NATIONAL CHENG KUNG UNIVERSITY MEDICAL COLLEGE

NATIONAL CHENG KUNG UNIVERSITY MEDICAL COLLEGE
MEDICAL MICROBIOLOGY COURSE
Wednesday, February 18, 2004, 8:10-9:00 a.m.
INTRODUCTION TO THE IMMUNE SYSTEM
Yee-Shin Lin, Ph.D.
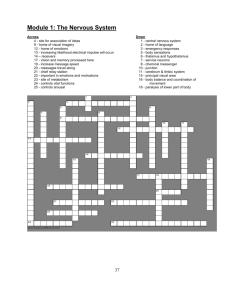
A. BACKGROUND
The immune system is the second line of defense against invasion by foreign organisms. [The integument is the first] [ Fig. 1.1
]. In addition, the immune system polices and destroys spontaneously arising tumor cells in the body. Sounds simple, doesn't it? However, the immune system must first make the distinction between normal tissues (self) and abnormal or foreign
(non-self) tissues. The molecular determinants recognized by the immune system are called epitopes . One or more epitopes are collectively called an antigen [ Fig. 1.11
].
Reading: Roitt, Brostoff & Male [ chapter 1 ]
Pre-class assigned reading: Page/Column 1R, 2, 3, 6R, 7, 8, 9L, 11R, 12L;
Fig. 1.1, 1.4, 1.9, 1.11, 1.13, 1.19
B. LECTURE SUMMARY
ANTIGENS -- SELF vs. NON-SELF
The immune system distinguishes what is SELF from what is NON-SELF, the "us" and the "them", on a cellular and molecular level. It recognizes bacteria, viruses, protozoa, fungi, etc.
Immunologists use the collective term antigen to identify any substance recognized by the immune system. There are 3 distinct subsets of antigens:
Immunogen: substance recognized by the immune system that provokes an immune response.
Hapten: a substance recognized by the immune system, but that does not, by itself, induce an immune response.
Tolerogen: a substance that paralyzes and doesn't allow the induction of the immune response or a substance that specifically turns off an immune response [ chapter 12 ].
Although the immune system does not respond to an isolated hapten, it will respond to a hapten physically coupled to an immunogen. The immunogen to which hapten is coupled is termed a carrier . When the immune system recognizes a hapten-immunogen (or hapten-carrier) complex, an
immune response occurs directed against both hapten and carrier.
Injection of an animal with an immunogen, resulting in the elicitation of an immune response, is called immunization .
What does the immune system recognize? Most immunogens contain multiple antigenic determinants called epitopes . An epitope is the basic minimal structure recognized by the immune system. Most immunogens are composed of a variety of epitopes, whereas most haptens comprise a single epitope. Some general characteristics of IMMUNOGEN :
1. must be recognized as non-self
2. physical properties
size -- usually proteins > 10,000 daltons (proteins and carbohydrates best, nucleic acids can also be immunogenic. Lipids in most cases are not.)
complexity -- more complex the molecule --> more potential epitopes --> more chance for these epitopes to be recognized as foreign
conformation and accessibility -- epitopes must be "seen" by and be available to the immune system (some tissues of the body are not normally "seen" by the immune system, e.g. anterior chamber of the eye, brain, etc.)
charge -- does not appear to be important
3. chemical properties -- the immunogen, in most cases, has to be subject to enzymatic cleavage by phagocytes
In the immune system, phagocytes ingest foreign materials, enzymatically cleave them, and display them on their cell membranes. This mechanism is called antigen processing and is usually necessary for the induction of an immune response.
The induction of an immune response is quite complex, involving the interaction of several different types of cells. Immune responses are also determined by the genetic characteristics of the individual [will be detailed in chapter 11 ].
INNATE vs. ADAPTIVE IMMUNITY
The immune response is mediated by a variety of molecules and cells, and can be broadly divided into two functional divisions, namely the innate immunity and the adaptive immunity [ p. 1 ]. The components of the immune system are listed in Fig. 1.4
.
INNATE IMMUNITY
If the body's exterior barrier fails to prevent the invasion of the infectious agents, the innate immunity will serve as a first line of defense against these infectious agents.
The cells and molecules involved in the innate immunity are as follows:
1.
Phagocytes : Their function is to engulf foreign materials, internalize them and destroy them.
The phagocytes include:
polymorphonuclear neutrophils (PMN): short-lived cells
monocytes/macrophages (reticuloendothelial system or mononuclear phagocyte system): long-lived cells [ Fig. 1.5
]
2.
Natural killer (NK) cells (Large granular lymphocytes, LGLs) : They are able to kill viral-infected and tumor cells to which they have not been previously sensitized [ Fig. 1.6
].
3.
Soluble factors
acute phase proteins, e.g. C-reactive protein (CRP): increase 2 to 100X during infection, and act as an opsonin to promote the binding of complement which facilitates phagocytosis.
complement: consists of a group of about 20 serum proteins which cause direct lysis of bacteria, chemotaxis and opsonization [ Fig. 1.7
and chapter 3 ].
interferons: limit the spread of viral infection and enhance NK cell activity [ Fig. 1.8
].
APTIVE IMMUNITY
Two key features of adaptive immune response are specificity and memory . This is accomplished by either B cells which produce antibodies or T cells which include T
H
, Tc [ Fig. 1.6
]. These are referred to as two arms of the immune system: humoral immunity and cell-mediated immunity .
These two systems of immunity act in concert to provide protection for the host.
INTERACTION BETWEEN INNATE AND ADAPTIVE IMMUNE SYSTEMS [ Fig. 1.3
]
Examples:
1.
Antibody acts as a flexible adaptor ( opsonin ) between the infectious agent and phagocyte [ Fig.
1.9
]. Antibody also causes the activation of complement, the infectious agent often has both antibody and C3b bound to the surface. The attachment and phagocytosis are therefore greatly enhanced [ Fig. 1.10
].
2.
Cytokines released by T cells activate the phagocytes to destroy infectious agents more effectively.
3.
Phagocytes process and present the antigen to T cells.
CLONAL SELECTION
Concept : The immune system has a specific cell for each the millions of possible epitopes.
Scientists estimate that the antigenic universe contains between 10 6 and 10 7 epitopes. This means that there are at least 10 6 to 10 7 different B or T cells. Lymphocytes are very specialized, whenever the term antigen specific is used, this means that there is a cell (B or T cell) resident in the immune system for each of the 10
6 and 10
7
epitopes! [ Fig. 1.11-1.13
]
INFLAMMATION [This process is described more fully in chapter 3 ]
Three major things occur:
Increased blood supply to the infected area.
Increased capillary permeability.
Leucocytes migrate out of the venules into the surrounding tissues. This process includes pavementing , diapedesis , chemotaxis , and phagocytosis . [ Fig. 1.17, 1.15
].
DEFENCES AGAINST EXTRACELLULAR AND INTRACELLULAR PATHOGENS: [ Fig.
1.2, 1.18
]
VACCINATION [ Fig. 1.19
] -- detailed in Tetanus Immunity Workbook
IMMUNOPATHOLOGY: Hypersensitivity, immunodeficiency, and autoimmunity [ Fig. 1.20
]
C. ImmunObjectives -- a self assessment
1. Define:
self/non-self
immunologic memory
inflammation
opsonization
vaccination
2. Define antigen, distinguish it from immunogen. What is an epitope?
3. Describe the soluble factors and cells involved in innate and adaptive immunity, respectively, and the function of each factor and cell.
4. Describe chemotaxis and phagocytosis that are involved in inflammation process.
5. Describe the difference between immune responses to extracellular and intracellular pathogens.
6. Describe how the immune system may itself cause diseases to a person.
NATIONAL CHENG KUNG UNIVERSITY MEDICAL COLLEGE
MEDICAL MICROBIOLOGY COURSE
Wednesday, February 18, 2004, 9:10-10:00 a.m.
CELLS, TISSUES AND ORGANS OF THE IMMUNE SYSTEM
Yee-Shin Lin, Ph.D.
A. BACKGROUND
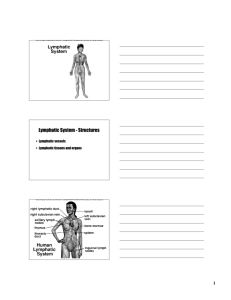
Leukocytes, the cells of the immune system, traverse the entire body via the circulatory system.
Accumulations of white blood cells are known as the spleen, thymus, lymph nodes, tonsils, Peyer's patches, and appendix. Each leukocyte has its own specific tasks to perform. Several cell types will be introduced in this lecture.
Reading: Roitt, Brostoff & Male [ chapter 2 ]
Pre-class assigned reading: Page/Column 15, 16L, 17, 19R, 20-22, 24, 25R, 27, 28, 29L, 30L, 31L,
32R, 33, 34L, 35L, 36R, 37L, 38R, 39R, 40L, 41R, 42L; Fig. 2.18, 2.21, 2.22, 2.36, 2.39, 2.41, 2.62
B. LECTURE SUMMARY
CELLS INVOLVED IN THE IMMUNE RESPONSE
The cells of the immune system arise from pluripotent hemopoietic stem cells through two main lines of differentiation:
1. Lymphoid lineage: T cells, B cells, and NK cells
2. Myeloid lineage: monocyte/macrophage, neutrophil, eosinophil, basophil/mast cell, platelets
The cells involved in the immune response can be divided into 3 general categories: lymphocytes,
phagocytes, and accessory cells.
[see also Fig. 2.1, 2.7
]
LYMOHOCYTES: The average human adult has about 10
12
lymphocytes. Lymphoid cells represent about 20% of the total leukocytes present in the circulation. Two distinct types of resting lymphocytes can be distinguished in the circulation: The first is relatively small, agranular, and has a higher N:C ratio (i.e., T and B cells). The second type is larger, has a lower N:C ratio, and contains granules (i.e., LGL). While the T and B cells look alike by both light and electron microscopy, they differ widely in function. Different categories of lymphocytes are based upon their embryological origin and this relates to their function and distinguishing surface molecules
(markers).
T cells : originate in the bone marrow as prothymocytes. They migrate via the circulation to the thymus. Lymphocytes within the thymus (thymocytes) are indoctrinated ("educated") by the mechanisms including positive and negative selections, such that they have the ability to distinguish self from non-self (foreign). T cells comprise 60-70% of all peripheral blood lymphocytes.
Collectively, T cells display a number of diverse functions: [will be detailed in subsequent lectures]
1.
Regulate humoral immune response, they can heighten or diminish an immune response.
2.
Regulate cellular immune responses (immune responses directly mediated by cells not Ab such as items 3-6 below).
3.
Delayed-type hypersensitivity (DTH): an example of this type of response would be the cellular infiltration causing swelling following a tuberculin skin test.
4.
Contact sensitivity (CS): cellular infiltration causing swelling and itching following exposure to poison ivy. Related to DTH.
5.
Transplantation immunity: graft rejection is usually mediated by T cells.
6.
Cytotoxic T lymphocyte (CTL) activity: when activated this T cell comes into contact with another cell and causes its lysis, the "kiss of death".
Distinguishing surface characteristics of T cells: [ Fig. 2.31; Appendix 2 ]
1. T cell receptor (TCR) and CD3 -- T cells have the ability to specifically recognize every epitope in the antigenic universe. This means that there are at least 10
6 to 10
7
distinct T cells resident in the immune system. The cell surface structure is called the T cell receptor.
Approximately 90-95% of blood T cells express TCR
, and the remaining 5-10% express TCR
[ Fig. 2.30
]. TCRs are associated with the CD3 complex to give the TCR-CD3 complex [see chapter 5 ].
2. CD4 and CD8 . These surface molecules are important in determining functionally different T
cell subsets [ Fig. 2.29, 2.30
]. The CD4
+
T cells have been further divided into subsets [ Fig. 2.30, chapter 7 ].
3. All human peripheral T lymphocytes express CD2 and spontaneously bind sheep erythrocytes (SRBC).
4. Other markers: e.g. CD5, CD28, CTLA-4 (CD152), CD45RO, and CD45RA.
T-cell differentiation:
1. Phenotypic changes during T-cell maturation [ Fig. 2.39
]
2. Positive and negative selection in the thymus [ Fig. 2.40, 2.41
]
3. Extrathymic T-cell development [ p. 34 ]
B cells are responsible for the production of immunoglobulins (antibodies). An organ in birds, a blind cloacal sac called the bursa of Fabricius , serves as the indoctrination site for these precursors of antibody secreting cells ( plasma cells ). Mammals do not have this organ, but bone marrow serves as the equivalent differentiation site. The term "B" cell is a mnemonic for the bursal or bone marrow origin of these cells. B cells normally comprise 5-15% of the peripheral blood lymphocytes.
Distinguishing surface characteristics of B cells: [ Fig. 2.31
]
1.
Surface Ig and Ig
(CD79a)/Ig
(CD79b) -- B cells express both surface and cytoplasmic Ig.
The pre-B cells express cytoplasmic but not surface Ig. Cells that secrete Ig are termed plasma cells. Moreover, B cells are specific, that is they produce Ig of only one Ab specificity that recognizes only one epitope. Like CD3 in the TCR-CD3 complex of T cells, Ig
and Ig
are involved in cellular activation.
2.
MHC class II molecules -- they are specifically recognized by T cells and are functionally important in the regulation of the immune response, i.e. I-A and I-E in mouse, and HLA-DP,
DQ and DR in human.
3.
CR1 (CD35) and CR2 (CD21) -- surface receptors for complement, which are associated with activation and possibly "homing" of the cells.
4.
FcR -- a surface receptor for the Fc portion of the Ig molecule (Fc
RII, CD32), which play a role in negative signaling to the B cells. [see chapter 11 ]
5.
Other markers: e.g. CD5, CD19, CD20, CD22, CD40, and CD72.
B-cell differentiation
1.
Mammalian B cells develop in the bone marrow and fetal liver [ p. 35 ].
2.
Expression of Ig and other markers: [ Fig. 8.3
]
Natural Killer Cells (or Third population cells): NK cells have been defined by morphology as large granular lymphocytes (LGL). They comprise up to 15% of the peripheral blood lymphocytes.
The surface markers of human NK cells are shown in Fig. 2.16
. At least 2 distinct types of killing are known:
1.
Non-specific killing by NK cell -- are responsible for immunity against spontaneously arising tumors, thus acting as an immune surveillance mechanism. They are also cytotoxic for virus-infected cells. NK cells do not require Ag priming although NK activity is enhanced by
IFN
and IL-2. [see also Fig. 10.1
]
2.
ADCC -- sees Ab bound to foreign cell surfaces and lyses them. This complement (C) independent process is called antibody-dependent cell-mediated cytotoxicity (ADCC) and is mediated through the receptor for IgG. It is also known as killer (K) cell activity. [see also Fig.
10.6
]
MONOCYTES : ImmunoSynonyms -- macrophage, Langerhans cell of the epidermis, histiocytes, and cells of the mononuclear phagocyte system (or the reticuloendothelial system, RES). These are the scavengers or garbage collectors of the body. They pick up cellular debris, foreign cells and particles, etc., and enzymatically degrade it. They are morphologically distinct from lymphocytes.
Distinguishing surface characteristics of monocyte/macrophage: [ Fig. 2.8
]
1.
FcR -- surface receptor for Fc portion of Ig molecule, i.e., CD64, CD32, CD16
2.
CR -- surface receptor for the 3rd component of complement, i.e., CR1 (CD35)
3.
MHC class II molecules (HLA-D for human and I-A/I-E for mouse) -- important in presentation of antigens to T cells and functionally important in the regulation of the immune response
4.
Other markers: e.g. LFA-1 (CD11a/CD18), CD14, CD23(Fc
RII)
Function: Macrophages engulf (by phagocytosis) foreign particles, dead cells, etc., enzymatically
degrade this matter ( antigen processing ), and display the enzymatically degraded material on their cell membranes. T cells must see both processed antigen and the MHC class II molecule as the necessary initiation step in an immune response. Cells displaying antigen and MHC class II molecules are referred to as antigen presenting cells (APC) and the process of displaying antigen and MHC class II molecules is called antigen presentation.
[ Fig. 2.18, 2.21
]
POLYMORPHONUCLEAR GRANULOCYTES
Neutrophils: the most prominent leucocyte in the circulation, accounting for over 90% of the circulating granulocytes or 60-70% of the circulating leucocytes. Possess two main types of granules. Ingested organisms are contained within vacuoles termed phagosomes which fuse with the enzyme-containing granules (lysosomes) to form phagolysosomes. An increase in the numbers of circulating neutrophils indicates acute bacterial infection.
Eosinophils: comprise 2-5% of blood leucocytes. They are capable of phagocytosing and killing ingested microorganisms, can be triggered to degranulate by appropriate stimuli. Often found at sites of parasitic infections.
Basophils: found in circulation (less than 0.2% of leucocytes), may be equivalent of mast cells found in tissue. Large basophilic granules contain heparin, SRS-A (slow reactive substance of anaphylaxis), ECF-A (eosinophil chemotactic factor of anaphylaxis) and histamine. Bear FcR for
IgE. IgE is important in immediate hypersensitivity reactions (also called allergic reactions).
LYMPHOID TISSUES AND ORGANS
The immune system is highly dynamic. This is especially true for lymphocytes. Approximately one half of the lymphocytes recirculate as individual cells in the blood and lymph. Lymphoid tissues can be classified as organs (thymus, spleen and lymph nodes) and lymphoid accumulations
(mucosa-associated lymphoid tissues such as Peyer's patches and lymphocytes within the lamina propria, etc.). Two major types of lymphoid organs are found: primary (central) and secondary
(peripheral) lymphoid organs and tissues [ Fig. 2.36
]. Primary lymphoid organs are the major sites of lymphocyte development. Thymus and bone marrow are primary lymphoid organs. The secondary lymphoid organs trap and concentrate antigens and they are where specific immune reactions are generated.
THYMUS GRAND: This bilobed organ is the first lymphoid organ to develop during ontogeny. It increases in size during fetal and neonatal life and progressively involutes following puberty.
A stem cell, derived from the bone marrow (prothymocyte) and committed to the T cell lineage,
migrates via the circulation to the thymic cortex (cell is now called a cortical thymocyte).
Subsequently, it migrates through the cortico-medullary border into the medulla to mature. The mature thymocyte enters the circulation and is known as a T cell. It takes about 3 days for a prothymocyte to mature to a T cell.
LYMPH NODES: small round- or oval-shaped peripheral of secondary lymphoid organs. They function as a filter to purify lymph and as sites of initiation of the immune response. The lymph node system and structure are shown in Fig. 2.48, 2.51
. Anatomically the node is divided into the cortex and medulla. The reticulum or "framework" of the organ is composed of phagocytes
(macrophages) and specialized kinds of reticular or dendritic cells. Lymphocytes are distributed mainly in two areas of the cortex: cortex (B cell area) -- closely packed clusters of lymphocytes forming nodules of follicles.
Sometimes called the T-independent area. Contains mostly B cells. When an immune response takes place, the follicles develop a central area with large proliferating cells termed a germinal center . paracortex (T-dependent area) -- T cell-rich area.
Antigen trapping. Antigen is trapped either in the sinuses or paracortex by the reticular cells. This is an important step in the induction of immune responses. Most of the Ag taken up by the macrophage is readily enzymatically digested, but a few molecules escape total break down and these are the ones that interact with lymphocytes.
As soon as Ag is taken up by macrophage or reticuloendothelial cell, inductive events occur whereby lymphocytes recognize and interact with some of the trapped antigen molecules. This is manifest 24 h after Ag enters the node. There follows a marked decrease in the number of lymphocytes leaving the node. Presumably, lymphocytes keep entering the node from the postcapillary venules.
2 to 5 d later, lymphocytes leaving the node increase in number and more lymphocytes enter the node from the postcapillary venules. Lymphocytes specifically reactive with the Ag remain in the node. Cellularity of the node increases, often resulting in a swelling (something that the physician looks for during physical diagnosis). Proliferation becomes abundant in the cortex and the first
Ab-containing cells appear. Development of the cortex proceeds and germinal centers become evident. The germinal centers and interfollicular areas are abundant with plasma cells.
After another 5 d (8 to 11 d elapsed time), total numbers of cells leaving the node are reduced.
However, lymphocytes that have reacted with Ag (called primed or activated cells) now leave the node and are disseminated throughout the tissues.
SPLEEN: Clears particulate matter from the blood and concentrates blood-borne Ag. Histologically divided into the lymphocyte-rich white pulp and erythrocyte-rich red pulp . Lymphocytes are organized around small arteries and arterioles. Immediately surrounding the arteriole is a T-cell rich area. The B cells are organized into either primary or secondary follicles. [ Fig. 2.46
]
THE MUCOSAL LYMPHOID SYSTEM: M cells, lamina propria lymphocytes (LPL), intraepithelial lymphocytes (IEL) [see Fig. 2.60, 2.61, p. 42 ]
LYMPHOCYTE TRAFFIC: [see Fig. 2.62, 2.65
]
C. ImmunObjectives -- a self assessment
1. Define:
leucocytes -- granular, agranular
lymphoid lineage
myeloid lineage
mononuclear phagocyte system
T cell -- its functions, surface markers, and differentiation
B cell -- its functions, surface markers, and differentiation
2. What is meant by primary and secondary lymphoid organs, what is the function of each.
3. Describe the lymph node in terms of structure and function. You should know cortex, paracortex, medulla, afferent and efferent lymphatics and blood supply. What types of cells populate each area and how do they function in antigen trapping and initiation of an immune response?