Luke Clements handout
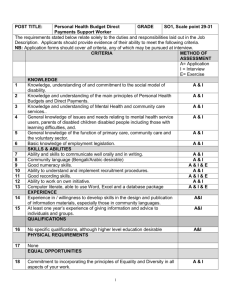
advertisement

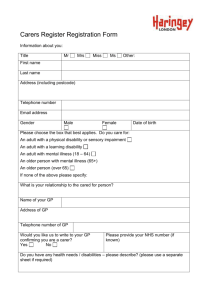
Community Care, Carers Rights and the Law overview notes Luke Clements1 The Key Community Care Statutes 1. National Assistance Act 1948 s21 - the duty / power to provide residential accommodation the provisions apply to persons aged 18 or over who by reason of age, illness, disability or any other circumstances2 are in need of care and attention which is not otherwise available to them. The duty is owed to persons ordinarily resident in the LA area, whereas a power exists to accommodate others. 2. Chronically Sick & Disabled Persons Act 1970 s2 - places a duty on the Local Authority to provided a range of services for disabled people (of any age) once it is ‘satisfied … that it is necessary in order to meet the needs of that person’ – the services being: (a) practical assistance in the home The Ombudsman has held: it to be maladministration for a council to have criteria which stipulate that no domestic assistance can be provided – unless accompanied by a need for personal care3 it is maladministration for a local authority to suggest that bathing is not an "essential activity - unless there was an identified medical need" 4 that the ability to properly manage bathing / washing with dignity is the entitlement of everybody5. (b) wireless. TV, library etc. (c) lectures, games outings and other recreational/educational facilities (d) assistance in travelling to community based care services (e) home adaptations (f) holidays (g) meals (at home or elsewhere) (h) a telephone 3. Mental Health Act 1983 (s117) When a person who has been detained under s3 MHA 1983 (or one of the criminal provisions) is discharged from hospital, he or she has a right to have their after care services provided free of charge under s117 Mental Health Act 1983. In R v Mental Health Review Tribunal ex p Hall (1999)6 the Divisional Court held that the duty to provide after care services under s117(2) was jointly shared by the health and social services authority in which the patient was resident at the time he was detained. 4. Community care services and children Section 17 Children Act 1989 enables social services departments to provide a comprehensive range of services (residential and non-residential) to ‘promote and safeguard the interests of children in need. However, services under s2 Chronically Sick and Disabled Persons Act 1970 are (by virtue of s28A) also available for disabled children. R v Bexley LBC ex p. B (1995) concerned the provision of care services for a severely disabled boy of 10. The respondent council sought to argue (amongst other things) that his home care services were being provided under the Children Act 1989 rather than under s2. Latham J rejected the argument. 1 Solicitor Scott-Moncrieff, Harbour & Sinclair (London) and Professor Cardiff Law School & author ‘Community Care & the Law’ Legal Action (4th ed) 2007. 2 Except destitution due to asylum status, see below. 3 Complaint No. 01/C/17519 against Salford CC 11.12.03 4 Complaint 02/A/11294 against Wycombe District Council 20 th October 2004. 5 Complaint 02/C/8679, 8681 & 10389 against Bolsover District Council 30 th September 2003. 6 (1999) 2 CCLR 361. 1 www.lukeclements.com November 2010 Assessments and eligibility criteria s47(1) NHS & Community Care Act 1990 obliges social services authorities to carry out an assessment of an individual’s needs for community care services. The assessment duty consists of three phases: 1. Gathering information concerning the disabled person’s needs and requirements (this will include contacting significant information sources such as family, carers, GP’s, housing etc. 2. Deciding which of these various requirements ‘call for the provision of services by the social services department’. 3. Constructing a care plan to detail how these need’s will be met by specified services. The Department of Health’s 2010 policy guidance ‘Prioritising need in the context of Putting People First: A whole system approach to eligibility for social care. Guidance on Eligibility Criteria for Adult Social Care, England 2010’ provides as follows: Critical7 – when life is, or will be, threatened; &/or Significant health problems have developed or will develop; &/or there is, or will be, little or no choice & control over vital aspects of the immediate environment; &/or serious abuse or neglect has occurred or will occur; &/or there is, or will be, an inability to carry out vital personal care or domestic routines; &/or vital8 involvement in work, education or learning cannot or will not be sustained; &/or vital social support systems & relationships cannot or will not be sustained; &/or vital family & other social roles & responsibilities cannot or will not be undertaken. Substantial – when there is, or will be, only partial choice & control over the immediate environment; &/or abuse or neglect has occurred or will occur; &/or there is, or will be, an inability to carry out the majority of personal care or domestic routines; &/or involvement in many aspects of work, education or learning cannot or will not be sustained; &/or the majority of social support systems & relationships cannot or will not be sustained; &/or the majority of family & other social roles & responsibilities cannot or will not be undertaken. Moderate – when there is, or will be, an inability to carry out several personal care or domestic routines; &/or involvement in several aspects of work, education or learning cannot or will not be sustained; &/or Several social support systems & relationships cannot or will not be sustained; &/or Several family & other social roles & responsibilities cannot or will not be undertaken. Low – when there is, or will be, an inability to carry out one or two personal care or domestic routines; &/or involvement in one or two aspects of work, education or learning cannot or will not be sustained; &/or one or two social support systems & relationships cannot or will not be sustained; &/or one or two family & other social roles & responsibilities cannot or will not be undertaken. 7 Critical means that life is threatened or individuals are at great risk of serious illness or harm (Q3.6 of the FACS 2003 practice guidance). 8 Vital means that without help, individuals are at great risk of either losing their independence, possibly necessitating admission to institutional care or making very little, damaging or inappropriate contributions to family and wider community life with serious consequences for the individual and others … [however] ‘what may be “vital” to one individual may not be “vital” to another’ (Q3.6 of the FACS 2003 practice guidance).]. www.lukeclements.com March 2011 2 Eligibility criteria and the question of resources In R v Gloucestershire County Council ex p Barry9 it was held that social services can take their available resources into account, in framing their eligibility criteria. This principle is, however, subject to four constraints: 1. When such authorities make their eligibility criteria more severe, existing service users must be the subject of a full individual community care re-assessment before any decision can be taken as to the withdrawal of services; 2. Once it has been decided that services should be provided, then they must be provided, regardless of resource constraints; 3. Resource availability alone cannot be ‘determinative’: it cannot be the only factor to be taken into account:. 4. Resource availability will not be a relevant factor where a disabled person would be at severe physical risk if the services were not provided. Failure to provide an assessed need Once an authority has made a decision under s47(1)(b) that a person’s need is such that community care services are called for, then the authority must make arrangements for those services to be provided. The practice guidance describes this final phase of the assessment process as “care planning”. Good practice requires that the authority specify in a care plan what services the individual is entitled to receive, their frequency, duration and so on. Financial resource shortages In R v South Lanarkshire Council ex p MacGregor (2000)10) the Outer House of the Court of Session held: once a local authority determines that an individual’s needs call for a particular provision the local authority is obliged to make that provision. In particular having decided that an individual requires the provision of a permanent place in a nursing home … a local authority could not ... refuse to make such a provision simply because it did not have the necessary resources. The Ombudsman in a complaint against Essex11 she stated: The Council believes it does not have to provide a care service or funding for care immediately it has decided that it is necessary to provide the service to meet a person's assessed needs. It considers that it is acting correctly by having a waiting list on which the time a person may have to wait for resources to become available is indeterminate and depends to a significant extent on the needs and priority of other people on the waiting list and those who may come on to the list. That cannot, in my view, be correct. Human and physical resource shortages In R v Islington LBC ex p Rixon (1996)12 Sedley J considered that a local authority could not assess someone as needing a service (eg a Day Centre) and then fail to provide it, merely because none was available. This reason, alone would be insufficient. He asserted: “There are two points at which, in my judgment, the respondent local authority has fallen below the requirements of the law. The first concerns the relationship of need to availability. … the local authority has, it appears, simply taken the existing unavailability of further facilities as an insuperable obstacle to any further attempt to make provision …”. Residential —v— non-residential care plans R v Southwark LBC ex p Khana and Karim (2001)13 The applicants, an elderly couple, sought judicial review of the council's decision to meet their care needs by provision of places in a residential care home. The applicants wanted, for personal and cultural reasons, to live in the community independently in a home of their own with the support of their relatives and the statutory services. The Court of Appeal held that: 9 10 11 12 13 1 CCLR 40; [1997] 2 All ER 1. 4 CCLR 188 (and also available on the Scottish Court Services’ web site). Complaint 00/B/00599 3rd September 2001. 1 CCLR 119. (2001) 4 CCLR 267 (CA). 3 www.lukeclements.com November 2010 (1) K was seeking to insist on preferences and beliefs. The council was required to consider those beliefs and preferences but the assessment of any needs in respect of the provision of accommodation ultimately remained with the council. (2) That whilst community care assessments should aim to preserve the independence of the elderly in the community for as long as possible, where the local authority concluded that those needs were best addressed in residential care it had satisfied its duties under the legislation. (3) K's refusal of the offer of accommodation was unreasonable and the council was not obliged to offer a two-bedroom flat in its place. Carers (Recognition & Services) Act 1995 The Act provides recognition for carers by requiring the social services authority (if so requested) to carry out a separate assessment of the carer at the same time as it assesses the person for whom the care is provided. The carer can be of any age (ie adult or child). In order to qualify for an assessment under the Act, a carer must satisfy the following criteria: 1. A community care assessment (or reassessment) of the person for whom he or she cares must be in the process of being carried out; 2. The carer must be providing (or intending to provide) a substantial amount of care on a regular basis. People who provide the care as a result of a contract of employment or as a volunteer placed by a voluntary organisation are excluded14. 3. The carer must request a carers assessment. The guidance however requires social workers to “inform any carer who appears eligible under this Act of their right to request an assessment15”. The Act entitles qualifying carers to an assessment of their ability to provide and continue to provide care. If as a result of such an assessment it transpires that the carer is no longer able (or willing16) to provide the same level of care, then the authority will have to decide whether to change the service user’s care plan by increasing the services provided by another agency or agencies to compensate. The Carers and Disabled Children Act 2000 The CDCA 2000 came into force in April 2001 in England and July 1st in Wales although the voucher scheme is likely to be delayed until April 2002. Section 1 : Right of carers to assessment Section 1 provides for ‘free standing carers assessments; that is a carer can be assessed even if the person for whom s/he cares refuses a community care assessment 17. The requirements being that the carer is over 15 years of age, is caring for someone aged 18 or over and the carer requests an assessment. The assessment enables the local authority to decide whether to provide services to the carer under s2. Section 2: Services for carers Section 2 enables the local authority to provide services to carers following a carer's assessment. Potentially there is little restriction upon the services that can be made available, provided the service helps ‘the carer care for the person cared for’. The explanatory notes to the Act indicated that these services may take the form of physical help, for example assistance around the house, or other forms of support such as training or counselling for the carer. Respite / short break care 14 s1(3) C(RS)A 1995 LAC (96)7 para 20. 16 Para 9.8 of the practice guidance accompanying the Act states that social workers should not “assume a willingness by the carer to continue, or continue to provide the same level of support”. 17 The government’s view being that such a provision is necessary to overcome the problem of a disabled person refusing an assessment under s47 NHSCCA 1990, and thereby denying the carer and assessment under the 1995 Act. 15 www.lukeclements.com March 2011 4 is not however a carers service. This has been explained by the Department of Health in the following way: People who care may be assessed as needing a break from their caring role. This need will be clearly recorded on their own assessment documentation. The person they care for will then be assessed for the additional support that they will need to allow their usual carer to take a break. This need will be recorded on their assessment documentation. The additional service remains a community care service delivered to the cared for person, not a carer service under the [2000] Act. The Carers (Equal Opportunities) Act 2004 Section 1 places an obligation on social services authorities to inform carers of the rights to be assessed under the Carers (Recognition and Services) Act 1995 and the Carers and Disabled Children Act 2000. Section 2 requires that in any assessment undertaken under the Carers (Recognition and Services) Act 1995 or the Carers and Disabled Children Act 2000 that consideration be given as to whether the carer: (i) works or wishes to work; (ii) is undertaking, or wishes to undertake, education, training or any leisure activity. Direct Payments The power to provide direct payments is governed by the Health and Social Care Act 2001 ss57 – 58. Regulations in England18 and Wales19 have been issued (the ‘regulations’) which provide that individuals can insist upon a direct payment in certain situations. The central criteria being: the person consents to the making of a direct payment (or in England a suitable third part receives them on behalf of a person who lacks capacity to consent to the payment); that payments can only be made to persons who appear to be capable of managing a direct payment alone or with ‘such assistance as may be available to him’; the person is entitled to services under the community care legislation or the Carers & Disabled Children Act 2000 (CDCA 2000) or (in the case of a parent of a child in need) the Children Act 1989 (CA 1989); the person is not a proscribed person (effectively someone who is subject to certain court or tribunal orders); the local authority is satisfied that the person’s needs for the relevant service can be met by securing the provision of it by means of a direct payment (or in the case of a child in need — that his/her welfare will be safeguarded and promoted by securing it by the provision of it by means of the direct payment); In addition to the regulations, detailed practice guidance has been issued by the Department of Health20 and policy guidance by the Welsh Assembly21. Budgeting impediments The Department of Health22 and the Assembly are eager to increase the numbers of service users taking up direct payments and to ensure that internal authority budgeting arrangements are not used to stifle schemes: as the guidance states23: The Community Care, Services for Carers and Children’s Services (Direct Payments) (England) Regulations 2009 SI 200 No. 1887. 19 Community Care, Services for Carers and Children’s Services (Direct Payments) (Wales) Regulations 2004 SI No 1748 (W.185). 20 Guidance on direct payments for community care, services for carers and children’s services England 2009. 21 Direct Payments Guidance Community Care, Services for Carers and Children's Services (Direct Payments) Guidance Wales 2004. 22 In England the numbers of direct payment arrangements in any particular authority has been included as a ‘high level performance indicator’ in the PSS Performance Assessment Framework Assessment Framework - see para 18 5 www.lukeclements.com November 2010 Problems with internal budget management procedures may not be used by authorities as a reason to refuse or delay the offering or start of a direct payment to a person to whom there is a duty to make a direct payment. Additional requirements (in addition to those cited above) include: 1. The exclusion of certain service users; 2. The exclusion of certain service providers; 3. The exclusion of certain services; 4. The amount of the payment; 5. The obligations upon the recipient of direct payments. Relevant extracts from the guidance include: Support Services 33. When discussing direct payments with people, councils should consider, wherever possible, putting them in touch with a support group or ULO such as a local centre for independent living, or a peer support group of people who already receive direct payments. In addition, people who are funding their own care and support are also likely to benefit from support services offering information and advice. 35. The experience of existing recipients of direct payments is that they find it easier to seek advice from someone who is independent of their local council. People with personal experience of receiving direct payments, either to arrange their own support or on behalf of another person, can often be very effective advocates or mentors for people opting to receive direct payments for the first time. They can offer a valuable source of emotional support, understanding and advice, and act as positive role models to others. Parents of disabled children often have informal networks with other parents of disabled children. Strengthening such local schemes and networks and using the Core Offer could be an effective way of providing information, advice and support to parents and could help aid the rapid expansion of the direct payment scheme. Consent (para 15) A person does not have to accept direct payments; if they wish, they can choose instead to receive services that are provided or arranged by the council. In this respect, the individual is still exercising choice over how their support is delivered. Individuals eligible for care and support should not be unfairly influenced in their choices one way or the other Ability to manage (para 48 & 49) Councils should not make blanket assumptions that whole groups of people will or will not be capable of managing direct payments. A council cannot make direct payments if it cannot be satisfied that the potential beneficiary is capable of managing the payments, by themselves or with available assistance. However, very many people will be able to do so, particularly if they have access to help and support.’24 In England, Health & Social Care Act 2008 s146 enables local authorities to make direct payments where the disabled person lacks capacity. The regulations25 permit such payments to be made in various situations, including: 1. if the person does not have a Court of Protection appointed ‘deputy’ or Lasting Power of Attorney (LPA), the authority will have discretion to decide whether a third party is suitable to be a recipient of direct payments. 2. However if the person does have a deputy or LPA then the arrangement will depend upon whether the LPA or deputy has authority to make ‘decisions about securing the provision of a community care service’ (known as a ‘surrogate’): if they have this power they can veto the making of a direct payment; but failing this the local authority, if it wishes to make a direct payment, must give the LPA or deputy first refusal on being the recipient of the payment. 10 of the English 2003 guidance and Section III of the 2002/2003 Framework at http://www.doh.gov.uk/scg/pssperform/module4.pdf. 23 Para 23 of the (now) superseded 2003 English Guidance and para 25 of the Welsh. 24 Para 69 of the English Guidance and para 50 of the Welsh. 25 The Community Care, Services for Carers and Children’s Services (Direct Payments) (England) Regulations 2009 www.lukeclements.com March 2011 6 The amount 111. It is up to the council to decide on the amount of direct payments. However, the direct payments legislation provides that it must be equivalent to the council’s estimate of the reasonable cost of securing the provision of the service concerned, subject to any contribution from the recipient. This means that the direct payments should be sufficient to enable the recipient lawfully to secure a service of a standard that the council considers is reasonable to fulfil the needs for the service to which the payments relate. There is no limit on the maximum or minimum amount of direct payment either in the amount of care it is intended to purchase or on the value of the direct payment. 114. In estimating the reasonable cost of securing the support required, councils should include associated costs that are necessarily incurred in securing provision, without which the service could not be provided or could not lawfully be provided. The particular costs involved will vary depending on the way in which the service is secured, but such costs might include recruitment costs, National Insurance, statutory holiday pay, sick pay, maternity pay, employers’ liability insurance, public liability insurance and VAT. Some councils have found it helpful to include a one-off start-up fund within the direct payments to meet these costs as well as other forms of support that might be required, such as brokerage, payroll services and Criminal Records Bureau checks on employees. Charging Direct payments must be calculated on the basis of the ‘reasonable cost of securing the cost of the service concerned’ albeit that the legislation permits them to be paid gross or net of any charge the local authority deems it is reasonably practicable for the service user to pay. 26 Close relatives (paras 197) is satisfied that it is necessary to satisfactorily meet the person’s needs, direct payments may not be used to secure services from the spouse, civil partner or partner of a person lacking capacity. Neither can they be used to secure services from a close relative, spouse or partner of a close relative of the person lacking capacity who is currently living in the same household as the person lacking capacity. There may be occasions when the council decides that it is necessary for the suitable person to use the direct payments to secure services from a member of the family of the person lacking capacity. However, such situations are likely to be exceptional and the council should be satisfied at all times that arrangements are made in the best interests of the person lacking capacity. Health and Safety (para 132) ... As a general principle, councils should avoid laying down health and safety policies for individual direct payment recipients. Individuals should accept that they have a responsibility for their own health and safety, including the assessment and management of risk. They should be encouraged to develop strategies on lifting and handling and other tasks, both in the home and outside it where lifting equipment, for example, may not be available. Direct Payments & the NHS R (Harrison) v Secretary of State for Health and others (2009)27 relying heavily on statutory construction the High Court held that there was no power in the NHS Acts to make direct payments (notwithstanding that there was nothing in the Acts to say they could not be made). A second application is now pending in the same case, as to whether the NHS can make indirect payments – ie by transferring funds to social services via s256 NHS Act 2006 (s194 NHS (Wales) Act 2006). This issue is equally complex – but a positive outcome would appear more promising – see paras 14.109 – 14.119 Clements, L & Thompson, P Community Care & the Law 4th edition (Legal Action Group, 2007). Health Act 2009 In January 2009 the Department of Health published its proposals Personal health budgets: first steps which referred to the forthcoming Health Act (see below) and suggested that the new powers would be piloted for 3 years. 26 27 HSCA 2001 s57(4) & (5) and reg 9 of the English Regulations and reg 6 of the Welsh. [2009] EWHC 574 (Admin) 23rd March 2009. 7 www.lukeclements.com November 2010 Section 12A of the NHS Act 200628 empowers PCTs to make direct payments to patients along similar lines to those paid by social services. In June 2010 the Government in England announced that this power would be piloted in 8 regions, with 7 having power to make direct payments and / or children in transition payments. 29 All other PCTs have the power to assist by contributing to a ‘personal budget. The Act provides for the detail of the scheme to be spelled out in regulations, which have been published and came into effect in June.30 Personalisation & individual budgets Personal budgets are not underpinned by the law. They appear however to have three basic characteristics: 1. Self assessment: the idea that an individual controls the assessment of their need for social care support. However in R (B) v. Cornwall CC (2009)31 Hickinbottom J observed that the ‘self assessment’ per se is unlawful 2. Resource allocation: a computation mechanism (generally termed a ‘resource allocation system’ (RAS)) converts the self assessment into a sum of money. The individual is informed of the value and of their entitlement to this sum – their ‘indicative amount’. 3. Service flexibility: individuals have considerable freedom to use their IBs to purchase services that they consider best meets their social care needs – sometimes referred to as ‘self directed support’ (SDS). A Direct Payment can be distinguished from a Personal Budget in that a Personal Budget need not be taken as a money payment by the individual, but is capable of being managed notionally (ie by social services or a broker) - and so, for instance, used to obtain local authority services (which in general is not a possible use of a Direct Payment) Local authority key performance indicator NI 130 requires that by April 2011 30% of all community based services should be delivered either as a direct payment or as a personal budget which has (1) an agreed support plan with clear outcomes and (2) which the disabled person or their representative can use in 'ways and at times of their choosing'. R (JL) v. Islington LBC (2009)32 is the first case that has addressed aspects of aspects of the ‘personalisation’ programme – albeit that it concerned disabled children’s services. Islington introduced a new system – which it claimed allocated services on the basis of ‘need rather than diagnosis’ and did so in a way that was ‘transparent’ and ‘equitable’ (para 13 of judgment). The authority did this by creating three bands with the top band providing for 12 hours a week. Although at the hearing the authority claimed that there was discretion in the application of these bands, the judge concluded that this in practice was not the case. The new system had the effect of reducing the applicant’s son’s care package by 50% - a decrease in respite care from 1,248 to 624 hours a year. The court considered that such a drastic reduction in provision required explicit justification (eg a ‘really marked improvement in the child’s condition or in family circumstances’) and considered that this was lacking (para 36 and para 42). In her judgment (para 39) Black J states: I find it hard to see how a system such as this one, where points are attributed to a standard list of factors, leading to banded relief with a fixed upper limit, can be sufficiently sophisticated to amount to a genuine assessment of an individual child’s needs. There will be times when, fortuitously, the needs assessed by such a system will coincide with the real needs of the family but it is difficult to have any confidence in that occurring sufficiently frequently to justify the use of eligibility criteria on their own. 28 Inserted by the Health Act 2009 s11 The areas on occasions extending to more than one PCT – the areas being Doncaster PCT, Eastern and Coastal Kent PCT, Central London (Hammersmith and Fulham PCT, Kensington and Chelsea PCT and Westminster PCT) Islington PCT, Oxford PCT and Somerset PCT 30 The National Health Service (Direct Payments) Regulations 2010 SI 1000 31 [2009] EWHC 491 (Admin) 16th March 2009, para 9. 32 [2009] EWHC 458 (Admin) 29 www.lukeclements.com March 2011 8 In R (JL) v. Islington LBC (2009)33 Black J accepted the applicant’s contention that the introduction of the new eligibility criteria scheme, may have extended the opportunity for some disabled people (those who are less disabled) but may also have curtailed it for others (the more disabled). Accordingly the local authority were required to produce evidence that it had due regard to its disability equality duty under 49A DDA 1995 and in Black J’s opinion this had not been done. Charging for residential accommodation The Choice of Accommodation Directions The Directions allow for individuals assessed as entitled to residential or nursing care home support, to choose where that care home is: anywhere in England or Wales, provided it meets the local authority’s contracting requirements (which usually means ‘cost’). They also permit third parties to ‘top-up’ the cost of more expensive accommodation (in certain situations). In R (S) v Leicester City Council (2004)34 it was held that the Choice of Accommodation Directions do not require a service user to live in the most suitable accommodation that is available to her. So long as the service user’s preferred accommodation is suitable to meet her needs, it should not matter that another residential placement would provide a better range of services – and a residential placement is not unsuitable merely because it is located some distance from the funding authority The Treatment of income The personal allowance is (as of April 2010 – March 2011) £22.30 (£22.50 in Wales). The Charging for Residential Accommodation Guide (CRAG) reminds local authorities that the Personal Expense Allowance must not be spent on aspects of care which have been assessed as necessary to meet the individual’s needs by the council and the NHS. Capital limits The limits from April 2010 are as follows (with the Welsh limits in brackets) Lower limit £14,250 (£22,000) Upper limit £23,250 (£22,000) Non-accommodation services Social services authorities have a discretionary power to charge for certain non-accommodation services. In relation to adult services this power derives from s17 Health and Social Services and Social Security Adjudications Act 1983. Section 17 enables local authorities to make reasonable charges for non-residential services, but also to have procedures for reducing or waiving the charge where it is not ‘reasonably practicable’ for the user to pay the full charge. Policy guidance ‘Fairer Charging Policies for Home Care and other non-residential Social Services’ has been issued by the department of health [LAC (2001)32] and the Welsh Assembly in 2007: in England practice guidance was issued in August 2002. The guidance requires that: service user’s net incomes should not be reduced below basic income support levels or the guarantee credit of pension credit, plus a buffer of 25 per cent; ‘basic levels’ of income support includes the personal allowance and all premiums, but it ‘need not include the Severe Disability Premium’ (para 18).35 The latest Welsh guidance gives a buffer of ‘no less than’ 35 per cent 33 [2009] EWHC 458 (Admin) [2004] EWHC 533 (Admin) Leveson J – presently only published on Lawtel. 35 Because the buffer is based on benefits which are paid at different rates according to age, it leads to large differences between what younger disabled people and older people are able to keep. A few authorities try to avoid this potential age discrimination by using the more generous pension credit rates for younger people. 34 9 www.lukeclements.com November 2010 where disability benefits are taken into account as income in assessing ability to pay a charge, councils should assess the individual user’s disability-related expenditure; councils should specifically consult on the need to assess disability-related expenditure for other users. It is not acceptable to make a charge on disability benefits without assessing the reasonableness of doing so for each user. As a minimum, the same savings limits as for residential care charges should be applied. Councils are free to operate more generous rules, as with other parts of the guidance. ‘To ensure that disabled people and their carers, who wish to do so, are able to enter and progress in work’, the guidance requires earnings to be disregarded in charge assessments. In relation to the assessment of charges, local authorities cannot simply put the onus on the disabled person or the carers to establish a particular fact (for existence the legitimacy of disability related expenditure). In R (B) Cornwall CC (2009)36 in Hickinbottom J’s opinion an authority ‘cannot avoid its obligation to assess needs etc by failing to make an appropriate assessment themselves, in favour of simply requiring the service user himself to provide evidence of his needs’. In the judges view the 2003 Fairer Charging Guidance required that an authority ‘engages with, and tries to agree with a service user and his carers, both the steps that the authority will take in relation to identified eligible needs and also in the assessment of charging for those steps’ (para 56). The case concerned a decision by the council to reject (without discussion with the disabled person and his carers) expenditure on an annual holiday, on carers expenses, on cleaning, swimming, alternative therapies etc. – all of which the Judge considered to be capable of being classified as disability related expenditure (para 66). In R v Coventry City Council ex p Carton (2000)37 the Administrative Court held: 1. Before fundamental changes can be made to a charging structure, there must be proper consultation with users; and 2. It was irrational, unlawful and unfair for the council to apply a charging policy which treated as income available for day care sums of DLA paid in respect of night care. The Ombudsman has held that it is maladministration for an authority to adopt a charging policy which only permits exceptions if users provide ‘proof of hardship’38; where a claimant produces evidence that expenditure exceeds income, then if the local authority persists in seeking the full charge, it is obliged to provide cogent reasons why it considers that the user is able to pay the amount claimed39. it is maladministration to allow a person to terminate their care services due to an inability to pay for them, without advising that social services cannot withdraw services for nonpayment40. Further on line resources Disabled Children: A Legal handbook (2010) A 500 page Guide to all aspects of the law at www.ncb.org.uk/cdc/resources/legal_handbook.aspx Carers & their Rights A 90 page Guide to the rights of carers http://www.carersnet.org.uk/acts/acts.html 36 37 38 39 40 [2009] EWHC 491 (Admin) 16th March 2009 para 68. 4 CCLR 41 Complaints 99/C/02509 & 02624 against Gateshead. Complaints 99/C/02509 & 02624 against Gateshead. Complaint against Durham 99/C/1983; 9th October 2000. www.lukeclements.com March 2011 10 A 25 page Guide to the social security rights of carers http://www.carersuk.org/Newsandcampaigns/CarersRightsDay/FreeCarersRightsGuide Legal rights and challenging the cuts www.ncb.org.uk/cdc/resources/cemented_to_the_floor_by_law.aspx 11 www.lukeclements.com November 2010