File
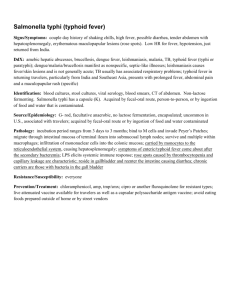
advertisement

St. Paul College of Ilocos Sur COLLEGE DEPARTMENT Bayubay, San Vicente, Ilocos Sur In partial fulfillment of the requirements for NCM 101 (Care of Individuals and Family with Maternal and Child Health) (Related Learning Experiences) A Case Study Respectfully Submitted to: Mrs. July Tricia Pili Clinical Instructor Respectfully Submitted by: Leizel R. Dait Mary Grace Incillo (BSN-II) Introduction: In constructing this case study, we decided to explore our self in dealing with different kind of diseases in which will help in developing our skills and knowledge particularly in formulating and rendering patient’s care and services. The primary purpose of this case study is to exhibit information regarding Typhoid fever which will help in easy recognition of the disease. Hence, preventing the complication or other consequences that might occur to patients with the disease. This is also to develop and enhance our nursing skills particularly in formulating appropriate nursing management to patients with such illness. As we encountered in the clinical setting, typhoid fever-its mechanisms and process was too vague for us. Through this case study, we were able to achieve information regarding the disease condition that will help In further formulating and providing appropriate care to the patient. Typhoid fever is a bacterial disease, caused by Salmonella typhi. It is transmitted through the ingestion of food or drink contaminated by the feces or urine of infected people. Symptoms usually develop 1–3 weeks after exposure, and may be mild or severe. They include high fever, malaise, headache, constipation or diarrhea, rose-colored spots on the chest, and enlarged spleen and liver. Healthy carrier state may follow acute illness. Typhoid fever can be treated with antibiotics. However, resistance to common antimicrobials is widespread. Healthy carriers should be excluded from handling food. It is important for the physician to understand that the typical causes and presentations of typhoid fever in infants and children are variable, depending upon the child’s age and underlying medical condition. Expansive comprehension regarding the disease condition will provide good perception and information that will benefit both the patient and the nurse in dealing, exploring and managing such kind of disease. The objectives that follow will contribute in attaining the benefits in knowledge and skills in recognizing the condition- Typhoid Fever. Definition Typhoid fever is a life-threatening bacterial infection caused by the bacterium Salmonella Typhi (S. Typhi). According to the CDC, typhoid fever is common in developing countries, where it affects about 22 million persons each year. Transmission: Humans serve as the natural host as well as reservoir. Faeco-oral contamination is the most common route of infection. Consuming raw fruit and vegetables contaminated with sewage water, shellfish, and ice creams are the significant risk factors for contracting S. typhi infection. Epidemiological studies have suggested that small inocula are sufficient for water borne transmission but large inocula is required for food borne organism transmission. Clinical features Symptomatology of typhoid fever is highly variable ranging from mild illness with low-grade fever, dry cough, and malaise to severe illness associated with complications. Depending on age of the patient clinical manifestations vary. School going children and adolescents: Onset is usually insidious. Fever, myalgia, anorexia, headache and abdominal pain are the initial features. In early phase diarrhea is common but later constipation ensues. Patient may develop cough, epistaxis and lethargy. Within a week of onset, fever increases in stepwise fashion and becomes unremitting and high grade. During second week of illness all the symptoms increase in severity and patient may appear toxic, lethargic, and disoriented. Delirium and Stupor may occur. On examination relative bradycardia (disproportionate to the degree of fever) is characteristic. Hepatosplenomegaly with abdominal distention and generalized tenderness are common findings. Few patients with typhoid fever may develop macular or maculopapular, discrete erythematous rash, raised from skin, blanching on pressure on about 7-10th day of illness (rose spots) usually seen on chest and abdomen in crops. On healing they leave small hyperpigmented areas. S. Typhi can be cultured from these lesions (60% yield). Chest examination may reveal scattered rhonchi and crepitations. Without complications all signs and symptoms subsides within 2-4 weeks except malaise and lethargy, which may persist for 1-2 months. Infants and young children: Typhoid fever usually presents as mild fever, malaise and diarrhea and is commonly labeled as acute gastroenteritis in this age group, however sepsis may occur. Neonatal typhoid fever: S. typhi can be transmitted vertically. Antenatally it can cause (may lead) to chorio-amnionitis, miscarriage, fetal death (58) and premature delivery. Neonatal typhoid usually presents within 72 hours of delivery with hypo or hyperthermia, vomiting, diarrhea, abdominal distention, convulsions, hepatomegaly and jaundice. Poor feeding and weight loss may be significant. Risk Factors S typhi are able to survive a stomach pH as low as 1.5. Antacids, histamine-2 receptor antagonists (H2 blockers), proton pump inhibitors, gastrectomy, and achlorhydria decrease stomach acidity and facilitate S typhi infection. HIV/AIDS is clearly associated with an increased risk of nontyphoidal Salmonella infection; however, the data and opinions in the literature as to whether this is true for S typhi infection are conflicting. If an association exists, it is probably minor. Other risk factors for clinical S typhi infection include various genetic polymorphisms. These risk factors often also predispose to other intracellular pathogens. For instance, PARK2 and PACGR code for a protein aggregate that is essential for breaking down the bacterial signaling molecules that dampen the macrophage response. Polymorphisms in their shared regulatory region are found disproportionately in persons infected with Mycobacterium leprae and S typhi. On the other hand, protective host mutations also exist. The fimbriae of S typhi bind in vitro to cystic fibrosis transmembrane conductance receptor (CFTR), which is expressed on the gut membrane. Two to 5% of white persons are heterozygous for the CFTR mutation F508del, which is associated with a decreased susceptibility to typhoid fever, as well as to cholera and tuberculosis. The homozygous F508del mutation in CFTR is associated with cystic fibrosis. Environmental and behavioral risk factors that are independently associated with typhoid fever include eating food from street vendors, living in the same household with someone who has new case of typhoid fever, washing the hands inadequately, sharing food from the same plate, drinking un purified water, and living in a household that does not have a toilet. As the middle class in south Asia grows, some hospitals there are seeing a large number of typhoid fever cases among relatively well-off university students who live in group households with poor hygiene. Complications: 10-20% of patients have occult blood in stools, 3% having malena and 0.5-3% of patients may develop intestinal perforation, followed by peritonitis presenting as sudden tachycardia, hypotension, abdominal distention with guarding, rigidity and rebound tenderness. Hypothermia usually occurs after the first week of disease. Perforation size may range from pinpoint to several centimeters. Gram-negative sepsis may ensue. X-ray abdomen may suggest free air in abdomen. Altered sensorium has high case fatality rate. Study from Malaysia showed that children with splenomegaly, thrombocytopenia and leucopenia are more likely to develop complications (20). Short duration of symptoms, inadequate antimicrobial treatment, male sex and leucopenia were the independent risk factors for enteric perforation from a study done in Turkey (23). Intestinal bleeding usually occurs from multiple, variable sized punched out ulcers in the distal ileum and proximal colon. Other complications include – Pneumonia by superinfection with organisms other than Salmonella typhi, bronchitis (10%), toxic myocarditis, neurological complications including raised intracranial pressure, cerebral thrombosis, acute cerebellar ataxia, chorea, aphasia, deafness, psychosis, transverse myelitis, peripheral neuritis, optic neuritis, meningitis, encephalomyelitis, Guillian-Barre syndrome, cranial nerve palsies. Other reported complications are – Disseminated intravascular coagulation (DIC), thrombocytopenia, Hemolytic Uremic syndrome (HUS), Hepatitis, Splenic and bone marrow granulomas, glomerulonephritis, leukocytoclastic pancreatitis, vasculitis, splenic Suppurative / liver abscess, cutaneous lymphadenitis, cutaneous ulcerations, thrombosis, phlebitis, fatal bone marrow necrosis, pyelonephritis, nephrotic syndrome, endocarditis, orchitis, osteomyelitis and suppurative arthritis especially in children with hemoglobinopathies. GENERAL OBJECTIVES: This case study aims to identify and determine the general health problems and needs of the patient with an admitting diagnosis of typhoid Fever. This presentation also intends to help patient promote health and medical understanding of such condition through the application of the nursing skills. Specific Objectives: To raise the level of awareness of patient on health problems that he may encounter. To facilitate patient in taking necessary actions to solve and prevent the identified problems on his own. To help patient in motivating him to continue the health care provided by the health workers. To render nursing care and information to patient through the application of the nursing skills. To be able to develop knowledge, skills and attitude in rendering nursing care and understand the course of the disease condition To be able to acquire medical information regarding Typhoid Fever and gain understanding on the pathophysiology and etiology of the disease To be able to formulate appropriate nursing management and intervention for the patient. To help the patient prevent complications that will situate life in danger through acquiring appropriate knowledge and awareness regarding the disease condition. To provide the patient and his family important information about the disease concerning the health status of the patient. To provide the patient and her family an awareness regarding the proper management of the patient including the do’s and the dont’s in his condition. To help the patient and the family recognize significance of having good health and it’s maintenance. Part I. Assessment A. General Information Name: mE. A. Campos Age: 9 y/o Gender: male Civil Status: single Nationality: Filipino Educational Attainment: grade school Occupation: none (still as student) Religion: Pentecost Address: Maratudo, Magsingal, Ilocos Sur Arrived on unit by: tricycle Accompanied by: Mrs. Campos (mother) Chief complaint: Abdominal pain and fever Date Admitted: September 21, 2009 Time: 1:05pm Admitted by: Dr. Rapisura/ Rondal Admitting Institution: Metro Vigan Cooperative Hospital Room/Ward: Ward C Admitting Diagnosis: t/c Dengue Fever vs. Typhoid fever Admitting Vital Signs: BP: 80/60mmHg Temp: 36.7 oC Pulse: 86 bpm RR: Medications: 21 bpm Ampicillin 500mg, IV ANST qo6 Chlonampenecol 500mg, IV ANST qo6 Paracetamol 250mg /ml PO qo4 B. Nursing History I. Health Perception – Health management Pattern Client’s description of his health: Before Admission: > “nasakit tiyan ko, makasar-sarwaen nak ken agtakki nak pay.” As verbalized by the patient >he is healthy before he had stomachache, diarrhea and vomiting At Present: >“nasakit pay lang tiyan ko, haan nak met agtakkin ken maulawen” as verbalized by the patient. >he is getting well and discovered the sign and symptoms of his illness. >he is suspected to typhoid fever and he also has UTI. He sees himself as a totally ill person because he cannot do anymore the things he usually does like playing with his siblings. He rely his present condition with the help of the therapeutic personnel and by following the prescribed medications. The patient perceived that he is not healthy because of his condition Health Management: Self: Mr. Campos can manage to look to his well-being with minimal assistance. He can walk but has unsteady gait, he asks someone to carry the IV stand in going to the toilet. Family: If the nurse is not around, his mother looks up to his condition and needs. He consider his loved ones as his pillar of support. History of Present Illness: >he ate a meat of dog on Sunday evening and that’s the time he started to have a stomached ache, diarrhea and vomiting according to the mother of the patient. History of Past Illness: According to the SO of the patient the patient did not yet experienced having serious health problems other than fever, colds and cough. He had no previous hospitalization. History of Hospitalization: >This is his first hospitalization (September 21, 2009) according to the mother. History of Illness in the Family: According to the SO of the patient, their family has the history of Hypertension, UTI and Heart Disease. Expectations of Hospitalization: > “namnamaek nga mapalaing da toy anak ko ken ipan da amin nga kabaelan da tapnu malaing sigud toy anakko” as verbalized by the mother. Anticipation of problem with caring for self upon discharge: >after he will be discharge in the hospital the mother does not expect any problem regarding to the health of his son. Knowledge of treatment or practices prescribed: >the patient have some knowledge about the medication he received. Reactions to above prescriptions: >The patient feels that he is getting well because of the Medication that he received. II. Nutrition and Metabolic Pattern 2.1 Usual food intake: Breakfast: he usually eats rice, meat & bread for breakfast. Lunch: he eats rice, fish, chicken, meat & vegetable. Supper: he eats rice, fish, chicken, meat & vegetable. Snacks: he eats crackers & biscuit, junk foods. 2.2 Usual fluid intake: Preferences: he likes to drink water &soft drinks : he said that for a day, he can drink the following with their corresponding amounts as follows: >5-6 glasses of water >1-2 bottles of 8ounce softdrinks 2.3 Any problems with ability to eat >He doesn’t have any problem with his ability to eat. 2.4 Any food restrictions > The patient has loss his appetite and hasn’t eaten a lot. He is on a DAT (Diet as Tolerated) EDCF (Except Dark Colored Foods). III. Elimination Pattern 3.1 Bladder: Usual Frequency/Day: >he urinated 2-3x a day Color: >Yellow Complaints on the usual pattern urination: >He has complaints to his urination pattern. The patient has problem on his elimination pattern. He usually urinates 2-3 times a day with difficulty. He feels pain in his urination. 3.2 Bowel: Usual Pattern/Day: >he usually defecates 0-1x a day Complaints on the usual pattern of bowel movement: No pain defecating. Consistency:>Modulate or in a small amount. The patient defecates once a day usually early in the morning before going to school with yellow to brown color. He verbalized that sometimes however, it is hard in consistency with dark color, which generally depends on what he eats. 3.3 Any assertive device: >He doesn’t use any assertive device. IV. Activity Exercise Pattern 4.1 Usual daily week activities: Before Exercise: Walking before and after going to school. Leisure: Before admission: he usually watch t.v and 4.2 Any limitation of physical activity: play with his friends. Before hospitalization: He could perform activities of his daily living. According to him, he often plays with his siblings and this serves as a form of exercise for him. During hospitalization: His activity was limited lying on bed but the patient is given his bathroom privileges. V. Sleep – rest pattern Before hospitalization: He has the normal 6-8 hours sleep. He also has his nap time for 1-2 hours a day. Sleeping and watching the television are his form of rest. During hospitalization: He doesn’t have the adequate time of sleep since he is disturbed with the nurses that enter the room every now and then, and because of the environmental changes of his surroundings. He also has inadequate time to rest since he doesn’t have enough time to sleep. VI. Cognitive – Perceptual Pattern Before hospitalization: He is normal in terms of his cognitive abilities. He has good memory and reasoning skills. He can easily comprehend on things. In terms of his perceptual pattern, he has no problems with his senses. During hospitalization: He was not as normal as before in his cognitive and perceptual pattern. He responds not so clearly and not well understood. He responds inappropriately to verbal and physical stimuli but sometimes still can obey simple commands. He was not that cooperative throughout the interview that is why his mothers is the one answering some of the questions asked.. VII. Self – Perception Pattern He sees himself as a person with a good personality. He has been a good friend, brother and a son. He said he has to be a good person in order not to hurt others. He also describes himself as a typical type of student and person. VIII. Role – Relationship Pattern 8.1 Language spoken: The patient can speak Filipino, and Iloco. He conversed mostly in Iloco and was able to express himself well. 8.2 Manage of Speaking: Client speaks more on Iloco. Client is not very fluent in speaking Filipino, but can understand the language a little. 8.3 Significant other to client: Client’s significant other is her mother. 8.4 Complaints Regarding the Family: The client has no complaints about her family. Before hospitalization: He has a close relationship with his family. They were five siblings in their family. He was at the middle. I was also able to ask his mother about his being a son and she confessed that he is a good son but at times he doesn’t obey her. He is also a responsible student and knows all his duties as a friend. During hospitalization: He learned to appreciate the beauty of having a family that gives you strength and support no matter what. But, he is very much irritable because he is sick. IX. Sexuality – Sexual Pattern He didn’t respond to this matter. X. Coping – Stress management Pattern Before hospitalization: He does not fully identify his situations having stress but he always tell his parents when something is wrong. During hospitalization: He shares his problems to his family. He verbalizes his feelings especially to his mother. XI. Value Belief System 11.1 Source of strength and meaning > For the client the primary source of strength in giving meaning to his life is God and next to God is his family. For his God is his greatest strength and savior especially in his difficult situation in his life…. 11.2 Importance of God to client > For the client God is very important to her and to his family for she consider God as their savior, protector and Lord in his life. 11.3 Religious Practices > The client seldom hears mass and seldom prays. 11.4 Request for religious person/practice > The patient doesn’t have any request for religious person. Paradigm of the Pathophysiology of the Disease Ingestion of Bacteria (Direct/indirect contact with a carrier of disease & ingestion of contaminated food or water) Bloodstream Reticuloendothelial system (Lympnodes, Peyer’s patches, spleen, liver) Lymph nodes are swollen Elevation of temperature Formation of sloughs which are often bile colored There is chilly Development of sensation & aching all rose spots, abdominal over the body pain and splenomegaly Intense intestinal inflammatory response particularly in the Peyer’s patches with associated necrosis The fever is accelerated &, nausea, vomiting, and diarrhea Hemorrhage & perforation occur Typhoid Fever Explanation: The pathophysiology of typhoid fever is a complex process which proceeds through several stages. The disease begins through ingestion of the bacteria Salmonella typhosa through contaminated food or water or having a direct or indirect contact with a carrier of the disease which later gains access to the blood stream (bacteremia). During which bacteria invade macrophages and spread throughout the reticuloendothelial system (Lympnodes, Peyer’s patches, spleen, liver) which result the lymph nodes swollen which is manifested by elevation of temperature. Then there is a Formation of sloughs which are often bile colored which is develod rose spots, abdominal pain and splenomegaly as manifested by chilling sensation & aching all over the body. From here a marked of a more intense intestinal inflammatory response particularly in the Peyer’s patches with associated necrosis is develops due to result of perforation and hemorrhage due to the extension of the lesion and continous erosion of the epithelial lining of the small intestines which is manifested by fever acceleration, nausea, vomiting, and diarrhea which results Typhoid Fever. Clinical Manifestation 1. Onset a. Headache, chilly sensation, aching all over the body b. Nausea, vomiting, and diarrhea c. By the 4th and 5th day, all symptoms are worst d. Fever is higher in the morning than it was in the afternoon e. Breathing is accelerated, the tongue is furred, the skin is dry and hot, abdomen is distended and tender f. Rose spots appear on the abdominal wall on the 7th to the 9th day g. On the second week symptoms become more aggravated. Temperature remains in uniform level. Rose spots become more prominent. 2. Typhoid State a. Intense symptoms decline in severity b. The tongue protrudes, becomes dry and brown c. Teeth and lips accumulate a dirty-brown collection of dried mucus and bacteria known as sordes (preventable by good nursing care) d. Patient seems to be starring blankly (Coma vigil) e. Twitching of the tendon sets in especially the wrist (subsultus tendinum) f. Patient mutters deliriously and picks up aimlessly at bedclothes with his fingers in continous fashion (Carphologia) g. There is constant tendency of the patient to slip down to the foot part of the bed h. In severe cases rambling delirium sets in, often ending in death What is typhoid fever? Typhoid fever is a life-threatening bacterial infection caused by the bacterium Salmonella Typhi (S. Typhi). According to the CDC, typhoid fever is common in developing countries, where it affects about 22 million persons each year. The incidence of typhoid fever in US citizens and residents who travel abroad is very low. How is typhoid fever spread? S. Typhi live only in humans, and are carried in the bloodstream and intestinal tracts of people who have typhoid fever. A small number of persons recover from typhoid fever but continue to carry the bacteria. Both the carriers and the people who have active typhoid fever shed S. Typhi in their stools. Typhoid fever is spread by consuming food or beverages that have been handled by a person who is shedding S. Typhi, or if sewage contaminated with S. Typhi bacteria gets into water used for drinking or washing food. What are the symptoms of typhoid fever? When S. Typhi bacteria are consumed, they multiply and spread into the bloodstream. The body reacts with signs and symptoms such as: a sustained fever as high as 103°F to 104° F (39 to 40 C) weakness stomach pains headache loss of appetite sometimes a rash of flat, rose-colored spots The symptoms of typhoid fever may resemble other medical conditions or problems. Always consult your physician for a diagnosis. How is typhoid fever diagnosed? Typhoid fever can be diagnosed using a blood test or stool sample to determine the presence of S. Typhi bacteria. How can typhoid fever be prevented? A vaccination for typhoid fever is available. However, it can lose effectiveness after several years, so a booster vaccination may be necessary. Other preventives for typhoid fever are: only use water that has been boiled or chemically disinfected for: o drinking, or preparing beverages such as tea or coffee o brushing teeth o washing face and hands o washing fruits and vegetables o washing eating utensils and food preparation equipment o washing the surfaces of tins, cans, and bottles that contain food or beverages do not eat food or drink beverages from unknown sources any raw food could be contaminated, including: o fruits, vegetables, salad greens o unpasteurized milk and milk products o raw meat o shellfish o any fish caught in tropical reefs rather than the open ocean Taking antibiotics is not a preventive for typhoid fever. Treatment for typhoid fever: See your physician immediately if you think you have been exposed to typhoid fever. People who do not get treatment may continue to have fever for weeks or months, and may eventually die from complications. Treatment will probably include an antibiotic to treat the disease. Specific treatment for typhoid fever will be determined by your physician based on: your age, overall health, and medical history extent of the disease your tolerance for specific medications, procedures, or therapies expectations for the course of the disease your opinion or preference It is important to remember that the danger of typhoid fever does not end when symptoms disappear. You could still be carrying S. Typhi and the illness could return, or you could pass the disease to other people. People who have typhoid fever should: take any prescribed antibiotics. wash your hands after using the bathroom. have a series of stool cultures - to ensure that the S. Typhi bacteria are no longer present. C. PHYSICAL ASSESSMENT Date assessed: September 23, 2009 General assessment: conscious and coherent Initial vital signs: BP: 80/60mmHg Temp: 36.7 oC Pulse: 86 bpm RR: 21 bpm A. Head 1. Skull Methods of Assessment: Palpation and Inspection > Proportional to size, oval with prominence in frontal, symmetrical in all planes, no lumps, smooth skull contour. 2. Scalp/ hair Methods of Assessment: Inspection > White scalp, no lies, nits and dandruff, no lesions, hair evenly distributed. Slightly thin, shiny, free from split ends. 3. Face Methods of Assessment: Inspection > Oval, symmetrical facial movements, facial expressions depend on mood, no involuntary movements. 4. Eyes/ Vision External eye structures Method of Assessment: Inspection Eyes are symmetrical in line with outer canthus and with pink conjunctiva, skin intact, lids closed symmetrically, sclera is white Eyeball No protrusion, scant amount of secretion Lid Margins No scaling, lid closed symmetrically, no discoloration, no discharges 18 involuntary-blinks/min Eyebrows/ lashes symmetrically, thin, raises and lower symmetrically, hair evenly distributed, parallel with each other. Visual Acuity Method of assessment: Inspection White sclera and Salmon pink, shinny moist conjunctiva Extraocular muscle function (cranial nerve III, IV and VI) Method of assessment: Inspection Eyes are able to move superiorly, laterally without experiencing pain. Pupillary Reflex Method of assessment: Inspection Both pupils react to light Internal Eye Structure with opthalmascope -----not done----5. Ears/ Hearing External Ear Method of Assessment: Inspection Pinna Parallel, symmetrical proportional to size of hand, bean shaped, skin is same as surrounding area in line with outer cantus of the eyes. Palpation Firm cartilage, non tender, recoils after it is folded External Canal Pinkish clean with scant amount of serum Hearing Method of Assessment: Inspection The patient has no hearing defect, he is able to hear sounds clearly and he can hear ticking sounds on both ears. Ear canal and tympanic membrane with otoscope ----not done---6. Nose Nasal system intact in midline, symmetrical, no discharge, no flaring 7. Mouth/ lips Pinkish, smooth, moist, well- defined, symmetrical Gums Pinkish, moist, no swelling, no discharge, no reaction Teeth well-aligned, free from caries, no halitosis Tongue Central position, medium,pink, slightly rough on top, moist, shiny and freely movable Palate Hart palate lighter pink, more irregular texture Soft palate light pink, smooth uvula in midline Oropharynx/ tonsils pink,smooth,no discharge behind tonsillar pillars, gag reflex 8. Cheeks smooth 9. Neck proportional to the size of the body and head, symmetrical and slightly able to move no lump, masses or tenderness 10. Chest Symmetrical, fair complexion, no deformities, with 18 breaths/ minute no lumps, masses and tenderness and area of deformities. 11. Heart No heaves or abnormal pulsation. apical pulse is 89 beats/min >jugular veins are not visible 12. Breast no heaves or abnormal pulsation. >jugular veins are not visible. >symmetrical, slightly brownish nipple, no dimpling, cracks and discharge. >uniform skin color, smooth intact, no lumps, masses and tenderness. 13. Abdomen >symmetrical, same color as the color of the body, no scars audible bowel sounds, no friction rub. >no masses, lumps, tenderness and distention. Tympany in all quadrants 14. Upper extremities Musculoskeletal structures, skin, nails Method of Assessment: Inspection and Palpation Muscles are equal in size with coordinated body movements without discomfort and pain; no noted swelling or masses. Lymph Nodes Method of Assessment: Palpation Non-palpable Thyroid gland Method of Assessment: Palpation Non-palpable 15. Lower Extremities Musculoskeletal structures, skin and toenails Method of Assessment: Inspection With fair skin color, with untrimmed toenails, symmetrical right and left lower extremities, no edema noted Musculoskeletal functions Method of Assessment: Inspection Able to move right lower extremity, with limitations, with(-) deformity,(-) tenderness Deep tendon reflexes and plantar reflex ----not done---16. Genitals and Pelvis External genitals: ----not done----17. Rectum -----not done---D. LABORATORY EXAMINATIONS Cross Matching Cross-matching blood, in transfusion medicine, refers to the complex testing that is performed prior to a blood transfusion, to determine if the donor's blood is compatible with the blood of an intended recipient, or to identify matches for organ transplants. Cross-matching is usually performed only after other, less complex tests have not excluded compatibility. Blood compatibility has many aspects, and is determined not only by the blood types (O,A,B,AB), but also by blood factors, (Rh, Kell, etc,) Blood Type: AB RH Type: positive Hematocrit and hemoglobin measurements are blood tests. They are part of a complete blood count, or CBC. Hematocrit measures the amount of red blood cells that are in blood. Hemoglobin is a protein-iron compound in the blood that carries oxygen from the lungs to all cells. A hemoglobin test determines how much hemoglobin is in the blood. Together, the hematocrit and hemoglobin tests help diagnose anemia and polycythemia. Anemia is a shortage of red blood cells due to reduced production of red cells, destruction of red cells, or loss of red cells from internal or external bleeding. Polycythemia is production of too many red blood cells. Test: Result Normal value Hematocrit 28% M(40-54%) Hemoglobin 96g/L M(135-180g/L) Nursing Responsibilities: Before the Test: Explain the test procedure and the purpose of the test. Assess the clients knowledge of the test During the Test: Adhere to standard precautions After the test: Apply pressure to the venipuncture site. Explain that some bruising, discomfort and swelling may appear at that site that warm, moist compress can alleviate this. Monitor signs of infection. Notify the doctor of significant findings and administer blood products as ordered based on the test results. Typhoid IgM- Negative IgG-Positive IgM Positive Only Acute typhoid fever -Implications for the presence of IgG antibodies include previous infection(in which case current fever may not be due to typhoid) or relapse or re infection. IgM and IgG positive Acute typhoid fever(in the middle of infection) IgM-IgG negative probably not typhoid Dengue Test Igm-Negative IgG- Negative Urinalysis Urinalysis is the physical, chemical, and microscopic examination of urine. It involves a number of tests to detect and measure various compounds that pass through the urine. Test Result Macroscopic Exam Color Yellow Transparency Slightly Chemical Exam Specific Gravity 1.005 pH 7.0 Sugar -(Neg) Albumin - Nitrites - Blood - Microscopic exam Pus cell 1-3 hpf RBC 3-6 hpf Epithelial cells few Amorphous Urates Occassional Radiology Department Normal Chest Findings The lungs are clear The heart is not enlarged Mediastinum, diaphragm and sulci are intact Ultrasound Ultrasonography is another procedure for viewing areas inside the body. Highfrequency sound waves that cannot be heard by humans enter the body and bounce back. Their echoes produce a picture called a sonogram. These pictures are shown on a monitor like a TV screen and can be printed on paper. Impression: Unremarkable liver, gallbladder, pancreas, spleen, kidneys and Urinary Bladder -Negative for Ascites or hydrothorax EVALUATION I. Discharge Planning Medications Ampicillin 500mg, IV ANST qo6 Chlonampenecol 500mg, IV ANST qo6 Paracetamol 250mg /ml PO qo4 Exercise Have physical activities in tolerable one Take enough rest and sleep. Treatment Should undergo medical procedure if instructed to prevent the progression of the disease. Health Teachings Stay away from factors that contribute to the occurrence of further harm to his condition and he must not eat raw foods, instead he must eat the ones that are nutritious OPD Follow – Up Should regularly consult her health care provider or the clinic to note for any changes in status. To have a follow – up check – up in the OPD after 1 week. Diet Eat variety of nutritious foods for energy source and reservation Law salt, sodium and cholesterol intake Increase intake of Vitamin C and protein rich foods. Iron rich foods to prevent anemia. References: Reyala, Jean P, et. Al. Community Health Nursing Services in the Philippines. 9th Edition.,2000 http://emedicine.medscape.com/article/231135-overview http://www.pediatriconcall.com/fordoctor/diseasesandcondition/infectious_diseases/ty phoid_fever.asp http://www.rapidlearningcenter.com/biology/anatomy-physiology/19-The-DigestiveSystem.html http://www.soulhealer.com/anatomy-dig.htm E. Data from TEXTBOOK Description: A systemic infection characterized by continued fever, malaria, anorexia, slow pulse, involvement of lymphoid tissues, especially ulceration of Peyer’s Patches, enlargement of spleen, rose spots on trunk and diarrhea. Many mild typical infections are often unrecognized. A usual fatality of 10% is reduced to 2 or 3 % by antibiotic therapy. Etiologic Agent: Salmonella typosa, typhoid bacillus Source of Infection: Feces and urine of infected persons Family contacts may be transient carrier. Carrier state is common among persons over 40 years of age especially females. Mode of Transmission: Direct or indirect contact with patient or carrier. Principal vehicles are food and water. Contamination is usually by hands of carrier. Flies are vectors. Incubation Period: Variable, average 2 weeks, usual range 1 to 3 weeks. Period of Communicability: As long as typhoid bacilli appear in excreta; usually from appearance of prodromel symptoms from first week through out convalescence. Susceptibility, Resistance and Occurrence: Susceptibility is general although many adults appear to acquire immunity through unrecognized infections. Attack rates decline with age after second or third decades. A high degree of resistance usually follows recovery. Methods of prevention and Control: Same preventive and control measures in Dysentery and in addition, immunization with a vaccine of high antigenecity. Nursing Responsibilities: Demonstrate to family how to give bedside care, such as tepid sponge, feeding, changing of bed linen, use of bedpan and mouth care. Any bleeding from the rectum, blood in stools, sudden acute abdominal pain, restlessness, falling of temperature should be reported at once to the physician or the patient should be brought to the hospital. CONCLUSIONS After having series of research about the disease, its management and after completing the case study, the group had come out with the following conclusions. That although the group had not monitored the patient’s discharge, follow – up check up must be done. That a specimen taken from him during the span of hospitalization and any other procedure be established for further diagnostic test, exams and detection for the progression of the disease. That there should be a continuous monitoring of the patient’s condition with regards to changes with his digestive system, skin turgor, respiratory status and other systemic affectations of his condition. That patient will be given nutritious foods rich in carbohydrates, proteins such as meat and beans, iron rich foods and vitamin C rich foods, including citrus fruits to regain energy. That the patient will closely monitor for administration of medicines to prevent further systemic complication and any other serious complications. RECOMMENDATIONS After dealing with the patient and studying his condition we recommend him the following: Should comply to any medical procedure so that more serious complications can be prevented. Have him visit regularly with the physicians for more intensive monitoring and treatment of the disease condition. Should undergo regular check-ups, medical procedure laboratory examinations to make definitive diagnosis, and other lab results and assess if it is a risk for the development of other serious complications Eat foods that have been thoroughly cooked and that are still hot and steaming. Avoid raw vegetables and fruits that cannot be peeled. Vegetables like lettuce are easily contaminated and are very hard to wash well. He must be very careful with the foods he will take in, and he must always remember the preventive measures. Avoid foods and beverages from street vendors. It is difficult for food to be kept clean on the street. REVIEW OF ANATOMY AND PHYSIOLOGY Each cell of the body requires a constant supply of nutrients to use as the basic building blocks of the body and for the hundreds of biochemical process that are continuously going on within the body. The digestive system is the way in which the body transforms food into the energy it needs to build, repair and fuel itself. To be absorbed and used by the body, however, food substances must first be broken down into pieces small enough to cross the cellular membrane. The first step in this process is digestion. Digestion begins in the mouth. Food, once chewed, travels through the throat or pharynx to the esophagus and then on to the stomach. From the stomach, it passes into the small, then large intestines where it is further digested with the aid of bile and enzymes from the pancreas and liver, and finally absorbed. Any waste materials of this process exit the body through the colon and rectum. Gastrointestinal tract The gastrointestinal tract (GIT) consists of a hollow muscular tube starting from the oral cavity, where food enters the mouth, continuing through the pharynx, oesophagus, stomach and intestines to the rectum and anus, where food is expelled. There are various accessory organs that assist the tract by secreting enzymes to help break down food into its component nutrients. Thus the salivary glands, liver, pancreas and gall bladder have important functions in the digestive system. Food is propelled along the length of the GIT by peristaltic movements of the muscular walls. The primary purpose of the gastrointestinal tract is to break down food into nutrients, which can be absorbed into the body to provide energy. First food must be ingested into the mouth to be mechanically processed and moistened. Secondly, digestion occurs mainly in the stomach and small intestine where proteins, fats and carbohydrates are chemically broken down into their basic building blocks. Smaller molecules are then absorbed across the epithelium of the small intestine and subsequently enter the circulation. The large intestine plays a key role in reabsorbing excess water. Finally, undigested material and secreted waste products are excreted from the body via defecation (passing of feces). In the case of gastrointestinal disease or disorders, these functions of the gastrointestinal tract are not achieved successfully. Patients may develop symptoms of nausea, vomiting, diarrhea, mal absorption, constipation or obstruction. Gastrointestinal problems are very common and most people will have experienced some of the above symptoms several times throughout their lives. In the digestive system, ingested food is converted into a form that can be absorbed into the circulatory system for distribution to and utilization by the various tissues of the body. This is accomplished both physically, by mastication in the mouth and churning of the stomach, and chemically, by secretions and enzymes of the gastrointestinal tract. Beginning at the mouth, all food passes through the alimentary canal (pharynx, esophagus, stomach, and intestines) before it reaches the anus, where undigested matter is eliminated as waste. The outer walls of the digestive tract are composed of layers of muscle and tissue that undergo waves of contraction (peristalsis), thereby pushing the food along its digestive path. The inner lining contains glands that secrete the acids and enzymes necessary to break down food into a form utilizable by the body. Digestion begins in the mouth, where chewing reduces the food to fine texture, and saliva moistens it and begins the conversion of starch into simple sugars by means of an enzyme, salivary amylase. The food is then swallowed, passing through the pharynx and down the muscular esophagus, or gullet, to the expanded muscular pouchlike section of the gastrointestinal tract, the stomach. Specialized cells in the stomach secrete digestive enzymes and gastric juices, which act on the partially digested food. The stomach also physically churns and mixes the food. The stomach secretions include the enzyme pepsin, which acts on proteins; hydrochloric acid, essential for the action of pepsin; and an enzyme, gastric lipase, which begins the breakdown of fats. The gastric juices of young children contain, in addition to those just mentioned, the enzyme rennin, which acts on milk. Some foods, including simple sugars and alcohol, are absorbed directly through the stomach wall and do not remain in the stomach. Most food, however, is not absorbed in the stomach and passes into the duodenum (first section of the small intestine) in the form of a thick liquid called chyme. Digestive enzymes from the pancreas and bile from the liver act on the chyme in the duodenum. These enzymes include pancreatic lipase, which breaks down fats into glycerol and fatty acids; pancreatic amylase, which continues the breakdown of starches and most other carbohydrates into disaccharides; and trypsin and erepsin, which break down whole and partially digested proteins (proteoses and peptones) into amino acids, the end products of protein digestion. Bile is essential for emulsifying large fat globules into smaller ones that are more easily digested by pancreatic lipase. In addition, intestinal juices are secreted by small glands in the intestinal wall called the crypts of LieberkUhn. Like the pancreatic juices, intestinal juices contain enzymes that continue the digestion of proteins and fats and also contain three enzymes that break down disaccharides into glucose, galactose, and fructose (simple sugars). The digested food is absorbed into the circulatory and lymphatic systems through small fingerlike projections of the intestinal wall, called villi. Undigested material passes into the large intestine, where most of the water is absorbed and the solid material, or feces, is excreted through the anus. Basic structure The gastrointestinal tract is a muscular tube lined by a special layer of cells, called epithelium. The contents of the tube are considered external to the body and are in continuity with the outside world at the mouth and the anus. Although each section of the tract has specialised functions, the entire tract has a similar basic structure with regional variations. The wall is divided into four layers as follows: Mucosa: The innermost layer of the digestive tract has specialised epithelial cells supported by an underlying connective tissue layer called the lamina propria. The lamina propria contains blood vessels, nerves, lymphoid tissue and glands that support the mucosa. Depending on its function, the epithelium may be simple (a single layer) or stratified (multiple layers). Areas such as the mouth and oesophagus are covered by a stratified squamous (flat) epithelium so they can survive the wear and tear of passing food. Simple columnar (tall) or glandular epithelium lines the stomach and intestines to aid secretion and absorption. The inner lining is constantly shed and replaced, making it one of the most rapidly dividing areas of the body! Beneath the lamina propria is the muscularis mucosa. This comprises layers of smooth muscle which can contract to change the shape of the lumen. Submucosa: The submucosa surrounds the muscularis mucosa and consists of fat, fibrous connective tissue and larger vessels and nerves. At its outer margin there is a specialized nerve plexus called the submucosal plexus or Meissner plexus. This supplies the mucosa and submucosa. Muscularis externa: This smooth muscle layer has inner circular and outer longitudinal layers of muscle fibres separated by the myenteric plexus or Auerbach plexus. Neural innervations control the contraction of these muscles and hence the mechanical breakdown and peristalsis of the food within the lumen. Serosa/ Mesentery: The outer layer of the GIT is formed by fat and another layer of epithelial cells called mesothelium. The Individual Components of the Gastrointestinal System Oral cavity The oral cavity or mouth is responsible for the intake of food. It is lined by a stratified squamous oral mucosa with keratin covering those areas subject to significant abrasion, such as the tongue, hard palate and roof of the mouth. Mastication refers to the mechanical breakdown of food by chewing and chopping actions of the teeth. The tongue, a strong muscular organ, manipulates the food bolus to come in contact with the teeth. It is also the sensing organ of the mouth for touch, temperature and taste using its specialised sensors known as papillae. Insalivation refers to the mixing of the oral cavity contents with salivary gland secretions. The mucin (a glycoprotein) in saliva acts as a lubricant. The oral cavity also plays a limited role in the digestion of carbohydrates. The enzyme serum amylase, a component of saliva, starts the process of digestion of complex carbohydrates. The final function of the oral cavity is absorption of small molecules such as glucose and water, across the mucosa. From the mouth, food passes through the pharynx and oesophagus via the action of swallowing. Salivary Glands Three pairs of salivary glands communicate with the oral cavity. Each is a complex gland with numerous acini lined by secretory epithelium. The acini secrete their contents into specialised ducts. Each gland is divided into smaller segments called lobes. Salivation occurs in response to the taste, smell or even appearance of food. This occurs due to nerve signals that tell the salivary glands to secrete saliva to prepare and moisten the mouth. Each pair of salivary glands secretes saliva with slightly different compositions. Parotids: The parotid glands are large, irregular shaped glands located under the skin on the side of the face. They secrete 25% of saliva. They are situated below the zygomatic arch (cheekbone) and cover part of the mandible (lower jaw bone). An enlarged parotid gland can be easier felt when one clenches their teeth. The parotids produce a watery secretion which is also rich in proteins. Immunoglobins are secreted help to fight microorganisms and aamylase proteins start to break down complex carbohydrates. Submandibular: The submandibular glands secrete 70% of the saliva in the mouth. They are found in the floor of the mouth, in a groove along the inner surface of the mandible. These glands produce a more viscid (thick) secretion, rich in mucin and with a smaller amount of protein. Mucin is a glycoprotein that acts as a lubricant. Sublingual: The sublinguals are the smallest salivary glands, covered by a thin layer of tissue at the floor of the mouth. They produce approximately 5% of the saliva and their secretions are very sticky due to the large concentration of mucin. The main functions are to provide buffers and lubrication. esophagus The esophagus is a muscular tube of approximately 25cm in length and 2cm in diameter. It extends from the pharynx to the stomach after passing through an opening in the diaphragm. The wall of the oesophagus is made up of inner circular and outer longitudinal layers of muscle that are supplied by the oesophageal nerve plexus. This nerve plexus surrounds the lower portion of the oesophagus. The oesophagus functions primarily as a transport medium between compartments. Stomach The stomach is a J shaped expanded bag, located just left of the midline between the esophagus and small intestine. It is divided into four main regions and has two borders called the greater and lesser curvatures. The first section is the cardia which surrounds the cardial orifice where the oesophagus enters the stomach. The fundus is the superior, dilated portion of the stomach that has contact with the left dome of the diaphragm. The body is the largest section between the fundus and the curved portion of the J. This is where most gastric glands are located and where most mixing of the food occurs. Finally the pylorus is the curved base of the stomach. Gastric contents are expelled into the proximal duodenum via the pyloric sphincter. The inner surface of the stomach is contracted into numerous longitudinal folds called rugae. These allow the stomach to stretch and expand when food enters. The stomach can hold up to 1.5 litres of material. The functions of the stomach include: 1. The short-term storage of ingested food. 2. Mechanical breakdown of food by churning and mixing motions. 3. Chemical digestion of proteins by acids and enzymes. 4. Stomach acid kills bugs and germs. 5. Some absorption of substances such as alcohol. Most of these functions are achieved by the secretion of stomach juices by gastric glands in the body and fundus. Some cells are responsible for secreting acid and others secrete enzymes to break down proteins. Small Intestine The small intestine is composed of the duodenum, jejunum, and ileum. It averages approximately 6m in length, extending from the pyloric sphincter of the stomach to the ileo-caecal valve separating the ileum from the caecum. The small intestine is compressed into numerous folds and occupies a large proportion of the abdominal cavity. The duodenum is the proximal C-shaped section that curves around the head of the pancreas. The duodenum serves a mixing function as it combines digestive secretions from the pancreas and liver with the contents expelled from the stomach. The start of the jejunum is marked by a sharp bend, the duodenojejunal flexure. It is in the jejunum where the majority of digestion and absorption occurs. The final portion, the ileum, is the longest segment and empties into the caecum at the ileocaecal junction. The small intestine performs the majority of digestion and absorption of nutrients. Partly digested food from the stomach is further broken down by enzymes from the pancreas and bile salts from the liver and gallbladder. These secretions enter the duodenum at the Ampulla of Vater. After further digestion, food constituents such as proteins, fats, and carbohydrates are broken down to small building blocks and absorbed into the body's blood stream. The lining of the small intestine is made up of numerous permanent folds called plicae circulares. Each plica has numerous villi (folds of mucosa) and each villus is covered by epithelium with projecting microvilli (brush border). This increases the surface area for absorption by a factor of several hundred. The mucosa of the small intestine contains several specialised cells. Some are responsible for absorption, whilst others secrete digestive enzymes and mucous to protect the intestinal lining from digestive actions. Large Intestine The large intestine is horse-shoe shaped and extends around the small intestine like a frame. It consists of the appendix, caecum, ascending, transverse, descending and sigmoid colon, and the rectum. It has a length of approximately 1.5m and a width of 7.5cm. The caecum is the expanded pouch that receives material from the ileum and starts to compress food products into faecal material. Food then travels along the colon. The wall of the colon is made up of several pouches (haustra) that are held under tension by three thick bands of muscle (taenia coli). The rectum is the final 15cm of the large intestine. It expands to hold faecal matter before it passes through the anorectal canal to the anus. Thick bands of muscle, known as sphincters, control the passage of faeces. The mucosa of the large intestine lacks villi seen in the small intestine. The mucosal surface is flat with several deep intestinal glands. Numerous goblet cells line the glands that secrete mucous to lubricate faecal matter as it solidifies. The functions of the large intestine can be summarised as: 1. The accumulation of unabsorbed material to form faeces. 2. Some digestion by bacteria. The bacteria are formation of intestinal gas. 3. Reabsorption of water, salts, sugar and vitamins. Liver responsible for the The liver is a large, reddish-brown organ situated in the right upper quadrant of the abdomen. It is surrounded by a strong capsule and divided into four lobes namely the right, left, caudate and quadrate lobes. The liver has several important functions. It acts as a mechanical filter by filtering blood that travels from the intestinal system. It detoxifies several metabolites including the breakdown of bilirubin and oestrogen. In addition, the liver has synthetic functions, producing albumin and blood clotting factors. However, its main roles in digestion are in the production of bile and metabolism of nutrients. All nutrients absorbed by the intestines pass through the liver and are processed before traveling to the rest of the body. The bile produced by cells of the liver, enters the intestines at the duodenum. Here, bile salts break down lipids into smaller particles so there is a greater surface area for digestive enzymes to act. Gall Bladder The gallbladder is a hollow, pear shaped organ that sits in a depression on the posterior surface of the liver's right lobe. It consists of a fundus, body and neck. It empties via the cystic duct into the biliary duct system. The main functions of the gall bladder are storage and concentration of bile. Bile is a thick fluid that contains enzymes to help dissolve fat in the intestines. Bile is produced by the liver but stored in the gallbladder until it is needed. Bile is released from the gall bladder by contraction of its muscular walls in response to hormone signals from the duodenum in the presence of food. Pancreas Finally, the pancreas is a lobular, pinkish-grey organ that lies behind the stomach. Its head communicates with the duodenum and its tail extends to the spleen. The organ is approximately 15cm in length with a long, slender body connecting the head and tail segments. The pancreas has both exocrine and endocrine functions. Endocrine refers to production of hormones which occurs in the Islets of Langerhans. The Islets produce insulin, glucagon and other substances and these are the areas damaged in diabetes mellitus. The exocrine (secretrory) portion makes up 80-85% of the pancreas and is the area relevant to the gastrointestinal tract. It is made up of numerous acini (small glands) that secrete contents into ducts which eventually lead to the duodenum. The pancreas secretes fluid rich in carbohydrates and inactive enzymes. Secretion is triggered by the hormones released by the duodenum in the presence of food. Pancreatic enzymes include carbohydrases, lipases, nucleases and proteolytic enzymes that can break down different components of food. These are secreted in an inactive form to prevent digestion of the pancreas itself. The enzymes become active once they reach the duodenum.