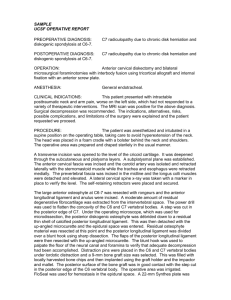
Surgical methods for cruciate ligament repair
advertisement

Database: Ovid MEDLINE(R) <1966 to January Week 3 2004> Search Strategy: -------------------------------------------------------------------------------1 exp Posterior Cruciate Ligament/in [Injuries] (381) 2 exp REHABILITATION/ (137928) 3 rehabilitation.af. or 2 (182323) 4 1 and 3 (47) 5 limit 4 to (human and english language) (39) 6 limit 5 to yr=1996-2004 (22) 7 exp posterior cruciate ligament/su (379) 8 method$.af. and 7 (90) 9 limit 8 to (human and english language) (65) 10 limit 9 to review articles (4) 11 limit 9 to yr=1996-2004 (52) 12 limit 11 to yr=1999-2004 (46) 13 from 12 keep 10,12,17-19,26,33,36-37 (9) 14 12 not 13 (37) 15 6 or 14 (55) 16 from 15 keep 1-55 (55) *************************** <1> Unique Identifier 8914730 Authors L'Insalata JC. Harner CD. Institution Department of Orthopaedic Surgery, University of Pittsburgh, Pennsylvania, USA. Title Treatment of acute and chronic posterior cruciate ligament deficiency. New approaches.[see comment]. [Review] [46 refs] Comments Comment in: Am J Knee Surg. 1996 Fall;9(4):171; PMID: 8914728 Source American Journal of Knee Surgery. 9(4):185-93, 1996 Fall. <2> Unique Identifier 9397264 Authors Noyes FR. Barber-Westin SD. Institution Cincinnati Sportsmedicine and Orthopaedic Center, Ohio, USA. Title Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Use of early protected postoperative motion to decrease arthrofibrosis. Source American Journal of Sports Medicine. 25(6):769-78, 1997 Nov-Dec. Abstract We report a critical rating of results for 11 patients with bicruciate ligament reconstructions and immediate protected knee motion after knee dislocations (seven acute and four chronic). Six patients had concurrent repair or reconstruction of medial ligamentous structures, and six had reconstruction of the lateral and posterolateral ligaments. All patients returned for followup at a mean of 4.8 years postoperatively. Follow-up arthrometric testing at 20 degrees of flexion showed 10 knees had less than 3 mm of increased total anterior-posterior displacement and 1 knee had 7 mm of increase. At 70 degrees of flexion, 9 knees had less than 3 mm of increased displacement and 2 knees had more than 6 mm of increase. The failure rates were as follows: 18% of posterior cruciate ligament reconstructions (2 of 11), 9% of anterior cruciate ligament reconstructions (1 of 11), 17% of lateral and posterolateral procedures, and 0% of medial collateral ligament procedures. At followup, five of the seven patients with acute injuries had no limitations with daily or sports activities. Three of the four patients with chronic ruptures were asymptomatic with daily activities, but only one was asymptomatic with light sports. Five patients (all acute injuries) required treatment for knee motion limitations. Nine patients had full range of motion at followup. We concluded that simultaneous bicruciate ligament reconstructions, performed with associated medial or lateral procedures, are warranted to restore function to all ligament structures. Even though immediate motion was used, several patients required early manipulation or arthroscopic debridement, which restored full motion and prevented permanent arthrofibrosis. <3> Unique Identifier 12239009 Authors Richter M. Bosch U. Wippermann B. Hofmann A. Krettek C. Institution Trauma Department, Hannover Medical School, Hannover, Germany. Title Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Source American Journal of Sports Medicine. 30(5):718-27, 2002 Sep-Oct. Abstract BACKGROUND: Studies of traumatic knee dislocations have failed to provide a consensus regarding the best method of treatment. PURPOSE: Our purpose was to evaluate the results after surgical repair or reconstruction versus nonsurgical treatment and to compare the influence of prognostic factors. STUDY DESIGN: Retrospective study. METHODS: Eighty-nine patients were treated for traumatic knee dislocation. Surgical repair or reconstruction of the cruciate ligaments was performed in 63 patients (repair, 49; reconstruction, 14). In 26 patients, nonsurgical treatment was undertaken. RESULTS: At an average follow-up of 8.2 years, the mean Lysholm and Tegner scores were 75 and 3.7, respectively. The outcome in the surgical group was better than in the nonsurgical group. The scores were higher in patients who were 40 years of age or younger, who had sports injuries rather than motor vehicle accident injuries, and who had undergone functional rehabilitation rather than immobilization. CONCLUSIONS: Surgical repair or reconstruction of the cruciate ligaments was superior to nonsurgical treatment. Functional rehabilitation was the most important positive prognostic factor. Surgical repair or reconstruction of the cruciate ligaments is mandatory to achieve sufficient stability for functional rehabilitation. In cases of cruciate ligament avulsion, repair with transosseous fixation is a reasonable alternative to reconstruction, provided that it is performed within 2 weeks of trauma. Copyright 2002 American Orthopaedic Society for Sports Medicine <4> Unique Identifier 12642252 Authors Stannard JP. Riley RS. Sheils TM. McGwin G Jr. Volgas DA. Institution Department of Surgery, Division of Orthopaedic Surgery, University of Alabama at Birmingham, Birmingham, Alabama 35294-3295, USA. Title Anatomic reconstruction of the posterior cruciate ligament after multiligament knee injuries. A combination of the tibial-inlay and two-femoral-tunnel techniques. Source American Journal of Sports Medicine. 31(2):196-202, 2003 Mar-Apr. Abstract BACKGROUND: Neither operative nor nonoperative treatment of posterior cruciate ligament rupture after multiligament knee injuries have shown very favorable outcomes. HYPOTHESIS: Reconstruction of the posterior cruciate ligament by combining the tibial-inlay and two-femoral-tunnel techniques will result in improved stability and functional outcomes. STUDY DESIGN: Prospective cohort study. METHODS: Twenty-nine patients with 30 posterior cruciate ligament ruptures and multiligament knee injuries treated with the combined technique were evaluated with clinical, radiographic, and functional outcome measures. RESULTS: All patients had a clinical examination result indicating joint stability (0 or 1+) at an average follow-up of 25 months (range, 15 to 39). Twenty-three knees had no laxity, and seven had 1+ laxity. The KT-2000 arthrometer data documented less than 0.5 mm of side-to-side mean difference for both posterior displacement and total anterior-posterior displacement at both 30 degrees and 70 degrees of knee flexion. Knee range of motion was a mean extension of 1 degrees (range, 0 degrees to 10 degrees ) and a mean flexion of 124 degrees (range, 75 degrees to 145 degrees ). Mean Lysholm knee score was 89.4. CONCLUSIONS: Reconstruction with a combination tibial-inlay and twofemoral-tunnel technique provides good results after multiligament knee injuries. All patients had a stable posterior cruciate ligament at most recent clinical follow-up, and 77% had no laxity at all. Copyright 2003 American Orthopaedic Society for Sports Medicine <5> Unique Identifier 12860540 Authors Gill TJ. DeFrate LE. Wang C. Carey CT. Zayontz S. Zarins B. Li G. Institution Orthopedic Biomechanics Laboratory, Massachusetts General Hospital, Boston, USA. Title The biomechanical effect of posterior cruciate ligament reconstruction on knee joint function. Kinematic response to simulated muscle loads. Source American Journal of Sports Medicine. 31(4):530-6, 2003 Jul-Aug. Abstract BACKGROUND: The effectiveness of posterior cruciate ligament reconstruction in restoring normal kinematics under physiologic loading is unknown. HYPOTHESIS: Posterior cruciate ligament reconstruction does not restore normal knee kinematics under muscle loading. STUDY DESIGN: In vitro biomechanical study. METHODS: Kinematics of knees with an intact, resected, and reconstructed posterior cruciate ligament were measured by a robotic testing system under simulated muscle loads. Anteroposterior tibial translation and internal-external tibial rotation were measured at 0 degrees, 30 degrees, 60 degrees, 90 degrees, and 120 degrees of flexion under posterior drawer loading, quadriceps muscle loading, and combined quadriceps and hamstring muscle loading. RESULTS: Reconstruction reduced the additional posterior tibial translation caused by ligament deficiency at all flexion angles tested under posterior drawer loading. Ligament deficiency increased external rotation and posterior translation at angles higher than 60 degrees of flexion when simulated muscle loading was applied. Posterior cruciate ligament reconstruction reduced the posterior translation and external rotation observed in posterior cruciate ligamentdeficient knees at higher flexion angles, but differences were not significant. CONCLUSION: Under physiologic loading conditions, posterior cruciate ligament reconstruction does not restore six degree of freedom knee kinematics. Clinical Relevance: Abnormal knee kinematics may lead to development of long-term knee arthrosis. <6> Unique Identifier 12016068 Authors McAllister DR. Markolf KL. Oakes DA. Young CR. McWilliams J. Institution Biomechanics Research Section, Department of Orthopaedic Surgery, University of California at Los Angeles, Center for Health Sciences, Box 956902, Los Angeles, CA 90095-6902, USA. Title A biomechanical comparison of tibial inlay and tibial tunnel posterior cruciate ligament reconstruction techniques: graft pretension and knee laxity. Source American Journal of Sports Medicine. 30(3):312-7, 2002 May-Jun. Abstract BACKGROUND: Most posterior cruciate ligament reconstruction techniques use a tibial bone tunnel, which results in an acute bend in the graft as it passes over the posterior portion of the tibial plateau. HYPOTHESIS: The tibial inlay technique will result in lower graft pretensions, less laxity, and less stretchout after cyclic loading. STUDY DESIGN: Controlled laboratory study. METHODS: Graft pretensions necessary to restore normal laxity at 90 degrees of knee flexion (laxity match pretension) and anteroposterior laxities at five knee flexion angles were recorded in 12 fresh-frozen knee specimens with bonepatellar tendon-bone posterior cruciate ligament graft reconstructions using both techniques and two femoral tunnel positions. RESULTS: When the graft was placed in a central femoral tunnel, the tibial tunnel reconstruction required an average 15.6 N greater laxity match pretension than the tibial inlay reconstruction. There were no significant differences in mean knee laxities between the tibial tunnel and tibial inlay techniques at any knee flexion angle; both reconstruction techniques restored mean knee laxity to within 1.6 mm of intact knee values over the entire flexion range. CONCLUSIONS: There was no important advantage of one technique over the other with respect to the biomechanical parameters measured. <7> Unique Identifier 12692672 Authors Zantop T. Rusch A. Hassenpflug J. Petersen W. Institution Department of Orthopaedic Surgery, Christian Albrechts University Kiel, Michaelisstr 1, 24105 Kiel, Germany. Title Intra-articular ganglion cysts of the cruciate ligaments: case report and review of the literature. [Review] [16 refs] Source Archives of Orthopaedic & Trauma Surgery. 123(4):195-8, 2003 May. Abstract BACKGROUND: A ganglion can arise as a cystic lesion from a tendon sheath or a joint capsule and contain a glassy, clear, and jelly-like fluid. They can occur within muscles, menisci, and tendons. Intra-articular ganglion cysts of the knee joint are rare. We report on three ganglion cysts of the cruciate ligaments: Two were intercruciate, and one was located around the posterior cruciate ligament. METHODS: The clinical diagnosis was established using magnetic resonance imaging. All patients were treated successfully using arthroscopic debridement by basket punch and shaver. Subsequent histological examination confirmed the diagnosis. RESULTS: All three patients were asymptomatic at the postoperative follow-up of 16-36 months. CONCLUSION: A review of the literature reveals a controversial discussion about the clinical significance as well as the etiology of ganglion cysts arising from the cruciate ligaments. These case reports show that an intra-articular ganglion cyst of the cruciate ligaments is difficult to diagnose. A cyst does not necessarily have to be associated with specific clinical symptoms or a previous trauma. Preoperatively, MRI is essential when diagnosing ganglion cysts of the knee joint. An intra-articular ganglion cyst of the knee joint can be successfully treated by arthroscopy. [References: 16] <8> Unique Identifier 12734718 Authors Schulz MS. Russe K. Weiler A. Eichhorn HJ. Strobel MJ. Institution Orthopaedische Gemeinschaftspraxis Straubing, Hebbelstr 14a, 94315, Straubing, Germany. strobel@ogp.de Title Epidemiology of posterior cruciate ligament injuries. Source Archives of Orthopaedic & Trauma Surgery. 123(4):186-91, 2003 May. Abstract BACKGROUND: The epidemiology of posterior cruciate ligament (PCL) injuries has not been well clarified. Isolated and combined PCL injuries are a frequently missed diagnosis. A better understanding of typical injury mechanisms may help in more accurate diagnosis of these injuries. METHODS: In this study the epidemiology of PCL insufficiency in 494 patients was retrospectively analysed. Stress-radiography was used to quantify posterior tibial displacement. RESULTS: The mean age at the time of injury was 27.5+/-9.9 years. Traffic accidents (45%) and athletic injuries (40%) were the most common injury causes. Motorcycle accidents (28%) and soccer-related injuries (25%) accounted for the main specific injury causes. The most common injury mechanisms were dashboard injuries (35%) and falls on the flexed knee with the foot in plantar flexion (24%). The mean side-to-side difference of posterior tibial displacement on posterior stress-radiographs in 90 degrees of flexion was 13.4+/-4.7 mm. According to the posterior displacement values, 232 (47%) patients had isolated PCL ruptures, while 262 (53%) patients with a posterior displacement of >12 mm were classified as having a combined posterior instability. There were significantly more combined PCL lesions due to vehicular trauma as compared with athletic trauma ( p<0.0001). CONCLUSIONS: In many PCL lesions, initiation of an adequate treatment regimen is delayed despite typical injury mechanisms and symptoms. In the future, a better understanding of the epidemiology of PCL injuries should enable us to diagnose the injury more reliably through a detailed history and a thorough physical and radiographic examination in the acute setting. <9> Unique Identifier 9685095 Authors Zuhosky JP. Dugan SA. Young JL. Bode RK. Kelly JP. Institution Department of Physical Medicine and Rehabilitation, Northwestern University Medical School, Chicago, IL, USA. Title A retrospective review of the incidence and rehabilitation outcome of concomitant traumatic brain injury and ligamentous knee injury. Source Archives of Physical Medicine & Rehabilitation. 79(7):805-10, 1998 Jul. Abstract OBJECTIVES: To estimate the incidence of ligamentous knee injuries in patients with traumatic brain injury (TBI) involved in pedestrian versus motor vehicle collisions (PVMVC), to identify associated risk factors, and to compare rehabilitation outcomes and costs in TBI patients with and without ligamentous knee injury. DESIGN: Retrospective, case control. SETTING: An academic rehabilitation hospital with a large metropolitan referral base. PATIENTS: Twenty-three consecutive adolescent and adult subjects admitted for acute inpatient rehabilitation after a PVMVC from January 1, 1994, to January 1, 1996. RESULTS: Five subjects (22%) were found to have a ligamentous knee injury, one with bilateral injuries. Two of these six injuries were diagnosed only after presentation to the rehabilitation setting. The most common injury was an anterior cruciate ligament (ACL) disruption in 5 of 6 knees. A coupled ACL and medial collateral ligament injury was identified in 4 of 6 injured knees. The risk of ligamentous knee injury was most closely associated with the presence of a tibial plateau fracture (n=3) (chi2=12.420, p < .001). There was no statistical difference between groups with and without ligamentous knee injuries with respect to age, gender, inpatient acute or rehabilitation length of stay, admission, discharge, or change in motor Functional Independence Measure (FIM) interval measures, or rehabilitation costs. Four of the 5 patients with ligamentous knee injuries were successfully managed nonoperatively. A case illustrating longitudinal management is presented. CONCLUSIONS: TBI and ligamentous knee injuries, in particular ACL injuries, are common comorbidities after PVMVC. Physicians must maintain a high index of suspicion for ligamentous knee injuries in this population, particularly when a tibial plateau fracture is present. TBI patients with and without ligamentous knee injuries can have comparable functional outcomes when the ligament injuries are identified and appropriately managed, without incurring undue cost or length of inpatient rehabilitation. <10> Unique Identifier 12209426 Authors Wheatley WB. Martinez AE. Sacks T. Schurhoff MR. Uribe JW. Hechtman KS. Zvijac JE. Institution UHZ Sports Medicine Institute, Coral Gables, Florida 33146, USA. Title Arthroscopic posterior cruciate ligament repair. Source Arthroscopy. 18(7):695-702, 2002 Sep. Abstract PURPOSE: We present our technique of arthroscopic repair for femoral avulsion soft-tissue tears of the posterior cruciate ligament (PCL) and its results. TYPE OF STUDY: Case series, retrospective review. METHODS: We performed 13 arthroscopic repairs of the PCL and reviewed them retrospectively. Follow-up was available for 11 (85%) patients. Nonabsorbable monofilament sutures were placed through the loose fibers of the ligament and tied over a bone bridge. Patients were evaluated using magnetic resonance imaging, comparative stress views, and according to the scoring systems of Lysholm and Gillquist and the International Knee Documentation Committee (IKDC). RESULTS: Mean follow-up was 51.4 months. IKDC scores revealed 4 (36.4%) patients with normal knee function, and 7 (63.6%) with nearly normal function. Average Lysholm and Gillquist score was 95.4 (90 to 100). All athletes returned to the same or a higher level of competition. CONCLUSIONS: Arthroscopic repair of the PCL in patients with a femoral avulsion is effective in reducing postoperative instability and improving functional outcome. <11> Unique Identifier 12209420 Authors Shafer BL. Simonian PT. Institution Department of Orthopaedics and Sports Medicine, University of Washington, Seattle, Washington 98195-6500, USA. bshafer@u.washington.edu Title Broken poly-L-lactic acid interference screw after ligament reconstruction. Source Arthroscopy. 18(7):E35, 2002 Sep. Abstract The interference screw is a reliable method used to secure tendon to bone and bone to bone in ligament reconstruction. Historically, metal interference screws have been used for this purpose in both anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) reconstruction. However, several problems associated with the use of metal interference screws have led to the increasing use of bioabsorbable implants. Poly-L-lactic acid (PLLA) biodegradable interference screws have been used successfully for graft fixation in ligament reconstruction. Although adverse reactions have been reported with the use of biodegradable implants, late screw breakage is rare. To our knowledge no case exists of late screw breakage with bioabsorbable interference screws used in ligament reconstruction. We present one case in the setting of an ACL reconstruction and one with combined PCL and posterolateral corner reconstruction. <12> Unique Identifier 12098121 Authors Chen CH. Chen WJ. Shih CH. Institution Department of Orthopaedic Surgery, Chang Gung Memorial Hospital, Taoyuan, Taiwan. afachen@doctor.com Title Arthroscopic reconstruction of the posterior cruciate ligament: a comparison of quadriceps tendon autograft and quadruple hamstring tendon graft. Source Arthroscopy. 18(6):603-12, 2002 Jul-Aug. Abstract PURPOSE: Considerable controversies remain on the graft choice and fixation methods in the posterior cruciate ligament (PCL) reconstruction. The purpose of this study was to compare, at minimal 2-year follow-up, the outcomes of PCL reconstruction between using quadriceps tendon autograft and using quadruple hamstring tendon autograft. TYPE OF STUDY: Case series. METHODS: All patients received only PCL reconstruction without combined severe associated posterolateral instability. From 1996 to 1998, there were 24 patients who had a quadriceps tendon autograft, and 30 patients with hamstring tendon autograft. Twenty-two of the quadriceps tendon group and 27 of the hamstring tendon autograft group with 2 more years of complete follow-up were included for final analyses. Clinical assessments consisted of Lysholm knee scores, International Knee Documentation Committee (IKDC) scores, thigh muscle girth and strength, and radiographic evaluation. RESULTS: On the Lysholm knee rating, 86% of patients showed good or excellent results in the quadriceps tendon group and so did 89% of patients in the hamstring tendon group. Fifty-nine percent of the quadriceps tendon group and 56% of the hamstring tendon group revealed a 3- to 5-mm ligament laxity. Two patients with quadriceps tendon grafts and 4 patients with hamstring tendon grafts revealed grade II laxity. The IKDC rating showed no significant difference between the 2 groups in terms of activity level, ligament laxity, and final rating. In the thigh girth side-to-side difference, 82% of the quadriceps tendon group and 78% of the hamstring tendon group had less than a 10-mm difference. CONCLUSIONS: Comparable satisfactory results between the 2 surgical groups were shown at a minimal 2 years follow-up. We suggested that both grafts could afford good ligament reconstruction likelihood and that they are reasonably acceptable graft choices for PCL reconstruction. <13> Unique Identifier 12966378 Authors Huang TW. Wang CJ. Weng LH. Chan YS. Institution Department of Orthopaedic Surgery, Chang Gung Memorial Hospital, Kaohsiung, Taiwan. Title Reducing the "killer turn" in posterior cruciate ligament reconstruction. Source Arthroscopy. 19(7):712-6, 2003 Sep. Abstract PURPOSE: Graft abrasion caused by sharp graft angulation at the graft-tunnel margin of the proximal tibia (the "killer turn") may cause graft failure after posterior cruciate ligament (PCL) reconstruction using the traditional anteromedial route tibial tunnel. One method to reduce the graft angulation is to use the anterolateral route tibial tunnel. However, less acute graft angulation may increase joint translation because of a decrease in graft compressive force. The purpose of this study was to compare the graft angulation and joint translation between anteromedial and anterolateral route tibial tunnels. TYPE OF STUDY: Biomechanical study. METHODS: Twelve above-the-knee amputation specimens were used in this study. Anteromedial and anterolateral tibial tunnels were made at the desired locations, and the same femoral tunnel was used. Graft angulation was measured by inserting a malleable pin into the tibial and femoral tunnels. Measurements of graft angulation were performed with the knee in extension and in 90 degrees of flexion. The joint translation was measured by the posterior translation of the tibia on the femur at 90 degrees of flexion with a 15-lb posterior force applied to the anterior proximal tibia after PCL reconstruction through the respective tunnels. RESULTS: The difference in graft angulation between anterolateral and anteromedial route tibial tunnels was statistically significant (P <.001); however, the difference in joint translation showed no statistical significance between the 2 tunnel routes. CONCLUSIONS: The anterolateral route tibial tunnel significantly reduced the sharp graft angulation ("killer turn") at the graft tunnel margin of the proximal tibia, but it did not increase the joint translation as compared with the traditional anteromedial route tibial tunnel. The anterolateral route tibial tunnel is thought to be a better choice when arthroscopic PCL reconstruction is performed with the tunnel technique. <14> Unique Identifier 10524821 Authors Mariani PP. Adriani E. Bellelli A. Maresca G. Institution Orthopaedic Clinic, University of Rome La Sapienza, Italy. ppm.las@iol.it Title Magnetic resonance imaging of tunnel placement in posterior cruciate ligament reconstruction. Source Arthroscopy. 15(7):733-40, 1999 Oct. Abstract The aim of this study was to define a reproducible method for evaluating posterior cruciate ligament (PCL) reconstructions using magnetic resonance imaging (MRI). A 2-fold investigation was performed. In part I, the "footprints" of an intact PCL were located on MRI and their coordinates were defined. Measurements were made on the images of 50 subjects using axial, coronal, and sagittal planes. Interobserver variability was calculated by averaging the measurements of the 2 reviewers and using the Kappa coefficient. Three points of reference were located: tibial attachment on the tibial axial plane, and two femoral attachments on the sagittal and coronal oblique planes. In part II, stability of 20 PCL reconstructions with a bone-patellar tendon-bone (BPTB) autograft were evaluated and scored using the IKDC evaluation form after a 2year follow-up. Stability was evaluated clinically and instrumentally using a KT-2000 arthrometer at 89 N with the knee flexed at a neutral quadriceps knee angle of approximately 70 degrees . Seven cases were graded A (0 to 2 mm), 11 graded B (3 to 5 mm), and 2 graded C (6 to 10 mm). All patients had an MRI after an average of 16 months (range, 12 to 24 months, 2 SD). The previous measurements from part I of the study were used to make a correlation between achieved stability and tunnel location. A 1-factor analysis of variance (ANOVA), nonparametric ANOVA, and the Fisher Exact test were used to determine if clinical outcome of the 3 groups was influenced by graft placement. At MRI evaluation, excessive deep placement was observed in 4 cases and a correlation between improper femoral tunnel location and stability was statistically significant (P < .05). A correct placement of tibial tunnel was observed in all patients. In our analysis, proper location of the femoral tunnel seems to be more critical and difficult to achieve than tibial tunnel placement, probably because of the lack of specific anatomic landmarks during surgery. <15> Unique Identifier 11774140 Authors Mariani PP. Margheritini F. Camillieri G. Bellelli A. Institution Rome University of Motor Sciences, Department of Diagnostic Radiology, San Pietro Hospital FBF, Rome, Italy. ppm.las@iol.it Title Serial magnetic resonance imaging evaluation of the patellar tendon after posterior cruciate ligament reconstruction. Source Arthroscopy. 18(1):38-45, 2002 Jan. Abstract PURPOSE: Our purpose was to prospectively analyze serial changes in magnetic resonance imaging (MRI) signal of the bone-patellar tendon-bone autograft when used for posterior cruciate ligament (PCL) reconstruction and to retrospectively determine at mid-term follow-up the relationship between MRI graft appearance and clinical stability in patients who have undergone arthroscopic PCL reconstruction with a bone-patellar tendon-bone autograft. TYPE OF STUDY: One prospective serial blinded study and 1 retrospective blinded study. METHODS: The first part of the study focused on MRI scans obtained at 3, 6, 9, and 12 months postoperatively in a case series of 10 consecutive patients who underwent arthroscopically assisted PCL reconstruction (group A), and of 10 patients who underwent combined ACL-PCL arthroscopic reconstruction (group B). For the second part of the study, MRI scans were obtained in a retrospective series of 10 patients at mid-term follow-up after PCL arthroscopic reconstruction (group C). Signal intensity of 3 zones, corresponding to the proximal, middle, and distal intra-articular graft zones, was evaluated according to the Howell et al. classification. Fiber continuity assessment was performed using a modified Kuhne et al. score. The signal intensity of the 3 zones was independently scored. Knee stability was clinically and instrumentally graded according to the IKDC evaluation form (group 4). A multivariance analysis and grouped t test were used for statistical evaluation. RESULTS: In group A, the average MRI evaluation score was 7.65 +/- 1.6 at 3 months, 3.8 +/- 0.6 at 6 months, 4.75 +/- 1 at 9 months and 6.25 +/- 1.2 at 1 year. The portion of graft exiting the femoral tunnel exhibited increased signal and faster maturation than the tibial tunnel. In group B (combined ACL-PCL reconstruction), the graft showed slower graft healing with an average MRI score of 4.85 +/- 0.7 at 3 months, 1.9 +/- 0.7 at 6 months, 3.9 +/- 0.9 at 9 months, and 5.3 +/- 1.1 at 1 year. At 1 year follow-up, there was no correlation between MRI appearance and stability in group A, even with MRI findings of fiber continuity. However, at long-term evaluation (group C), a strict correlation between MRI appearance and achieved stability was found. CONCLUSIONS: The patellar tendon when used for PCL reconstruction requires more than 1 year to achieve a low-signal intensity over its entire course, and the distal zone near the tibial tunnel shows a slower healing process. MRI graft assessment is useful only 1 year or more following PCL reconstruction. <16> Unique Identifier 11536101 Authors Kim SJ. Shin SJ. Cho SK. Kim HK. Institution Department of Orthopaedic Surgery, Arthroscopic Surgery Unit, Yonsei University College of Medicine, Seoul, Korea. os@yumc.yonsei.ac.kr Title Arthroscopic suture fixation for bony avulsion of the posterior cruciate ligament. Source Arthroscopy. 17(7):776-80, 2001 Sep. Abstract We describe a new arthroscopic technique for suture fixation of a posterior cruciate ligament (PCL) avulsion fracture from the tibia. This technique is indicated when the size of the avulsed fragment is small and fixation with a screw or pins is inadequate. Three portals are used: a parapatellar anteromedial portal, a high posteromedial portal, and a posterolateral portal. Using a PCL tibial guide, 2 bone tunnels are made from the anterior cortex of the tibia to the medial and lateral border of the avulsed site. One or 2 strands of 23-gauge wire or multiple nonabsorbable sutures are used for fixation through the tunnels. If the bony fragment is small or comminuted, fixation with wires or sutures leads to rigid fixation and early rehabilitation. <17> Unique Identifier 11536088 Authors Mariani PP. Margheritini F. Camillieri G. Institution Rome University of Motor Sciences, Rome, Italy. ppm.las@iol.it Title One-stage arthroscopically assisted anterior and posterior cruciate ligament reconstruction. Source Arthroscopy. 17(7):700-7, 2001 Sep. Abstract PURPOSE: To retrospectively evaluate 15 consecutive patients who underwent simultaneous isolated, arthroscopically assisted anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) reconstruction. Type of Study: Case series. METHODS: A bone-patellar tendon-bone autograft was used as the PCL substitute and doubled hamstring tendons were used as the ACL graft. The IKDC evaluation form and the HSS, Lysholm, and Tegner clinical rating scales were used to make clinical evaluations. Anteroposterior translation was measured with the KT-2000 arthrometer and stress view radiography. RESULTS: At final IKDC evaluation, 3 patients (20%) were graded A, 7 (46.7%) were graded B, 3 (20%) were graded C, and 1 patient (6.7%) was graded D. One patient underwent revision surgery in another hospital for severe postoperative residual laxity. Two Cgraded patients had an unsatisfactory outcome as a result of serious complications related to knee injuries. All patients with a grade A or B returned to sports activity. At stress view examination, mean posterior side-toside translation measured at the lateral tibial plateau was 5.8 +/- 1.1 mm and the mean translation at the medial tibial plateau was 7.3 +/- 1.5 mm; the mean anterior dislocation was 3.3 +/- 0.4 mm. The preoperative HSS score rated an average of 32 +/- 9. Postoperatively, the average score reached was 89.6 +/8.3. The preoperative Lysholm score was 65.5 +/- 9.1 (range, 48 to 78) in patients with chronic lesions and at follow-up was 95.1 +/- 4.5 (range, 88 to 100). The average Tegner activity score decreased in patients with chronic lesions from 6.9 +/- 1.7 (range, 4 to 9) before injury to 5.5 +/- 1.6 (range, 2 to 9) at follow-up (P =.053 ). At follow-up, 7 patients (50%) returned to their preinjury level after surgery. CONCLUSIONS: These results show the effectiveness and safety of simultaneous arthroscopic reconstruction of both cruciate ligaments using autografts that can adequately restore satisfactory stability, even in the presence of minimal peripheral laxity (1 degrees or 2 degrees ). We conclude that the use of autografts can restore ligament function with good patient compliance and without significant surgical complications. <18> Unique Identifier 10976124 Authors Makris CA. Georgoulis AD. Papageorgiou CD. Moebius UG. Soucacos PN. Institution Department of Orthopaedic Surgery, University of Ioannina Medical School, Ioannina, Greece. grakos@otenet.gr Title Posterior cruciate ligament architecture: evaluation under microsurgical dissection. Source Arthroscopy. 16(6):627-32, 2000 Sep. Abstract PURPOSE: Our objective was to verify the fiber anatomy of the posterior cruciate ligament (PCL) and to measure the main dimensions and the femoral and tibial attachment site distances of the ligament after microsurgical dissection. We hypothesized that PCL anatomy is more complex than the 2 traditionally characterized bands. TYPE OF STUDY: This is a purely anatomic description of microdissections of the PCL, focused on the fine anatomy of the ligament. MATERIALS AND METHODS: Twenty-four fresh-frozen cadaveric knees were dissected using magnifying loupes and an operative microscope, being careful to avoid creating artificially separated bundles. The main dimensions of the PCL were measured using a micrometer. RESULTS: The anterior, central, posteriorlongitudinal, and posterior-oblique were the 4 fiber regions identified based on their orientation and the osseous sites of their insertions. These were partially separable anatomically but were functionally distinct. The anterior and central fiber regions made up the bulk of the ligament, while the remaining 15% consisted of the posterior fiber regions. During manual joint motion, the behavior of these fiber regions was observed. The anterior fiber region appeared to be the most nonisometric and remained in tension mainly between 30 degrees and 90 degrees of flexion. The posterior fiber regions appeared to be the most isometric (especially the posterior-oblique) and remained in tension mainly in extension and partially in deep flexion. The central fiber region appeared to have an intermediate behavior and remained in tension mainly between 30 degrees and 120 degrees of flexion. Additionally, it appeared to be the widest of all fiber regions. CONCLUSIONS: These findings should be of interest and help in interpreting some of the anatomy encountered during arthroscopic examination of the PCL, both from the anterior and posterior lateral portals. Furthermore, this information should prove useful in selecting treatment for the PCL. <19> Unique Identifier 10976129 Authors Espejo-Baena A. Lopez-Arevalo R. Urbano V. Montanez E. Martin F. Institution Department of Orthopaedic Surgery, University Hospital of Malaga, Malaga, Andalucia, Spain. Title Arthroscopic repair of the posterior cruciate ligament: two techniques. Source Arthroscopy. 16(6):656-60, 2000 Sep. Abstract SUMMARY: Isolated posterior cruciate ligament injuries are rare and their treatment is controversial. These lesions have commonly been treated by open reduction and internal fixation using a posterior approach. However, this approach makes it difficult to explore other combined injuries of the knee joint. We report 2 cases of posterior cruciate ligament avulsion of the tibia that were arthroscopically reduced and fixed using 2 different methods, cannulated screws and tension band wire. <20> Unique Identifier 11078536 Authors Brand J Jr. Hamilton D. Selby J. Pienkowski D. Caborn DN. Johnson DL. Institution Alexandria Orthopaedics and Sports Medicine, Alexandria, Minnesota, USA. Title Biomechanical comparison of quadriceps tendon fixation with patellar tendon bone plug interference fixation in cruciate ligament reconstruction. Source Arthroscopy. 16(8):805-12, 2000 Nov. Abstract PURPOSE: The purpose of this study was to use current fixation techniques and compare the stiffness and ultimate tensile failure of the tendinous end of the quadriceps tendon (QT) with the bone plug end of the bone-patellar tendon-bone (BPTB) graft using current techniques of fixation. Type of Study: Randomized trial of elderly cadaver knees. Materials and Methods: Tibial and femoral biodegradable interference fixation and femoral EndoButton (Smith & Nephew, Acufex, Mansfield, MA) fixation in bone tunnels with the QT and the BPTB graft were compared by using 10 pairs of elderly cadavers and biomechanical testing. Two groups, fixation at time zero (simulating fixation in the operating room) and testing after 1, 000 loading cycles (simulating patient rehabilitation exercises), were used. RESULTS: At time zero fixation, stiffness of the soft tissue QT tibial tunnel interference fixation was 59% less stiff than the stiffness of the interference fixation of a BPTB plug in a femoral tunnel (P =.11). The EndoButton femoral fixation resulted in a decrease in stiffness at time zero compared with femoral tunnel interference fixation of the soft tissue QT (P =.03). All groups improved stiffness with cycling the construct to 1,000 cycles. CONCLUSIONS: Placement of the QT tendinous end of the graft in the femoral bone tunnel when using a interference fixation will approximate the stiffness of a bone plug in the tibial bone tunnel with interference fixation. The EndoButton fixation is not as stiff as either of the femoral interference fixation options. The addition of more than 20 loading cycles could remove laxity from the graft fixation-graft cruciate ligament complex and improve its stiffness. <21> Unique Identifier 11078535 Authors Matava MJ. Sethi NS. Totty WG. Institution Department of Orthopaedic Surgery, Washington University, St. Louis, Missouri, USA. matavam@msnotes.wustl.edu Title Proximity of the posterior cruciate ligament insertion to the popliteal artery as a function of the knee flexion angle: implications for posterior cruciate ligament reconstruction. Source Arthroscopy. 16(8):796-804, 2000 Nov. Abstract PURPOSE: The purpose of this study was to determine if an optimal knee flexion angle existed that would minimize the risk of neurovascular injury from the passage of transtibial hardware during posterior cruciate ligament (PCL) reconstruction. Type of Study: Cadaveric. Materials and Methods: Fourteen freshfrozen cadaveric knees were mounted in a Plexiglas apparatus that could be set at 5 different knee flexion angles (0 degrees, 45 degrees, 60 degrees, 90 degrees, and 100 degrees ) while joint distention was maintained. Each knee underwent magnetic resonance imaging in the axial and sagittal planes at each of the 5 flexion angles to determine the distance between the PCL tibial insertion and popliteal artery. RESULTS: The mean distance, over all 5 flexion angles, between the PCL insertion and the popliteal artery in the axial plane was 7.6 mm, whereas the mean distance in the sagittal plane was 7.2 mm. There was a significant increase in distance with progressive flexion in both planes. Maximum mean distances were noted at 100 degrees of flexion in both the axial (9.9 mm) and sagittal (9.3 mm) planes. An artificial line mimicking the path of a transtibial drill passed through the popliteal artery in 10 of 10 cases at the 0 degrees, 45 degrees, 60 degrees, and 90 degrees angles, and in 6 of 10 cases at the 100 degrees angle. CONCLUSIONS: The results of this study suggest that increasing knee flexion reduces, but does not completely eliminate, the risk of arterial injury during arthroscopic PCL reconstruction. <22> Unique Identifier 12209425 Authors Brand JC Jr. Cole J. Sumida K. Caborn DN. Johnson DL. Institution Alexandria Orthopaedics and Sports Medicine, Alexandria, Minnesota, USA. Title Radiographic analysis of femoral tunnel position in postoperative posterior cruciate ligament reconstruction. Source Arthroscopy. 18(7):688-94, 2002 Sep. Abstract PURPOSE: The purpose of this study was to test the hypothesis that plain radiographs are accurate in assessing femoral tunnel positions in posterior cruciate ligament (PCL) reconstruction. TYPE OF STUDY: Cadaveric study. METHODS: Femoral tunnels were drilled in cadaveric distal femurs using standard techniques at the 12 o'clock, 1:30, and 3 o'clock positions in the left femora and at the 12 o'clock, 10:30, and 9 o'clock positions in the right femora. At each of the three positions, a 9-mm tunnel was drilled with its anterior edge 2 mm posterior to the articular surface of the medial femoral condyle (MFC). Posterior or "malpositioned" tunnels were drilled with the anterior edge 11 mm posterior to the articular surface of the MFC. Four radiographs; a true lateral, a 10 degrees externally rotated lateral, a 10 degrees internally rotated film in the sagittal plane, and an anteroposterior (AP) radiograph were then taken of each tunnel with a radiopaque dilator in the tunnel. All radiographs were analyzed with the 4-quadrant method (4 is the posterior quadrant) and the ratio method (0 is anterior and 1 is posterior). The AP radiograph was measured using a new technique, the intersection of the angle of a line through the center of the femoral tunnel and a line placed tangential to the femoral condyles. RESULTS: Means were calculated for each of the 6 tunnel positions on the 4 radiographs (lateral, external rotation, internal rotation, and AP). Of the 15 comparisons among tunnel postions, 13 could be discriminated using the lateral and AP radiographs. The high-anterior (HA) (12 o'clock position) could not be differentiated on any radiograph from the high-posterior (HP) (12 o'clock position). The internally rotated lateral radiograph could discriminate the midanterior (MA) (1:30 and 10:30 positions) from the low-anterior (LA) (the 3 and 9 o'clock positions). CONCLUSIONS: Three radiographs; the AP, lateral, and internally rotated lateral, can be used to detect a significant difference in the majority of tunnel locations. The tunnel positions that could not be differentiated with these measurements were posterior and may not be clinically important. We concluded that a plain radiograph is an accurate indicator of PCL tunnel position. <23> Unique Identifier 12861215 Authors Oakes DA. McAllister DR. Institution University of California, Los Angeles, Department of Orthopaedic Surgery, Los Angeles, California 90095-6902, USA. Title Failure of heat shrinkage for treatment of a posterior cruciate ligament tear. Source Arthroscopy. 19(6):E1-4, 2003 Jul-Aug. Abstract Incomplete tears or traumatic elongations of either the native cruciate ligaments or cruciate ligament reconstructions represent a therapeutic dilemma for orthopaedic surgeons. We report a case of a partially torn posterior cruciate ligament that was treated unsuccessfully with an electrothermal shrinkage procedure. Although the use of thermal energy to selectively shrink tissues may ultimately prove to be an invaluable tool, the lack of welldesigned, randomized controlled studies to firmly establish its efficacy in the treatment of partial cruciate injuries mandates cautious use of this technique at this time. <24> Unique Identifier 12861201 Authors Stannard JP. Sheils TM. Institution McGwin G. Volgas DA. Alonso JE. Department of Orthopaedic Surgery, University of Alabama at Birmingham, Birmingham, Alabama 35294-3295, USA. James.Stannard@ortho.uab.edu Title Use of a hinged external knee fixator after surgery for knee dislocation. Source Arthroscopy. 19(6):626-31, 2003 Jul-Aug. Abstract PURPOSE: This study documents short-term clinical outcomes in patients with knee dislocations after blunt trauma and evaluates the compass knee hinge (CKH) external fixator for their treatment. TYPE OF STUDY: Nonrandomized prospective functional outcome study. METHODS: Forty patients with 43 knee dislocations were evaluated. Twelve knees underwent ligament reconstruction followed by placement of a CKH; this was group A. Group B included 27 knees that underwent the same treatment and rehabilitation protocol except that an external brace was used rather than a CKH. RESULTS: Thirty-six patients with 39 knee dislocations underwent follow-up ranging from 14 to 41 months (mean, 24). Four patients with 4 knee dislocations were lost to follow-up (1 group A, 3 group B). Group A underwent 27 knee ligament procedures with 2 (7%) failures based on clinical examination. Group B underwent 102 ligament procedures with 30 (29%) failures (P <.05). Anterior cruciate ligament (ACL) reconstruction revealed that 7 group A patients experienced 1 (14%) failure and 25 Group B patients experienced 7 (28%) failures. Posterior cruciate ligament (PCL) reconstruction in 7 group A patients included no failures, and 20 PCL reconstructions in group B included 1 failure. Reconstruction of the posterolateral corner (PLC) yielded no failures in 2 group A patients and 5 (25%) of 20 in group B. Repair of 8 PLCs in group A yielded 1 (12.5%) failure and 26 PLC repairs in group B had 14 (54%; P =.05). SF-36 data revealed low mean values with no significant differences between groups with current enrollment. CONCLUSIONS: Knee dislocation after blunt trauma requires aggressive surgical treatment and physical therapy. In the short-term evaluation, the CKH allows aggressive physical therapy without placing repaired or reconstructed ligaments under high stresses that can result in failure. <25> Unique Identifier 14608330 Authors Lee MC. Park YK. Lee SH. Jo H. Seong SC. Institution Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul, South Korea. leemc@snu.ac.kr Title Posterolateral reconstruction using split Achilles tendon allograft. Source Arthroscopy. 19(9):1043-9, 2003 Nov. Abstract Injury to the cruciate ligaments of the knee commonly occurs in association with posterolateral instability, which can cause severe functional disability including varus, posterior translation, and external rotational instability. Failure to diagnose and treat an injury of the posterolateral corner in a patient who has a tear of the cruciate ligament can also result in the failure of the reconstructed cruciate ligament. Unlike isolated posterior cruciate ligament injury, there seems to be a consensus of opinion that injury to the posterolateral corner, whether isolated or combined, is best treated by reconstructing the posterolateral corner along with the coexisting cruciate ligament injury, if combined. Commonly proposed methods of reconstructing the posterolateral corner have focused on the reconstruction of the popliteus, the popliteofibular ligament, and the lateral collateral ligament. We introduce a new technique for reconstructing the posterolateral corner using a split Achilles tendon allograft. Our method reasonably addresses the several pitfalls in the reconstruction of the posterolateral corner, including (1) concurrent reconstruction of important posterolateral structures, (2) regaining the isometry of the lateral collateral ligament, (3) repositioning the reconstructed popliteus into its original position, and (4) providing a secure fixation method. <26> Unique Identifier 14608326 Authors Chen CH. Chen WJ. Shih CH. Institution Department of Orthopaedic Surgery, Chang Gung Memorial Hospital, Kweishan, Taoyuan, Taiwan. afachen@doctor.com Title Double-bundle posterior cruciate ligament reconstruction with quadriceps and semitendinosus tendon grafts. Source Arthroscopy. 19(9):1023-6, 2003 Nov. Abstract This study presents a novel arthroscopic technique for double-bundle reconstruction of the posterior cruciate ligament. A quadriceps tendon-patellar bone autograft is used to reconstruct the major anterolateral bundle. An additional double-stranded semitendinosus tendon is used to reconstruct the posteromedial bundle. In 70 degrees of flexion and full extension with anterior drawer force, the quadriceps tendon graft and semitendinosus tendon graft are fixed inside the anterior aspect of the single tibial tunnel, respectively. An anatomic reconstruction can be achieved by using these 2 autografts. <27> Unique Identifier 14608314 Authors Deehan DJ. Salmon LJ. Russell VJ. Pinczewski LA. Institution Freeman Hospital, Newcastle upon Tyne, UK England. Title Endoscopic single-bundle posterior cruciate ligament reconstruction: results at minimum 2-year follow-up. Source Arthroscopy. 19(9):955-62, 2003 Nov. Abstract PURPOSE: The goal of this study was to evaluate the clinical outcome of single-bundle posterior cruciate ligament (PCL) reconstruction with retention of the PCL remnant and hamstring tendon autograft with interference screw fixation in patients with isolated PCL laxity. TYPE OF STUDY: Prospective case series with minimum 2-year follow-up evaluation. METHODS: Thirty-one patients for whom conservative management had failed underwent surgery using a 4-strand hamstring tendon autograft with interference screw fixation. The median time from injury to reconstructive surgery was 9 months (range, 4 to 120 months). At a minimum of 2 years after surgery, patients were assessed with the International Knee Documentation Committee (IKDC) Knee Ligament evaluation, Lysholm knee score, and KT-1000 instrumented testing. RESULTS: Before surgery, the median Lysholm knee score was 64 (95% confidence interval, 51 to 67). No patient rated knee function as normal, and all patients showed at least grade 2 posterior drawer laxity. At review, the median Lysholm knee score was 94 (95% confidence interval, 83 to 94), 56% rated the knee as normal and only one patient was found to exhibit grade 2 laxity on posterior drawer testing. Before injury, 94% of patients participated in moderate or strenuous activity. This figure fell to 26% after injury and had increased to 63% at review. CONCLUSIONS: Endoscopic reconstruction of PCL laxity using single-bundle 4-strand hamstring tendon autograft, without removal of the PCL stump, provides a significant reduction in knee symptoms and allows 63% of patients to return to moderate or strenuous activity. This is an effective procedure for symptomatic patients who have isolated PCL laxity and for whom conservative management has failed. <28> Unique Identifier 14551544 Authors Ohkoshi Y. Nagasaki S. Yamamoto K. Shibata N. Ishida R. Hashimoto T. Yamane S. Institution Department of Orthopaedic Surgery, Hakodate Central General Hospital, Hakodate, Japan. ohkoshi.myk@nifty.com Title Description of a new endoscopic posterior cruciate ligament reconstruction and comparison with a 2-incision technique. Source Arthroscopy. 19(8):825-32, 2003 Oct. Abstract PURPOSE: We introduce our technique (a new route for the graft) of endoscopic posterior cruciate ligament (PCL) reconstruction and describe the advantages in comparison with the conventional surgical technique. TYPE OF STUDY: Nonrandomized control study. METHODS: The idea of this surgical technique is to minimize graft angulation at the inner edge of the bone tunnel. The tibial entry point of the guide pin is under the tibial lateral subcondylar flare, approximately 1 to 2 cm anterior to the posterior cortex. This creates less graft angulation on the posterior aspect of the tibia. A new drill system has been devised to allow antegrade femoral drilling starting from inside the notch. This method also allows better femoral tunnel orientation. As a substitute graft material, we use autogenous hamstring tendons, and we secure them with an EndoButton (Smith & Nephew, Andover, MA) and post screw. From 1992 to 1995, 43 2-incision PCL reconstructions using autogenous hamstring tendons were performed. From 1995 to 2001, 90 endoscopic PCL reconstructions using looped autogenous hamstring tendons and an EndoButton were performed. Cases were specified according to the inclusion criteria of this study. As a result, 51 patients were included in this study. The 2-incision group comprised 22 patients, and the endoscopic group comprised 29 patients. The clinical evaluation was performed using the International Knee Documentation Committee (IKDC) form. The quadriceps strength was measured using Biodex System II (Biodex, New York, NY). The period of time to achieve 90 degrees flexion after surgery was also compared. RESULTS: No significant differences were seen between the 2 groups tested with respect to the overall IKDC rating score. Side-to-side differences of anteroposterior total laxity (KT-1000, manual maximum) was 3.95 +/- 1.96 mm in the 2-incision group and 2.38 +/- 1.42 mm in the endoscopic group (P <.05). The average time to achieving 90 degrees of flexion after surgery was 16.6 +/- 8.6 days in the 2-incision group and 12.1 +/- 3.5 days in the endoscopic group. Achievement of range of motion in the endoscopic group was significantly shorter. The peak torque of isokinetic contraction in the endoscopic group was significantly greater than in the 2-incision group 1 year after surgery. CONCLUSIONS: Better posterior stability and quicker postoperative recovery of range of motion and muscle strength were advantages of the endoscopic technique over the 2-incision technique in PCL reconstruction. <29> Unique Identifier 9442333 Authors Choi NH. Kim SJ. Institution Department of Orthopaedic Surgery, Eulji Medical Center, Seoul, Korea. Title Arthroscopic reduction and fixation of bony avulsion of the posterior cruciate ligament of the tibia. Source Arthroscopy. 13(6):759-62, 1997 Dec. Abstract Bony avulsion fractures of the posterior cruciate ligament of the tibia have commonly been treated by open reduction and internal fixation using the posterior approach. However, this approach, using the prone position, makes it difficult to investigate and treat other combined injuries of the knee joint. We report a case of posterior cruciate ligament avulsion of the tibia that was arthroscopically reduced and firmly fixed with two cannulated screws. The posterior sag was absent after the operation and the result was excellent. By arthroscopy, we got rigid fixation of the avulsed fragment for early rehabilitation, and detection of a concomitant injury was also possible. <30> Unique Identifier 12966390 Authors McGuire DA. Wolchok JC. Institution Clinical Faculty, Orthopedics and Sports Medicine, University of Washington, Seattle, Washington, USA. Title Posterolateral corner reconstruction. Source Arthroscopy. 19(7):790-3, 2003 Sep. Abstract One should suspect a compromise of the lateral structures when presented with a posterior cruciate ligament (PCL) injury, especially if grade III laxity is present. In our experience, if a combined injury to the PCL and posterolateral corner is diagnosed, a combined PCL and posterolateral reconstruction is needed to restore stability. This article describes a posterolateral reconstruction procedure. This procedure, when used in combination with an intra-articular PCL reconstruction, restores rotary and posterior knee stability. This procedure uses allograft tissue and interference screw fixation, although autograft tissue may be used. <31> Unique Identifier 14551557 Authors Noyes FR. Medvecky MJ. Bhargava M. Institution Cincinnati Sportsmedicine Research and Education Foundation, Cincinnati, Ohio, USA. sbwestin@csmref.org Title Arthroscopically assisted quadriceps double-bundle tibial inlay posterior cruciate ligament reconstruction: An analysis of techniques and a safe operative approach to the popliteal fossa. Source Arthroscopy. 19(8):894-905, 2003 Oct. Abstract The arthroscopically assisted posterior cruciate ligament tibial inlay technique, frequently used in athletic individuals and in revision cases, requires a thorough and comprehensive understanding of posterior knee anatomy. Importantly, variations in the posterior vascular anatomy may be encountered. A safe and methodical posteromedial approach in a layered fashion to achieve proper and safe tibial inlay graft placement and fixation is described. The authors advocate use of a double-bundle quadriceps tendon autograft. Graft position of the double strands, fixation, and tensioning issues are presented. <32> Unique Identifier 10564868 Authors Hara K. Kubo T. Shimizu C. Suginoshita T. Minami G. Hirasawa Y. Institution Department of Orthopaedic Surgery, Kyoto Interdisciplinary Institute Hospital of Community Medicine, Kyoto, Japan. Title A new arthroscopic method for reconstructing the anterior and posterior cruciate ligaments using a single-incision technique: simultaneous grafting of the autogenous semitendinosus and patellar tendons. Source Arthroscopy. 15(8):871-6, 1999 Nov-Dec. Abstract We established a simultaneous reconstruction method for ruptured anterior and posterior cruciate ligaments (ACL, PCL) using a single-incision technique. Residual PCL was used to determine the position of bone tunnel for ACL reconstruction. The bone tunnel position on the tibia for PCL reconstruction was arthroscopically confirmed by conducting through debridement from the posteromedial portal. Reconstruction substitutes were patellar-tendon bonetendon-bone for ACL, and semitendinosus tendon for PCL. In the fixation procedure, the PCL substitute was fixed using the Endobutton (Smith & Nephew, Andover, MA) and a ceramic button, and the ACL substitute was fixed with an interference screw. During the surgery, radiographic monitoring and the PCL guide system were not required. <33> Unique Identifier 14551559 Authors Veselko M. Saciri V. Institution Department of Traumatology, University Medical Center, Ljubljana, Slovenia. matjaz.veselko@mf.uni-lj.si Title Posterior approach for arthroscopic reduction and antegrade fixation of avulsion fracture of the posterior cruciate ligament from the tibia with cannulated screw and washer. Source Arthroscopy. 19(8):916-21, 2003 Oct. Abstract Avulsion fracture of the posterior cruciate ligament (PCL) is a rare condition, and arthroscopically assisted reattachment of the surgical fixation of the fragment is not always an easy task. Only a few reports describe techniques for arthroscopic fixation of avulsion of the PCL.We report on a case treated arthroscopically with reduction and antegrade fixation of an avulsion fracture of the tibial attachment of the PCL with a cannulated screw and washer through an additional posterolateral portal. Postoperative morbidity was reduced, and rehabilitation was accelerated. Fixation with a cannulated screw and washer is technically simple and allows for stable fixation and immediate postoperative mobilization and pain-limited weight-bearing, even in cases of a comminuted fragment. The safe zone for an additional posterolateral portal and the technique for placing instruments and a guidewire to avoid neurovascular structures is defined. <34> Unique Identifier 12209427 Authors Fanelli GC. Edson CJ. Institution Department of Orthopaedic Surgery, Geisinger Medical Center, Danville, Pennsylvania 17822, USA. gfanelli@geisinger.edu Title Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Source Arthroscopy. 18(7):703-14, 2002 Sep. Abstract PURPOSE: This study presents the 2- to 10-year results of 35 arthroscopically assisted combined anterior cruciate ligament and posterior cruciate ligament (ACL/PCL) reconstructions evaluated preoperative and postoperatively using Lysholm, Tegner, and Hospital for Special Surgery knee ligament rating scales, KT-1000 arthrometer testing, stress radiography, and physical examination. TYPE OF STUDY: Case series. METHODS: This study population included 26 men and 9 women with 19 acute and 16 chronic knee injuries. Ligament injuries included 19 ACL/PCL/posterolateral instabilities, 9 ACL/PCL/medial cruciate ligament (MCL) instabilities, 6 ACL/PCL/posterolateral/MCL instabilities, and 1 ACL/PCL instability. All knees had grade III preoperative ACL/PCL laxity and were assessed preoperatively and postoperatively with arthrometer testing, 3 different knee ligament rating scales, stress radiography, and physical examination. Arthroscopically assisted combined ACL/PCL reconstructions were performed using the single-incision endoscopic ACL technique and the single femoral tunnel-single bundle transtibial tunnel PCL technique. PCLs were reconstructed with allograft Achilles tendon (in 26 cases), autograft bonepatellar tendon-bone (BPTB) (in 7 cases), and autograft semitendinosus/gracilis (in 2 cases). ACLs were reconstructed with autograft BPTB (16 cases), allograft BPTB (12 cases), Achilles tendon allograft (6 cases), and autograft semitendinosus/gracilis (1 case). MCL injuries were treated with bracing or open reconstruction. Posterolateral instability was treated with biceps femoris tendon transfer, with or without primary repair, and posterolateral capsular shift procedures as indicated. RESULTS: Postoperative physical examination revealed normal posterior drawer/tibial step-off in 16 of 35 (46%) knees. Normal Lackman and pivot-shift test results were found in 33 of 35 (94%) knees. Posterolateral stability was restored to normal in 6 of 25 (24%) knees, and tighter than normal knee results were found in 19 of 25 (76%) knees evaluated with the external rotation thigh foot angle test. In this group, 30 degrees varus stress testing was normal in 22 of 25 (88%) knees, and grade 1 laxity was found in 3 of 25 (12%) knees. 30 degrees valgus stress testing was normal in 7 of 7 (100%) surgically treated MCL tears, and in 7 of 8 (87.5%) brace-treated knees. Postoperative KT-1000 arthrometer testing mean side-to-side difference measurements were 2.7 mm (PCL screen), 2.6 mm (corrected posterior), and 1.0 mm (corrected anterior) measurements, a statistically significant improvement from preoperative status (P =.001). Postoperative stress radiographic side-to-side difference measurements measured at 90 degrees of knee flexion and 32 lb posteriorly directed proximal force were 0 to 3 mm in 11 of 21 (52.3%) knees, 4 to 5 mm in 5 of 21 (23.8%), and 6 to 10 mm in 4 of 21 (19%) knees. Postoperative Lysholm, Tegner, and HSS knee ligament rating scale mean values were 91.2, 5.3, and 86.8, respectively, showing a statistically significant improvement from preoperative status (P =.001). CONCLUSIONS: Combined ACL/PCL instabilities can be successfully treated with arthroscopic reconstruction and the appropriate collateral ligament surgery. Statistically significant improvement is noted from the preoperative condition at 2- to 10-year follow-up using objective parameters of knee ligament rating scales, arthrometer testing, stress radiography, and physical examination. Postoperatively, these knees are not normal, but they are functionally stable. Continuing technical improvements will probably improve future results. <35> Unique Identifier 10656979 Authors Toutoungi DE. Lu TW. Leardini A. Catani F. O'Connor JJ. Institution Cambridge Consultants Ltd., Science Park, Milton Rd, Cambridge, UK. Title Cruciate ligament forces in the human knee during rehabilitation exercises. Source Clinical Biomechanics. 15(3):176-87, 2000 Mar. Abstract OBJECTIVE: To determine the cruciate ligament forces occurring during typical rehabilitation exercises.Design. A combination of non-invasive measurements with mathematical modelling of the lower limb.Background. Direct measurement of ligament forces has not yet been successful in vivo in humans. A promising alternative is to calculate the forces mathematically. METHODS: Sixteen subjects performed isometric and isokinetic or squat exercises while the external forces and limb kinematics were measured. Internal forces were calculated using a geometrical model of the lower limb and the "dynamically determinate one-sided constraint" analysis procedure. RESULTS: During isokinetic/isometric extension, peak anterior cruciate ligament forces, occurring at knee angles of 35-40 degrees, may reach 0.55x body-weight. Peak posterior cruciate ligament forces are lower and occur around 90 degrees. During isokinetic/isometric flexion, peak posterior cruciate forces, which occur around 90 degrees, may exceed 4x bodyweight; the anterior cruciate is not loaded. During squats, the anterior cruciate is lightly loaded at knee angles up to 50 degrees, after which the posterior cruciate is loaded. Peak posterior cruciate forces occur near the lowest point of the squat and may reach 3.5x body-weight. CONCLUSIONS: For anterior cruciate injuries, squats should be safer than isokinetic or isometric extension for quadriceps strengthening, though isokinetic or isometric flexion may safely be used for hamstrings strengthening. For posterior cruciate injuries, isokinetic extension at knee angles less than 70 degrees should be safe but isokinetic flexion and deep squats should be avoided until healing is well-advanced. RELEVANCE: Good rehabilitation is vital for a successful outcome to cruciate ligament injuries. Knowledge of ligament forces can aid the physician in the design of improved rehabilitation protocols. <36> Unique Identifier 11240057 Authors Durselen L. Hehl G. Simnacher M. Kinzl L. Claes L. Institution Institute of Orthopaedic Research and Biomechanics University of Ulm -Medical Faculty, Helmholtzstr. 14, 89081 Ulm, Germany. lutz.duerselen@medizin.uni-ulm.de Title Augmentation of a ruptured posterior cruciate ligament provides normal knee joint stability during ligament healing. Source Clinical Biomechanics. 16(3):222-8, 2001 Mar. Abstract OBJECTIVE: To identify an augmentation technique which would provide mechanical protection for the healing posterior cruciate ligament. DESIGN: Six human knee specimens were tested in vitro for posterior knee joint stability after augmenting the cut posterior cruciate ligament by six different techniques using a resorbable double strand Polydioxanone augmentation device. BACKGROUND: A fresh isolated rupture of the posterior cruciate ligament is often treated conservatively. Results have shown that it can heal, but ligament elongations occur frequently. Therefore a method is needed to provide posterior knee joint stability during ligament healing. METHODS: The effect of different femoral augmentation insertions on posterior knee stability was tested by recording the antero-posterior (AP) position of the tibia and the augmentation force. Testing was performed during flexion--extension cycles and under posterior shear loads. RESULTS: The insertion combination that proved to stabilize the joints best consisted of one augmentation strand leading along the antero-lateral posterior cruciate ligament fibres and inserting at the distal end of the Blumensaat line and one strand leading along the posteriormedial fibres and inserting in the middle of the Blumensaat line. AP translations similar to those occurring in healthy knee joints could be achieved. CONCLUSIONS: It is possible to restore normal posterior knee joint stability by implanting a double strand augmentation device. This can help a posterior cruciate ligament to heal under non-elongated conditions. <37> Unique Identifier 10512342 Authors MacLean CL. Taunton JE. Clement DB. Regan WD. Stanish WD. Institution School of Human Kinetics, University of British Columbia, Vancouver, Canada. Title Eccentric kinetic chain exercise as a conservative means of functionally rehabilitating chronic isolated insufficiency of the posterior cruciate ligament. Source Clinical Journal of Sport Medicine. 9(3):142-50, 1999 Jul. Abstract OBJECTIVE: To determine the efficacy of a home eccentric kinetic chain exercise program in improving isokinetic strength, knee function, and symtomatology in athletes with isolated posterior cruciate ligament (PCL) injury. DESIGN: Experimental design. SETTING: Allan McGavin Sports Medicine Centre, University of British Columbia, Vancouver, British Columbia, Canada. PARTICIPANTS: The study included 13 athletes with isolated PCL injury (n = 13) and 13 healthy sedentary subjects (n = 13). All participants were men and between 18 and 35 years of age. The group with isolated PCL injury all had been diagnosed at the Allan McGavin Sports Medicine Centre, all had been treated without surgery, and had been injured at least 6 months ago. Diagnosis was based on presentation of a positive posterior sag and posterior drawer. INTERVENTION: The group with isolated PCL injury (treatment group) underwent 12 weeks of eccentric kinetic chain exercise. The control group of healthy sedentary individuals did not undergo any form of rigorous training during the course of this study. Both groups were tested for isokinetic strength, knee function, and symptomatology at weeks 0, 6, and 12. Compliance was insured through frequent phone contact and progressive journal records of completion of daily exercise. Only those who completely executed the 12-week exercise program were included in the study. MAIN OUTCOME MEASURES: Hamstring and quadriceps isokinetic torque (Nm) at constant velocities of 60 and 120 degrees per second (degrees/s), Tegner Hop Test (meters), and Lysholm Knee Scale scores. RESULTS: A subject-versustreatment data analysis clearly indicated significant increases in eccentric and concentric torque over the 12-week period in the treatment group. Tegner Hop Test and Lysholm Knee Scale scores also increased significantly after the eccentric squat exercise program. Quadriceps eccentric/concentric ratios at both testing velocities increased significantly after 12 weeks of rehabilitation. There were no significant differences in strength between extremities in the treatment group at any time during the course of this study. Before rehabilitation, there were no significant differences between eccentric and concentric torque values in either muscle group (quadriceps and hamstrings) of the treatment group. After the eccentric exercise program, the quadriceps in the injured extremity did exhibit significantly greater eccentric than concentric torque. The treatment group was significantly weaker than the control group in eccentric torque at both testing velocities at week 0. After the 12-week exercise program, however, there were no significant differences between groups in eccentric quadriceps strength. CONCLUSION: The results of this investigation support the eccentric squat program as a viable means of functionally rehabilitating chronic PCL insufficiency. <38> Unique Identifier 10078139 Authors Kim SJ. Kim HK. Kim HJ. Institution Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea. Title Arthroscopic posterior cruciate ligament reconstruction using a one-incision technique. Source Clinical Orthopaedics & Related Research. (359):156-66, 1999 Feb. Abstract Thirty-seven patients with a posterior cruciate ligament injury underwent arthroscopic posterior cruciate ligament reconstruction using a one-incision technique with bone-patellar tendon-bone autograft or allograft. The tibial tunnel was started at the distal end of the graft donor site on the proximal tibia and exited posteriorly at the flat spot 15 mm below the articular margin and just lateral to the midline. The femoral tunnel was made through the lateral anterolateral portal. The 25 mm long proximal bone plug was passed easily through the tibial tunnel using a specially designed suture pusher and guided into the femoral tunnel by pulling the leading suture with the knee flexed 30 degrees. Firm proximal and distal fixations were achieved with interference screws. At a minimum 2 year followup (range, 24-68 months), average knee ligament evaluation scores were 91.1 (range, 67-99) in the Lysholm knee scoring scale and 89.3 (range, 67-99) in the Hospital for Special Surgery knee ligament rating form. The average side to side difference of the posterior translation measured by the KT 2000 arthrometer was 6.08 (range, 5-7 mm) mm preoperatively and 2.2 (range, 0-6 mm) mm postoperatively. There were no significant differences between the acute and the chronic cases. The results of the isolated posterior cruciate ligament injury group were better than the combined ligamentous injury group. The one-incision technique minimizes injury to the extensor mechanism, especially the vastus medialis obliquus muscle, and medial scar. Rigid fixation of the long proximal bone plug allows early rehabilitation. <39> Unique Identifier 10918965 Authors Irrgang JJ. Fitzgerald GK. Institution Department of Physical Therapy, University of Pittsburgh School of Health, Pennsylvania, USA. jirrgang@pitt.edu Title Rehabilitation of the multiple-ligament-injured knee. [Review] [40 refs] Source Clinics in Sports Medicine. 19(3):545-71, 2000 Jul. Abstract Rehabilitation for a patient with a multiple-ligament knee injury should be designed to reduce pain and swelling, restore range of motion, strength, and endurance, and to enhance proprioception, and dynamic stability of the knee, with the goals of restoring function and minimizing disability. The biomechanics of the knee must be considered when designing a rehabilitation program. General guidelines for rehabilitation of the multiple-ligament-injured knee include considerations for promoting tissue healing, decreasing pain and swelling, restoring full motion, increasing muscular strength and endurance, improving proprioception, enhancing dynamic stability of the knee, and reducing functional limitations and disability. A patient's progression through this sequence must be individualized and depends on the pattern of ligament injury or surgical procedure that was performed, and the principles of tissue healing. Specific guidelines for rehabilitation following ACL reconstruction combined with MCL repair, PCL reconstruction, combined ACL-PCL reconstruction, and reconstruction of the LCL and posterolateral corner have been provided. [References: 40] <40> Unique Identifier 10028122 Authors St Pierre P. Miller MD. Institution Department of Surgery, Madigan Army Medical Center, Tacoma, Washington, USA. Title Posterior cruciate ligament injuries. [Review] [62 refs] Source Clinics in Sports Medicine. 18(1):199-221, vii, 1999 Jan. Abstract Treatment of posterior cruciate ligament (PCL) injuries has received renewed attention over the past few years. This article reviews the anatomy, natural history, and pathophysiology of posterior cruciate ligament injuries. Also described are the physical examination and proper imaging modalities used to diagnose the injury. Appropriate operative and nonoperative management methods are discussed. [References: 62] <41> Unique Identifier 14519354 Authors Wang CJ. Chen HS. Huang TW. Institution Department of Orthopedic Surgery, Chang Gung Memorial Hospital at Kaohsiung, Kaohsiung, Taiwan. w281211@adm.cgmh.org.tw Title Outcome of arthroscopic single bundle reconstruction for complete posterior cruciate ligament tear. Source Injury. 34(10):747-51, 2003 Oct. Abstract PURPOSE: To evaluate the clinical outcome and correlate the results and degenerative change of the affected knees with the duration of injury, ligament laxity and follow-up time in 30 patients with 31 knees undergoing arthroscopic single bundle reconstruction for complete posterior cruciate ligament (PCL) tear with 2-9-year follow-up. MATERIALS AND METHODS: This series included 22 men and 8 women with an average age of 32 years. High-energy trauma accounts for 93.5% of PCL injury, while only 6.5% are sports related. Arthroscopic single bundle PCL reconstruction was performed in all knees. The average follow-up time was 40 (range: 24-108) months. The methods of evaluation included functional assessment, ligament laxity and radiograph of the knee. RESULTS: The overall clinical results showed 77.4% satisfactory (61.3% excellent and 16.1% good) and 22.6% unsatisfactory (16.1% fair and 6.5% poor). Complete restoration of ligament stability was noted in 52% of the knees with one third showing mild (05 mm) and 9.7% moderate (5-10 mm) ligament laxity. The incidence of radiographic degenerative changes was 52% (16/31), and it correlated with the duration of injury, severity of ligament laxity and length of follow-up time. CONCLUSION: Arthroscopic single bundle reconstruction produced 77.4% satisfactory clinical results in medium term follow-up. Despite good clinical results, complete restoration of ligament stability was achieved in only 52% of the knees. The incidence of degenerative changes of the affected knees was 52% that correlated with the duration of injury, ligament laxity and follow-up time. <42> Unique Identifier 12379393 Authors Wang CJ. Chen HS. Huang TW. Yuan LJ. Institution Department of Orthopedic Surgery, Chang Gung Memorial Hospital at Kaohsiung, 123 Ta-Pei Road, Niao Sung Hsiang, Kaohsiung, Taiwan. w281211@adm.cgmh.org.tw Title Outcome of surgical reconstruction for posterior cruciate and posterolateral instabilities of the knee. Source Injury. 33(9):815-21, 2002 Nov. Abstract PURPOSE: To evaluate the clinical outcome and the incidence of degenerative changes in 25 patients with 25 knees undergoing surgical reconstruction for combined posterior cruciate ligament (PCL) and posterolateral instabilities of the knee with 2-5-year follow-up. MATERIALS AND METHODS: This series included 16 men and 9 women with an average age of 28 years. The average time from injury to surgery was 10 (range 2-24) months, and the average follow-up time was 40 (range 32-60) months. The mechanisms of injury were 88% due to trauma, and 12% sports related. Arthroscopic single bundle posterior cruciate reconstruction and reconstruction of the posterolateral structures were performed in all cases. Clinical evaluations included functional assessment, ligament laxity and radiograph of the knee. The results were correlated with the duration of injury, the severity of ligament laxity and the follow-up time. RESULTS: The overall results were 68% satisfactory (28% excellent and 40% good) and 32% unsatisfactory (20% fair and 12% poor). Despite functional improvement, complete restoration of ligament stability was observed in only 44% of the knees, while 36% of the knees showed mild (<5 mm), and 20% moderate (5-10 mm) ligament laxity. There was no correlation of the clinical outcome with the duration from injury to surgery. The incidence of degenerative changes of the affected knee was 44%, and the rate correlated with the severity of ligament laxity, the duration from injury to surgery and the length of follow-up time. CONCLUSION: Despite the functional improvement, the currently devised surgical techniques only have modest success in restoration of ligament stability in knees with combined PCL and posterolateral instabilities. Further improvement in surgical technique including a dynamic reconstruction of the popliteus tendon complex seems necessary. The rate of degenerative changes of the affected knee appeared proportional to the duration of injury, the severity of ligament laxity and the length of follow-up time. The results of this study led us to recommend early surgical reconstruction for knees with combined posterior cruciate and posterolateral instabilities. <43> Unique Identifier 11940609 Authors Markolf KL. Zemanovic JR. McAllister DR. Institution Department of Orthopaedic Surgery, University of California at Los Angeles 90095-6902, USA. kmarkolf@mednet.ucla.edu Title Cyclic loading of posterior cruciate ligament replacements fixed with tibial tunnel and tibial inlay methods. Source Journal of Bone & Joint Surgery - American Volume. 84-A(4):518-24, 2002 Apr. Abstract BACKGROUND: The optimal method of replacement of the posterior cruciate ligament with a bone-patellar tendon-bone graft is not known. The purpose of this study was to compare the mechanical responses to cyclic loading tests of bone-patellar tendon-bone allograft replacements fixed to the tibia with one of two methods: a tibial tunnel or a tibial inlay technique. METHODS: The proximal ends of sixty-two posterior cruciate graft replacements, thirty-one fixed with the tibial tunnel technique and thirty-one fixed with the tibial inlay technique in cadaver knees, were subjected to 2000 cycles of tensile force of 50 to 300 N with the angle of pull at 45 to the tibial plateau. The central 10 mm of the medial and lateral halves of previously fresh-frozen bone-patellar tendon-bone preparations from cadaver knees were used as the grafts. Two pairs of tibiae were used for testing; the two types of fixation and the medial and lateral halves of the patellar tendons were distributed between the tibial pairs. Graft thickness was measured at the point of highest anticipated tissue deformation and at two additional locations at distances from these points. The total change in graft length after cyclic loading at an applied force level of 200 N was recorded. Elongation of the graft during loading cycles between 20 and 200 N of applied tensile force was also measured. A repeated-measures analysis of variance was used to compare all measurements between the inlay and tunnel techniques, and between the medial and lateral halves of the graft used for the inlay method. RESULTS: Ten of the thirty-one grafts that had been passed through a tibial tunnel failed at the acute angle before 2000 cycles of testing could be completed; all thirty-one grafts that had been fixed to the tibia with use of the inlay method survived the testing intact. Evaluation of the twenty-one graft pairs that survived testing after both fixation techniques revealed that the grafts that had been fixed with the inlay method had significantly less thinning at all three measurement sites at the completion of testing; the mean reduction of thickness was 40.6% (at the acute angle) in the grafts fixed with the tunnel method and 12.5% (adjacent to the bone block) in those fixed with the inlay method. After 2000 cycles, the mean lengths of the grafts fixed with the inlay and tunnel methods increased 5.9 and 9.8 mm, respectively; 38% of this increase occurred during the first six loading cycles. After both methods of fixation, the mean graft elongation during a loading cycle decreased approximately 50% from cycle 1 to cycle 2000, resulting in an effectively stiffer graft construct. There was no significant difference in any measured parameter between medial and lateral graft halves. CONCLUSIONS: These tests showed that the inlay technique of posterior cruciate ligament replacement was superior to the tunnel technique with respect to graft failure, graft thinning, and permanent increase in graft length. <44> Unique Identifier 12954836 Authors Markolf KL. O'Neill G. Jackson SR. McAllister DR. Institution Department of Orthopaedic Surgery, University of California at Los Angeles, David Geffen School of Medicine, USA. kmarkolf@mednet.ucla.edu Title Reconstruction of knees with combined cruciate deficiencies: a biomechanical study. Source Journal of Bone & Joint Surgery - American Volume. 85-A(9):1768-74, 2003 Sep. Abstract BACKGROUND: Clinical results of dual cruciate-ligament reconstructions are often poor, with a failure to restore normal anterior-posterior laxity. This could be the result of improper graft tensioning at the time of surgery and stretch-out of one or both grafts from excessive tissue forces. The purpose of this study was to measure anterior-posterior laxities and graft forces in knees before and after reconstructions of both cruciate ligaments performed with a specific graft-tensioning protocol. METHODS: Eleven fresh-frozen cadaveric knee specimens underwent anterior-posterior laxity testing and installation of load cells to record forces in the native cruciate ligaments as the knees were passively extended from 120 degrees to -5 degrees with no applied tibial force, with 100 N of applied anterior and posterior tibial force, and with 5 N-m of applied internal and external tibial torque. Both cruciate ligaments were reconstructed with a bone-patellar tendon-bone allograft. Only isolated cruciate deficiencies were studied. We determined the nominal levels of anterior and posterior cruciate graft tension that restored anterior-posterior laxities to within 2 mm of those of the intact knee and restored anterior cruciate graft forces to within 20 N of those of the native anterior cruciate ligament during passive knee extension. Both grafts were tensioned at 30 degrees of knee flexion, with the posterior cruciate ligament tensioned first. Measurements of anterior-posterior knee laxity and graft forces were repeated with both grafts at their nominal tension levels and with one graft fixed at its nominal tension level and the opposing graft tensioned to 40 N above its nominal level. RESULTS: The anterior and posterior cruciate graft tensions were found to be interrelated; applying tension to one graft changed the tension of the other (fixed) graft and displaced the tibia relative to the femur. The posterior cruciate graft had to be tensioned first to consistently achieve the nominal combination of mean graft forces at 30 degrees of flexion. At these levels, mean forces in the anterior cruciate graft were restored to those of the intact anterior cruciate ligament under nearly all test conditions. However, the mean posterior cruciate graft forces were significantly higher than the intact posterior cruciate ligament forces at full extension under all test conditions. Anterior-posterior laxity was restored between 0 degrees and 90 degrees of flexion with both grafts at their nominal force levels. Overtensioning of the anterior cruciate graft by 40 N significantly increased its mean force levels during passive knee extension between 110 degrees and -5 degrees of flexion, but it did not significantly change anterior-posterior laxity between 0 degrees and 90 degrees of flexion. In contrast, overtensioning of the posterior cruciate graft by 40 N significantly increased posterior cruciate graft forces during passive knee extension at flexion angles of <5 degrees and >95 degrees and significantly decreased anterior-posterior laxities at all flexion angles except full extension. CONCLUSIONS: It was not possible to find levels of graft tension that restored anterior-posterior laxities at all flexion positions and restored forces in both grafts to those of their native cruciate counterparts during passive motion. Our graft-tensioning protocol represented a compromise between these competing objectives. This protocol aimed to restore anterior-posterior laxities and anterior cruciate graft forces to normal levels. The major shortcoming of this tensioning protocol was the dramatically higher posterior cruciate graft forces produced near full extension under all test conditions. <45> Unique Identifier 12783997 Authors Simmons R. Howell SM. Hull ML. Institution Department of Mechanical Engineering, Bainer Hall, 1 Shields Avenue, University of California at Davis, Davis, CA 95616, USA. Title Effect of the angle of the femoral and tibial tunnels in the coronal plane and incremental excision of the posterior cruciate ligament on tension of an anterior cruciate ligament graft: an in vitro study. Source Journal of Bone & Joint Surgery - American Volume. 85-A(6):1018-29, 2003 Jun. Abstract BACKGROUND: High tension in an anterior cruciate ligament graft adversely affects both the graft and the knee; however, it is unknown why high graft tension in flexion occurs in association with a posterior femoral tunnel. The purpose of the present study was to determine the effect of the angle of the femoral and tibial tunnels in the coronal plane and incremental excision of the posterior cruciate ligament on the tension of an anterior cruciate ligament graft during passive flexion. METHODS: Eight cadaveric knees were tested. The angle of the tibial tunnel was varied to 60 degrees, 70 degrees, and 80 degrees in the coronal plane with use of three interchangeable, low-friction bushings. The femoral tunnel, with a 1-mm-thick posterior wall, was drilled through the tibial tunnel bushing with use of the transtibial technique. After the graft had been tested in all three tibial bushings with one femoral tunnel, the femoral tunnel was filled with bone cement and the tunnel combinations were tested. Lastly, the graft was replaced in the 80 degrees femoral and tibial tunnels, and the tests were repeated with excision of the lateral edge of the posterior cruciate ligament in 2-mm increments. Graft tension, the flexion angle, and anteroposterior laxity were recorded in a six-degrees-of-freedom loadapplication system that passively moved the knee from 0 degrees to 120 degrees of flexion. RESULTS: The graft tension at 120 degrees of flexion was affected by the angle of the femoral tunnel and by incremental excision of the posterior cruciate ligament. The highest graft tension at 120 degrees of flexion was 169 +/- 9 N, which was detected with the graft in the 80 degrees femoral and 80 degrees tibial tunnels. The lowest graft tension at 120 degrees of flexion was 76 +/- 8 N, which was detected with the graft in the 60 degrees femoral and 60 degrees tibial tunnels. The graft tension of 76 N at 120 degrees of flexion with the graft in the 60 degrees femoral and 60 degrees tibial tunnels was closer to the tension in the intact anterior cruciate ligament. Excision of the lateral edge of the posterior cruciate ligament in 2 and 4-mm increments significantly lowered the graft tension at 120 degrees of flexion without changing the anteroposterior position of the tibia. CONCLUSIONS: Placing the femoral tunnel at 60 degrees in the coronal plane lowers graft tension in flexion. Our results suggest that high graft tension in flexion is caused by impingement of the graft against the posterior cruciate ligament, which results from placing the femoral tunnel medially at the apex of the notch in the coronal plane. <46> Unique Identifier 12063327 Authors Oakes DA. Markolf KL. McWilliams J. Young CR. McAllister DR. Institution Biomechanics Research Section, Department of Orthopaedic Surgery, University of California Los Angeles, 90095-6902, USA. Title Biomechanical comparison of tibial inlay and tibial tunnel techniques for reconstruction of the posterior cruciate ligament. Analysis of graft forces. Source Journal of Bone & Joint Surgery - American Volume. 84-A(6):938-44, 2002 Jun. Abstract BACKGROUND: The tibial inlay technique of reconstruction of the posterior cruciate ligament offers potential advantages over the conventional transtibial tunnel technique, particularly with regard to the graft force levels that develop over a functional range of knee flexion. Abnormally high graft forces generated during rehabilitation activities could lead to stretch-out of the graft during the critical early healing period. The purpose of this study was to compare graft forces between these two techniques and with forces in the native posterior cruciate ligament. METHODS: A load cell was installed at the femoral origin of the posterior cruciate ligament in twelve fresh-frozen cadaveric knees to measure resultant forces in the ligament during a series of knee loading tests. The posterior cruciate ligament was then excised, and the femoral ends of 10-mm-wide bone-patellar tendon-bone grafts were attached to the load cell to measure resultant forces in the grafts. For the tunnel reconstruction, the distal bone block of the graft was placed into a tibial tunnel and thin stainless-steel cables interwoven into the bone block were gripped in a split clamp attached to the anterior tibial cortex. With the inlay technique, the distal bone block was fixed in a tibial trough with use of a cortical bone screw with a washer and nut. The proximal ends of all grafts were pretensioned to a level of force that restored intact knee laxity at 90 degrees of flexion, and loading tests were repeated. RESULTS: There were no significant differences in mean graft forces between the two techniques under tibial loads consisting of 100 N of posterior tibial force, 5 N-m of varus and valgus moment, and 5 N-m of internal and external tibial torque. Mean graft forces with the tibial tunnel technique were approximately 10 to 20 N higher than those with the inlay technique with passive knee flexion beyond 95 degrees. Mean graft forces with both reconstruction techniques were significantly higher than forces in the native posterior cruciate ligament with the knee flexed beyond approximately 90 degrees for all but one mode of loading. CONCLUSIONS: In this cadaveric testing model, neither technique for reconstruction of the posterior cruciate ligament had a substantial advantage over the other with respect to generation of graft forces. <47> Unique Identifier 12634532 Authors Yang CK. Wu CD. Chih CJ. Wei KY. Su CC. Tsuang YH. Institution Department of Orthopedic Surgery, Taiwan Provincial Tao-Yuan General Hospital, Taoyuan City, Republic of China. Title Surgical treatment of avulsion fracture of the posterior cruciate ligament and postoperative management. Source Journal of Trauma-Injury Infection & Critical Care. 54(3):516-9, 2003 Mar. Abstract BACKGROUND: Avulsion fractures of the posterior cruciate ligament have long been regarded as rare injuries. In the past, it was common practice to use cast immobilization as an external adjunct after open reduction and internal fixation of fractures. METHODS: Sixteen patients with displaced avulsion fractures of the posterior cruciate ligament were treated with open reduction and internal fixation between August 1989 and July 1993. Malleolar screws were chosen as fixation devices in 14 patients. In the other two, pull-through sutures were used because the size of the fractured fragments was too small to obtain purchase of screws. The postoperative management protocol evolved from an initial regimen of 6 weeks' immobilization in a cast with the knee flexed to 40 degrees for the first five patients (group I), to 4 weeks' immobilization in a cast for the next six patients (group II), to the present protocol of immediate postoperative range of motion (40-70 degrees) with muscle-strengthening exercises in a functional brace for the last five patients (group III). The average follow-up period was 36 months (range, 24-58 months). Hughston's criteria were used to assess the clinical results. RESULTS: Overall, there were 12 (75%) good and 4 fair (25%) results. There was no poor result. CONCLUSION: Avulsion fractures of the posterior cruciate ligament should be treated with open reduction and stable internal fixation if any displacement is seen on initial radiographs at presentation. With the use of functional brace and aggressive postoperative rehabilitation program (i.e., immediate range of motion of 40-70 degrees with muscle-strengthening exercises), satisfactory results can be expected and achieved. <48> Unique Identifier 11988663 Authors Chen CH. Chen WJ. Shih CH. Institution Department of Orthopaedic Surgery, Chang Gung Memorial Hospital, Kweishan, Taoyuan, Taiwan. afachen@doctor.com Title Arthroscopic reconstruction of the posterior cruciate ligament with quadruple hamstring tendon graft: a double fixation method. Source Journal of Trauma-Injury Infection & Critical Care. 52(5):938-45, 2002 May. Abstract BACKGROUND: Surgical reconstruction is indicated for posterior cruciate ligament (PCL) reconstruction for a grade III or IV injury, combined ligament or meniscus injuries, and chronic symptomatic posterior instability. Considerable controversy continues over the choice of graft tissues. Hamstring tendon has been popular in recent years. The purpose of this study is to prospectively assess the outcomes of PCL reconstruction using quadruple hamstring tendon autograft with a double-fixation technique at minimal 2-year follow-up. METHODS: Only patients who received PCL reconstruction without combined associated posterolateral injury reconstruction were included in the series. A hamstring tendon graft is composed of a quadruple-stranded semitendinosus tendon and gracilis tendon 10 cm in length. An arthroscopic technique using a two-incision method and a double-fixation technique were used. Clinical assessments were performed for 30 patients, of which 27 were available for final outcome analysis. Clinical review of patients included the Lysholm knee scores, International Knee Documentation Committee (IKDC) scores, thigh muscle assessment, and radiographic evaluation. RESULTS: On the Lysholm knee rating, 89% of the patients demonstrated good or excellent results in the final assessment. In the IKDC rating analyses, 56% of the patients revealed 3- to 5-mm ligament laxity. Four patients (15%) had grade II laxity. For the IKDC final rating, 26% were normal and 55% were nearly normal. Seventy-eight percent of the patients had less than a 10-mm difference in thigh girth between their reconstructed and opposite limbs. CONCLUSION: Arthroscopic PCL reconstruction with quadruple hamstring tendon autograft appears to produce acceptable results at a minimal 2-year follow-up. The four-stranded hamstring tendon graft is adequate in graft size and associated with minimal harvesting morbidity. The double-fixation method for the graft could provide a rigid fixation. We believe that this technique could afford good ligament function after reconstruction and could be a reasonably acceptable choice for PCL injury. <49> Unique Identifier 10217236 Authors Yeh WL. Tu YK. Su JY. Hsu RW. Institution Division of Trauma & Emergency Surgery, Chang Gung Memorial Hospital, Taipei, Taiwan, ROC. Title Knee dislocation: treatment of high-velocity knee dislocation. Source Journal of Trauma-Injury Infection & Critical Care. 46(4):693-701, 1999 Apr. Abstract BACKGROUND: We report the outcomes of patients treated with a new arthroscopic treatment modality for knee dislocation after high-velocity trauma. METHODS: Twenty-three patients (12 men, 11 women; 25 knees) with traumatic knee dislocation were treated with this technique. Under arthroscopy with gravity inflow irrigation, the ruptured posterior cruciate ligament was reconstructed with a patellar bone-tendon-bone graft, and the anterior cruciate ligament was debrided subacutely. The collateral ligament, meniscus, and capsules were repaired through additional incisions. RESULTS: The average interval between injury and surgery was 11.1+/-5 days (range, 5 to 25 days). After a mean followup period of 27.2+/-7.86 months, the mean extension was 1+/-2 degrees and the average flexion was 129.6+/-4.91 degrees. The mean Lysholm score was 84. There were no major complications. CONCLUSION: Arthroscopic posterior cruciate ligament reconstruction seems to be an effective treatment for traumatic knee dislocation. <50> Unique Identifier 12355300 Authors Nyland J. Hester P. Caborn DN. Institution Division of Sports Medicine, Department of Orthopedic Surgery, University of Louisville, 550 S. Jackson Street, Louisville, KY 40202, USA. john.nyland@louisville.edu Title Double-bundle posterior cruciate ligament reconstruction with allograft tissue: 2-year postoperative outcomes. Source Knee Surgery, Sports Traumatology, Arthroscopy. 10(5):274-9, 2002 Sep. Abstract In addition to minimizing graft site morbidity, providing stable fixation, and enabling early progressive rehabilitation, the ideal PCL reconstruction would closely simulate natural ligament function. This study retrospectively examined the 2-year postoperative outcomes of 19 athletically active patients referred with clinically symptomatic PCL-deficient knees. Preoperatively 18 patients had severely abnormal knee ligament examination scores, and one had an abnormal score (IKDC). All but one patient was confirmed negative for observable posterolateral corner injury via MRI. Eighteen patients had clinical evidence of posterolateral instability. All patients underwent double-bundle PCL reconstruction (using allograft tissue) without concomitant posterolateral corner reconstruction. Two years after surgery 100% of patients had normal ( n=18) or near normal ( n=1) passive knee joint motion. The results were: one-leg hop test, 58% normal, 37% nearly normal, 5% abnormal; knee ligament examination, 47% normal, 42% nearly normal, 5% abnormal, 5% severely abnormal; knee arthrometry, 2.4+/-2 mm posterior tibial displacement; IKDC subjective assessment section, 47% normal, 42% nearly normal, 5% abnormal, 5% severely abnormal; IKDC symptom-activity level section, 47% normal, 42% nearly normal, 5% abnormal, 5% severely abnormal; final knee ligament evaluation, 47% normal, 42% nearly normal, 5% abnormal, 5% severely abnormal; Lysholm knee scoring scale, 63% excellent, 27% good, 5% fair and 5% poor. Improved stability with clinical ligamentous laxity tests and good IKDC subjective and symptom-activity results 2 years after surgery suggest that for patients with PCL rupture and grade I or II posterolateral instability the double-bundle procedure alone sufficiently restores PCL function through a greater range of knee motion than traditional single-bundle techniques. <51> Unique Identifier 11734868 Authors Harner CD. Fu FH. Irrgang JJ. Vogrin TM. Institution Center for Sports Medicine, Department of Orthopaedic Surgery, University of Pittsburgh Medical Center, South Water Street, Pittsburgh, PA 15223, USA. harnercd@msx.upmc.edu Title Anterior and posterior cruciate ligament reconstruction in the new millennium: a global perspective. [Review] [8 refs] Source Knee Surgery, Sports Traumatology, Arthroscopy. 9(6):330-6, 2001 Nov. <52> Unique Identifier 11528346 Authors Escamilla RF. Fleisig GS. Zheng N. Lander JE. Barrentine SW. Andrews JR. Bergemann BW. Moorman CT 3rd. Institution Michael W. Krzyzewski Human Performance Laboratory, Division of Orthopaedic Surgery and Duke Sports Medicine, Duke University Medical Center, Durham, NC 27710, USA. rescamil@duke.edu Title Effects of technique variations on knee biomechanics during the squat and leg press. Source Medicine & Science in Sports & Exercise. 33(9):1552-66, 2001 Sep. Abstract PURPOSE: The specific aim of this project was to quantify knee forces and muscle activity while performing squat and leg press exercises with technique variations. METHODS: Ten experienced male lifters performed the squat, a high foot placement leg press (LPH), and a low foot placement leg press (LPL) employing a wide stance (WS), narrow stance (NS), and two foot angle positions (feet straight and feet turned out 30 degrees ). RESULTS: No differences were found in muscle activity or knee forces between foot angle variations. The squat generated greater quadriceps and hamstrings activity than the LPH and LPL, the WS-LPH generated greater hamstrings activity than the NS-LPH, whereas the NS squat produced greater gastrocnemius activity than the WS squat. No ACL forces were produced for any exercise variation. Tibiofemoral (TF) compressive forces, PCL tensile forces, and patellofemoral (PF) compressive forces were generally greater in the squat than the LPH and LPL, and there were no differences in knee forces between the LPH and LPL. For all exercises, the WS generated greater PCL tensile forces than the NS, the NS produced greater TF and PF compressive forces than the WS during the LPH and LPL, whereas the WS generated greater TF and PF compressive forces than the NS during the squat. For all exercises, muscle activity and knee forces were generally greater in the knee extending phase than the knee flexing phase. CONCLUSIONS: The greater muscle activity and knee forces in the squat compared with the LPL and LPH implies the squat may be more effective in muscle development but should be used cautiously in those with PCL and PF disorders, especially at greater knee flexion angles. Because all forces increased with knee flexion, training within the functional 0-50 degrees range may be efficacious for those whose goal is to minimize knee forces. The lack of ACL forces implies that all exercises may be effective during ACL rehabilitation. <53> Unique Identifier 11528332 Authors Hooper DM. Morrissey MC. Drechsler WI. McDermott M. McAuliffe TB. Institution Department of Health Sciences, Department of Psychology, University of East London, London E15 4LZ, United Kingdom. Title Validation of the Hughston Clinic subjective knee questionnaire using gait analysis. Source Medicine & Science in Sports & Exercise. 33(9):1456-62, 2001 Sep. Abstract INTRODUCTION: Subjective questionnaires, completed by the patient, are often used to document the status of a disabled knee. The purpose of this study was to validate the Hughston Clinic subjective knee questionnaire by describing how knee kinematics and kinetics correlated to subjective knee scores after knee injury and surgery. METHODS: Five groups were studied: patients 2 (N = 37), 6 (N = 37), and 24 (N = 8) wk after ACL reconstruction (ACLR); patients with a chronic PCL deficiency (N = 9); and uninjured controls (N = 8). A threedimensional motion analysis system and force platform were used to measure flexion angles and knee moments during level walking and stair climbing. RESULTS: Hughston Clinic questionnaire scores were significantly correlated to mechanical descriptors measured during stair ascent and descent in the 2- and 6wk ACLR groups (P < 0.05). The Hughston Clinic questionnaire score was correlated to several kinematic variables in the ACL reconstructed knee at 24 wk postoperative, e.g., knee flexion during walking. In the PCL deficient group, the Hughston Clinic questionnaire score was correlated with several kinetic measures, e.g., the peak moment (knee extensors). The Hughston Clinic questionnaire score was not correlated to knee mechanics in the control group. CONCLUSION: The Hughston Clinic questionnaire score has been shown to be valid in this study as it reflects some mechanical descriptors during activities of daily living in the first 6 wk post ACL reconstruction. The questionnaire also provides information on gait modifications by people coping with knee injuries. <54> Unique Identifier 10623985 Authors Janousek AT. Jones DG. Clatworthy M. Higgins LD. Fu FH. Institution Center for Sports Medicine and Rehabilitation, University of Pittsburgh Medical Center, Pennsylvania, USA. Title Posterior cruciate ligament injuries of the knee joint. [Review] [49 refs] Source Sports Medicine. 28(6):429-41, 1999 Dec. Abstract Posterior cruciate ligament (PCL) injuries have a reported incidence of between 3 and 37%, depending on the clinical setting. The most common mechanism of injury in motor vehicle accidents is a dashboard injury or direct force to the proximal anterior tibia. Sports related injuries result from hyperflexion of the knee with the foot typically plantarflexed. The latter mechanism is the most common cause of isolated PCL injuries, while in the trauma population as many as 95% of patients with knee injuries have combined ligamentous damage. Improved knowledge at an anatomical, biomechanical and clinical level has provided the orthopaedist with a more defined treatment algorithm. Isolated, partial PCL injuries (grades I and II) can best be treated nonoperatively while complete injuries (grade III) may require operative treatment based on clinical symptoms. All combined ligamentous injuries usually respond best with surgical management. [References: 49] <55> Unique Identifier 11980502 Authors Margheritini F. Rihn J. Musahl V. Mariani PP. Harner C. Institution Musculoskeletal Research Center, University of Pittsburgh Medical Center, Pennsylvania 15213, USA. fab.mar@iol.it Title Posterior cruciate ligament injuries in the athlete: an anatomical, biomechanical and clinical review. [Review] [86 refs] Source Sports Medicine. 32(6):393-408, 2002. Abstract Recently, the posterior cruciate ligament (PCL) has become an increasingly popular subject of orthopaedic research and debate. In the past several years, anatomic and biomechanical studies have provided invaluable information concerning the structure and function of the PCL. However, many aspects of PCL injury are still not fully understood. Diagnosis of the injury is often missed because of subtlety of symptoms and clinical findings, and current management strategies of PCL injury have experienced relatively poor clinical outcomes. Controversy exists concerning the most appropriate treatment, especially in cases of isolated PCL injury. The purpose of this review is to present a complete overview of the current knowledge regarding the basic science and clinical aspects of PCL injuries, with a specific focus on the athletic population. [References: 86]