File - Kathy Bowers Nurse Educator Portfolio
advertisement

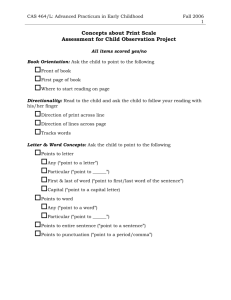
Running head: SCHOLARLY PRACTICUM SYNTHESIS Scholarly Practicum Synthesis: High-Fidelity Simulation Teaching Kathy Bowers Ferris State University 1 SCHOLARLY PRACTICUM SYNTHESIS 2 Abstract Orienting in a nurse educator role is a demanding and rewarding process to pursue. Working with an experienced mentor, and using the National League of Nursing’s (NLN) core competencies for reference are beneficial for guiding novice nursing educators through the process. Utilizing the teaching-learning process new nursing educators may gain needed training in the skills and high-fidelity simulator laboratory. A duo project of developing a high-fidelity simulation scenario and a debriefing tool for educating students in the simulation laboratory was completed during this practicum experience. The clinical practicum has provided an opportunity to gain experience as a neophyte in the nursing faculty role. Keywords: nursing students, high-fidelity simulation, practicum nurse educator SCHOLARLY PRACTICUM SYNTHESIS 3 Scholarly Practicum Synthesis Nurses transitioning from an experienced clinical position to a novice educator role often find it a daunting experience. Understanding the role of nurse educator is crucial for long term success in a faculty position (Penn, Wilson, & Rosseter, 2008). The National League for Nursing (NLN) has developed eight core competencies to follow as a guide for nursing faculty (NLN, 2007). By employing the NLN’s core proficiencies into teaching practice, novice nursing educators can become competent in transitioning from beginner to an expert role. The purpose of this practicum was to offer a student teaching role in the skills/high-fidelity simulation laboratory at North Central Michigan College (NCMC). Utilization of Patricia Benner’s Novice to Expert theory was the basis of the learning experience (Benner, 2001). Also by applying Joanne Duffy’s Quality-Caring theoretical framework as an educational model, and working under the supervision of an experienced preceptor, provided me guidance through the student practicum experience (Duffy, 2009). This paper discusses the practicum experience at NCMC as well as challenges and issues related to the function of the role. The strategies and methods developed to address the concerns and challenges encountered throughout the practicum will be discussed. Also, a description and analysis in understanding practice and theory, a depiction of the clinical project, and evaluation of the practicum with data, is included in this paper. Practicum Experience Preparing to become a novice nurse educator, possessing strong clinical skills is significant but there is much more to being an effective nurse educator, than expert skills (Tartavoulle, Manning, & Fowler, 2011). SCHOLARLY PRACTICUM SYNTHESIS 4 When transitioning from staff nurse to nurse educator it could be assumed to be an effortless process but without formal training would be an unsuccessful enterprise (Cangelosi, Crocker, & Sorrell, 2009). Conversion to a faculty role, the novice nurse educator should become capable of identifying individual student learning styles and become familiar with their own teaching style and the outcome it has on learner growth and socialization (Pettigrew, Dienger, & King, 2011). In order to fulfill the practicum requirements for the Masters of Science Nursing (MSN) degree at Ferris State University (FSU), over 300 student teaching hours in the simulation/skills laboratory at North Central Michigan College (NCMC) was completed. With the guidance of an experienced mentor, I was able to meet my objective of fulfilling four of the NLN’s core competencies. To meet the objectives for my clinical practicum, implementing educational strategies that incorporated evidence-based practice, developing curriculum design, and providing experiences for students to develop critical thinking skills were utilized throughout the experience (NLN, 2007). Attached in Appendix A is a copy of the practicum planning guide. During the teaching practicum there were several challenges identified in the skills and highfidelity simulation laboratory. A few of the issues discovered were challenges in altering assignments in the clinical setting, student professionalism, and student procrastination. Lastly, another challenge that was identified was the lack of a formal debriefing tool used for postsimulation case experience. Issues, Concerns, Challenges with Strategies Flexibility in Clinical Assignments The first challenge encountered was changing clinical assignments. One clinical group of students was not allowed to go to an assigned clinical day at an extended care facility (ECF). Information was given to my preceptor Mary Miles that one of the nursing home rotations would SCHOLARLY PRACTICUM SYNTHESIS 5 not be able to accept students due to an upper respiratory virus among clients and workers. It was decided by the laboratory coordinator, clinical instructor, the dean of nursing, and my-self, to bring the students to the high fidelity simulation lab for eight hours so that they would not lose valuable clinical time. I was asked to develop two scenarios to be performed, and create charts for each patient, that would meet learning objectives and outcomes for second year students. The scenarios would be performed in the high-fidelity simulation laboratory on the student’s clinical rotation day, and I was given three days to prepare. This happened two consecutive weeks in a row and I was able to create separate scenarios each week for student learning and socialization. High-fidelity simulation has been proven to be an effective substitute for conventional clinical practice by way of higher test scores for students that participated in simulation practice (Gates, Parr, & Hughen, 2012). I found the high fidelity simulation to be beneficial learning for the students by gaining experience with physical assessment, medication administration, and critical decision making skills. It was significant to see how each student fell into their respective roles, and always an evolving leader emerged. We spent approximately twenty minutes debriefing by verbalizing thoughts and observations. However, there was no formal debriefing tool used so the students were asked to write their reflections in a journal. Used as a teaching tool, simulation promotes clinical skills, interpersonal relationships, and competencies in critical thinking, psychomotor, and affective learning skills (Dillon, Noble, & Kaplan, 2009). According to Yildirim & Ozkahraman (2011), the practice of nursing necessitates "creative, personalized solutions to unpredictable client circumstances'' (p. 176) and the needs of student were met by the objectives and outcomes despite the need to alter a clinical situation. The students were offered an alternative environment to practice critical events in an organized and safe area that facilitates student confidence (Decker, Sportsman, Puetz, & Billings, SCHOLARLY PRACTICUM SYNTHESIS 6 2008). In designing student simulation scenarios NLN’s Competency III-Use Assessment and Evaluation Strategies by providing timely feedback in debriefing, and Competency IVParticipate in Curriculum Design and Evaluation of Program Outcomes by developing scenarios for student learning were met (NLN, 2007). Student Professionalism The second challenge was a lack of student professionalism at the college during a clinical rotation day that was changed to a clinical simulation mock practice. The first week the ECF clinical instructor told the students they could wear street clothing in to the simulation lab practice. It was identified that some of the students were just a little too lackadaisical when dressed in jeans, sweatshirts, and hats. Many of the students did not come prepared and forgot to bring their stethoscopes, pen lights, and scissors. The following week, the students were asked to come in full uniform, prepared with the equipment they would need in a real clinical scenario. I noticed that when in uniform, the students seemed to act in a more professional manner. When in uniform the students role-played with a serious attitude, and there was less verbalizing over the patient. Nursing uniforms increase pride and confidence and in turn create enhanced performance in clinical practice by student nurses (Shaw & Timmons, 2010). The profession of nursing is immersed in tradition. It is essential for educators to act as role models and teach students to preserve a reverence for nursing history (Shaw & Timmons, 2010). The nursing department maintains the required student uniforms professional but modern, due to multi-generational and increased male gender in the student population. Therefore, it was decided by the nursing faculty and the lab coordinator that for future simulation scenarios students will be mandated to wear full uniform to the simulation lab. As role models for nursing students educators need to SCHOLARLY PRACTICUM SYNTHESIS 7 maintain a neat and professional appearance in the classroom as well as in the clinical areas. Nursing instructors wear dress attire with professional lab coats in the clinical sites. Student Procrastination Another issue that was discovered was student procrastination with practice time in the skills lab. Often, the students waited until the last minute or late on a Friday to come in to the lab for practicing skills. The students must sign in and out using name, date, and time, when utilizing the lab this helps the coordinator track student activity. Many of the students did not come to practice, prior to test out skill sessions. Procrastination is a common problem for college students and has been associated with fear of failure, poor study behavior, rejection from peers, and distress with test taking, while others use it as a motivational tool (Chow, 2011). Occasionally, procrastination can be a great motivator for those who use the last minute technique to inspire them into completing an assignment. Therefore, it is vital to recognize high risk students and assist them with interventions to prevent procrastination such as enhanced study habits, tutors, time management, and coping mechanisms for test taking (Chow, 2011). An email was sent to the clinical instructors with the names of students who were not coming in to practice skills before the testing out period. After talking with the skills lab coordinator to devise strategies, the students were offered extended lab hours. The lab was opened up one extra evening per week, to help those students who had work commitments and would benefit from expanded lab times. In addition, students were encouraged to come in with a partner to practice with so that they could assist each other with the competencies. The domains of learning include cognitive, psychomotor, and affective domains (Billings & Halstead, 2012). With advances in technology nurse educators are challenged to find new innovative methods of assessment and evaluation in each domain. Cognitive learning may be evaluated by electronic testing, while SCHOLARLY PRACTICUM SYNTHESIS 8 psychomotor can be evaluated through skills and simulation. Evaluation of affective domains identifies performance levels as each student develops and gains experience (Billings & Halstead, 2012). The lab coordinator preceptor decided to allow the students to videotape each other, which is usually reserved for test out, so that they could reflect on their performance. Students often overestimate their performance and there can be contradictions between student and educator over technical steps. Consequently, videotaping the student is an important teaching strategy for monitoring each sequence of the skill presentation (Watt, Rush & White, 2009). Since the lab coordinator is present and the clinical instructor is not in the lab for testing the video can be saved and watched by the clinical instructor at a later date. This gives the clinical instructor additional knowledge as to how their students are performing. In applying these strategies the NLN’s Competency II- Facilitate Learner Development and Socialization by nurturing cognitive, affective and psychomotor growth of the students was met (NLN, 2007). Application of Knowledge from Practice, Theory, and Research Teaching Transition During my practicum I was able to utilize my past nursing clinical experiences and expert skills to educate students in the skills and high-fidelity simulation laboratory. It was realized early on that being a clinical expert helps in the academic setting, conversely there was much more to learn as a novice educator. Therefore, with the guidance of an expert preceptor and using the NLN core competencies and nursing theoretical frameworks of Patricia Benner’s Novice to Expert and Joanne Duffy’s Quality Caring Theory the transition process began. Benner’s premise is that through the learning course the student goes through five stages of competency novice, advanced beginner, competent, proficient, and expert (Benner, 2001). As a SCHOLARLY PRACTICUM SYNTHESIS 9 novice the goal is to progress through these stages and with time and experience achieve expert skill as a nursing instructor. Skills Lab Teaching Being a novice at anything is always a difficult process. Thinking back to entering nursing school many years ago as a student, it was a frightening and intimidating experience. A novice is someone who has no experience in the circumstance that they are assuming (Stuart, 2008). Nursing skills are critical learning experiences that all nursing students must perform and pass in the skills laboratory before performing in the clinical setting (Billings & Halstead, 2012). Having previous experience with adjunct teaching, in the clinical hospital setting I would consider myself proficient in that position. However, this is my first time teaching in the skills laboratory and I would be considered an apprentice in this area of academia. Going in to the skills lab proved to be a smooth transition because of my strong personal clinical skills. However, knowing that some of my nursing skills were not up to par I reviewed the skills that students would be performing throughout the semester. During this practicum, teaching nursing students various clinical skills such as intravenous (IV) and foley catheter insertions, priming IV and intravenous piggy back (IVPB) tubing, tracheotomy care, suctioning, and administering medications by all routes, enabled me to foster learning. Also, a new diabetic skills station was taught by crafting an instruction module on insulin injections, insulin pumps, and insulin infusions. Handouts and skills check off sheets were provided for review before performing student test out. As preparation for graduating from the MSN program becomes closer there is some apprehension about being qualified to be a nurse educator. Learning and applying aspects of the NLN core competencies helps the novice educator advance through Benner’s five stages, gaining compulsory experience in the role of nurse educator. SCHOLARLY PRACTICUM SYNTHESIS 10 Simulation Lab Teaching By creating activities for student learning, it is essential to assign structured activities. Simulation laboratory teaching is an example of a structured teaching activity and takes an enormous amount of work to develop and complete (Billings & Halstead, 2012). In the highfidelity simulation lab, scenarios were developed and carried out educating students while in the role of lead educator. I performed in the role as the facilitator for the simulation case experiences and debriefing discussions. In structured activity the rationale, goals, and objectives need to be unambiguous and succinct for student learning (Billings & Halstead, 2012). Starting simulation instruction there are three basic steps that should be included with every scenario (Rose, Courey, Ball, Bowler, & Thompson, 2012). The first stage is a brief overview of the case presented to the students, to provide them the opportunity for preparation of the scenario. The second step is to carry out the intra- simulation of the actual scenario. This provides an opportunity for the students to perform the nursing process, and complete the interventions and outcomes outlined for the simulation. The final and most important phase is the debriefing reflection phase once the simulation is carried out with instructors present for questions and feedback (Rose, et. al, 2012) I have incorporated Duffy’s theory in my teaching philosophy with students in the simulation lab. Duffy’s Quality-Caring Theory Model is a middle range nursing theory that identifies the nursing role as a unique partner of the healthcare team (Peterson & Bredow, 2008). Caring and nurturing relationships are at the core of the nursing profession and caring for ones’ self, patients, families, colleagues, and community are the foundation of the theory (Duffy, 2009). I instructed the students on the importance of caring for themselves, balancing work with home life so that they do not experience burn out hastily in their practice. Equally, I try to instill SCHOLARLY PRACTICUM SYNTHESIS 11 that each patient is at the core of nursing care and that learning to become a patient advocate is a key element of the nursing profession. This theory of caring was also adapted into the simulation lab teaching as students carried out scenarios, they were encouraged to provide a caring atmosphere for the patient, family and the entire healthcare team (Duffy,2009). Duffy’s theory model consists of eight carative factors, including shared problemsolving, thoughtful reassurance, respect, encouraging behavior, and appreciation of distinctive meaning, healing environment, attachment needs, and basic human needs (Duffy, 2009). All aspects of the caring factors are essential for students to embrace and employ in their clinical nursing practice. Students should be able provide compassionate and individualized care to patients, families, and offer mutual respect to peers. Therefore, through introduction and application of this middle range theory students are encouraged to make the most of the eight carative factors throughout their clinical practice. Shared problem solving in the simulation lab helps students to become more confident in real life situations where they will be more prepared to recognize changes in a patient’s condition (Neill & Wotton, 2011). Description Analysis of Clinical Project High-Fidelity Simulation Scenario It was determined by my preceptor that there was a need for a diabetic ketoacidosis (DKA) simulation scenario for the college high-fidelity simulation laboratory. Therefore, I was asked to create the scenario as my project for this practicum. Originally, I had planned to create a debriefing tool for the project and frankly I had no idea where to start developing a simulation scenario. In creating the DKA scenario, the focus was on meeting the first NLN CompetencyFacilitate Learning and the fourth Competency- Participate in Curriculum Design and Evaluation of Program Outcomes (NLN, 2007). SCHOLARLY PRACTICUM SYNTHESIS 12 Description and Analysis High-fidelity patient simulation laboratories have been established to develop critical thinking skills and provide a safe environment for nursing student education (Wayne & Lotz, 2013). In order to begin the process, I felt it was important to have formal training on the highfidelity simulator from the manufacturer, the Laerdal Company, to be able to manage a project of this magnitude. By attending this eight hour class it helped me to understand the complexity of high-fidelity simulator operations and how to successfully connect the DKA scenario for the project. I also viewed several training videos on the high-fidelity simulator the first week of the practicum experience. The main focus for the first NLN competency was to help students develop critical thinking and analytical reasoning skills. The scenario had to be aimed at adapting to the curriculum of the college. In creating a scenario that was tailored to the student’s needs, the objectives needed to be uniform with the course syllabus (Durham & Alden, 2008). After I began writing the simulation scenario it was decided by the class room faculty, that I should make a duo learning simulation by incorporating a psychology component. Therefore, the course syllabus for NUR 150 Health Issues and Concepts and NUR 170 Holistic Health Concepts had to be reviewed to meet the expectation of mutually consistent goals and objectives for student learning. As the scenario began to take form, the situation was shaped into a patient with type 1 diabetes mellitus who had a previous below knee amputation (BKA). The patient lived alone, had been extremely depressed, and subsequently stopped taking life saving exogenous insulin in an attempt to end his life. Often, in chronic illnesses there may be an element of depression that goes undiagnosed by healthcare professionals (Katon, 2008). Therefore, I had to research depression in people with diabetes in order to provide evidence based nursing practice for the SCHOLARLY PRACTICUM SYNTHESIS 13 simulation scenario. The fact that this was a suicide attempt is not inclusive in the title of the scenario so it was expected that the students would be able to recognize through assessment, evaluation, and communication with the patient. It was planned that once the DKA simulation scenario case was completed there would be a two day simulation experience carried out by students. The simulation was carried out in two sessions with two rooms running simultaneously. The first simulation was from 8-10 a.m. and the second from 10-12p.m. with five students, each assigned a role. Therefore, 40 students performed the simulation case experience over a two day period. Once the scenario was completed the post simulation debriefing discussion was to be carried out and students were to complete a debriefing tool evaluation. Attached in Appendix B is a copy of the DKA simulation scenario. Evaluation of Project The college was not using a formal debriefing tool therefore I created a tool during the practicum experience to evaluate the simulation experience for my DKA case scenario. Therefore, with evaluation of teaching and learning in mind I focused on meeting the objective for the third NLN Competency-Use Assessment and Evaluation strategies (NLN, 2007). Debriefing is an integral part of the simulation experience because it evaluates student learning objectives and outcomes (Neill & Wotton, 2011). The method applied, consisted of gathering, analyzing, and summarizing (GAS) and was used to develop a meaningful discussion that allowed the students to identify and reflect on performance (Levine, DeMaria, Schwartz & Sims, 2013). It was crucial for student learning, that as the facilitator I used questions with cues to enhance critical reflection, and provided constructive feedback immediately after the simulation experience (Levine et al., 2013). The debriefing tool Appendix C, evaluates learning SCHOLARLY PRACTICUM SYNTHESIS 14 outcomes and collecting and interpreting the data from the debriefing tool provided feedback to faculty for improvements in the teaching-learning method for future semesters (Neill & Wotton, 2011). It was decided that student names were optional so that the students would not be intimidated in reporting truthfully and making comments on the evaluation tool. The student evaluations were extremely positive in reflecting that the simulation practice was a valuable method for teaching strategies and learning outcomes. For every evaluation the students scored a 1 or 2 either agree or strongly agree. None scored either a do not agree or not applicable on any of the questions in the debriefing tool in the student evaluations Appendix D. Many of the students verbalized during the debriefing discussion that they would have benefitted from having more simulation case experiences earlier in the semester. Several of the evaluations had written comments on them. The students also reported during the debriefing session, that they liked having assigned roles for the activity as it created less confusion about their respective responsibilities. Due to the request by students to have simulations earlier in the semester, to help them feel more confident in the clinical setting, it was decided that next year the college would have simulations started prior to ECF and hospital clinical rotations. Evaluation of Clinical Practicum There are several examples of evaluations of this clinical practicum. First, my preceptor offered verbal feedback and assessment of my teaching throughout the course of the practicum experience. I was given positive and constructive feedback in my teaching performance for the skills and simulation lab. Mary also provided me ongoing feedback as I developed the simulation scenario and the debriefing tool. This offered me the opportunity to improve on certain aspects of my teaching presentation. The mentor-student relationship should be based on open dialogue and respect in an ethical manner (Billings & Halstead, 2012). Mary was SCHOLARLY PRACTICUM SYNTHESIS 15 extremely open to my suggestions and guided me in a respectful approach throughout the scholarly practicum student teaching process. By continually meeting and reviewing the goals and objectives set up throughout the semester, Mary was able to help keep me on track in meeting those goals and objectives. In encountering each challenge she was able to help me brainstorm and develop strategies for resolving the issues almost immediately. Second, evaluation for my teaching performance by my preceptor and the students helped me to learn from my limitations and enhance growth and maturity in the role of nurse educator. Many nursing faculty are afraid of the new technology available in nursing education today and it takes skill to master it (Axley, 2008). Although I was intimidated in the beginning, by delving into learning and utilizing the simulator during my practicum experience allowed me to increase confidence and enhanced my ability to use the high-fidelity simulator. Evaluation of my performance in the simulation and skills laboratory will be provided in Appendix D and it offered me desired feedback for moving forward as a novice nurse educator. Last, self evaluation provides an opportunity to reflect on my own learning and subsequent growth through the process of teaching. Attached in Appendix F will be a self evaluation of my scholarly practicum teaching performance. I also maintained a journal that encompassed teaching in the skills/ high-fidelity simulation laboratory, development and performance of the DKA simulation case scenario, and development and performance of the debriefing tool discussion; from beginning to end. Conclusion The scholarly practicum experience afforded me the opportunity to explore the role of a nurse educator teaching 1st and 2nd year nursing students. I experienced some frustration and a number of issues during the process but learned strategies, with the help of my preceptor, to SCHOLARLY PRACTICUM SYNTHESIS 16 successfully meet my goals and objectives for learning. The evaluation process gave me the opportunity to improve my teaching skills as I move forward in pursuing further opportunities in a nursing faculty role. I found engaging with and teaching the students a beneficial and rewarding experience. I am also grateful for the chance to network and develop relationships with faculty in the academic arena. SCHOLARLY PRACTICUM SYNTHESIS 17 References Axley, L. (2008).The integration of technology in nursing curricula: Supporting faculty via the technology fellowship program. The Online Journal of Issues in Nursing, 13 (3) doi10.3912/OJIN.Vol13No03PPT01. Benner, P. (2001).From novice to expert: Excellence and power in clinical nursing practice. (Commemorative ed.). Upper Saddle River, NJ: Prentice Hall. Billings, D.M, & Halstead, J.S. (2012).Teaching in nursing: A guide for faculty. (4th ed.). St. Louis, MO: Elsevier. Cangelosi, P.R., Crocker, S., & Sorrell, J.M. (2009). Expert to novice: Clinicians learning new roles as clinical nurse educators. Nursing Education Perspectives, 30 (6), 367-371. Chow, H. (2011). Procrastination among undergraduate students: Effects of emotional intelligence, school life, self-evaluation, and self-efficacy. Alberta Journal of Educational Research, 57 (2) 234-240. Decker, S., Sportsman, S., Puetz, L., & Billings, L. (2008).The evolution of simulation and its contribution to competency. Journal of Continuing Education in Nursing, 39(12), 74-80. Dillon, P., Noble, K., & Kaplan, L.(2009).Simulation as a means to foster collaborative interdisciplinary education. Nursing Education Perspectives, 30 (2), 87-90. Duffy, J. (2009). Quality caring in nursing: Applying theory to clinical practice, education and leadership. New York, NY: Springer Publishing. Durham, C., & Alden, K.(2008).Enhancing patient safety in nursing education through patient simulation, Patient safety and quality and evidence-based handbook for nurses. Rockville, MD: AHRQ Publication. SCHOLARLY PRACTICUM SYNTHESIS 18 Gates, M., Parr, M., & Hughen, M.(2012).Enhancing nursing knowledge using high-fidelity simulation. Journal of Nursing Education, 51(1) 9-15. Katon, W.(2008).The co-morbidity of diabetes mellitus and depression.The American Journal of Medicine, 11(2), S8-S15. Levine, A., DeMaria, S., Schwartz, A., & Sims, A.(2013).The comprehensive textbook of healthcare simulation, Springer, NY: Library of Congress. National League for Nursing [NLN](2007).Nurse educator competencies: Creating an evidenced based practice for nurse educators, New York, NY. Neill, M., & Wotton, K.(2011).High fidelity simulation debriefing in nursing education: A literature review: Clinical Simulation in Nursing, 7(5), e168-e181. Penn, B., Wilson, L., & Rosseter, R.(2008).Transitioning from nursing practice to a teaching role.The Online Journal of Issues in Nursing 33(3).Retrieved from http:www.nursing world.org. Peterson, S. J., & Bredow, T. S. (2009). Middle range theories: Application to nursing research. Philadelphia, PA: Lippincott Williams & Wilkins. Pettigrew, A., Dienger, M., & King, M. (2011). Nursing students today: Who are they and what are their learning preferences? Journal of Professional Nursing, 27(4), 227-236. doi:10.1016/j.profnurs.2011.03.007. Rose, S., Courey, T., Ball, M., Bowler, C., & Thompson, Z. (2012). Bringing simulation to life through a therapeutic encounter: A pedagogical approach used for associate degree nursing students. Teaching and Learning in Nursing, 7 (1) 2-5. Shaw, K., & Timmons, S. (2010).Exploring how nursing uniforms influence self image and professional identity. Nursing Times, 106 (10) 21-23. SCHOLARLY PRACTICUM SYNTHESIS 19 Stuart, T.(2008).Examining the transition for new graduate professional RN RN Journal. Retrieved from: http://www.rnjournal.com/journal_of_nursing/newgraduate_professional_rn.htm. Tartavoulle, T., Manning, J., & Fowler, L.(2011). Smoothing the transition from bedside to classroom. American Nurse Today, 6 (5).Retrieved fromwww.americannursetoday.com/ article.aspx?id=7832&fid=7770 . Watt, W., Rush, K., & Wright, M. (2009).Evaluating first-year nursing students’ ability to self assess psychomotor skills using videotape Nursing Education Perspectives, 30(4), 214-19. Wayne, D., & Lotz, K. (2013).The simulated clinical environment as a platform for refining critical thinking in nursing students: A pilot program. Nursing Education Perspective, 34 (3), 163-166. Yildirim, B., & Ozkahraman, S. (2011).Critical thinking in nursing process and education. International Journal of Humanities and Social Science.1 (13), 176-185. SCHOLARLY PRACTICUM SYNTHESIS 20 Appendix A- Practicum Proposal Planning Guide Goals Goal 1: Gain development in the nurse educator advanced specialty role by utilizing NLN’s Competency 1Facilitate learning. Spring/2014 Objectives Activities Timeline/Complete by: 1.1 Identify and start to implement teaching and learning approaches in the skills/simulation lab for NCMC students January 2014 semester. 1.1a. Review nursing January 15th 2014 program mission and student handbook for the nursing program 1.1b Research teaching and February 1, 2014 learning strategies incorporating cognitive, psychomotor and affective domains. 1.1c Research innovative February 25, 2014 learning environments to develop critical thinking skills by utilizing role playing & simulation scenarios. 1.1d Complete and carry out critical thinking scenarios for each week of SIM class with debriefing sessions at the end of class each day. 1.1e Meet with preceptor January 15- May 6 during course of practicum for guidance and feedback SCHOLARLY PRACTICUM SYNTHESIS Goal 2 To meet core competency 2 Facilitate learner development and socialization. 2.1 Identify objectives to promote student learning. 2.2 Identify individual diverse student learning styles. Goal 3 To meet the competency of the third core competency of Use Assessment and Evaluation Strategies 3.1 Identify education module assessments, evaluation tools and debriefing philosophy and evaluation tool. 21 2.1a Encourage student participation and collaboration by role playing. 2.2b Create learning atmosphere conducive to socialization and reflection by using journaling. 3.1a Research literature on assessments and evaluation applications. 3.1b Provide constructive and timely feedback to students 3.1c Provide an evaluation tool for students and preceptor to evaluate my teaching. 3.1d Develop a debriefing evaluation tool for student’s simulation experience. March 5, 2014. March 12, 2014 March 25th, 2014 March 30, 2014. April 1-5, 2014 April 10,2014 SCHOLARLY PRACTICUM SYNTHESIS 22 Appendix B-DKA Simulation Scenario Burt McReynolds-Diabetic Ketoacidosis-BKA Burt McReynolds Age: 53 years Weight: 70.0 kg Base: Stan D. Ardman II Overview Synopsis The learner is caring for a 53 year old who is divorced and lives alone in an apartment on the second floor He has no insurance and has been seeing the local federally qualified health clinic for management of his Type 1 diabetes mellitus. He attempts to manage but has trouble remembering to monitor his blood sugar 4 times a day and admits to missing insulin doses at times. His neighbor had not seen Burt in a few days so he called Burt’s daughter who had a key to the apartment. Upon entering the apartment they found him lying on the floor unresponsive so EMS was called. When EMS arrived the blood sugar reading was 550 so they gave 12 units of regular insulin and transported to the emergency department of the local hospital. The SCE prepares the student for the following items of the NCLEX-RN test format: NCLEX_RN Test Plan: X Safe and Effective patient care X Management of patient care X Health promotion and maintenance of patient X Psychosocial integrity of patient X Physiological integrity of patient X Basic care and comfort of patient X Pharmacological therapies X Reduction of patient risk potential X Physiological adaptations of patient ______________________________________________________________________________ Background Patient History Past Medical History: Diagnosed with Type 1 diabetes mellitus at the age of 13, hyperlipidemia Past Surgical History: Right below knee amputation 2yrs ago Allergies: No known drug allergies Medications: Insulin glargine 40 units at bedtime, aspart insulin 1 unit for every 15gms carbs ac tid, aspart insulin per sliding scale before meals and at bedtime 0-12 units, Lipitor 20mg daily Code Status: Full code SCHOLARLY PRACTICUM SYNTHESIS 23 Social/Family History: Married at age 20. His wife helped him with a proper diet, exercise and blood glucose level monitoring. At age 50, his wife divorced him and he moved into an apartment and after his BKA went on full disability. He has been following up at the federally qualified health clinic for management of diabetes but has missed several appointments. ______________________________________________________________________________ Handoff Report The learner is to assess and stabilize patient for admission to the ICU The report should follow the SBAR format and include: Situation: The patient was found unconscious in his apartment with a blood sugar of 550. He has been living alone and after his wife divorced him he became depressed and has had trouble remembering to check blood sugars and take insulin. He has been going the federally qualified health clinic because he has no insurance, but has missed several appointments. His daughter states that he has not been eating well and that her father may have missed some insulin doses. She reports he has been very depressed and last time she visited he appeared to have poor hygiene but she could not get him to go to the doctor. She stated that he told her he “just did not want to live like this anymore.” ______________________________________________________________________________ Assessment Vital Signs: HR 120, BP 110/60, RR 30 and rapid with fruity smell, SpO2 98% on 3L NC, Temperature 37C General Appearance: Clothing is old, worn and does not fit well. Appears older than stated age Cardiovascular: Sinus rhythm Respiratory: Breath sounds clear GI: Normal bowel sounds GU: Incontinent of urine Extremities: Full range of motion in all four extremities Skin: Pale, cool, and poor turgor. Mucous membranes dry Neurological: Semi conscious pupils equal and reactive to light bilaterally Labs: Blood glucose 530 Fall Risk: High-risk for falls Pain: Moans with painful stimulation ______________________________________________________________________________ Initial Providers Orders: Start IV fluid 0.9NS @ 15mL/kg/hr for 2 hours, then run at 7.5/kg/hr. SCHOLARLY PRACTICUM SYNTHESIS 24 Start 2nd IV Humulin Regular Insulin infusion at 2units hr Give 20 units aspart (novolog) now x1. Monitor blood sugars q 15 mins and vital signs every 30mins. NPO Monitor I &O if no void in 6 hours, foley catheter insertion Neurological checks every 1 hr. Labs Chem. Panel, CBC, Phosphorus, serum ketones & ABG stat EKG and chest X-ray stat Transfer patient to ICU after IV infusion, subcutaneous insulin and labs and x-rays completed __________________________________________________________________________ Preparation Learning Objectives Student will demonstrate knowledge of the nursing process in planning and caring for patients with diabetes. Student will demonstrate knowledge of integrating evidence based practice research into clinical practice to provide safe care for patients with health alterations. Student will demonstrate use of appropriate technology to gather information regarding the patient’s disease process, and plan and document interventions. Student will demonstrate therapeutic communication skills through verbal and non-verbal means with patient and family. Student will demonstrate recognition of the distinction between moderate depression and major depression disorder This SCE addresses the following QSEN Competencies; X Patient-Centered Care X Team Work and Collaboration X Evidence-Based Practice SCHOLARLY PRACTICUM SYNTHESIS 25 Quality Improvement Safety Informatics EHR Learning Performance Measures Essential Performance Measures for the SCE: Reviews patient’s medical record Performs hand hygiene before and after patient contact Demonstrates appropriate use of personal protective equipment Introduces self to patient Verifies patient identity with two identifiers Conducts basic environmental safety assessment and maintains safety measures Uses therapeutic communication to establish rapport and reduce patient anxiety Provides developmentally appropriate education Evaluates effectiveness of education Documents all findings, interventions and patient responses Preparation Questions Describe the difference between type 1 and type 2 diabetes mellitus. Why is the recognition and treatment of acute changes in blood sugar levels important? Identify chronic complications of diabetes mellitus. What risk factors are associated with diabetes mellitus? Outline a teaching plan for a patient with type 1 diabetes mellitus. What is the cardinal rule of insulin administration? Why is it best to take blood sugar readings in pairs (before and after administration of insulin)? What laboratory values indicate a patient has diabetes mellitus? SCHOLARLY PRACTICUM SYNTHESIS 26 Why is a patient with diabetes mellitus at risk for developing neuropathies, macro-vascular and microvascular diseases? What is carbohydrate counting and why is it the preferred diet regimen for patients with diabetes? Why is depression a psychological component in diabetes? What is the role of the nurse for a patient with suicidal ideation or attempt? ______________________________________________________________________________ Equipment & Supplies Medication Supplies Alcohol wipes Distilled water 10mL vials (2) labeled Aspart insulin Human insulin regular Miscellaneous Patient chart with appropriate forms and order sheets Patient identification band Stethoscope BP cuff adapted for use with simulator Non-sterile gloves (1 box) Sharps container Audio and video recording devices Glucometer Glucometer test strips Jar of cotton balls Jar of tongue depressors Flash light SCHOLARLY PRACTICUM SYNTHESIS 27 Notes Facilitator Notes This SCE was created with the patient Burt McReynolds and only this patient can be used. The physiological values documented indicate appropriate and timely interventions. Differences will be encountered when care is not appropriate or timely. The facilitator should not click "Run" until ready to start the SCE. Students should perform an appropriate physical exam. The facilitator or patient should verbalize the physical findings the students are seeking but not enabled by the simulator (such as pain on palpation). The facilitator should use the microphone and/or preprogrammed vocal or audio sounds to respond to the learners' questions, if present on your simulator. ______________________________________________________________________________ Where appropriate, do not provide information unless specifically asked by the student. In addition, ancillary results (e.g., ECG, chest x-ray, labs) should not be provided until the students request them. For the patient: Dress the simulator in tattered, worn, ill-fitting clothing appropriate for the weather Place the simulator in a laying position Simulation personnel should role- play the following: Transferring nurse Make up a patient chart with the appropriate written order forms, medical administration record, diagnostic results, etc. for students to use. The chart should include the patient identification information. Begin the simulation with a transferring nurse (simulation personnel) offering verbal handoff using SBAR. Have the student’s role-play inter-professional communication with simulation personnel role playing back communication for the simulator. Highlight the importance of data organization and comprehensiveness when communicating. Debriefing and reflection after the scenario are crucial. When possible view a video of the scenario afterward for instructional and debriefing purposes. ______________________________________________________________________________ Debriefing Points The facilitator will begin by introducing the process of debriefing: Introduction: Discuss faculty role as a facilitator, expectations, confidentiality, safe-environment. Personal Reactions: Allow student to display emotions, explore student's reactions Discussion of Events: Analyze events of the SCE, using video tape if available Summary: Appraise what went well and what did not, identify areas for improvement and evaluate the experience using a debriefing tool Questions to be asked during debriefing: What was the practice experience like for you? What occurred and why? What action took place and was it valuable? SCHOLARLY PRACTICUM SYNTHESIS Teaching Q & A What is the rule of insulin administration? How would the nurse assess the patient's willingness to learn? What is the patient's level of education? What is the patient’s socioeconomic and psychological level? What are the barriers to learning? What are the patient’s physical capabilities? How to identify community resources? What priorities should be included in this patient's discharge teaching? How to recognize the signs and symptoms and management of hypoglycemia and hyperglycemia? When should nurse contact healthcare provider? How to monitor blood glucose levels? Proper administration of medications using 5 rights What are sick day guidelines? What possible referrals would be ordered for this patient? Social services Dietitian Diabetic nurse educator Local community resources Community case nurse manager 28 SCHOLARLY PRACTICUM SYNTHESIS 29 References Butler, M. K., Kaiser, M., Johnson, J., Besse, J., & Horswell, R. (2010).Diabetes mellitus disease management in a safety net hospital system: Translating evidence into practice. Population Health Management, 13(6), 319-324. doi:10.1089/pop.2009.0078 DeFronzo, R. A., Stonehouse, A. H., Han, J., & Wintle, M. E. (2010).Relationship of baseline HbA1cand efficacy of current glucose-lowering therapies: A meta-analysis of randomized clinical trials. Diabetic Medicine, 27(3), 309-317. doi:10.1111/j.14645491.2010.02941.x Edelman, C.L., & Mandle, C.L.(2010). Health promotion throughout the life span (7th ed.). St. Louis, MO: Mosby Elsevier. Forehand, M. (2010).Bloom's taxonomy: Emerging perspectives on learning, teaching, and technology .Department of Educational Psychology and Instructional Technology, University of Georgia. Retrievedfromhttp://projects.coe.uga.edu/epltt/index.php?title=Bloom%27s_Taxonomy Giger, J.N., & Davidhizar, R.E. (2008) Transcultural nursing: Assessment and intervention (5th ed.). St.Louis, MO: Mosby Elsevier. Johnson-Russell, J. (2010).Facilitated debriefing In W.M. Nehring & F.R. Lashely (Eds.), High fidelity patient simulation in nursing education, pp. 369-385. Sudbury, MA: Jones and Bartlett. Lewis, S.L., Dirkse, S.R., Heitkemper, M.M., & Bucher, L. (2011).Medical-surgical nursing: Assessment and management of clinical problems (8th ed.). St. Louis, MO: Elsevier Mosby. SCHOLARLY PRACTICUM SYNTHESIS 30 Melnyk, B.M., & Fineout-Overholt, E.(2010). Evidence-based practice in nursing & healthcare: A guide to best practice (2nd ed.). Philadelphia, PA: Lippincott Williams & Wilkins National Council of State Boards of Nursing.(2010).2010 NCLEX-RN test plan. Retrieved from https://www.ncsbn.org/2010_NCLEX_RN_Testplan.pdf Quality and Safety Education for Nurses.(2011).Quality and safety competencies. Retrieved February 19, 2014, from http://www.qsen.org/competencies.php The Joint Commission.(2014).National patient safety goals. Retrieved February 19, 2014 from http://www.jointcommission.org/standards_information/npsgs.aspx SCHOLARLY PRACTICUM SYNTHESIS 31 Appendix C- Debriefing Tool: Simulation Case Experience (SCE) Date: ___________ Course: _________________ Instructor: ________________________ Name (Optional):______________ Please rate the statements below on the scale. Mark N/A if there is no experience. Do Not Agree Agree Strongly Not Applicable Agree The debriefing questions helped me to critically think 0 1 2 N/A I feel more confident in making decisions 0 1 2 N/A I gained better understanding of the pathophysiology of conditions in the SCE 0 1 2 N/A I feel I will be more prepared to recognize changes in my real patient’s condition 0 1 2 N/A I feel my assessment skills improved with the SCE 0 1 2 N/A I feel I have improved my medication administration skills 0 1 2 N/A I learned from my active role as well as observing peers throughout the SCE 0 1 2 N/A Debriefing and discussion with the team were valuable 0 1 2 N/A Performing the SCE helped me to better understand the classroom content 0 1 2 N/A SCHOLARLY PRACTICUM SYNTHESIS Appendix D- Student Evaluations 32 SCHOLARLY PRACTICUM SYNTHESIS 33 SCHOLARLY PRACTICUM SYNTHESIS 34 SCHOLARLY PRACTICUM SYNTHESIS 35 SCHOLARLY PRACTICUM SYNTHESIS 36 SCHOLARLY PRACTICUM SYNTHESIS 37 SCHOLARLY PRACTICUM SYNTHESIS 38 SCHOLARLY PRACTICUM SYNTHESIS 39 SCHOLARLY PRACTICUM SYNTHESIS 40 SCHOLARLY PRACTICUM SYNTHESIS 41 SCHOLARLY PRACTICUM SYNTHESIS 42 SCHOLARLY PRACTICUM SYNTHESIS Appendix E-Preceptor Evaluation 43 SCHOLARLY PRACTICUM SYNTHESIS 44 SCHOLARLY PRACTICUM SYNTHESIS 45 Appendix F-Self Evaluation Objectives Met Facilitates Learning: 1.Engages in teaching and learning strategies incorporating cognitive, psychomotor and affective domains in the skills lab 1a. Effective use of Critical thinking scenarios in Simulation Lab. Facilitates Socialization and Learner Development: 2. Encourage student participation and collaboration by engaging students in role play. 2a. Effectively uses journaling for reflective X Use Assessment and Evaluation Strategies: 3. Provides constructive and timely feedback to students. X Not Met Comments I was able to engage students in learning in various domains of learning. Stimulated critical thinking by questions and cues. X Carried out several simulation experiences for students engaging them in role-play for effective learning. Even though students used journaling I was not able to read them. I provided the students with real-time feedback and constructive communication. SCHOLARLY PRACTICUM SYNTHESIS Participates in Curriculum Design and Evaluation of Outcomes: 3. a. Provides a student and preceptor evaluation tool for assessment of teaching. 3. b. Develops a high-fidelity simulation scenario meeting the goals and objectives for NUR 150 & NUR 170 3. c. Develops a debriefing tool for evaluation of simulation teachinglearning experience successfully. X 46 Evaluations performed in the skills lab. I developed a DKA highfidelity simulation scenario and a debriefing tool for evaluation. I completed over 300 hours of student teaching at NCMC from January-May.2014. I feel I have grown from this experience and had the pleasure of working with a wonderful group of students and faculty at NCMC. This experience will help me in my future aspiration of becoming a full time faculty nurse educator. Kathy Bowers SCHOLARLY PRACTICUM SYNTHESIS 47 Bibliography Butler, M. K., Kaiser, M., Johnson, J., Besse, J., & Horswell, R. (2010).Diabetes mellitus disease management in a safety net hospital system: Translating evidence into practice. Population Health Management, 13(6), 319-324. doi:10.1089/pop.2009.0078 DeFronzo, R. A., Stonehouse, A. H., Han, J., & Wintle, M. E. (2010).Relationship of baseline HbA1cand efficacy of current glucose-lowering therapies: A meta-analysis of randomized clinical trials. Diabetic Medicine, 27(3), 309-317. doi:10.1111/j.14645491.2010.02941.x Edelman, C.L., & Mandle, C.L.(2010). Health promotion throughout the life span (7th ed.). St. Louis, MO: Mosby Elsevier. Forehand, M. (2010).Bloom's taxonomy: Emerging perspectives on learning, teaching, and technology .Department of Educational Psychology and Instructional Technology, University of Georgia. Retrievedfromhttp://projects.coe.uga.edu/epltt/index.php?title=Bloom%27s_Taxonomy Giger, J.N., & Davidhizar, R.E. (2008) Transcultural nursing: Assessment and intervention (5th ed.). St.Louis, MO: Mosby Elsevier. Guillaume, A. (2011).Developing high-fidelity health care simulation scenarios: A guide for educators and professionals. Journal of Simulation and Gaming, 42 (1), 9-26. Neill, M., &Wotton, K.(2011). High fidelity simulation debriefing in nursing education: A literature review. Clinical Simulation in Nursing, 7 (5), e168-e181. Pettigrew, A., Dienger, M., & King, M. (2011). Nursing students today: Who are they and what are their learning preferences? Journal of Professional Nursing, 27(4), 227-236. doi:10.1016/j.profnurs.2011.03.007. SCHOLARLY PRACTICUM SYNTHESIS 48 Quality and Safety Education for Nurses.(2011).Quality and safety competencies, Retrieved February19, 2014 from http://www.qsen.org/competencies.php. Su, W., & Osisek, P.(2011). The revised Bloom’s Taxonomy: Implications for educating nurses. Journal of Continuing Education for Nurses,42(7) 321-7. doi:10.3928/0022012420110621- 05. The Joint Commission.(2014).National patient safety goal, Retrieved February 19, 2014 from http://www.jointcommission.org/standards_information/npsgs.aspx.