Renal Chart Note
advertisement

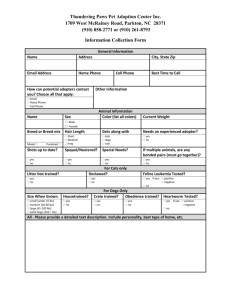
Nutrition First Office Call Client Name: HD DOB: XX/XX/XXXX Age: 70 Appointment length: 60 minutes Client History Reason for visit/HPI: referred by nephrologist for help implementing a renal diet PMH: ESRD, hemodialysis 3 times/week. Type 2 diabetes, dx 10+ years ago. Family Med Hx: not assessed Environmental and Medication Allergies: NKA Tobacco / Drug use: quit smoking 5 years ago. No drug use. RX/OTC: atenolol, EPO, mirilax, sertraline, ferrlecit, lantus basal insulin, nephrocaps, zemplar, tums Physical activity: not assessed Social Hx: Lives alone, daughter lives nearby. Daughter takes pt to dialysis appointments or takes Access Ride. Mostly homebound. Fixed income. Food and Nutrition History 24 hour recall/ Typical day or Nutrition Intake Analysis Results - ESHA: B: Often skips as he sleeps late and doesn’t have much of an appetite. Drinks 1 cup of coffee with 2 tbsp half and half when wakes up. S (11 am): 8 ounces orange juice and 2 slices toast with butter, handful M&M’s. L (1:00 pm): 2 cups canned tomato soup, 12 saltine crackers, 1 ounce sliced cedar cheese, 8 ounces 2% milk. D (8 pm): Hungry man TV dinner, 12 ounces iced tea. S (10 pm): 1 cup chocolate ice cream NIA: Fluid: 61 fluid ounces = 190% of rec 32 fluid ounces/day Sodium: 4576 mg = 229% of rec 2000 mg/day recommend Potassium: 3950 mg = 132-198% of rec 2-3 grams/day Food and Nutrition History: having trouble with dietary changes, previously attended a class on renal diets. Does not adjust well to new and unfamiliar foods. Dietary preferences: canned and frozen foods, likes tomato soup and Salasbury steak Hungry man dinner Food allergies / intolerances: NKA ETOH: none Weight History: Weight 1 year ago- 170 lbs (77.3 kg), weight 3 months ago- 159 lbs (72.3 kg) Meals away from home: none Restaurant Type: not assessed Who prepares food: pt or sometimes daughter. Where shops for food: Grocery Outlet, Safeway. Daughter does grocery shopping. Other nutrition notes: doesn’t like the taste of tums, often forgets to take with meals. No energy to cook, prepares to heat foods up. Has dentures that fit loosely. Physical Findings GI Function: chronic constipation, BM every 2-3 days. Doesn’t bother pt. Sleep hx: sleeps on dialysis, trouble sleeping at night, muscle cramps keep pt awake Energy level: fatigued, appears sleepy Stress level: not assessed Overall clinic observation: slow in movements and reaction time, swollen ankles (edmea). Biochemical Data (Pertinent Labs): Urine output = 240 mL BP = 143/92 mm/Hg, BUN=20 mg/dL, Creatinine=2.8 mg/dL, WNL HbA1C=7.2%, Albumin=3.0 mg/dL, Na+=126 mEq/L, PO4=7.2 mg/dL, HCT=36%, HGB=12.2 g/dL, TIBC=455 mcg/dL, Transferrin=366 mg/dL, Total Cholesterol=190 mg/dL, WNL FBS=140 mg/dL, WNL K+=6.4 mEq/L, Serum calcium = 8.1 mg/dL, Ferritin-21 ng/mL, Triglycerides=244 mg/dL, Anthropometrics Height: 70’’, 178 cm Dry Weight: 153 lbs, 69.5 kg Weight before last dialysis session: 165 lbs (75 kg) Weight after last dialysis session: 160 lbs (72.7 kg) BMI: 22 Ideal weight: 166 lbs (75.5 kg) IBW Range: 149-183 lbs (67.7-83.1 kg) %ideal weight: 153 lbs/166 lbs= 92% Usual weight: 159 lbs (72.3 kg) %usual weight: 160/159= 101% % Wt change: ((159 lbs-153 lbs )/153 lbs) x 100 = 4% Weight change classification: not significant Weight change between dialysis sessions: 165 lbs/153 lbs = 108%, gained 8%, Desired weight: 153 lbs (69.5 kg) Estimated Needs / Nutrition Prescription REE/Kcal: 35-40 kcal/kg IBW= 35-40 x 69.5 = 2433-2780 kcal Protein: 1.2 g/kg= 1.2 x 69.5kg = 84 grams Fluids (ml/kg): 240 ml = 1 cup (urine output) 3 cups + 1 cup = 4 cups 4 cups x 8 fluid ounces/cup = 32 fluid ounces/day Fiber (g/day): 25 g/day DRI Other: Potassium: 2000-3000 mg/day for ESRD/hemodialysis diet Sodium: 2000 mg/day for ESRD/hemodialysis diet Nutrition Diagnosis Problem: Excessive mineral intake (potassium) (NI-5.10.15) Etiology: difficulty implementing previous ESRD nutrition education due to forgetfulness Signs and Symptoms: 24 hour diet recall containing 132-198% of potassium recommended for ESRD/hemodialysis patient and a serum potassium level of 6.4 mEq/L (high). Problem: Excessive fluids intake (NI-3.2) Etiology: difficulty implementing previous ESRD nutrition education due to forgetfulness and limited willingness to change Signs and Symptoms: edema, 8% weight gain between dialysis visits, 24 hour diet recall indicating consumption of 190% of fluid recommendation for ESRD/hemodialysis patient and 229% of sodium recommendation for ESRD/hemodialysis patient. Nutrition Intervention and Professional Goals Intervention 1: Nutrition education content, survival information (E-1.3) Described the time sensitive relationship between high dietary potassium intake and the risk for cardiac arrest. Educated pt on the importance of choosing foods that are lower in potassium. Suggested alternatives to high potassium foods such as drinking cranberry juice instead of orange juice and decreasing servings of dairy to 1/day. Goals: on f/u in two days, to manage ESRD, pt’s food record will reflect a decrease in potassium to 2-3 grams/day, with the long term goal of decreased serum potassium levels. Intervention 2: Nutrition counseling, strategies, problem solving (E-2.4) Educated pt on the importance of decreasing sodium intake as means of helping to decrease thirst. Showed pt and pt’s daughter how to read labels in order to find low sodium options (700 mg of less per serving). Educated the pt on the importance of only drinking allotted amount of fluids. Talked to pt and pt’s daughter about what is considered a fluid and how to appropriately measure it. Discussed ways to help with thirst such as sucking on frozen grapes. As part of meal planning, brainstormed ways for pt to adhere to renal diet while still maintaining dietary preferences. For instance, incorporating low sodium saltines instead of the traditional ones. Goals: on f/u in two days, to manage ESRD, pt’s food recoded will reflect a decrease in fluid consumption to 32 ounces/day and sodium consumption of 2000 mg or less/day, with the long term goal of 4% weight gain or less between dialysis treatments and decreased edema. Follow up: Address DNIs and compliance with medications. Patient may benefit from changing TUMS to a different brand of phosphate binders. Address the need to increase protein to 84 grams/day and 2434-2800 kcal due to catabolic nature of disease state and slow decrease in weight over the past year. Ensure phosphorus and calcium levels are in balance. Address mechanical issues associated with poor dentition. Address diabetes comorbidity in meal planning. Explore exercise routine to support sleep, energy and muscle strength Handouts provided: High and low potassium foods, High and low sodium foods, fluid tracking sheet Materials provided: measuring cup Involvement in appointment: pt nods off during appointment, daughter attentive and involved