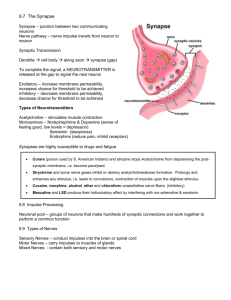
short revew of history of neurology
advertisement

LECTURE I SHORT REVEW OF HISTORY OF NEUROLOGY …it is true that those who ignore the lessons of history are likely to repeat the mistakes of earlier generations. Neurology is a science about the development and functioning of the nervous system in norm and pathology. The problem of research of the brain of the person, the problem of the ratio between the brain and mentality is one of the most important tasks which were considered by the science. The modern neurology (neuropathology) as an independent science has been established in the second half of the 19th century and it is a result of thousand-year work of many talented observers of antiquity; namely doctors, biologists, physiologists, morphologists, who studied the role of the nervous system in normal and unhealthy conditions of an organism. An ancient Egyptian treatise concerning trauma surgery, the Edwin Smith papyrus, contains descriptions and suggests treatments for various injuries, including some of neurological nature. They describe the meninges, the external surface of the brain, the cerebrospinal fluid and the intracranial pulsations. The Sumerians illustrated paraplegia caused by physical trauma. In the Ayurvedic text Charaka Samhita (ancient India) discusses epilepsy and its symptoms and of possible treatments. Slightly later, the ancient Greek physician Hippocrates was convinced that epilepsy has a natural cause, not a sacred one. The ancient Greeks also dissected the nervous system. For example, Aristotle (although he misunderstood the function of the brain) describes the meninges and also distinguishes between the cerebrum and the cerebellum. More lately, in Rome, Galen performed many dissections of the nervous system in a variety of species, including the ape. One particular discovery he made was of the importance of the recurrent laryngeal nerves. Originally, he cut through them accidentally while performing an experiment Neuropathology (neurology) as an independent clinical science appeared in 1862 when the department for patients with diseases of the nervous system in hospital Salpetrier near Paris was opened. Jean-Martin Sharko (1835-1893) whom we quite often we name the father of neuropathology headed it. The first Kiev Department of neurology was founded in 1884 by M.M. Lapinsky (B.M. Mankovsky, D.I. Panchenko their mantle had fallen). The first Kharkiv Department of neurology was founded in 1884 by P.I. Kovalevsky (S.M. Davidenkov, K.I. Platonov, O.M. Grinshtein, G.D. Leshchenko their mantle had fallen). In 1922 the Ukrainian Research Institute of psychiatry and neurology was founded in Kharkiv by G.I. Geimanovitch. In 1926 the Ukrainian Institute of Clinical Psychiatry was founded by V.P. Protopopov. Now its headed professor P.V. Voloshin. The first Russian neurologic department was opened in 1869, on the base of Catherine’s hospital. The initiator of its creation and its first head was A.J. Kozhevnikov (1836-1902). Under his initiative the first clinic of nervous diseases was constructed in Russia in 1890. Kozhevnikov is the founder of the Moscow school of neuropathologists, which was represented by the famous scientists such as L.O. Darshkevitsh, G.I. Rossolimo, S.S. Korsakov and other. In St. Petersburg neurological science began to develop on the basis of the Department of mental diseases of Medical-surgical academy created in 1857 (since 1881- Military Medical Academy). From the end of the 80s of the 19th century the course of nervous diseases at this chair was given by Merezhkovskiy (1838-1908). In 1932 surgeon N.N.Burdenko together with neurologist V.V.Kramer created in Moscow independent institute of neurosurgery where such scientists as Irger, Arutjunov and also representative of new fields in neurology such as neurophthalmology, otorhinoneurology, neuroradiology. In 1944 in Moscow the research institute of neurology was founded. The new stage of the development of neurology was opened by Marushi. He has described the reaction of the activation of the brainstem through the implanted electrodes. Academician Anochin described the theory of functional system. 3 The newest period, since the 60s-70s years of the 20th century. The ultra structure of synapses was discovered, the theory of ligand-synaptic communications was specified. In peripheral nervous system albuminous or axonal transport was found. SOME SIGNIFICANT DATES ABOUT NEUROLOGY 2700 B.C. - Shen Nung originates acupuncture. 1700 B.C. - Edwin Smith surgical papyrus written. First written record about the nervous system. 460-379 B.C. - Hippocrates discusses epilepsy as a disturbance of the brain. 460-379 B.C. Hippocrates states that the brain is involved with sensation and is the seat of intelligence. 387 B.C. - Plato teaches at Athens. Believes brain is seat of mental process. 335 B.C. - Aristotle writes about sleep; believes heart is seat of mental process 1000 - Al-Zahrawi (also known as Abulcasis or Albucasis) describes several surgical treatments for neurological disorders. 1025 - Avicenna writes about vision and the eye in The Canon of Medicine. 1500 - 1600 1504 - Leonardo da Vinci produces wax cast of human ventricles. 1536 - Nicolo Massa describes the cerebrospinal fluid. 1538 - Andreas Vesalius publishes Tabulae Anatomicae. 1550 - Vesalius describes hydrocephalus. 1600 - 1700 1641 - Franciscus de la Boe Sylvius describes fissure on the lateral surface of the brain (Sylvian fissure). 1649 - Rene Descartes describes pineal as control center of body and mind. 1650 - Franciscus de la Boe Sylvius describes a narrow passage between the third and fourth ventricles (the aqueduct of Sylvius). 1658 - Johann Wepfer theorizes that a broken brain blood vessel may cause apoplexy (stroke) 1661 - Thomas Willis describes a case of meningitis. 1662 - Rene Descartes De homine is published. 1686 - Thomas Sydenham describes a form of chorea in children and young adults. 1700 - 1800 1705 - Antonio Pacchioni describes arachnoid granulations. 1709 - Domenico Mistichelli describes pyramidal decussation. 1717 - Antony van Leeuwenhoek describes nerve fiber in cross section. 1764 - Domenico F.A. Cotugno describes spinal subarachnoid cerebrospinal fluid; shows that ventricular and spinal fluids are connected. 1764 - The interventricular foramen (Foramen of Monroe) is named after Alexander Monroe; it was described earlier by Vieussens. 1773 - John Fothergill describes trigeminal neuralgia (tic douloureux, Fothergill's syndrome). 4 1778 - Samuel Thomas von Soemmerring presents the modern classification of the twelve cranial nerves. 1798 - John Dalton, who was red-green colorblind, provides a scientific description of color blindness 1800 - 1850 1805 - Felix Vicq d'Azyr discovers the red nucleus. 1809 - Luigi Rolando uses galvanic current to stimulate cortex. 1811 - Julien Jean Legallois discovers respiratory center in medulla. 1811 - Charles Bell discusses functional differences between dorsal and ventral roots of the spinal cord. 1817 - James Parkinson publishes An Essay on the Shaking Palsy. 1824 - F. Magendie provides first evidence of cerebellum role in equilibration. 1825 - Robert B. Todd discusses the role of the cerebral cortex in mentation, corpus striatum in movement and midbrain in emotion. 1825 - Luigi Rolando describes the sulcus that separates the precentral and postcentral gyri. 1836 - Charles Dickens (the novelist) describes obstructive sleep apnea. 1839 - Theordor Schwann proposes the cell theory. 1850 - 1900 1850 - Augustus Waller describes appearance of degenerating nerve fibers. A. Kolliker describes how motor nerves originate from the neurons in the anterior horn of the spinal cord. 1854 - Louis P. Gratiolet describes convolutions of the cerebral cortex. 1855 - Richard Heschl describes the transverse gyri in the temporal lobe (Heschl's gyri). 1859 - Rudolph Virchow coins the term neuroglia. 1862 - William Withey Gull describes clinical signs of syringomyelia. 1863 - Ivan Mikhalovich Sechenov publishes Reflexes of the Brain. 1863 - Nikolaus Friedreich describes a progressive hereditary degenerative CNS disorder (Friedreich's ataxia). 1865 - Otto Friedrich Karl Deiters differentiates dendrites and axons. 1869 - Johann Friedrich Horner describes eye disorder (small pupil, droopy eyelid) later to be called "Horner's syndrome". 1872 - George Huntington describes symptoms of a hereditary chorea. 1874 - Jean Martin Charcot describes amyotrophic lateral sclerosis. 1874 - Vladimir Alekseyevich Betz publishes work on giant pyramidal cells. 1875 - Richard Caton is first to record electrical activity from the brain. 1887 - Sergei Korsakoff describes symptoms characteristic in alcoholics. 1889 - Sir Victor Horsley publishes somatotopic map of monkey motor cortex. 1891 - Heinrich Quinke develops the lumbar puncture (spinal tap). 5 1896 - Joseph Babinski describes the Babinski Sign. 1897 - Ivan Petrovich Pavlov publishes work on physiology of digestion. .1898 - John Newport Langley coins the term autonomic nervous system 1900 - 1950 1900 - Sigmund Freud publishes The Interpretation of Dreams. 1902 - Julius Bernstein proposes membrane theory for cells. 1903 - Ivan Pavlov coins the term conditioned reflex. 1906 - Alois Alzheimer describes presenile degeneration. 1908 - Vladimir Bekhterew describes the superior nucleus of the vestibular nerve (Bekhterew's nucleus). 1909 - Korbinian Brodmann describes 52 discrete cortical areas. 1913 - Edwin Ellen Goldmann finds blood brain barrier impermeable to large molecules. 1914 - Robert Barany-Nobel Prize-Vestibular apparatus. 1914 - Henry H. Dale isolates acetylcholine. 1916 - George Guillain, Jean Alexander Barre and Andre Strohl describe an acute inflammatory demyelinating polyneuropathy (Guillain-Barre Syndrome). 1918 - Walter E. Dandy introduces the ventriculography. 1919 - Walter E. Dandy introduces the air encephalography. 1932 - Jan Friedrich Tonnies develops multichannel ink-writing EEG machine. 1932 - Edgar Douglas Adrian and Charles S. Sherrington share Nobel Prize for work on the function of neurons. 1936 - Henry Hallett Dale and Otto Loewi share Nobel Prize for work on the chemical transmission between nerves. 1944 - Joseph Erlanger and Herbert Spencer Gasser share Nobel Prize for work on the functions of single nerve fiber 1950 - present 1950 - Eugene Roberts and J. Awapara independently identify GABA in the brain. 1956 - L. Leksell uses ultrasound to examine the brain. 1960 - Oleh Hornykiewicz shows that brain dopamine is lower than normal in Parkinson's disease patients. 1961 - Levadopa successfully treats parkinsonism. 1968 - Alexander Romanovich Luria publishes The Mind of a Mnemonist; A Little Book About a Vast Memory. 1970 - Julius Axelrod, Bernard Katz and Ulf Svante von Euler share Nobel Prize for work on neurotransmitters. 1972 - Godfrey N. Hounsfield develops x-ray computed tomography. 1974 - M.E.Phelps, E.J.Hoffman and M.M.Ter Pogossian develop first PET scanner. 6 1977 - Roger Guillemin and Andrew Victor Schally share Nobel Prize for work on peptides in the brain. 1981 - Roger Wolcott Sperry awarded Nobel Prize-functions brain hemispheres. 1982 - Bengt Ingemar Bergstrom, John Robert Vane and Sune K. Bergstrom awarded Nobel Prize for the discovery of prostaglandins. 1986 - Stanley Cohen and Rita Levi-Montalcini awarded Nobel Prize for their work on the control of nerve cell growth 1991 - Erwin Neher and Bert Sakmann share the Nobel Prize for their work on the function of single ion channels. 1997 - Stanley B. Prusiner awarded the Nobel Prize for the discovery of prions; a new biological principle of infection. 2000 - Arvid Carlsson, Paul Greengard and Eric Kandel share the Nobel Prize for their discoveries concerning signal transduction in the nervous system. The elements of the NS of the person develop from embryonal ectoderm (neurons and neuralgia) and mesoderm (meninges, vessels, mesoglia). By the end of the 3rd week of the development human embryo from ectoderm the neural plate, which is located longitudinal on the back side of embryo, is formed. On the neural plate appears a neural groove which turns to the neural tube then. In the generated neural tube distinguish three layers: the inner ependymal layer; the middle layer of the mantle and the outer layer. The cells of the inner layer turn into glia cells, the cells of the mantle layer give neuroblasts, which turn to mature nervous cells and spongioblasts, giving rise to various kinds of neuroglia (astrocyte, oligodendrocyte). The nervous system develops from the (initially) longitudinally oriented neural tube, which consists of a solid wall and a central fluid-filled cavity. The cranial portion of the neural tube grows more extensively than the rest to form three distinct brain vesicles, the rhombencephalon (hindbrain), the mesencephalon (midbrain), and the prosencephalon (forebrain). The nervous system is composed of cells, called neurons that are specialized for information processing and transmission. Neurons make contact with each other at junctions called synapses, at which information is transferred from one neuron to the next by means of chemical messenger substances called neurotransmitters. In general, neurons can be divided into two classes: excitatory and inhibitory. The structure of neurons is various. There are numerous classifications of nervous cells based on the form of their body, extent and the form of dendrite and other features. On functional value these cells are subdivided into motor, sensory and interneuron. A nervous cell carries out two basic functions: 1) specific – processing the information coming to the neuron and transferring of a nerve impulse; 2) biosynthetic, directed on the maintenance of the ability to live. It is reflected in the ultra structure of the nervous cell. The structure of a nervous cell includes: mitochondrion, determining its energy metabolism; nucleus, nucleolus, granular and not granular endoplasmic reticulum, Golgi complex, polysomes and ribosomes, basically providing synthesis of protein; lysosomes and phagosomes (the basic organelles of «endocellular digestive system»); axons, dendrites, synapses, providing morphofunctional connection of separate cells. The polymorphism of the cell structure is due to the various role of separate neurons in system activity of the brain as a whole. The axons are exposed to myelinization and in such a way myelinated nerve fibers are formed. The fascicles of nerve fibers which can include separate non-myelinated fibers form the white substance of the brain, the cranial and peripheral nerves. The dendrites and the processes of glia cells forms complex and unique pictures of the neuropile. However it is the allocation of the axons and the dendrites, their interposition, afferent-efferent interrelation and the regularity of architectonics of the synapses that are determining in mechanisms of the integral function of the brain. 7 The synapses are divided into axosomatic, axoaxonic and axodendritic synapses; dendrodendritic synapses are observed less often. In the synapses they distinguish presynaptic part, which contains the vesicles and postsynaptic part. The active zone of synaptic contact where the release of mediator and nerve impulse transmission take place is characterized by the increase of the electronic density of presynaptic and postsynaptic membranes. Different systems of interneuronic connections use various mediators. It is the essential moment in the synaptic transmission. Now about 30 chemically active substances (acetylcholine, dopamine, noradrenaline, serotonin, GABA (gamma aminobutyric acid) and etc.), which take part in synaptic transmission from one cell to another are known. Recently numerous neuropeptides such as enkephalins, endorphines and P-substance are actively studied as mediator in synaptic transmission. The reflex principle of the work of the NS underlies the functioning of the motor system of the person. The complex of nervous mechanisms takes part in the realization of motor reflex activity: peripheral motor neuron (the cells of anterior horns of the spinal cord and nuclei of the cranial nerves), central motor neuron - or the pyramidal tract, and also numerous structures of the brainstem and the extrapyramidal system, which provide the automatism of stereotyped movements, smooth regulation of muscular tone, the realization of consensual movements. All these movements give to the motor activity of a person individual character. The cerebellum with its system of afferent and efferent tracts plays an important role in the development of automatic coordination of movements, the maintenance of equilibrium of a body. Thus motor activity is the result of integral activity of the NS. They distinguish voluntary movement which is realized with the help of the cerebral cortex, and involuntary, which is constructed as simple and complex reflex acts. Voluntary movements are controlled by the pyramidal tract, involuntary – the extrapyramidal system, the reticular formation and the segmental apparatus of the spinal cord. Central Nervous System (CNS) The forebrain or prosencephalon (supratentorial portion of the brain) comprises the telencephalon (the two cerebral hemispheres and the midline structures connecting them) and the diencephalon. The midbrain or mesencephalon lies between the fore brain and the hind brain. It passes through the tentorium cerebelli. The hindbrain or rhombencephalon (infratentorial portion of the brain) comprises the pons, the medulla oblongata (almost always called “medulla” for short), and the cerebellum. The mid brain, pons, and medulla together make up the brain stem. Spinal Сord The spinal cord is approximately 45 cm long in adults. Its upper end is continuous with the medulla; the transition is defined to occur just above the level of exit of the first pair of cervical nerves. Its tapering lower end, the conus medullaris, terminates at the level of the L3 vertebra in neonates, and at the level of the L1–2 intervertebral disk in adults. Thus, lumbar puncture should always be performed at or below L3–4. The conus medullaris is continuous at its lower end with the threadlike filum terminale, composed mainly of glial and connective tissue, which, in turn, runs through the lumbar sac amidst the dorsal and ventral roots of the spinal nerves, collectively called the cauda equine (“horse’s tail”), and then attaches to the dorsal surface of the coccyx. The cervical, thoracic, lumbar, and sacral portions of the spinal cord are defined according to the segmental division of the vertebral column and spinal nerves. Peripheral Nervous System (PNS) The peripheral nervous system connects the central nervous system with the rest of the body. All motor, sensory and autonomic nerve cells and fibers outside the CNS are generally considered part of the PNS. Specifically, the PNS comprises the ventral (motor) nerve roots, dorsal (sensory) nerve roots, spinal ganglia, and spinal and peripheral nerves, and their endings, as well as a major portion of the autonomic nervous system (sympathetic trunk). Peripheral nerves may be purely motor or sensory but are usually mixed, containing variable fractions of motor, sensory, and autonomic nerve 8 fibers (axons). A peripheral nerve is made up of multiple bundles of axons, called fascicles, each of which is covered by a connective tissue sheath (perineurium). The connective tissue lying between axons within a fascicle is called endoneurium, and that between fascicles is called epineurium. Fascicles contain myelinated and unmyelinated axons, endoneurium, and capillaries. Individual axons are surrounded by supportive cells called Schwann cells. Tight winding of the Schwann cell membrane around the axon produces the myelin sheath that covers myelinated axons. The Schwann cells of a myelinated axon are spaced a small distance from one another; the intervals between them are called nodes of Ranvier. The nerve conduction velocity increases with the thickness of the myelin sheath. Autonomic Nervous System (ANS) The autonomic nervous system regulates the function of the internal organs in response to the changing internal and external environment. ANS realize its functions independently of consciousness. It consists in two major parts: the sympathetic and parasympathetic systems. According to the anatomy it divides into central part, which include segmental level (limbic system, hypothalamus, reticular formation) and segmental level and peripheral part (all the other structures). 9 LECTURE II THE PHYSIOLOGY AND PATHOLOGY OF MOTOR FUNCTION PART I Fig.2.1. Basic motor pathway ( from http://www.humanneurophysiology.com) All movements are effected by contractions of striated muscles through the control of the nervous system. Thus motor activity is the result of integral activity of the nervous system. They distinguish voluntary movement which is realized with the help of the cerebral cortex, and involuntary, which is constructed as simple and complex reflex acts. Voluntary movements are controlled by the pyramidal tract, involuntary – the extrapyramidal system, the reticular formation and the segmental apparatus of the spinal cord. By means of our motor system we move our bodies in space. The motor system controls the timing, direction, amplitude, and force of movement. The examination of motor functions includes the determination of muscle power, an evaluation of muscle tone and muscle bulk and the observation of abnormalities of movement. 10 The motor impulses for voluntary movement are mainly generated in the precentral gyrus of the frontal lobe (first motor neuron). They pass in the long fiber pathways (mainly the corticonuclear and corticospinal tracts (pyramidal pathway) through the brainstem and down the spinal cord to the anterior horn, where they make synaptic contact with the second motor neuron—usually by way of one or more intervening interneurons. Pyramidal system The pyramidal system appears only at mammals (at the elephant – 4,8 %, at the primates - 20,1 %, at the person - 30 %). Pyramidal system is consisting in two neurons - central (the first) and peripheral (the second) ones. The pyramidal tract (the one forming a pair) basically begins from Betz (large pyramidal) cells, in the 3rd and 5th layers of the precentral gyrus (the 4th Brodmann's area). Some part of the fibers begins from the neurons of the 1st somatosensory area (the postcentral gyrus; the 3rd, 1st, 2nd Brodmann's areas); the part - from the neurons of superior and middle frontal gyri (the 6th and the 8th areas). In the precentral gyrus there is a determined somatotopical distribution of the central motoneurons (homunculus). The motoneurons are located both on convex, and on the internal surface of hemispheres (Fig.2.2). In the brain stem, the pyramidal tract gives off fibers to the motor nuclei of the cranial nerves (corticopontine and corticobulbar tracts). Its function is the realization of voluntary movements of muscles of face, pharynx and larynx. The corticospinal tract begins from the top and average third of the precentral gyrus and ends along the whole length of the spinal cord at the motor neurons of the anterior horns. This tract realizes voluntary movements of the muscles of the limbs and trunk. The axons of the pyramidal tract pass through the radiate crown to the anterior two thirds of the posterior limb of the internal capsule (the posterior third is occupied by sensory and cerebellar tracts; while the anterior limb of the internal capsule – by frontopontine tracts). Further the pyramidal tract passes into the basis of the mesencephalon, goes into the base of the brain and the medulla oblongata where it forms "pyramids". After that the corticonuclear tract branches off, the majority of the remaining fibers of the corticospinal tract (85 %) at the level of the great occipital foramen cross over to the other side and descend in the lateral white column of the spinal cord and end at the level of the anterior horns: for hands - at the level of the cervical intumescence, for legs -lumbosacral intumescence. About 15 % of fibers do not cross to the opposite side, providing bilateral innervation of the muscles of the trunk and the sphincters of the urinary bladder. The peripheral motor neurons are located in the anterior horns. Among them are distinguished big alpha motoneurons, (whose axons end in muscle fibers which can make fast contraction) and small α-motoneurons (whose axons end in muscle fibers, capable to support long tonic contraction). Besides in the pyramidal tract there are γ-motoneurons with thin and slow-conducting axons, which provide the innervation of the proprioceptors of the muscular spindle and provide the maintenance of the muscular tone. Among intercalary neurons of the pyramidal tract it is necessary to distinguish Renschaw cells braking the action of big alpha motoneurons. The axons of the neurons of the pyramidal tract form the anterior motor root. The distal fibers making these root, are located next to the spinal ganglion which contains the sensory cells - the first sensory neurons. The dendrites of the neurons of the spinal ganglion form the spinal nerve. The spinal nerves from several segments form the plexus. Large nerve trunks are formed from the plexus: ulnar, radial and median nerves – for a hand; femoral and sciatic nerves for a leg from which in turn peripheral nerves to separate muscles depart. The zone of the contact of the ending of the motor nerve and the muscle is called neuromuscular synapse. The acetylcholine is the mediator of synaptic transmission in it. The part of the dendrites of the nerve cells of the spinal ganglion ends in the receptors of the tendons (Golgi’s organs). They are receptors for the conduction of the impulses, braking activity of the alpha motoneurons. The axons of these sensory cells end at intercalary neurons which contact with alpha motoneurons. 11 Lesions of the first motor neuron in the brain or spinal cord usually produce spastic paresis, while lesions of the second motor neuron in the anterior horn, anterior root, peripheral nerve, or motor end plate usually produce flaccid paresis. Motor deficits rarely appear in isolation as the result of a lesion of the nervous system; they are usually accompanied by sensory, autonomic, cognitive, and/or neuropsychological deficits of various kinds, depending on the site and nature of the causative lesion. The flaccid paralysis is characterized by a loss of tone and atrophy of the involved muscles; this is called flaccidity, or hypotonicity. Denervated muscle fibers undergo spontaneous contractions, known as fibrillations or fasciculations; these are too fine and rapid to be seen with the naked eye but can be demonstrated electromyographically. No pathologic reflexes are found. The spastic paralysis is characterized by diminished muscular strength and impaired fine motor control, spastic increased tone, abnormally brisk stretch reflexes, possibly with clonus, hypoactivity or absence of exteroceptive reflexes (abdominal, plantar, and cremasteric reflexes), pathological reflexes (Babinski, Oppenheim, Gordon, and Bekhterev reflexes, preserved muscle bulk. If the anterior horn are affected it may provoke fibrillation. A lesion of the cerebral cortex, may caused by a tumor, an infarct, or a traumatic injury and brings on weakness of part of the body on the opposite side. brachiofacial weakness is frequently than elsewhere, because these parts of the body have a large cortical representation. If the internal capsule is involved (e. g., by brain stroke), there will be a contralateral spastic hemiplegia—lesions at this level affect both pyramidal and nonpyramidal fibers, because fibers of the two types are in close proximity here. The corticonuclear tract is involved as well, so that a contralateral facial palsy results, perhaps accompanied by central hypoglossal nerve palsy. No other cranial nerve deficits are seen, however, because the remaining motor cranial nerve nuclei are bilaterally innervated. The contralateral paresis is flaccid at first (in the “shock phase”) but becomes spastic within hours or days because of concomitant damage to nonpyramidal fibers. Lesions at the level of the cerebral peduncle, such as a vascular process, a hemorrhage, or a tumor, produce contralateral spastic hemiparesis, possibly accompanied by an ipsilateral oculomotor nerve palsy (Weber syndrome). Pontine lesions involving the pyramidal tract cause contralateral or possibly bilateral hemiparesis. Lesions of the pyramidal tract in the spinal cord. A pyramidal tract at a cervical level lesion causes ipsilateral spastic hemiplegia: ipsilateral because the tract has already crossed at a higher level, and spastic because it contains nonpyramidal as well as pyramidal fibers at this level. A bilateral lesion in the upper cervical spinal cord can cause quadriparesis or quadriplegia. A lesion affecting the pyramidal tract in the thoracic spinal cord (causes spastic ipsilateral monoplegia of the lower limb. Bilateral involvement causes paraplegia. (See lecture V). The lesion of anterior horn or motor nucleus of cranial nerves. It causes peripheral paralysis of certain muscles. At chronic process we can observe fasciculation of muscles. Also there are early atrophy and degenerative reaction. The lesion of anterior roots. It caused peripheral paralysis or paresis too. But we can see the clinical presentation if the several roots are damaged. The lesion of nerve plexus. The clinical presentations are peripheral paralysis, pain, sensory and autonomic disorders. The clinical presentations of peripheral nerve lesion are peripheral paralysis of the muscle, innervated by this nerve, pain, sensory and autonomic disorders. Irritation of the corticospinal system, especially stimulation of the pyramidal cortex, causes an increased motor response with involuntary movements on the opposite side of the body. This may result in jacksonian convulsive seizures. 12 THE EXAMINATION OF MOTOR FUNCTIONS The examination of motor function consist in: 1. Muscle volume and contour. The volume and contour of the muscles give information about the presence of either atrophy or hypertrophy. Muscle atrophy, or amyotrophy, may be defined as the wasting or diminution in size of a muscle part. It is usually accompanied by changes in shape or contour. Its results from disorders affecting the anterior horn cell, the nerve root, the peripheral nerve, or the muscle itself. Muscle hypertrophy is an increase in the bulk, or volume, of muscle tissues. It may be the result of excessive use of the muscles, or it may occur on a pathologic basis. Muscle volume and contour are examined and atrophy or hypertrophy by inspection, palpation, and measurement. By means of inspection the general muscular development of the size of the muscles are noted, and special attention is paid to abnormalities in volume and contour and to evidence of atrophy and hypertrophy. Symmetric parts of the two sides of the body should be compared. The muscle masses should also be carefully palpated, and their volume, contour, and consistency noted. To determine the degree of atrophy or hypertrophy, measurements may be essential. The appraisal of muscle bulk and contour should be correlated with the other items of the motor examination, especially with the evaluations of strength and tone. If muscular changes in the form of atrophy or hypertrophy are present, and if we need refine the etiology of lesion a muscle biopsy should be considered. Electromyography aids in the differential diagnosis of muscular atrophy. It helps to decide the level of lower motor neuron and its peripheral axons lesion. B. Motor strength and power. Motor strength and power indicate the capacity to exert and release force. It’s necessary to examine both the power of movement and the strength of contraction. In examining strength and power we are interested especially in voluntary, or active, motility. This is tested by having the patient carry out movements against the resistance of the examiner, and by having him resist active attempts on the part of the examiner to move fixed parts. Impairment of strength and power results in weakness, or paresis, absence of strength. Associated functions and abnormalities must be also noted. Abnormal fatigability may precede other objective manifestations of some neuromuscular disorders (such as myasthenia). There is a marked individual variation in muscle strength. The paralysis may involve one muscle, a group of muscles, certain movements, or one or more extremities. A monoplegia is the paralysis of one extremity; diplegia- is the paralysis of extremities on the two sides of the body; hemiplegia, of one half of the body; paraplegia, the legs or the lower parts of the body; quadriplegia (tetraplegia) – the paralysis of all extremities. Hemiplegia alternans affects the upper extremity on one side of the body and the lower extremity on the other side. When a muscle is maintained in a position of contraction or shortening for a period of time, a contracture may develop: the muscle cannot be stretched to normal limits without considerable pressure and the production of pain. Contractures may develop following prolonged spasm of muscles, in association with spastic paralysis. Examination of motor strength and power To test motor power, the various movements at each joint and the strength of each important muscle should be examined individually. He is instructed to either resist active attempts by the examiner to move fixed parts or to initiate and carry out movements that are resisted by the examiner. Corresponding muscles on the two sides of the body should always be compared. Both active and passive movements should be tested and if limitation of movement is accompanied by discomfort or pain, this should be noted. In the presence of coma assessment of motor function may have to depend upon the presence of spontaneous movements, the position of the extremities, asymmetries of voluntary movements on the two sides, or withdrawal of an extremity in response to painful stimulation. Hemiplegia may be diagnosed if the contraction of the facial muscles on one side is absent or and the similar extension and external rotation of the thigh and leg is present. It is usually possible to evaluate muscle strength and power sufficiently well without recourse to special instruments (e.g. dynamometer). Muscle function may be graded in various ways, but the following is an acceptable classification: 13 0. No muscular contraction occurs; 1. A flicker, or trace, of contraction occurs without actual movement, or contraction may be palpated in the absence of apparent movement; there is minimal or no motion of joints (0% - 10% of normal movement); 2. The muscle moves the part through a partial arc of movement with gravity eliminated (11% 25% of normal movement); 3. The muscle completes the whole arc of movement against gravity (26% - 50% of normal movement); 4. The muscle completes the whole arc of movement against gravity together with variable amounts of resistance (51% - 75% of normal movement); 5. The muscle completes the whole arc of movement against gravity and maximum amounts of resistance several times without signs of fatigue. This is normal muscular power (76% - 100% of normal movement). C. Examination of muscle tone Tone, or tonus, has been defined as the tension of the muscles when they are relaxed, or as their resistance to passive movement when voluntary control is absent. In testing tone, the examiner should attempt to secure the complete cooperation of the patient, who should be comfortable and relaxed. Palpation of the muscles is revealed their consistency, passive elasticity, firmness, or turgor. The most important criterion in the examination of tone is the resistance of muscles to passive manipulation when they are relaxed and when voluntary control is absent. Loss or diminution of tone is classified as hypotonicity, and pathologic increase, as hypertonicity. Hypotonicity or flaccidity results from involvement of the spinomuscular level or interference with the proprioceptive pathways, but may also be present with cerebellar lesions. It is characterized by a decrease in or loss of normal tone. The muscle is flaccid and flabby, or soft to palpation. The excursion at the joint may be normal, but is usually increased. The decrease in tone appears in the anterior horn cell damage, abnormalities of the muscle itself or of the myoneural junction. Hypertonicity is usually caused by lesions central to the anterior horn cells, or by interruption of impulses from supraspinal regions. It is seen most frequently with dysfunction of the so-called extrapyramidal and corticospinal levels, and is caused by either interruption of impulses that normally inhibit lower centers or imbalance of facilitatory and inhibitory centers, with consequent alteration of the - and -motor neuron balance or lowering of the threshold of the spinal reflexes. Spasticity. This occurs in association with lesions of the pyramidal or corticospinal level of function. There may be an elastic, springlike resistance to stretching at the beginning of movement, especially if the part is moved abruptly or suddenly, following which the muscle resists to a certain point and then suddenly relaxes – the phenomenon sometimes referred to as the clasp-knife type of resistance. Extrapyramidal rigidity occurs with lesions of the basal ganglia or of some other portion of the extrapyramidal level of motor function or its connections with the brain stem reticular formations. It phenomenon is called “cogged-wheel symptom”. Tonus is expressed in the same manner in the group of flexors and extensors. THE REFLEXES The investigation of the reflexes is often considered to be the most important part of the neurologic examination. The testing of the reflexes is the most objective procedure of the neurologic examination. Reflex activity is essential to the normal functions of the human body. All involuntary and many voluntary acts are reflex in nature. A reflex is an invariable adaptive response to the stimulation of a sense organ, which involves the use of a center of adjustment and of the conductors necessary to connect this center with the appropriate receptor and effector apparatus. By neurologycal examination mainly involuntary reflexes are investigated. An intact sensory system and an intact motor system are needed for a normal reflex response, and knowledge of both sensory and motor functions is necessary to an understanding of reflex action. The stimulus is received by the receptor, which may be a sensory ending in the skin, mucous membranes, muscle, tendon, or 14 periosteum etc. The stimulation of the receptor initiates an impulse that is carried along the afferent (sensory) nervous fibers, and then is transmitted to the CNS. There a synapse takes place with the intercalated neuron, which relays the impulse to the center of adjustment, the cell body of the efferent neuron. The neuraxis of the efferent neuron, transmits the impulse to the effector (the cell, muscle, gland, or blood vessel that then responds). A disturbance in function of any of the above parts of the reflex arc will cause a break in the reflex arc and a consequent decrease or loss of the reflex. Some hundreds of reflexes have been identified; only the more important ones will be described. The muscle stretch (proprioceptive or deep) reflexes The muscle stretch reflexes are those that are elicited in response to application of the stimulus to either tendons or periosteum, or occasionally to bones, joints, fascia, or aponeurotic structures. Because the stimulus is mediated through the deeper sense organs such as the neuromuscular and neurotendinous spindles, they may be referred to as the proprioceptive (or deep) reflexes. The proprioceptive reflexes are best tested by the use of a rubber percussion hammer. The stimulus should be quick and direct, and should be a threshold one, and no greater than necessary. The patient should be comfortable and relaxed. The part of the body to be tested should be in a position for optimal muscular response. In order to compare the reflexes on the two sides of the body, the position of the extremities should be symmetric. Reflexes may be classified as normal, absent, sluggish (diminished), and exaggerated. The response should always be compared on the two sides of the body; unequal reflexes may be as significant as either increased or diminished reflexes. The Orbicularis Oculi (blinking) Reflex. Percussion at the outer aspect of the supraorbital area and other kinds of irritation is followed by a reflex contraction of this muscle, with resulting closing of the eye. The response is usually bilateral. The afferent portion of the arc may be carried through the trigeminal nerve; the efferent impulses pass through the facial nerve, and the reflex center is in the pons. The Jaw (Masseter or Mandibular Reflex). To elicit the jaw reflex the examiner places his index finger over the middle of the patient's chin, holding the mouth slightly opened and the jaw relaxed. Then he taps his finger with the reflex hammer. The response is a contraction of the masseter and temporal muscles, causing a sudden closing of the mouth. The afferent impulses of this reflex are carried through the sensory portion of the trigeminal nerve, and the efferent impulses through its motor portion; the reflex center is in the pons. The upper extremities. The Biceps Reflex. The arm is held in a relaxed position, with the forearm midway between flexion and extension and in slight pronation. The examiner places his thumb or finger over the biceps tendon and taps the thumb with a reflex hammer. The major response is a contraction of the biceps muscle with flexion of the forearm. The sensory supply of this reflex is through the midcervical nerves, and the motor supply to the biceps is through the musculocutaneous nerve. The reflex center is at the CV-CVI segments. The Triceps Reflex is elicited by tapping the triceps tendon just above its insertion on the olecranon process of the ulna. The arm is held midway between flexion and extension, and it may be rested on the examiner's hand or on the patient's thigh. The response is one of contraction of the triceps muscle, with extension of the forearm. The sensory and motor innervations are through the radial nerve, and the center is in the lower cervical portion of the spinal cord (CVI-CVIII). The Brachioradialis (Radial Periosteal or Supinator) Reflex. If the styloid process of the radius is tapped while the forearm is in semi-flexion and semipronation, there will be flexion of the forearm, together with supination. The supination is more marked if the forearm has been extended and pronated, but there is less flexion. If the reflex is exaggerated there is associated flexion of the wrist and fingers, with adduction of the forearm. The innervation of this reflex is through the radial nerve and spinal segments CV-CVI. The lower extremities. The Patellar (Quadriceps) Reflex. The patellar, or quadriceps, reflex, usually called the knee jerk, is characterized by contraction of the quadriceps femoris muscle, with 15 resulting extension of the leg, in response to a stimulus directed toward the patellar tendon. The patellar reflex is innervated by the femoral nerve and spinal segments LII-LIV. This reflex may be elicited with the patient seated in a chair with his feet resting on the floor or with the patient lying in bed or by having the patient sit with one leg crossed over the other and tapping the patellar tendon of the superior leg. Reinforcement of the patellar reflexes may be carried out according to the method of Jendrassik: on testing reflex the patient is asked to hook the flexed fingers of the two hands together, placing the palmar surfaces of the fingers of one hand against the palmar surfaces of the other, and to attempt to pull them apart at the time the reflex is being stimulated. The Achilles (Triceps Surae) Reflex. The Achilles, or triceps surae, reflex, or the ankle jerk, is obtained by tapping the Achilles tendon just above its innervation on the posterior surface of the calcaneus. This is followed by contraction of the posterior crural muscles, the gastrocnemius, soleus, and plantaris, with resulting plantar flexion of the foot at the ankle. If the patient is seated or is lying in bed, the thigh should be moderately abducted and rotated externally, the knee should be flexed, and the foot should be in moderate inversion; the examiner should place one hand under the foot to produce moderate dorsiflexion at the ankle. If it cannot be elicited in this manner, the patient should be asked to kneel on his knees on a chair, while the feet project at right angles; the Achilles tendons are percussed while the patient is in this position. The Achilles reflex is innervated by the tibial nerve and LV and SI-SII spinal segments. The muscle stretch reflexes are increased with lesions of the corticospinal or pyramidal system. These changes are due to involvement of a variety of structures in the descending motor pathways at cortical, subcortical, midbrain and brain stem levels as well as in the spinal cord. The flexor reflexes are exaggerated to a greater degree in the upper extremities, and the extensor reflexes in the lower. The superficial (cutaneous) reflexes The superficial reflexes are those that are elicited in response to the application of a stimulus to either the skin or mucous membrane, they are sometimes known as exteroceptive reflexes. The Corneal Reflex. To elicit the corneal reflex, the examiner touches the cornea lightly with a wisp of cotton or a piece of a thin paper to avoid irritating the cornea. In response to this stimulus there is a blinking, or closing of the ipsilateral eye, the direct corneal reflex, and also a closing of the opposite eye, the consensual corneal reflex. The afferent portion of the reflex arc is mediated by the ophthalmic division of the trigeminal nerve, whereas the efferent or motor response is a function of the facial nerve. The reflex center is in the pons. The pharyngeal, or gag, reflex is elicited by applying a stimulus, such as a tongue blade or an applicator, to the posterior pharyngeal wall, tonsillar regions or even the base of the tongue. If the reflex is present, there will be elevation and constriction of the pharyngeal musculature. The afferent impulses of the reflex arc are primarily carried through the glossopharyngeal, the efferent elements primarily through the glossopharyngeal and vagus nerve. The reflex center is in the medulla. The palatal or uvular reflex is tested by stimulating the lateral and inferior surface of the uvula, or soft palate, with a tongue blade or a cotton applicator. Elevation of the soft palate and retraction of the uvula occur simultaneously. The center for this reflex is also in the medulla. Both the sensory and the motor portions of the reflex arc are carried through the vagus and glossopharyngeal nerves. The superficial abdominal reflexes. Gentle stroking of the abdomen or scratching it with a blunt object is followed by homolateral contraction of the abdominal muscles and retraction or deviation of the linea alba and umbilicus toward the area stimulated. These reflexes should be tested with the patient recumbent and the abdominal wall thoroughly relaxed. The Upper Abdominal Reflex is elicited by stimulating the skin of the upper abdominal quadrants, usually in a diagonal fashion, downward and outward from the tip of the sternum. This reflex is innervated by the intercostal nerves from ThVI-ThVIII. The Middle Abdominal Reflex. Stimulation of the skin of the abdomen at the level of the umbilicus, either by a horizontal stimulus, starting externally and proceeding medially is followed 16 by a lateral deviation of the linea alba and umbilicus. This reflex is innervated by the intercostal nerves from ThIX-ThX. The Lower Abdominal Reflex. This is elicited by stimulating the skin of the lower abdominal quadrants, either diagonally in an upward and outward direction from the region of the symphysis pubis. There is a contraction of the abdominal muscles and a diagonal deviation of the umbilicus toward the site of the stimulation. This reflex is innervated by the lower intercostal and the iliohypogastric and ilioinguinal nerves ThXI-ThXII. These reflexes may be difficult to obtain or absent in obese individuals and those with relaxed abdominal walls, and in women who have borne children. In pathology the absence of superficial abdominal reflexes is a significant finding. The Cremasteric Reflex is elicited by stroking the skin on the upper, inner aspect of the thigh, from above downward, with a blunt point, or by pricking or lightly pinching the skin in this area. The response consists of a contraction of the cremasteric muscle with homolateral elevation of the testicle. This reflex may be absent in elderly males, in individuals who have a hydrocele or varicocele, and in those who have had orchitis or epididymitis. The innervation is through ilioinguinal and genitofemoral nerves LI-LII. The Plantar Reflex. In the normal individual, stimulation of the plantar surface of the foot is followed by plantar flexion of the toes. It innervated by the LV-SII segments by means of the tibial nerve. The Superficial Anal Reflex consists of a contraction of the external sphincter in response to stroking or pricking the skin or mucous membrane in the perianal region. This reflex is innervated by the inferior hemorrhoidal nerve SIV-SV. Abnormalities of the superficial reflexes The superficial reflexes are either diminished or absent in the event of a disturbance in the continuity of the reflex arc: in the afferent nerve, motor center, or efferent nerve. The superficial reflexes, however, especially the abdominal and cremasteric reflexes, have a special significance when their absence is associated with an exaggeration of the deep reflexes (dissociation of reflexes) or when they are absent in instances where signs of corticospinal tract involvement are elicited (since the superficial reflexes have, in addition to a spinal reflex arc, a superimposed cortical pathway). CORTICOSPINAL (PYRAMIDAL) TRACT RESPONSES With disease of the corticospinal or pyramidal system, certain abnormalities are found in the reflex pattern. This is true whether the disorder is in the motor cortex itself or anywhere along the descending tracts. The superficial reflexes may be decreased or absent, and deep reflexes are exaggerated. Clonus. If the muscle tonus is markedly increased, there is also a pathologic response in the form of clonus – a series of rhythmic involuntary muscular contractions induced by the sudden passive stretching of a muscle or tendon. The most frequently are occurred ankle clonus, patellar clonus. Corticospinal tract responses in the upper extremities The corticospinal tract responses in the upper extremities are rarely occure than those found in the lower extremities. In the Rossolimo sign, flexion of the fingers and supination of the forearm follow either percussion of the palmar aspect of the metacarpophalangeal joints or tapping the volar surface of the patient's fingertips. Flexion of the fingers and hand may follow not only stimulation of the flexor tendons on the velar surface of the forearm, but also percussion of the dorsal aspect of the carpal and metacarpal areas (the Mendel-Bechterev sign). Jukovski sign caused by hammer impact on a plant on a palm under fingers; response is flexing of II-V fingers. Jackobson-Laske reflex. It’s caused by hammer impact on processus styloideus. The thumb is flexing. Corticospinal tract responses in the lower extremities The corticospinal tract responses in the lower extremities are more constant and more clearly defined than those in the upper limbs and may be elicited with more ease. They may be classified as 17 those characterized in the main by dorsiflexion of the toes, and those characterized by plantar flexion of the toes. Corticospinal Responses Characterized in the Main by Extension (Dorsiflexion) of the Toes The Babinski Sign (Fig 2.3). In disease of the corticospinal system there is an inversion of the plantar reflex, the Babinski sign or extensor plantar response. Stimulation of the plantar surface of the foot is followed by dorsiflexion of the toes, especially of the great toe, together with a separation or fanning of the toes. The Babinski sign has been called the most important sign in clinical neurology. It is considered to be one of the most significant indications of disease of the corticospinal system at any level from the motor cortex through the descending pathways. It is the most delicate, the first to be evident in the presence of disease, and the one that occurs most frequently. The Oppenheim sign is elicited by applying heavy pressure with the thumb and index finger to the anterior surface of the tibia, mainly on its medial aspect, and stroking down from the infrapatellar region to the ankle. The response is a slow one and usually occurs toward the end of stimulation. The Gordon sign is obtained by squeezing or applying deep pressure to the calf muscles. The Schaefer sign is produced by deep pressure on the Achilles tendon. Corticospinal Tract Responses Characterized by Plantar Flexion of the Toes There is a group of reflexes in which the pathologic response is one of plantar flexion of the toes. The Rossolimo sign is elicited by tapping to the tips of the toes. The Mendel – Bechterev sign is elicited by tapping or stroking the outer aspect of the dorsum of the foot in the region of the cuboid bone. Plantar flexion of the toes may also be elicited by application of the stimulus to other portions of the foot and ankle. Bechterew found that percussion of the middle of the sole or of the heel was followed by a plantar flexion response. Reflexes of spinal automatism The reflexes of spinal automatism are also termed defense reflexes. Like the corticospinal tract signs, they become manifest when the inhibiting action of the higher centers has been removed, and thus indicate, in part at least, a release from such inhibition. The Flexion Spinal Defense Reflex (or the Marie–Foix–Bechterev) sign most frequently may be evoked by an uncomfortable or nociceptive irritation. Pricking, pinching the skin on the dorsal aspect of the foot or sharp flexion of the foot may initiate the response, as may squeezing the toes or extreme passive plantar flexion of the toes or foot. Associated movements (pathologic synkinesis) Certain voluntary movements have a tendency to be accompanied by other involuntary responses called the associated, or synkinetic, movements. These are defined as automatic modifications of the attitude of certain parts of the body as a reflex response to the volitional motion of some other portion. Associated movements may be either physiological or pathological phenomenon. Pathologic associated movements are usually expressions of activity in paretic groups of muscles that are stimulated by active innervation of other groups. There may be generalized (global) associated movements, symmetric (imitative, mirror) associated movements and coordinated associated movements. Most often they can be seen in patients with hemiparesis or hemiplegia of cerebral origin. Generalized associated movements tend to produce the characteristic position of the extremities in patient with hemipareis: the upper limb is held in a position of flexion of the fingers and wrist, and the elbow, and flexion and adduction at the shoulder (the paralysis of the extensors is more marked than that of the flexors). The lower extremity is held with extension at the hip and knee and plantar flexion at the ankle and toes, and with more marked paralysis of the flexors. These characteristics are increased with exertion. Straining and attempts to grip with the paretic hand may cause an increase in the spasticity, with increased flexion of the wrist, elbow, and shoulder. Involuntary movements such as yawning, coughing, and stretching may also increase the tonus and cause the affected arm to extend at the elbow, wrist, and fingers. 18 Symmetric associated movements are usually seen in the paretic limb when the opposite healthy one is forcibly moved. Thus, in squeezing the examiner's hand with the healthy hand the paretic hand is seen to flex. Coordinated associated movements are characterized by a spread of response from one muscle or group of muscles to others. They alter the position of the part and lead to the adoption of new postures. Fig. 2.2. Somatotopical distribution of the central motoneurons (homunculus) Fig.2.3. Babinski sign (D.Purves, D. Fitzpatrick et al., 2001) 19 LECTURE II THE PHYSIOLOGY AND PATHOLOGY OF MOTOR FUNCTION PART II. CEREBELLUM. Fig.2.4. Main cerebellar connections (J.D. Fix, 1994) 20 The cerebellum is a central organ for motor control. The main functions of the cerebellum are control of balance, posture, gait, and goal-directed movement, and the regulation of muscle tone. Cerebellum lies in the fossa posterior and has got two hemispheres and the vermis. It’s connected to the brain by the three cerebellar peduncles. In superior or inferior views, the shape of the cerebellum is like a butterfly. Each hemisphere consists of 3 lobes separated by deep and distinct fissures. The cerebellum has 3 functional parts: 1. Archicerebellum (vestibulocerebellum): The central area is the vermis (“worm”). It includes the flocculonodular lobe, which is located in the medial zone. It helps maintain equilibrium and coordinate eye, head, and neck movements; it is closely connected with the vestibular nuclei. 2. Midline vermis (paleocerebellum): It’s a lateral "wings" or lobes are the cerebellar hemispheres. It helps coordinate trunk and leg movements. Vermis lesions result in abnormalities of stance and gait. 3. Lateral hemispheres (neocerebellum): They control quick and finely coordinated limb movements, predominantly of the arms. Cerebellar cortex contains three layers: The molecular layer contains stellate cells, basket cells, and the dendritic arbor of the Purkinje cells. The Purkinje cell layer is found between the molecular and granule cell layers. The granular layer is the inner layer overlying the white matter. It contains granule cells, Golgi cells, and cerebellar glomeruli. Neural Pathways 1. Afferent connections. The three large whitematter tracts (peduncles) of the cerebellum convey afferent input to the cerebellar cortex from the cerebral cortex, pontine nuclei, the brain stem nuclei of the trigeminal, vestibular, and cochlear nerves, and the spinal cord. This structure contains the major output from the cerebellum, the dentatothalamic tract, which terminates in the ventral lateral nucleus of the thalamus. It contains one major afferent pathway, the ventral superior cerebellar tract The middle cerebellar peduncle carries fibers of pontine origin The inferior cerebellar peduncle carries fibers from the vestibular nerve and nucleus to the flocculonodular lobe and fastigial nucleus, and from the contralateral inferior olive to the cerebellar hemispheres (olivocerebellar tract), as well as proprioceptive input from the posterior spinocerebellar tract and fibers from the brain stem reticular formation. 2. Efferent connections. The cerebellar nuclei (fastigial, globose, emboliform, and dentate) project via the (contralateral) superior cerebellar peduncle to the red nucleus, thalamus, and reticular formation. The thalamus projects in turn to the premotor and primary motor cortex, whose output travels down to the pons, which projects back to the cerebellum, forming a neuroanatomical circuit. Cerebellar output influences (ipsilateral) spinal motor neurons by way of the red nucleus and rubrospinal tract. The inferior cerebellar peduncle projects to the vestibular nuclei and brain stem reticular formation (completing the vestibulocerebellar feedback loop) and influences spinal motor neurons by way of the vestibulospinal and reticulospinal tracts. 3.Posterior and Anterior Spinocerebellar Tracts There are two such tracts on each side, one anterior and one posterior. Posterior spinocerebellar tract (Flechsig's). The fibers from the muscle spindles and tendon organs divide into numerous collaterals after entering the spinal cord. Some of these collateral fibers make synaptic contact directly onto the large α motor neurons of the anterior horn. Other collateral fibers arising at thoracic, lumbar, and sacral levels terminate in a column-shaped nucleus occupying the base of the posterior horn at levels C8-L2, which is named the intermediolateral cell column or thoracic nucleus, or Clarke’s column. The postsynaptic second neurons with cell bodies lying in this nucleus are the origin of the posterior spinocerebellar tract, whose fibers are among the most rapidly conducting of any in the body. The posterior spinocerebellar tract ascends the spinal cord ipsilaterally in the posterior portion of the lateral funiculus and then travels by way of the inferior cerebellar peduncle to the cerebellar vermis. The anterior (Gowers') spinocerebellar tract (tractus 21 spinocerebellaris anterior).The first neuron is common with the posterior tract. The cells of the second neurons are in the posterior horn. Their axons form the anterior spinocerebellar tract and stretch in the anterior parts of the lateral white column on their side and on the opposite side to which they cross through the white commissure. The tract ascends through the medulla oblongata and the pons - to the superior medullary velum where it again crosses to the other side. Then the fibres enter the cerebellum through its superior peduncles and terminate in the cortex of the vermis. Thus, this tract forms two decussations and proprioceptive sensibility is carried to the same side from which it had gone. Cerebellar disorders have numerous causes, including congenital malformations, hereditary ataxias, and acquired conditions. Symptoms vary with the cause but typically include ataxia (impaired muscle coordination). Main Signs of Cerebellar Disorders Disorders of the cerebellum and its inflow or outflow pathways produce deficits in the rate, range, and force of movement. Anatomically, the cerebellum has three subdivisions. The archicerebellum (vestibulocerebellum) comprises the flocculonodular lobe, helps maintain equilibrium and coordinate eyehead-neck movements, and is closely interconnected with the vestibular nuclei. The midline vermis (paleocerebellum) helps coordinate movement of the trunk and legs. Vermis lesions result in abnormalities of stance and gait. The lateral hemispheres, which make up the neocerebellum, control ballistic and finely coordinated limb movements, predominantly of the arms. Signs of cerebellar disease are listed below. Ataxia - it’s reeling, wide-based gait; decomposition of movement its inability to correctly sequence fine, coordinated acts; Static ataxia develops at vermix lesion and means standing and walking disorders. Dinamic ataxia develops at lesion of hemispheres. The patient is asked to touch the tip of his nose with the tip of his index finger slowly with his eyes open (the finger nose test). Then this is repeated with the eyes closed. To test the lower extremities the patient is asked to touch the knee by the opposite knee and slide it down the shin bone (the heel knee test) with the opened and closed eyes. Incoordination, not of sensory origin (cerebellar), is present with both the eyes open and closed. These tests recognized dinamic ataxia. The Romberg test recognizes static ataxia. Your patient stand with heels and toes together with open eyes and then with closed eyes. The tendency unstable position with the eyes close provides a positive Romberg probe. Other tests: the patient is asked to touch his index finger to the examiner's finger which gradually recedes from the patient's finger. The same test is carried out with the feet, the patient attempts to touch examiner's finger with his big toe. A steadiness in movement without tremor is normal. The cerebellar patient has a tendency to move his finger in short jerky decomposed movements and not a smoothly coordinated total sweep dysmetria, or overshooting of the mark, is an accompaniment of cerebellar lesions. To compensate for this the patient quickens his speed and shorts out his finger at the target to get there before the unsteadiness appears. An intentional tremor which is brought on by action and ceases at rest is also characteristic. Dysdiadochokinesia-inability to perform rapid alternating movements. The normal individual is able to perform successive movements rapidly, as alternate pronation and supination of the forearm, or extension and flexion of the fingers. In cerebellar lesions the patient's successive movements are increasingly clumsy and irregular in time. Dysmetria - inability to control range of movement; Hypotonia - decreased muscle tone. Weakness may interfere with the testing procedure. The hypotonicity or atonicity can be tested by forcible swinging and flopping of the extremities. Nystagmus - involuntary, rapid oscillation of the eyeballs in a horizontal, vertical, or rotary direction, with the fast component maximal toward the side of the cerebellar lesion; 22 Scanning speech-slow enunciation with a tendency to hesitate at the beginning of a word or syllable. Dysarthria - inability to articulate words correctly, with slurring and inappropriate phrasing. Dysarthria should be carefully described, as these are often present in cerebellar diseases. Speech is usually tested while the history is taken. In cerebellar disturbances speech is slow, monotonous and interrupted by breath-taking pauses not at punctuation points. Tremor - rhythmic, alternating, oscillatory movement of a limb as it approaches a target (intention tremor) or of proximal musculature when fixed posture or weight bearing is attempted (postural tremor); Macrographia. Nystagmus or spontaneous oscillatory movements are seldom seen in the position of fixation. It may de horizontal, vertical, rotatory, dissotiated (different in each eye). There are two components, quick and slow. Nystagmus is described as follows: direction of quick component, direction of gaze which produces it, speed, amplitude, and rotatory or linear direction of movement. Important Features of Cerebellar Pathways Vestibulo-cerebellar tract Receives inputs from the vestibular system and visual areas; Output to vestibular nuclei; Controls equilibrium (balance) and eye movements; Spino-cerebellar tract Is medially placed and it consists of the vermis and the intermediate zones; Input from spinal interneurons, sensorimotor cortex, auditory, visual and vestibular systems; Output from the vermis to fastigial nucleus and then to vestibular nucleus and reticular formation in brainstem; Output from intermediate zone to interposed nucleus and then to red nucleus of brainstem and ventrolateral nucleus of thalamus; Fastigial nucleus is important in posture and locomotion; Interposed nucleus acts to control stretch reflexes and other somatosensory reflexes and damp tremor; Cerebro-cerebellar pathway Input from cerebral cortex Output to dentate nucleus and then to ventrolateral thalamus to motor cortex and premotor cortex Important for planning and initiation of volitional movement 23 LECTURE II THE PHYSIOLOGY AND PATHOLOGY OF MOTOR FUNCTION PART III. THE SUBCORTICAL STRUCTURES EXTRAPYRAMIDAL SYSTEM (anatomy, functioning and disorders) Fig. 2.5. Basal ganglia of the hemispheres (J.D. Fix, 1995) The extrapyramidal system consists of the following gray structures: caudate nucleus, putamen, pallidum, subthalamic nucleus, substantia nigra and red nucleus. The basal ganglia of the hemispheres Except of the grey cortex on the surface of the hemisphere, masses of grey matter are present in the depth of its tissue. These are called basal, central, or subcortical nuclei. They include three conglomerates of subcortical nuclei: corpus striatum, claustrum, and the amygdaloid nucleus (Fig. 2.5). 1. Corpus striatum consists of two parts, the caudate and lentiform nuclei, which are incompletely separated one from the other. The caudate nucleus (nucleus caudatus) is located above and medial to the lentiform nucleus and is separated from it by a layer of white matter called the internal capsule (capsula interna). The thickened anterior part of the nucleus, its head (caput nuclei caudati) forms the lateral wall of the anterior horn of the lateral ventricle, the body and tail (corpus and cauda nuclei caudati), stretch to the back on the floor of the central part of the lateral ventricle; the tail curves onto the superior all of the inferior horn. The caudate nucleus is separated from thalamus by the stria semicircularis (stria terminalis). Anteriad and deeper the head of the nucleus approaches the anterior perforated substance where it is united with the lentiform nucleus (with the part called the putamen). The lentiform nucleus (nucleus lentiformis) is located laterally to the caudate nucleus and the thalamus and is separated from them by the internal capsule. On a frontal section the lentiform nucleus is wedge-shaped, the apex of the wedge is directed medially, and the 24 base laterally. Two parallel white layers called the medullary laminae (laminae medullares) divide the lentiform nucleus into three segments, one lateral grey segment called the putamen and two medial lighter coloured segments united under the term globus pallidus. The globus pallidus has a distinctive macroscopic appearance and also differs from the other parts of the corpus striatum histologically. It is phylogenetically older (palaeostriatum) than the putamen of caudate nucleus (neostriatum). 2. The claustrum is a thin sheet of grey matter in the region of the insula between it and the putamen. It is separated from the putamen by a thin layer of white matter, the external capsule (capsula externa) and from the cortex of the insula by a similar layer called the capsula extrema. 3. The amygdaloid nucleus (corpus amygdaloideum), or the epistriatum is located under the putamen in the anterior end of the temporal lobe. It does not reach the temporal pole, but lies in front of the apex of the inferior horn of the lateral ventricle. Morphologically, the amygdaloid nucleus is a posteroventral continuation of the claustrum. As the formation of the cerebral cortex expands, the phylogenetically older motor centers (paleostriatum and neostriatum) become increasingly controlled by the new motor system, the system of the pyramidal tracts. Major afferent and efferent connections of the striatal system. The striatum receives major input from three sources: the thalamus, the neocortex, and the substantia nigra. The striatum projects to the globus pallidus and the substantia nigra. The globus pallidus is the effector nucleus of the striatal system; it projects to the thalamus and to the subthalamic nucleus. The substantia nigra also projects to the thalamus. The striatal motor system expresses itself via the corticobulbar and corticospinal tracts. Major neurotransmitters of the striatal motor system. Within the striatum, globus pallidus, and pars reticularis of the substantia nigra, γ-aminobutyric acid (GABA) is the predominant neurotransmitter. GABA may coexist in the same neuron with enkephalin or substance P. Dopamine-containing neurons are found in the pars compacta of the substantia nigra. Acetylcholine is found in local circuit neurons of the striatum. The subthalamic nucleus projects excitatory glutaminergic fibers to the globus pallidus. SIGNS CAUSED BY LESIONS IN EXTRAPYRAMIDAL GRISEA The main signs of extrapyramidal lesions are disorders of muscle tone (dystonia) and involuntary movement disorders (hyperkinesia, hypokinesia, akinesia) absent during sleep. Two clinical syndromes can be differentiated. One is characterized by a combination or hyperkinesia and hypotonia and is caused by a disease of the neostriatum. The other presents as a combination of hypokinesia and hypertonia or rigidity and stems from a disease of the substantia nigra. CLINICAL FEATURES OF EXTRAPYRAMIDAL DISEASE a) The Hypokinesia-Hypertonia Syndrome It may be primary Parkinson's disease. In this situation, the pigmented neurons of the substantia nigra, locus caeruleus, and other brain stem dopaminergic cell groups are lost. The cause is not known. The loss of substantia nigra neurons, which project to the caudate nucleus and putamen, results in depletion of the neurotransmitter dopamine in these areas. Onset is generally after age 40, with increasing incidence in older age groups. Secondary parkinsonism results from loss of or interference with the action of dopamine in the basal ganglia due to other idiopathic degenerative diseases, drugs, or exogenous toxins. The most common cause is ingestion of antipsychotic drugs or reserpine, which produce parkinsonism by blocking dopamine receptors. Less common causes include carbon monoxide or manganese poisoning, hydrocephalus, structural lesions (tumors, infarcts affecting the midbrain or basal ganglia), subdural hematoma, and degenerative disorders, including striatonigral degeneration and multiple systems atrophy. In postencephalitic parkinsonism, which is rare now (it occurred after the epidemic of von Economo's encephalitis in 1918 to 1924), an inflammatory process destroys the region of the midbrain containing the substantia nigra. 25 Cardinal Manifestations Bradykinesia, hypokinesia, and akinesia. Motor disturbances include slow initiation of movement (akinesia), sluggishness of movement (bradykinesia) and diminished spontaneous movement (hypokinesia); these terms are often used nearly interchangeably, as these disturbances all tend to occur together. Spontaneous fluctuations of mobility are not uncommon. The motor disturbances are often more pronounced on one side of the body, especially in the early stages of disease. They affect the craniofacial musculature to produce a masklike facies (hypomimia), defective mouth closure, reduced blinking, dysphagia, salivation (drooling), and speech that is diminished in volume (hypophonia), hoarse, poorly enunciated, and monotonous in pitch (dysarthrophonia). It may be hard to initiate speech, or repeat syllables. Postural changes include stooped posture, a mildly flexed and adducted posture of the arms, and postural instability. Gait disturbances appear in the early stages of disease and typically consist of a small-stepped gait, shuffling, and limping, with reduced arm swing. Difficulty initiating gait comes about in the later stages of disease, along with episodes of “freezing” — complete arrest of gait when the patient is confronted by doorway or a narrow path between pieces of furniture. It becomes difficult for the patient to stand up from a seated position, or to turn over in bed. Festination-an involuntary quickening of gait, as in some persons with Parkinson's disease. Impairment of fine motor control impairs activities of daily living such as fastening buttons, writing (micrographia), eating with knife and fork, shaving, and hair-combing. It becomes difficult to perform two activities simultaneously, such as walking and talking. Accompanying Manifestations. Behavioral Changes: Depression. The range of depressive manifestations includes worry, anxiety, avoidance of social contact, general unhappiness, listlessness, querulous, brooding, somatoform disturbances, and (rarely) suicidal ideation. Anxiety, tension, worry, mental agitation, lack of concentration, and dizziness are relatively common complaints. In 50 to 80% of patients, the disease begins with a resting 4- to 8-Hz pill-rolling tremor of one hand. The tremor is maximal at rest, diminishes during movement, and is absent during sleep; it is enhanced by emotional tension or fatigue. Usually, the hands, arms, and legs are most affected, in that order. Jaw, tongue, forehead, and eyelids may also be affected, but the voice escapes the tremor. Rigidity progresses, and movement becomes slow (bradykinesia), decreased (hypokinesia), and difficult to initiate (akinesia). Rigidity and hypokinesia may contribute to muscular aches and sensations of fatigue. In contrast to spastic elevation of muscle tone, rigor can be felt in extensors as a sticky, waxy resistance to all passive movements. The muscles cannot be relaxed. In passive movements one can feel that the tone of the antagonist muscles decreases in steps and not in an even, continuous fashion (cog-wheel phenomenon). The lifted head of a lying person, when suddenly released, does not fall down as usual but sinks gradually back onto the pillow (headdropping test). In contrast to their behavior in a spastic condition, the proprioceptive reflexes are not increased, and no pathologic reflexes can be observed. Paresis is absent. If it too difficult to elicit reflexes, it is not possible to intensify the patellar reflex by Jendrassik's maneuver. (The patient hooks his hands together by the flexed fingers and tries to pull them apart as hard as he can while the patellar reflexes are checked). The result is an increase in the tonic stretching reflex, that is, an activated rigidity. The face becomes masklike, with mouth open and diminished blinking, which may be confused with depression. The posture becomes stooped. Patients find it difficult to start walking; the gait becomes shuffling with short steps, and the arms are held flexed to the waist and do not swing with the stride. Steps may inadvertently quicken, and the patient may break into a run to keep from falling (festination). The tendency to fall forward (propulsion) or backward (retropulsion) when the center of gravity is displaced results from loss of postural reflexes. Speech becomes hypophonic, with a characteristic monotonous, stuttering dysarthria. Hypokinesia and impaired control of distal musculature are results in micrographia and increasing 26 difficulty with activities of daily living. Dementia affects about 50% of patients, and depression is common (Fig. 2). During examination, passive movement of the limbs is met with a plastic, unvarying lead-pipe rigidity; superimposed tremor bursts may have a ratchet-like cogwheel quality. The sensory examination is usually normal. Signs of autonomic nervous system dysfunction (e.g., seborrhea, constipation, urinary hesitancy, orthostatic hypotension) may be found. Muscle strength is usually normal, although useful power may be diminished and the ability to perform rapid successive movements is impaired. Reflexes remain normal but may be difficult to elicit in the presence of marked tremor or rigidity. b) The Hyperkinesia-Hypotonia Syndrome This syndrome develops if the neostriatum is damaged. Occasionally, such lesions are accompanied by others in the globus pallidus, thalamus, or cerebral cortex; in such cases the hyperkinesia is possibly caused by a loss of inhibitory neurons of the neostriatum that descend to pallidum and substantia nigra. In other words, a loss of a neuronal system of higher order has occurred, producing excessive excitation of the neurons of the next lower system. The resulting hyperkinesias are of different kinds: athetosis, chorea, spasmodic torticollis, torsion dystonia, ballism, and other conditions . Clinical Features of the Hyperkinesia-Hypotonia Syndrome. Athetosis This kinetic disorder is usually caused by perinatal damage to the striate bodies. Involuntary movements are slow and wormlike, with a tendency to overextend the peripheral portions of the extremities. In addition, there are irregular, spasmodic increases in muscle tensions between agonists and antagonists. As a result, postures and movements are rather bizarre. Voluntary movements are severely distorted by the spontaneous appearance of hyperkinetic movements that may include face and tongue and thus cause grimacing with abnormal tongue movements like laughing or crying. The athetosis may be combined with a contralateral paresis; it may also be bilateral and is then called double athetosis, which usually occurs in association with spastic paraplegia (Little's disease). Chorea The chorea syndrome is characterized by short, fast, involuntary jerks occurring in single muscles, random and producing various patterns of movements. At first the peripheral portions of the extremities are involved and the proximal portions follow. Involuntary jerks of the facial muscles produce grimacing. A combination of choreiform and (distal) dystonic movements is termed choreoathetosis. Huntington disease, an autosomal dominant disorder, is the best-known cause of chorea Others include hereditary diseases (e. g., neuroacanthocytosis, and benign hereditary chorea) and neurodegenerative diseases (e. g., Alzheimer disease, multisystem atrophy). Secondary chorea may be caused by infections (e. g., Sydenham’s chorea due to streptococcal infection; herpes encephalitis, toxoplasmosis), vascular disease (e. g., lupus erythematosus, stroke), brain tumor, drug therapy (e. g., estrogen, neuroleptic drugs), or old age (senile chorea). Spasmodic torticollis and torsion dystonia These are the most important types of dystonia syndromes. In both diseases there are usually alterations within the putamen and the centromedian nucleus of the thalamus and in other extrapyramidal nuclei (pallidum, substantia nigra, and others). Blepharospasm. Spasmodic contraction of the orbicularis oculi muscle causes excessive blinking and involuntary eye closure. It can often be accompanied by ocular foreign-body sensation and be ameliorated by distracting maneuvers, and is worse at rest or in bright light. There may be involuntary clonic eye closure, tonic narrowing of the palpebral fissure, or difficulty opening the eyes. Blepharospasm may be so severe as to leave the 27 patient no useful vision. Cervical dystonia Cervical dystonia may involve head rotation (torticollis), head tilt to one side (laterocollis), or flexion or extension of the neck (anterocollis, retrocollis), often accompanied by tonic shoulder elevation or head tremor. It may be difficult to distinguish nondystonic from dystonic head tremor; only the latter can be improved by antagonistic maneuvers. Dystonia often causes pain, usually in the neck and shoulder. Torsion dystonia Torsion dystonia is characterized by rather extensive turning and twisting movements of trunk and proximal extremities. They can be so severe that the patient can neither stand nor walk without support. The disease may be idiopathic or symptomatic; in the latter case the cause may be birth injury, kernicterus, former encephalitis, early Huntington's chorea. Hallervorden-Spatz disease, or a hepatocerebral degeneration (Wilson's diease, Westphal-Strumpell disease). Tics Tics are rapid, irregular, involuntary movements (motor tics) or utterances (vocal tics) that interrupt normal voluntary motor activity. They are triggered by stress, anxiety, and fatigue but may also occur at rest; they can be suppressed by a voluntary effort, but tend to re-emerge with greater intensity once the effort is relaxed. Tics are often preceded by a feeling of inner tension. They may be transient or chronic. Simple tics. Simple motor tics involve isolated movements, e. g., blinking, twitching of abdominal muscles, or shrugging of the shoulders. Simple vocal tics may involve moaning, grunting, hissing, clicking, shouting, throat clearing, sniffing, or coughing. Complex tics. Complex motor tics consist of stereotyped movements that may resemble voluntary movements, e. g., handshaking, scratching, kicking, touching, or mimicking another person’s movements (echopraxia). Complex vocal tics may involve obscene language (coprolalia) or the repetition of another person’s words or sentences (echolalia). Gilles de la Tourette syndrome (often abbreviated to Tourette syndrome) is a chronic disease in which multiple motor and vocal tics begin in adolescence and progress over time. Other features of the disease are personality disturbances, obsessive-compulsive phenomena, and an attention deficit. Hemiballism (Ballism) Ballism consists of violent flinging movements of the limbs due to involuntary contraction of the proximal limb muscles, and usually affects only one side of the body (hemiballism). It may be continuous or occur in attacks lasting several minutes. The most common cause is an infarction or other destructive lesion of the subthalamic nucleus (STN). Diminished neural outflow from the STN leads to increased activity in the thalamocortical motor projection. Myoclonus Myoclonus consists of involuntary, brief, sudden, shocklike muscle contractions producing visible movement. It has a variety of causes and may be focal, segmental, multifocal, or generalized. It’s cortical, subcortical, or spinal origin can be determined by neurophysiological testing. Attacks of myoclonus may be spontaneous or may be evoked by visual, auditory, or somatosensory stimuli (reflex myoclonus) or by voluntary movement (postural myoclonus, action myoclonus). 28 a) b) Fig.2.6. Patient with parkinsonism c) Fig. 2.7. a)athetosis; b)cervical dystonia; c)ballism Clinical features of the internal capsule lesions. As a result of compact location of the different passways, damages of the capsulae internae include disorders of the movement, decrease in the threshold for perceiving touch, pain, and temperature and deep sensations, and the visual problems. The complete syndrome is called “the syndrome of three hemi”. Signs that may be found as a result of unilateral or bilateral involvement of the capsulae internae: Unilateral paralysis (hemiplegia) of the opposite side of the body and contralateral III nerve palsy. Contralateral hemihypesthesia, usually involving trunk and extremities more severely than the face. Visual field deficit (contralateral homonymous hemianopia). Fragmentary lesions of the anterior part of the posterior limb result in abnormalities only of the movement (contralateral hemiplegia). If damage is localized in the posterior part of the posterior limb capsulae internae the “syndrome of three hemi” is formed (contralateral homonymous hemianopia, hemihypesthesia and hemiataxia). 29 LECTURE III SENSATION AND ITS DISORDERS Fig. 3.1. Sensory pathways (Lecture notes. The University of Western Ontario Department of Anatomy and Cell Biology, 2007). Sensation is the ability of an organism to perceive the irritations caused by the environment or by its own tissues and organs. Receptors are special sensitive structures, capable to perceive any 30 changes inside or outside of an organism and to transform them to nervous impulses. All kinds of external effects are transformed into nervous impulses, and are reached the brain as signals. Depending on functional features the receptors are subdivided into exteroceptors, that respond to external stimuli (mechanical, thermal, optic, acoustic, olfactory, gustatory), proprioceptors (they give the information about tendon and muscle tension, movements and position of the body) and interoceptors (informing of the condition inside an organism). There are osmoreceptors, chemoreceptors, baroreceptors and others. Skin receptors are divided into mechanoreceptors (touch, tension), thermoreceptors (cold, heat) and nociceptors (pain). A great number of these receptors is situated between epidermis and connective tissue. Therefore the skin can be considered as a sensitive organ covering the whole surface of the body. There are free nerve endings and capsulated nervous bodies in the skin. Free nerve endings are located between epidermal cells and perceive painful irritations. Tactile Merkel’s corpuscles are located basically on tips of fingers and react to touch. Meissner’s corpuscles are on palms, soles, lips, tongue tip, mucous membrane of genitals and are very sensitive to touch. Pacinian Vater-Pacini corpuscles, located in deep layers of skin, perceive tension. Krause's end bulbs are considered as cold receptors and Ruffini’s corpuscles are thermal receptors. Receptors are founded in deeper tissues such as muscles, tendons, fasciae and joints. Muscular receptors include some types, most important of which are neuromuscular spindles. They react to muscle strain and are responsible for the realization of the stretch reflex. Golgi-Mazzoni corpuscles are located between the tendon and the muscle. From the receptor, information is transmitted to the afferent fibers of the pseudounipolar spinal ganglion cells, whose efferent fibers reach the spinal cord by way of the dorsal root. A synapse onto a second neuron in the sensory pathway is made either immediately, in the posterior horn of the spinal cord (protopathic system), or more rostrally, in the brain stem (lemniscal system). The highest level of the somatosensory pathway is the contralateral primary somatosensory cortex. The somatotopic organization of the somatosensory pathway is preserved at all levels. The classification of sensation: 1) Superficial sensation (exteroceptive) such as pain, temperature and tactile; 2) Deep sensation (proprioceptive) such as joint position sense, vibratory sense, the sense of body weight and pressure sense, kinesthesia; 3) Compound sense such as sense of localization, posture sense (the recognition of signs and letters written on the skin), sense of discrimination (the recognition of pricks made at close distance), stereognosis; 4) Interoceptive sensation. Protopathic sensation is phylogenetically a more ancient kind characterised by limited opportunities of differentiation of irritations by their modality, intensity and localization. Epicritic sensation is phylogenetically new kind of sensitivity. The general scheme of the structure of sensory system is the following: 1. All the first neurons of sensation are in spinal ganglions (sensory ganglions of cranial nerves). 2. The axons of the second neurons always pass onto the opposite side (the neurons of superficial sensation in the spinal cord, neurons of deep sensation in the brain). 3. The third neurons of all kinds of sensation are in the thalamus. Sensory irritations are conducted by two sensory systems, namely by the extralemniscus system (superficial sensation) and the lemniscus system (deep sensation). The extralemniscus system includes conductors of pain, temperature and partly tactile sensation. The first neuron is in the spinal ganglion. The dendrites of these pseudounipolar neurons as a part of peripheral nerves arrive at skin where they end by specific receptors. The axons of these neurons form the dorsal root of the spinal nerve enter into the posterior horn of the spinal cord and contact with second sensory neuron. Their axons come over to the opposite side and in lateral columns of the spinal cord go to the thalamus (lateral spinothalamic tract). Central fibers of the first sensory neuron ascend 1 or 2 segments before making a synapse in the substantia gelatinosa of 31 the posterior horn. Fibers from the posterior horn decussate and enter the lateral spinothalamic tract, which, like the anterior spinothalamic tract, projects to ventral posterolateral nucleus; which projects in turn to the postcentral gyrus. Fibers from the posterior horn decussate and enter the lateral spinothalamic tract, which, like the anterior spinothalamic tract, projects to ventral posterolateral nucleus, which projects in turn to the postcentral gyrus. The lemniscus system includes the conductors of deep sensation. The dendrites of pseudounipolar neurons of deep sensation of the spinal nerves as a part of peripheral nerves pass to receptors in muscles, tendons, periosteum and to tactile receptors of the skin. The axons of first sensory neurons don’t enter to the grey substance. They form posterior columns in which there is somatotopical localization. Fibers mediating sensation in the legs are in the fasciculus gracilis (medial), while those for the arms are in the fasciculus cuneatus (lateral). These fibers synapse onto the second sensory neuron in the corresponding somatosensory nuclei of the lower medulla (nucleus gracilis, nucleus cuneatus). Fibers from these nuclei decussate and ascend in the contralateral medial lemniscus and ascend to the postcentral gyrus through thalamus (ventral posterolateral nucleus) and internal capsule. SENSORY DIORDERS Kinds of the sensory disorders: anesthesia (local or general loss of bodily sensation), hypesthesia (partial loss), analgesia, hyperesthesia (increased sensitivity). The corresponding terms for pain appreciation are analgesia, hypalgesia, and hyperalgesia or hyperpathia (strong, unpleasant, badly localized sensation); dysesthesia (perversion of sensation), topanesthesia (loss of localization sense), thermoanesthesia (loss of temperature sense), astereognosis (inability to recognize objects by touch), paresthesia (an abnormal or inappropriate sensation in an organ, part, or area of the skin, as of burning, prickling, tingling, etc.), causalgia (a burning sensation along the course of a peripheral nerve together with local changes in the appearance of the skin), polyesthesia (means sensation of one stimulus as several ones), alloesthesia (sensation of stimuli in the other place of body), allocheiria (sensation of stimuli in the symmetrical site of body), phantom-limb pains (pain in stump limb). Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage (International Association for the Study of Pain). Pain results from the interaction of a pain-producing stimulus with a receptor, and the following transmission and processing of pain-related signals in the peripheral or central nervous system. This process is called nociception. Pain evokes a behavioral response involving nocifensor activity as well as motor and autonomic reflexes. Nociceptive pain, the “normal” type of pain, is that which arises from actual or potential tissue damage and results from the activation of nociceptors and subsequent processing in an intact nervous system. Somatic pain is the variety of nociceptive pain mediated by somatosensory afferent fibers; it is usually easily localizable and of sharp, aching, or throbbing quality. Postoperative, traumatic, and local inflammatory pain are often of this variety. Visceral pain is harder to localize (e. g., headache in meningitis, biliary colic, gastritis, mesenteric infarction) and may be dull, cramplike, piercing, waning. This may explain the unpleasant and emotionally distressing nature of visceral pain. Visceral pain may be felt in its site of origin or may be referred to another site (e. g., from the diaphragm to the shoulder) or to a cutaneous zone (of Head) specific to that organ. Neuropathic pain is that which is caused by damage to nerve tissue. It is always referred to the sensory distribution of the affected neural structure: e. g., calf pain in S1 radiculopathy, frontal headache in tentorial meningioma. Types of the sensory disorders. 1. Peripheral type: polyneuritic, neural, plexal. 2. Segmentary type: ganglionary, radicular and segmental-dissociated. 3. Central: conduction, central, cortical. 4. Symptoms of loss and irritating signs (sensitive "Jackson"). Examination. Somatic sensation is tested with the patient’s eyes closed and on the symmetrical parts of body. The appreciation of sense of light touch is evaluated with a wisp of cotton wool, 32 which is brought down carefully on a small region of skin. The patient lies quietly, with the eyes closed, and makes a signal each time the stimulus is felt. General tactile sensibility is tested by the use of a light stimulus such as a camel's hair brush, a wisp of cotton, a feather, a piece of tissue paper, or even a very light touch with a fingertip. Touch is tested along with pain by stimulating alternately (but not in an even rhythm) with the sharp and blunt portions of a pin. The stimulus should be so light that no pressure on subcutaneous tissues is produced. Allowance must be made for thicker skin on the palms and soles and the especially sensitive skin in the fossae. The patient is asked to say «Now» or «Yes» when he feels the stimulus and to name or point to the area stimulated and state the nature of the stimulus. Similar stimuli are used for evaluating discriminatory tactile sensation but this is best tested on the hairless skin, since motion of the hairs must be avoided. It is also tested by noting the patient's ability to localize the stimuli accurately and by investigating two-point discrimination. Topoanesthesia may be used to indicate loss of tactile localization. Graphanesthesia is the inability to recognize numbers or letters written on the skin. Pressure sensation, or touchpressure, may be regarded as a distinct type of tactile sensation, involving more gross pressure from the skin. Pressure sense is tested by firm touch upon the skin with a finger or a blunt object, and by pressure on the subcutaneous structures, such as the muscle masses, the tendons, and the nerves themselves, either by the use of a blunt object or by squeezing between the fingers, and one tests both the appreciation and the localization of pressure. Two-point, or spatial, discrimination is the ability to differentiate cutaneous stimulation by one blunt point from stimulation by two points. A compass or a calibrated two-point esthesiometer is used, and the patient is stimulated randomly by a single point and by two points. The distance varies considerably in different parts of the body. Two points can be differentiated from one at a distance of 1 mm on the tip of the tongue, at 2 - 4 mm on the fingertips, at 4 - 6 mm on the dorsum of the fingers, at 8-12 mm on the palm, and at 20 - 30 mm on the dorsum of the hand. Two-point discrimination is a highly discriminatory tactile sensibility, carried mainly through the posterior columns (dorsal funiculi). Loss of two-point discrimination with preservation of other discriminatory tactile and proprioceptive sensation may be the most subtle sign of a lesion of the opposite parietal lobe. Barognosis is the recognition of weight, or the ability to differentiate between weights. It is tested by the use of objects of similar size but of different weights, such as a series of plastic or wooden balls, or blocks loaded with different weights, which are appraised by holding them in the hand, either unsupported or resting on a table, but preferably the former. The senses of motion and position should be intact. Pinprick appreciation is tested by asking the patient to indicate whether the point of a pin feels sharp or blunt. Appreciation of sense of pressure or sense of touch by the pinpoint must not be confused with the appreciation of sharpness. Temperature sensation is evaluated by application to the skin of containers of hot or cold water or, better, by the use of cold or warm metal tubes or other metal objects. The patient is asked to respond by saying «hot» or «cold». Changes in temperature sensibility are recorded by the terms thermanesthesia, thermhypesthesia, and thermhyperesthesia, modified by the adjectives hot and cold. Deep pressure sensibility is evaluated by pressure on the tendons, such as the Achilles tendon at the ankle. Sense of vibration is evaluated with a tuning fork (128 Hz) that is set in motion and then placed over a bony prominence; the patient is asked to indicate whether vibration, rather than simple pressure, is felt. Joint position sense is tested by asking the patient to indicate the direction of small passive movements of the terminal interphalangeal joints of the fingers and toes. Sensations of motion and position may also be tested by placing the fingers of one of the patient's hands in a certain position while his eyes are closed, then asking him to describe the position or to imitate it with the other hand. The foot may be passively moved while the eyes are closed, and the patient asked to point to his great toe or his heel. The patient may be asked to hold his hands outstretched; with loss of position sense one hand may waver or droop. One of the outstretched hands may be passively raised or lowered while the patient's eyes are closed, and the patient is asked to place the other extremity at the same level. One of the hands may be passively moved while the eyes are closed, and the patient asked to grasp the thumb or forefinger of that hand 33 with the opposite hand. These latter tests, however, do not denote the side of involvement when a unilateral lesion is present. Certain tests for ataxia, such as the finger-to-nose test and the heel-to-knee-to-toe test, are methods for examining the senses of motion and position if they are executed while the eyes are closed, assuming the tests are normal when the eyes are open. The senses of motion and position are also examined by observation of the station and gait. A patient with significantly disturbed sensations of movement and of position in the lower extremities is not aware of the position of his feet or of the posture of his body. A patient can assume a stable, erect posture when standing with his eyes open, but when his eyes are closed he tends to sway and fall; he can walk fairly well when his eyes are open, but when his eyes are closed he throws out his feet, staggers, and may fall (sensory ataxia). The Romberg sign is positive when the patient is able to stand with his feet together while his eyes are open, but sways or falls when they are closed; it is one of the earliest signs of posterior column disease. Fig. 2.2 Segmental innervation of the skin 34 SYNDROMES OF LESION OF SENSORY SYSTEM ON DIFFERENT LEVELS Peripheral Nerve Lesions Mononeuropathy. A mononeuropathy is a lesion of one nerve by a local process, usually compression, trauma or a vascular cause. Clinical examination typically demonstrates negative and positive sensory disturbances restricted to the territory of the nerve involved. Polyneuropathy. In patients with polyneuropathies, sensory loss is symmetric and more frequently distally than proximally (stocking-and-glove sensory loss). The peripheral nervous system is involved diffusely. Sensory loss may be accompanied by a motor deficit. Plexus lesion. It is appeared by hypo- or anesthesia of all sorts of sensation in the region of plexal innervation with pain, paresthesias and vegetative disorders Root lesion. Pain due to root compression is generally accompanied by sensory loss in appropriate dermatom, muscle weakness, and decreased or absent tendon reflexes. If the spinal ganglion is involved, the herpes zoster is appeared. Cord lesion. In patients with a cord lesion, there may be a transverse sensory level. Physiologic areas of increased sensitivity do occur, however, at the costal margin, over the breasts, and in the groin, and these must not be taken as abnormal. Therefore, the level of a sensory deficit affecting the trunk is best determined by careful sensory testing over the back rather than the chest and abdomen. Central cord lesion.(Fig. 3.3) Central cord lesion (such as syringomyelia, following trauma, certain cord tumors) may cause a loss of pain and temperature appreciation with sparing of other modalities. This loss is due to the interruption of fibers conveying pain and temperature that cross from one side of the cord to the spinothalamic tract on the other. Such a loss is usually bilateral, may be asymmetric. It may be accompanied by lower motor neuron weakness in the muscles supplied by the affected segments. Fig. 3.3. Cord lesions (Greenberg et al., 2002) a) Central cord lession b) Anterior lesion cord c) Cord hemisection The level of the posterior horn. Disorders in the posterior horn are characterized by pain and temperature sensivity diorders. Anterolateral cord lesion. Lesions involving the anterolateral portion of the spinal cord (lateral spinothalamic tract) can cause contralateral abnormality of pain and temperature sensation in segments below the level of the lesion. Anterior grey commissure. Lesion in its region cause dissociated disorders – pain and temperature sensations disorders in symmetrical parts of body like a “butterfly” or “jacket”. Anterior cord lesion (Fig.3.3). With destructive lesions involving the anterior portion of the spinal cord, pain and temperature appreciation are impaired below the level of the lesion from lateral spinothalamic tract involvement. Weakness or paralysis of muscles supplied by the involved segments of the cord results from damage to motor neurons in the anterior horn. Posterior column lesion. There is loss of vibration and joint position sense below the level of the lesion, with preservation of other sensory modalities. Cord hemisection.(Fig. 3.3) Lateral hemisection of the cord leads to Brown-Sequard's syndrome. Below the lesion, there is an ipsilateral pyramidal deficit and disturbed appreciation of 35 vibration and joint position sense, with contralateral loss of pain and temperature appreciation that begins two or three segments below the lesion. Brainstem lesion. Sensory disturbances may be accompanied by a motor deficit, cerebellar signs, and cranial nerve palsies when the lesion is in the brainstem. In patients with lesions involving the spinothalamic tract in the dorsolateral medulla and pons, pain and temperature appreciation are lost in the limbs and trunk on the opposite side of the body. When such a lesion is located in the medulla, it also typically involves the spinal trigeminal nucleus, impairing pain and temperature sensation on the same side of the face as the lesion. The result is a crossed sensory deficit that affects the ipsilateral face and contralateral limbs. In contrast, spinothalamic lesions above the spinal trigeminal nucleus affect the face, limbs, and trunk contralateral to the lesion. With lesions affecting the medial lemniscus, there is loss of touch and proprioception on the opposite side of the body. In the upper brainstem, the spinothalamic tract and medial lemniscus run together so that a single lesion may cause loss of all superficial and deep sensation over the contralateral side of the body. Medial lemniscus lesion cause hemianesthesia and sensitive hemiataxia (anesthesia of deep sorts of sensation). Thalamic Lesions. Thalamic lesions may lead to loss or abnormality of all forms of sensation on the contralateral side of the body and is appeared by hemianesthesia, sensitive ataxia, hemianopsia, hemialgia. Spontaneous pain, hyperpathia may occur on the affected side. Patients may describe it as burning, tearing, knifelike, or stabbing. Any form of cutaneous stimulation can lead to painful or unpleasant sensations. Some later develop persistent severe pain and choreoathetoid movements on the affected side, mild hemiataxia, and astereognosis. Called also Dejerine-Roussy syndrome. Lesion of internal capsule. Involvement of the sensory radiations in the internal capsule causes variable and sometimes extensive diminution of all types of sensation on the opposite side of the body. The changes are similar to those which follow a thalamic lesion, and it may be difficult to differentiate between the two. Pain, however, is rarely experienced. There are hemianesthesia, hemiataxia, hemiplegia. Lesions of the sensory cortex (postcentral gyrus). Cortical sensory disturbances are usually appeared by monoanesthesia in the opposite side of body. Stimulation of postcentral gyrus cause sensitive "Jackson"-the feeling of tingling or numbness in the opposite side. Lesion of upper parietal lobule is be characterized by astereognosis. 36 LECTURE V SPINAL CORD SYNDROMES The spinal cord contains motor, sensory, and autonomic fibers and nuclei in a tight spatial relationship with one another. Lesions of the spinal cord can cause a wide variety of neurological deficits, which can be combined with each other in many different ways. The spinal cord, like the brain, is composed of gray matter and white matter. The white matter contains ascending and descending fiber tracts. The gray matter contains neurons of different kinds: the anterior horns contain mostly motor neurons, the lateral horns mostly autonomic neurons, and the posterior horns mostly somatosensory neurons participating in a number of different afferent pathways. In addition, the spinal cord contains an intrinsic neuronal apparatus consisting of interneurons, association neurons, and commissural neurons, whose processes ascend and descend in the fasciculus proprius. Fig. 4.1. Cross section of the spinal cord The average length of the cord is 42 cm in women and 44.7 cm in men. In normal adults the cord ends between the twelfth thoracic vertebra (T12) and the lower third of the third lumbar vertebra (L3). The nerve roots, however, still exit from the spinal canal at the numerically corresponding levels. Spinal cord ends as the conus medullaris at the L1 or L2 level (rarely at L3). Below this level, the lumbar sac (theca) contains only nerve root filaments, the so-called cauda equina. The spinal cord has got the cervical and lumbar enlargements. The cervical enlargement contains the segments corresponding to the upper limbs (C4-T1), which form the brachial plexus; the lumbar enlargements contains the ones for the lower limbs (L2-S3), which form the lumbosacral plexus. Attached to the spinal cord are 31 pairs of nerves: 8 cervical (C), 12 thoracic (T), 5 lumbar (L), 5 sacral (S), and one or more (1-3) rudimentary coccygeal pairs. The spinal nerves are formed by the union of a dorsal and a ventral root. The spinal cord is surrounded by pia mater, arachnoid, and dura mater. The pia mater is a delicate membrane that closely invests the spinal cord. The arachnoid is a transparent membrane that is close to the inner surface of the dura, but fine strands extend to the pia. The dura mater is a strong, fibrous membrane, penetrated by the nerve roots, which forms a firm, tubular sheath. It is separated from the wall of the vertebral canal by the epidural space, which contains areolar tissue and a plexus of veins. The subdural space is a potential space containing a small amount of fluid. The subarachnoid space, which extends to about the level of the second sacral vertebra, is a welldefined cavity containing cerebrospinal fluid. The dentate ligaments extend along the lateral surface 37 of the spinal cord, between the anterior and posterior nerve roots, from the pia to the dura mater. They suspend the spinal cord in the vertebral canal. On cross section (Fig. 4.1, 4.2) the spinal cord is seen to be divided into an H-shaped core of gray matter and a surrounding white matter. The superior limbs of the H are called the dorsal horns and the inferior, the ventral horns. This gray matter consists largely of neurons and glia, while the white matter consists of nerve fibers and glia. Within the center of the gray matter and running throughout the entire length of the cord is a minute remnant of the central canal consisting of a single layer of ependymal cells. The nerve fibers of the white matter of the cord group into definite tracts, most of which have a somatotopic arrangement. The origin and termination of the tracts is of critical importance clinically. Surrounding the gray matter are the so-called fasciculi proprii or ground bundles, consisting of many short and some long fibers linking the spinal segments into reflex patterns. The longer coursing tracts are located peripheral to these ground bundles. Most nerve fibers of the dorsal columns originate from the dorsal root ganglia. Many dorsal column axons ascend to the junction of the spinal cord with the medulla oblongata; there they synapse in the nuclei gracilis and cuneatus, leg fibers going to the nucleus gracilis and arm fibers to the nucleus cuneatus. These dorsal column fibers are primary; they are a direct extension of the entering dorsal root axons which form the dorsal columns without synapsing. From the nuclei gracilis and cuneatus, the sensory pathway decussates to travel to the thalamus and the cerebral cortex. The other sensory tracts of the spinal cord are composed of secondary or tertiary fibers, having one or more neurons interposed between the entering primary dorsal root axons and the cell of origin of the tract in the spinal cord. In addition to these intrinsic systems, the spinal cord contains many tracts originating from the brain. The essential tracts can be summarized briefly, according to whether they are motor or sensory. Fig. 4.2. Main pathways of the spinal cord Lesions of the spinal cord are characterized by sensory, motor, and autonomic changes. Its occasionally affect only the white matter or only the gray matter (e. g., acute poliomyelitis), but more often affect both. The symptoms depend upon the location and extent of damage to various functional elements, and often upon the type of damage and the rapidity with which the lesion develops. Syndrome of the dorsal root ganglion. Infection of one or more spinal ganglia by a neurotropic virus occurs most commonly in the thoracic region and causes painful erythema of the corresponding dermatomes, followed by the formation of a variable number of cutaneous vesicles. This clinical picture, called herpes zoster, is associated with very unpleasant, stabbing pain and paresthesiae in the appropriate area. Posterior root syndrome. If two or more adjacent posterior roots are completely divided, sensation in the corresponding dermatomes is partially or totally lost. Incomplete posterior root lesions affect different sensory modalities to variable extents, with pain sensation usually being most strongly affected. Because the lesion interrupts the peripheral reflex arc, the sensory deficit is accompanied by hypotonia and hyporeflexia or areflexia in the muscles supplied by the affected roots. These typical deficits are produced only if multiple adjacent roots are affected. 38 Posterior column syndrome. Lesions of the posterior columns usually cause disturbances of position and vibration sense, discrimination, they also produce a positive Romberg sign, as well as gait ataxia that worsens significantly when the eyes are closed (unlike cerebellar ataxia, which does not). Posterior column lesions also often produce hypersensitivity to pain. Possible causes include vitamin B12 deficiency (“funicular myelosis”), AIDS-associated vascular myelopathy, and spinal cord compression (e. g., in cervical spinal stenosis). Posterior horn syndrome can be a clinical manifestation of syringomyelia, hematomyelia, and some intramedullary spinal cord tumors. Like posterior root lesions, posterior horn lesions produce a segmental somatosensory deficit. Only pain and temperature sensation are lost in the corresponding ipsilateral segments, only second neuron of sensory pathway are in the posterior horn (whose axon ascends in the lateral spinothalamic tract). Loss of pain and temperature sensation with sparing of posterior column sense is called a dissociated somatosensory deficit. Graymatter syndrome. Damage to the central gray matter of the spinal cord by syringomyelia, hematomyelia, intramedullary spinal cord tumors, or other processes interrupts all of the fiber pathways passing through the gray matter. The fibers which originate in posterior horn cells and conduct pressure, touch, pain, and temperature sensation; decussate in the central gray matter and then ascend in the anterior and lateral spinothalamic tracts. A lesion affecting them produces a bilateral dissociated sensory deficit in the cutaneous area supplied by the damaged fibers. Anterior horn syndrome. Both acute poliomyelitis and spinal muscle atrophy of various types affect the anterior horn cells, particularly in the cervical and lumbar enlargements of the spinal cord. In poliomyelitis (a viral infection), a variable number of anterior horn cells are lost, mainly in the lumbar region, causing flaccid paresis of the muscles in the corresponding segments. Proximal muscles tend to be more strongly affected than distal ones. The muscles become atrophic and, in severe cases, may be completely replaced by connective tissue and fat. Combined anterior horn and pyramidal tract syndrome (e.g. amyotrophic lateral sclerosis) is the result of degeneration of cortical and spinal motor neurons. The clinical picture is a combination of flaccid and spastic paresis. The spinal cord hemisection syndrome (Brown-Sequard syndrome) is rare and usually incomplete. It’s usually caused by trauma and cervical disk herniation. Interruption of the descending motor pathways on one side of the spinal cord causes an initially flaccid, ipsilateral paresis below the level of the lesion (spinal shock), which later becomes spastic and is accompanied by hyperreflexia, Babinski signs, and vasomotor disturbances. At the same time, the interruption of the posterior columns on one side of the spinal cord causes ipsilateral loss of position sense, vibration sense, and tactile discrimination below the level of the lesion. The ataxia that would normally be caused by the posterior column lesion cannot be demonstrated because of the coexisting ipsilateral paresis. Pain and temperature sensation are spared on the side of the lesion, because the fibers subserving these modalities have already crossed to the other side to ascend in the lateral spinothalamic tract, but pain and temperature sensation are lost contralaterally below the level of the lesion, because the ipsilateral (crossed) spinothalamic tracts are interrupted. SPINAL CORD TRANSECTION SYNDROMES Acute spinal cord transection syndrome. Complete transection of the spinal cord, whether of traumatic, neoplastic, vascular, or other origin, causes isolation of the segments below the level of the lesion. The upper portions of the cerebrospinal axis function normally, but motor, sensory, and autonomic functions are lost distal to the lesion. Acute spinal cord trauma initially produces socalled spinal shock, a clinical picture whose pathophysiology is incompletely understood. Below the level of the lesion there is complete, flaccid paralysis, and all types of sensation are lost. Bladder, bowel, and sexual function are lost too. There are also trophic changes below the level of the lesion e. g. decubitus ulcers). The upper border of the sensory deficit (the “sensory level”) is often demarcated by a zone of hyperalgesia. In the days and weeks after the causative event, the spinal neurons gradually regain their function, at least in part, but remain cut off from most of the centrally derived neural impulses that normally regulate them. They thus become “autonomous,” and so39 called spinal automatisms appear. In many cases, a stimulus below the level of the lesion induces sudden flexion of the hip, knee, and ankle (flexor reflex); if the spinal cord transection syndrome is complete, the limbs retain the flexed position for a long time after the stimulus because of a spastic elevation of muscle tone. (In incomplete spinal cord transaction syndrome, on the other hand, the legs are initially flexed upon stimulation, but then return to their original position.) Defecation and urination gradually function again, but are no longer under voluntary control; instead, the bladder and bowel are emptied reflexively once they are filled to a certain point. Detrusorsphincter dyssynergia causes urinary retention and frequent, reflexive micturition. The deep tendon reflexes and muscle tone gradually return and can become pathologically elevated. Progressive spinal cord transection syndrome. When spinal cord transaction syndrome arises gradually rather than suddenly, e. g., because of a slowly growing tumor, spinal shock does not arise. Progressively severe spastic paraparesis develops below the level of the lesion, accompanied by a sensory deficit, bowel, bladder, and sexual dysfunction, and autonomic manifestations. Cervical spinal cord transection syndrome. Spinal cord transection above the level of the third cervical vertebra is fatal, as it abolishes breathing (total loss of function of the phrenic and intercostal nerves). Transection at lower cervical levels produces quadriparesis with involvement of the intercostal muscles; breathing may be dangerously impaired. Thoracic spinal cord transection syndrome. Transection of the upper thoracic cord spares the upper limbs but impairs breathing and may also cause paralytic ileus through involvement of the splanchnic nerves. Transection of the lower thoracic cord spares the abdominal muscles and does not impair breathing. Lumbar spinal cord transection syndrome. Traumatic transection of the spinal cord at lumbar levels often causes especially severe disturbances because of concomitant damage of the major supplying artery of the lower spinal cord, the great radicular artery (of Adamkiewicz). The result is infarction of the entire lumbar and sacral spinal cord. Epiconus syndrome, caused by a spinal cord lesion at the L4 to S2 level. Unlike it is associated with spastic or flaccid paresis of the lower limbs, depending on the precise level of the lesion. There is weakness or total paralysis of hip external rotation (L4S1) and extension (L4L5), and possibly also of knee flexion (L4S2) and flexion and extension of the ankles and toes (L4S2). The Achilles reflex is absent, while the knee-jerk reflex is preserved. The sensory deficit extends from L4 to S5. The bladder and bowel empty only reflexively; sexual potency is lost. Conus syndrome, due to a spinal cord lesion at or below S3, is also rare. It can be caused by spinal tumors, ischemia, or a massive lumbar disk herniation. An isolated lesion of the conus medullaris produces the following neurological deficits: detrusor areflexia with urinary retention and overflow incontinence, fecal incontinence, impotence saddle anesthesia (S3S5), loss of the anal reflex, the lower limbs are not paretic. Cauda equina syndrome involves the lumbar and sacral nerve roots, which descend alongside and below the conus medullaris, and through the lumbosacral subarachnoid space, to their exit foramina; a tumor (e. g., ependymoma or lipoma) is the usual cause. Patients initially complain of radicular pain in a sciatic distribution, and of severe bladder pain that worsens with coughing or sneezing. Later, variably severe radicular sensory deficits, affecting all sensory modalities, arise at L4 or lower levels. Lesions affecting the upper portion of the cauda equina produce a sensory deficit in the legs and in the saddle area. There may be flaccid paresis of the lower limbs with areflexia; urinary and fecal incontinence also develop, along with impaired sexual function. SIGNS OF THE SPINAL CORD LESION C1-C5: spastic palsy below the lesion (tetraplegia) flaccid palsy of muscles of head and neck and diaphragm sensory loss below the lesion upper neuron type of bladder dysfunction 40 C5-T1 (cervical enlargement): flaccid palsy of hands spastic palsy of legs sensory loss below the lesion upper neuron type of bladder dysfunction Horner’s syndrome T1-T12: spastic palsy of legs sensory loss below the lesion upper neuron type of bladder dysfunction trophic changes in lower part of the body and legs L1-S2 (lumbar enlargement): flaccid palsy of legs sensory loss in legs and saddle (paranesthesia) upper neuron type of bladder dysfunction L4-S2 (epiconus): flaccid palsy of posterior group of muscles of the leg, absent Achilles reflex sensory loss in shin, foot, buttocks and saddle (paranesthesia) upper neuron type of bladder dysfunction S3-Co (conus): sensory loss in saddle region lower neuron type of bladder dysfunction trophic changes in sacral region L2-S5 (cauda equine): flaccid palsy in legs sensory loss in legs, buttocks and saddle lancinating pain tension symptoms lower neuron bladder dysfunction B. The site of the lesion Anterior root: segmental flaccid palsy Posterior root: segmental sensory loss lancinating pain no reflexes tension symptoms Spinal nerve: segmental flaccid palsy segmental sensory loss lancinating pain tension symptoms 41 LECTURE VI SHORT REVIEW OF CRANIAL NERVES Fig.6.1. Cranial nerves (J. David Spence, MD) 42 The twelve pairs of cranial nerves are named so because they pass through various apertures in the cranial bones. Like the 31 pairs of spinal nerves, they are the part of the peripheral nervous system (PNS). Each cranial nerve has both a number, designated by a roman numeral, and a name. The numbers indicate the order, from anterior to posterior, in which the nerves arise from the brain. The names designate a nerve's distribution or function. Cranial nerves emerge from the nose (cranial nerve I), the eyes (cranial nerve II), the inner ear (cranial nerve VIII), the brainstem (cranial nerves III-XII), and the spinal cord (part of cranial nerve XI). Two cranial nerves, I (olfactory) and II (optic), contain only sensory axons and thus are called sensory nerves. The rest are mixed nerves because they contain axons of both sensory and motor neurons. The cell bodies of sensory neurons are located in ganglia outside the brain, whereas the cell bodies of motor neurons lie in nuclei within the brain. Cranial nerves III (oculomotor), IV (trochlear), VI (abducens), XI (accessory), and XII (hypoglossal) are mainly motor. While a few of their axons are sensory axons from muscle proprioceptors, most of their axons are motor neurons that innervate skeletal muscles. Cranial nerves III, VII, IX, and X include both somatic and autonomic motor axons. The somatic axons innervate skeletal muscles whereas the autonomic axons, which are the part of parasympathetic division, innervate glands, nonstriated muscles, and cardiac muscle. I. Olfactory nerve (sensory) Origin: Bipolar olfactory neurons in olfactory mucosa. Site where nerve leaves the brain or enters it: Olfactory bulb; Site of exit from the cranium: Cribriform plate ethmoid bone; Arises in olfactory mucosa, passes through foramina in the cribriform plate of the ethmoid bone, and ends in the olfactory bulb. The olfactory tract extends via two pathways to olfactory areas of cerebral cortex; Function: Smell; Clinical application: Loss of the sense of smell, called anosmia (partial loss of sense of smell called hemianosmia), may result from head injuries in which the cribriform plate of the ethmoid bone is fractured and from lesions along the olfactory pathway. Diseases involving the anterior temporal lobe and its base (intrinsic or extrinsic tumors), which may produce olfactory hallucinations (signs of irritation). Temporal lobe seizures may start with an olfactory aura. II. Optic nerve (sensory) (Fig.6.2). Origin: Ganglion of the retina; Site where nerve leaves the brain or enters it: Optic chiasma on base of brain; Site of exit from the cranium: Canalis opticus; Arises in the retina of the eye, passes through the optic foramen, forms the optic chiasm and then the optic tracts, and terminates in the lateral geniculate nuclei of thalamus. From the thalamus, axons extend to the primary visual area of the cerebral cortex; Function: Vision; Clinical application: Fractures in the orbit damage along the visual pathway, of the nervous system may result in visual field defects and loss of visual acuity. Amaurosis. It is partial or complete blindness. Hemianopia-absence of half of the normal field of vision. The commonest type is homonymous hemianopia, in which the same half (right or left) is lost in both eyes. Sometimes the inner halves of the visual field are lost in both eyes, producing a binasal hemianopia, while in others the outer halves are lost, producing a bitemporal hemianopia (Oxford Medical Dictionary, 2003). Result of irritation of visual cortex is visual hallucination. 43 Fig. 6.2. Anatomy & function of optic nerve III. Oculomotor nerve (mixed, mainly motor) Nuclei: a) nucleus of oculomotor nerve and nucleus (Yakubovich) and unaired median, which locates in a tegmentum pedunculi cerebri; Site where nerve leaves the brain or enters it: Median sulcus, cerebral peduncle, interpeduncular fossa; Site of exit from the cranium: Superior orbital fissure; Sensory portion: Consists of axons from proprioceptors in eyeball muscles that pass through the superior orbital fissure and terminate in the midbrain; Motor portion: Originates in the midbrain and passes through the superior orbital fissure. Axons of somatic motor neurons innervate the levator palpebrae superioris muscle of the upper eyelid and four extrinsic eyeball muscles (superior rectus, medial rectus, inferior rectus, and inferior oblique); Parasympathetic axons innervate the ciliary muscle of eyeball and the circular muscles (sphincter pupillae) of the iris; Function: Proprioception. Somatic motor function: Movement of upper eyelid and eyeball. Autonomic motor function (parasympathetic): accommodation of lens for near vision and constriction of pupil; Clinical application: Nerve damage causes strabismus divergent (a deviation of the eye in which both eyes do not fix on the same object), ptosis (drooping) of the upper eyelid, dilation of the pupil, movement of the eyeball downward and outward on the damaged side, loss of accommodation for near vision, and diplopia (double vision). IV. Trochlear nerve. (mixed, mainly motor) Nuclei: Nucleus of trochlear nerve, which locates in tegmentum pedunculi cerebri; Site where nerve leaves the brain or enters it: Dorsally, behind lamina quadrigemina, from superior medullary velum; Site of exit from the cranium: Superior orbital fissure; Sensory portion: Consists of axons from proprioceptors in the superior oblique muscles, which pass through the superior orbital fissure and terminate in the midbrain; 44 Motor portion: Originates in the midbrain and passes through the superior orbital fissure. Innervates the superior oblique muscle, an extrinsic eyeball muscle; Functions: Proprioception. Somatic motor function: Movement of the eyeball; Clinical application: In trochlear nerve paralysis diplopia and gaze downward strabismus occur. V. Trigeminal nerve (mixed). (Fig. 6.3, 6.4.). Nuclei: a) motor nucleus of trigeminal nerve (locates in upper part of pars dorsalis pontis; b) superior sensory nucleus of trigeminal nerve (same as that of previous nucleus, laterally of it); c) nucleus of spinal tract of trigeminal nerve (continuation of previous one along the length of medulla oblongata); d) mesencephalic nucleus of trigeminal nerve (tegmentum of cerebral peduncle lateral of aqueduct of midbrain); Site where nerve leaves the brain or enters in; Anteriad of middle cerebellar peduncle; Site of exit from the cranium: Ophthalmic nerve, superior orbital fissure, maxillary nerve – foramen rotundum, mandibular nerve – foramen ovale; Sensory portion: Consists of three branches, all of which end in the pons. The ophthalamic nerve contains axons from the skin over the upper eyelid, eyeball, lacrimal glands, nasal cavity, side of nose, forehead, and anterior half of scalp that pass through superior orbital fissure. The maxillary nerve contains axons from the mucosa of the nose, palate, parts of the pharynx, upper teeth, upper lip, and lower eyelid that pass through the foramen rotundum. The mandibullar nerve contains axons from the anterior two-thirds of the tongue (somatic sensory axons but not axons for the special sense of taste), the lower teeth, skin over mandible, cheek and mucosa deep to it, and side of head in front of ear that pass through the foramen ovale; Motor portion: It’s part of the mandibular branch, which originates in the pons, passes through the foramen ovale, and innervates muscles of mastication (masseter, temporal is, medial pterygoid, lateral pterygoid, anterior belly of digastric, and mylohyoid muscles); Functioins: Sensory: Conveys impulses for touch, pain, and temperature sensations and proprioception. Motor: Chewing; Clinical application: Neuralgia (pain) of one or more branches of the trigeminal nerve is called trigeminal neuralgia (tic douloureux). Injury of the mandibullar nerve may cause paralysis of the chewing muscles and a loss of the sensations of touch, temperature, and proprioception in the lower part of the face. “Trismus” is a tonic spasm of the masticatory muscles caused by acute encephalitic lesions in the pons, by rabies, by tetanus, or by other conditions. Because of the strong abnormal tension in these muscles, the patient is not able to open his mouth. Fig. 6.3. Anatomy of nucleus of III, IV, VI cranial nerves (Skoromets, 1995) 45 Fig. 6.4. Inervation of facial skin and head skin (Skoromets, 1995) VI. Abducens nerve (mixed, mainly motor) Nuclei: Nucleus of abducens nerve (locates in dorsal portion of pons, in region of facial colliculus); Site where nerve leaves the brain or enters in: posterior edge of pons in sulcus between pons and pyramid; Site of exit from the cranium: superior orbital fissure; Sensory portion: Consists of axons from proprioceptors in the lateral rectus muscle, which passes through the superior orbital fissure and end in the pons; Motor portion: Originates in the pons, passes through the superior orbital fissure, and innervates the lateral rectus muscle, an extrinsic eyeball muscle; Function: Proprioception. Movement of the eyeball; Clinical application: With damage to this nerve, the affected eyeball cannot move laterally beyond the midpoint, and the eye usually is directed medially. All three motor nerves of one eye are interrupted, the eye looks straight ahead and cannot be moved in any direction, and its pupil is wide and does not react to light (ophthalmoplegia totalis). Bilateral paralysis of the eye muscles is usually the result of the nuclear damage. The most frequent causes of nuclear paralysis are encephalitis, neurosyphilis, multiple sclerosis, circulatory condition, hemorrhages, and tumors. The most frequent causes of peripheral eye muscle palsies are meningitis, sinusitis, cavernous sinus thrombosis, aneurysm of internal carotid artery or posterior communicating artery, fractures, tumors of the cranial base as well as of the orbit, diphtheria, and botulism. VII. Facial nerve (mixed). (Fig.6.5, 6.6). Nuclei: a) nucleus of tractus solitaries; b) superior salivary nucleus (situate in dorsal portion of pons, reticular formation); Site where nerve leaves the brain or enters in: At the back of middle cerebellar peduncle; Site of exit from the cranium; Sensory portion: Arises from taste buds on the anterior two-thirds of the tongue, passes through the stylomastoid foramen and geniculate ganglion (located beside the facial nerve), and ends in the pons. From there, axons extend to the thalamus, and then to the gustatory areas of the cerebral cortex. Also contains axons from proprioceptors in muscles of the face and scalp; Motor portion: Originates in the pons and passes through the stylomastoid foramen. Axons of somatic motor neurons innervate facial, scalp, and neck muscles. Parasympathetic axons innervate lacrimal, sublingual, submandibular, nasal, and palatine glands. Sensory function: proprioception and taste; Somatic motor function: Facial expression; Autonomic motor function(parasympathetic): Secretion of saliva and tears; 46 Clinical application: Injury produces Bell´s palsy (paralysis of the facial muscles), loss of taste, decreased salivation, and loss of ability to close the eyes. Fig. 6.5. Left peripheral facial palsy (Rockham, Fig. 6.6. Anatomy of facial nerve (Rockham, 2004) 2004) VIII. Auditory nerve (mixed, mainly sensory) Nuclei: Ventral and dorsal cochlear nuclei medial, lateral superior and inferior vestibular nuclei (In region of lateral angle of rhomboid fossa (area vestibularis); Site where nerve leaves the brain or enters in: Lateral of facial nerve, on posterior edge of pons laterally of olive; Site of exit from the cranium: Porus acusticus internus. Vestibular nerve Sensory portion: Arises in the semicircular canals, saccule, and utricle and forms the vestibular ganglion. Axons end in the pons and cerebellum; Motor portion: Originates in the pons and terminates on hair cells of the semicircular canals, saccule, and utricle. Cochlear nerve, sensory portion: Arises in the spiral organ (organ of Corti), forms the spiral ganglion, passes through nuclei in the medulla, and ends in the thalamus. Axons synapse with thalamic neurons that relay impulses to the primary auditory area (areas 41 and 42) of the cerebral cortex. Cochlear nerve Motor portion: Originates in the pons and terminates on hair cells of the spiral organ; Function: Vestibular branch sensory function: Conveys impulses related to equilibrium. Vestibular branch motor function: Adjust sensitivity of hair cells. Cochlear branch sensory function: Conveys impulses for hearing. Cochlear branch motor function: Modifies function of hair cells by altering their response to sound waves; Clinical application: Injury to the vestibular branch may cause vertigo (a subjective feeling of rotation), ataxia (muscular incoordination and nystagmus (involuntary rapid movement of the eyeball). Injury to the cochlear branch may cause tinnitus (ringing in the ears) or deafness; IX. Glossopharyngeal nerve (mixed) Nuclei: a) nucleus tractus solitarius b) inferior salivary nucleus c) nucleus ambiguous. In medulla oblongata dorsally, in region of trigonum of vagal nerve as continuation of nucleus of this nerve b)cells of nucleus scattered in reticular formation of medulla oblongata between nucleus ambiguus and nucleus of olive c)reticular formation of medulla oblongata); Site where nerve leaves the brain or enters in: Lower than two previous ones, in superior posterolateral sulcus passing dorsally of olive; Site of exit from the cranium: Jugular foramen; 47 Sensory portion: Consists of axons from taste buds and somatic sensory receptors on posterior one-third of the tongue, from proprioceptors in swallowing muscles supplied by the motor portion, and from stretch receptors in carotid sinus and chemoreceptors in carotid body near the carotid arteries. Axons pass through the jugular foramen and end in the medulla; Motor portion: Originates in the medulla and passes through the jugular foramen. Axons of somatic motor neurons innervate the stylopharyngeus muscle, a muscle of pharynx that elevates the larynx during swallowing. Parasympathetic axons innervate the parotid (salivary) gland; Function: Sensory function: Taste and somatic sensation (touch, pain, temperature) from posterior third of tongue; proprioception in swallowing muscles; monitoring of blood pressure; monitoring of O2 and CO2 in blood for regulation of breathing rate and depth. Somatic motor function: Elevates the pharynx during swallowing and speech. Autonomic motor function (parasympathetic): Stimulates secretion of saliva; Clinical application: Injury causes difficulty in swallowing, reduced secretion of saliva, loss of sensation in the throat, and loss of taste sensation. X. Vagus nerve (mixed) Nuclei: a) nucleus of tractus solitarii b) dorsal nucleus of vagus nerve c) nucleus ambiguous. a) Region of vagal triangle in medulla oblongata; b) same region dorsally of previous one; c) reticular formation of medulla oblongata, deeper than dorsal nucleus of vagus nerve; Site where nerve leaves the brain or enters in: From same sulcus as glossopharyngeal nerve but more caudally of it; Site of exit from the cranium: jugular foramen; Sensory portion: Consists of axons from small number of taste buds in the epiglottis and pharynx, proprioceptors in muscles of the neck and throat, stretch receptors and chemoreceptors in carotid sinus and carotid body near the carotid arteries, chemoreceptors in aortic body near arch of the aorta, and visceral sensory receptors in most organs of the thoracic and abdominal cavities. Axons pass through the jugular foramen and end in the medulla and pons; Motor portion: Originates in medulla and passes through the jugular foramen. Axons of somatic motor neurons innervate skeletal muscles in the throat and neck. Parasympathetic axons innervate smooth muscle in the airways, esophagus, stomach, small intestine, most of large intestine, and gallbladder; cardiac muscle in the heart; and glands of the gastrointestinal (GI) tract; Sensory function: Taste and somatic sensations (touch, pain, temperature, and proprioception) from epiglottis and pharynx; monitoring of blood pressure; monitoring of O2 and CO2 in blood for regulation of breathing rate and depth; sensations from visceral organs in thorax and abdomen. Somatic motor function: Swallowing, coughing, and voice production; Autonomic motor function (parasympathetic): Smooth muscle contraction and relaxation in organs of the gastrointestinal tract; slowing of the heart rate; secretion of digestive fluids; Clinical application: Injury interrupts sensations from many organs in the thoracic and abdominal cavities, interferes with swallowing, paralyzes vocal cords, and causes heart rate to increase. XI. Accessory nerve (mixed, mainly motor) Nuclei: a) Nucleus ambiguous b) spinal nucleus of accessory nerve medulla oblongata as continuation of the nucleus of the same name in the IX and X pairs b) spinal cord, between anterior and posterior horns of grey matter); Site where nerve leaves the brain or enters in: Cranial roots from the same sulcus as vagus nerve, but more caudally spinal roots between anterior and posterior roots of cervical nerves, at level of segments C2 - C5 ; Site of exit from the cranium: Jugular foramen; Sensory portion: Consists of axons from proprioceptors in muscles of the pharynx, larynx, and soft palate that pass through the jugular foramen and end in the medulla; Motor portion: Consists of a cranial root and a spinal root. Cranial root arises in the medulla, passes through the jugular foramen, and supplies muscles of the pharynx, larynx, and soft palate. Spinal root originates in the anterior gray horn of the first five cervical segments of the spinal cord, 48 passes through the jugular foramen, and supplies the sternocleidomastoid and trapezius muscles Sensory function: Proprioception. Somatic motor function: Cranial part mediates swallowing movements; spinal part mediates movement of head and shoulders; Clinical application: If nerves are damaged, the sternocleidomastoid and trapezius muscles become paralyzed, with resulting inability to raise the shoulders and difficulty in turning the head. Irritation of in field of innervation may cause torticollis. XII. Hypoglossal (mixed, mainly motor) Nuclei: Nucleus of hypoglossal nerve (locates in medulla oblongata in hypoglossal triangle); Site where nerve leaves the brain or enters in: Anterolateral sulcus of medulla oblongata between pyramid and olive; Site of exit from the cranium: Anterior condylar canal; Sensory portion: Consists of axons from proprioceptors in tongue muscles that pass through the hypoglossal canal and end in the medulla; Motor portion: Originates in the medulla, passes through the hypoglossal canal, and supplies muscles of the tongue; Sensory function: Proprioception; Motor function: Movement of tongue during speech and swallowing; Clinical application: Injury results in difficulty in chewing, speaking, and curls toward the affected side, and the affected side atrophies. Glossoplegia - paralysis of the tongue. Hemiglossoplegia - paralysis of the half of tongue. 49 LECTURE VII CLINICAL ANATOMY OF THE BRAINSTEM The brain stem is a small, narrow region connecting the spinal cord with the rest of the brain. It lies ventral to the cerebellum, which it connects by the cerebellar peduncles. Its functions are critical to survival. The brain stem is densely packed with many vital structures such as long ascending and descending pathways that carry sensory and motor information to and from higher brain regions. It contains the nuclei of cranial nerves III through XII and their intramedullary fibers. In short, it is a complicated but highly organized structure that controls motor and sensory activities, respiration, cardiovascular functions, and mechanisms related to sleep and consciousness. The medulla (bulb) is the direct rostral extension of the spinal cord. It contains the nuclei of the lower cranial nerves (IX, X, XI, and XII) and the inferior olivary nucleus. The dorsal column pathways decussate in its central region to form the medial lemniscus, whereas the corticospinal tracts cross on the ventral side as they descend caudally. Together with the pons, the medulla also participates in vital autonomic functions such as digestion, respiration, and regulation of heart rate and blood pressure. The pons (bridge) lies rostral to the medulla and appears as a bulge mounting from the ventral surface of the brain stem. The pons contains nuclei for cranial nerves V, VI, VII, and VIII as well as a large number of neurons that relay information about movement from the frontal cerebral hemispheres to the cerebellum (frontopontocerebellar pathway). Other clinically pertinent pathways in the pons are those for the control of saccadic eye movements (medial longitudinal fasciculus [MLF]) and the auditory connections. The midbrain, the smallest and most rostral component of the brain stem, plays an important role in the control of eye movements and coordination of visual and auditory reflexes. It contains the nuclei for cranial nerves III and IV. Other important structures are the red nuclei and substantia nigra. The periaqueduct area has an important but poorly understood influence on consciousness and pain perception. Significant bilateral brain stem lesions produce altered mental status or coma As a consequence of the unique anatomic arrangements in the brain stem, a unilateral lesion within this structure often causes “alternating syndromes”, in which ipsilateral dysfunction of one or more cranial nerves is accompanied by hemiplegia and/or hemisensory loss on the contralateral body. Magnetic resonance imaging (MRI) is the examination of choice for suspected brain stem lesions. It provides a highly sensitive and noninvasive method of examine the posterior fossa. SYMPTOMS AND SIGNS OF BRAINSTEM LESIONS Double vision Nystagmus Vertigo Sympathetic dysfunction (Horner's Nausea syndrome) Incoordination Hearing loss Gait imbalance Dysphagia Numbness of the face Dysarthria Hoarseness Dysphonia Difficulties with swallowing and speaking Tongue deviation or atrophy Signs Paresis or dysesthesia of the face with Multiple cranial nerve dysfunctions contralateral motor or sensory deficits in Gaze palsies the body (crossed symptoms) Unilateral hemiparesis with ataxia The medulla is supplied by the vertebral arteries and their branches. Its blood supply may be further subdivided into two groups, the paramedian bulbar and the lateral bulbar arteries. The paramedian bulbar arteries are penetrating branches, mainly from the vertebral artery, that supply the midline structures of the medulla. At the lower medulla, branches from the anterior spinal artery 50 also contribute to this paramedian zone. The lateral portion of the medulla is supplied by the lateral bulbar branches of the vertebral artery or the posterior inferior cerebellar artery. The basilar artery is the principal supplier of the pons. It gives off three types of branches. The paramedian arteries supply the medial basal pons, including the pontine nuclei, corticospinal fibers, and medial lemniscus. The short circumferential arteries supply the lateral part of the pons and the middle and superior cerebellar peduncles. The long circumferential arteries with branches from the anterior inferior cerebellar and superior cerebellar arteries supply the pontine tegmentum and the dorsolateral quadrant of the pons. Arteries supplying the midbrain include branches of the superior cerebellar artery, posterior cerebral artery, posterior communicating artery, and anterior choroidal artery. Branches of these arteries, like those of the pons, can be grouped into paramedian arteries, which supply the midline structures, and the long and short circumferential arteries, which supply the dorsal and lateral midbrain. The central medullary area may be supplied by a single dominant anterior spinal artery. Occlusion of this vessel cause the bilateral infarction of the medial medulla, resulting in quadriplegia (with face sparing), complete paralysis of the tongue, and complete loss of position and vibratory sensation. The patient will be mute, but fully conscious. The lateral medullary (Wallenberg's) syndrome is caused by vertebral artery or posterior inferior cerebellar artery occlusion and results in the following signs: 1. Ipsilateral loss of pain and temperature sensation of the face (damage to descending spinal tract and nucleus of cranial nerve V) 2. Ipsilateral paralysis of palate, pharynx, and vocal cord (damage to nuclei or fibers of IX and X) with dysphagia and dysarthria 3. Ipsilateral Horner's syndrome (damage to descending sympathetic fibers) 4. Ipsilateral ataxia and dysmetria (damage to inferior cerebellar peduncle and cerebellum) 5. Contralateral loss of pain and temperature on the body (damage to spinothalamic tract) 6. Vertigo, nausea, vomiting, and nystagmus (damage to vestibular nuclei) Other signs and symptoms may include hiccups, diplopia, or unilateral posterior headache. The ventral pontine (Millard-Gubler) syndrome is caused by paramedian infarction of the pons and results in the following signs: 1. Ipsilateral paresis of the lateral rectus (damage to cranial nerve VI) with diplopia 2. Ipsilateral paresis of the upper and lower face (damage to cranial nerve VII) 3. Contralateral hemiplegia (damage to corticospinal tract) with sparing of the face The lower dorsal pontine (Foville's) syndrome is caused by lesions in the dorsal tegmentum of the lower pons, resulting in the following signs: 1. Ipsilateral paresis of the whole face (damage to nucleus and fibers of VII) 2. Ipsilateral horizontal gaze palsy (damage to paramedian pontine reticular formation and/or VI nucleus) 3. Contralateral hemiplegia (damage to corticospinal tract) with sparing of the face The upper dorsal pontine (Raymond-Cestan) syndrome is caused by obstruction of the long circumferential branches of the basilar artery and results in: 1. Ipsilateral ataxia and coarse intention tremor (damage to the superior and middle cerebellar peduncles) 2. Ipsilateral paralysis of muscles of mastication and sensory loss in face (damage to sensory and motor nuclei and tracts of V) 3. Contralateral loss of all sensory modalities in the body (damage to medial lemniscus and spinothalamic tract) 4. Contralateral hemiparesis of the face and body (damage to corticospinal tract) may occur with ventral extension of the lesion 5. Horizontal gaze palsy may occur, as in the lower dorsal pontine syndrome The upper dorsal pontine (Raymond-Cestan) syndrome is caused by obstruction of the long circumferential branches of the basilar artery and results in: 51 1. Ipsilateral ataxia and intention tremor (damage to the superior and middle cerebellar peduncles) 2. Ipsilateral paralysis of muscles of mastication and sensory loss in face (damage to sensory and motor nuclei and tracts of V) 3. Contralateral loss of all sensory modalities in the body (damage to medial lemniscus and spinothalamic tract) 4. Contralateral hemiparesis of the face and body (damage to corticospinal tract) may occur with ventral extension of the lesion. 5. Horizontal gaze palsy may occur. The ventral midbrain (Weber's) syndrome is caused by occlusion of median and paramedian perforating branches and may result in: 1. Ipsilateral oculomotor paresis, ptosis, and dilated pupil (damage to fascicle of cranial nerve III, including parasympathetic fibers) 2. Contralateral hemiplegia, including the lower face (damage to corticospinal and corticobulbar tracts) The dorsal midbrain (Benedikt's) syndrome results from a lesion in the midbrain tegmentum caused by occlusion of paramedian branches of the basilar or posterior cerebral arteries or both. Its signs are: 1. Ipsilateral oculomotor paresis, ptosis, and dilated pupil (damage to fascicle of cranial nerve III, including parasympathetic fibers as in Weber's syndrome). 2. Contralateral involuntary movements, such as intention tremor, ataxia, and chorea (damage to red nucleus). 3. Contralateral hemiparesis may be present if the lesion extends ventrally. 4. Contralateral hemianesthesia may be present if the lesion extends laterally, affecting the spinothalamic tract and medial lemniscus The dorsolateral midbrain syndrome is caused by infarction of the circumferential arteries and results in: 1. Ipsilateral Horner's syndrome (damage to sympathetic tract) 2. Ipsilateral severe tremor that may be present at rest and grossly worsened by attempted movement (damage to superior cerebellar peduncle prior to crossing to the opposite red nucleus). Tremor and ataxia can be present bilaterally if both the superior and cerebellar peduncle and red nucleus are affected. 3. Contralateral loss of all sensory modalities (damage to spinothalamic tract and medial lemniscus that now ascend together). The “locked-in syndrome” occurs in patients with bilateral ventral pontine lesions. Its most common cause is pontine infarction, pontine hemorrhage, trauma, tumor, and encephalitis. The patient is quadriplegic because of bilateral damage of the corticospinal tracts in the ventral pons. The patients can to speak and cannon of facial movement because the corticobulbar tracts are damaged. Horizontal eye movements are also limited by the bilateral involvement of the nuclei and fibers of trochlear nerve. Consciousness is preserved because the reticular formation is not damaged. The patient has intact vertical eye movements and blinking because the supranuclear ocular motor pathways that run dorsally are spared. The patient is able to communicate by movement of the eyelids. Parinaud syndrome. It’s also known as the dorsal midbrain or collicular syndrome. The lesion is in the rostral dorsal midbrain, damaging the superior colliculi and pretectal structures. It may be caused by stroke, hemorrhage, trauma, hydrocephalus, or multiple sclerosis. Its signs are: 1. Patients report difficulty in looking up and blurring of distant vision. 2. Paralysis of upgaze and accommodation but sparing of other eye movements 3. Normal-to-large pupils with light-near dissociation (loss of pupillary reflex to light with preservation of pupilloconstriction in response to convergence) 4. Eyelid retraction 52 5. Convergence-retraction nystagmus (eyes make convergent and retracting oscillations following an upward saccade) Jackson syndrome. It’s paralysis of structures innervated by the tenth, eleventh, and twelfth cranial nerves, including the soft palate, larynx, half of the tongue, and the sternomastoid and trapezius muscles. It’s caused by occlusion of the vertebral artery. Its signs are: 1. Paralysis of the soft palate and vocal cords on one side which cause dysphagia and dysphonia 2. Loss of pain sensation and temperature sense on the other side. 3. Horner's syndrome may be associated. Avellise syndrome. It usually results from occlusion of the vertebral artery. Its signs are: 1. Paralysis of the soft palate and vocal cords on one side which cause dysphagia and dysphonia 2. Loss of pain sensation and temperature sense on the other side, including the extremities, trunk, and neck. 3. Horner's syndrome may be associated. 4. In the original description, the vagus and glossopharyngeal nerves were involved; concomitant involvement of the neighbouring cranial nerves was observed later. Bulbar palsy is a syndrome of lower motor neuron paralysis, affecting muscles innervated by cranial nerves (mainly IX-XII) that have their nuclei closely approximated in the lower brain stem. Muscles of the face, palate, pharynx, larynx, sternocleidomastoid, upper trapezius, and tongue are usually affected. Patients may present clinically with dysarthria, dysphagia, hoarseness, nasal voice, palatal deviation, diminished gag reflex, or weakness of the sternocleidomastoid, upper trapezius, or tongue. The main causes are brain stem infarct, syringobulbia, glioma, poliomyelitis, encephalitis, and motor neuron disease (amyotrophic lateral sclerosis or progressive bulbar palsy), tumors, chronic meningitis, aneurysms, neck trauma, and congenital abnormalities (Chiari malformation or basilar impression). Pseudobulbar palsy is a syndrome of upper motor neuron paralysis that affects the corticobulbar system above the brain stem bilaterally. Although it presents with most of the signs and symptoms of bulbar palsy, the causative lesion is not in the brain stem. This condition causes dysphagia, dysarthria, and paresis of the tongue (without atrophy or fasciculations). The reflex movements of the soft palate and pharynx are frequently hyperactive (incontrast to bulbar palsy). Frontal signs (grasp, snout, suck, and glabellar reflex) may be present. Emotional incontinence with exaggerated crying (or, less often, laughing) is also common and may be due to disruption of frontal efferents subserving emotional expression. The main causes are multiple lacunar infarcts or chronic ischemia in the hemispheres. Other causes are ALS and multiple sclerosis. The examination of comatose patients with brainstem dysfunction include next items: 1. Mental status 2. Breathing 3. Pupillary size and light response 4. Spontaneous eye movement or deviation 5. Oculocephalic reflex on head turning (doll's eye movement) 6. Oculovestibular test of gaze response to ice-water calorics 7. Motor response to supraorbital nerve pressure (noxious stimulus) 8. Presence of other brain stem reflexes (corneal, gag, and ciliospinal) Brain death is a clinical diagnosis of cessation of all cerebral and brain stem function. Its signs are: 1. All brain stem reflexes (corneal, pupillary, gag, ciliospinal) are absent. 2. The pupils are midposition or large and fixed. 3. Oculocephalic and oculovestibular reflexes are absent. 53 4. Muscle tone is flaccid, with no spontaneous facial movement and no motor response to stimuli. This condition should be present for 6-24 hours in adults. Metabolic causes (hypothermia, hypotension) and drug effects (neuromuscular blockers, sedative drugs) need to be ruled out. VOLUNTARY AND REFLEX INNERVATION OF THE EYE MUSCLES The extremely precise cooperation among the individual ocular muscles that move the eye charge of ocular movements. Such intimate connections are provided by the medial longitudinal fasciculus, which runs bilaterally parallel to the midline from the tegmentum of the midbrain down to the cervical cord. It interconnects the nuclei of the motor nerves of the eye muscles. It also receives impulses from the cervical cord (serving anterior and posterior neck muscles), from the nuclei of the vestibular nerves, from the reticular formation controlling pontine and mesencephalic “centers of vision”, and from cerebral cortex and basal ganglia. The eyes can be moved both voluntarily and by reflex. They can, however, move only jointly – in other words, in conjugation (Fig.). In whatever direction the eyes move, all eye muscles participate in the action, in part by increasing muscular tension (agonists), in part by relaxation (antagonists). When looking voluntarily at an object, the eyes perform very fast jerking and most precise movements (saccades). Most eye movements take place by reflex, however, and are not voluntary. Any object entering the field of vision attracts attention, and vision is involuntarily directed to it. As the object moves, the eye follows involuntarily in an attempt to keep the image of the object continuously in the area of most acute vision, the fovea of both maculae. If we voluntarily focus on an object of interest, the eye is automatically kept on it, even if we as well as the object of interest are moving. Thus, all voluntary eye movements are appended by involuntary reflex movements. This reflex (holding the image of the object of interest in the retinal area of most acute vision) is called the fixation reflex. The afferent portion of this reflex runs from the retina over the visual pathway to the visual cortex (area 17). Then the impulses are transmitted to areas 18 and 19. The efferent fibers probably originate in these areas and temporarily join the optic radiation on their course to contralateral mesencephalic and pontine centers of oculomotion From there they join the corresponding nuclei of the ocular motor nerves. It is likely that some of the efferent fibers go directly to the ocular motor centers and the rest do so indirectly, making a detour over Brodmann's area 8. Special components of the reticular formation contained in the anterior portion of the midbrain regulate individual directions of vision. E.g. the nucleus of the posterior commissure – downward movements, and the interstitial Cajal's nucleus and Darkschewitsch's nucleus – rotatory movements of the eyes. Segments of the superior colliculi can also produce eye movements in certain directions. Upward movements are represented at the anterior margin of the superior colliculi. Destruction of this area produces paralysis of upward gaze (Parinaud's syndrome). Impulses originating at the convexity of the occipital lobes also travel to contralateral pontine centers for eye movement and produce conjugate lateral movements of the eyes. Voluntary eye movements are triggered in the frontal eye field of Brodmann's area 8, located in front of the precentral gyrus, and perhaps also in parts of areas 6 and 9. A conjugate movement of the eyes (deviation conjugué) toward the opposite side (the patient looks away from the side of irritation) is the most frequent response to stimulation in this territory. The movement of the eyes is sometimes accompanied by a movement of the head toward the opposite side. Unilateral destruction of area 8 creates a predominance of the contralateral area, producing a conjugate movement toward the side of the lesion (the patient looks towards the paralyzing focus). This deviation abates with time. The situation is reversed with pontine lesions, because the corticopontine pathways cross. A pontine paralysis of gaze is seldom followed by full recovery. It is not quite clear how the frontal eye fields are connected with the nuclei for ocular motion. The fibers accompany the corticonuclear tract on its way to the internal capsule and cerebral 54 peduncle. They do not terminate directly in the nuclei of the cranial nerves, however. It appears that their impulses arrive at the nuclei via intercalated neurons in the reticular formation and via the medial longitudinal fasciculus. All voluntary movements of the eyes are under the influence of reflex arcs. Some of these arcs belong to the optical and others to the acoustic, vestibular, and proprioceptive reflex arcs (originating in ventral and dorsal muscles of the neck and transmitted via the spinotectal tract and the medial longitudinal fasciculus). After unilateral destruction of the frontal eye field, the eyes for a time cannot be turned voluntarily to the opposite side, but such movement is still possible by reflex action. The patient is able to pursue with his eyes an object that moves slowly through his field of vision even if he is not able to follow its direction voluntarily (pursuit reflex). In contrast, if the occipital fields are destroyed, the reflex movements of the eyes are abolished. The patient can move his eyes voluntarily in every direction, but he cannot pursue an object. It immediately escapes from the area of highest acuity and must be searched for again by voluntary eye movements. LECTURE VIII CEREBRAL CORTEX 55 Fig. 8.1Functional and Structural Areas of the Cerebral Cortex (L. Hendon, University of Alabama, 2005) The cerebral cortex, the thin, gray covering of both hemispheres of the brain consists of two types: the neocortex (90%) and the allocortex (10%). The neocortex consists in six layers. I. Lamina zonalis, or the molecularlayer or plexiform layer, is the most superficial. II. Lamina granularis externa, or the external granular layer of small pyramidal cells, consists of many small, closely packed pyramidal cells. III. Lamina pyramidalis, or the external pyramidal layer. It gives rise to association and commissural fibers and is the major source of corticocortical fibers. IV. Lamina granularis interna, or the internal granular layer is characterized by the presence of a large number of small multipolar cells with short axons, among which are some small pyramidal cells. V. Lamina ganglionaris, or the internal pyramidal layer of medium-sized and large pyramidal cells, contains the largest cells of the cortex. In the motor region these are known as the giant pyramidal cells of Betz., which gives rise to corticobulbar and corticospinal fibers. VI. Lamina multiformis or the layer of polymorphic cells. It gives rise to projection, commissural, and association fibers. Fissures – deep grooves – separate major regions of the brain. Transverse fissure – separates cerebrum and cerebellum. Longitudinal fissure – separates cerebral hemispheres. Sulci – grooves on the surface of the cerebral hemispheres. Gyri – twisted ridges between sulci. Prominent gyri and sulci are similar in all people. Deeper sulci divide cerebrum into lobes. Lobes are named for the skull bones overlying them. The two hemispheres are connected by commissural fibers, which enable bihemispheric coordination of function. The most important commissural tract is the corpus callosum; because many tasks are performed primarily by one of the two hemispheres (cerebral dominance), interruption of the corpus callosum can produce various disconnection syndromes. Total callosal transection causes splitbrain syndrome, in which the patient cannot name an object felt by the left hand when the eyes are closed, or one seen in the left visual hemifield (tactile and optic anomia), and cannot read words projected into the left visual hemifield (left hemialexia), write with the left hand (left hemiagraphia), or make pantomimic movements with the left hand (left hemiapraxia). Anterior callosal lesions cause alien hand syndrome (diagonistic apraxia), in which the patient 56 cannot coordinate the movements of the two hands. Disconnection syndromes are usually not seen in persons with congenital absence (agenesis) of the corpus callosum. The functional organization of the cerebral cortex can be studied with various techniques: direct electrical stimulation of the cortex during neurosurgical procedures, measurement of cortical electrical cortical activity (electroencephalography and evoked potentials), and measurement of regional cerebral blood flow and metabolic activity. Highly specialized areas for particular functions are found in many different parts of the brain. A lesion in one such area may produce a severe functional deficit, though partial or total recovery often occurs because adjacent uninjured areas may take over some of the function of the lost brain tissue. (The extent to which actual brain regeneration may aid functional recovery is currently unclear.) The specific anatomic patterns of functional localization in the brain are the key to understanding much of clinical neurology LESIONS OF THE FRONTAL LOBE The motor and premotor function. Primary motor cortex (somatic motor area) are located in precentral gyrus. This region includes the giant pyramidal cells of Betz in layer V; at this site the gray matter is of maximum thickness. The motor area gives rise to impulses that initiate volitional movements on the opposite side of the body. It is subdivided into centers; each of these preferentially controls muscles that govern movements of individual parts of the opposite half of the body. It is somatotopically organized. These are represented in inverted order. Destruction of this area caused paresis or paralysis of the opposite side of the body. This paralysis affects predominantly the distal portions of the extremities, and fine, skilled volitional movements are entirely abolished. Because the larynx, pharynx, palate, trunk muscles, diaphragm, rectum, and bladder are bilaterally innervated, the functions of these structures are little affected with unilateral lesions. The premotor locates anteriorly of the precentral gyrus and effects opposite half of the body motor control. It involved in the planning of movements. Irritation of the motor (and/or pre-motor) cortex causes focal or jacksonian convulsions. The frontal motor eye field. Lies anteriad the premotor cortex and controls voluntary movement of the eyes, especially when moving eyes to follow a moving target. Stimulation of this region results strong, rapid conjugate deviation of the eyes to the opposite side, which may be accompanied by conjugate movement of the head and rotation of the trunk. Destruction of this area is followed by paresis of conjugate gaze to the opposite side. The motor speech areas. The lower portion of the motor and premotor region is known as Broca's area, or the motor speech area. Destructive lesions of this region produce an oral expressive type of aphasia. Destruction of the anterior two-thirds of the frontal lobe convexity results in deficits in the following functions: concentration, orientation, abstracting ability, loss of initiative, inappropriative behavior, release of grasping reflexes, gait apraxia and sphicteric incontinenced. LESIONS OF PARIETAL LOBE The postcentral region occupies the postcentral gyrus and is stretch from the superomedial border to the adjoining part of the paracentral lobule. There is the typical sensory cortex with all well developed six layers. The postcentral region is the sensory receptive area. It receives information from the nuclei ventralis posterolateralis and posteromedialis of the lateral nuclear mass of the thalamus. These relay impulses from the spinothalamic tracts, medial lemnisci, and secondary trigeminal tracts, and traverse the posterior limb of the internal capsule. The functions of the parietal lobe are analysis, synthesis, integration, interpretation, and elaboration of the primary sensory impulses that are received from the thalamus. The sensory cortex is somatotopically organized too. Destruction of this area results in contralateral hemihypestesia and astereognosis. Stimulation of this area by either artificial excitation or disease processes produces paresthesias on the opposite side of the body (sensory jacksonian epilepsy). The superior parietal lobule. Destruction of this lobule results in contralateral astereognosis and sensory neglect. The angular and supramarginal gyri of the dominant hemisphere are important in relation to language and related functions, and lesions in these areas may be responsible for various types of 57 receptive aphasia, alexia, acalculia, and sensory apraxia. Destruction of nondominant hemisphere result autotopagnosia or somatotopagnosia (the loss of power to orient the body or the relation of its individual parts; there may be loss of identification of one limb or one part of the body), anosognosia (the ignorance of the existence of disease), pseudomelia (a sensation of presence or absence of additional extremities). LESIONS OF THE TEMPORAL LOBES The auditory receptive region is located in the transverse temporal gyri (Heschl's convolutions), which lie on the dorsal surface of the posterior part of the superior temporal convolution. The auditory radiations pass from the medial geniculate body to the auditory receptive region. Hearing is bilaterally represented in the temporal lobes, although a greater number of impulses may be received from the contralateral ear. Stimulation of the superior temporal gyrus produces vague auditory hallucinations in the form of tinnitus and sensations of roaring and buzzing, and stimulation of adjacent areas causes vertigo and a sensation of unsteadiness. Unilateral destruction of the transverse temporal gyri does not cause deafness (because of bilateral representation of hearing. Destruction of Wernicke’s speech area in the dominant hemisphere (posterior part of the superior temporal gyrus) results in a receptive aphasia (Wernicke’s aphasia), in which patient cannot understand any form of language. Speech is spontaneous, fluent, and rapid but makes little sense. The optic radiations pass through the temporal lobe and curve around the descending horn of the lateral ventricle; lesion of them may cause either a superior quadrantic or hemianopic defect in the visual fields. Destruction of olfactory tract results in ipsilateral anosmia. The stimulation of the temporal lobe cortex in epileptic patients gives rise to illusions of perception, olfactory, visual and gustatory hallucinations, dreamy states and reminiscences and automatisms. Petit mal is a typical symptom of temporal lobe lesion. These phenomena have been found to be associated with abnormal discharges or pathologic lesions of the anterior and medial portions of the temporal lobes, including the hippocampal gyrus, uncus, amygdaloid complex, and hippocampus, or the subcortical connections of these structures, many of which actually belong to the limbic system. Hippocampal cortex (archicortex). Bilateral lesion result in the inability to consolidate short-term memory into long-term memory; earlier memories are retrievable. Olfactory and gustatory hallucination are results of the uncus irritative lesion. LESIONS OF THE OCCIPITAL LOBE. The occipital lobe is more nearly a structural and functional entity than are any of the other cerebral lobes. All of its functions are concerned either directly or indirectly with vision. The visual receptive area is located on the lips of the calcarine fissure and adjacent portions of the cuneus and lingual gyrus, and extends around the occipital pole to occupy a portion of the lateral surface of the hemisphere. The optic radiations pass from the lateral geniculate body to the striate cortex on the upper and lower lips of the calcarine fissure. Stimulation, or irritation, of the calcarine cortex produces unformed visual hallucinations, such as fotomas and flashes of light, in the corresponding fields of vision. Destructive lesions result in defects in the visual fields supplied by the affected areas. Bilateral lesion may result in cortical blindness. Unilateral lesions may resulting contralateral hemianopia or quadrantanopia. LESIONS OF THE LIMBIC LOBES The hippocampal gyrus, uncus, isthmus, and gyrus cinguli are usually grouped together as the limbic lobe or limbic system. Closely related are the subcallosal and retrosplenial gyri, pyriform area, hippocampus, and various subcortical structures including the amygdala and septal nuclei. Certain of these are often included in the temporal lobe, but anatomically and physiologically they are placed in the limbic system, or "visceral brain." Irritation, or stimulation, of these produces either olfactory or gustatory hallucinations. These are often very disagreeable and are described with difficulty. For example, the patient may describe the taste of blood, the odor of burning rubber, or of decaying material. The hallucinations may be accompanied by smacking or licking of the lips, tasting movements of the tongue, swallowing, and salivation, and constitute an important part of the 58 complex partial seizure. Destruction of these areas is not followed by loss of smell or taste because of their bilateral connections. The limbic lobe and related structures have rich connections with the hypothalamus and thalamus, and play an important part in the central regulation of the autonomic nervous system. Abnormal affective and emotional responses, fear and aggressive behavior may be lessened by interruption of the connections between these cortical areas and the thalamus and hypothalamus. Bilateral or even unilateral lesions or resection of the hippocampus and hippocampal gyrus are followed by marked impairment of recent memory. Bilateral lesions of the cingulate gyrus cause apathy, akinesia, and mutism. HIGHER CORTICAL FUNCTIONS This section concerns the more important higher cortical functions and the typical clinical findings associated with their impairment. An adequate understanding of these very complex functions requires knowledge of certain basic concepts of neuropsychology and neuropsychological testing, which will be briefly explained where necessary. We will discuss language, aspects of perception, the planning of complex patterns of movement and motor activities, and the control of social behavior. These functions are mostly subserved by the multimodal association cortices, which make up more than half of the brain surface and which receive afferent input from the primary somatosensory, special sensory, and motor cortices, the mediodorsal and lateroposterior pulvinar portions of the thalamus, and other association areas in both hemispheres. Apraxia. It is inability to execute purposeful, previously learned motor tasks, despite physical ability and willingness, as a result of brain damage. Diagnosis is clinical, often including neuropsychologic testing, with brain imaging (e.g., CT, MRI) to identify cause. Prognosis depends on the cause and extent of damage and patient age. There is no specific treatment, but physical and occupational therapy may modestly improve functioning and patient safety. Apraxia results from brain damage (e.g., by infarct, tumor, or trauma) or degeneration, usually in the parietal lobes or their connections, which retain memories of learned movement patterns. Less commonly, apraxia results from damage to other areas of the brain, such as the premotor cortex (the part of the frontal lobe anterior to the motor cortex), other parts of the frontal lobe, or the corpus callosum, or from diffuse damage related to degenerative dementias. Patients cannot conceptualize or do learned complex motor tasks despite an ability to do the individual component movements. For example, patients with constructional apraxia may be unable to copy a simple geometric shape despite being able to see and recognize the stimulus, hold and use a pen, and understand the task. Typically, patients do not recognize their deficits. Tests include asking patients to do or imitate common learned tasks (e.g., saluting, stopping or starting to walk, combing hair, striking and blowing out a match, opening a lock with a key, using a screwdriver or scissors, taking a deep breath and holding it). Amnesia. It is inability to identify an object using one or more of the senses. Agnosias are uncommon. They result from damage to (e.g., by infarct, tumor, trauma) or degeneration of areas of the brain that integrate perception, memory, and identification. Typically, only one sense is affected. Examples are hearing (auditory amnesia, the inability to identify objects through sound such as a ringing telephone), taste (gustatory amnesia), smell (olfactory amnesia), touch (tactile amnesia), and sight (visual amnesia). Other forms of amnesia involve very specific and complex processes within one sense. For example, prosopagnosia is inability to identify well-known faces, including those of close friends, or to otherwise distinguish individual objects among a class of objects, despite the ability to identify generic facial features and objects. Anosognosia often accompanies damage to the right, nondominant parietal lobe. Patients deny their deficit, insisting that nothing is wrong even when one side of their body is completely paralyzed. When shown the paralyzed body part, patients may deny that it is theirs. In an often 59 related phenomenon, patients ignore the paralyzed or desensitized body parts (hemi-inattention) or the space around them (hemineglect). Hemineglect most often involves the left side of the body. Occipitotemporal lesions may cause an inability to recognize familiar places (environmental agnosia), visual disturbances (visual agnosia), or color blindness (achromatopsia). Right-sided temporal lesions may cause an inability to interpret sounds (auditory agnosia) or impaired music perception (amusia). At bedside, patients are asked to identify common objects through sight, touch, or another sense. If hemineglect is suspected, patients are asked to identify the paralyzed parts of their body or objects in their hemivisual fields. Aphasia. It is language dysfunction that may involve impaired comprehension or expression of words or nonverbal equivalents of words. It results from dysfunction of the language centers in the cerebral cortex and basal ganglia or of the white matter pathways that connect them. Language function resides predominantly in the following: Poster superior temporal lobe, which contains Bernice’s area, adjacent inferior parietal lobe, poster inferior part of the frontal lobe just anterior to the motor cortex (which contains Boca’s area), sub cortical connection between those regions— usually in the left hemisphere, even in left-handed people. Aphasia is distinct from developmental disorders of language and from dysfunction of the motor pathways and muscles that produce speech (dysarthria). Receptive (sensory, fluent, or Wernicke's) aphasia: patients cannot comprehend words or recognize auditory, visual, or tactile symbols. It is caused by a disorder of the posterosuperior temporal gyrus of the language-dominant hemisphere (Wernicke's area). Often, alexia (loss of the ability to read words) is also present. Patients speak normal words fluently, often including meaningless phonemes, but do not know their meaning or relationships. The result is a jumble of words or “word salad.” Patients are typically unaware that their speech is incomprehensible to others. A right visual field cut commonly accompanies Wernicke's aphasia because the visual pathway is near the affected area. Expressive (motor, nonfluent, or Broca's) aphasia: The ability to create words is impaired, but comprehension and ability to conceptualize are relatively preserved. It is due to a disorder that affects the dominant left frontal or frontoparietal area, including Broca's area. It often causes agraphia (loss of the ability to write) and impairs oral reading. Patients can comprehend and conceptualize relatively well, but their ability to form words is impaired. Usually, the impairment affects speech production and writing (agraphia, dysgraphia), Broca's aphasia may include anomia (inability to name objects). 60 LECTURE IX AUTONOMIC NERVOUS SYSTEM The autonomic nervous system (ANS) regulates physiologic, metabolic processes and functions of internal organs (blood vessels, sweat glands, and salivary and lachrymal glands). ANS realize its functions independently of consciousness. It consists in two major parts: the sympathetic and parasympathetic systems. According to the anatomy it divides into central part, which include segmental level (limbic system, hypothalamus, reticular formation) and segmental level and peripheral part (all the other structures). Each peripheral division of the autonomic nervous system is characterized by a two-neuron chain and consists of two anatomic elements: the preganglionic neuron terminates in a peripheral ganglion, and the post-ganglionic neuron, which carries impulses to their destination in the viscera. The sympathetic and parasympathetic systems each consist of two types of nerve cells: one of them sits in the CNS and connects to cell in ganglia, which locate outside the CNS. Efferent fibers from the ganglia (postganglionic fibers) lead to effector organs. The preganglionic cell bodies of the sympathetic system are located in the intermediolateral horn of the spinal cord between T1 and L2 or L3. The sympathetic ganglia are adjacent to the spine and consist of the vertebral (sympathetic chain) and prevertebral ganglia, including the superior cervical, celiac, superior mesenteric, and aorticorenal ganglia. Long fibers from these ganglia pass to effector organs, including the smooth muscle of blood vessels, viscera, lungs, scalp (piloerector muscles), and pupils; the heart; and glands (sweat, salivary, and digestive). The preganglionic cell bodies of the parasympathetic system are located in the brain stem and sacral portion of the spinal cord. Preganglionic fibers exit the brain stem with the 3rd, 7th, 9th, and 10th cranial nerves. Parasympathetic ganglia are located within the effector organs, and postganglionic fibers are only 1 or 2 mm long. Thus, the parasympathetic system can produce specific, localized responses in effector organs, including blood vessels of the head, neck, and thoracoabdominal viscera; lacrimal and salivary glands; smooth muscle of viscera and glands (liver, spleen, colon, kidneys, bladder, genitals); and ocular muscles. The ANS activity CNS regulate by the hypothalamus, nucleus of the solitary tract, reticular formation, amygdala, hippocampus, and olfactory cortex. Physiology The ANS controls BP, heart rate, body temperature, weight, digestion, metabolism, fluid and electrolyte balance, sweating, urination, defecation, sexual response, and other processes. Many organs are controlled by either the sympathetic or parasympathetic system (although they may receive input from both, e.g., sympathetic input increases heart rate; parasympathetic decreases it). The sympathetic nervous system is catabolic. It increases heart rate and contractility, bronchodilation, hepatic glycogenolysis and glucose release, and muscular strength; it also causes sweaty palms. Less immediately life-preserving functions (e.g., digestion, renal filtration) are decreased. The parasympathetic nervous system is anabolic. Gastrointestinal secretions and motility (including evacuation) are stimulated, heart rate is slowed, and blood pressure decreases. Two major neurotransmitters in the ANS are acetylcholine and nor epinephrine. Fibers that secrete acetylcholine are termed cholinergic; they include all preganglionic fibers and all postganglionic parasympathetic fibers. Fibers that secrete norepinephrine are termed adrenergic; they include most postganglionic sympathetic fibers, except for those that innervate piloerectors, sweat glands, and blood vessels, which are cholinergic. Central Regulation of Autonomic Function The peripheral autonomic nervous system is under the control of higher centers at all levels of neuronal integration. The anatomy and physiology of the autonomic nervous system and its disturbances of function cannot be discussed without consideration of those centers in the cerebral 61 cortex, hypothalamus, midbrain, brain stem, and spinal cord that regulate and influence the function of its peripheral components. The Hypothalamus The hypothalamus is composed of numerous nerve cells, which arranged into six nuclear groups: 1. The preoptic region lies above and anterior to the optic chiasm and below the anterior commissure. It contains the medial and lateral preoptic areas. 2. The anterior group of nuclei, or rostral or supraoptic middle region, lies above the optic chiasm and is continuous anteriorly with the preoptic region. 3. The middle group, or tuberal or infundibular middle region, occupies the middle portion of the tuber cinereum. It is composed of the dorsomedial hypothalamic nucleus, the ventromedial hypothalamic nucleus, the dorsal hypothalamic area, the posterior hypothalamic area, and the perifornical area. 4. The lateral group, or region, occupies the lateral part of the tuber cinereum and includes both the lateral hypothalamic area and the nuclei tuberis lateralis. 5. The posterior group, or caudal or mammillary region, includes the premammillary area, the supramammillary area, and the mammillary bodies, containing the medial and lateral mammillary nuclei and the nucleus intercalatus. 6. The periventricular region contains many cellular masses that form the substantia grisea centralis. Included in this area are the nucleus periventricularis preopticus and the nucleus periventricularis arcuatus. Under control of the hypothalamus are body temperature regulation; basal metabolism; water, glucose, and fat metabolism; cardiovascular regulation including adjustment of the blood pressure and circulation; control of respiration; regulation of bladder functions; influence over sexual activity; and endocrine correlation in general. Vasopressin and oxytonin originate in the neurohypophysis, the supraoptic and paraventricular nuclei. Corticotropin releasing factor originates mainly from the paraventricular nucleus. Gonadotropin-releasing hormone is produced in the arcuate nucleus, as is prolactin-releasing factor. Growth hormone releasing factor and somatostatin (inhibits release of growth hormone) is synthesized in the posterior arcuate, ventromedian, premammillary, periventricular, and paraventricular parts of the hypothalamus. Thyrotropin-releasing factor is produced by many hypothalamic nuclei, except for those in its posterior portion. The Cortex The hypothalamus receives communications, either directly or indirectly, from various portions of the cerebral cortex. Both experimental and clinical evidence indicates that these cortical areas comprise a suprasegmental level for the integration of autonomic functions and the maintenance of a constant internal environment for the body. The term "visceral brain" has been applied to the limbic system. Authorities differ as to just how many structures are included in the so-called limbic system. The limbic lobe, or gyrus fornicatus, is composed of the cingulated gyrus, isthmus, hippocampal gyms, and uncus, but closely related are the subcallosal and retrosplenial gyri, pyriform area, hippocampus, and various subcortical structures including the amygdala and septal nuclei. The insula, medial portion of the temporal lobe, and medial and posterior orbital gyri are also closely allied, although not actually a part of the limbic system. The hypothalamus receives discharges from all these structures, as well as from certain frontal and temporal lobe areas. No separate cortical centers for parasympathetic and sympathetic control have been established with certainty, and the character of the reaction that follows either stimulation or destruction of these areas is dependent upon the general physiologic state of the organism. The anatomic pathways responsible for these reactions are not precisely known. For the most part, perhaps, the impulses are relayed to the hypothalamus, either directly or indirectly through the 62 thalamus, but there may also be projection pathways to the autonomic centers in the brain stem and spinal cord that travel in the lateral columns in close relationship with the corticospinal pathways. The sensory portions of the cerebral cortex play a part in relaying impulses to the motor areas; it is well known that visual, auditory, and other stimuli that call forth emotional responses may cause variations in autonomic reactivity with changes in circulatory and respiratory function, bladder disturbances, either sweating or anhidrosis, and pupillary dilation. The Midbrain and Brain Stem There are some important centers beside cranial nerves nuclei in the brain stem: a vasomotor center that exerts an influence in vasodilation and vasoconstriction and regulates blood; a heart rate regulating center; a respiratory reflex center. These are probably situated in the reticular formation of the medulla near the floor of the fourth ventricle in close association with the dorsal efferent nucleus of the vagus nerve. Examination of Patients History Symptoms suggesting autonomic dysfunction include orthostatic hypotension, heat intolerance, and loss of bladder and bowel control. Erectile dysfunction is an early symptom. Other possible symptoms include dry eyes and dry mouth, but they are nonspecific. Physical examination. Valuable information about the functional state of the autonomic nervous system may be obtained from the general observation of the patient. The habitus, body build, state of nutrition, deformities, and abnormalities of configuration are important criteria. Note should be to the following aspects of the physical examination: endocrine status, the regulation of vital processes (body temperature, blood pressure pulse, respiratory rate and rhythm, etc.), the skin and mucous membranes, perspiration, hair and nails, salivation, lacrimation and other secretory responses, fat metabolism, bones and joints, presence of specific and focal changes, such as Horner's syndrome. The examination of the autonomic nervous system provides valuable information in neurologic diseases, and the examiner should be familiar with the important methods of evaluation. Autonomic nervous system reflexes Among the autonomic nervous system reflexes these are the pupillary, lacrimal, salivary, sneeze, sucking, cough, vomiting, carotid sinus, and oculocardiac reflexes. Sweat Tests. These are important objective tests of autonomic function. The production of sweat, or perspiration, is a function of the sympathetic division of the autonomic nervous system. Sweating is produced by drugs such as acetylcholine and pilocarpine, which are classed as parasympathomimetic, and is decreased by atropine, scopolamine, and other drugs that inhibit structures innervated by postganglionic cholinergic nerves. The Pilomotor Response. Piloerection is also a function of the sympathetic division of the autonomic nervous system. Stimulation of the sympathetic nerves causes contraction of the erectors pilorum muscles and erection of the cutaneous hairs, known as cutis anserina or "goose flesh." The response may be elicited with ease, but it is inconstant and transient and cannot be demonstrated adequately on the hands or feet. Piloerection may be provoked by gentle stroking of the skin, tickling, scratching with a sharp object, or the application of cold. Ice, cotton soaked in alcohol or ether, or a methyl chloride spray may be used. Piloerection is elicited best at the nape of the neck, in the axillas, on the abdominal wall, and at the upper border of the trapezius. Piloerection is absent in lesions that involve the descending autonomic pathways in the brain stem and spinal cord, sympathetic trunk, preganglionic and postganglionic fibers, and peripheral nerves. It is abolished below transverse spinal lesions, and the descending reaction to a massive stimulus stops at this level. Reflex Erythema. Stimulation of the skin by stroking it with a blunt point is followed by focal vasodilation. There is first a local reaction, seen as a red line along the site of stimulation, which is followed in about ½min by a spreading flush, or flare, on each side of the scratch. Depending upon 63 the intensity of the stimulus and individual susceptibility, the site of stimulation becomes elevated, with the development of a welt, or wheal, sometimes with a white line in its center. Exaggeration of reflex erythema is called dermatographia. This phenomenon is present whenever the sympathetic influence is diminished. It is marked in individuals with overactivity of the parasympathetic division and in those with labile autonomic nervous systems or with evidence of sympathetic and parasympathetic imbalance. It may also occur on an allergic basis and as a reaction to chemical and thermal stimuli. Skin Temperature Studies. The determination of the skin temperature is an important part of the examination of the autonomic nervous system. The vasomotor tonus is reflected in the surface temperature of the body, and interruption of the sympathetic division with resulting vasodilation is followed by a rise in temperature. Conversely, stimulation of the sympathetic with consequent vasoconstriction is accompanied by a fall in surface temperature. Skin temperature studies can be useful in the diagnosis of lesions of the sympathetic division, in determining the level of a transverse spinal lesion, in delineating the extent of a peripheral nerve lesion, in the preoperative appraisal of the continuity of sympathetic pathways, and in the differential diagnosis of Raynaud's and Buerger's diseases, peripheral atherosclerosis, and other vascular diseases of the extremities. The Cold Pressor Test. Stimulation of the vasomotor center by cold with resultant rise in blood pressure may be used in the diagnosis of hypertension. The sphygmomanometer cuff is applied to one arm while the other hand and arm are immersed in water of about 4°C. Blood pressure readings are taken every 30-60 sec until the highest reading is reached. This is termed the index of response. The arm and hand are then removed from the cold water and readings are taken every 2 min until the basal level is reached. In the normal individual there is a slight rise in both systolic and diastolic blood pressure, with a fall to normal within 3 min after the stimulus is removed. A response of more than 20 mm Hg systolic, and more than 15 mm Hg diastolic, is considered significant. In hypertension there is a greater and more prolonged rise, with a delayed fall; this effect disappears after the administration of tetraethyl-ammonium chloride. There is also increased vasopressor reactivity in patients with cerebral atherosclerosis. Other Tests of Circulation. Postural effects on blood pressure may be tested by recording with the patient recumbent and erect. More precise evaluation is possible with the use of a tilt table. With orthostatic hypotension due to sympathetic failure the systolic and diastolic blood pressure values fall on assumption of the vertical position. The blood pressure and pulse responses to Valsalva's maneuver may be studied, but this procedure requires an indwelling arterial catheter for recording the pressure. Changes in heart rate with respiration, alteration of body posture, exercise, or drugs can also be noted and recorded as part of autonomic assessment. The parasympathetic innervation of the heart may be tested by the so-called diving reflex in response to immersion of the face in water. Pharmacologic Tests Although the autonomic nervous system does not lend itself to as complete clinical testing as does the voluntary nervous system, certain information regarding its function may be obtained by inference, especially by noting the effect of drugs that either stimulate or depress its component parts. It may be of diagnostic value to determine the relative irritability of the sympathetic and parasympathetic divisions and to note the effect of both autonomic stimulants and depressants in the relief of symptoms. May be used tests by injection of epinephrine, pilocarpine, atropine, methantheline and, physostigmine, neostigmine. Disorders of Autonomic Nervous System The disorders of autonomic function are complex, varied, and difficult to classify. Disorders of function of the peripheral autonomic nervous system Lesions of the peripheral portions of the autonomic nervous system are usually manifested by a deficiency or loss of function of one of the component of the system. Occasionally, however, irritation of one division may result in an increased activity of that portion. In general a lesion of the parasympathetic division, the individual fibers of which are supplied to special structures, is manifested by focal changes, whereas a lesion of the sympathetic division causes more generalized 64 changes. With loss of function of the constituent portions of the parasympathetic division there may be mydriasis, paralysis of visual accommodation, diminution of lacrimal and salivary secretion, cardiac acceleration, bronchial dilation, gastrointestinal atony with decreased secretion, spasm of the sphincters, bladder atony, and impotence. A lesion of the sympathetic component may cause vasodilation, anhidrosis, loss of piloerection, reflex erythema, fall in blood pressure, bradycardia, pupillary constriction, bronchial constriction, and impairment of ejaculation. The effect on gastrointestinal and bladder functions is less definite. These symptoms are increased by further inhibiting the action of the sympathetics or by stimulating the parasympathetics, and relieved, if the paralysis is not complete, by the administration of sympathomimetic drugs. Such diminution or loss of sympathetic function may be caused either by brain stem or spinal lesions that affect the descending sympathetic pathways, or by involvement of the intermediolateral cell groups, the preganglionic fibers, the sympathetic ganglia, the postganglionic fibers, or the peripheral nerves. Following a transverse spinal cord lesion above the eighth cervical or first thoracic segment, loss of sympathetic function of the entire body results, and if it is complete and interferes with vital functions such as respiration and cardiac function, it is incompatible with life. If partial, it may only cause loss of sweating, piloerection, and vasoconstriction of the face and body. A partial lesion at the eighth cervical and upper thoracic levels, especially if it involves only the intermediolateral cells, may affect only sympathetic fibers to the head and neck, causing anhidrosis, vasodilation, and Horner's syndrome. With a transverse lesion at any level of the thoracic or upper lumbar spinal cord there is loss of sympathetic function below the level of the lesion, with anhidrosis, vasodilation, loss of piloerection, and increase in skin temperature. Later there is vasoconstriction with a decrease in temperature; sweating and piloerection may reappear in an exaggerated form as part of the spinal defense reflex. Impairment of bowel, bladder, and sexual functions may also be present, and occasionally orthostatic hypotension or transient hypertension precipitated by bladder or bowel distention. Changes in the body protein and electrolytes, osteoporosis, testicular atrophy, altered excretion of 17-ketosteroids, and occasionally gynecomastia may develop. There are no changes in sympathetic function with lesions below the third lumbar segment, and only the sacral parasympathetics and somatic nerves are affected. With lesions of the mixed spinal nerves there are also sympathetic changes characterized by loss of sweating, piloerection, and vasoconstriction. With severe involvement there may be extensive alterations in the skin and subcutaneous tissues, described subsequently. In severe neuropathies, such as the autonomic neuropathy that may be present with diabetes, there sometimes are more extensive deficits, with a neurogenic bladder, impotence, bowel incontinence or nocturnal diarrhea, orthostatic hypotension, and neurogenic arthropathy. The sympathetic nerves have been sectioned in the treatment of Raynaud's disease, causalgia, hypertension, and other conditions, and to relieve the pain of angina pectoris and pancreatitis. Disorders of central autonomic regulation In disorders of function that involve predominantly the central regulatory centers concerned with the autonomic nervous system, signs and symptoms are generalized rather than focal. Some of them are referable to specific visceral systems; others are more diffuse. Clinical literature as well as experimental data relating to the hypothalamus and to disorders arising from the injury or disease of its parts has increased rapidly, and many characteristic syndromes have been described. There may be disturbances of sleep, abnormalities of temperature regulation, changes in carbohydrate and water metabolism, dysfunction of fat metabolism, or respiratory abnormalities, together with, in many instances, behavioral abnormalities and personality changes. Many of the hypothalamic syndromes that are encountered clinically are residuals of encephalitis or are associated with neoplasms. The hypothalamus is, however, under the influence of the cortex, and it may be difficult to distinguish between cortical and diencephalic manifestations. Hypothalamic syndromes is accumulated term are those that are associated with the lesion or deficiency of hypothalamus by injury, tumor, encephalitis. Autonomic-vascular-visceral is associated with crisis of paroxysmal character: sympathoadrenal, vago-insular or mixed. Neuro65 trophic is associated with trophic disturbances (dryness, neurodermitis, ulcers, bed sores, acute perforates of stomach and esophagus). Neuro-endocrine-metabolic is associated with increasing or decreasing of hypophisis function (Itsenko-Kushing symdrome, acromegaly, early climacterium, impotence, diabetes insipidus, thyrotoxicosis). Sleeping disorders include insomnia, sleeping inversion, lethargy (narcolepsy) – sudden attack of sleepiness that can happen in any place and position of the patient. Sometimes we can observe thermoregulation disturbances. It may be low grade fever, associated with asymmetry under the arms, in the mouse and rectum. The thermoregulation disturbances may have paroxysmal character. The signs of sympathoadrenal crisis: skill is pail, dryness of skin, tachycardia, high blood pressure, midriasis and widening of eye-slit, tremor, diarrhea, gooseflesh, frequend urination, hyperglycemia. The signs of vagoinsular crisis: hyperemia, hyperhydrosis, bradycardia, low blood pressure, miosis, salivation, breathlessness, abdominal spastic pain, diarrhea. Disturbances of Temperature Regulation. Either hypothermia or hyperthermia may result from hypothalamic involvement. Hyperthermia may result from involvement of the tuberal region, and especially of the supraoptic nuclei or the rostral portion of the anterior hypothalamic area. It is associated with sweating, vasodilation, and other mechanisms for heat loss. Hyperthermia is a common symptom with third ventricle tumors, and may follow cerebral trauma or surgery, brain stroke. Hypothermia is associated with mechanisms for heat production including vasoconstriction, increased visceral and somatic activity, and shivering. It may follow involvement of the posterior hypothalamic area and the mammillary bodies, or of the caudal portion of the lateral hypothalamus. Disturbances of Water Metabolism. The hypothalamus is closely related with the posterior lobe of the hypophysis. It is probable the water metabolism is regulated through the posterior lobe, where antidiuretic hormone is produced. Lesions of the supraoptic nuclei or the supraopticohypophyseal tract are followed by diabetes insipidus with polydipsia and polyuria. Diabetes insipidus is a common symptom of tumors in the parasellar region, of encephalitis, and of meningitis, and may develop following intracranial surgery or cerebral trauma. It can also be congenital. Disturbances of Glucose Metabolism. Hyperglycemia with glycosurea, a syndrome resembling diabetes mellitus, may result from lesions of the tuberal region, whereas hypoglycemia with abnormal sensitivity to insulin may follow lesions of the paraventricular nuclei. Disturbances of Fat Metabolism. The adiposogenital syndrome was the first hypothalamic syndrome to be described. This disorder usually occurs in boys and is characterized by disturbances of fat metabolism together with sexual underdevelopment. There is obesity of feminine distribution, often with girdles of fat about the pelvis. Other symptoms of manifestations include gynecomastia, underdevelopment of the external genitalia, and retardation of development of the secondary sexual characteristics. The Laurence – Moon - Biedl syndrome is characterized by obesity, hypogenitalism, mental retardation, polydactylism, and pigmentary degeneration of the retina; it is an inherited disorder. Disturbances of Blood Circulation. Through its regulatory effect upon the autonomic nervous system, the hypothalamus plays an important part in the regulation of circulation, heart rate and rhythm, and blood pressure. Stimulation of the posterior and lateral hypothalamic nuclei causes vasoconstriction, an increased heart rate, and a rise in blood pressure, whereas stimulation of the anterior and midline hypothalamic nuclei and the tuber cinereum produces vasodilation and a reduction in heart rate. Disturbances of Respiration. Abnormalities of the rate, rhythm, and amplitude of respiration, such as hyperpnea, apnea, Cheyne - Stokes respiration, Biot’s breathing, may caused by central, probably hypothalamic, involvement. Disturbances of Gastrointestinal Function. Lesions of the hypothalamus and its connections can cause accelerated gastrointestinal motility, increased secretion, hypersalivation, and excessive hunger (bulimia or hyperphagia), or they can cause decreased motility and secretion, dry mouth, and decreased appetite. Bulimia is an important symptom of bilateral temporal lobe dysfunction; it 66 may also be present with other cerebral disorders. The Kleine-Levin syndrome consists of periodic attacks of hypersomnia accompanied by bulimia, irritability, behavioral changes, and uninhibited sexuality. It usually occurs in young males. Disturbances of the Sleep Cycle. The hypothalamus, especially its posterior portions, including the mammillary bodies, is important in the maintenance of normal sleep rhythm, and hypothalamic lesions may cause hypersomnia, inversion of the sleep cycle, or insomnia. The hypersomnia and other abnormalities of sleep may be produced by involvement of the midbrain reticular system, or to interruption of the pathways from the cortex to the hypothalamus. Disturbances of Sexual Function Sexual infantilism may occur as an isolated phenomenon or as a part of Frohlich's and other syndromes. It is a manifestation of damage to the nuclei in the middle portion of the tuberal region. Sexual precocity has been described as a characteristic symptom of the pineal syndrome; the hypothalamus, however, is the critical site for lesions causing pubertas praecox, and it is probably due to pressure on or involvement of the ventromedial and lateral tuberal nuclei and mammillary bodies. Both sexual infantilism and sexual precocity may be manifestations of dysfunction of the endocrine glands, especially the pituitary, gonads, and adrenal glands; such changes may be secondary to underlying hypo-thalamic involvement. Increased libido, decreased libido, impotence, amenorrhea, hypermenorrhea, and other manifestations of sexual dysfunction are sometimes partly hypothalamic in origin. The somatic manifestations of the orgasm may be due to hypothalamic stimulation. Disturbances of the Emotions The hypothalamus is the center that reinforces and coordinates the neural and humoral mechanisms of emotional expression. When the posterior portion of the hypothalamus is released from control by higher centers of the brain, a complex of primitive pseudoaffective reactions takes place. These physical manifestations suggest that an intense emotional reaction is taking place, but there may be merely a motor expression of rage without a change in affect. Similar manifestations have been produced by stimulation of the posterior and lateral hypothalamic areas and by bilateral removal of the frontal or temporal lobes. Abnormal affective and emotional reactions, fear, and aggressive behavior, however, may also be lessened by interruption of the pathways connecting various cortical areas in the frontal and limbic lobes with the thalamus and hypothalamus. The physical concomitants of emotion, namely, tachycardia, tachypnea, elevation of the blood pressure, perspiration, flushing, piloerection, and various disturbances of gastrointestinal function, are in reality manifestations of hypo-thalamic function with secondary visceral effects. In many of the neuroses the symptoms are largely somatic, or vegetative, in nature, and are similar to the physical symptoms encountered in various emotional states. Those referable to the cardiorespiratory system include tachycardia, palpitation, dyspnea, irregular respiration, and pain in the chest. Those referable to the gastrointestinal tract consist of gaseous indigestion, pain, nausea, vomiting, pylorospasm, hyperacidity, spastic constipation, flatulent constipation, and diarrhea. Those referable to the genitourinary system include frequency, dysuria, impotence, lack of libido, amenorrhea, and frigidity. The symptoms of the anxiety neuroses or of normal individuals during periods of stress, namely, tension, palpitation, hyperpnea, nausea, frequency, mydriasis, cold hands and feet, dry mouth, and variable blood pressure, are often the result of hypothalamic stimulation. All are symptoms of autonomic imbalance, and may be of central origin. Many disease syndromes such as hypertension, coronary artery disease, hyperthyroidism, peptic ulcer disease, spastic constipation, ulcerative colitis, migraine, bronchial asthma, and arthritis may have definite psychosomatic correlations. Disturbances of Endocrine Function Consequently abnormalities of hypothalamic function may have a close relationship to the various disturbances of endocrine function. The nuclei of the hypothalamus regulate the internal secretions of the thyroid, adrenal, and other glands. The hypothalamus may play a part in the development of either hyperthyroidism or hypothyroidism. Lesions of the hypothalamus may affect the islet cells of the pancreas, causing either diabetes mellitus or hyperinsulinism with 67 hypoglycemia. The effect on the sexual glands may be direct, rather than through the pituitary, and may cause sexual precocity, impotence, amenorrhea, deficient development of primary or secondary sexual characteristics, and sexual infantilism. Miscellaneous disturbances of autonomic function Allergic Disturbances. The predominant autonomic manifestations of allergy are vasodilation and exudation. There is exudation in cutaneous manifestations, such as urticaria, eczema, and angioneurotic edema. There is vasodilatation in hay fever and allergic rhinitis, with hypersecretion of the mucous membranes and lacrimal glands. There is spasm of the bronchial musculature in asthma with vasodilatation and mucosal exudation. Trophic Disorders. The trophic disturbances are affected the bones, joints, and muscles. They are usually associated with lesions of the motor or sensory nerves or both. Trophic changes involving the bones and joints. There is first an osteoporosis accompanied by an abnormal brittleness of the bones that may lead to spontaneous fractures, but the most characteristic changes are those in the joints. There are secretory disturbances of the synovia with swelling of the joints, destruction of joint surfaces and ligaments, atrophy of cartilage or bone, and often painless intraarticular fractures and dislocations. There is atrophy of the skin, subcutaneous tissues, muscles, and bones. There may be alopecia and scleroderma in the atrophic areas. 68 LECTURE X METHODS OF INVESTIGATIONS IN NEUROLOGY Lumbar puncture and the examination of the cerebrospinal fluid. Diagnostic lumbar punctures (LP) are performed for the purpose of examining either the fluid itself or the hydrodynamics of the fluid. The test is enabled to determine the composition of cerebrospinal fluid (CSF), cerebrospinal fluid pressure, to investigate abnormalities in pressure in such conditions as spinal subarachnoid block. Therapeutic lumbar punctures are made possible to increase intracranial pressure. The indications for lumbar puncture: meningitis, encephalitis, acute inflammatory polyneuritis (Guillain-Barre syndrome), acute demyelinating disorders, seizure, stroke, polyneuropathy; dementia; altered level of consciousness, therapeutic administration of antibiotics or antineoplastic agents, subarachnoid hemorrhage. Contraindications to lumbar puncture: clinical signs of impending uncal, central transtentorial, or cerebellar herniation, and when; the needle must pass through an area of infection that could result in infection in the subarachnoid space. Technique of lumbar puncture. In adults, the LP is best performed with the patient in the lateral decubitus position with the head and spine parallel to the floor. This positioning is particularly important for the accurate measurement of the opening and closing pressures. After positioning the patient, certain landmarks should be palpated, beginning with the iliac crest. An imaginary line that runs between the crests will intersect approximately the L3-L4 interspace. Once this area is located, the spinal processes of L3 and L4 should be palpated and between them the interspace may be felt. In infants and children the inter-space between the fourth and fifth lumbar spinous processes is the one of choice. This procedure is easily accomplished in thin patients but may be difficult in obese or edematous individuals. When the landmarks are located, the patient should pull the knees into the chest and assume the so-called fetal position. This maneuver helps widen the vertebral interspace. The clinician should appropriately prepare the skin surface using a sterilizing agent and then place the sterile draping. One to two percent lidocaine should be injected intradermally and then is infiltrated into the deeper tissues. Once the patient is anesthetized, a spinal needle with a stylet should be inserted into the skin toward the interspace. The patient should be comfortable, warm, and relaxed, and reassured of the simplicity and relative painlessness of the test. If the patient is tense or nervous, some sedation by mouth may be administered before the puncture is to be done. When fluid appears at the needle hub, a threeway stopcock and manometer are attached. The fluid is allowed to rise slowly in the manometer. The upper limit of normal CSF opening pressure with a patient in the lateral recumbent position is 110 mm H2O in young infants, 150 mm H2O in children, 180 mm H2O in adults. Myelography: X-rays are taken after a radiopaque agent is injected into the subarachnoid space via lumbar puncture. Magnetic resonance imaging (MRI) has replaced myelography for evaluation of intraspinal abnormalities, but computed tomography (CT) myelography is still done when MRI is unavailable. Contraindications are the same as those for lumbar puncture. Myelography may exacerbate the effects of spinal cord compression, especially if too much fluid is removed too rapidly. 69 Table 10.1. Cerebrospinal Fluid Abnormalities in Various Disorders (Merck Manual) Condition Pressure Wbc/μL Predominant Cell Glucose Type Protein Normal 100–200 mm H2O 0–3 L 50–100 mg/dL (2.78–5.55 mmol/L) 20–45 mg/dL Acute bacterial ↑ meningitis 100– 10,000 PMN ↓ > 100 mg/dL* Acute syphilitic N or ↑ meningitis 25–2000 L N ↑ Lyme disease of N or ↑ CNS 0–500 L N N or ↑ Brain abscess or N or ↑ tumor 0–1000 L N ↑ Viral infections N or ↑ 100–2000 L N N or ↑ Cerebral hemorrhage ↑ Bloody RBCs N ↑ Cerebral thrombosis N or ↑ 0–100 L N N or ↑ 0–50 L N N or ↑ 0–100 L N > 100 mg/dL Spinal tumor cord N Guillain-Barré syndrome N L = lymphocyte; N = normal; PMN = polymorphonuclear leukocyte; ↑ = increased; ↓ = decreased. Electroencephalograpy. The electroencephalogram (EEG) remains the primary test for identifying and characterizing many physiological disturbances of the brain, particularly in the evaluation of seizures, encephalopathies, coma, and focal cerebral dysfunction. EEG is generated by synchronized synaptic activity on the dendrites of cortical pyramidal neurons. The EEG results from a myriad of such processes, each of which individually generates a signal too feeble to be detected at the scalp. EEG is an irreplaceable test in the evaluation of possible seizures. Significant epileptiform abnormalities are a useful and reliable confirmation that a patient's spells are epileptic seizures, and allow them to be classified as partial or generalized in onset. The EEG is often used to evaluate patients with encephalopathy or coma, when it may give valuable information on the location and the severity of the process and on the neurological prognosis. The EEG may be diagnostic in cases of Creutzfeldt-Jakob disease. Recording. The recording is performed with metal disk electrodes, filled with conductive gel or paste and attached on the scalp wiped with alcohol. Often an elastic cap that holds the entire electrode array in place is used. 21 electrodes are applied usually. The patient must be fully alert during a portion of the record, his eyes are normally closed. A number of activating procedures like hyperventilation, photic and sound stimulation, sleep and sleep deprivation are commonly used to bring out abnormalities, particularly in patients with suspected seizures. The signal is amplified, recorded and then undergoes computer analysis. Various kinds of quantitative measures of the EEG 70 activity are available, the most important of them are frequency (Fourier) analysis with topographic mapping and event detection in the practice of long-term monitoring of epileptic patients. Description of EEG activity. The EEG is usually described in the terms of amplitude and frequency, which are measured in μV and hertz, respectively. Frequency may also be described in terms of four bands: delta, under 4 hertz; theta, from 4 to under 8 hertz; alpha, from 8 to 13 hertz; and beta, over 13 hertz. The polarity and localization of the signal is determined by bipolar and referential montages. Fig. 10.1. Normal EEG (L.R. Zenkov, 2004) Other EEG-based techniques. Clinical polysomnography includes EEG, eye movements, the chin electromyography, and respirations monitoring. It provides additional information to determine sleep stages and is used to detect and quantitate various sleep disorders, most often respiratory problems (sleep apnea). Measurement of evoked responses (EP). Visual, auditory, or tactile stimuli are used to activate corresponding neuroanatomic tracts and relay stations, resulting in small cortical wave potentials. Ordinarily, these small potentials are lost in the background noise of the EEG, but computer averaging of a series of stimuli, time-locked to the EEG, cancels out the noise to reveal a waveform. The latency, duration, and amplitude of the evoked responses reflect the physiologic integrity of the tested sensory pathway. For example, visual evoked responses may reveal unsuspected optic nerve damage by multiple sclerosis. Somatosensory evoked responses may pinpoint the physiologic disturbance when multiple levels of the neuraxis are affected by structural disease (e.g., metastatic carcinoma that invades the plexus and spinal cord). Clinical Electromyography. The pattern of electrical activity in muscle [i.e., the electromyogram (EMG), both at rest and during activity, may be recorded from a needle electrode inserted into the muscle. When determining whether weakness is due to nerve, muscle, or neuromuscular junction disorder is clinically difficult, these studies can identify the affected nerves and muscles. In electromyography, a needle is inserted in a muscle, and electrical activity is recorded while the muscle is contracting and resting. Normally, resting muscle is electrically silent; with minimal contraction, action potentials of single motor units appear. As contraction increases, the number of potentials increases, forming an interference pattern. Denervated muscle fibers are recognized by increased activity with needle insertion and abnormal spontaneous activity (fibrillations and fasciculations); fewer motor units are recruited during contraction, producing a reduced interference 71 pattern. Surviving axons branch to innervate adjacent muscle fibers, enlarging the motor unit and producing giant action potentials. In muscle disorders, individual fibers are affected without regard to their motor units; thus, amplitude of their potentials is diminished, but the interference pattern remains full. In nerve conduction velocity studies, a peripheral nerve is stimulated with electrical shocks at several points along its course to a muscle, and the time to initiation of contraction is recorded. Ultrasonography. Diagnostic ultrasonography (US) uses sound waves above the audible level to generate diagnostic medical images. The patient is not exposed to ionizing radiation. US has various imaging applications, with specific uses in neurological disorders. Diagnostic US can be coupled with Doppler devices, with or without color, allowing flow measurements in vascular structures, such as commonly employed for carotid artery studies. Echoencephalography: Ultrasonography can be used at the bedside (usually in the neonatal ICU) to detect hemorrhage and hydrocephalus in children < 2 yr. CT has replaced echoencephalography in older children and adults. Duplex Doppler ultrasonography: This noninvasive procedure can assess dissection, stenosis, occlusion, and ulceration of the carotid bifurcation. It is safe and rapid, but it does not provide the detail of angiography. It is preferable to periorbital Doppler ultrasonography and oculoplethysmography for evaluating patients with carotid artery transient ischemic attacks and is useful for following an abnormality over time. Transcranial Doppler ultrasonography helps evaluate residual blood flow after brain death, vasospasm of the middle cerebral artery after subarachnoid hemorrhage, and vertebrobasilar stroke. NEUROIMAGING IN NEUROLOGIC DISORDERS A dramatic increase in the role of imaging in diagnosis of neurologic diseases occurred with the development of computed tomography (CT) in the early 1970s and of magnetic resonance imaging (MRI) in the 1980s. MRI has gradually replaced CT for many indications and has also replaced many of the invasive neuroimaging techniques, such as myelography and angiography. In general, MRI is more sensitive than CT for the evaluation of most lesions affecting the brain and spinal cord parenchyma. CT is more sensitive than MRI for visualizing osseous detail and brain hemorrhage (parenchymal or subarachnoid). Recent developments, such as helical CT, CT angiography (CTA), MR angiography (MRA), positron emission tomography, Doppler ultrasound, and interventional angiography have continued to advance diagnosis and therapy. Computed Tomography. The CT image is a computer-generated cross-sectional representation of anatomy created by an analysis of the attenuation of x-ray beams passed through various points around a section of the body. As the x-ray source, collimated to the desired slice thickness, rotates around the patient, sensitive x-ray detectors aligned 180o from the source detect x-rays attenuated by the patient's anatomy. A computer calculates a “back projection” image from the 360o x-ray attenuation profile. Greater x-ray attenuation, as caused by bone, results in areas of high “density”, while soft tissue structures, which attenuate x-rays less, are lower in density. The density is measured in Hounsfield units (HU). The resolution of an image depends on the radiation dose, the collimation (slice thickness), the field of view, and the matrix size of the display. A typical modern CT scanner is capable of obtaining sections 1 to 2, 5, and 10 mm thick at a speed of 1 to 3 s per section; complete studies of the brain can be completed in 2 to 3 min. Intravenous contrast is often administered prior to or during a CT study to identify vascular structures and to detect defects in the blood-brain barrier (BBB) associated with pathologies such as tumors, infarcts, and infections. An intact BBB prevents contrast molecules from exiting the intravascular compartment. In the normal CNS, only vessels and those structures not having a BBB (e.g., the pituitary gland, choroid plexus, and dura) enhance. The use of contrast agents carries a risk of allergic reaction, increases the dose of radiation when both noncontrast and contrast CT scans are to be obtained, adds expense, and may mask hemorrhage; thus before contrast is administered, the indication for its use should always be considered carefully. 72 Fig. 10.2. a)CT-scan. Ischemic stroke (Sumy, Fig. 10.2. b) CT-scan. Brain hemorrhage (Sumy, 2006) 2006) Brain Magnetic Resonance Imaging (MRI). The phenomenon of magnetic resonance is a complex interaction between protons in biologic tissues, a static and alternating magnetic field (the magnet), and energy in the form of radiofrequency waves of a specific frequency (Rf), introduced by coils placed next to the body part of interest. The energy state of the hydrogen protons is transiently excited. The subsequent return to equilibrium (relaxation) of the protons results in a release of Rf energy (the echo) which can be measured by the same surface coils that delivered the Rf pulses. The complex Rf signal or echo is transformed by Fourier analysis into the information used to form an MR image. MRI provides better resolution of neural structures than CT. This difference is most significant clinically for visualizing brain stem lesions and other abnormalities of the posterior fossa; CT images of this region are often marred by bony streak artifacts. Also, MRI is better for detecting demyelinating plaques, early infarction, subclinical brain edema, cerebral contusions, incipient transtentorial herniation, abnormalities of the craniocervical junction, and syringomyelia. It is especially valuable for identifying spinal abnormalities (e.g., tumor, abscess) compressing the spinal cord and requiring emergency intervention. MRI is contraindicated in patients who have had a pacemaker, cardiac or carotid stents ferromagnetic aneurysm clips or other metallic objects that may overheat or be displaced within the body by the intense magnetic field. Magnetic Resonance Angiography. Magnetic resonance angiography (MRA) uses MRI with or without a contrast agent to show cerebral vessels and major arteries and their branches in the head and neck. Although MRA has not replaced cerebral angiography, it is used when cerebral angiography cannot be done (the patient refuses or has increased risk). Magnetic resonance venography uses MRI to show the major veins and dural sinuses of the cranium. MRV obviates the need for cerebral angiography in diagnosing cerebral venous thrombosis and is useful for monitoring thrombus resolution and guiding the duration of anticoagulation. Magnetic resonance spectroscopy can measure metabolites in the brain regionally to distinguish tumors from abscess or stroke. Positron Emission Tomography. Positron emission tomography (PET) relies on the detection of positrons emitted during the decay of a radionuclide that has been injected into a patient. Images 73 reveal differences in regional radionuclide activity among normal and pathologic brain structures. PET scanning has been used to assist in differentiating radiation necrosis from active neoplasm following therapy, in localizing temporal lobe epileptic foci, and in detecting metastatic disease and determining cardiac viability. Positron emission tomography (PET) is a nuclear medicine imaging technique which produces a three-dimensional image or picture of functional processes in the body. The system detects pairs of gamma rays emitted indirectly by a positron-emitting radionuclide (tracer), which is introduced into the body on a biologically active molecule. More frequently are used FDG (Fluorodeoxyglucose is a glucose analog. Its full chemical name is 2-fluoro-2-deoxy-Dglucose) Images of tracer concentration in 3-dimensional space within the body are then reconstructed by computer analysis. 74 REFERENSES 1. Тексти лекцій для студентів. 2. Нервові хвороби: підруч. для студ. вищ. мед. навч. закл. III-IV рівнів акредитації [Текст] / С. М. Вінничук, Є. Г. Дубенко и др.; - К. : Здоров'я, 2001. - 696с. 3. Нервные болезни: Учебное пособие [Текст] / А.А. Скоромец, А.П. Скоромец, Т.А. Скоромец. – М.: МЕДпресс-информ, 2007. – 552 с. 4. Сандригайло Л.И. Анатомо-клинический атлас по невропатологии. [Текст] / Л.И. Сандригайло. Минск: Вышэйшая школа,1988. - 319 с. 5. Триумфов А.В. Топическая диагностика заболеваний нервной системы. [Текст] / А.В. Триумфов. М.: Медицина, 1974.- 338 с. 6. Duus’ Topical Diagnosis in Neurology. 4th edition. [Текст] / P. Duus. Thieme, 2005. – 517 pp. 7. Michael J. Aminoff. Clinical Neurology [Текст] / Michael J. Aminoff, David A. Greenberg, Roger P. Simon. Lange Medical Books/McGraw-Hill, 2005. - 401 pp. 7. The Merck manual of diagnostic and therapy. Neurologic Disorders. [Електронний ресурс] / Режим доступу: URL: http://www.merck.com/mmpe/sec16.html. 8. R. Rohkamm. Color Atlas of Neurology. [Текст] / R. Rohkamm – Thieme, 2004. – 448 pp. 9. National Center for Biotechnology Information. Neuroscience. Purves Dale; Augustine George J.; Fitzpatrick David; Katz Lawrence C.; LaMantia Anthony-Samuel et al. [Електронний ресурс] / Режим доступу: http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=neurosci 10. http://www.wrongdiagnosis.com 11. E-medicine. Medscape’s Continually Updated clinical References. [Електронний ресурс] / Режим доступу: http://emedicine.medscape.com/neurology 75