Erythrocytes
advertisement
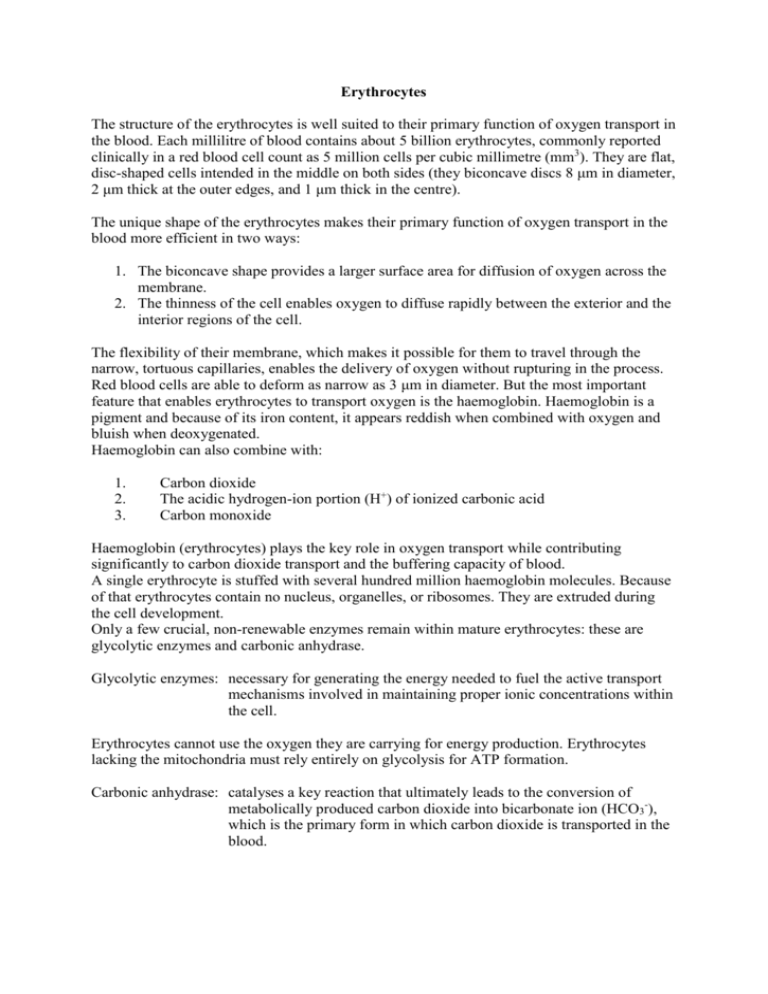
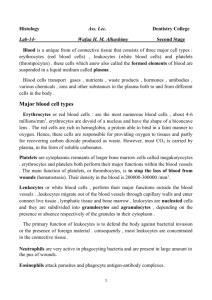
Erythrocytes The structure of the erythrocytes is well suited to their primary function of oxygen transport in the blood. Each millilitre of blood contains about 5 billion erythrocytes, commonly reported clinically in a red blood cell count as 5 million cells per cubic millimetre (mm3). They are flat, disc-shaped cells intended in the middle on both sides (they biconcave discs 8 μm in diameter, 2 μm thick at the outer edges, and 1 μm thick in the centre). The unique shape of the erythrocytes makes their primary function of oxygen transport in the blood more efficient in two ways: 1. The biconcave shape provides a larger surface area for diffusion of oxygen across the membrane. 2. The thinness of the cell enables oxygen to diffuse rapidly between the exterior and the interior regions of the cell. The flexibility of their membrane, which makes it possible for them to travel through the narrow, tortuous capillaries, enables the delivery of oxygen without rupturing in the process. Red blood cells are able to deform as narrow as 3 μm in diameter. But the most important feature that enables erythrocytes to transport oxygen is the haemoglobin. Haemoglobin is a pigment and because of its iron content, it appears reddish when combined with oxygen and bluish when deoxygenated. Haemoglobin can also combine with: 1. 2. 3. Carbon dioxide The acidic hydrogen-ion portion (H+) of ionized carbonic acid Carbon monoxide Haemoglobin (erythrocytes) plays the key role in oxygen transport while contributing significantly to carbon dioxide transport and the buffering capacity of blood. A single erythrocyte is stuffed with several hundred million haemoglobin molecules. Because of that erythrocytes contain no nucleus, organelles, or ribosomes. They are extruded during the cell development. Only a few crucial, non-renewable enzymes remain within mature erythrocytes: these are glycolytic enzymes and carbonic anhydrase. Glycolytic enzymes: necessary for generating the energy needed to fuel the active transport mechanisms involved in maintaining proper ionic concentrations within the cell. Erythrocytes cannot use the oxygen they are carrying for energy production. Erythrocytes lacking the mitochondria must rely entirely on glycolysis for ATP formation. Carbonic anhydrase: catalyses a key reaction that ultimately leads to the conversion of metabolically produced carbon dioxide into bicarbonate ion (HCO3-), which is the primary form in which carbon dioxide is transported in the blood. Erythrocytes – Replacement and production Erythrocytes have a short life span and must be replaced at the average rate of 2 to 3 million cells per second. This is the price erythrocytes pay for their generous content of haemoglobin. Without DNA and RNA, erythrocytes cannot synthesize proteins for cellular repair, growth and division or for renewal of enzyme supplies. Erythrocytes are able to survive an average of only 120 days. In this time each erythrocyte travels about 700 miles through the entire circulatory system. In time, their irreparable plasma membrane becomes fragile and shows the tendency to rupture as the cell squeezes through tight spots in the vascular system. Most of the old erythrocytes have their final destination in the spleen, because this organ has a narrow, winding capillary network. Erythropoiesis (erythrocyte formation): Erythrocytes are produced in the bone marrow (soft, highly cellular tissue that fills the internal cavities of bones). The erythrocyte production takes place in a process known as erythropoiesis. In children most of the bones are filled with red bone marrow, which is capable of erythrocyte production. As a person becomes older, fatty yellow bone marrow, which is incapable of erythrocyte production gradually replaces red bone marrow. Red bone marrow in adults only remains in the sternum, the vertebrae, ribs, base of the skull and in the epiphysis of long limb bones. The red bone marrow synthesizes also leukocytes and platelets as well as erythrocytes, because the bone marrow includes undifferentiated pluripotent stem cells. Regulatory factors act on the hemopoietic marrow to govern the type and number of cells generated and discharged in to the blood. Usually the number of circulating erythrocytes remains constant. But when the erythrocyte concentration in the blood is decreased, the primary stimulus that increases erythrocyte production is the reduced oxygen delivery to the tissues (not the number of erythrocytes in the blood). But the reduced oxygen delivery to the tissues acts not directly on the bone marrow to increase erythropoiesis. In fact the reduced oxygen delivery to the kidneys stimulates them to secrete the hormone erythropoietin into the blood. This hormone in turn stimulates erythropoiesis. Erythropoietin acts on derivatives of undifferentiated stem cells that are already cells committed to become erythrocytes. It stimulates their proliferation and maturation into mature erythrocytes. Once normal oxygen delivery to the kidneys is achieved, erythropoietin secretion stops until it is needed once again. In response to severe loss of erythrocytes (haemorrhage or abnormal destruction of young circulating erythrocytes) the rate of erythropoiesis can be increased to more than six times. But the preparation of an erythrocyte involves several steps, such as synthesis of haemoglobin and extrusion of the nucleus and the organelles. Cells closest to maturity need a few days to be released from the bone marrow. For less developed and newly proliferated cells it will take several weeks before reaching maturity. When demands for erythrocytes production are high (haemorrhage) the bone marrow may release large numbers of immature erythrocytes, known as reticulocytes (contain residual ribosomes and organelle remnants). Their presence above the normal value of 0,5 % to 1,5 % of the total number of circulating erythrocytes indicates a high rate of erythropoietic activity. At very high rates, there can be 30 % of the circulating erythrocytes at the immature reticulocyte stage. In addition to erythropoietin, testosterone (major male sex hormone) increases the basal rate of erythropoiesis. This hormone is responsible for the normally higher hematocrit in male compared to female. Additional erythrocytes in male provide extra oxygen capacity to meet the needs of the larger muscles in male.