Appendix 8a - Blackpool Borough Council
advertisement

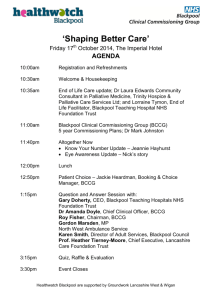
Quality Improvement Strategy For Commissioning High Quality Health and Healthcare June 2012 CONTENT Page INTRODUCTION 3 AIM OF THE STRATEGY 3 PRIORITIES 3 DEFINITIONS 3 QUALITY FRAMEWORK 5 HOW THE QUALITY FRAMEWORK WILL BE IMPLEMENTED 6 MEASURING QUALITY 8 EXTERNAL REGULATORS 10 GOVERNANCE 10 CLINICAL ENGAGEMENT 11 CLINICAL CAPABILITY 11 IMPLEMENTATION OF THE STRATEGY 11 SUMMARY 13 REFERENCES 13 2 1.0 INTRODUCTION Blackpool Clinical Commissioning Group (CCG) commissions a wide range of services for Blackpool people in partnership with Blackpool Council and aims to secure the highest quality and value within finite resources. Delivering the highest quality of care for all is a fundamental goal of the NHS and is priority for Blackpool CCG. This strategy provides positive assurances around quality and safety needed to demonstrate to the Board that high standards of care are commissioned for the people of Blackpool. This Strategy will also provide assurances for external inspectors, regulators, service users and the wider public. 2.0 AIM OF THE STRATEGY To set out the strategic approach Blackpool CCG will ensure that services commissioned on behalf of the population of Blackpool are of the highest quality. The strategy is to ensure that quality is at the heart of Blackpool’s commissioning process and there is commitment in place to continually improve the quality of services for the people of Blackpool 3.0 PRIORITIES Our priorities are to: o o o o o o o 3.1 Improve the patient experience and to listen and act on patient feedback Ensure health care is clinically and financially effective Receive assurances that quality standards are implemented and targets are achieved in Blackpool Support continual improvement in safety and quality outcomes year on year Identify clinical risks and manage underperformance Develop a culture of transparency and consistency to quality improvement Ensure that patients are kept safe during contact with health care Scope All services commissioned by NHS Blackpool will have a contract containing quality schedules based on this strategy. These will include quality indicators, and in some contracts Commissioning for Quality and Innovation incentives (CQUIN). 4.0 DEFINITIONS 4.1 What is quality? Quality is defined in “High Quality Care for All” (DoH, 2008) as encompassing patient safety; patient experience and clinical effectiveness. In addition to quality encompassing patient safety, experience and clinical effectiveness NHS Blackpool have expanded the definition to include timelines, efficiency and equity. ‘Interface’ quality was also seen to be important particularly in relation to communication across provider services. The framework (Figure 1) to support the strategy sets out the approach that NHS Blackpool will take to ensure that the services commissioned on behalf of the people of Blackpool are of the highest quality. The framework will apply to all commissioned and contracted services. All contracts and Service Level Agreements will include quality schedules based on the framework, including service specific quality performance indicators. All newly commissioned pathways will be evidence based and outcome measures will be agreed as part of the development work. 3 Blackpool CCG has made progress in developing itself as the local leader of the NHS; and as an outward facing and proactive commissioning organisation. This commitment has been demonstrated across the whole commissioning cycle, from the development of quality schedules within the contracting framework through to the development of newly procured and commissioned services. 5.0 QUALITY FRAMEWORK OPERATING PRINCIPLES • • • • • • • The patient comes first – not the needs of any organisation Quality is everybody’s business – from the ward to the board; from the supervisory bodies to the Regulators, from the commissioners to primary care clinicians and managers If we have concerns, we speak out and raise questions without hesitation We listen in a systematic way to what our patients and our staff tell us about the quality of care If concerns are raised we listen and ‘go and look’ We share our hard and soft intelligence on quality with others and actively look at the hard and soft intelligence on quality of others If we are not sure what to decide or do, then we seek advice from others The Quality framework will be shaped around the three pillars or goals of High Quality Care for All: • • • Safety Effectiveness Patient Experience Figure 1 5.1 Quality Goal - Safety We will ensure systems are in place to track and manage performance including taking action when required standards are not met. To ensure patient and staff safety, it is important that we encourage learning from mistakes and make changes in practice to ensure that incidents do not repeatedly occur. Where serious incidents occur, Blackpool CCG will be informed within an agreed timeframe and will monitor the investigation and learning from the incident. Blackpool CCG will expect the providers to demonstrate a reduction in HealthCare Associated Infections (HCAI) in line with agreed trajectories. Additionally, there must be robust infection prevention and control plans, policies and capacity in place to demonstrate full compliance with the 4 Health Act 2006 Hygiene Code. We will require infection control reports, root cause analysis (RCA) investigations of infection occurrences and will review data captured from patient/service user experiences reports. Blackpool CCG will ensure that systems and processes are in place to fulfil specific duties of cooperation and best practice in relation to safeguarding is embedded. All contracts and SLAs will require providers to adhere to Blackpool’s Safeguarding policies, which promote the welfare of adults and children. Blackpool CCG will be informed of all incidents involving children and adults, including death or harm, whilst in the care of the provider. We will have senior clinical leadership in the oversight of safeguarding arrangements at Board level for both Adults and Children. Providers will also be required to ensure the safety indicators are in place: 5.2 Ensure National Patient Safety Agency (NPSA) guidance is implemented Identify safeguarding issues relevant to their areas of provision Ensure that policies and procedures related to safety are implemented and monitored Ensure that safe recruitment procedures are in place including vetting and barring requirements of the Independent Safeguarding Authority Staff will be able to identify and report safeguarding concerns Robust incident reporting and monitoring systems that include escalation procedures for serious untoward incidents will be in place Care Quality Commission (CQC) regulations to be met Quality Goal - Effectiveness In order to provide cost and clinically effective care and treatment, providers will be required to comply with national and local standards/guidance such as National Service Frameworks and NICE technology appraisals and guidance. Blackpool CCG will expect to see evidence of compliance with guidance from other professional bodies. We will continue to support the Advancing Quality programme which is based on international best practice to reduce deaths, lengths of stay and readmissions to hospital. Clinical and practice audit is one of the key mechanisms that monitors the performance and quality of services and demonstrates continuous quality improvement at service level. NHS Blackpool will expect all providers to have in place, or continue to have, jointly agreed prioritised clinical and practice audit programmes and demonstrate active participation in audit, including national audits. Providers will be required to share outcomes of clinical and practice audits. Additionally, Blackpool CCG will undertake independent audits where necessary. Through balanced score card and quality framework monitoring, NHS Blackpool will ensure that providers can evidence benchmarking. 5.3 Quality Goal - Patient Experience We will strive to promote compassion, dignity and respect and demonstrating positive patient experiences. Quality will be measured by public perception of the NHS in Blackpool such as outcomes of the annual national patient satisfaction survey and the governmental IPSOS MORI survey. We will shorten feedback cycles of these surveys by monitoring feedback locally using local mechanisms and acting on that feedback. We will inform people of how their involvement in these surveys has improved services. We will facilitate this locally developed engagement mechanism as identified in the Communication and Engagement Strategy. Blackpool CCG will lead on the engagement of public and patients in the planning of services. We have developed ways that will assist all people in Blackpool to have the opportunity to get involved in service development. Providers will be expected to use feedback to improve services. Providers are also expected to work with Blackpool CCG to regularly inform, consult and involve patients, their families and carers and the public in the planning and review of services. The aim of this 5 engagement and improved patient experience is to ensure compassion, by engaging staff and promoting an environment of empathy and listening to service users. We will promote dignity and respect and aim to achieve this by monitoring dignity and single sex accommodation requirements. 5.4 Patient Experience The measures and metrics linked to patient experience that capture real time views and experiences of patients will require extra energy and focus. Existing measures will continue to mature and inform us as commissioners. We will work in partnership to respond to issues of quality raised through patient experience feedback, building on the national programme Patient Reported Outcome Measures (PROMS) and strengthening this through local projects that will build on among others, the implementation of the new complaints system Making Experiences Count. 5.5 How will we respond to poor performance? The quality framework will be embedded into the commissioning arrangements for existing and potential providers using a consistent and robust approach to the commissioning cycle. Figure 3 outlines the approach to poor performance. Figure 3 6. 0 MEASURING QUALITY 6.1 Nationally Agreed Quality Toolkits There are a number of new methodologies to support measuring and analysis of quality. We will utilise these tools to support commissioning performance management and monitoring of contracts. These include: Commissioning for Quality and Innovation (CQUIN) Patient Reported Outcome Measures (PROMs) Quality Accounts Quality Observatories (Advancing Quality Alliance - AQuA) Nationally Agreed Quality Metrics National Quality Board 6 6.2 CQUIN Incentives Part of the quality incentive payment to providers we will continue to encourage achievement of local, regional and nationally agreed quality outcomes. CQUIN is an incentivised money rewarding scheme that has been developed to allocate payments to providers if they meet quality outcomes on domains such as safety, effectiveness and patient experience. CQUIN schemes will focus on an innovative approach to improving the patient/service user experience. This approach can offer incentives up to 2.5% of contract value – robust data capture and milestone monitoring will be agreed with providers. 6.3 PROMs Patient Reported Outcome Measures (PROMs) are questions asked of patients before and after a specific treatment, to measure improvements to quality of life from the patient’s point of view. PROMs are included in provider CQUIN payments. 6.4 Quality Metrics and Quality Markers The vision is that all NHS staff will measure what they do as a basis for improving quality. In partnership with professionals across the NHS, the Department of Health and the NHS Information Centre have identified an initial, but evolving, set of indicators to describe the quality of a broad range of services – the Indicators for Quality Improvement. The long-term vision is to build an extensive menu of indicators that will help every tier of the NHS understand and improve the quality of services it provides to patients/service users. The indicators can be found on the Measuring for Quality Improvement website: http://www.ic.nhs.uk/services/measuring-for-quality-improvement Quality is systemic: it depends upon many different individuals, inputs, process and organisations. It is also, to a degree, subjective. The data required to assess quality, therefore, needs to be drawn from many different sources, to ensure that we are capturing relevant information on the three domains of quality: effectiveness, safety and patient experience. The metrics used to populate the national quality dashboard should be used as a starting point although other data sources should be included. In this context the following is a list of additional sources/areas which should be used. Please note that this is not a comprehensive list; all relevant and appropriate sources should be drawn upon: Performance data on the priorities set out in the Operating Framework relevant to quality (i.e. waiting times, infection rates etc.) • Never Events and serious incident data • CAS alerts closure rates and outstanding issues • Hospital Mortality • Patient survey results, PROMS and other patient data such as Net Promoter scores if available and website material such as NHS Choices) • Staff survey results • Complaints and litigation data • Monitor ratings • CQC inspections - registration details, warning notices and related CQC notifications • Quality Risk Profile data • Quality Accounts • Adult and Child safeguarding • Homicides/unlawful killings – historic and ongoing including action plans • Serious case reviews • Maternity Services, Local Supervisory Midwifery Authority reports and audits 7 • • • • • • 6.5 Data from the Quality Observatory Safety Thermometer and Energising for Excellence Quality impact assessment of Provider Cost Improvement Programmes Peer reviews, recommendations and action plans Clinical Audits/ Confidential enquiries FT Quality assessments National Quality Board The National Quality Board recommend (May 2012) that whilst there have been improvements in recent years in capturing hard data about quality, we must not lose sight of the importance of ‘soft’ intelligence. We have national staff patient surveys included in the dashboard, but in addition we should also be looking at and listening to: • • • • • • Media – traditional and social – negative and positive Patient websites such as Patient Opinion, NHS Choices, local user groups OSCs, local MPs, LinKs, etc. Social Partnership Forum, staff side Professional Regulators and Royal Colleges Trainee feedback / Deanery reports Whistleblowing and similar reports from staff One of the lessons from the National Quality Board assurance visits was that much of the data tended to focus on acute settings. It is crucial that we acknowledge the importance of ensuring that quality data and knowledge is captured for non-acute settings, including primary care, independent sector, ambulances, mental health services, screening programmes under health. The above list is not exhaustive; we will use our judgement and common sense to proactively capture the intelligence that exists within our systems. 7.0 EXTERNAL REGULATORS All service providers are subject to assessment and audit by a range of external regulators and assessors including the Care Quality Commission, Monitor, and Royal Colleges, Peer Reviews, the Health and Safety Executive, the National Audit office and LINKs. It is important that as commissioners we are aware of the findings of all external regulator reports in order to inform commissioning decisions and monitor any required development. 7.1 Care Quality Commission Regulation Essential levels of quality and safety will be externally assessed through the new system of registration with the Care Quality Commission (CQC). Statutory guidance about compliance with registration requirements has been issued by the CQC with more detail on the requirements under each area. Contractors will need to assure the commissioner that they have met the criteria and submitted robust compliance evidence. As commissioners we will work with Providers and monitor compliance as part of the contract monitoring process. 8.0 GOVERNANCE NHS Blackpool reports compliance and exception reports in relation to quality standards through an internal committee structure to the Board. The framework in Figure 5 outlines the reporting arrangements. The quality components of the contracts will be monitored through ongoing Quality Review meetings with providers and by a range of announced and unannounced visits to provider settings. The sub Committee will oversee the provider performance to ensure consistency of achievement. The PPI Forum will be a crucial part of the governance framework relating to patient experience, engagement and involvement in service redesign and delivery. 8 8.1 The Quality Reporting framework Figure 5 Clinical Commissioning Group Board and Committee Structure 1 April 2013 CCG Chairs Network Clinical Commissioning Group Governing Body Commissioning Advisory Board Broken line - Advisory Health and Wellbeing Board Blackpool Safeguarding Adults Board Solid line - Delegated responsibility/authority Quality and Engagement Committee Blackpool Safeguarding Childrens Board Audit Committee Remuneration Committee Patient and Public Involvement Forum Finance and Performance Committee Clinical Commissioning Group Member Practices CCG Board and Committee Structure as at 13 June 2012 NHS Blackpool’s Assurance Framework captures all the organisation’s key risks including commissioning poor quality services. The Assurance Framework is also monitored internally through the Quality and Engagement Sub Committee under delegation authorised by the Clinical Commissioning Group. 9.0 CLINICAL ENGAGEMENT Clinicians who are fully engaged with NHS Blackpool will share its aims for patient safety and care quality and will be committed to helping achieve them. We will establish a structure for clinical engagement that will enable clinicians to be engaged in the purpose, objectives and strategy of NHS Blackpool with a depth of understanding of how we work to achieve high quality, safe, personalised and effective care for all. The importance of clinical engagement is reflected in the partnership working between the Clinical Commissioners across the Fylde Coast; integrated commissioning with Blackpool Council and ongoing collaboration at a Fylde Coast Commissioning Advisory Board. Regular GP link meetings will continue to be held and we are developing a CCG newsletter and website to ensure information is up to date and accessible to clinicians. Implementation of NHS Blackpool’s Communication and Engagement Strategy will support further development and involvement of clinicians in the quality agenda. 10.0 CLINICAL CAPABILITY We need to promote capability building for quality improvement at all levels in the organisation. The appropriate use of staff clinical knowledge to inform the delivery of this strategy is imperative. We will want to encourage quality champions throughout the organisation and develop an open culture for reporting quality errors with providers. Throughout each element of the commissioning cycle, different ‘bundles’ of knowledge will be an essential component to promote quality performance discussions. 9 A key enabler for this strategy is the clinical knowledge necessary to determine and assure quality, safety and clinical effectiveness. The aim will be to develop a clinical knowledge information structure that supports and enables lead commissioners to achieve sustainable improvement in patient safety and quality. The key components essential to achieving this are listed below: NICE Guidance Implementation National Health Services Litigation Authority (NHSLA) Standards Achievement Robust safeguarding arrangements National & Local review recommendations (CQC or SHA) National & Local Clinical Audit findings Local and national research and innovation developments Local and national incident trend analysis Infection control benchmarking analysis Complaints and compliments Serious incident lessons learned evaluations Patient and staff satisfaction surveys Quality Outcomes Framework and Quality Assessment Framework reviews of independent contractors 11.0 IMPLEMENTATION OF THE STRATEGY Through clear approaches to commissioning, contract development and management we will aim to support contractors to deliver improvements in service. In addition local, regional national and international benchmarks will be shared to provide the impetus for quality improvement. The development of a quality dashboard demonstrating progress and areas of concern will be a key way in which commissioners can identify and review performance in relation to quality. 11.1 Quality Ambitions To deliver best practice the following Quality performance indicators will be monitored:No 1.0 QUALITY DOMAIN Safety 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 2.0 2.1 2.2 2.3 Experience OUTCOME No methicillin resistant staphylococcus aureus (MRSA) bacteraemia in hospital more than 48 hours after admission Reduction in clostridium difficile in hospital Achieve and maintain performance for cleanliness in all Blackpool facilities in the top 10% nationally A year-on-year reduction in harm arising from medical and clinical error demonstrated through the National Reporting and Learning System statistics Full implementation of National Patient Safety Agency safe practice guidance To demonstrate learning from complaints, incidents, Serious Untoward Incidents % reduction in falls year on year To demonstrate learning from safeguarding incidents and compliance with national standards Safeguarding concerns are identified, reported and investigated Safeguarding procedures are embedded Elimination of mixed sex accommodation Improvement in national and local Patient Survey results Improved discharge planning and management e.g. 95% discharge letters being transmitted electronically within 24 hours of discharge Promotion of dignity and respect Transparent and accessible complaints procedures in place Engagement with patients and the public embedded 10 3.0 3.1 3.2 Effectiveness 3.3 4.0 Efficiency/ Productivity 4.1 4.2 4.3 4.4 11.2 Learning lessons from complaints and untoward incidents Providers will meet the requirements of CQC registration and regulations Implementation of Technology Appraisal guidance published by the National Institute of Health and Clinical Excellence Progress against an agreed range of clinical metrics e.g. Advancing Quality and Quality Outcomes Framework Partnership working across agencies evident Improvement in National Staff Survey % staff sickness absence reduced % staff turnover compares well with national benchmarks % improvement in staff appraisal through Personal Development Review Implementation of LEAN methodology How will we deliver on these ambitions? We will develop a learning and innovation culture, building effective collaborative partnerships for continuous quality improvement to drive system reform Strong clinical leadership will be recognised as being key to promoting quality All commissioned and contracted services will be expected to participate in the National Patient Safety Campaign facilitated by the National Patient Safety Agency We will learn from best practice nationally and internationally and use the learning to drive forward innovation We will further develop safe and effective prescribing advice The views and experiences of patients will be sought to ensure that they are at the centre of decision making and service development The involvement of patients and the public at all stages of the commissioning cycle (health needs analysis, pathway redesign procurement and evaluation). Through the involvement and empowering of clinicians and teams in developing quality improvement techniques and in service redesign with the aim of Improving clinical value and productivity Through use of the contracting mechanisms with our providers we will incentivise improvements in patient safety, experience and effectiveness We will develop quality dashboards for all the commissioning work stream activities that are consistently reviewed We will utilise the contracting process to penalise unacceptable practice and withhold payments when quality thresholds have not been achieved We will maintain a standardised and consistent approach to quality monitoring and reporting 12.0 SUMMARY The Strategy has set out the context of how NHS Blackpool will commission quality services. It has also set out a draft Quality Framework and a range of quality monitoring approaches. The strategy highlights that there needs to be robust performance management regimes in place to measure quality and to tackle areas of concerns. The quality ambitions and associated work plans will be regularly monitored. The achievement of this strategy cannot be assessed by a single measure – qualitative as well as quantitative data will be reviewed and assessed. In order to achieve continuous quality improvement in the services commissioned by Blackpool CCG the strategy will need to be reviewed annually in order to be responsive to the needs of Blackpool’s resident’s new quality standards emerging external regulators. 11 13.0 REFERENCES Manifesto for the Care Quality Commission. Care Quality Commission (2008). High quality care for all: NHS Next Stage Review final report, Department of Health (DH) Darzi (2008). Using the Commissioning for Quality and Innovation (CQUIN) payment framework DoH (2008). Measuring for Quality Improvement: the approach. Nicholson, D. (2008). From Good to Great vision. 2010/2011 Operating Framework for the NHS. Department Of Health (DH) (2009) Communication and Engagement strategy NHS Blackpool. 2010-2015 Clinical Governance Strategy 2009 - 12 NHS Blackpool. (2009) The Local Authority Social Services and National Health Service Complaints (England) Regulations 2009 Putting Quality First in the Boardroom. The Kings Fund (2010) Review of early warning systems in the NHS (February 2010):Maintaining and improving quality during the transition: safety, effectiveness, experience (March 2011) How to maintain quality during the Transition. National Quality Board (2012) 12