Word - Changesurfer Consulting
advertisement

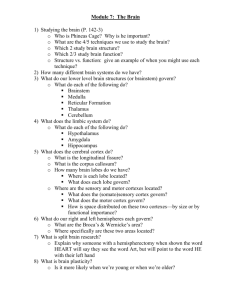
Machado C. Consciousness as a definition of death: its appeal and complexity. Clin Electroencephalogr. 1999 Oct;30(4):156-64. Institute of Neurology and Neurosurgery CONSCIOUSNESS AS A DEFINITION OF DEATH: ITS APPEAL AND COMPLEXITY Author: Calixto Machado, MD, Ph.D. Word count :7534 Correspondence: I Calixto Machado, MD, Ph.D. Instituto de Neurología y Neurocirugía 29 y D, Vedado Ciudad de La Habana 10400 CUBA Tel/Fax:53-7-322233 E.mail: braind@infomed.sld.cu Havana, Cuba 1998 1 Machado C. Consciousness as a definition of death: its appeal and complexity. Clin Electroencephalogr. 1999 Oct;30(4):156-64. ABSTRACT Many controversies in the actual discussions on human death concern the lack of rigorous separation and ordered formulation of three distinct elements: the definition of death, the medical criterion (anatomical substratum) for determining that death has occurred, and the tests to prove that the criterion has been satisfied. In this paper I review the three brain-oriented standards of death (whole brain, brainstem and higher brain) according to these three distinct elements, and will propose a new formulation of death, based on the basic physiopathological mechanisms of consciousness generation in human beings. Two physiological components control conscious behavior: arousal and awareness (content of consciousness). We cannot simply differentiate and locate arousal as a function of the ascending reticular activating system, and awareness as a function of the cerebral cortex. Substantial interconnections among the brainstem, subcortical structures and the neocortex, are essential for subserving and integrating both components of human consciousness. Therefore, consciousness generation is based on anatomy and physiology throughout the brain. The three brain-oriented standards are inconsistent because they present discrepancies among the elements: definition-criterion-tests. I propose a standard of human death that includes consciousness as the most important function of the body, because it provides the capacity for integrating the main human attributes with an integrative functioning of the body. I have also emphasized that consciousness does not bear a simple one-to-one relationship with higher or lower brain structures, because the physical substratum for consciousness is based on anatomy and physiology throughout the brain. This notion of consciousness as the ultimate integrative function is more consistent with the biologically-based systems than the more philosophically-based notions of personhood 2 INTRODUCTION Many controversies in the actual discussions on human death are mainly due to "the lack of rigorous separation and ordered formulation of three distinct elements: the definition of death, the medical criterion (anatomical substratum) for determining that death has occurred, and the tests to prove that the criterion has been satisfied". 1-7 To define death is mainly a philosophical task, meanwhile the criterion and tests are medical chores. Specific criteria and tests must harmonize with a given definition. The definition must recognize the "quality that is so essentially significant to a living entity that its loss is termed death". 1-3,7 During the last decades, three main brain-oriented formulations of death have been discussed: whole brain, brainstem death and higher brain standards. 8,9 The whole brain criterion refers to the irreversible cessation of all intracranial structure functions. 15,10-19 It has been accepted by society mainly for practical reasons. 8 Physicians have constructed batteries of bedside tests (and of confirmatory laboratory procedures) to show that this criterion of death has been satisfied. 10,12,13,19-21 Until recently, whole brain strategists had not provided a conceptual framework to support specific criteria and tests. 10-12 Moreover, this view has not answered the key point question about the critical number and location of neurons, subserving the essential brain activities to execute the functioning of the "organism as a whole" 22-27 Christopher Pallis has powerfully articulated the brainstem death view. were also practical reasons that promoted this view, 33-35 28-32 There because according to Pallis 28 "a dead (i. e, irreversibly non-functioning) brainstem can be diagnosed at bedside, without resort of complicated investigations, and it predicts inevitable asystole within a 3 short while". Therefore, so-called brainstem death was adopted in several Commonwealth countries. 28-36 Pallis emphasized that the "capacity for consciousness" and “respiration” are the two hallmarks of life of the human being, and that brainstem death predicts an inescapable asystole. 28-32 The physiopathological review of consciousness generation and respiration will provide a framework for not accepting Pallis' definition of death. 8,9,37 Moreover, recent clinical cases have shown that brain death will not always predict an "inevitable asystole within a short while". 37 Higher brain theorists have defined human death as the "the loss of consciousness", (definition) related to the irreversible destruction of the neocortex (criterion), or “higher brain”. 38-44 In this paper, I will explain that consciousness does not bear a simple one-to-one relationship with higher or lower brain structures, and therefore, the higher brain formulation is wrong, because the definition (consciousness) does not correspond directly to the criterion (neocortex). 9 I will also review the three brain-oriented standards using to the three distinct elements proposed by Bernat and others,1-7 and will propose a new formulation of death, based on the basic physiopathological mechanisms of consciousness generation in human beings. 8,9 PHYSIO-PATHOLOGICAL MECHANISMS OF CONSCIOUSNESS GENERATION IN HUMAN BEINGS Before proceeding, it is necessary to review the physiopathological mechanisms of consciousness generation. 4 Plum and Posner 18 defined consciousness as “the state of awareness of self and the environment”. Two physiological components control conscious behavior: arousal and awareness. 9,18 Arousal represents a group of behavioral changes that occurs when a person awakens from sleep or transits to a state of alertness. 45 "Normal consciousness requires arousal, autonomic-vegetative brain function subserved by ascending stimuli from the pontine tegmentum, posterior hypothalamus and thalamus that activate wakefulness". 46 The most discernible change that occurs when waking is the eyes opening. 9,18,45,46 Arousal is also known as capacity for consciousness. 9,28-32 Awareness, also known as content of consciousness, represents the sum of cognitive and affective mental functions, and denotes the knowledge of one's existence, and the recognition of the internal and external worlds. 9,18 It has been argued that consciousness has two dimensions: wakefulness and awareness. 46 Awareness is the same as the content of consciousness. 9 Wakefulness is provided by the arousal. 9,18,45,46 Plum 47 has recently defined not two but three components, subdividing the content of consciousness in two levels or components. According to this author, the second component or level, "which importantly regulates the sustained behavioral state function of affect, mood, attention, cognitive integration, and psychic energy (cathexis) depends on the integrity of the limbic structures including the hypothalamus, the basal forebrain, the amygdala, the hippocampal complex, the cingulun, and the septal area". The limbic system is important for the homeostasis of the internal milieu, and hence the second component of consciousness is crucial for integrating affective, cognitive and vegetative functions. Plum considers the third component as the "cerebral level, along with the 5 thalamus and basal ganglia". This component is related to the processes of higher levels of perception, self-awareness, language, motor skill, and planning. Memory can be impaired by injury of either cerebral or limbic levels. In summary, a human being's state of consciousness reflects both his or her level of arousal that depends on subcortical arousal-energizing systems and, the sum of the cognitive, affective, and other higher brain functions (content of consciousness or awareness), related to "complex physical and psychologic mechanisms by which limbic systems and the cerebrum enrich and individualize human consciousness". 48 Therefore, I will use the term arousal when referring to those subcortical arousalenergizing systems, and awareness, to denote the sum of those complex brain functions, related to limbic and cerebrum levels. 9,18,48 Unfortunately, most authors 38,41,43 mention human consciousness, without considering its two components originally described by Plum and Posner . 18 For example, higher brain theorists 38-44 habitually describe the persistent vegetative state (PVS) as patients with "irreversible loss of consciousness" or "permanent unconscious", but in these patients arousal is preserved, while awareness is apparently lost. On the other hand, some authors refer to the higher brain criterion as "the irreversible loss of the capacity for consciousness", 41 but they are really referring to awareness. As the use of the term "capacity for consciousness", 28-32 could be confusing, I will identify this function with the original term used by Plum and Posner, i. e., arousal. I will use awareness as a synonym for content of consciousness. 18 8,9 Arousal depends on the integrity of physiological mechanisms that take their origin in the ascending reticular activating system (ARAS): "it originates in the upper brainstem 6 reticular core and projects through synaptic relays in the thalamus to the cerebral cortex, where it increases excitability". 48 Moruzzi and Magoun, 49 in their pioneer studies, discovered “the presence in the brainstem of a system of ascending reticular relays, whose direct stimulation activates or desynchronizes the EEG, replacing highvoltage low waves with low voltage fast activity”. Nonetheless, Steriade et al . 48,50-59 have recently emphasized that this desynchronization related to wakefulness “is now more apparent than real”, because although large slow waves disappear during waking, the EEG shows high frequency oscillations (30-40 Hz), known as gamma oscillations, that reflect synchronized and enhanced intracortical and corticothalamic activity. Bogen 60 has emphasized that the intralaminar nuclei complex of the thalamus is a cardinal component of the ARAS. The thalamic intralaminar neurons receive inputs from many sensory modalities and widely project to the cerebral cortex. Moreover, these nuclei are a major target for the brainstem reticular formation involved in waking. Recent reports strengthen the idea that intralaminar nuclei are thus essential in coordinating activity among cortical areas, and contribute to the formation of global perception to complex stimuli. 60,61 The connections from the brainstem to the cerebral cortex, relayed through intralaminar and other thalamic nuclei, and their main neurotransmitters (acetylcoline and glutamate) have been identified. 48 Additional important pathways participating in arousal have been recently recognized. 45 There are neurotransmitter systems that take origin in the brainstem, hypothalamus and basal forebrain, projecting monosynaptically to the cerebral cortex without relaying through the thalamus. These systems include different neurotransmitter projections: cholinergic from the basal forebrain and 7 mesopontine reticular formation, serotoninergic from the brainstem raphe nuclei, histaminergic from the posterior hypothalamus and noradrenergic from the brainstem locus coeruleus. Experimental studies have also shown that an almost complete destruction of the thalamus does not block cortical activation. Furthermore, the EEG arousal pattern characterized by desynchronization disappears with the administration of drugs to block serotoninergic and cholinergic transmission. 18,62 Therefore, it is reasonable that arousal is due to several ascending systems stimulating the cerebral cortex and thalamus in parallel. 9,45 Thus, "thalamo-cortical transmission may not be sufficient or even necessary to produce cortical activation". 18 The discovery that the cerebral cortex is organized in vertical columns that represent functional units was crucial for further understanding of the functional organization of the brain. "The basic functional unit of the neocortex is a vertically oriented group of cells extending across the cellular layers and heavily interconnected in the vertical direction, sparsely so horizontally". 63 At present there are arguments that the functional organization of the entire cerebral cortex is a complex of these vertical columns. Contiguous columns are interconnected by local circuits into "information-processing modules", characterized by specific afferent and efferent connections with other modular units from other cortical and subcortical areas. 45,63 It seems that the brain operates in "parallel processing", because cortical regions are linked in parallel networks with each other and with subcortical structures. Thus, a specific component of a certain cognitive function is scattered among interconnected regions, each one implicated in a distinct aspect of the cognitive ability. 45,64 According 8 to Feinberg, 65 one of the most remarkable peculiarities of the brain is "the seemingly enormous redundancy, parallelism, and distributiveness" of its connections. The cerebral cortex and thalamus make up "a unified oscillatory machine" that exhibit spontaneous rhythms and that are conditional to behavioral state and vigilance. 51 The brain uses spatiotemporally distributed systems to "capture high-order perceptual features". 65 Singer and Gray 66 have argued that fast rhythms of corticothalamic neurons, known as gamma oscillations, are probably implicated in synchronizing mechanisms that respond to different features of the same perceptual object, leading to several hypothesis of high cognitive mechanisms. Normal conscious behavior requires both arousal and awareness. 18 Patients in coma are unconscious because both arousal and awareness are disturbed . 9,18 The Multi-Society Task Force in PVS has classified the causes of PVS in 3 main groups: Acute injuries, where the most common causes are traumatic and hypoxicischemic encephalopathy; degenerative and metabolic disorders, including dementia; developmental malformations, where the most important is anencephaly. Nonetheless, the most prevalent causes of acute PVS in all ages are head trauma and hypoxicischemic encephalopathy. These causes have been taken as models to describe the three main patterns of the neuropathological damage in PVS cases. In persistent vegetative state (PVS) cases arousal is preserved (the PVS has periods of wakefulness), but awareness is seemingly is lost. 9 Thus, in PVS there is an apparent dissociation of awareness from arousal. 9,45 It has been argued that "separate anatomic pathways mediate arousal and awareness, and that brain diseases can differentially affect each component of consciousness". 45 9 This raises the question: Why is awareness lacking in PVS, while arousal is preserved? The neuropathology in the PVS provides a suitable background to discuss the pathophysiology of consciousness generation. Kinney 45 has recently presented a detailed review of this subject. According to this author, PVS denotes a "locked-outsyndrome" because "the cerebral cortex is disconnected from the external world, and all awareness of the external world is lost". She suggested that the loss of awareness in the PVS is caused by three main patterns: widespread and bilateral lesions of the cerebral cortex, diffuse damage of intra- and subcortical connections in the cerebral hemispheres white matter, and necrosis of the thalamus. In widespread and bilateral lesions of the cerebral cortex, hypoxic-ischemic encephalopathy is the main etiology. It is the consequence of acute hypoxic-ischemic insults after cardio-respiratory arrest, strangulation, suffocation, near-drawing, prolonged hypotension, and perinatal asphyxia in neonates. 45,67 The description of this pattern was the reason that PVS was first known as "apallic syndrome", characterized by the destruction of the "pallium, the cortical gray matter that covers the thelencephalon". 68 In the cerebral cortex a laminar necrosis is found that is multifocal or diffuse and extensive. Other ischemic lesions may be superimposed mainly in the border zones of the main intracranial cerebral arteries, as the parasagittal parietooccipital region, for example. 45,69 Other damages, such as neuronal loss and small infarcts, are also typically found in the cerebellum, basal ganglia, thalamus and hippocampus; the later being particularly sensitive. Other anatomical structures of the brain are relatively undamaged: brainstem, 10 hypothalamus, basal forebrain and amygdala. This distribution of brain damage reflects the differential vulnerability of brain regions to hypoxia-ischemia. 45,68,70 In PVS cases with diffuse damage of the cerebral cortex the lack of awareness is understandable. The widespread involvement of the association cortices combined with primary and secondary cortices damage, is the faultfinding anatomical ground. 45 It has been suggested that in diffuse cerebral cortical lesions, the brainstem and the thalamus can maintain arousal. 9,45 Nonetheless, other parallel pathways projecting monosynaptically to the cerebral cortex without relaying through the thalamus could partake to maintain the arousal in these cases. Thus, arousal could be preserved without a functional cerebral cortex. This has been also supported by experimental data. In animals with a total removal of the cerebral cortex or transection at the rostral midbrain level, arousal is preserved, showing waking/ sleep cycles. 71 been argued that the brainstem alone could be sufficient for arousal. Therefore, it has 45,71 The mechanism of this pattern could be explained in head trauma and hypoxicischemic injury. After head trauma, a widespread damage of axons in the cerebral hemispheres white matter occurs, known as diffuse axonal injury (DAI). The DAI is probably caused by the acceleration suffered by the head immediate after the injury. 45,72 The cerebral hemisphere white matter could be also damaged after hypoxic-ischemic accidents in a pattern known as "leukoencephalopathy". 73 It is characterized by "extensive symmetrical necrotic lesions in the central white matter of the cerebral hemispheres, with minimal or no damage to gray matter structures". 45 These patients 11 yield antecedents of prolonged periods of hypotension, hypoxemia and increased venous pressure. 45,72,73 This pattern also provides a disconnection of the cerebral cortex from the environment that can explain the lack of awareness in the PVS. The functionally unaltered brainstem and thalamus preserve arousal. The participation of other parallel pathway not relaying through the thalamus has to be also considered. 9 Reports in PVS patients and experimental data of diffuse axonal injury to cerebral hemispheres with cerebral cortex remaining largely normal suggest that, "acute diffuse disconnection of the cerebral cortex from its subcortical activating mechanisms can block arousal as well as cognitive activity in the primate brain". 47 Other pattern is characterized by a selective necrosis of the thalamus and, although the cortex is not totally spared, the lesions are focal and restricted. 45,74 It has been explained by several possible factors, such as: partial or immediately reversed transtentorial herniation, cerebral edema causing hypoxia-ischemia, and intrinsic metabolic vulnerability of the thalamus. 45 The lesions of the thalamus provide a disconnection of the cerebral cortex from the external world, and therefore, all awareness from the environment is lost. The lack of awareness in this pattern is not only a consequence of lesions destroying the sensory relay nuclei that block sensory information from the external world, but the damage of the thalamic intralaminar nuclei is probably the critical anatomical substratum . 45,61,69 These thalamic nuclei receive inputs from many sensory modalities and project over wide areas of the cerebral cortex with a “non discernible topography”. 45 These nuclei integrate important pathways to subserve fundamental cognitive and affective functions 12 such as the attention to the external world. 45,69 It has been argued that lesions in a thalamic nucleus that is preferentially connected with an association cortex provoke functional impairments similar to damage in the association cortex itself. 69,75 For instance, contrary to the generalized expectancy, the neuropathological examination of Karen Ann Quinlan's brain showed a disproportional severe damage of the thalamus, as compared with the cerebral cortex. 69 Bilateral thalamic infarcts are commonly accompanied by mental impairment, such as dementia and amnesia . 60,76 In this pattern arousal could be preserved by a functionally intact brainstem and the other parallel pathways which project to the cerebral cortex, without relaying through the thalamus. 9 It has been argued that "the thalamus is critical for cognition and awareness and may be less essential for arousal". 69 The Multi-Society Task Force in PVS 46 has defined the precise use of the terms "persistent" and "permanent". "Persistent refers only to a condition of past and continuing disability with an uncertain future, whereas permanent implies irreversibility". The Multi-society Task Force likewise addressed that "A patient in a persistent vegetative state becomes permanently vegetative when the diagnosis of irreversibility can be established with a high degree of clinical certainty". According to the etiology, a period of observation has been proposed to define that a "persistent vegetative state", has become a "permanent vegetative state. PVS patients reflect the only situation in which an apparent dissociation of both components of consciousness is found. 9,45 Conversely, recent evidence has shown that cortical-subcortical interactions are necessary to subserve and make both components active. 9,47 Regarding the above-mentioned subjects, two main questions 13 may arise: Are subcortical structures capable of mediating some form of awareness? Is the lack of awareness in the PVS really permanent or irreversible? There is striking evidence that subcortical structures are capable of mediating some form of awareness. 9 Plum has emphasized that the "non-specific mechanisms ascending from the rostral brainstem and diencephalon importantly and possibly inseparably activate and integrate both the arousal and the cognitive aspects of human consciousness". The participation of the thalamus to provide the awareness has been already mentioned. Additionally, Shewmon 77 9,45,69 has discussed some examples of clear participation of subcortical structures in awareness. Experimental animals with complete decortication have shown to be capable of complex interactions with the environment, which is evidence of some awareness. 78 In lesions of the somatosensory cortex an evident loss of tactile, vibration and joint position sense is observed; nonetheless, conscious experience of pain and temperature is preserved, mediated by subcortical structures, probably the thalamus. 77,79 This author also commented that two hydranencephalic patients ("prenatal destruction of the cerebral hemispheres with intact skull and scalp") unquestionably manifested conscious behavior. These two cases are examples of the brainstem "plasticity" in newborns. 77,81 Clinical and experimental evidence convincingly suggests that the brainstem of newborns is potentially capable of much more complex integrative functioning. This includes some functions commonly considered to be cortical, even in animals. 81 Based on these subjects, the potential presence of some primitive form of awareness in anencephalics, and the possibility of subjective feeling of pain, has been suggested. 77,81 Thus, according to Shewmon 77 "the human brainstem 14 and diencephalon, in the absence of cerebral cortex, can mediate consciousness and purposeful interaction with the environment". The use of deep brain stimulation (DBS) has shown possible that the cerebral hemispheres could mediate arousal producing some wakefulness behavior, even after complete loss of the brainstem's reticular activating system. 9 Hassler 82 used DBS in "apallic" or "coma vigil" cases (PVS patients), stimulating the reticular formation in the thalamus and in the pallidum. It caused these patients to awaken with an undoubted recovery of awareness (recognition of their families and emotional expressions). Katayama et al., 83 also employing DBS of the ARAS (mesencephalic reticular formation and/or non-specific thalamic nuclei) in PVS cases, have reported a persistent increment in pain-related P250, which indicates non-specific cortical activation. Sturm et al. 84 reported the use of DBS at the thalamic level, in a case with probable dysfunction of the mesencephalic reticular formation due to the rupture of a sacular aneurysm at the tip of the basilar artery. DBS resulted in autonomic and behavioral reactions and the patient was able to respond to simple commands. Kohadon and Richer, 85 from a series of 25 PVS cases treated by DBS, reported a definitive improvement in arousal with some degree of awareness and interpersonal relationship, in 13 of them. PVS provides a model in which arousal is preserved and awareness is apparently 9 lacking. Therefore, it has been suggested that both component of consciousness "are mediated by distinct anatomic, neurochemical and/or physiological systems". 45 Nonetheless, the potential plasticity of the brain has demonstrated that subcortical structures could mediate awareness, even with the complete absence of the cerebral cortex. 77 Austin and Grant 86 reported 3 cases who undergone total hemispherectomy 15 (comprising cortex, white matter and basal ganglia), that continued speaking and were aware of their environment during the operation, done under local anesthesia. Thus, awareness is not only related to the function of the neocortex (although it is primary important), but to complex physical and psychological mechanisms, due to the interrelation of the ARAS, limbic system, and the cerebrum. 9,47 Plum 47 has emphasized that the ARAS substantially and inseparably activates and integrates both the arousal and the cognitive aspects of human consciousness. He recognized a brainstem-diencephalic participation not only in arousal, but also in cognitive function. In lesions affecting thalamic-mesencephalic structures that comprise the ARAS, the presence of important cognitive and affective deficits can be found. Alterations in the cerebral cortex after severe damage restricted to mesencephalicdiencephalic activating systems have been reported. They reflect transneural degeneration, and suggest that these pathways not only activate the cerebral cortex but they also trophically influence cortical neurons. 9,47 Therefore, it can be concluded that we cannot simply differentiate and locate arousal as a function of the ARAS, and awareness as a function of the cerebral cortex. Substantial interconnections among the brainstem, subcortical structures and the neocortex, are essential for subserving and integrating both components of human consciousness. 9,18,47,77 The above considerations lead one to conclude that there is no single anatomical place of the brain "necessary and sufficient for consciousness". 77 Shewmon has discussed the existence of a "physiological kernel of consciousness" 28-32 or a "reticular formation/cortical unit". 77 In a broad sense this "physiological kernel of consciousness" 16 or "reticular formation/cortical unit" (RF/CU) is conformed by the widespread interconnections among the ARAS, diencephalon, other subcortical structures, and the cerebral cortex. 9,77 BRAIN ORIENTED STANDARDS OF DEATH The whole brain criterion James Bernat and his collaborators have presented the most complete defense of this standard. 1-5, 87-92 He has been one the main advocates to recognize that any standard should include three distinct elements: definition-criterion-tests. Bernat proposed the following standard: DEFINITION CRITERION TESTS The permanent cessation of The permanent cessation of The permanent the functioning of the the functioning of the entire absence of breathing organism as a whole brain and heartbeat. Brain cessation tests Definition Early whole brain advocates failed to propose a conceptual framework to support this criterion. 9 Nonetheless, Bernat and his colleagues 1-5, 87-91 fully elaborated this 17 standard of death clearly presenting the three main elements: definition-criterion-tests. These authors defined death as "the permanent cessation of the functioning of the organism as a whole". They also emphasized that by "organism as a whole" they are not referring to the "whole organism", as a sum of its parts, "but rather to that characteristics that makes the living organism greater than the sum of its parts". Moreover, they explained their view of integration in physiological terms: "functions of the organism as a whole include respiration, temperature control, fluid and electrolyte homeostasis, consciousness, food-seeking behavior, sexual behavior, neuroendocrine regulation, and autonomic control”. 5 Bernat sustained that the organism as a whole could be kept functioning despite destruction of some subsystems. 2,4,5 Criterion "The permanent cessation of the functioning of the entire brain". Tests Bernat 1-5,92 proposed two sets of tests for determining this criterion. The cardiorespiratory standard is used to document the permanent loss of all brain functions, because a prolonged absence of circulation or respiration will inevitably cause ischemia, anoxia and necrosis of the brain. The neurological standard included preconditions and a battery of tests and clinical procedures performed at bedside. It is applied "in all cases except when death needs to be declared in a patient with heartbeat on a ventilator". 5 18 Critique Several authors have described patients "whole-braindead" and yet expressed surprise when they find that the EEG was still retained. The persistence of EEG activity is however incompatible with the diagnosis of "whole brain death". 22-24,93,94 Other authors have reported the preservation of visual evoked potentials in primary brainstem lesions. 95 The persistence of hypothalamic neuroendocrine functions in "whole braindead" patients has been also advocated against this formulation. 25-27,96-99 Bernat 92 slightly modified his definition to "the permanent cessation of the critical functions of the organism as a whole". This author referred that the critical functions consist of "three distinct and complementary categories": 1) "vital functions of spontaneous breathing and autonomic control of circulation". 2) "Integrating functions that assure homeostasis of the organism, including the appropriate physiologic responses to baroceptors, chemoreceptors, neuroendocrine feedback loops". 3) "Consciousness, which is required for the organism to respond to requirements for hydration, nutrition, and protection, among other needs". Nonetheless, "this modified position still doesn't answer the above mentioned electrophysiological findings in "whole-braindead patients", and it is difficult to know when the persistence of hypothalamic neuroendocrine functions in these cases is related or not to a "neuroendocrine feedback loop". Moreover, Bernat now includes consciousness as the third category of the critical integrative functions, but as I will demonstrate, consciousness is the ultimate integrative function of the body. These arguments pointed out again a controversy in the fulfillment of the three main elements of any standard of death (definition-criterion-tests), because the whole brain 19 criterion does not, and which is the critical number and location of neurons, subserving the essential activities of the hemispheres, diencephalon and brainstem to execute the functions of the "organism as a whole", that permanently cease functioning? 8 Brainstem (brain as a whole) criterion Pallis, 28-32,93,100-102 has proposed the following standard, that I will separate according the three main elements: definition, criterion and tests. DEFINITION CRITERION TESTS There is only one kind of The permanent cessation of No brainstem reflexes human death: the the functioning of brainstem Apnea irreversible loss of the capacity for consciousness, combined with the irreversible loss of the capacity to breathe (and hence to sustain a spontaneous heart beat) 20 Definition and criterion. In his definition, Pallis 28 emphasizes that the "capacity for consciousness" and respiration are the two hallmarks of life of the human being, and that brainstem death predicts an inescapable asystole. According to Pallis, 28,101 the ascending reticular formation discovered by Moruzzi and Magoun 49 produces a generalized activation of the cortex, producing the necessary arousal to endow the functioning of the "brain as a whole". This author also emphasized that the physiological and anatomical background is the irreversible damage of the paramedial tegmental areas of the mesencephalon and rostral pons. Since ancient times, respiration was considered the vital function which defined the frontiers between life and death. 28,100,101 Pallis has also emphasized that in many older cultures death was considered: "the departure of the soul from the body", and that the words that stand for "soul" are in many idioms the same as those standing for "breath". 28 He also emphasized that the "loss of breath" locates its anatomical and physiological basis in irreversible damage of the lower brainstem. Moreover, he considered that the anatomical and physiological basis to produce an irreversible apnea is an irreversible damage to the lower brainstem, where "crucial mechanisms concerned with breathing are located". 28,100 Pallis 28 presented a detailed review to answer the question: "How long may cardiac action persist after a diagnosis of brain death?" He suggested that in most cases asystole occurred within days. This author emphasized that time variations in somatic survival after brain death presumably reflect three main factors: 21 “The time on the ventilator before the diagnosis of brain death was made” “The quality of ‘care’ administered” “The age composition of the sample” Tests Pallis 28,101 addressed that as the "brainstem death is a clinical concept", "a dead brainstem" can be diagnosed at bedside. It is necessary to diagnose an unconscious patient, with irreversible apnea and irreversible loss of brainstem reflexes, provided that "all reversible causes of brainstem dysfunction have been excluded”. Critique Pallis 28-32,93,100-102 includes in his definition “the capacity for consciousness”, or arousal, as has been previously discussed. Nonetheless, in any definition that incorporates consciousness as a main hallmark, both components should be included, because a normal conscious behavior demands integration or widespread interconnections among the ARAS, subcortical structures, and the neocortex, i. e., an interaction of both components. 9 Moreover, some authors using deep brain stimulation have found non-specific cortical activation in PVS and comatose patients. 82-85 Then, in cases fulfilling the brainstem criteria of brain death with primary brainstem lesions and spared cerebral hemispheres, stimulation of the non-specific thalamic nuclei might produce some degree of arousal. 9 In primary brainstem lesions a quasi-normal EEG could be recorded. 22-24,93-95 22 The other hallmark of Pallis’ definition is respiration. 28 I had previously discussed that if by respiration is meant gases exchange in the lungs or oxidative processes taking place at the cellular level, mechanically ventilated patients are capable of "breathing". 8 In patients with a non-brain functioning the heart beat, pulmonary and circulatory functions are preserved, and the physiological changes associated with normal respiration are in fact taking place, at the cellular level. 8,104 Brainstem function is not necessary for this to happen, provided one is situated in an intensive care unit. 105 In fact, what is irreversibly absent in the in brain-dead is ventilation. 8 Patients affected with polio, may be incapable of spontaneous ventilation, i. e., they fulfill one of the hallmarks of Pallis' definition of death: "the irreversible loss of the capacity to breathe", 28 but the patients are not dead. 8 Before the era of modern types of ventilatory assistance, such patients would have not survived. 8,105 Nowadays, the recognition that pulmonary gas exchange may be maintained successfully for prolonged periods by mechanical ventilation in the intensive care environment 106,107 leads to conclude that respiration (and more particularly, ventilation) is not so essential to life, that its loss constitutes death. 8 Recent reports shows that some brain-dead patients do not develop an inevitable asystole within hours or days. 108-110 Shewmon 104 has recently presented a detailed review of prolonged survivals in about 156 braindead patients. This author made a compilation of cases with survival of more than "a few days, i. e. one week or more", taking this information from sources including, personal experience, the medical literature and the news media. He described a striking case, may be the record of 23 prolonged somatic survival, who was diagnosed (well documented) as "braindead", 14 years ago. The age factor at onset of brain death plays a significant role in somatic survival: "the younger the age, the greater the capacity for survival". 77,104 Shewmon 104 also addressed two other factors involved in survival: 1) "associated systemic injuries directly due to whatever caused the brain insult", and 2) "systemic pathology secondarily induced by the process of brain herniation". Withdrawal of life support is a "confounding factor", because it leads to underestimate the survival potential in brain-dead cases. Other factors related to somatic survival could be: the quality of nursing care, an adequate homeostatic control, prevention and early treatment of infections, etc. 28 Therefore, an “inevitable asystole” can’t be a justification for accepting a brainoriented standard of death. Higher brain criterion The "higher brain" view is closely related to the management of PVS patients, and has been mainly defended by philosophers. 7,38-44,111-114 DEFINITION CRITERION TESTS The loss of that which is The permanent cessation of No cognitive and affective significant to the nature of the functioning of the man neocortex functions 24 Definition "Higher brain" formulations proposed defining death as "the loss of that which is significant to the nature of man". 38 "Higher brain" constructionists sustained that the irreversible loss of perception, sentience and cognition was necessary and sufficient for diagnosing death.7-38-44,111-14 Bartlett and Youngner 7 stated "we believe that only the higher brain functions, consciousness and cognition, define the life and death of a human being". Robert M. Veatch 38-40,114 was a pioneer of this standard of death, and one of its main defenders. This author 114 argued to include in the definition either of “capacity for consciousness or social interaction”, and presented a detailed discussion about “the functions considered to be ultimately significant to human life”: rationality, consciousness, personal identity, and social interaction. He concluded that death should be appropriately defined “as the irreversible loss of embodied capacity for social interaction”. Some authors have also advocated this definition as the "loss of personhood" 42,44 Criterion and Tests Higher brain advocates emphasized that the neocortex assumes a critical role by providing the consciousness and cognition, that characterize a human being 7,38-44,111114 They proposed to functionally classify the brain into the lower brain (brainstem), that 25 governs primarily vegetative functions, and the higher brain (the cerebral hemispheres, particularly the neocortex), that controls consciousness and cognition. Veatch 114 emphasized that "we could be quite conservative and hold that the entire brain must be destroyed in order to be sure that the capacity for consciousness and social interaction is lost". This author referred to the "higher brain locus", or used other terms, such as "cerebral", "cortical", or "neocortical". Veatch clearly argued that elaborating a set of tests to measure the irreversible loss of the capacity for consciousness or social interaction is rather difficult. 38-40,114 Critique I have shown that we cannot simply differentiate and locate arousal as a function of the ARAS, and the content of consciousness as a function of the cerebral cortex, because substantial interconnections among the brainstem, subcortical structures and the neocortex, are essential for subserving and integrating both components of human consciousness. 9,18,44,47 Consciousness does not bear a simple one-to-one relationship with higher or lower brain structures, and therefore, the identification of the definition (consciousness, capacity for consciousness or social interaction, personal identity, etc.) does not correspond directly to the criterion (higher brain, cerebral hemispheres, neocortex) that most, if not all, higher brain defenders have used. In fact, the physical substratum for consciousness is based on anatomy and physiology throughout the brain. 9 Some reports about “neocortical death” have presented a neuropathological substratum of a “dead neocortex” with the brainstem relatively spared, suggesting that "higher brain-dead *patients" could preserve brainstem reflexes and spontaneous 26 breathing. 22,24,93,95 I have discussed that three neuropathological patterns are found in these patients, rather than simply one related to the destruction of the neocortex. 9 Moreover, it is necessary to discuss the potential reversibility of the awareness in the PVS. As it has previously discussed, the use of deep brain stimulation (DBS) has shown the possibility that the cerebral hemispheres could mediate arousal producing wakefulness behavior, even after complete loss of the brainstem's reticular activating system, and an undoubted recovery of awareness (recognition of their families and emotional expressions) has been reported in PVS cases. 81-84 Some reports of misdiagnosis or recovery in PVS have also appeared in recent literature. Unexpected and well-documented recoveries of cognitive functions have been described in patients, where it was believed that neurologists experienced and skilled in the diagnosis of this condition correctly applied the criteria. 115-118 Childs 119 reported that 37 % of 49 cases admitted in a special unit for rehabilitation were incorrectly diagnosed. Andrews et al. 120 reported that 43% of patients also admitted in a rehabilitation unit were incorrectly diagnosed. Therefore, the main inconsistencies of higher brain theorists are: 1) the definition of death (consciousness, capacity for consciousness or social interaction, personal identity, etc.) does not correspond directly to the criterion (higher brain, cerebral hemispheres, neocortex), because they don’t confuse the physiopathological substratum of consciousness with the neocortex; 2) the classify PVS case as dead. 27 NEW STANDARD OF HUMAN DEATH DEFINITION CRITERION TESTS Irreversible loss of the Irreversible destruction of Unresponsiveness, no capacity for integrating the the anatomo-functional arousal to any stimuli, no main human attributes with substratum for subserving cognitive and affective an integrative functioning of both components of functions the body consciousness: arousal and awareness Definition Several authors 114,121,122 have quoted words used by Beecher, Chairman of the Harvard Committee, in his address to the American Association for the Advancement of Science, when he explained the importance of the brain for human life: “the individual’s personality, his conscious life, his uniqueness, his capacity for remembering, judging, reasoning, acting, enjoying, worrying, and so on”. Cranford 42 stated: "our major premise is that consciousness is the most critical moral, legal, and constitutional standard, not for human life itself, but for human personhood". Therefore, higher brain defenders stressed that consciousness provides the most significant attributes of human existence. 38,42,43 28 Botkin and Post 123 presented an interesting dichotomy considering major and minor clusters of attributes related with life. For example, braindead patients retain several attributes associated with life, as skin color, warm skin, heartbeat, kidney function, etc. Even, subjects diagnosed as dead by the cardiorespiratory standard will preserve during day's vestiges of life attributes: hair and nails still grow. 6,9 Therefore, I completely agree with higher brain defenders that consciousness provides the most significant attributes that characterize human life. Hence, It is reasonable to state that any vestige of consciousness is inconsistent with death. 29 Integration Korein, applying thermodynamics and information theory powerfully defended the notion of integration. 16,124 He argued that all living organisms could be classified as open systems that exchange energy and matter with environment. He emphasized that within any organism there is a critical system which "supersedes all other subsidiary systems" or subsystems. This author proposed that the "critical system" of the human being is the brain, "which is irreplaceable by an artifice, be it biological, chemical, or electromechanical". Therefore, according to this view if the brain is irreversibly destroyed, the critical system is abolished. Even if, other subsystems are functioning spontaneously or overtaken by machines, the organism as an individual assemblage no longer exists. Varela125 also assumed that living organisms are complex dynamical systems with energy states characterized as a discontinuous "eigenbehavior", and discontinuities in state transition. The Swedish Committee 126 also applied the notion of integration to define death: "total and irreversible loss of all capacity for integrating and co-ordinating the functions of the body -physical and mental- into a functional unit. Shewmon 77,78 had also emphasized the central role of the brain "in the coordination or performance of virtually all functions necessary for the unity of the post-embryonic human body, including internal homeostasis, adaptative interaction with the environment, and the intimate connection between mental and physiological states". Nonetheless, this author made recently a complete turn in his position, emphasizing that the brain is not the "central integrating organ of the body". 104 He remarked that 30 "clinical evidences of brain death is more attributable to multisystem damage and spinal shock than to destruction of the brain per se", and proposed to return to a "circulatoryrespiratory" standard of death. However, this author accepted that the brain plays a role in integrating functions of the intact organism. He used as an example the field of psychoneuroimmunology, emphasizing that "the brain role is one of modulating, finetuning, and enhancing an already established and well functioning immune system". If we accept Shewmon's view, then a specific emotional state could influence the immune system, either diminishing or enhancing the immune response. We can ask ourselves: Can we consider this brain's effect over other systems, of "modulating" or "finetuning", "the highest level of integration within the organism"? According to Bernat, 5 the brain produces signals "for breathing through brainstem ventilatory centers, and aids in the control of circulation through medullary blood pressure control centers". For example, if a young man meets in front of him, his girl friend (love), or sees a lion (fear), we can explain a complex mechanism of brain control over the whole body. After the visualization of the visual target (girl friend or lion), and recognition comparing with backup memory, complex signals are generated, through interconnected pathways spread throughout extensive brain areas (neocortex, diencephalon and other limbic structures, brainstem, reticular formation, etc.) that produces faster heartbeats and deeper ventilatory movements. 127 Trained Yoga practitioners are capable of slowing heartbeats until they are almost imperceptible to auscultation. 128 Psychological influences in menstrual cycle, and in reproduction in general, both in humans and in other animal species, have been vastly discussed in the 31 literature. 129 Conscious behavior has allowed human beings to transform and govern their environment. 8,38 These examples show how consciousness controls and regulate the functioning of the organism. It can be considered as "modulating" or "fine tuning", 104 but it is in fact, the highest level of control in the hierarchy of integrating functions within the organism. At the same time consciousness integrates, in a single individual, the human attributes with the integrative functioning of the body. Each subject reacts differently to stimuli and daily life situations, according to his personality and knowledge. I am not denying the existence of multiple complex processes such as controlled by subsystems not directed commanded by consciousness, as most of the so-called vegetative functions. Nonetheless, consciousness can overcome any subsystem in the control of any specific vegetative function, and it is the ultimate integrating function. Plum extensively discusses this issue, 47 when he describes the importance of the second component in the regulation and integration of affect, mood, attention, cognitive integration, and psychic energy (cathexis) by limbic structures. Therefore, my notion of consciousness as the ultimate integrative function is more consistent with the biologically-based systems concepts of Korein 16,124 and Bernat et al. 1-5,87-92 than the more philosophically-based notions of personhood favored by Veatch, 38-40,114 Barlett and Youngner, 7 Wikler, 44,111,112 and others. 42,43 Criterion 32 As it has been shown, substantial interconnections among the brainstem, subcortical structures and the neocortex, are essential for subserving and integrating both components of human consciousness. 9,18,47,77 Therefore, consciousness generation is based on anatomy and physiology throughout the brain (criterion). Feinberg 65 quoted an interesting Sherrington's address: "Where it is a question of mind the nervous system does not integrate itself by centralization upon one pontifical cell". Tests Establishing a reliable system to measure the irreversible loss of consciousness is very difficult. The already difficult physiologic proof of loss of consciousness is compounded by the philosophic complexity of assessing the subjective dimension of consciousness. 60,65 Most sets of brain cessation tests require evidence of unresponsiveness. This is mainly measured by applying painful stimuli. 10,12,131 Reactivity to pain explores the arousal component of consciousness that endows cognitive and affective functions. 9 The substratum for consciousness is based on anatomy and physiology throughout the brain. 9,18,47,77 Therefore, sets of criteria should include tests to evaluate both brainstem and cerebral hemispheres. Comparing this standard of death, with whole brain, brainstem, and higher brain views, differences and similarities can be found. WHOLE BRAIN VIEW 33 SIMILARITIES DIFFERENCE Both views are based on anatomy and In my view, only one function is physiology throughout the brain (criterion) PVS cases are classified as alive considered (consciousness) as the hallmark of the definition rather than all functions of the brain BRAINSTEM VIEW SIMILARITIES DIFFERENCE In both views one of the components of In the brainstem view, the consciousness is included as a hallmark brainstem is only considered as the (capacity for consciousness or arousal) anatomical substratum (criterion). PVS cases are classified as alive HIGHER BRAIN SIMILARITIES DIFFERENCE 34 In both views consciousness is considered as hallmark for defining death In this view, the neocortex is only considered as the anatomical substratum (criterion). PVS cases are classified as dead My definition consciousness identifies as the ultimate integrating function My notion of consciousness as the ultimate integrative function is more consistent based with systems the than philosophically-based biologicallythe more notions of personhood Persistent vegetative state patients are alive! The main finding in PVS is the preservation of arousal with an apparently loss of awareness. 9,78 As has been previously discussed, according to Kinney, 45 PVS denotes a "locked-out-syndrome", because the “cerebral cortex is disconnected from the external world”, explained by three main neuropathological patterns. Can we deny the existence of internal awareness in PVS, because they apparently seem to be 35 disconnected from the external world? The subjective dimension of awareness is philosophically impossible to test. 65 The Karen Ann Quinlan's brain showed a severe damage of the thalamus, with the cerebral hemispheres relatively spared. 69 We can ask ourselves if in a case like this, other activating pathways projecting to the cerebral cortex without relaying through the thalamus, could stimulate the cerebral cortex to provide internal awareness, although an apparently disconnection to the outer world is found by physicians. 9 The use of deep brain stimulation showed that the cerebral hemispheres could mediate arousal producing some wakefulness behavior, even after complete loss of the brainstem's reticular activating system. 82-85 it has been discussed that there is striking evidence that subcortical structures are capable of mediating some forms of awareness. 9,45 Therefore, in PVS cases it is impossible to deny a possible preservation of internal awareness, because according to the neuropathological pattern, either subcortical structures could provide internal awareness, or some remaining activating pathways projecting to the cerebral cortex without relaying through the thalamus, could stimulate the cerebral cortex. 9 As consciousness is based on anatomy and physiology throughout the brain, it is impossible to classify a PVS case as dead, where the brain is damaged, but not fully and irreversible destroyed. Some reports of misdiagnosis or recuperation in PVS have also appeared in recent literature. Unexpected and well-documented recoveries of cognitive functions have been described in patients, where it was believed that the criteria were correctly applied by neurologists experienced and skilled in the diagnosis of this condition. 132, 133 Moreover, it is necessary to consider the potential reversibility of the awareness in the 36 PVS, as has been reported by some authors using deep brain stimulation. 82-85 it is crucial to develop controlled multi-centered studies to test and elaborate new protocols for sensory and pharmacologic stimulation. 117,132 In fact, the possibility of brain function restoration in such patients, by actual or still not developed techniques, are a challenge for the near future. 9 FINAL REMARKS In conclusion, I propose a standard of human death that includes consciousness as the most important function of the body, because it provides the capacity for integrating the main human attributes with an integrative functioning of the body. I have emphasized that consciousness does not bear a simple one-to-one relationship with higher or lower brain structures, because the physical substratum for consciousness is based on anatomy and physiology throughout the brain. 37 ACKNOWLEDGMENTS I would like to thanks Dr. Stuart Younger because of his careful reviews and precise suggestions, during the elaboration of this paper. 38 REFERENCES 1. Bernat JL: On the definition and criterion of death. Ann Int Med 1981;94:389-394. 2. Bernat JL. Brain death. Occurs only with destruction of the cerebral hemispheres and the brain stem. Arch Neurol 1992;49(5):569-570 3. Bernat JL: The definition, criterion and statute of death. Seminars in Neurology 1984; 4:45-51. 4. Bernat JL. How much of the brain must die in brain death. The Journal Clinical Ethics 1992; 3:21-28. 5. Bernat JL. Ethical issues in Neurology. In: Joynt, RJ, ed. Clinical Neurology. Philadelphia: JB Lippincott Company; 1991:1-105. 6. Halery A, Brody B. Brain death: reconciling definitions, criteria and tests. Ann Int Med 1993; 119:519-525. 7. Bartlett ET, Youngner SJ. Human death and the destruction of the neocortex. In: Zaner RM, ed. Death: Beyond the Whole-Brain Criteria. New York: Kluwer Academic Publisherm; 1988:199-215. 8. Machado C. Death on neurological grounds. J Neurosurgical Sciences 1994;38: 209-222. 9. Machado C. A new definition of death based on the basic mechanisms of consciousness generation in human beings. In: Machado C, ed. Brain Death (Proceedings of the Second International Symposium on Brain Death). Amsterdam: Elsevier Science, BV; 1995:57-66. 39 10. Beecher HK. A definition of irreversible coma: report of the Ad Hoc Committee of the Harvard Medical School to examine the definition of brain death. JAMA 1968; 205:85-88. 11. Molinari GF. The NINCDS collaborative study of brain death: a historical perspective. In: U. S. Department of Health and Human Services, NINCDS Monograph No. 24 NIH Publication No. 81-2226, 1980:1-32. 12. Walker AE. An appraisal of the criteria of cerebral death. A summary statement. A collaborative study. JAMA 1977; 237:982-986. 13. Guidelines for the Determination of Brain Death. Report of the Medical Consultants on the Diagnosis of Death to the President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. JAMA 1981; 246:2184-2186. 14. President's Commission for the Study of Ethical Problems in Medicine and Behavioral Research: Defining Death. Medical Legal and Ethical Issues in the Determination of Death. Washington, DC: U. S. Government Printing Office; 1981. 15. Walker A. E. (Ed.): Cerebral Death. Baltimore: Urban & Schawarzenberg, 1981. 16. Korein J. The problem of brain death: Development and history. In: Korein J, ed. Brain Death: Interrelated Medical and Social Issues. New York: Ann NY Acad Sci, 1977; 315:19-38. 17. Ingvar DH, Widen L. Brain death: summary of a symposium. Lakartidningen 1972; 69:3804-3814. 18. Plum F, Posner JB. The Diagnosis of Stupor and Coma. Philadelphia: FA Davis Company; 1980. 40 19. Black PMcL. Criteria of brain death. Review and comparison. Postgraduate Medicine 1975; 57:69-74. 20. Ouaknine G. Bedside procedures in the diagnosis of brain death. Resuscitation 1975; 4:159-177. 21. Machado C. Multimodality evoked potentials and electroretinogaphy in a test battery for an early diagnosis of brain death. J Neurosurgical Sciences 1993; 37:125-131. 22. Deliyannakis E, Loannou F, Davaroukas A. Brain-stem death with persistence of bioelectric activity of the cerebral hemispheres. Clin Electroencephalograph 1975; 6:75-79. 23. Ashwal S, Schneider S. Failure of electroencephalography to diagnose brain death in comatose patients. Ann Neurol 1979; 6:512-517. 24. Chatrian G. electrophysiological evaluation of brain death: a critical appraisal. In: Aminoff MJ, ed. Electrodiagnosis in Clinical Neurology. New York: Churchill Livingstone, 1986:669-736. 25. Truog RD. Is it time to abandon brain death? Hasting Center Report 1997;27:2937. 26. Howlett TA, Keogh AM, Perry L, et al. Anterior and posterior pituitary function in brain-stem-dead donors. A possible role for hormonal replacement therapy. Transplantation 1989; 47:828-834. 27. Fiser DH, Jimenez JF, Wrape V, et al. Diabetes insipidus in children with brain death. Crit Care Med 1987; 15:551-553. 28. Pallis C. Brainstem death. In: Braakman R, ed. Handbook of Clinical Neurology: Head Injury. Amsterdam:Elsevier Science Publisher BV, 1990: 13 (57): 441-496. 41 29. Pallis C. Death-Beyond the whole-brain criteria. J Neurol Neurosurg Psychiatry 1989; 52:1023-1024. 30. Pallis C, Maggillivray B. Brain death and the EEG. Lancet 1980; 2:1085-1086. 31. Pallis C, Prior PF. Guidelines for the determination of death. Neurology 1983; 33:251-252. 32. Pallis C. Whole-brain reconsidered - physiological facts and philosophy. J Medical Ethics 1983; 9:32-37. 33. Conference of Royal Colleges and Faculties of the United Kingdom: Diagnosis of brain death. Lancet 1976; 2:1069-1070. 34. Conference of Royal Colleges and their Faculties of the United Kingdom: Memorandum on the diagnosis of brain death. Br Med J 1979; 1:322. 35. Jennett B. Brain death (Editorial). Br J Anaesth 1981; 53:1111-1119. 36. Jennett B, Hessett C. Brain death in Britain as reflected in renal donors. Br Med J 1981; 283:359-362. 37. Shewmon A. Recovery from “brain death”: a neurologist’s apologia. Linacre Quartely 1997; pp:30-96. 38. Veatch RM. The definition of death: ethical, philosophical, and policy confusion. In: Korein J, ed. Brain Death: Interrelated Medical and Social Issues. New York: Ann NY Acad Sci 1977; 315:307-317. 39. Veatch RM, ed. Death, dying, and the biological revolution. Our last responsibility. New Haven: Yale University Press; 1989. 40. Veatch RM. Brain death: welcome definition… or dangerous judgment? Hasting Center Report 1972; 11:10-13. 42 41. Truog RD, Flacker JC. Rethinking brain death. Critical Care Medicine 1992; 20:1705-1713. 42. Cranford RE, Smith DR. Consciousness: the most critical moral (constitutional) standard for human personhood. American Journal of Law and Medicine 1990; 332:669-674. 43. Youngner SJ, Bartlett ET. Human death and high technology: the failure of the whole-brain formulations. Ann Intern Med 1983;99:252-258. 44. Green, MB, Wikler, D. Brain death and personal identity. Philosophy and Public Affairs 1908; 2:105-133. 45. Kinney, HC, Samuels, MA. Neuropathology of the persistent vegetative state: A Review. J. Neuropathology and Experimental Neurology 1994; 53:548-558. 46. The Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state. N Engl J Med 1994;330:1499-1508. 47. Plum P. Coma and related global disturbances of the human conscious state. In: Peters A, ed. Cerebral Cortex, Vol 9. New York: Plenum Publishing Corporation; 1991:359-425. 48. Steriade M. Arousal: revisiting the reticular activating system. Science 1996;272:225-226. 49. Moruzzi G, Magoun HW. Brain stem reticular formation and activation of the EEG. Electroencephalogr Clin Neurophysiol 1949; 1:455-473. 50. Destexhe A, Contreras D, Steriade M. Mechanisms underlying the synchronizing action of corticothalamic feedback through inhibition of thalamic relay cells. Neurophysiol 1998;79:999-1016. 43 51. Steriade M. Synchronized activities of coupled oscillators in the cerebral cortex and thalamus at different levels of vigilance. Cereb Cortex 1997;7:583-604. 52. Amzica F, Neckelmann D, Steriade M. Instrumental conditioning of fast (20- to 50Hz) oscillations in corticothalamic networks. Proc Natl Acad Sci USA 1997;94:1985-1989. 53. Contreras D, Destexhe A, Sejnowski TJ, Steriade M. Control of spatiotemporal coherence of a thalamic oscillation by corticothalamic feedback. Science 1996;274:771-774 54. Steriade M, Contreras D, Amzica F, Timofeev I. Synchronization of fast (30-40 Hz) spontaneous oscillations in intrathalamic and thalamocortical networks. J Neurosci 1996;16:2788-2808. 55. Steriade M. Arousal: revisiting the reticular activating system. Science 1996;272:225-226. 56. Steriade M, Amzica F. Intracortical and corticothalamic coherency of fast spontaneous oscillations. Proc Natl Acad Sci U S A 1996;93:2533-2538. 57. Steriade M, Amzica F, Contreras D. Synchronization of fast (30-40 Hz) spontaneous cortical rhythms during brain activation. J Neurosci 1996;16:392-417. 58. Steriade M. Awakening the brain. Nature 1996;383:24-25. 59. Contreras D, Steriade M. Cellular basis of EEG slow rhythms: a study of dynamic corticothalamic relationships. J Neurosci 1995;15:604-622. 60. Bogen, JE. Some neurophysiological aspects of consciousness. Seminars in Neurology 1997; 17:95-103. 61. Kinsbourne, M. The intralaminar thalamic nuclei: subjectivity pumps or attentionaction coordinators? Consciousness and cognition 1995; 4:167-171. 44 62. Villablanca J, Salinas-Ceballos ME. Sleep-wakefulness, EEG and behavioral studies of chronic cats without the thalamus. The ‘athalamic cat’. Arch Ital Biol 1972;110:383-411. 63. Mountcastle, VB. An organization principle for cerebral function: the unit module and the distributed system. In: Edelman, GM, Mouncastle, VB, eds. The mindful brain. Cambridge: The MIT Press;1978:7-50. 64. Goldman-Rakic PS. Topography of cognition: Parallel distributed networks in primate association cortex. Ann Rev Neurosci 1988;11:137-156. 65. Feinberg TE. The irreducible perspectives of consciousness. Semin Neurol 1997;17:85-93 66. Singer W, Gray CM. Visual feature integration and the temporal correlation hypothesis. Annu Rev Neurosci 1995; 18:555-586. 67. Schneider H, Ballowitz L, Schachinger H, Hanefeld F., Droszus JU. Anoxic encephalopathy with predominant involvement of basal ganglia, brain stem and spinal cord in the perinatal period. Report of seven newborns. Acta Neurpathol 1975; 32:287-298. 68. Ingvar, DH, Brun, A, Johansson, L, Sammuelsson, SM. Survival after severe cerebral anoxia with destruction of the cerebral cortex: the apallic syndrome. In: Korein J, ed. Brain Death: Interrelated Medical and Social Issues. New York: Ann NY Acad Sci;1977,315:184-214. 69. Kinney HC, Korein J, Panigraphy A, Dikkes P, Goode R. Neuropathologic findings in the brain of Karen Ann Quinlan: The role of the thalamus in the persistent vegetative state. N Engl J Med 1994;330:1469-1475. 45 70. Brierley JB, Adams JH, Graham DI, Simpsom JA. Neocortical death after cardiac arrest. A clinical, neurophysiological, and neuropathological report of two cases. Lancet 1972;2:560-565. 71. Villablanca, JR. Independent forebrain and brainstem controls for arousal and sleep. Behav Brain Sci 1981;4:494-496. 72. Adams JH, Grahan DI, Murray LS, Scott G. Diffuse axonal injury due to nonmisile head injury in humans: An analysis of 45 cases. Ann Neurol 1982; 12:557-563. 73. Ginsberg MD, Hedley-Whyte ET, Richardson EP. Hypoxic-ischemic leukoencephalopathy in man. Arch Neurol 1976;33:5-14. 74. Carota A, Pizzolato GP, Gailloud P, et al. A panencephalopathic type of Creutzfeldt-Jakob disease with selective lesions of the thalamic nuclei in 2 Swiss patients. Clin Neuropathol 1996;15:125-134. 75. Squire LR, Moore RY. Dorsal thalamic lesion in a noted case of human memory dysfunction. Ann Neurol 1979; 6:503-506. 76. Guberman A, Stuss D. The syndrome of bilateral paramedian thalamic infarction. Neurology 1983; 33:540-546. 77. Shewmon, DA. “Brain Death”: A valid theme with invalid variations, blurred by semantic ambiguity. In: Angstwurm H, Carrasco de Paula I, ed. Working Group on The Determination of Brain Death and its Relationship to Human Death: Vatican City: Pontificia Academia Scientiarum, 1992; pp:23-51. 78. Shewmon, DA. The metaphysics of brain death, persistent vegetative state, and dementia. The Thomist 1985;49:24-80. 46 79. Villablanca JR, Burgess JW, Olmstead CE, Levine MS. Recovery of function after neonatal or adult hemispherectomy in cats: I-III. Behav. Brain Res 1986;19:205226. 80. Brodal A, ed. Neurological Anatomy in Relation to Clinical Medicine, 3rd ed, New York: Oxford University Press;1981:394-447. 81. Shewmon DA, Holmes GL. Brainstem plasticity in congenitally decerebrated children. Brain & Devel 1990;12:664. 82. Hassler R, Dalle Ore G, Bricolo OA, et al. Behavioral and EEG arousal induced by stimulation of unspecific projection systems in a patient with post-traumatic apallic syndrome. Electroencephalogr Clin Neurophysiol 1969; 27:306-310. 83. Katayama Y, Tsubokawa T, Yamamoto T, et al. Characterization of brain activity with deep brain stimulation in patients in a persistent vegetative state: pain-related late positive component of cerebral evoked potential. Pace 1991;14:116-121. 84. Sturm V, Kühner A, Schmitt HP, Assmus H, Stock G. Chronic electrical stimulation of the thalamic unspecific activating system in a patient with coma due to midbrain and upper brain stem infarction. Acta Neurochirurgica 1979;47:235-244. 85. Cohadon F, Richer E. Stimulation cérébrale profonde chez des patients en état végétatif post-traumatique. 25 observations. Neurochirurgie 1993;39:281-292. 86. Austin GM, Grant FC. Physiologic observations following total hemispherectomy in man. Surgery 1958; 38:239-258. 87. Bernat JL. Ethical issues in brain death and multiorgan transplantation. Neurol Clin 1989; 7:715-728 88. Bernat JL. Ethical and legal aspects of the emergency management of brain death and organ retrieval. Emerg Med Clin North Am 1987;5:661-676. 47 89. Bernat JL, Culver CM, Gert B. Definition of death. Ann Intern Med 1984 Mar;100(3):456 90. Bernat JL, Culver CM, Gert B. Defining death in theory and practice. Hastings Cent Rep 1982;12(1):5-8. 91. Bernat JL, Culver CM, Gert B. Definition of death. Ann Intern Med 1981;95:652 92. Bernat JL. A defense of the whole-brain concept of death. Hasting Center Report 1998;28:14-23. 93. Pallis, C. ABC of the brain stem death. The arguments about the EEG. Brit Med J 1983; 286:284-287. 94. Rodin E, Tahir S, Austin D, Andaya L. Brainstem death. Clin Electroencephalogr 1985; 16:63-71. 95. Ferbert A, Buchner H, Ringelstein EB, Hacke W. Isolated brain-tem death. Case report with demonstration of preserved visual evoked potentials. Electr Clin Neurophsyiol 1986;65:157-160. 96. Lugo N, Silver P, Nimkoff L, Caronia C, Sagy M. Diagnosis and management algorithm of acute onset of central diabetes insipidus in critically ill children. J Pediatr Endocrinol Metab 1997;10:633-639 97. Hagl C, Szabo G, Sebening C, Tochtermann U, Vahl CF, Sonnenberg K, Hagl S. Is the brain death related endocrine dysfunction an indication for hormonal substitution therapy in the early period? Eur J Med Res 1997;2:437-440 98. Outwater, KM, Rockoff, MA. Diabetes insipidus accompanying brain death in children. Neurology 1984; 34:1243-1246. 99. Fackler, JC, Troncoso, JC, Gioia, FR. Age-specific characteristics of brain death in children. American Journal of Diseases of Childhood 1988; 142:999-1003. 48 100. Pallis, C. Brainstem death: the evolution of the concept. Seminars in Thoracic and Cardiovascular Surgery 1990; 2:135-152. 101. Pallis, C.: Death. Encyclopaedia Britanica. Vol 16. 1986:1030-1042. 102. Pallis, C. Death-Beyond the whole-brain criteria. J Neurol Neurosurg Psychiatry 1989; 52:1023-1024. 103. Lamb D (ed). Death, brain death and ethics. Australia:Croom Helm Ltd., 1985:1120. 104. Shewmon, AD. "Brain-stem death", "brain death" and death. A Critical reevaluation of the purported equivalence. Issues in Law and Medicine (In press). 105. Wikler D, Weisbard AJ. Appropriate confusion over `brain death'. JAMA 1989; 261:2246. 106. Milhaud A, Riboulot M, Gayet H. Disconnecting tests and oxygen uptake in the diagnosis of total brain death. In: Korein J, ed. Brain Death: Interrelated Medical and Social Issues. New York: Ann NY Acad Sci, 1977; 315:241-251. 107. Schwarz G, Lischer G, Pfurtscheller G, et al. Brain death: timing of apnea testing in primary brain stem lesions. Intensive Care Med 1992; 18:315-316. 108. Parisi JE, Kim RC, Collins GH, Hilfinger MF. Brain death with prolonged somatic survival. N Engl J Med 1982;306:14-16. 109. Fabro F. Brain death with prolonged somatic survival (Letter). New Engl Med 1982;306:1361. 110. Kim RC, Parisi JE, Collins GH, Hilfinger MF. Brain death with prolonged somatic survival (Response to letter). New Engl J Med 1982;306:1362-1363. 49 111. Wikler D. Who defines death? Medical, legal and philosophical perspectives. In: Machado C, ed. Brain Death (Proceedings of the Second International Symposium on Brain Death). Amsterdam:Elsevier Science, BV;1995:13-22. 112. Wikler, D. Not dead, not dying? Ethical categories and the persistent vegetative state. Hastings Center Rep 1988; 18:41-47. 113. Puccetti, R. Does anyone survive neocortical death? In Zaner RM, ed. Death: Beyond Whole-Brain Criteria. Boston:Kluwer Academic Publishers;1988:75-90. 114. Veatch RM. Defining death: the role of brain function. JAMA 1979;242:2001-2002. 115. Rosenberg, GA, Johnson, SF, Brenner, RP. Recovery of cognition after prolonged vegetative state. Ann. Neurol. 1977; 2:167-168. 116. Steinbock B. Recovery from persistent vegetative state? The case of Carrie Coons. Hastings Cent Rep 1989; 19:14-15. 117. Giacino JT. Disorders of consciousness: Differential diagnosis and neuropathological features. Seminars in Neurology 1997;2:105-111. 118. Cohen-Almagor R. Some observations on post-coma unawareness patients and on other forms of unconscious patients: policy proposals. Med Law 1997;16:45147. 119. Childs NL, Mercer WN, Childs HW. Accuracy of diagnosis of persistent vegetative state. Neurology 1993; 43:1465-1467. 120. Andrews K, Murphy L, Munday R, Littlewood C. Misdiagnosis of the vegetative state: retrospective study in a rehabilitation unit. Brit Med J 1996;313:13-16. 121. Ott B. Defining and redefining death. Am J Crit Care 1995;4:476-480. 50 122. Singer P. Is the sanctity of life terminally ill? In: Machado C. Brain Death (Proceedings of the Second International Symposium on Brain Death). Amsterdam: Elsevier Science BV;1995:231-244. 123. Botkin JR, Post SG. Confusion in the determination of death: Distinguishing philosophy from physiology. Perspectives in Biology and Medicine 1992;36:129138. 124. Korein J. Ontogenesis of the brain in the human organism: definitions of life and death of the human being and person. In: Edwards RB, Ed. Advances in Bioethics, Vol 2. New York: JAI Press Inc;1997:1-74. 125. Varela FJ. Principles of Biological Autonomy. New York: North Holland, 1979. 126. Swedish Committee on Defining Death: The concept of death. Summary. Stockholm: Swedish Ministry of Health and Social Affairs; 1985. 127. García OD, Machado C, Román JM, et al. Heart rate variability in coma and brain death. In: Machado C, ed. Brain Death (Proceedings of the Second International Symposium on Brain Death). Amsterdam: Elsevier Science BV, 1995:191-200. 128. Telles S, Nagarathna R, Nagendra HR. Autonomic changes during "OM" meditation. Indian J Physiol Pharmacol 1995;39:418-420. 129. Schou M. Treating recurrent affective disorders during and after pregnancy. What can be taken safely? Drug Saf 1998;18:143-152. 130. Christie GL. Some socio-cultural and psychological aspects of infertility. Hum Reprod 1998; 13:232-241. 131. Machado, C. and García, A. Guidelines for the determination of brain death. In: Machado C, de. Brain Death (Proceedings of the Second International Symposium on Brain Death). Amsterdam: Elsevier Science B V, 1995:75-80. 51 132. Wilson SL, Powell GE, Brock D, Thwaites H. Vegetative state and responses to sensory stimulation: an analysis of 24 cases. Brain Inj 1996;10:807-818 133. Caplan L. Late improvement after post-traumatic vegetative state. N Engl J Med 1996; 334:1201-1202 52 53