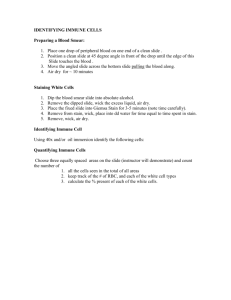
Wright's Stain SOP: Manual Differential Cell Counts
advertisement

Penny Stevens Procedure Number Date Author(s), Name & Title International QA/QC Coordinator Pro64-B-04 Version 1 Jan 06 SMILE Comments: This document is provided as an example only. It must be revised to accurately reflect your lab’s specific processes and/or specific protocol requirements. Users are directed to countercheck facts when considering their use in other applications. If you have any questions contact SMILE. Copy _______ of ________ Effective Date: YOUR LAB HEMATOLOGY SECTION C. DIFFERENTIAL CELL COUNTS C.2. WRIGHT’S STAIN MANUAL METHOD C.2.1. PRINCIPLE: Wright’s stain is a polychromatic stain consisting of a mixture of eosin and methylene Blue. When applied to blood cells, the dyes produce multiple colors based on the ionic charge of the stain and the various components of the cell. The eosin ions are negatively charged and stain basic cell components an orange to pink color. The methylene blue ions are positively charged and stain the acid cell components in varying shades of blue. The neutral components of the cell are stained by both components of the dye producing variable colors. C.2.2. SPECIMENS 1. Thin wedge blood smears are prepared on pre-cleaned glass slides from freshly drawn capillary or venous blood anticoagulated with EDTA. 2. The blood smear slide must be properly prepared, labeled and completely dry before commencing with the staining procedure. 3. For best results, prepare and stain smears within two (2) to three (3) hours of specimen collection. C.2.3. EQUIPMENT AND REAGENTS: 1. EQUIPMENT: 1.1. Four (4) coplin jars Page 1 of 8 DIFFERENTIAL CELL COUNTS C.2. WRIGHTS STAIN MANUAL METHOD 1.2. Pre-clean glass slides 1.3. Whatman Grade 41 filter paper – 110mm diameter 1.4. Funnel – short neck 2. REAGENTS: 2.1. Diff Quick Fixative Solution 2.2. Diff Quick Solution I (Red) 2.3. Diff Quick Solution II (Blue) 2.4. Distilled Water NOTE: The reagents are flammable and must be stored in the flammable cabinet. Keep only the minimum working supply, appropriately labeled with hazard warnings, in the section. C.2.4. PROCEDURE: 1. Dip the blood smear into the Diff Quick fixative solution five times for one (1) second each time. Wipe the back of the slide with gauze to prevent carry over into the next stain. Do not allow the fixative to dry on the slide as this will result in an over-fixed wet appearance. Immediately proceed to the next step while the slide is still wet. 2. Dip the fixed blood smear into the Diff Quick solution I five times for one (1) second each time. Wipe the back of the slide with gauze to prevent carry over into the next stain. Do not allow the stain to dry on the slide. Immediately proceed to the next step while the slide is still wet. 3. Dip the fixed blood smear into the Diff Quick solution II five times for one (1) second each time. Wipe the back of the slide with gauze to prevent carry over into the next stain. Do not allow the stain to dry on the slide. Immediately proceed to the next step while the slide is still wet. 4. Rinse the fixed blood smear with distilled water five times for one (1) second each time. Wipe the back of the slide to decrease drying time. Set the slide upright to air dry. Allow the slide to dry thoroughly before reading. 5. To decrease drying time, slides may be blown dry. Set the blow dryer on cool and hold the slide at least 12 inches from the air flow until completely dry. Page 2 of 7 DIFFERENTIAL CELL COUNTS C.2. WRIGHTS STAIN MANUAL METHOD C.2.5. PROCEDURAL NOTES: 1. Properly stained smears will display the following characteristics when examined microscopically: 1.1. Red to buff pink colored red blood cells. 1.2. White blood cell nucleus coloration: 1.2.1. 1.2.2. Lymphocyte and Neutrophil nucleus are dark purple. Monocyte nucleus is light blue to purple. 1.3. White blood cell and platelet cytoplasm appearance: 1.3.1. 1.3.2. 1.3.3. 1.3.4. 1.3.5. 1.3.6. Neutrophil cytoplasm is light pink with lilac granules. Lymphocyte cytoplasm varies from light to dark blue. Monocyte cytoplasm is gray-blue with few fine reddish granules. Basophil cytoplasm is clear with few blue-black granules. Eosinophil cytoplasm is pink to clear with many large red to orange granules. Platelets appear as light blue to colorless with red violet granules. NOTE: The Diff Quick Fixative is insufficient to adequately fix the basophil granules. As a result, most of the granules are lost in the staining process and the basophils appear ‘agranular’, which can result in misidentification. This basophil appearance is inconsistent with images presented in current literature. 1.4. Precipitation: Rare to slight precipitation is acceptable. As stain solution II evaporates, excess precipitation will form. Filter the stain solution II as needed to remove excess precipitation. 1.5. Contamination: Bacterial or semen contamination can occur as a result of shared use between microbiology and hematology. If either is present in the stain solution, replace all reagents and perform maintenance as indicated in section C.2.7. 2. Sources of error: 2.1. Fixation: 2.1.1. Inadequate fixation may result in a detached specimen, indistinct nuclear detail or poor granule staining. This is especially evident in basophils and primary myeloid granules. Page 3 of 7 DIFFERENTIAL CELL COUNTS C.2. WRIGHTS STAIN MANUAL METHOD 2.1.2. Dry freshly prepared smears for at least fifteen (15) minutes to prevent drying artifacts. Use only pre-cleaned glass slides. Slides other than pre-cleaned may result in improper fixation and the presence of haze over the slide due to acid-base disturbance. Pre-cleaned slides are necessary for quality stain appearance. 2.1.3. Use only anhydrous methanol for fixative. Keep it tightly closed and away from moisture or chemical fumes. 2.1.4. If fixation problems occur or increased granularity visualization is necessary, increase the fixation period to one (1) minute. 2.2. Staining: 2.2.1. Excessively blue stain appearance may be due to improper smear preparation, prolonged staining time or increased stain alkalinity. 2.2.2. Excessively pink stain appearance may be due to insufficient or decreased staining time, prolonged washing time or increased stain acidity. 2.3. Rinse: 2.3.1. Use only distilled water or phosphate buffered saline for the final rinse. Tap water is never acceptable as a substitute for the rinse since it can disturb the acid base balance and may contain chlorine. 2.3.2. Vigorous or prolonged washing may dislodge cell from under-fixed smears, cause nuclear clumping or under-staining. 2.3.3. Insufficient rinsing may result in a blue smear or excessive precipitate. 2.4. Drying: Air drying is the preferred method. Forced rapid drying may alter the color intensities by shortening the exposure time to the wash water because the red spectrum of colors continues to develop as long as the cellular elements are wet. C.2.6 QUALITY CONTROL 1. Prepare one differential slide daily using a patient sample with a normal MCV, MCH, MCHC and total white count. Stain the slide as indicated in procedure section C.2.4. Review the slide for Color, Precipitation and Contamination. 2. If the color does not meet the specifications identified in the SOP as indicated above or precipitation and/or contamination are present, the quality is determined to be Page 4 of 7 DIFFERENTIAL CELL COUNTS C.2. WRIGHTS STAIN MANUAL METHOD unsatisfactory. Indicate unsatisfactory on the Quality Control (QC) form and replace the stain as indicated in the following section. Document the problem and corrective action in the appropriate section of the QC form. If the stain is determined to be satisfactory, indicate satisfactory on the QC sheet. C.2.7. MAINTENANCE 1. Perform maintenance weekly or as needed for problems indicated in previous sections. 2. Discard reagents into the gram stain hazardous waste containers located in the microbiology department. 3. Clean the coplin jars using mild soap and tap water. Perform a final rinse using distilled water and allow the jars to air dry. 4. Use two sets of coplin jars and rotate the sets weekly allowing the jars to dry thoroughly before use. 5. Replace the fixative, stain and water into the appropriately labeled jars with accurate hazard warning labels. Filter the stain solution II (blue stain) using a short neck funnel and 110 mm diameter filter paper folded into a cone. NOTE: The gravimetric filtration process is slow – do not attempt to speed it up or it will force particulates into the filtered stain. B.2.8. APPENDICES: 1. Diff Quick Maintenance / Quality Control Form. 2. SOP Validation Form and SOP Change Control. 3. SOP Approval. B.2.9. REFERENCES: 1. Brown, Barbara A.; Hematology: Principles and Procedures, Sixth Edition, Lea and Febriger Book Publisher, 1993, Pages 97-100. 2. Hoffman, Donald; Hematology: Principles and Practice, Second Edition, American Book Publisher, 1995, Pages 2202-2203. 3. Carr, Jacqueline H. and Rodak, Bernadette F.; Clinical Hematology Atlas, W.B. Page 5 of 7 DIFFERENTIAL CELL COUNTS C.2. WRIGHTS STAIN MANUAL METHOD Saunders Company, 1999, Pages 33-86. 4. Laboratory CQI SOP, 8 April 2004. Page 6 of 7 DIFFERENTIAL CELL COUNTS C.2. WRIGHTS STAIN MANUAL METHOD SOP VALIDATION SOP NAME: C.2. WRIGHT’S STAIN MANUAL METHOD Clear and specific title and principle: yes / no Comments: All necessary supplies, equipment, and materials are listed: yes / no Comments: SOP is sufficiently detailed to be understood but not overly complex: yes / no Comments: SOP text adequately describes process/procedure: yes / no Comments: SOP accomplishes purpose: yes / no Comments: Reviewed by: (Name & Title) Signature: __________________________ Date: __________________ SOP CHANGE CONTROL Date Change QA Page 7 of 7 OIC Med Dir DIFFERENTIAL CELL COUNTS C.2. WRIGHTS STAIN MANUAL METHOD SOP APPROVAL SIGNATURE DATE PREPARER QA COORDINATOR LABORATORY OIC MEDICAL DIRECTOR ANNUAL REVIEW REVIEWER SIGNATURE DATE DOCUMENT COPY CONTROL LOCATIONS REVIEWER SIGNATURE DATE: ___________ DATE # COPIES __________ 1 9 2 10 3 11 4 5 6 7 8 SUPERSEDES: _21 Jan 1998_____ DATE SOP RETIRED: __________ Page 8 of 7