Lab 9
advertisement
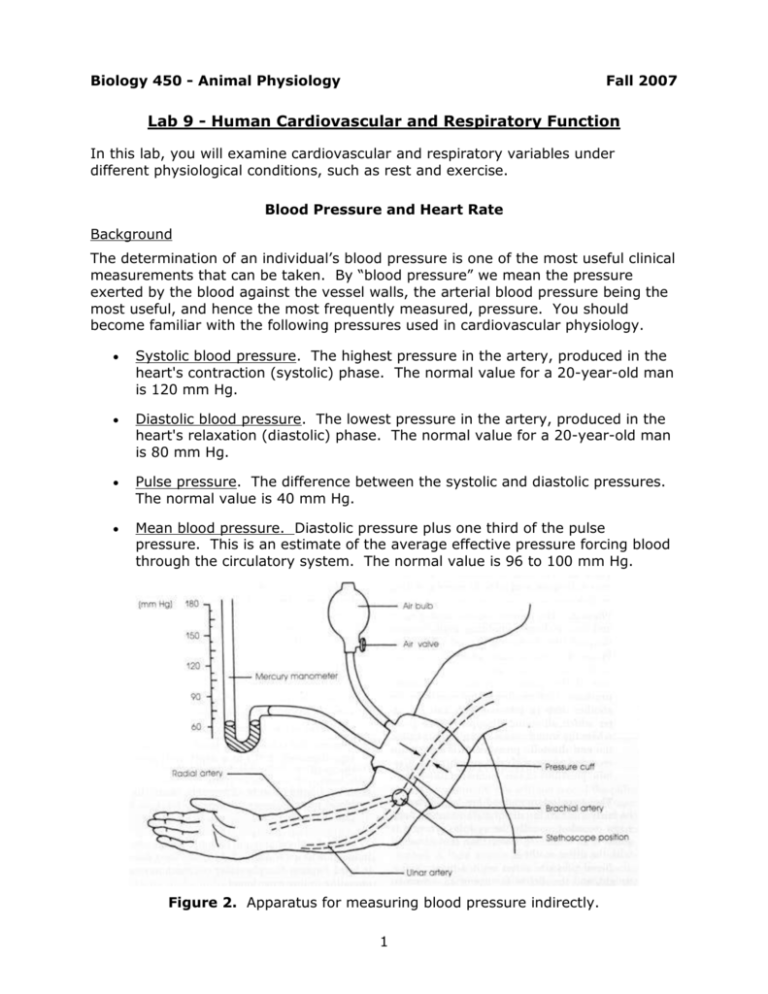
Biology 450 - Animal Physiology Fall 2007 Lab 9 - Human Cardiovascular and Respiratory Function In this lab, you will examine cardiovascular and respiratory variables under different physiological conditions, such as rest and exercise. Blood Pressure and Heart Rate Background The determination of an individual’s blood pressure is one of the most useful clinical measurements that can be taken. By “blood pressure” we mean the pressure exerted by the blood against the vessel walls, the arterial blood pressure being the most useful, and hence the most frequently measured, pressure. You should become familiar with the following pressures used in cardiovascular physiology. Systolic blood pressure. The highest pressure in the artery, produced in the heart's contraction (systolic) phase. The normal value for a 20-year-old man is 120 mm Hg. Diastolic blood pressure. The lowest pressure in the artery, produced in the heart's relaxation (diastolic) phase. The normal value for a 20-year-old man is 80 mm Hg. Pulse pressure. The difference between the systolic and diastolic pressures. The normal value is 40 mm Hg. Mean blood pressure. Diastolic pressure plus one third of the pulse pressure. This is an estimate of the average effective pressure forcing blood through the circulatory system. The normal value is 96 to 100 mm Hg. Figure 2. Apparatus for measuring blood pressure indirectly. 1 The mean blood pressure is a function of two factors – cardiac output (CO) and total peripheral resistance (TPR). Peripheral resistance depends on the caliber (diameter) of the blood vessels and the viscosity of the blood. Mean BP = Cardiac output (ml/sec) × Total peripheral resistance (TPR units) Cardiac output (ml/min) = Heart rate/min × Stroke volume (ml) Thus, the measurement of blood pressure provides us with information on the heart's pumping efficiency and the condition of the systemic blood vessels. In general, we say that the systolic blood pressure indicates the force of contraction of the heart, whereas the diastolic blood pressure indicates the condition of the systemic blood vessels (for instance, an increase in the diastolic blood pressure indicates a decrease in vessel elasticity). Blood pressure may be measured either directly or indirectly. In the direct method, a cannula is inserted into the artery and the direct head-on pressure of the blood is measured with a transducer or mercury manometer. In the indirect method, pressure is applied externally to the artery and the pressure is determined by listening to arterial sounds (using a stethoscope) below the point where the pressure is applied (Figure 2). This is called the auscultatory method, because the detection of the sounds is termed auscultation. An older and less accurate method is the palpatory method, in which one simply palpates, or feels, the pulse as pressure is applied to the artery. In either of these indirect methods, pressure is applied to the artery using an instrument called the sphygmomanometer. It consists of an inflatable rubber bag (cuff), a rubber bulb for introducing air into the cuff, and a mercury or anaeroid manometer for measuring the pressure in the cuff. Human blood pressure is most commonly measured in the brachial artery of the upper arm. In addition to being a convenient place for taking measurements, it has the added advantage of being at approximately the same level as the heart, so that the pressures obtained closely approximate the pressure in the aorta leaving the heart. This allows us to correlate blood pressure with heart activity. Procedures We will practice the auscultatory method, combined with a fingertip pulse pressure transducer 1. Have the subject seated, with his or her arm resting on a table. Attach the pulse transducer to the subject’s finger and set up Chart to record the relative pressure changes in the fingertip. 2. Wrap the pressure cuff of the sphygmomanometer snugly around the bare upper arm, making certain that the inflatable bag within the cuff is placed over the inside of the arm where it can exert pressure on the brachial artery. Wrap the end of the cuff around the arm and tuck it into the last turn, or press the fasteners together to secure the cuff on the arm. Close the valve on the bulb by turning it clockwise. 3. Place the bell of the stethoscope below the cuff and over the brachial artery where it branches into the radial and ulnar arteries (Figure 17.2). Use your fingers, rather than your thumb, to hold the stethoscope over the artery; otherwise you may be measuring the thumb arterial pressure rather than the brachial artery pressure. With no air in the cuff no sounds can be heard. 2 4. Inflate the cuff so the pressure is above diastolic (80-90 mm Hg), and you will be able to hear the spurting of blood through the partially occluded artery. Increase the cuff pressure to around 160 mm Hg; this pressure should be above systolic pressure so that the artery is completely collapsed and no sounds are heard. The pulse transducer should show a constant output at this time. 5. Now, open the valve and begin to slowly lower the pressure in the cuff. As the pressure decreases you will be able to hear four phases of sound changes; these were first reported by Korotkoff in 1905 and are called Korotkoff sounds. Note the corresponding changes in the output of the pulse transducer as the pressure of the cuff drops below the systolic and then diastolic pressures. Phase 1. Appearance of a fairly sharp thudding sound that increases in intensity during the next 10 mm Hg of drop in pressure. The pressure when the sound first appears is the systolic pressure. Phase 2. The sounds become a softer murmur during the next 10 to 15 mm Hg of drop in pressure. Phase 3. The sounds become louder again and have a sharper thudding quality during the next 10 to 15 mm Hg of drop in pressure. Phase 4. The sounds suddenly become muffled and reduced in intensity. The pressure at this point is termed the diastolic pressure. This muffled sound continues for another drop in pressure of 5 mm Hg, after which all sound disappears. The point where the sound ceases completely is called the end diastolic pressure. It is sometimes recorded following the systolic and diastolic pressures in this manner: 120/80/75. Postural Effects on Blood Pressure Measure your partner's blood pressure and pulse rate while she or he is lying down (supine), sitting, and standing. Record your results on your worksheet. Exercise Test This test examines the short-term effects of exercise on blood pressure. Note – The subject should be in good health, with no known cardiovascular or respiratory problems. 1. Have the subject sit comfortably. 2. Record the systolic and diastolic blood pressure and pulse rate every few minutes until a constant level is obtained. 3. Have him or her run up and down several flights of stairs, and then return to the sitting position. 4. Obtain and record the blood pressure and pulse immediately, then every minute for 5 minutes. 3 Cold Pressor Test This test is used to demonstrate the effect of a change in total peripheral resistance on blood pressure. The normal reflex response to a cold stimulus is an increase in arteriolar vasoconstriction, and here you will observe the effects of this change on arterial blood pressure. 1. Have the subject sit down comfortably or lie supine. 2. Record the systolic and diastolic blood pressure and pulse rate every few minutes until a constant level is obtained. 3. Immerse the subject's free hand in ice water (approximately 5 °C) to a depth well above the wrist. The hand should remain immersed until the recordings below have been completed, or the discomfort becomes too intense to continue. 4. After the hand has been immersed for 10 to 15 seconds, obtain the blood pressure and pulse every 20 seconds for 1 or 2 minutes and record. If there is insufficient time to obtain both systolic and diastolic pressure, just measure the systolic value. Respiratory Movements Background Of the many processes occurring in our bodies each instant, those that function in the movement of oxygen to the tissues are among the most important. If tissues are deprived of oxygen for too long a time, they die; this time factor is especially critical for the cells of vital organs such as the heart and brain. Because of the importance of O2 and CO2, their concentration in the lungs and blood is finely regulated by a variety of receptors, reflexes, and feedback processes that control our respiratory patterns. You can gain insight into some of these control processes by observing a person's respiratory movements and the alteration of these movements caused by various factors. Also important in oxygen delivery are the capacity of the lungs for air intake and the ability of the lungs to move air in and out quickly. You will analyze these functions when you study the various lung volumes and capacities and conduct the pulmonary function tests. In our setup, respiratory movements are recorded using a piezoelectric pneumograph (called “Pneumotrace II”) that wraps around the subject’s chest. Piezoelectric devices generate a voltage in response to stretching or bending, which can then be measured directly by our MacLab units. The disadvantage of this type of recorder for a pneumograph is that a constant degree of stretch does not produce a constant voltage – instead, the voltage declines to zero with time. As a result, the Pneumotrace is quite sensitive to rapid changes thoracic (= lung) volume, but not to slower changes. You may have to adjust the sensitivity in Chart to get a useable reading, and the apparent volume of an inhalation or exhalation will be confounded with the speed of volume changes. 4 In these experiments, the subject should be seated close to the recorder when being tested but should not look at the record. Use a suitable recording rate so that respiratory rates can be determined. Procedures Be sure to answer the worksheet questions accompanying each exercise. Setup The Pneumotrace is attached directly to one of the input channels on the MacLab unit. Use Chart to record the resulting voltages. (You should be able to handle the details yourself by now.) Normal Respiratory Pattern Record the subject's normal cyclic pattern of respiration for 1 to 2 minutes using chart. Note the amplitude of the inspiration and expiration cycles. Forced Hyperventilation 1. Record normal ventilation for a few cycles. 2. At a given signal, mark the recording and have the subject breathe as fast and as deeply as possible for 30 seconds. 3. At the end of this period, obtain a record of the aftereffects of the hyperventilation. The subject should allow his breathing to be as involuntary as possible during this post-hyperventilation period. If the subject gets dizzy while hyperventilating, have him stop, but record the respiratory response. Forced Hyperventilation in a Closed System Repeat the hyperventilation experiment with the subject breathing in and out of a paper or plastic bag. (The bag should be held tightly around the nose and mouth. Be sure to avoid leakage of air from the bag.) Record the respiratory movements after hyperventilation. Rebreathing Record respiratory movements while the subject breathes in and out of a paper or plastic bag for several minutes. In this case, the subject should allow his breathing to be as involuntary as possible. Observe the rate and amplitude (as well as you can from the Pneumotrace) of ventilation and how these values change over time. Effect of Exercise Record respiratory movements after the subject has exercised by running up and down several flights of stairs (as before, only healthy individuals should participate). 5 Respiratory Volumes Background The total capacity of the lungs is divided into various volumes and capacities according to the function of these in the intake or exhalation of air. For a proper understanding of respiratory processes, it is necessary that you become familiar with these volumes and capacities. As shown in Figure 3, the total amount of air one’s lungs can possibly hold can be subdivided into four volumes, defined as follows: Tidal volume (TV). The amount of air inspired or expired during normal, quiet respiration. Inspiratory reserve volume (IRV). The amount of air that can be forcefully inspired above and beyond that taken in during a normal inspiration. Expiratory reserve volume (ERV). The amount of air that can be forcefully expired following a normal expiration. Residual volume (RV). The amount of air that remains trapped in the lungs after a maximal expiratory effort. In addition to these four volumes, which do not overlap, there are four capacities, which are combinations of two or more volumes. Total lung capacity (TLC). The total amount of air the lungs can contain-the sum of all four volumes. Vital capacity (VC). The maximal amount of air that can be forcefully expired after a maximal inspiration. Functional residual capacity (FRC). The amount of air remaining in the lungs after a normal expiration. Inspiratory capacity (IC). The maximal amount of air that can be inspired after a normal expiration. 6 Figure 3. Long volumes and capacities for a normal adult male. The milliliter values given for these volumes and capacities in Figure 3 are for a normal adult male. In the female they are all 20% to 25% smaller. The respiratory volumes can be measured with a simple instrument called a spirometer. This consists of a lightweight plastic bell inverted in a drum filled with water. A mouthpiece and hose allow the collection of air in the inverted bell. In this experiment you will use your own disposable mouthpiece. Record your results in the table on your worksheet. Procedures The spirometers will be set up and demonstrated by the instructor. Place a clean mouthpiece on the spirometer, and a clean noseclip (or fingers) on the subject’s nose to prevent leakage of air. With Chart running, have the subject breath through the spirometer until the ventilation pattern becomes relatively normal. You will use these breaths to make your measurements of tidal volume and minute ventilation. Next, after an exhalation the subject should inhale maximally, then exhale back to normal exhalation volume. This provides a measure of inspiratory capacity. After taking a few more normal breaths, have the subject stop at the end of an exhalation, then exhale further as much as possible. This provides a measure of expiratory reserve volume. Finally, have the subject inhale as much as possible, then exhale as much as possible, to give the vital capacity. 7 Auscultation of Heart Sounds (Optional) Auscultation of the heart means to listen to and study the various sounds arising from the heart as it pumps blood. These sounds are the result of vibrations produced when the heart valves close and blood rebounds against the ventricular walls or blood vessels. The heart sounds may be heard by placing the ear against the chest or by using a stethoscope. The vibrations producing the sounds can be visually displayed through the use of a heart sound microphone and physiological recorder to produce a phonocardiogram. There are four major heart sounds, but only the first two can be heard without use of special amplification. First heart sound. Produced at the beginning of systole when the atrioventricular (AV) valves close and the semilunar (SL; the aortic and pulmonary) valves open. This sound has a low-pitched tone commonly termed the “lub” sound of the heartbeat. Second heart sound. Occurs during the end of systole and is produced by the closure of the SL valves, the opening of Figure 1. The four auscultatory areas. the AV valves, and the resulting vibrations in the arteries and ventricles. Owing to the higher blood pressures in the arteries, the sound produced is higher pitched than the first heart sound. It is commonly referred to as the “dub” sound. Third heart sound. Occurs during the rapid filling of the ventricles after the AV valves open and is probably produced by vibrations of the ventricular walls. Fourth heart sound. Occurs at the time of atrial contraction and is probably due to the accelerated rush of blood into the ventricles. Procedure Using a stethoscope, listen to your partner’s heart sounds, paying special attention to the four major auscultatory areas on the chest where the sounds from each valve can be heard most clearly (Figure 1). 8 Electrocardiogram Background The electrocardiogram (ECG or EKG) detects the action potentials that occur in the heart using skin surface electrodes. The waveforms seen in the EKG result from a combination of the degree of depolarization at any given time, the direction of travel of the AP propagation, and the location of the electrodes. Medical EKG’s use a twelve lead (= electrode) system to allow detection of subtle alterations in heart electrical function. In lab, we will use a modified form of the original three lead system. The normal EKG contains the following components: P wave – Represents the depolarization of the atrial muscle as AP’s spread from the sinoatrial node. PR segment – The delay between atrial and ventricular ECG events is caused in part by the antrioventricular node. QRS complex – The major components of this complex are the QR segment, which reflects the wave of depolarization passing down the ventricular septum (mainly in the bundle of His), and the RS segment, reflecting the depolarization spreading up the outer walls of the ventricle. ST segment – Represents the plateau phase of the ventricular AP’s, when no changes in membrane potential are occurring. T wave – Represents the repolarization of the ventricular muscle as the AP’s. Figure 2. Key to the components of a normal EKG. Normal durations of phases: P wave 0.1 sec PR segment 0.03-0.06 sec QRS complex 0.08-0.012 sec ST segment 0.08 sec T wave 0.16-0.27 sec Procedure The instructor will demonstrate the procedure for recording an EKG. You will record the ventilation and pulse of your subject as well, using the Pneumotrace and pulse transducer. 9 Note the pattern of the EKG in a sitting subject. How does the timing of the electrical events in the heart compare to the generation of systolic pressure as detected by the pulse transducer? You may also wish to use a stethoscope to see the timing of the heart sounds in comparison to the EKG. Note any changes in heart rhythm with the breathing cycle. Have the subject run up and down several flights of stairs, and then return to the sitting position. Reconnect the EKG leads and note how the pattern of the EKG changes in comparison to the resting state. 10