ARTICLE: Laying Siege to a Deadly Gene
advertisement

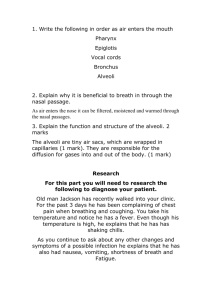
Laying Siege to a Deadly Gene Thanks to a series of breakthroughs, doctors are closing in on a cure for cystic fibrosis By: Andrew Purvis Brianna Oas has never drawn an easy breath. When she was a baby, her tiny chest convulsed at the slightest irritation. Instead of laughing, she would cough: instead of crying, gag. She succumbed to an endless string of respiratory infections-pneumonia, a cold, bronchitis, and pneumonia again-that ordinary antibiotics seamed powerless to curb. Diagnosed with a "failure to thrive," Brianna weighed less at one year than she did at 6 months. Finally, last August, just after the child's third birthday, her anxious parents took her to the University of Washington pulmonary clinic in Seattle. Chest X-rays revealed that thick, bluish mucus had started to accumulate in her airways. "She already had some permanent scarring to the lungs," recalls Dr. Bonnie Ramsey, Brianna's physician and expert in lung disease. "She was a very sick little girl." Brianna was suffering from cystic fibrosis, the most common inherited disorder among whites and a disease that afflicts 25,000 Americans, killing more than 500 every year. Just 10 years ago, the prospects for a girl her age were as bleak as they were inevitable. As the combination of chronic infections, clogged airways and digestive problems took their toll, she could not have expected to outlive her teens. But now, says Ramsey, "Brianna has an excellent chance of living into adulthood." In fact, although Ramsey and other clinicians are reluctant to raise false hopes, Brianna and thousands of other babies born with CF in the past few years may even live to see a cure. Says Ramsey: "In the next decade, we are going to see a revolution in treatment of this disease. We can really, truly think about a cure." In the past two years alone, researchers have reported preliminary success with two separate therapies that for the first time treat the underlying cellular disorder as opposed to just the symptoms of the disease. More promising still, doctors are closing in on a technique for replacing the defective CF gene, which was discovered in 1989. The discovery has spawned an unprecedented proposal to screen tens of millions of Americans for the defect, so that couples can avoid having an affected child. After decades of relative quiet on the CF front, scientists have their eye on the prize. "This is a wonderful place to be right now," says Michael Knowles, a CF researcher at the University of North Carolina. "Just a decade ago, these therapies were abstractions." For half a century, doctors have been treating cystic fibrosis symptom by symptom, doing their best to stem the rising tide of mucus triggered by the disease. As this abnormally thick fluid builds up in the lungs, pancreas, liver, and other organs, it not only serves as fertile ground for damaging infections but also blocks the passage of the vital digestive enzymes to the intestine and stops up sperm in the testes. As a result, patients have difficulty breathing, digesting food, and even reproducing. "This is a disease that simply wears you down," says Ramsey. Using simple therapies, such as clapping young patients on the back and chest several times a day to clear the lungs, or providing a special nutrient-rich diet, scientists have made impressive strides against the ailment, extending the average life span from just five years in the 1950's to 28 today. Recent developments in genetic engineering may refine this tactical approach still further. One drug promises to prevent a protein called elastase, produced in dangerous quantities by the CF patient's own immune cells, from attacking lung tissue. Another synthetic enzyme called DNase instantly dissolves leftover DNA from dead immune cells, one of the bulkiest components of the accumulating mucus. The thinner fluid can then be cleared by the body's own self-cleansing mechanisms. But even such sophisticated mucus busters would do little to stop the buildup of fluid at its source. In the early 1980's, scientists at the University of North Carolina opened the way for a radically new kind of therapy that would attempt just that. The doctors noticed that cells taken from the lungs of CF patients contain abnormally high levels of sodium and chloride -- the constituents of salt. This did not come as a complete surprise, since CF patients’ sweat is known to be abnormally salty, a sign that their bodies do not handle the mineral properly. But the U.N.C researchers realized that this imbalance in the lungs could explain why thick mucus was accumulating there. An excess of salt within cells was leaching water out of the mucus. This apparently was the basic defect behind the disease. In the past 24 months, the U.N.C team hit upon two drugs that could help repair this cellular malfunction. One, a blood pressure medication called amiloride, slows the uptake of sodium. The other, containing naturally occurring substances called ATP and UTP (for adenosine and uridine triphosphate), stimulates the secretion of chloride. Both have proved effective in early trials, although a marketable treatment is still several years away. "The ultimate fantasy," said U.N.C 's Knowles, "would be to give these drugs in tandem to very young children and keep them healthy until another therapy comes along." Another therapy may be coming along sooner than Knowles thinks. Since Francis Collins and Lap-Chee Tsui discovered the CF gene on chromosome 7 in the summer of 1989, researchers from around the world have been struggling to devise a way to bring that finding to the bedside. The challenge: to transport corrected versions of the DNA into the lungs of CF patients. Dr. Ronald Crystal at the National Heart, Lung, and Blood Institute believes the best vehicles are ordinary cold viruses, which (as most people know too well) have a special fondness for the linings of the airway. Ordinarily, these viruses infect host cells by injecting their own DNA through the targets' outer membranes. Crystal hopes to harness this propensity by first disabling the microbes, so that they no longer cause colds, and then inserting a corrected version of the CF gene into the viral DNA. When laboratory rats had this reconstructed virus sprayed into their tiny lungs, they not only absorbed the foreign gene but actually sprouted, in their airways, the human protein that scientists believe will cure CF. (Since the cells that line the lungs are shed periodically, this aerosol gene therapy will probably have to be repeated every two or three months.) While Crystal has yet to try the therapy in humans, he is supremely optimistic: "We now know it works in the test tube and in animals. I can guarantee that we can correct the defective protein in humans.” Another futuristic therapy involves the manipulation of the errant protein itself. This molecule, which scientists have already reconstructed using the blueprint provided by the CF gene, could conceivably be goaded into working properly with the right medication. Alternatively, doctors could implant a healthy version of the CF gene in embryonic mice or goats, harvest the resulting protein from the adult animals' milk, and then spray the protein directly into patients' lungs. "Basically, we're talking about a four-legged manufacturing plant," said Dr. Robert Beall of the Cystic Fibrosis Foundation. The Discovery of the CF gene has revolutionized the diagnosis of CF. Some public health experts believe that since doctors can identify the defective DNA (which occurs in 1 out of 25 Americans) they should screen all prospective parents. Men and women who find that they are both carriers might then choose to adopt or conceive with donor sperm or eggs. Last November the National Institutes of Health financed a handful of pilot projects to help it decide whether a massive screening program would be worth the considerable cost. Many doctors are not so sure. “Just because we technically know how to test for the DNA, doesn’t mean we are ready to do this on a large scale,” asserts Collins. The test is imperfect, he notes; it picks up just 85% of carriers. A positive result, moreover, means only that the couple has a 1 in 4 chance of having a baby with the disease. Without proper counseling, Collins says, people might feel needlessly alarmed. For those already suffering from CF these are exciting but still trying times. The promise of new discoveries is tempered by the knowledge that most patients past puberty have already suffered too much lung damage to be saved by even the most sophisticated therapies. Younger patients have a chance, but there are no guarantees. In Poulsbo, Washington, Brianna Oas’ parents are philosophical. “We’re fully aware that whatever they come up with may not be in time for our daughter,” concedes Jim Oas, a naval-yard manager. Brianna has been in and out of the hospital in recent weeks, but, he adds earnestly, “we are still very hopeful.” For the first time in the history of this devastating disease, that hope is warranted. TIMELINE Before the 1980’s: Doctors understood and treated only the symptoms, including the accumulation of mucus in the lungs and pancreas, chronic infections, and poor digestion. Typical treatments: Clapping on the back, chest, and sides to loosen phlegm; special diets; supplemental enzymes; antibiotics. Early 1980’s: Scientists discovered that cells lining the lungs are high in salt, drawing water from the surrounding mucus. This explains the buildup of thick mucus. Experimental treatments: ATP/UTP and amiloride, which help restore the balance of salt in these cells. 1989: Gene is discovered. Future treatment: A genetically engineered cold virus containing a replacement for the defective gene could be sprayed into the lungs. NOW: Capitalizing on the gene discovery, researchers have identified the protein in the cell wall that causes the salt imbalance and are working to produce quantities of it. Future treatments: An aerosol spray that provides patients with the protein they lack; Drugs that enable the defective protein to work properly.