I. Immunosuppression & HIV/AIDS Progression - HHV
advertisement
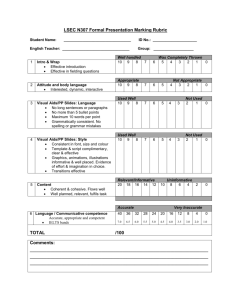
HHV-6 & Immunosuppression, HIV/AIDS, and Autoimmunity Immunosuppression and HIV/AIDS Progression HHV-6 (especially HHV-6A) can cause selective immunosuppression in the otherwise immunocompetent host through a variety of mechanisms (Lusso 2006). In a 2012 study, HHV-6 was identified as a leading cause of transient neutropenia among previously healthy children (Husain 2012). HHV-6 is also associated with transient hypogammaglobulinemia (Kano 2004). Both clinical and experimental evidence suggest that HHV-6A may foster the progression of HIV disease toward AIDS. Synergistic cytopathic effects in primary CD4+ T lymphocytes coinfected in vitro with HHV-6A and HIV-1 have been observed (Lusso 1989). Furthermore, HHV-6 not only upregulates the expression of the primary HIV receptor CD4, but also induces functional CD4 in cells that physiologically do not express it (Lusso 1991; Flamand 1998). Several studies also have shown that HHV-6 infection increases production of inflammatory cytokines that enhance in vitro expression of HIV-1 (Flamand 1991; Inagi 1996; Arena 1997). The first conclusive in vivo evidence that HHV-6A acts as a promoting factor in the progression of immunodeficiency virus disease was observed in experimental coinfection studies in pigtailed macaques (Lusso 2007). Coinfection with HHV-6A was shown to dramatically accelerate the immunological and clinical progression toward AIDS in monkeys infected with a pathogenic simian immunodeficiency virus (SIV) strain. Furthermore, the progression of SIV toward RANTES resistance in macaques has been shown to progress more rapidly to AIDS upon coinfection with HHV-6A (Biancotto 2009). Several clinical observations also suggest a significant role of HHV-6 in AIDS progression. For example, HHV-6 has been frequently isolated from HIVinfected patients (Salahuddin 1986; Levy 1990; Agut 1988) and widespread HHV-6 infection is documented in patients with AIDS at post-mortem examination (Corbellino 1993; Knox 1994). Additionally, sustained HHV-6 replication has been observed in the lymph nodes of HIV-infected patients associated with increased HIV-1 load (Knox 1996; Emery 1999), HHV-6 is frequently reactivated in early symptomatic HIV-1 infected patients (Secchiero 1995), and the disease progression is accelerated in infants with early acquisition of HHV-6 infection (Kositanont 1999). Neurological morbidity in HIV/AIDS patients has also been ascribed to HHV-6 (Corti 2011). While HHV-6 by itself causes significant immunologic damage and dysregulation, the combination of active HIV and HHV-6 leads to more severe immunosuppression in AIDS patients, thereby enhancing the progression of the disease. HHV-6 in Autoimmune Diseases A role for HHV-6 has been proposed in several autoimmune disorders, including autoimmune hemolytic anemia/neutropenia (Yagasaki 2010), autoimmune acute hepatitis (Grima 2008), and multiple sclerosis (TejadaSimon 2003, Alvarez-LaFuente), among others. A 2012 study has linked HHV-6A to Hashimoto’s thyroiditis (HT), a common autoimmune thyroid disease (AITD) (Caselli 2012). The study found that HHV-6 was detected significantly more frequently among thyroid fine needle aspirates (FNA) from HT individuals than controls (82% vs. 10%, respectively), and low-grade acute infection was identified in all HHV-6 positive HT samples compared to 0% of controls. In addition, the group demonstrated that thyroid cells infected with both HHV-6A and HHV-6B became susceptible to NK-mediated killing, providing evidence of a potential mechanism for HHV-6-induced autoimmunity. www.HHV-6Foundation.org HHV-6 & Immunosuppression, HIV/AIDS, and Autoimmunity Selected Abstracts I. Immunosuppression & HIV/AIDS Progression: HHV-6 and the immune system: mechanisms of immunomodulation and viral escape. Lusso P. San Rafaele Scientific Institute, Milano, Italy J Clin Virol. 2006 Dec Clinical and experimental evidence indicates that human herpesvirus 6 (HHV-6) can interfere with the function of the host immune system through a variety of mechanisms. Both HHV-6A and B can infect, either productively or nonproductively, several types of immune cells. The primary target for HHV-6 replication, both in vitro and in vivo, is the CD4+ T lymphocyte, a pivotal cell in the generation of humoral and cell-mediated adaptive immune responses. HHV-6A, but not B, also replicates in various cytotoxic effector cells, such as CD8+ T cells, gammadelta T cells and natural killer cells. In professional antigen-presenting cells like macrophages and dendritic cells, HHV-6 infection is typically nonproductive; yet, it induces dramatic functional abnormalities, including a selective suppression of IL-12, a critical cytokine in the generation of Th1-polarized antiviral immune responses. This and other immunomodulatory effects seem to be mediated by the engagement of the primary HHV-6 receptor, CD46. Moreover, HHV-6 infection results in a generalized loss of CD46 expression in lymphoid tissue, which may lead to an aberrant activation of autologous complement. Additional mechanisms of immunomodulation by HHV-6 include alterations in cell surface receptor expression and cytokine/chemokine production. HHV-6 can also modulate influence responses through the expression of virally-encoded homologs of chemokines and chemokine receptors. By modulating specific antiviral immune responses, HHV-6 can facilitate its own spread and persistence in vivo, as well as enhance the pathogenic effects of other agents, such as human immunodeficiency virus. Infectious etiologies of transient neutropenia in previously healthy children. Husain EH, Mullah-Ali A, Al-Sharidah S, Azab AF, Adekile A. Department of Pediatrics, Faculty of Medicine, Kuwait University, Kuwait City, Kuwait Pediatr Infect Dis J. 2012 Jun;31(6):575-7. BACKGROUND: Healthy children presenting with neutropenia are often hospitalized and treated empirically with antibiotics without an evidence of infection. The objective of this study was to investigate the infectious causes of isolated transient neutropenia in otherwise previously healthy children. METHOD: A 2-year prospective study was conducted at a tertiary hospital in Kuwait. All previously healthy children (aged 1 month to 12 years) hospitalized with isolated neutropenia defined as absolute neutrophil count (ANC) ≤ 1.5 × 10/L were enrolled in the study. Investigations to identify the infectious causes included blood and urine culture for bacteria whereas for viruses, serology for Epstein-Barr virus, cytomegalovirus, adenovirus, parvovirus and polymerase chain reaction for human herpes virus 6 and enterovirus were performed. RESULTS: Fifty-five children were enrolled during the study. Children less than 2 years of age constituted 73% of the sample. There were 2 peaks of presentation: March-May (33%) and September-November (38%). Associated features were congested throat (56%), runny nose (53%) and cervical lymphadenopathy (20%). The median ANC on admission was 0.6 × 10/L. Associated infections were documented in 55% of enrolled children and were as follows: human herpesvirus 6, 30%; enterovirus, 23%; influenza A H1N1, 13%; parvovirus, 10%; Epstein-Barr virus, 10%; urinary tract infection, (Eshcherichia coli) 7%; and adenovirus, 7%. No serious bacterial infection was identified, and the mean time for recovery of the ANC was 16.7 ± 15 days. CONCLUSIONS: Neutropenia in previously healthy children in Kuwait is caused by demonstrable infections in 55% of cases. Majority of children will recover their ANC completely within 1 month without significant infectious complications. www.HHV-6Foundation.org 2 HHV-6 & Immunosuppression, HIV/AIDS, and Autoimmunity Human herpesvirus 6: report of emerging pathogen in five patients with HIV/AIDS and review of the literature. Corti M, Villafañe MF, Trione N, Mamanna L, Bouzas B. Hospital de Enfermidades Infecciosas Francisco Javier Muñiz, Buenos Aires, Argentina. Rev Soc Bras Med Trop. 2011 Jul-Aug;44(4):522-5. The reactivation of human herpesvirus 6 (HHV-6) in patients with AIDS can result in an acute and severe diffuse meningoencephalitis. We describe the epidemiological, clinical and outcome findings of five patients with diagnosis of HIV/AIDS and central nervous system involvement (CNS) due toHHV-6. Fever was present in all the patients. Meningeal compromise, seizures and encephalitis were present in some of the patients. Polymerase chain reaction (PCR) of cerebrospinal fluid (CSF) specimens was positive for HHV-6 in all the patients. HHV-6 should be included among opportunistic and emerging pathogens that involve the CNS in patients with AIDS. Evolution of SIV toward RANTES resistance in macaques rapidly progressing to AIDS upon coinfection with HHV-6A. Biancotto A, Grivel JC, Lisco A, Vanpouille C, Markham PD, Gallo RC, Margolis LB, Lusso P. National Institute of Child Health and Human Development, Bethesda, MD 20892, USA. Retrovirology. 2009 Jul 2;6:61 BACKGROUND: Progression to AIDS is often associated with the evolution of HIV-1 toward increased virulence and/or pathogenicity. Evidence suggests that a virulence factor for HIV-1 is resistance to CCR5-binding chemokines, most notably RANTES, which are believed to play a role in HIV-1 control in vivo. HIV-1 can achieve RANTES resistance either by phenotypic switching from an exclusive CCR5 usage to an expanded coreceptor specificity, or by the acquisition of alternative modalities of CCR5 usage. An infectious agent that might promote the evolution of HIV-1 toward RANTES resistance is human herpesvirus 6A (HHV-6A), which is frequently reactivated in HIV-1-infected patients and is a potent RANTES inducer in lymphoid tissue. RESULTS: SIV isolates obtained from pig-tailed macaques (M. nemestrina) after approximately one year of single infection with SIV(smE660) or dual infection with SIV(smE660) and HHV-6A(GS) were characterized for their growth capacity and sensitivity to HHV-6A- and RANTES-mediated inhibition in human or macaque lymphoid tissues ex vivo. Four out of 4 HHV-6A-coinfected macaques, all of which progressed to full-blown AIDS within 2 years of infection, were found to harbor SIV variants with a reduced sensitivity to both HHV-6A and RANTES, despite maintaining an exclusive CCR5 coreceptor specificity; viruses derived from two of these animals replicated even more vigorously in the presence of exogenous HHV-6A or RANTES. The SIV variants that emerged in HHV-6A-coinfected macaques showed an overall reduced ex vivo replication capacity that was partially reversed upon addition of exogenous RANTES, associated with suppressed IL-2 and enhanced IFN-gamma production. In contrast, SIV isolates obtained from two singly-infected macaques, none of which progressed to AIDS, maintained HHV-6A/RANTES sensitivity, whereas the only AIDSprogressor among singly-infected macaques developed an SIV variant with partial HHV-6A/RANTES resistance and increased replication capacity, associated with expanded coreceptor usage. CONCLUSION: These results provide in vivo evidence of SIV evolution toward RANTES resistance in macaques rapidly progressing to AIDS. RANTES resistance may represent a common virulence factor allowing primate immunodeficiency retroviruses to evade a critical mechanism of host antiviral defense. Human herpesvirus 6A accelerates AIDS progression in macaques. Lusso P, Crowley RW, Malnati MS, Di Serio C, Ponzoni M, Biancotto A, Markham PD, Gallo RC. San Raffaele Scientific Institute, Milan, Italy. Proc Natl Acad Sci U S A. 2007 Mar 20;104(12):5067-72. Although HIV is the necessary and sufficient causative agent of AIDS, genetic and environmental factors markedly influence the pace of disease progression. Clinical and experimental evidence suggests that human herpesvirus 6A (HHV-6A), a cytopathic T-lymphotropic DNA virus, fosters the progression to AIDS in synergy www.HHV-6Foundation.org 3 HHV-6 & Immunosuppression, HIV/AIDS, and Autoimmunity with HIV-1. In this study, we investigated the effect of coinfection with HHV-6A on the progression of simian immunodeficiency virus (SIV) disease in pig-tailed macaques (Macaca nemestrina). Inoculation of HHV-6A resulted in a rapid appearance of plasma viremia associated with transient clinical manifestations and followed by antibody seroconversion, indicating that this primate species is susceptible to HHV-6A infection. Whereas animals infected with HHV-6A alone did not show any long-term clinical and immunological sequelae, a progressive loss of CD4(+) T cells was observed in all of the macaques inoculated with SIV. However, progression to full-blown AIDS was dramatically accelerated by coinfection with HHV-6A. Rapid disease development in dually infected animals was heralded by an early depletion of both CD4(+) and CD8(+) T cells. These results provide in vivo evidence that HHV-6A may act as a promoting factor in AIDS progression. Association between anticonvulsant hypersensitivity syndrome and human herpesvirus 6 reactivation and hypogammaglobulinemia. Kano Y, Inaoka M, Shiohara T. Kyorin University School of Medicine, Tokyo, Japan. Arch Dermatol. 2004 Feb;140(2):183-8. BACKGROUND: Anticonvulsant hypersensitivity syndrome (AHS) is a life-threatening, drug-induced, multiorgan system reaction. The identification of predisposing factors is clearly needed to predict the incidence and outcome of AHS; attention has recently been focused on reactivation of human herpesvirus 6 (HHV-6). OBJECTIVE: To determine whether immunosuppressive conditions that can allow HHV-6 reactivation could be specifically detected in association with the onset of AHS. DESIGN: We analyzed patients with AHS who were treated during 1997-2002. Two groups of patients receiving anticonvulsants served as controls. SETTING: Department of Dermatology, Kyorin University School of Medicine, Tokyo, Japan. Patients Ten patients with AHS. MAIN OUTCOME MEASURES: The results of serologic tests for antibody titers for various viruses, including HHV6, HHV-6 DNA detection by real-time polymerase chain reaction, immunoglobulin levels by turbidimetric immunoassay, IgG subclass levels by nephelometry, and CD19(+) B-cell counts by flow cytometric analysis, were sequentially assessed. RESULTS: Serum IgG levels (mean, 745 mg/dL) and circulating B-cell counts (mean, 88/ micro L) in patients with AHS were significantly decreased at onset compared with control groups (P<.001 and P =.007, respectively). These alterations returned to normal on full recovery. Reactivation of HHV-6 as judged by a greater than 4-fold increase in HHV-6 IgG titers was exclusively detected in most patients with AHS associated with decreased IgG levels and B-cell counts. CONCLUSIONS: A decrease in immunoglobulin levels and B-cell counts can be associated with HHV-6 reactivation and the subsequent onset of AHS. These immunological alterations might be a useful predictor of the development of AHS. www.HHV-6Foundation.org 4 HHV-6 & Immunosuppression, HIV/AIDS, and Autoimmunity II. HHV-6 & Autoimmune Diseases: Virologic and Immunologic Evidence Supporting an Association between HHV-6 and Hashimoto's Thyroiditis. Caselli E, Zatelli MC, Rizzo R, Benedetti S, Martorelli D, Trasforini G, Cassai E, Degli Uberti EC, Di Luca D, Dolcetti R. University of Ferrara, Ferrara, Italy. PLoS Pathog. 2012 Oct;8(10):e1002951. doi: 10.1371/journal.ppat.1002951. Hashimoto's thyroiditis (HT) is the most common of all thyroid diseases and is characterized by abundant lymphocyte infiltrate and thyroid impairment, caused by various cell- and antibody-mediated immune processes. Viral infections have been suggested as possible environmental triggers, but conclusive data are not available. We analyzed the presence and transcriptional state of human herpesvirus 6 (HHV-6) in thyroid fine needle aspirates (FNA) and peripheral blood mononuclear cells (PBMCs) from 34 HT patients and 28 controls, showing that HHV-6 DNA prevalence (82% vs. 10%, p≤0.001) and viral load were significantly increased in FNA from HT patients, and thyrocytes from HT FNA displayed a 100-fold higher HHV-6 DNA load compared to infiltrating lymphocytes. In addition, while HHV-6 was strictly latent in positive samples from controls, a low grade acute infection was detected in HT samples. HHV-6 variant characterization was carried out in 10 HT FNA samples, determining that all specimens harbored HHV-6 Variant A.The tropism of HHV6 for thyroid cells was verified by infection of Nthy-ori3-1, a thyroid follicular epithelial cell line, showing that thyrocytes are permissive to HHV-6 replication, which induces de novo expression of HLA class II antigens. Furthermore, HHV-6infected Nthy-ori3-1 cells become targets for NK-mediated killing, NK cells from HT patients show a significantly more efficient killing of HHV-6infected thyroid cells than healthy controls, and HT patients have increased T-cell responses to HHV-6 U94 protein, associated to viral latency. These observations suggest a potential role for HHV-6 (possibly variant A) in the development or triggering of HT. Severe hepatitis with autoimmune features following a HHV-6: a case report. Grima P, Chiavaroli R, Calabrese P, Tundo P, Grima P. Division of Infectious Disease, "Santa Caterina Novella" Hospital, Galatina, Italy. Cases J. 2008 Aug 18;1(1):110. HHV-6 has been identified as the aetiologic agent of exanthem subitum in infants and an acute febrile illness in young children. HHV-6probably remains latent in the body after the primary infection and it reactivates upon host immunosuppression in a manner similar to other human herpes viruses. Primary HHV-6 infection in adults is very rare and it is not clear whether disease manifestations are similar to those observed in children.We report the case of acute hepatitis in a 18-year-old immunocompetent woman presenting with sever jaundice and liver dysfunction. Serum immunoglobulin levels were elevated (3.8 gr/dl) with a titre of anti nucleus antibody of 1:640. Serological data demonstrated the presence of IgM antibodies against human herpesvirus-6 in the serum and of viral DNA on liver biopsy by real time quantitative polymerase chain reaction, with a viral load of 280 genomes/106 of cellular genomes. No other etiologic agents were found to induce hepatitis and the patient was diagnosed as havingHHV-6 triggered autoimmune acute hepatitis. Anti-HHV-6 IgG titer significantly predicts subsequent relapse risk in multiple sclerosis. Simpson S Jr, Taylor B, Dwyer DE, Taylor J, Blizzard L, Ponsonby AL, Pittas F, Dwyer T, van der Mei I. Menzies Research Institute Tasmania, University of Tasmania, Australia. Mult Scler. 2012 Jun;18(6):799-806. BACKGROUND: Some of the strongest associations with MS onset are for human herpesviruses, particularly EpsteinBarr virus (EBV) and human herpesvirus 6 (HHV-6). Their role in MS clinical course is less clear, however. www.HHV-6Foundation.org 5 HHV-6 & Immunosuppression, HIV/AIDS, and Autoimmunity METHODS: Prospective cohort of 198 persons with clinically definite MS, followed 2002-5, and serum samples obtained from all subjects at study entry to measure anti-HHV-6 and anti-EBV (Epstein-Barr nuclear antigen [EBNA] and viral capsid antigen [VCA]) IgG titers. Association with relapse evaluated using survival analysis; association with disability/progression evaluated using linear regression or multilevel mixed-effects linear regression. RESULTS: For the 145 persons with relapsing-remitting MS followed beyond one review, anti-HHV-6 IgG titer was positively associated with the hazard of relapse with a dose-dependent trend (p = 0.003), not affected by adjustment for anti-EBV IgG titers, neither of which were independently associated with relapse. There was no significant association between anti-human herpesvirus IgG titers and baseline-measured disability scores, or change in disability scores; however, anti-HHV-6 IgG titers were 2.8 times higher among progressive-course females than progressive-course males. DISCUSSION: These findings suggest that, in addition to a potential etiological role in MS, HHV-6 infection or the immune response to HHV-6antigens may have an effect on the risk of MS relapses and possibly on progressive courses of MS. The observed effect was directly related to anti-HHV-6 IgG titers and may indicate that either HHV-6 infection or factors associated with an altered humoral immune response to HHV-6 may have an effect on MS clinical course. AntiHHV-6 IgG titer may be a useful prognostic factor in relapsing-remitting MS clinical course. Cross-reactivity with myelin basic protein and human herpesvirus-6 in multiple sclerosis. Tejada-Simon MV, Zang YC, Hong J, Rivera VM, Zhang JZ. Department of Neurology and Baylor Multiple Sclerosis Center, Baylor College of Medicine, Houston, TX Ann Neurol. 2003 Feb;53(2):189-97. Viral infections are though to play an important role in the pathogenesis of multiple sclerosis (MS) potentially through molecular mimicry. An identical sequence was found in both myelin basic protein (MBP, residues 96-102), a candidate autoantigen for MS, and human herpesvirus-6 (HHV-6 U24, residues 4-10) that is a suspected viral agent associated with MS. In this study, we showed that greater than 50% of T cells recognizing MBP(93-105) cross-reacted with and could be activated by a synthetic peptide corresponding to residues 1 to 13 of HHV-6 U24 in MS patients. The estimated precursor frequency of these cross-reactive T cells recognizing both peptides, MBP(93-105) and HHV-6 (U24)(1-13), was significantly elevated in MS patients compared with that in healthy controls. These cross-reactive CD4+ T cells represented the same Th1 phenotype as that of monospecific T cells recognizing MBP(93-105). There were increased antibody titers for both peptide HHV-6 (U24)(1-13) and peptide MBP(93-105) in the same patients with MS compared with those in healthy controls, suggesting B-cell sensitization to the antigens in MS patients. The study provides important evidence in the understanding of the potential role of HHV-6 infection/reactivation in the activation of autoimmune reactivity to MBP and its implication in the pathogenesis of MS. www.HHV-6Foundation.org 6