sexual abuse. Involving survivors themselves in this work would be critical to its success. 7.8. Models of care – national work 7.8.1. This report highlights the need for a structured approach to a problem of such complexity. The Scottish Executive’s change agenda provides the focus and emphasis for service change, and is ideally placed to lead and encourage coherence in improving how survivors’ needs are planned for, and met. 7.8.2. An emphasis on self-help and non-statutory service responses is likely to be sustainable. The national helpline, Breathing Space, could be developed with the need of adult survivors in mind. Self-help materials need to be tested, developed and made available widely – on the web, in schools, libraries, resource centres, health centres etc. This work links closely with the work if the National Programme for Mental Health and Wellbeing in developing awareness raising and a culture of hope and recovery. It also links with the domestic abuse prevention strategy and community-based child protection programmes. NHS Health Scotland clearly has a role to play here. Recommendation 7 NHS Health Scotland should encourage self-help tools, for instance through the marketing of Breathing Space, the national helpline as a source of help for adult survivors. The Justice and Education Departments of the Scottish Executive should develop materials for use in schools, communities and the web. Uptake should be evaluated to assess its impact. 7.9. Models of care – local work 7.9.1. As far as individual and group counselling goes, the biggest source of help in local areas tends to be in non-statutory services. Their biggest source of referrals is usually the health 28 service, yet few receive funding from NHS boards. There needs to be recognition of the different needs of male and female survivors, with skills and staff mix to match. Whilst there are both male and female survivors, it is also true that the majority of perpetrators are male. The shared understanding of gender-based violence set out in the Scottish Executive policies on domestic abuse apply here also. 7.9.2. Local partnerships are therefore essential for making an impact in terms of service provision for adult survivors. GPs in particular are a crucial first point of access for survivors seeking help. Pathways of care that connect primary care, non-statutory services and specialist mental health services can help. Again, there are models developing for domestic abuse that can be adapted for adult survivors. Indeed, there is a case to be made for local domestic abuse forums to broaden their remit to cover this area of need. 7.9.3. The existing framework for psychological services offers a useful tiered model of care (part of the National Framework for Mental Health Services in Scotland). What is needed is for psychological services to make explicit that they provide treatment and support to survivors and monitor the effectiveness of this. 7.9.4. Developing more specialist services requires the energy and commitment of local champions, who may be found in different parts of the health and social care network. Building on existing strengths and experience is important, enhancing capacity in non-statutory services and improving the training and development of staff in statutory services all helps. Again, survivors themselves are often willing to be part of induction and training packages. 7.9.5. Children affected by sexual abuse who disclose whilst still children often face an uncertain future once they reach the age of 18. There are few services available to help them manage the transition into adulthood. This needs to be brought to the attention of agencies working with vulnerable children and young people. Recommendation 8 10. Local commissioners need to urgently develop services to support adult survivors in line with best practice. This means supporting non-statutory services where they exist, ensuring they are put on a more secure financial footing, and evaluating good practice models. It also means dedicating resources towards and improving the quality of care in existing mainstream services in recognition of the strong association between CSA and significant mental health problems, reflecting the needs of survivors. More specialist services to provide support and treatment for survivors at the severe end of the spectrum are needed. There is also a need to join up approaches around services for children affected by sexual abuse and adult services in this area. Progress on implementing local service change should be monitored through the NHS Performance Assessment and Accountability Framework, and the Community Planning/Health Improvement process. 7.10. Data collection 7.10.1. Current information systems measure behavioural and pathological patterns, but not their underlying cause. Obtaining better baseline data from current services is therefore a priority. But this takes awareness raising and training for staff. Again, there is potential to link with work already underway in the area of domestic abuse, but the barriers are more cultural than technical. 29 7.10.2. For this reason, it would be helpful to set up better data collection systems in services likely to have high numbers of adult survivors such as addiction services, mental health services, prisons, primary care, genito-urinary medicine (GUM), obstetrics and gynaecology and accident and emergency. Recommendation 9 Better data collection about survivors is needed in addiction services, primary care, mental health, GUM, obstetrics and gynaecology, and accident and emergency departments. This will help to improve our understanding of the extent of the health needs of survivors. 7.11. Research and Development 7.11.1. Scotland is uniquely placed with a small scientific community closely linked to clinical services. It would be helpful to formally develop a network of practitioners and researchers from different disciplines and services alongside survivors to enhance our understanding and develop new ways of responding to the needs of this population. 7.11.2. This group would have a wide remit e.g. from evaluating good practice in settings such as voluntary sector or making inroads into the understanding of the neurobiological impact of early trauma. 7.11.3. The cross fertilisation of these approaches will enhance knowledge of the biological underpinnings of trauma which can be utilised to maximum effect in the therapeutic field. 7.11.4. A further neglected area is the preventative measures that may be developed to minimise future risk of the repeating of the cycle of abuse. 7.11.5. The Chief Scientist Office, other research bodies and the universities should be encouraged to support this area of work. Recommendation 10 It is recommended that there should be support for a network of researchers, practitioners and survivors with an interest in improving the care and treatment of adult survivors. 30 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. Protecting children - A shared responsibility. 1998. Edinburgh, The Scottish Office. Baker AW,.Duncan SP. Child sexual abuse: A study of prevalence in Great Britain. Child Abuse Negl 1985;9:457-67. World Health Report 2002. 2002. World Health Organisation. Gallop R, McCay E, Guha M, Khan P. The experience of hospitalization and restraint of women who have a history of childhood sexual abuse. Health Care for Women International 1999;20:401-16. Noell J, Rohde P, Seeley J, Ochs L. Childhood sexual abuse, adolescent sexual coercion and sexually transmitted infection acquisition among homeless female adolescents. Child Abuse Negl 2001;25:137-48. Wilson J. Abuse and misuse. The ultimate hidden population. Druglink 1998;13. Berry R,.Sellman JD. Childhood adversity in alcohol- and drug-dependent women presenting to out-patient treatment. Drug & Alcohol Review 2001;20:361. Schiff M, El-Bassel N, Engstrom M, Gilbert L. Psychological Distress and Intimate Physical and Sexual Abuse among Women in Methadone Maintenance Treatment Programs. Social Service Review 2002;302-20. Swift W, Copelan J, Hall W. Characteristics of women with alcohol and other drug problems: findings of an Australian national survey. Addiction 1996;91:1141-50. Lab DD, Feigenbaum JD, De Silva P. Mental health professionals' attitudes and practices towards male childhood sexual abuse. Child Abuse Negl 2000;24:391-409. Doll LS, Joy D, Bartholow BN, Harrison JS, Bolan G, Douglas JM et al. Self-reported childhood and adolescent sexual abuse among adult homosexual and bisexual men. Child Abuse Negl 1992;16:855-64. Coid J, Petruckevitch A, Feder G, Chung W-S, Richardson J, Moorey S. Relationship between childhood sexual and physical abuse and risk of revictimisation in women: a cross-sectional survey. Lancet 2001;358:450-54. Finkelhor D. The international epidemiology of child sexual abuse. Child Abuse Negl 1994;18:409-17. Beitchman JH, Zucker KJ, Hood JE, DaCosta GA, Akman D. A review of the short-term effects of child sexual abuse. Child Abuse Negl 1991;15:537-56. Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP. The long-term impact of the physical, emotional, and sexual abuse of children: a community study. Child Abuse Negl 1996;20:7-21. Cawson, P., Wattam, C., Brooker, K., and Kelly, G. Child maltreatment in the United Kingdom: a study of the prevalence of child abuse and neglect. 2000. London, NSPCC publications. Leventhal JM. A decline in substantiated cases of child sexual abuse in the United States: good news or false hope? Child Abuse Negl 2001;25:1137-8. Butler JR,.Burton LM. Rethinking teenage childbearing: Is sexual abuse a missing link. Family Relations 1990;39:73-80. Golding JM, Taylor DL, Menard L, King MJ. Prevalence of sexual abuse history in a sample of women seeking treatment for premenstrual syndrome. Journal of Psychosomatic Obstetrics & Gynaecology 2000;21:69-80. Blau GM, Whewell MC, Gullotta TP, Bloom M. The Prevention and Treatment of Child Abuse in Households of Substance Abusers: A Research Demonstration Progress Report. Child-Welfare 1994;73:83-94. Paredes M, Leifer M, Kilbane T. Maternal variables related to sexually abused children's functioning. Child Abuse Negl 2001;25:1159-76. Fergusson DM, Horwood J, Lynskey MT. Child sexual abuse and psychiatric disorder in young adulthood: I. Prevalence of sexual abuse and factors associated with sexual abuse. Journal of the American Academy of Child & Adolescent Psychiatry 1996;14:1355-64. Leifer M, Shapiro J, Kassem L. The impact of maternal history and behaviour upon foster placement and adjustment in sexually abused girls. Child Abuse Negl 1993;17:755-66. Paveza GJ. Risk-factors in father-daughter child sexual abuse. Journal of Interpersonal Violence 1988;3:290306. Gibson LE,.Leitenberg H. The impact of child sexual abuse and stigma on methods of coping with sexual assault among undergraduate women. Child Abuse Negl 2001;25:1343-61. Barker-Collo SL. Adult reports of child and adult attributions of blame for childhood sexual abuse: predicting adult adjustment and suicidal behaviors in females. Child Abuse Negl 2001;25:1329-41. Hazzard A, Gould J, Lawry S, Webb C. Prediciting symptomatology and self-blame among child sexual abuse victims. Child Abuse Negl 1995;19:707-14. Rew L. Relationships of Sexual Abuse, Connectedness, and Loneliness to Perceived Well-Being in Homeless Youth. Journal for Specialists in Pediatric Nursing /6;7:51. Palmer SE, Brown RA, Rae-Grant NI, Loughlin MJ. Survivors of childhood abuse: their reported experiences with professional help. Social Work 2001;46:136-45. 31 30. Beitchman JH, Zucker KJ, Hood JE, DaCosta GA, Akman D, Cassavia E. A review of the long-term effects of child sexual abuse. Child Abuse Negl 1992;16:101-18. 31. Henderson D, Hargreaves I, Gregory S, Williams JMG. Autobiographical memory and emotion in a nonclinical sample of women with and without a reported history of childhood sexual abuse. British Journal of Clinical Psychology 2002;41:129-41. 32. Whealin JM,.Jackson JL. Childhood Unwanted Sexual Attention and Young Women's Present Self-Concept. Journal of Interpersonal Violence 2002;17:854. 33. Wonderlich SA, Wilsnack RW, Wilsnack SC, Harris TH. Childhood Sexual Abuse and Bulimic Behavior in a Nationally Representative Sample. American Journal of Public Health 1996;86:1082-6. 34. Heath V, Bean R, Feinauer L. Severity of childhood sexual abuse: Symptom differences between men and women. American Journal of Family Therapy 1996;24:305-14. 35. van der Kolk BA, Pelcovitz D, Roth S, Mandel RS, McFarlane A, Herman JL. Dissociation, somatization, and affect dysregulation. The complexity of adaptation to trauma. Am J Psychiatry 1996;153 (suppl):83-93. 36. Boney-McCoy S,.Finkelhor D. Is youth victimization related to trauma symptoms and depression after controlling for prior symptoms and family relationships? A longitudinal, prospective study. Journal of Consulting and Clinical Psychology 1996;64:1406-16. 37. Briere J, Evans BA, Rutz M, Wall T. Symptomatology in men who were molested as children: A comparison study. American-Journal-of-Orthopsychiatry 1988;58:457-61. 38. Peters DK,.Range LM. Childhood sexual abuse and current suicidality in college women and men. Child Abuse Negl 1995;19:335-41. 39. Scott KD. Childhood sexual abuse: Impact on a community's mental health status. Child Abuse Negl 1992;16:285-95. 40. Briere J. Medical Symptoms, Health Risk, and History of Childhood Sexual Abuse. Mayo Clin Proc 1992;67:603-4. 41. Draucker CB,.Spradlin D. Women Sexually Abused as Children: Implications for Orthopaedic Nursing Care. Orthopaedic Nursing 2001;20:41-8. 42. Glod CA. Long-term consequences of childhood physical and sexual abuse. Archives of Psychiatric Nursing 1993;7:163-73. 43. Davidson JRT. Recognition and Treatment of Posttraumatic Stress Disorder. Journal of the American Medical Association 2001;286:584-8. 44. Pitzner JK, McGarry-Long J, Drummond PD. A history of abuse and negative life events in patients with a sexually transmitted disease and in a community sample. Child Abuse Negl 2000;24:715-31. 45. Barthalow BN, Doll LS, Joy D, Douglas JM, Bolan G, Harrison JS et al. Emotional, behavioural, and HIV risks associated with sexual abuse among adult homosexual and bisexual men. Child Abuse Negl 1994;18:74761. 46. Mullings JL, Marquart JW, Brewer VE. Assessing the Relationship between Child Sexual Abuse and Marginal Living Conditions on HIV/AIDS-Related Risk Behaviour among Women Prisoners. Child Abuse Negl 2000;24:677-88. 47. Lisak D,.Luster L. Educational, occupational, and relationship histories of men who were sexually and/or physically abused as children. Journal of Traumatic Stress 1994;7:507-23. 48. DeLillo D, Tremblay GC, Peterson L. Linking childhood sexual abuse and abusive parenting: The mediating role of maternal anger. Child Abuse Negl 2000;24:767-79. 49. Schechter DS, Brunelli SA, Cunningham N, Brown J, Baca P. Mother-daughter relationships and child sexual abuse: A pilot study of 35 dyads. Bulletin of the Menninger Clinic 2002;66:39. 50. Cohen T. Motherhood among incest survivors. Child Abuse Negl 1995;19:1423-29. 51. Potter K, Martin J, Romans S. Early developmental experiences of female sex workers: a comparative study. Australian and New Zealand Journal of Psychiatry 1999;33:935-40. 52. Seng MJ. Child sexual abuse and adolescent prostitution. Adolescence 2003;24:665-75. 53. McMahon J,.Clay-Warner J. Child Abuse and Future Criminality: The Role of Social Service Placement, Family Disorganization, and Gender. Journal of Interpersonal Violence 2002;17:1002-19. 54. Cavaioloa AA,.Schiff M. Behavioural sequelae of physical and/or sexual abuse in adolescents. Child Abuse Negl 1988;12:181-8. 55. Widom CS,.Ames M. Criminal consequences of childhood sexual victimization. Child Abuse Negl 1994;18:303-18. 56. Pederson W,.Skrondal A. Alcohol and sexual victimization: a longitudinal study of Norwegian girls. Addiction 1996;91:565-81. 57. Stewart SH, Pihl RO, Conrod PJ, Dongier M. Functional Associations Among Trauma, PTSD and SubstanceRelated Disorders. Addictive Behaviours 1998;23:797-812. 58. Cheasty M, Clare AW, Collins C. Child sexual abuse - a predictor of persistent depression in adult rape and sexual assault victims. Journal of Mental Health 2002;11:79-84. 59. Bouvier P. Child sexual abuse: vicious circles of fate or paths to resilience? Lancet 2003;361:446-7. 32 60. Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M et al. Costs of Health Care Use by Women HMO Members With a History of Childhood Abuse and Neglect. Arch Gen Psychiatry 1999;56:60913. 61. Richardson J, Feder G, Eldridge S, Chung W-S, Coid J, Moorey S. Women who experience domestic violence and women survivors of childhood sexual abuse: a survey of health professionals' attitudes and clinical practice. British Journal of General Practice 2001;51:468-70. 62. Nelson, S. Beyond Trauma: Mental Health Care Needs of Women Who Survived Childhood Sexual Abuse. 2001. Edinburgh, Edinburgh Association for Mental Health. 63. Centre for Health and Social Research. A Safe Place to Talk: A needs assessment of adult survivors of childhood sexual abuse. 2001. Fife, Scotland, Fife Mental Health Strategy Group. 64. Nemeroff et al Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma" Proceedings of the National Academy of Sciences, November 25, 2003 , 100, 24, 14293- 14296 65. Bremner et al Neural correlates of declarative memory for emotionally valenced words in women with PTSD related to early childhood sexual abuse Biological Psychiatry, 2003, 53: 879-889 33 Appendix A Short-Life Working Group Membership Dr Margaret Hannah(Chair) Consultant in Public Health, Fife NHS Board Anne Black Association of Directors of Social Work (ADSW) Mari Branigan Glasgow Institute of Psychosocial Interventions Katie Cosgrove Women’s Unit, Greater Glasgow NHS Board Marnie Collins Kingdom Abuse Survivors Project Dr Anne Douglas Clinical Psychology Department, Stobhill Hospital Dr Mary Hepburn Princess Royal Maternity Hospital Catriona Laird Open Secret Tom Leckie Scottish Executive Social Work Services Inspectorate *Dr Ian Pullen Scottish Executive Health Department Anne Macdonald Cross Party Working Group on CSA Dr Graham Mackenzie Public Health, Fife NHS Board Laurie Matthew 18 and Under Dr Mini Mishra Scottish Executive Health Department Dr Lyndsey Myskow General Practitioner Sarah Nelson Researcher Peter Reid Men Against Sexual Abuse (MASA) Sarah Smith Health in Mind Dr Maureen Sturrock Scottish Executive Health Department Dr Linda Treliving Grampian NHS Board Dave McLeod (Secretary) Scottish Executive Health Department *Replaced Dr John Loudon who had been instrumental in establishing the SLWG Remit Using knowledge of the best evidence-based practice, and experience of the most appropriate ways to provide services in a local area, and accepting the recent World Health Organisation estimate (2002) (http://www.who.int/whr/2002/en/) that the prevalence of non-contact, contact and intercourse types of CSA totalled 21% in women and 2% in men is as valid for Scotland as elsewhere, to consider: Ways of improving the commissioning and management of care for all people in Scotland who are CSA survivors, in the community, in primary health-care services and in secondary health services, (obstetrics and gynaecology, substance misuse and mental health in particular). What supports could be offered to voluntary organisations, to the Primary Health Care Team, to local authority services and to community mental health teams in providing appropriate help to CSA survivors. The training requirements for staff in all organisations, particularly in the matters of disclosure and immediate response. How individuals who are CSA survivors and who require help should be assisted to access skilled care at the level they need. How the accumulated experience of CSA survivors and the expertise of voluntary organisations can best be utilised in partnership with the local statutory organisations to increase public awareness of the impact CSA has on public mental health, and what can be done by the local community to change this. How the continued care of a young person already in receipt of help for an experience of CSA can be assured as that person moves into adulthood. What should be the particular focus of any research in Scotland into the prevalence and treatment of CSA survivors. 34 Appendix B Improving Care Responses for Adult Survivors of Childhood Sexual Abuse Conference held on 28 April 2004, Edinburgh Testimonies of Survivors Nicole I suppose if you start by some plain fact details, I am a survivor, I got out when I was twenty six which is what shocks me. In all that time nobody had asked me anything, I had gone through school, college, university and it wasn’t until I was at university that I finally got out. So no mental health involvement all the time up till then. The reason I got out was because I went along to the voluntary organisation, and I have to say some things about the voluntary organisations, I don’t see the, the under funding, they were the only ones that helped me, and this organisation particularly which is Eighteen and Under, only works with kids aged eighteen and under. I was twenty six, so they broke the rules for me. I am glad they did because I am here. They were the only ones that would help, they were the only ones that would intervene and I needed intervention. This model of empowerment that people go on about I don’t think it would have worked. I wasn’t in a position to empower myself, yes I was at university and yes I was twenty six and there is a whole range of assumptions that are made by all services and all people about yes you are twenty six, you have these life skills, you have the ability and being at university you are intelligent so you have all these life skills and intelligence to be able to make your way in the world. I didn’t! Nobody asked what my life skills were and nobody asked what the situation was. I couldn’t shop – I had never handled money – I had never handled a key to a house – and I was twenty six. So I kind of spoke to a lecturer who then handed me over to a women’s aid worker who I met for about half an hour and she took me to Eighteen and Under. I kind of felt like you know the purse that nobody wants to open. Yes I can’t say that I have regrets about going to Eighteen and Under. I was there for, I would say, about an hour, I can’t ever remember saying very much. I was met by this very dippy woman who tried to pretend that she was really really dippy so that I wouldn’t be totally scared or put off. But was the only one that had ever sat down and took the time to even try and have a conversation with me, it was a good experience. I am not sure how it was for her but. The next week I wasn’t given the option of having another appointment, I was made another appointment. So I came back the next week. That week I was introduced to a Police Officer. Later on that same day I was moved into a ‘Safe House’. That was all within a week. Yes after twenty six years of nobody doing anything, and there were plenty of signs for people to see, I went to school with bruising, I went to university with bruising, but this was the only person that had actually intervened and did something, they realised that I couldn’t do something, it was too far gone for that. So the Police were called in and I was moved out of my family home into a Safe House in university, which was extremely safe, locked doors all the way. I did the whole key thing, playing the key because I had never had one before, it was quite funny. I had, at that point I had the clothes that I stood up in, the bag that I had on my back which was a constant companion of mine, and that was it, and then I was left. The first time I had ever been away from home in a very very secure accommodation. I didn’t really know what to do with myself. There is, I think there is situations that if people don’t have the awareness then they don’t understand that suddenly being in a safe place does not mean that you are safe. 35 Appendix B There was little things, like I didn’t have permission to sleep on the bed so I didn’t, it wasn’t mine. But these were things that I couldn’t tell people. All through growing up I couldn’t tell people about the abuse because I was not allowed to. I had been taught very very well not to tell. Then somebody out of the Mental Health Services came in and I don’t know how, I think it was through the Police who thought the best thing for me was to go and see a Doctor. I think that’s when I stopped being a Nicole and started being a disorder, post traumatic stress disorder, personality disorders. And then I started needing pills because of some apparent chemical imbalances and I think for me the hardest was that nobody actually asked me. Nobody asked me what went on, nobody had asked me what I had been through, but they prescribed the pills, it was like trying to put me the square peg through a round hole because that’s what they knew. Services aren’t provided for people’s benefits, not survivors, but the doctors, the ones that think they know best without asking. It was, I think it was hard for me to be able to talk and I have to admit that people who met me, I feel sorry for them, because I didn’t speak to them, I didn’t trust them why should I. To meet someone for an hour a week or an hour a month doesn’t build trust. Eventually things kind of got to the point where it was pretty serious, the Safe House wasn’t working, I was going back home because I couldn’t cope with, there was expectations from family that I had to, I had to meet their expectations, I had always met their expectations and suddenly to say no don’t do this any more doesn’t work. So this nice dippy woman from this voluntary organisation took me home, breaking all the rules and all the boundaries. Eventually I kind of settled in there and got my feet under the table and became her daughter. The whole informal adoption thing. And this person cared for me 24/7. Going to the Mental Health Services was never my idea, it wouldn’t have been something I would have thought about because I didn’t know they existed. So my mum at the time used to drag me along, it was her that made me go, saying that yes maybe we can help. None of them ever did. I think the only one that knew me best and the only one that I trusted was my mum. The person that they didn’t listen to was my mum. I could talk to my mum to a point, I am not saying I was like a mouth the size of the Mersey Tunnel because I didn’t, but she knew, she was with me 24/7, she knew the way I was, what experiences, and I had the good thing about lying to people. Yes everything was fine! I used to go to one appointment and then the next week or the next two weeks or the next month, go back and it was like well how things have been over the past month, och they have been fine! Because that was the way it was, why should, it’s not really a question that you can answer because do people really want to know. And in all my experiences people didn’t want to know. It was a can of worms that people did not want to open. The first Consultant I saw, the Policeman took me, the very nice Policeman. In the room there was the Policeman, there was me, there was the Consultant and there was a CPN who knelt on the floor beside my chair and patted my hand all the way through. There, there, you are OK. The consultant then turned round and said that it was the worst case of abuse he had ever seen and I thought then that he cannot be talking about me because it’s not actually as bad as that. To have someone say that to you when you didn’t in all innocence for a long time realise that it was abuse, it was the way it was, it was the way I grew up and there was nothing that I could have done to change that, because I needed to rely on other people, other people needed to do something not me and so I was the survivor, the survivors responsibility to make themselves 36 Appendix B better. And in the end that’s what I had to do. Because Mental Services did not provide for me, Social Work did not provide any service for me. Things kind of continued to get worse from there. I have experienced one ‘Section’. I have to say it was the most traumatic experience of my life. Yes taking into account the whole twenty six years I was with my family, the ‘Sectioning’ had to be the most traumatic part of my life. My mum at the time was threatened with arrest. I was, the whole big orderly kind of person grabbing hold of your arms and stuff and then taken into hospital and observed for however long. Observed is from the point of sitting there all day doing absolutely nothing, to going to the toilet, to having a shower, to going for a smoke. How they need to observe me going for a smoke, just to check how I do it I suppose, make sure I do it right, whatever. But yes, and it was all about keeping me safe. I walked out, I walked out of that hospital, nobody spoke to me, and I walked out on the third day, they were meant to be keeping me safe. It was the easiest thing in the world to do. I went to lunch and then walked out the door. There is no point. What was the point in me being in there. There wasn’t any. I had a nice chase police cars and all this stuff. I then got taken back up where I proceeded to say that I wasn’t staying there and then they had to get me a Doctor to discharge me. That was about the only time I was ever really forceful. I have to say that yes I would speak to people in hospital. I would tell them what they wanted to hear. If they said to me the only way that you are going to get out of here is to speak to me, then I would speak to them. I would tell them whatever they wanted to hear. Because I knew as soon as I got out there was no way on this planet I was going to go back. They had, yes I had given them some amount of trust because I was there, I was in the room, I went to see them, so the trust was there as far as I was concerned, and they broke that. So there was no way on this planet I was going to go back. But you say what you have to say to get out of the situation that you are in. Being in hospital is like being back at home. The control was there, you eat when they say, you drink tea when they say, you smoke when they say, you go to bed when they say. And the pills, you have to trot along like good little school kids, pat you on the head and give you a pill, away you go, everything is alright. Yeah. But they don’t talk to you. The hospital I was in didn’t provide any recreation; there was a pool table upstairs that I wasn’t allowed to go near. I had to be respectful of other patients which I am generally a kind of respectful person, but there was no radio, TV was only allowed on at certain times and if people had a problem with a TV it had to be switched off. I am kind of young in my outlook, I kind of like music, I love TV, and to be in a situation where you can’t do either because you are in a ward with people who have acute mental health problems, which suddenly I developed. What you have then is people who hear voices through TVs and Radios, so you can’t watch it and you can’t listen to the radio. So I was left there twiddling my thumbs. The next major thing was after that ‘Section’ I didn’t go near a Doctor for about a year, any Doctor, that included the GP. So my mum had to deal with me in all that time. I am sure I wasn’t easy to deal with sometimes. So I got ill and went to the GP and asked for an urgent referral to CPNs, which is three days or five days they are meant to come out and see you. It’s now two years later, three years later, and I am still waiting. In the end I was taken to where CPNs were based, two CPNs came into the room and shouted my name, so I asked my mum to come with me, as is my right to take someone in with me. I wasn’t allowed to take someone in with me, I had to see them on my own, if I didn’t see them on my own I was refusing their service, so I could just go. So there was a big stooshy, mum shouting at them, them shouting at mum, I walked out, no I didn’t walk out I ran out. And you know how they lock doors with a stupid key thing that you have to press, could I find the key, I was like standing at the door, some way I found the key and was out, so I don’t need to be here, I don’t need to deal with this. 37 Appendix B What happened then was mum came out after me to try and calm me down and get me back in the car and sort things out, and the two CPNs alongside an Orderly, that I sort of found out later, were looking out of the window, it was a nice little afternoons entertainment for them to watch the crazy person being helped back into the car. We complained about it, well I didn’t. It was kind of a joint complaint I think, I was extremely angry at the way they had treated mum, but more for the fact that it could happen to someone else, that wasn’t allowed to be. So we complained and we actually got an independent review, it’s apparently quite a rare thing to get. So we had to go and do all these interviews and speak to these people from outside. And eventually after a long long while they put out a report which found in my favour and the CPNs had lied, a Consultant had written a report on me and hadn’t actually met me and he had lied. I think the thing that he had said was that he, he I had asked for a female and I got a male, I hadn’t met him. He had made an appointment an appointment in May, I had gotten ill in February, an appointment had been made for May. I am still waiting on the service. So the report found in my favour, I got this nice little action plan as to how they were going to try and give me a service, which I have not at this point in time accessed because I really don’t see the point. Your slides in the morning said about self help, self help yes I have done because I have had to and I think I have done pretty well if I don’t say so myself. Where I am at now, I am going back to university because I kind of missed out. My father got arrested on the day of my first junior final exam and I couldn’t do it. I was in third year and I was doing extremely well. What have I done so far. I have spent six months in America by myself. The main thing that the Doctors had said was there was this co-dependency between me and my mum. I think I have to say there had to be dependency, I had never depended on anyone and suddenly I could depend on someone and they wanted to take that away. I used to say to myself, for twenty six years I have stayed with my family and nobody ever wanted to take me away from them, suddenly I find someone who helps me, who I can depend on and who doesn’t hurt me and they want to take me away from her. I couldn’t quite understand it. And this codependency, I live on my own, I have my own house, I have my own car, I want to go back to university, I spent six months in America on my own and hopefully at the end of this year I am going to travel around Europe on my own. I think dependency is needed and when it is not I am the one to decide when it’s not needed, I am the one that can now depend on myself but know that I can depend on my mum as well, and I did that by myself with no help from anyone. The last thing that I want to say is that I am Nicole, I am a survivor not a victim, and I am not a walking disorder. I am not something that needs to be treated, the symptoms and the consequences yes they are there and they are affective, they affect the way I think, I am a human being, treat me like one. Don’t treat me like some case study, some client because I am not, I am not a statistic either, things happened but I am a person the same as everyone else in this room and I need to be treated with the same respect. I don’t need to be dictated to, I know what I need even if I can’t figure that out sometimes for myself, eventually I will get there, and so will everyone else. And that’s all I have to say. Ronnie Hello everybody, my name is Ronnie. I am a survivor of female sexual abuse. I am not going to talk about that, I am going to talk about what happened when I went to get help. I was going to my GP for years because I never had any sleep, I was only getting between 1 hour and 2 hours a night and that was bringing on other problems as well, like migraines, eating disorders, mood swings, argumentative, speaking through my teeth and even my body language told you to stay away from me. 38 Appendix B So I went to my Doctor, this was over years and I had had enough, I was ready to explode and I knew I was going to explode. I went in and I took in a Dictaphone and I put it on his table and I put it on record, and he says what’s that for this is private and confidential, I said it is private and confidential if I say it is. I was then going to go out there, I come here for you to help me and if you refuse me and I then go out there and beat somebody up or smash something up, it’s coming to your door not mine. I am up to here with you people over the years. So he said wait a minute, wait a minute. So he went away and he came back and he says I have spoken to your Doctor, I goes well you just told me a minute ago that he wasn’t here. So you lied to me straight away. First contact. He goes right I am going to refer you up to this institution. So I went away up there and there was a Psychiatrist and I was telling him about that sexual abuse that I was dealing with at the time, and he starts laughing in my face, and I says to him what are you laughing at, if you don’t take that smile off your face I am going to come over and kick ????? out of your head, out of your neck. Now he had a nurse sitting there and this guy was about 6’2” and I says to him if I want to get you I will take that smile off your face. Then he turns round and says do you remember the Bogey Man when you were three, and I said to him what do you mean, and he went you were standing in the garden, you looked in the kitchen, there’s your mum but there’s the Bogey Man coming down the road he is coming after you. And I said to him I don’t remember the Bogey Man at three and I went do you and then he shut up. So I says to him you are not going to help me here are you, and he goes well what do you want me to do, I said help us, that’s why I am here. So he became cheeky and abruptive, abruptness and I says to him right that’s it and I got up and walked out. The following week I went back to my Doctor, I was referred back up again. Now they wanted to take me into a locked ward and I said no. Being in institutions it was always locked doors and I didn’t like that at all. So I got up and I left and I went back a week and a half later and I got this woman. I was in that room for about two and a half three hours just talking to this woman. She says can you last three weeks and I says no I can’t. I want to come in now. I was shivering and I was shaking, this anger was just wanting to come out and I didn’t know how to control it any longer. So I came out and my wife went in for about an hour or an hour and a half and she spoke to her about what it was like to live with me over the years. And she come out and she says Ronnie can you not wait three weeks and I says no I can’t. She said well I can’t get you a bed for three weeks, and I said well I am sorry. So I went home and I was lucky, I got a letter a week and two days later to go up to a locked ward up in Ninewells Hospital. Now I went in and I was like that well I am going to give this place a go. And what you do is you see this Professor on a Thursday, he sees everybody, and you are supposed to speak to him about your problems. So I went in and he goes well what’s your problem and I started to tell him, and I noticed he was just sitting going Hmm Hmm yeah hmm hmm and then wasn’t talking. And I am saying why are you going hmm yeah hmm hmm how come you have not asked any questions. So he says tell us about your problem, I says in front of all these people, you have about ten, twelve people in this room, and I said to him you are an idiot, I don’t even know these people, who they are, and I noticed one of the nurses who was allocated to me, he was sitting there and I says to him, I have been in here now for a month and not one nurse has came to me and spoke to my about my problems and that’s why I am in here. Because I says to them, you are not talking to me, so what they started doing is they put us on medication and they gave us a brain scan and they found out there was a chemical imbalance in my brain, so they gave us medication for that. But I had never had sleep before so I didn’t know what it was like so I was waking up in the morning like 8am full of energy and I am like what’s this because I had never had a good nights sleep. 39 Appendix B So anyway I was in there and what I started doing was questioning the medication they were putting me on because it seemed to be going up and up and up and I am like what’s this for, well that’s to counteract the side effects of that. I didn’t want all this, all this medication I just want to see a book, so it was called the MUMS, I don’t exactly know it was called but we called it MUMS for short and I kept going to the nurse and I was just getting worse and worse and she says wait two seconds and I says I cant wait two seconds, so she took us in, she gave us an injection and then locked you up out of the way. So I says to her is that the side effect of every person you have gave it to and she went yes, I said why don’t you give them the antidote when you give them this medication. So after a period of time I was sitting in the smoke room, I was having a fag, it was about 3 or 4 in the morning and this young lad came in, one of the nurses, and he started trying to speak to me about my problems and I says to him do you know anything about rape, do you know anything about depression, do you know anything about alcoholism, do you know about drug taking, depression, anything like that. Oh I did a years course in Counselling in Perth. And I says to him how old are you and he went 19 so I says well what you should do is give up your job, go out experience life about ten fifteen years and if you still want to do this job come back in and do it. So it was getting near the time and I knew they was going to get rid of us because that’s the way it was going because I just kept arguing with them about everything. So eventually I got out and went to see this Psychologist and he gave up after about I would say three and a half months, he just couldn’t handle me. So I asked for somebody else and I got that person and that person helped me a lot. She gave me feedback like you wouldn’t believe, I had never had that before and this is what I was saying to them I want to find out why it was like this. Why am I thinking like this. But I have heard all the stories that when I left Ninewells Hospital Psychiatric Ward other patients were going up and asking for this MUMS book to look at medication and what effect they had. All of the nurses that were there, they all got split up to different parts of Dundee and other institutions, so that was cleared out. And every time other people went up they would say yeah that was Ronnie, it was him that did this, and I am like that well you are in here to do a job helping these poor people with sexual abuse or depression or anything like that and you are just sitting up there yapping about what you do at the weekend. I mean I wouldn’t do that personally if I was qualified to help people. And so after a while somebody planted a seed in my head to go to college. So I am up there now doing an NQ in Social Care but I did two years at Abertay, last year and the year before and then I was diagnosed with Dyslexia and Learning Difficulties. Now the people that were put in place to help us it was like being back in the institutions, they were all giving up on me because they say my disabilities were severe and they were going nuts with me, I just needed more help than a normal student. So last year I sat exams, I passed three and I had another one that was getting me down so I went back up to Dundee college, so I went up there and did an NQ in Social Care and I am sitting my exams shortly, so I will be looking to get an HNC. But the thing that I would like to say here today is its like those who have been sexually abused need to educate the educators because this has been a lot of frictions coming in because it is a professional person who would need to come in and train him, but I think there should be specialist groups, training, people that are specifically here to hear the words sexual abuse because you have heard about opening the can of worms, but these people are trained not to deal with these problems and that is why everybody gets pushed pillar to post. And another thing you need to do is every time a person comes in with a problem he shouldn’t have to speak to a different person all the time. 40 Appendix B Because when I got help I wrote down four A4 books what I had been through and the Psychologist at times says Ronnie have you ever spoke about it and I said no, but when I thought of speaking about it then I got help. But I think there is a lot of barriers, like we say as professionals if you are counselling someone the first thing that they see is a suit, if you see a suit they are not going to open up to you, there is a barrier straight away, and we say to them what’s wrong with just wearing casual like clothes, that’s nothing hard. Oh but every professional I have got this, look I am not arguing with you about your qualifications, I am saying to you if you have got casual white clothes on these people would open up. Because its people in authority that abuse them the suit to them is an authority so they will clamp up. But we speak and speak and speak and it’s the professionals in authority that say they will listen, they do not listen. I mean you have said about using training packages or training seminars and things like that, but who is training them, its not those who have been sexually abused, why not, I mean they have got a wealth of knowledge that maybe we can speak to about it, that these professionals like they have got these seminars you can go on TV and newspapers, we don’t we just come to places like this and hope that somebody says Oh right that’s a good idea. And so, and another thing, I tried to get the woman charged five years ago and I found out that she did my two brothers as well and that was news to me. We went to the court every year and for every angle we had they had like ten to get her off. The latest was from the QC and he says its time barred. That was a shock to me. Time barred. That’s needing to be changed dramatically, the whole rape whatever they call it should be changed. When I heard that the QC says to me it was time barred if it had been five years earlier it would have went to court because the police had evidence. So my Solicitor got in touch with the police they had destroyed it. We went to the Social Work information was lost. We went to the Social Services couldn’t be found. Now that’s just my case. In my Doctors notes, its all in there “Father had resentment towards Ronnie, that was me, they knew he had resentment towards me, they knew he was beating me up because I had mentioned it, they knew that I wasn’t getting fed, I was going to peoples houses I was going to classroom teachers and telling them what was going on and its all there in record but I can not just get this woman out of court. Now I wrote a six page letter to the Procurator Fiscal and it says one, you never talk to me, you never talk to my brothers, you have never looked at my psychological approach, you have not used anybody that I have went to, to get help to bring them and speak to them or my wife to get her opinion of what I was like to live with. But like I say its like all these barriers when it comes to sexual abuse come up, its like no I don’t want to talk about this but even the law is not there for you so what are you supposed to do. Let them away with it and that’s the biggest problem, there is not a lot of places for males where I come from but we have got a little group going called M Line and Andy my colleague he has been doing that for like about seven year he does support work and I do, well I have done a couple of support but I have been at a couple of things that Andy has done, talks and things like that so well that’s me going to finish. Oh just one more thing Dr ?? I would just like to thank you for the help that you gave I really appreciate that, that helped me a lot with your feedback, so I would just like to thank you for that. 41 Appendix C Attendance List - Improving Care Responses for Adult Survivors of Childhood Sexual Abuse Conference held on 28 April, Edinburgh Name Barcus, Shona Bienkowski, Geraldine Black, Anne Black, Janette Bolt, Susan Brannigan, Mari Brindley, Sandy Brown, Norma Brown, Sandra Cafferkey, Lorraine Campbell, Margaret Carol, Gillian Collin, Marnie Coote, Nick Cosgrove, Katie Cuthbert, Jean Devine, Kay Dewey, Caroline Dobson, Caroline Douglas, Anne Duboust, Sheena Duff, Heather Ersoy, Liz Forbes, Fiona Franklyn, Myra Gilbert, Irene Gordon, Simon Grant, Beatrice Greenan, Lily Hampson, Sue Hands, Sandra Hannah Margaret Hendry, Julie Henegan, Cath Hepburn, Mary Huddart, Paula Irvine, Linda Johnston, Christine Organisation Chief Executive, SAMH Consultant Clinical Psychologist, Member of Lothian Sexual Abuse Development Group ADSW Rape Crisis, Glasgow SEJD: Victims and Witnesses Unit Senior Nurse Practitioner, Glasgow Institute of Psychosocial Interventions, Glasgow Primary Care NHS Trust Rape Crisis Scotland, Glasgow Activity Team Leader, North Cunningham CMHT Moira Anderson Foundation Domestic Abuse Support Workers, KASP Child Protection Co-ordinator, South Lanarkshire Council Moira Anderson Foundation Project Manager, Kingdom Abuse Survivors Project Lead Clinician, Centre for the Vulnerable Child, Fife NHS Women's Unit, GGHB Independent Trainer (in Violence Against Women) Victim Support Scotland (Borders) Health Improvement Officer, South Ayrshire LHCC Chartered Clinical Psychologist, Area Clinical Psychology Service, New Craigs Hospital Specialist, NHS Sexual Abuse/Sexual Assault Clinic and Glasgow PCT Occupational Therapist, Nairn Community MH Team (Highland PCT) Community Nurse, LPCT City of Edinburgh Social Work Lothian PCT East Renfrewshire Council Sister, Aberdeen Maternity Hospital Orkney Alcohol Counselling and Advisory Service (Vol) Larbert West Parish Church The EVA Project, Coathill Hospital Health in Mind Head of Health Care, Polmont Young Offenders Institute Consultant in Public Health, Fife NHS Board Co-ordinator of the CSA Team at the Child and Family Mental Health Service at Royal Hospital for Sick Children MH/Sexual Abuse Worker, KASP Consultant Obstetrician & Gynaecologist, Princess Royal Maternity Hospital Lothian NHS Board, Social Inclusion and Community Care Children's Services Manager, Barnardo's Scotland 42 Appendix C Johnston, Lesley Kettle, Martin Laird, Catriona Leckie, Tom Lee-Campbell, P Lumsden, Allyson Macdonald, Morag Macdonald, Anne Mackenzie, Graham Malan, Lene Martin, Yvonne Matthew, Anne Matthew, Laurie Mayne, Liz McGuinness, Andy McGuire, Helen McKinlay, Fiona McLeod, Dave McMonagle, Dorothy Mearns, Kate Meldrum, Margaret Mishra, Mini Moore, Louise Myers, Fiona Nelson, Sarah Nisbet, Isabel Pilkington, Wendy Rae, Gail Reid, Peter Ross, Eileen Rowley, Margaret Anne Samuel, Robert Simpson, Lynne Smith, Sarah Stephenson, Theresa Sturrock, Maureen Thomas, Ian Treliving, Linda Troy, Liz Watson, Andy Watt, Kathryn Winslow, George Public Health Practitioner, NHS Lothian SEED Child Protection Reform Programme Open Secret SEED, Social Work Inspectorate Clinical Manager Mental Health, Polmont Young Offenders Institute Nurse Psychotherapist, Sexual Abuse Service, St John's Hospital Mental Health Services Development Co-ordinator, North Ayrshire Vice-Convenor, Cross Party Group Specialist Registrar in Public Health, Fife NHS Board Clinical Psychologist, Young People's Unit, Royal Edinburgh Hospital Day Hospital, Lanarkshire Health Care Trust Education and Research Officer, Royal College of Midwives UK Board for Scotland 18 and Under Department of Health M Line Women and Children First Children and Families Division SEHD CMHT Larkhall, NHS Lanarkshire Child Protection Development Manager, Angus Council CPN Team Co-ordinator, St John's Hospital SEHD, Medical Adviser Women and Children First Researcher, Scottish Development Centre for MH Researcher City of Edinburgh Social Work Community LD Nurse, Lothian Health MH/Sexual Abuse Workers, KASP MASA Day Hospital, Lanarkshire Health Care Trust Nursing Officer, SE Nursing Directorate Asst Project Manager, KASP Depute Director, Health in Mind Rosyth Social Work, Fife Council SEHD Advisor ACPOS Child Protection Working Group and Lothian and Borders Police Consultant Psychiatrist, Grampian PCT Day Hospital, Lanarkshire Health Care Trust SEJD Police Division Clinical Psychologist, St John's Hospital Scottish Parliament Cross Party Group on Survivors of Childhood Sexual Abuse 43