Immunity- an organisms cap a city to resist and combat infection
advertisement

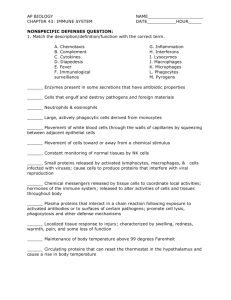
Unit 5-Chapter 37 Immunity Immunity- an organisms cap a city to resist and combat infection. Humans constantly come across a huge number of viruses, bacteria, fungi, parasitic worms and other pathogens However humans coevolved with many of these pathogens so you have defenses that protect you from them It is very important to be able to detect self from nonself All modern multi-cellular eukaryotes bear a set of receptors that collectively recognize around 1000 different nonself cures called pathogen- associated molecular patterns (PAMP’s) PAMP’s may include bacterial cell wall components, flagellum, pilus proteins, and double stranded RNA. PAMP is an antigen which means it helps recognize nonself molecules or cell components Binding of cell receptors to antigen trigger activation of a complements A compliment is a set of proteins that circulate through the body when activated they can destroy invading cells or mark them for uptake by phagocytic cells http://www.youtube.com/watch?v=z3M0vU3Dv8E Bozeman Immune System 2 types of immunity Innate immunity- fast general defenses against infection, pattern receptors and responses we are born with. Adaptive immunity- immune defenses to vast array of specific pathogens that an individual may encounter in their lifetime. Immunity is a 3 step defense system. 1st- physical, chemical, and mechanical barriers usually keep pathogens outside of the body. 2nd- Imnate immunity issues a general response after tissue is damaged or after antigen is detected. 3rd- adaptive immunity is initiated as leukocytes (WBC’s) divide to form huge populations that a specific antigen and destroy anything bearing it. Some of the WBC’s remain after the infection so if the same antigen returns these “memory cells” mount a secondary response. Surface barriers Your skin teems with about 200 different kinds of yeast protists and bacteria especially moist areas and cavities on a daily basis. These microorganisms called your normal flora are part of your first line of defense against negative invaders. HOWEVER! When these external Flora get inside they wreak havoc. Some common culprits include… Pneumonia, ulcers, colitis, whooping cough, meningitis, cancers o fcolon, stomach, intestines and more. Overuse of antibiotics has helped turn some of our natural flora against us. ORAL flora – There are about 400 species but causes dental plaque which is just a thick biofilm of bacterial and archae colonies. Problems arise – due to some of their extracellular products such as lactic acid → weakening connections between teeth and gums allow for pockets to form as we age. Bacteria accumulate and secrete destructive enzymes and acids, this is called Peridontis. → Worst yet a contributor to periodontist (also called periodontal disease) is a species called Pgingivitalis which is associated with a atherosclerotic plaque or coronary artery disease. SO TAKE CARE OF YOUR TEETH PEOPLE! Thinner barriers such as in the sinuses, mouth and urethra have their own way of dealing with intruders. Many secrete mucus containing lysozyme which may trap microorganisms and kill them. Others produce other enzymes low in pH which the organisms cannot withstand. Triggering innate defensesthese defenses do not change over the lifetime they are carried out by complements and phagocytic white blood cells. COMPLEMENTS There are about 30 different complement proteins circulating through the blood and interstitial fluid at all times, most are in activated. When they complement detects antibodies clustered on the surface of an antigen they initiate a series of reactions. C-3 is an extremely abundant complement which will coat an area marking it for destruction. Some complements can target pathogens even without an anti-body response. One such complement combined to six different pathogens yeast, HIV, flu, salmonella, strep, and leishmania. Normal body cells continually make protein that inactivate complements so they do not spread too far into healthy tissue. Phagocytic (WBC’s) leukocytes phagocytic leukocytes use chemotaxis to detect their target 3 main types include… Neutrophils, macrophages, dendritic cells INFLAMMATION and FEVER Inflammation is a fast multiple response which destroys active tissue and jump starts the healing process. Inflammation begins when cells degranulate into affected tissue in response to pattern receptor binding to an antigen. Fragments of see three complement trigger de granulation. Among the substances released by Degranulating leukocytes are prostaglandins as histamines. This causes nearby arterioles to widen, blood flow to the area increases, more phagocytes arrive attracted to cytokines. Phagocytes migrate out a blood vessel into interstitial fluid. Swelling and pain occur because prostaglandins and histamines widen the spaces between cells in capillary walls so they make capillaries in the affected tissue leakier to plasma proteins. This makes interstitial fluid hypertonic water follows by osmosis, tissue swells. Once these stimuli subside macrophages begin to produce compounds that suppress inflammation and promote tissue repair. Chronic inflammation is not a normal condition. file:///F:/Media/PowerPoint_Lectures/chapter37/videos_animations/inflamation_mhtml FEVER fever occurs in response to infection, cytokeines stimulate brain cells to release prostaglandins acting on the hypothalamus to raise bodies internal temperature. Fever enhances immune defenses by increasing the rate of enzyme activity, speeding up metabolism, tissue repair, and formation and activity of phagocytes. Pathogens multiply slower at high temperatures. Fever signifies the body is fighting something and should not be ignored HOWEVER brain damage or death can occur if core temperature reaches 107.6°F. Antigen receptors if innate immune mechanisms do not rid the body of invading pathogens and infection may become established. Innate immune responses are triggered by leukocytes that detect antigen by antigen receptors. Several antigen receptors exist plasma membrane proteins that recognize PAMPs are one type T cells they are another type called T cell receptors or TCRs for short. Another part recognizes certain proteins in the plasma membrane of body cells as being part of themselves these are called MHC markers. Antibodies are another type of antigen receptor. Antibodies are Y-shaped protein made only by B cells and can bind to an antigen. They activate complement and facilitate phagocytosis, neutralize toxic molecules, prevent pathogens from attaching to body cells. Antibody molecules consist of four polypeptide chains to light chains to heavy chains each chain has a theory of and constant region the variable region form 2 antigen binding sites which are antigen receptors. Each antibody having constant region that determines its structural identity or class, there are five antibody classes – IgG, IgA, IgE, IgM, and IgD – [IGE stands for immunoglobulin] most of antibodies circulating in the bloodstream and tissue fluids are IgG which bind pathogens, neutralize toxins, and activates complements. It is the only antibody that can cross the placenta to protect a fetus. IGA – is the main antibody in mucus and other exocrine gland secretions. IGE made by B cells is incorporated into plasma membrane of mast cells, Basophils, and some dendritic cells. It triggers the anchoring cell to release its granules. Humans can make billions of unique antigen receptors. Genes that code for the receptors do not occur in a continuous stretch one chromosome, they occur in several segments on different chromosomes. Several versions exist and segments are spliced together during B and T cell differentiation. This results in 2.5 billion different combinations of gene segments. Before a new be cell leaves the bone marrow is already making antigen receptors. In time that the cell has more than 100,000 antigen receptors they mature after encountering hormones in the thymus gland stimulating them to make T cell receptors. file:///F:/Media/PowerPoint_Lectures/chapter37/vide os_animations/antibody_diversityhtml ADAPTIVE IMMUNITY Lymphocytes and phagocytes interact to effect the 4 defining characteristics of adaptive immunity, which are self/nonself recognition, specificity, diversity, and memory. Self/nonself recognition- t cell recepotors have the ability to recognize self by MHC markers. TCRs, and other antigen receptors recognize nonself in the form of antigens Specificity- tailored to combat specific antigens. Diversity- antigen receptors on a bodys collection of B and T cells Memory- It takes about a week for B and T cells to respond in force the first time they encounter an antigen. Two Arms of Adaptive Immunity-The antibodymediated and cell-mediated immune response. Antibody-mediated immune response- Bcells produce antibodies targeting a specific invader. Cell-mediated immune response-targets intracellular pathogens where cytotoxic Tcells and NK cells detect and destroy infected body cells or cancers. Antigen Processing Both types of adaptive immunity are initiated by recognition of antigen by Tcell receptors. Intercepting and clearing out antigen Self notes went here The Antibody-Mediated Immune Response B cells are triggered to make antibodies specific to a particular pathogen or toxin in extracellular fluid. The secreted antibodies bind to the pathogen causing uptake by phagocytic WBCs, and keep pathogens from infecting other cells and neutralize toxins, and help eliminate both from body. http://www.cengage.com/biology/book_content/9781 111425692_starr_udl13e/animations/PowerPoint_Le ctures/chapter37/videos_animations/antibody_mediat ed_v2.html The Cell-Mediated Immune Response A cell mediated immune response involves the production of cytotoxic T cells and other lymphocytes that recodgnize specific intracellular pathogens. (does not involve antibodies) Cytotoxic Tcells kill ailing body cells that may be missed by an antibody-mediated response. These cells would display certain antigens, altered proteins and polypeptides. (responsible for transplant rejections) http://www.cengage.com/biology/book_content/9781 111425692_starr_udl13e/animations/PowerPoint_Le ctures/chapter37/videos_animations/cell_mediated.ht ml NK Cells Natural Killer cells will kill body cells that lack MHC markers or have altered markers. Cytokines secreted by helper T cells stimulate NK cell division. The new effector NK cells attack body cells tagged by antibodies for destruction. When Immunity Goes Wrong When Exposure to harmless substances stimulates an immune response than you have an allergy Allergens are often drugs, foods pollen, dust mites, fungal spores, poison ivy, venom from bees and other insects Some people are genetically predisposed to allergies, however infections, stress and changes in air and temp can also trigger reactions 1st exposure to allergens stimulates B cells to secrete IgE which anchors to mast cells and basophils Later, exposure causes antigens to bind to IgE the anchoring cells (mast cells and basophils) then degranulate and inflammation occurs Reactions can include swelling, itching, redness, and mucus formation Antihistamines relieve symptoms by acting on histamine receptors other meds can prevent degranulation A Balance of Immune Response is Really Important Immune defenses that kill pathogens can also kill body tissues So-C3 compliment is activated continuously to inhibit proteins that deactivate fragments or else compliment cascades would occur at all times. Anaphylactic Shock may occur if immune responses are too extreme and not kept in check o Shock occurs when cytokines and histamines are released in all parts of the body causing everything to swell including airways Severe asthma or septic shock may occur when too many neutrophils degranulate at once. o “cytokine storms”- when leukocytes release too many cytokines at the same time and widespread inflammation can result in organ failure (H5N1) flu is known for this Auto Immune Disorders Usually people do not make antibodies to molecules which occur on their own healthy body cells (normal MHC markers) BUT sometimes things go wrong Usually the Thymus “weeds out” defective T cell receptors if this mechanism fails mature lymphocytes that do not discriminate between self and non self are produced and these lymphocytes mount an Auto Immune Response. Examples: o Graves Disease occurs when antibodies bind to stimulatory receptors on thyroid gland causing excess production of thyroid hormone Quickens metabolic rate, uncontrollable weight loss, rapid irregular heart best, sleeplessness, mood swings, bulging eyes o Multiple Sclerosis- self reactive T cells attack myelin sheaths of axons Weakness and loss of balance paralysis and blindness Specific alleles on MHC markers, bacterial and viral infections are often underlying causes of autoimmune disorders Immune Deficiency Impaired immune function is dangerous and sometimes lethal Primary immune deficiencies present at Birth are the outcomes of mutations o Ex. SCID’s Secondary immune deficiency is caused by exposure to an outside agent usually a virus o Ex. Aids HIV and AIDS AIDS is a collection of disorders which results from infection with HIV virus that cripples the immune system. 33.3 million individuals have HIV it’s considered a pandemic. There is no cure for HIV → at first people appear to be in good health possibly fighting a cold or flu → eventually fever, enlarged lymph nodes, fatigue, and weight loss with night sweats occur. → Then yeast infections of the mouth, esophagus, and vagina often occur. Pneumonia, gastrointestinal inflammation and diarrhea appear. Colored lesions from Kaposi’s sarcoma erupt over the body. Other cancers are also common. HIV – is a retrovirus with a lipid envelope consisting of small pieces of plasma membrane. Proteins jut from the envelope, span it, and line its inner surface. Beneath the envelope viral proteins enclose two RNA strands and reverse transcriptase enzyme. When a retrovirus particle infects a cell, reverse transcriptase copies the viral RNA into DNA integrating it into the hosts cell’s DNA. Now the host begins to produce viral proteins. HIV mainly infects macrophages, dendritic cells, and helper T cells. Viral particles enter the body, dendritic cells engulf antigen to naïve T cells army of HIV neutralizing IgG antibodies and HIV specific cytotoxic T cells form. HIV and AIDS The initial response rids the body of most-but not all- of the virus HIV infects a few helper Tcells in a few lymph nodes Years or even decades-the level of HIV remains low Patients are contagious at this stage, though symptoms are not apparent Eventually-level of virus-neutralizing IgG plummets, production of Tcells slows Adaptive immune system becomes less and less effective at fighting the virus Transmission-mostly by unprotected sex with an infected partner o Infected mothers may pass virus during pregnancy, labor, delivery or breast feeding o Contact with blood Ex. Iv drug users, hospital patients in less developed nations and blood transfusion Testing done through blood, saliva or urine Treatments-No cure-but slow the progression. Drugs target retroviral replication Historyo HIV-1 evolved to infect humans from a SIV (simian immune deficiency virus) that effects chimpanzees in west central Africa o Earliest known evidence was blood from a man in 1959 and a lymph node removed from a woman in 1960 (in west central Africa) o The gene sequences were a little different suggesting the virus had been around for a while and had mutated o Mutation rates of HIV suggest that it may have been around since the early 1900s Vaccines Immunization-process designed to induce immunity o Active immunization is preparation that contains antigen ( a vaccine ) 1st immunization elicits a primary immune response 2nd booster elicits a secondary immune response for enhanced immunity o Passive immunization-made from antibodies purified from another persons blood Has an immediate benefit when exposed to potentially lethal agents Ex. Tetanus, rabies, Ebola, venom or toxin Only lasts as long as the original antigens do (no memory cells are made) 1st vaccination developed in late 1700s against small pox by using pus from cowpox sores! Yuck!