Surgery: is any procedure performed on the human body that uses
advertisement

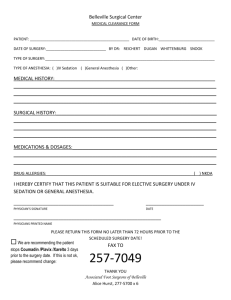
Surgery: is any procedure performed on the human body that uses instruments to alter tissue or organ integrity. Purposes of Surgical Procedures 1-Diagnostic: Confirms or establishes a diagnosis; for example, biopsy of a mass in a breast. 2-Palliative: Relieves or reduces pain or symptoms of a disease) it does not cure; for (resection of nerve roots) 3-Ablative : Removes a diseased body part; for example, removal of a gallbladder (cholecysteclomy) 4-Constructive: Restores function or appearance that has been lost or reduced (breast implant) 5-Transplant: Replaces malfunctioning structures; for example, kidney transplant. Categories of Surgery Based on Urgency 1-Emergency: Immediate; condition is life-threatening, requiring surgery at once (Gunshot wound, Severe bleeding and Small bowel obstruction) 2-Urgent: Within 24 to 30 hours; client requires prompt attention Kidney stones and acute gallbladder infection 3-Required: Planned for a few weeks or months after decision; client requires surgery at some point ( Benign prostatic hypertrophy, Cataracts and Hernia without strangulation) 4-Elective: Client will not be harmed if surgery is not performed but will benefit if it is performed (revision of scars) 5-Optional Personal preference Cosmetic surgery Surgical incision and location A. Sternal split: Begins at the top of the sternum and extends downward to the sternal notch (Heart) B. Oblique subcostal Begins in the epigastric area and extends laterally and obliquely below the lower costal margin Right side: Gallbladder, biliary and Left side: Spleen C. Upper vertical midline Begins below the sternal notch and extends distally around the umbilicus (Stomach, duodenum and pancreas). 1 D. Thoracoabdominal Begins midway between the xiphoid process and the umbilicus and extends across the seventh or eighth intercostal space to the midscapular line (Thorax and heart) E. McBurney Begins below the umbilicus, goes through McBurney’s point, and extends toward the right flank Appendix F. Lower vertical midline Begins below the umbilicus and extends downward toward the symphysis pubis (Bladder and uterus). G. Pfannenstiel Begins 1.5 inches above the symphysis pubis with a curved transverse cut across the lower abdomen (Uterus, fallopian tubes and ovaries) Surgical risk factor and potential complications 1-Age Older adults: Decreased metabolism and excretion of anesthetics and medications and fluid overload. 2-Nutritional Status *Malnourished: Fluid and electrolyte imbalances, delayed wound healing *Obese: Stressed cardiovascular system, decreased circulation, and decreased pulmonary function. 3-Substance Abuse: Altered respiratory function, nutritional status, liver function pneumonia, altered effectiveness of anesthetics and pain medications and drug interactions, 4-Medical Problems (Systematic problem) A-Immune: Allergies and immunosuppression secondary to corticosteroid therapy and chemotherapy. B-Respiratory; Acute and chronic respiratory problems and history of tobacco use atelectasis and respiratory failure C-Cardiovascular: Hypertension, coronary artery disease, peripheral vascular disease and congestive heart D-Hepatic:Liver dysfunction delayed drug metabolism leading to drug toxicity, disrupted clotting mechanisms leading to excessive bleeding or hemorrhage E-Renal: renal failure fluid and electrolyte imbalances and delayed excretion of drugs F-Endocrine—Diabetes, Hypoglycemia, hyperglycemia and hypokalemia 2 Perioperative phases 1. The preoperative phase begins when the decision to have surgery is made: it ends when the client is transferred to the operating table.. 2.The intraoperative phase begins when the client is transferred to the operating table and ends when the client is admitted to the postanesthesia care unit (PACU). also called the poslanesthetic room or recovery room 3. The postoperative phase begins with the admission of the client to the pos [anesthesia area and ends when healing is complete. The preoperative phase Surgical Consent Informed Consent/ Operative Permit: A form signed by the patient and a witness, granting permission to have the operation performed as described by the patient’s physician. Incompetent Client Legal: Individual who is not autonomous and cannot give or withhold consent (e.g., individuals who are cognitively impaired, mentally ill and urologically incapacitated) Rationale/Purposes of the Operative Permit: 1. It guards the client from unwanted surgical procedures. 2. It protects the health care facility staff from legal action. Preoperative Assessment 1-Review Client’s Health History and Preparation for Surgery • History of present illness and medical history • Any past problems with anesthesia and allergies • Substance use: alcohol, tobacco, street drugs • Vital signs • Level of consciousness: confusion ,drowsiness and unresponsiveness • Weight and height • Skin integrity • Level of exercise • Assess Psychological Needs 3 2-Review Preoperative Laboratory and Diagnostic Studies • Complete blood count • Blood type and crossmatch • Serum electrolytes • Urinalysis • Chest x-ray • Electrocardiogram • Other tests related to procedure Patient teaching in preoperative phase: • • • • • The goal of preoperative teaching Attainment of a sense of well-being with minimal fear of the unknown. Decreased need for analgesics Absence of complications Decrease time for hospitalization Preoperative exercise a. Diaphragmatic breathing b. Coughing exercises c. Leg exercises d. Turning to the side e. Getting out of bed Preoperative Medications • Anticholinergics, which decrease respiratory tract secretions, dry mucous membranes, and interrupt vagal stimulation • Histamine2-receptor antagonists, which decrease gastric acidity and volume • Opioids which decrease the amount of anesthesia needed, help reduce anxiety and pain, and promote sleep • Sedatives, which promote sleep, decrease anxiety, and reduce the amount of anesthesia needed Psychological Preparation: Reduction of preoperative anxiety and fear. Rationale/Purposes: 1. Less anesthesia administered during surgery and less analgesia required after surgery. 2. Rapid stabilization of pulse rate and blood pressure after surgery. 3. Faster physical recovery. 4. More active participation by patient in his recovery 4 Nursing Actions to reduce anxiety • Provide explanations or printed information about hospital routines including meal times and visiting hours. • Explain the procedures involved in the upcoming surgery. The patient and family should have a complete idea of what the pre, intra and postoperative phases may include. • Explain all nursing care and any possible discomfort that may result as a consequence of nursing intervention. • Allow the client to take the lead in asking questions. Give only as much information as the person wishes to know. Physical preparation 1-skin preparation: skin around the operative site is prepared to reduce the number of organisms present and to inhibit rebound growth. before or the day of surgery, the client washes the area involved in the surgical procedure with an antimicrobial soap and removing hair in the operative site. 2-nutrition: Clients scheduled for surgical procedures requiring only local anesthetic agents may be allowed a light breakfast or clear liquids the day of surgery. However, clients scheduled for general anesthesia are instructed not to eat or drink (NPO) for 6 to 8 hours before surgery. Restricting food and fluids decreases the risk of aspiration of gastric contents into the lungs during anesthesia. 3-gastrointestinal preparation 3.a: Nasogastric Tube. Some clients may require a nasogastric tube to facilitate stomach decompression to prevent postoperative abdominal distension 3.b :Bowel Preparation. The surgeon prescribes the type of bowel preparation on the basis of the surgical procedure. Enemas and laxatives are not routinely administered unless the client is having abdominal surgery. 3.c: Urinary elimination .The client is instructed to void before receiving the preoperative medication or being transferred to the operation room . The bladder needs to be empty to prevent distension and incontinence during the surgery .the nurse usually inserts a Foley catheter before or during surgery. 4-safety precautions: clients are instructed to leave their jewelry at home and to avoid the use of makeup the day of surgery for safety reasons. Jewelry and other metal objects can cause burns when electrocautery is used during surgery. Rings can compromise circulation. Hair pins can injure the scalp when the head is positioned for anesthesia. Makeup and nail polish can interfere with the practitioner’s assessment of oxygenation. Unnecessary prosthetic devices (ex. eye glass) should also be left at home to prevent client injury or loss 5 INTRAOPERATIVE PHASE Functions of operating team 1-Surgeon: • Responsible for determining the preoperative diagnosis. • The choice and execution of the surgical procedure. • Explanation of the risks and benefits, obtaining inform consent • Postoperative management of the patient’s care. 2-Circulating nurse o Manage the operating room o Protect the safety and health needs of the patient o Ensuring cleanliness, proper temperature, humidity lighting, safety of equipment, availability of supplies and materials o Coordinate the activities other personnel e.g. X-ray o Monitor aseptic practice 3-Scrub activities Scrubbing of the operation room Setting up the sterile table, preparing sutures and special equipment Assisting the surgeon and the surgical assistance Keeping the time the patient is under anesthesia Check all equipments used in operation are accounted Send specimens to lab 4 Anesthetists and Anesthesiologist: • Anesthetist: Person who has been trained to administer anesthetic. Example: Nurse Anesthetist • Anesthesiologist: The doctor responsible for inducing anesthesia, maintaining anesthesia at the required levels and managing untoward reactions of anesthesia, throughout the operation. 1. The sterile team: a. Operating surgeon b. Assistants to the surgeon c. Scrub nurse or surgical technologist Note: A surgical technologist may act as a scrub technician or as a circulator. 2. The unsterile team: a. Anesthesiologist or anesthetist b. Circulating nurse c. Others: Medical orderly example radiology technician 6 Types of anesthesia 1-General anesthesia: Total unconscious state, placement of a tube into the trachea 2-Local anesthesia a) Local anesthesia Administered topically or Infiltration anesthesia is the injection of a solution containing the local anesthetic into the tissues at the planned incision site b) Epidural block Local anesthetic injected into the extradural space near the spinal cord, anesthetizing several spinal nerves at once c) Spinal anesthesia Local anesthetic injected into the subarachnoid space of the lumbar area (usually L4 or L5), which contains cerebrospinal fluid . Used for surgery involving the abdomen, perineum, and lower extremities d) Major/minor nerve block (with and without sedation) Temporary loss of feeling or movement of a specific limb or area As general nursing care in intraoperative phase 1-Surgical Asepsis Surgical asepsis is used to decrease the client’s risk for an infection. Surgical asepsis refers to hand washing, wearing surgical attire, handling sterile instruments and equipment, and establishing and maintaining sterile fields. 2-Skin Preparation nurse should provide the client with an explanation of the procedure, privacy, comfort, and safety. Common agents for prepping the skin include povidone-iodine, chlorhexidine, alcohol, and hexachlorophene. 3-Positioning and Draping Proper positioning ensures client comfort and safety, preserves vascular supply, and prevents neuromuscular damage to tissue; the same time, positioning also provides access to the surgical site, airway, intravenous lines, and all monitoring devices. Prevent all sharp surfaces in contact with the client’s skin and Bony prominences (e.g., sacrum, elbows, and heels). 4-Electrical Hazards During surgery the client can be exposed to an electrical surgical generator (electrocautery device to eliminate bleeding and reduce contamination). 7 5-Heat Loss Injury from hypothermia is prevented by measures implemented to minimize heat loss. During surgery, body heat is lost by positioning on a cold and administration of cold gases . Body temperature is maintained by applying warming mattresses or warmed blankets, warming and humidifying inhaled gases, warming irrigating and intravenous solutions, and increasing room temperature. 6-Monitoring Physiological Functioning Ventilation and circulation ECG and oxygen analyzer alterations Fluid intake, urinary output, and calculated blood loss Behavioral changes Body temperature Diagnostic testing (collection of specimens and cultures, x-rays, and fluoroscopy COMMONLY USED OPERATIVE PATIENT POSITIONS Supine position. Patient lies straight on back face upward. with arms at sides, legs extended parallel and uncrossed, feet slightly separated. Strap is placed above knees. Head is in line with spine. Note small pillow supporting feet to prevent foot drop. This position is commonly used in Laparotomy Recumbent position. Patient lies on back with arms at sides. Knees are slightly flexed with a small pillow under each. Thighs are externally rotated. This position is commonly used in exploration of groin. lvmphnode, blood vessel. femoral hernia. inguinal hernia varicocele. 8 Trendelenburg’s position. Note the knees are over the lower break in the table, knees strap is above the knees and shoulder braces are in place. Commonly used in Pelvic Surgery (bladder, lower ureters, uterus, ovaries, prostate). Reverse Trendelenburg’s position. Patient lies on back. The foot board is padded and raised. The entire table is tilted so head is higher than feet. The strap is below the knees. Note the operative area is over the raised thyroid elevator on the table. This position is commonly used in the surgery of Thyroid. Head and Neck. Right kidney position. Patient is in a lateral position with kidney region over table break Note kidney strap across hip to stabilize body. raised kidney elevator for hvper extending operative area, and pillow between legs. Patient’s side is horizontal from shoulder to hip. Commonly used in surgery of Kidney and Suprarenal. Kraske position. Hips are over central break in table and knee strap is below the knees. Note chest rolls in place and pillow under feet. Commonly used in - Spinal surgery (Laminectomy) and Anal surgery. 9 Right lateral position. Note strap across hip and body rest to stabilize body. Pillow between legs relieves pressure. Commonly used in Chest suroerv (Thoracotomy) Prone position. Patient lies on abdomen. Note chest rolls under axillae and sides of chest to iliac crests raise body weight from the chest to facilitate respiration. and pillow under feet to protects toes. Patient is anesthetized in supine position before being turned into prone position, This position is common used in the surgery of Pilonidal sinus. Lipoma of back. Bed sore. Lithotomy position. Patient is on back with foot section of table lowered to a right angle with body on the table. Knees are flexed and legs are on inside of metal posts with feet supported by canvas straps. Note that buttocks are even with the table edge. Commonly used in Anal surgery, Gyraecological surgery, Urological surgery, Endoscopy of urinary & Reproductive system 10 GUIDELINES FOR NURSING ACTIONS IN POSITIONING ALL PATIENTS 1. To prevent damage to the brachial plexus, arms are never abducted beyond 90 0. 2. Legs must not be crossed as this creates pressure on blood vessels and nerves. 3. Body surfaces should not be in contact with one another. 4. Hands and feet should be protected and not allowed to hang off the table. 5. The patient should not be touching any metal part of the table. If the elbow rests on the table edge, ulnar nerve damage may occur. 6. Patient exposure is limited to the area required for the surgical procedure. 7. If the patient is conscious, all activities as well as the rationale should be explained. 8. The instrument table, the mayo stand, or other equipment should not be in contact with the patient’s toes or legs. 9. During the surgical procedure, if the mayo stand, the instrument table or operating table is moved, the patient must be checked for pressure points. 10. Movement of the anesthetized patient is done gently and slowly. Turning the patient too quickly may cause circulatory depression. 11. To ensure the patient’s safety, adequate numbers of personnel must always be present when positioning the patient. The patient is lifted into position, never pushed or pulled. 12. When moving an anesthetized patient, the anesthesiologist guards the endotracheal tube and protects the patient’s head and neck. 13. The position must not obstruct any catheters, tubes or drains. 14. Team members must be reminded not to lean on the patient. 15. If the surgical procedure is on an extremity, such as an amputation, both extremities should be exposed for comparison. 16. The patient, position is documented as part of the intraoperative notes. POST ANESTHESIA care The immediate postanesthetic period is critical. The patient must be observed very closely and must receive intensive physical and psychological support until the major effects of the anesthetic have worn off and the overall condition of the client becomes stable. The nurse is largely responsible for the care of the patient at this time. 11 POST ANESTHESIA ASSESSMENT Airway Patency, presence/adequacy of artificial airway Respiratory rate, depth, character Heart rate (Pulse, pulse oximeter or cardiac monitor) Blood Pressure (Cuff or arterial line) Temperature Ability to follow commands, sensation and ability to move Level of Consciousness extremities following regional anesthesia Vital signs Patient position Tissue oxygenation Dressing/ Suture line Fluid lines/ tubes Position to facilitate breathing, to prevent position pressure on body parts or invasive lines and to promote comfort Skin: color, temperature, moisture Nail beds: color, capillary refill Lips/Oral mucosa: color Pulse oximetry Peripheral pulses: presence, strength Dressings: Dry or minimal drainage Suture line (if visible): color, approximation of wound edges Intravenous fluids: rate, amount in bottle/bag, infusion site Other lines (examples: CVP line, Arterial line): patency, connection Drainage tubes: patency, connection, character and amount of drainage Discharge from the Recovery Room Criteria for Discharge of Patients from the Recovery Room: 1. Vital signs are stable and indicate normal respiratory and circulatory function. 2. Patient is awake or easily aroused and can call for assistance, if needed. 3. Postsurgical complications have been thoroughly evaluated and are under control. 4. After regional anesthesia, motor and partial sensory functions have returned to all anesthetized area 12 Transfer of the Patient to the Clinical Unit/Ward Two ward nurses usually collect the patient from the Operating Room. A report is given by the Recovery Room Nurse about the surgery and condition of the patient. The patient’s chart is also handed over. The patient’s room is prepared to facilitate patient transfer and monitoring. Most surgeons discuss the result of the surgery with the family immediately after surgery and also visit the patient to describe the findings and to provide reassurance. COMMON POSTOPERATIVE DISCOMFORTS 1. Nausea and vomiting 2. Thirst 3. Constipation and gas cramps!abdominal distention. 4. Pain 5. Hiccups 6. Restlessness COMMON POSTOPERATIVE COMPLICATIONS IN THE CLINICAL UNIT COMMON CAUSE OCCURRENCE MANIFESTATIONS A-EARLY COMPLICATIONS 1-Abdominal Distension Surgical manipulation of bowel; swallowed air Within 48 hours Increased abdominal girth, tympanic percussion, complaint of “gas pains” or “fullness” Within 48 hours Fever, increased pulse and respirations, dyspnea, cyanosis Within 48 hours Same as atelectasis; bloody sputum 2-Atelectasis Mucus, shallow respirations 3-Hypostatic Pneumonia Shallow respirations 13 4-Hypoxia Respiratory depression, mucus, pain, poor positioning Within 48 hours Increased blood pressure, bounding pulse, restlessness, difficult breathing Most common immediately postop but may occur anytime. Drop in blood pressure, bounding pulse, clammy skin, decreased urine output, restlessness, lethargy, marked increase in temperature. 6 - 8 hours postop Inability to void, Positioning restlessness, bladder distention Within 48 hours Same as in shock; profuse restlessness, bladder distention. 5-Shock Loss of fluids and electrolytes trauma, medications sepsis 6-Urinary Retention Medication, local edema, 7-Wound hemorrhage Slipped suture, dislodged clot wound evisceration 2-Later complication 1-Thrombophiebitis Variable Skin warm to touch, red, Venos stasis, IV irritation 2-Wound Infection tender; fever; calf pain with dorsiflexion firmness 3 - 6 days postop Skin warm to touch, red, tender; fever; chills; malaise; purulent drainage 6-8 days postop Separation of wound edges; sudden profuse sudden strain pink drainage 6 - 8 days postop Dehiscence with protrusion of abdominal viscera through incision Poor aseptic technique 3-Wound dehiscence Old age and malnutrition 4-Wound Evisceration Same as in wound dehiscence 14 Postoperative Care 1-Respiratory function is maintained. Monitor respiratory rate and characteristics. Auscultate lung sounds once a shift or more often if indicated. Help client turn and deep breathe every 1 to 2 hours. Reinforce use of incentive spirometer. Show client how to splint incision before coughing Assess client’s ability to mobilize secretions; suction if necessary. Administer oxygen as ordered. Refrain from administering narcotic analgesics if respiratory rate is less than 12 breaths/minute. Encourage early ambulation. 2-Circulatory function is maintained Assess vital signs and monitor laboratory values. Ensure that IV fluids are infusing at the prescribed rate and site is patent. Monitor postoperative intake and output for at least 48 hours or until all drains and tubes have been removed, client is tolerating oral intake, and urine output is normal. Report in intake and output, hypotension, dizziness, palpitations, or abnormal laboratory values. Keep head of bed flat unless contraindicated. Assess surgical site for excessive external bleeding. Reinforce dressing or apply pressure if bleeding is frank. Monitor for internal bleeding: peri-incisional hematoma and swelling, abdominal distention if abdominal surgery was performed, 3-Pain and discomfort are recognized and effectively treated pain Assess pain level using an established scale (visual or numerical). Determine source of pain (e.g., incision, body position, flatus, IV lines or drainage tubes, distended bladder). Provide pain medication and evaluate effectiveness 30 minutes after administration. Reposition client to improve comfort. Teach client non pharmacologic methods of pain relief: breathing exercises, relaxation techniques, and distraction 15 4-Altered Comfort Encourage client to breathe deeply to help eliminate inhaled anesthetics. Help client sit up and turn head to one side while vomiting to avoid aspiration. Record intake and output. Administer antiemetics as ordered. Provide mouth care and fresh linens after vomiting. Monitor intake and output and assess for signs or symptoms of dehydration or electrolyte imbalance 5-Self-care and mobility encouraged Encourage progressive activity. Help client dangle legs over bedside the evening of surgery or the next morning, if allowed, followed by sitting out of bed for 15 minutes (or more if tolerated). Progress to ambulation in room and hall way. Collaborate with client in establishing goals to increase ambulation. Help client with hygiene the evening of surgery; encourage increased self-care as appropriate. Schedule regular rest periods 6-Promoted of wound healing Inspect surgical site and peri-incisional drain sites for signs or symptoms of infection (redness, warmth, tenderness, separation of wound edges, purulent drainage). Wash hands before and after dressing changes; follow aseptic or sterile technique. Use skin barrier to protect skin and wound from irritating drainage. Avoid using excessive tape. Keep drainage tube exit sites clean. Prevent excess tension on drainage tubes by securing tubes to dressing. Empty collection devices frequently to promote drainage; note characteristics of drainage. Teach client to splint wound when coughing or changing position. 16 7-Complication potential is continuously assessed, and any complications are immediately and effectively treated. 7.a- Deep Vein Thrombosis Reinforce need to perform leg exercises every hour while awake. Instruct client not to cross legs or prop pillow under knees. Apply compression and antiembolic stockings as ordered. Ambulate or encourage client to ambulate for a few minutes each hour while awake. Help client avoid prolonged sitting and poorly fitting, constrictive antiembolic hose. Do not massage calves or thighs. Administer anticoagulant medication as ordered; monitor laboratory values for therapeutic levels. 7. b- Acute Urinary Retention Assess for bladder distention, discomfort, and urge to void. Encourage client to try to void within the first 4 hours after surgery. Assess volume of first voided urine to determine adequacy of output (voiding frequent, small amounts indicates retention of urine with elimination of overflow only). If client cannot void within 8 hours of surgery, consult with physician regarding instituting intermittent catheterization until voluntary voiding returns 7. c- Paralytic Ileus (no bowel sound) Assess bowel sounds every shift or more often if indicated. Assess returning bowel function as evidenced by passage of flatus or stool. Maintain NPO status until bowel sounds return. Report large amounts of emesis (more than 300 mL). Provide client with moistened gauze to wet lips and tongue until oral intake is allowed. Assist with passage of nasogastric tube, if ordered 17