Problem 33-hallucinations2
advertisement

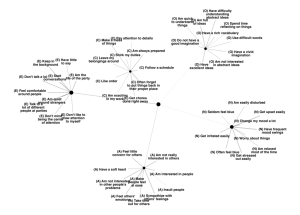
Hallucinations/Disordered thinking Hallucination A false perception arising without an external stimulus: it is experienced as real and vivid and occurring in external space Auditory Visual Somatic Olfactory and gustatory Hypnagogic- when a person goes asleep Extracampine- occurs outside the limit of person’s normal sensory field Functional- a normal sensory stimulus is required to precipitate the hallucination Illusion Misperceptions of real external stimuli e.g. mistaking a dressing gown for a person in a dark room Pseudohallucination Is a perceptual experience which differs from a hallucination, in that it appears to arise in the subjective inner space of the mind, not through one of the external sensory organs. Delusion An unshakeable false belief that is not accepted by other members of the patient’s culture. To the patient they are true The delusion is false because of faulty reasoning The belief is out of keeping with the patient’s social and cultural background Classified as: Primary- do not occur in response to any previous psychopathological state, occur typically in schizophrenia and other primary psychotic disorders Secondary- consequences of pre-existing psychopathological states usually mood disorders Mood congruent or mood incongruent Bizarre or non-bizarre According to the content of the delusion, see table Overvalued ideas A plausible belief that a patient becomes preoccupied with to an unreasonable extent. Key feature- the pursuit of this idea causes considerable distress to the patient or those living around them Circumstantial and tangential thinking Circumstantial- over-inclusion of details however if allowed to finish person comes the original starting point Tangential- speaker diverts from the initial train of thought but never returns to the orginal point Flight of ideas Thinking is markedly accelerated resulting in a stream of connected concepts, links can be normal or through a pun or clang association or through a vague idea Loosening of association When the patients train of thought shifts suddenly from one very loosely or unrelated idea to the next Neologisms and idiosyncratic word use New words created by the patient, often combining syllables of other known words. Patients can use words idiosyncratically by attributing them with unrecognized meaning. Thought blocking A sudden cessation to their flow of thought, often in mid-sentence (observe sudden breaks in speech). Patients have no recollection of this and continue on a different topic. Perservation Patients unnecessarily repeat a word or phrase they have previously expressed-highly suspicious of organic brain disease. Echolalia When patients senselessly repeat words or phrases spoken around them by others-parrot like. Irrelevant answers Give answers completely unrelated to the question Negative symptoms Indicate a clinical deficit and include- marked apathy, poverty of thought and speech, blunting of affect, social isolation, poor self-care and cognitive deficits. Able to differentiate psychotic illness from other causes Bloods- FBC, ESR, U+E, LFTs, thyroid function, glucose, calcium, syphilis serology Urine drug screen EEG, CT ECG- check ok to take anti-psychotics because they prolong QT interval Medical conditions Cerebral neoplasm, infarcts, trauma, infection including HIV, CJD, neurosyphilis, herpes encephalitis Endocrine- thyroid, parathyroid, adrenal disorders Epilepsy- temporal lobe Huntingtons disease SLE Acute intermittent porphyria Vitamin B12 and thiamine deficiency Substances Alcohol Amphetamines Anticholinergics Antiparkinsonian drugs Cocaine Corticosteroids Hallucinogens Inhalants/solvents Organophosphates Phencyclidine Basic pharmacology of antipsychotic drugs Antipsychotics are thought to work by their ability to block dopamine D2 receptors on the mesolimbic dopamine pathway Typical antipsychotics- chlorpromazine, promazine, thioridazine, pipotiazine, trifluoperazine, fluphenazine, haloperidol, flupentixol, zuclopenthixol, sulpiride, pimozide Atypical antipsychotics- clozapine, olanzapine, risperidone, quetiapine, amisulpride Common index conditions Schizophrenia Prevalence- approximately 1% Mid-teens- late thirties, women have later onset First-rank symptoms Delusional perception Delusions of thought control:insertion, withdrawal, broadcast Delusions of control: passivity experiences of affect (feelings), impulse, volition and somatic passivity (influence controlling the body) Hallucinations: audible thoughts (first person or thought echo), voices arguing or discussing the patient, voices giving a running commentary Mood disorders-see other core problems Steroid psychosis- teroid psychosis is a psychotic disorder caused by the use of corticosteroid medications. Affected people develop psychiatric symptoms such as depression and mania. The treatment options vary depending on the patient's preexisting medical condition. Corticosteroids are drugs that mimic cortisol, a hormone produced by the body. They reduceinflammation and suppress the immune system. Doctors prescribe corticosteroid medications such as cortisone and prednisone to treat autoimmune disorders such as lupus and rheumatoid arthritis. Researchers believe steroid psychosis occurs when high doses of corticosteroids cause an increase in dopamine levels in the brain. Increased dopamine levels lead to symptoms such as depression, mood swings and psychosis. Corticosteroids also lower the serotonin levels in the brain, worsening the patient's depressive symptoms. Most patients who develop steroid psychosis begin to manifest symptoms between three and 11 days after starting corticosteroid therapy. Many people become overly excited, irritable or depressed. Others have rapid mood swings, and some become suicidal. Severely affected patients may hallucinate or lose contact with reality. Gender may play a role in determining who develops steroid psychosis. Studies indicate that women are somewhat more likely to develop the condition than men. This may have to do with the fact that women are more likely than men to develop conditions such as lupus that require corticosteroid treatment. Able to specify type of psychotic illness- see flow chart Knows relevant aspects of common law which may need to be applied when managing mentally ill patients, Knows when and how to employ the Mental Health Act- SEE powerpoint on Minerva- search mental health act Jan 2011 Able to manage acutely disturbed or violent patient (e.g. physical restraint, drug therapy)