Methodical instructions to practical classes.
advertisement

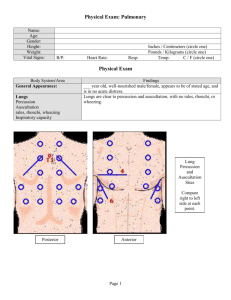
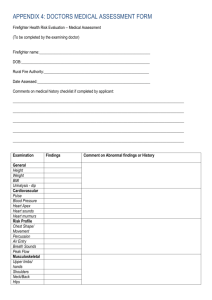
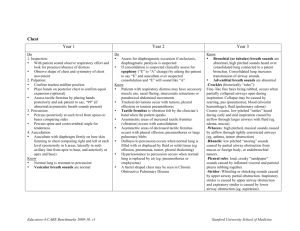
Danylo Halytskyi National Medical University Faculty of medicine Department of Propedeutic to Internal Medicine Methodological Guide for Patients Skills in Therapeutic Department for English-speaking Students of Medical Faculty (3-th Year of Studies) Lviv-2012 Topic 1. The History of the disease. Patients interviewing. Diagnostics value of symptoms and syndromes. Type of a lesson – tutorial and bedside. The aim – to perform a complete history of the patient. Contents: 1. Deontological ethics in medical professions. 2. The main methods of examination. 3. The auxiliary examinations methods. 4. The inquiry of the patient. 5. Signs or symptoms of the disease. Subjective and objective symptoms. Specific and nonspecific symptoms. 6. Syndromes and complexes of symptoms. 7. Parts of The History of the disease: - Identification - Patients present complaints - History of the presence disease (anamnesis morbi) - Past history (anamnesis vitae) - Habits - Family history and familial tendency 6. Present Complaints. 7. Anamnesis Morbi. 8. Anamnesis Vitae. Progress of a lesson (tutorial) - theoretical consideration, bedside interviewing of a patient. Interrogations: 1. Medical ethics. Hippocratic Oath. 2. What do main methods of examination include? 3. What is diagnostics and diagnosis? 4. What is sign or symptom of the disease? 5. What are subjective and objective symptoms? 6. What is difference between specific and nonspecific symptoms? 7. What is difference between syndrome and complexes of symptoms? 8. What types of diagnosis do you know (preliminary, clinical, final)? 9. What structure has a diagnosis (the main disease, complications of the main disease, concomitant diseases). 10.From what parts is consist the History of the disease? Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с. Sample Multiple Choice Questions Topic 2 General examination of the patient. A thorough physical examination. Examination of the head, neck, thoraces, extremities. Type of a lesson – theoretical consideration, practical (bedside). Contents: 1. The main methods of examination (inspection, palpation, percussion, auscultation). 2. The general patient’s condition. 3. Consciousness of the patient. 4. The posture of the patients. 5. The habits (the body-built, height, body weight, BMI). 6. Face of the patient. 7. Examination of the skin (color, eruption, turgor, moisture and elasticity). 8. The skin derivates (nails, hair). 9. Examination of subcutaneous fat. Types of obesity according to the fat distribution). 10.Examination of lymph nodes. 11.The muscular system. 12.The bones system. 13.The joints system. 14.Examination of the head (size, shape, position, movements). 15.Examination of the eyes (eyelids, eye slit, eyeball, sclera, cornea of the eye, pupils). 16.Examination of the mouth (size, shape, symmetry of the angles, form, color of the lips and mouth mucosa, teeth, tongue, gums). 17.Examination of the neck (the shape, size, symmetry, skin color, presence of scars and visible pulsation). 18.The auxiliary examinations methods (instrumental and laboratory methods). Interrogations: 1. What types of general patient’s conditions do you know? 2. What clinical features are criteria of patient’s general condition? 3. What type of consciousness disorders do you know? 4. What are differences between passive and forced (specific) posture? 5. Characterize posture of health person. 6. Describe specific gates (spastic, paretic, hemiplegic, puppet, peroneal, cerebellar, ataxic, gait as “a duck”, retarded, “proud” gates). 7. How is correct to assess a weight? The formula to calculate BMI. Classification of overweight and obesity in adults. 8. Describe facies in patients with pathology of respiratory system (facies pneumonica, tuberculous, asthmatica, adenoidea, aortale). 9. Describe facies in patients with pathology of cardiovascular system (facies mitrale, aortale, Corvisara, plethorica). 10.Describe facies in patients with endocrine pathology (facies acromegalica, mixedemica, basedovica, in Cushing’s syndrome, in hypogonadism). 11.Describe facies nefritica. 12.Describe facies in patients with pathology of nervous system(facies amimica, myopathica, asymmetrica, risus sardonicus). 13.Describe facies in patients with pathology of blood system (facies anemica, facies as a “wax-doll”). 14.Describe facies in patients with pathology of digestive system (facies Hippocratica). 15.What color of the skin has health individual? 16.What pathological changes of the skin do you know? In what pathologies can you observe them? 17.How many types of pathological jaundice according to the etiology do you know? Describe them. 18.What eruptions of the skin do you distinguish? 19.What hemorrhage lesions of the skin do you know? 20.What is teleangioectasia? 21.What is decubitus? 22.What are scars? Sings of which pathologies can they be? 23.What reflects turgor and elasticity of the skin? The technique of assessing of turgor and elasticity of the skin. 24.Caracteristics of normal nails. Affection of what systems can reflect nails in form of “watch glass”, spoon-shaped nails, “half and half” nails? 25.What is hirsutism? What specificity has hair growth in hypothyreosis, myxedema, Cushing’s syndrome, expose to radiation, liver cirrhosis. 26.Kinds of general edema. Ascitis, hydrothorax, hydropericardium. Anasarca. 27.How to asses the degrees of subcutaneous fat? 28.What is peripheral and central obesity? What additional criteria of central (abdominal) obesity do you know? 29.What is a consequence of lymph nodes examination? 30.What diagnostic meaning of the pathological lymph nodes do you know? 31.What are macrocephalia and microcephalia? 32.What abnormalities of the head shape and position do you know? 33.Symptoms of which pathology is shaking head synchronous with head function? 34.Characterize pathological changes of the eyelids. 35.Describe pathological colors of sclera. 36.Describe pathological colors of lips and mucous membrane of cavity of the mouth. 37.What diagnostic significance has shape, size and surface of the tongue? 38.What diagnostic purpose has pulsation of the carotid artery, swollen and pulsation of jugular veins? Sample Multiple Choice Questions 1. Clear conciousness is characterized by A. adequate behaviour, correct orientation to the surroundings, timely answer to the question, and preservation of all reflexes. B. disorientation in space, indifferent, the answers adequate, but delayed, reflexes are present. C. Unconsciousness with absence of response to external stimuli, absence of reflexes, deranged vital function. D. disorientation in space, surroundings, the answers inadequate and delayed, reflexes are present. 2. Active posture of the patients is defined as A. Patient is motionless, he lies, his head and his limbs hand down. B. Patient wants to relieve or remove pain, cough, dyspnea, or other sings of disease. C. Patient has ability to walk, stand, to change his posture. 3. Passive posture of the patients is defined as A. Patient has ability to walk, stand, to change his posture. B. Patient wants to relieve or remove pain, cough, dyspnea, or other sings of disease. C. Patient is motionless, he lies, his head and his limbs hand down. 4. Forced posture of the patients is defined as A. Patient has ability to walk, stand, to change his posture. B. Patient is motionless, he lies, his head and his limbs hand down. C. Patient wants to relieve or remove pain, cough, dyspnea, or other sings of disease. 5. Body mass index is defined as: 1. the individual’s body weight in kilograms divided by the square of their height in meters (kg/m2). 2. the individual’s height in meters divided by the square of their body weight in kilograms (m /kg 2). Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с. Topic 3 The main complaints of the patients with disease of the respiratory system. Static and dynamic inspection of the chest. Palpation of the chest. Type of a lesson – theoretical consideration, practical (bedside). Contents: 1. The dyspnea. Types of the dyspnea – physiological and pathological; subjective and objective; inspiration, expiration and mixed dyspnea. 2. The clinical analysis of cough. Dry and moist cough. The timing of coughing. Periodic or permanent cough. 3. The sputum expectoration and its characteristics: the amount, the time of day, posture of the patient, properties of sputum (color, odor). 4. The clinical analysis of the hemoptysis. Characteristics of the blood from the respiratory tree. 5. The clinical analysis of the chest pain: the pleural pain, the chest-wall pain, tracheobronchial tree sensations. 6. Static inspection of the chest. Normal and pathological shapes of the chest. The symmetry of the chest. 7. Dynamic inspection of the chest. Type, rate, depth, rhythm of respiration. 8. Palpation of the chest. Identification of the tender areas. Elasticity of the chest. The tactile fremirus. Interrogations: 1. What are the main complaints of the patients with disease of the respiratory tract? 2. What objective signs of dyspnea do you know? 3. What types of dyspnea quality are differentiated? 4. What is physiology of the cough? 5. What type of cough do you know? 6. What is hemoptysis? The difference between blood-stained material from respiratory and gastrointestinal tract. 7. What parts of the respiratory tract are sensitive to pain? 8. What typical signs of pleural pain do you know? 9. What is difference between pleural and chest-wall pain? 10.What mediastinal structures can cause a retrosternal pain? 11.What is difference between normosthenic, hypersthenic and asthenic shape of the chest? 12.The rules of determination of the epigastric angle. 13.What pathological changes can caused formation of pathological shapes of the thorax? 14.What pathological shapes of the chest can be formed due to the pathology of the pulmonary system? 15.What pathological shapes of the chest can be formed due to the pathology of the thorax costal skeleton? 16.What pathological shapes of the chest can be formed due to the pathology of the spine? 17.Describe the normal symmetrical chest. 18.What should examine doctor in dynamic inspection of the chest? 19.What respiration types do you know? 20.What is respiration rate? 21.What is difference between tachypnea and bradypnea? 22.What are the changes of respiration rate in different physiological conditions? 23.Please characterize respiration of healthy person. 24.What is difference between shallow and deep respiration? 25.What is difference between rhythmic and periodic respiration? 26.What types of periodic respiration do you know? 27.Please describe Cheyne-Stokes respiration, Grocco’s respiration and Biot’s respiration. 28.What information can give to the physician palpation of the chest? 29.What method of assessing of elasticity of the chest do you know? 30.How to examine tender areas of the thorax? 31.How to assess the elasticity of the chest? 32.What is vocal fremitus and how to examine it? 33.In what cases vocal fremitus is increased? 34.In what cases vocal fremitus is decreased? 35.In what cases vocal fremitus can be absent? Sample Multiple Choice Questions 1. The morning cough is sign of: A. chronic bronchitis; B. bronchiectasis; C. lung abscess; D. all of the above. 2. A sharp stabbing and knife-like character that is accentuated by respiratory movement is typical to the: A. acute bronchitis; B. pneumonia; C. pleurisy; D. all of the above. 3. The shape of the chest, its symmetry can be examined in: A. dynamic inspection; B. static inspection; C. palpation; D. auscultation. 4. The emphysematous chest in its shape resembles: A. hyperstenic; B. paralytic; C. rachitic; D. kyphoskoliotic. 5. In consolidation of the pulmonary tissue the vocal fremitus is: A. increased; B. decreased; C. absent; D. without any changes. Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с. Topic 4 Percussion of the lungs. The technique of comparative percussion. The technique of topographic percussion. Type of a lesson – theoretical consideration, practical (bedside). Contents: 1. Topographic regions and lines of the chest. 2. The physiological principles of the percussion. 3. The intensity of the percussion. 4. The task and technique of the comparative percussion. 5. The basic qualities of the percuss sound: intensity, pitch and duration. 6. The task and technique of the topographic percussion. 7. The upper borders of the lung. The lower borders of the lung. Respiratory excursion. Interrogations: 1. What are physiological principles of the percussion? 2. Why it is applied different force of tapping? 3. What is the position of the patient during percussion? 4. What areas of the chest should be percussed? 5. What is pleximeter finger and plexor finger? What is correct position of them? 6. What types of percussion of the lungs do you know? 7. What is the task of comparative percussion? 8. What types of the intensity, pitch and duration of the percussion sound can be distinguished? From what factors is it depends? 9. What percussion sound is typical to normal air-containing lung tissue? 10.What are physiological changes of the percussion sounds over the lungs? 11.What more types of the percussion sounds do you know? 12.In what cases clear pulmonary sound become duller (intermediate)? 13.When dullness replaces resonance? 14.When may be heard bandbox sound and tympany? 15.What is the task of topographic percussion of the lungs? 16.How to determine upper borders of the lung anteriorly and posteriorly? 17.Along what lines is carried out percussion in order to determine the lower lungs borders? 18.Where are the normal lower borders of the lungs? 19.When can be observed bilateral lowering of the lower border of the lung? 20.When can be observed unilateral lowering of the lower border of the lung? 21.When can be observed bilateral elevation of the lower border of the lung? 22.When can be observed unilateral elevation of the lower border of the lung? 23.What is respiratory excursion of the lower border of the lung? Sample Multiple Choice Questions 1. Anteriorly on the left side percussion is carried out to the A. 2nd interspace; B. 3rd interspace; 2. 3. 4. 5. C. 4th interspace; D. 5th interspace. The loud percuss sound is over the: A. fluid-filled organs; B. solid organs; C. air-filled organs; D. all of the above. In hemothorax over pathological region the percuss sound is A. Dull; B. resonance; C. bandbox; D. tympany. What potential uses has topographic percussion of the lungs? A. determination of the apices of the lungs; B. determination of the lower borders of the lungs; C. determination of the excursion of the lower borders of the lungs; D. all of the above. Bilateral lowering of the lower lung borders is observed in: A. emphysema; B. pneumosclerosis; C. obstructive atelectasis; D. meteorism. Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с. Topic 5 Auscultation of the lungs. The main respiratory sounds (vesicular and bronchial breath sounds). The adventitious sounds(rales, crepitation, pleural friction sounds). Type of a lesson – theoretical consideration, practical (bedside). Contents: 1. Auscultation technique. Points of auscultation. 2. The main respiratory sounds (vesicular and bronchial breath sounds). 3. Physiological difference of the vesicular breath sound over lungs. 4. Pathologic changes of the vesicular breathing: pathologically decreased and pathologically increased of the vesicular breathing. 5. Bronchial breath sounds. 6. Pathological bronchial breathing. 7. The adventitious sounds (rales, crepitation, pleural friction sounds). 8. Dry and moist rales. 9. Mechanism of crepitation. Auscultatory phenomenon in crepitation 10.Pleural friction sound. Differential diagnosis of crepitation and Pleural friction sound. Interrogations: 1. Which is the correct position of the patient during auscultation? How should the patient breathe during auscultation? 2. Is auscultation comparative method? 3. What areas should be listened? 4. What types of sounds can be heard coming from the lungs? 5. What main respiratory sounds do you know? 6. Please describe vesicular breathing. 7. Please characterize physiological difference of the vesicular breath sound over lungs. 8. Under what physiological conditions vesicular respiration can vary? 9. Under what pathological conditions vesicular respiration can vary? 10.What is the physiology of the formation of bronchial breathing? 11.What is the pathophysiology of formation of pathological bronchial breathing? 12.What is amphoric respiration? 13.What is bronchovesicular or mixed breathing? 14.What types of added respiratory sounds do you know? 15.What is mechanism and site of dry rales generation? 16.On which types are divided dry wheezing? 17.What is mechanism and site of moist rales generation? 18.What types of moist rales do you know? 19.What is mechanism of crepitation generation? 20.What is mechanism of pleural friction sound generation? 21.What is different between crepitation and pleural friction sound? Sample Multiple Choice Questions 1. How much respiratory cycles should be listened in one location? A. only inspiration is enough; B. only expiration is enough; C. at least one full breath; D. at least three full breathing acts. 2. Are added sounds abnormal? A. in case of pneumonia; B. always; C. never; D. when they are listened over bronchial bifurcation. 3. Through which period of auscultation vesicular breathing should be headed? A. during inspiration; B. during inspiration and one third of expiration; C. during inspiration and expiration; D. during expiration. 4. Laryngotracheal breathing is same as: A. amphoric; B. mixed; C. pathologically increased vesicular breathing; D. bronchial. 5. Louder by pressure with stethoskope can be: A. crepitation; B. pleural friction sound; C. moist rales; D. all of the above. Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с. Topic 6 Instrumental and laboratory methods of examination the patients with respiratory system disease. Final session on methods for evaluation of patients with respiratory system disease. Type of a lesson – theoretical consideration, practical (bedside). Contents: 1. Imaging studies used to examine the patients with disorders of the respiratory system: roentgenoscopy, radiography, computed tomography, magnetic resonance imaging, bronchography, pulmonary angiography, ultrasound examination. 2. Examination of biological specimens: collection of the sputum, thoracocentesis, bronchoscopy. 3. Sputum analisis: macroscopic, microscopic and bacterioscopic studies. 4. Study of the pleural fluid. Transudates and exudates. 5. Methods of functional studies. Tests of ventilatory function. Interrogations: 1. What method is routine for assessing the patients with disorders of the respiratory system? 2. What method is more sensitive to distinguish small focuses? 3. What is the physics basement of computer tomography? 4. What is principle of the pulmonary angiography? 5. In what cases ultrasound can be helpful for evaluation of pulmonary system disorders? Sample Multiple Choice Questions 1. The routine method for assessing the patients with disorders of the respiratory system is: A. computer tomography; B. ultrasound examination; C. bronchoscopy; D. radiography. 2. To distinguish small focuses in pulmonary tissue more sensitive is: A. magnetic resonance imaging; B. radiography; C. computer tomography; D. pulmonary angiography. 3. Mucopurulent sputum is: A. mixture of mucus and pus; B. consists of mucus; C. consists of mucus with streaks of blood; D. consists of pus. 4. Single erythrocytes in sputum can be visible in: A. inflammatory process in bronchi; B. lung infarction; C. any sputum; D. tumor endobronchially. 5. The criteria of classification of exudate and transudate are: A. the relative density; B. protein level; C. qualitative protein content; D. all of the above. Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с. Topic 7. Inquiring and general inspection of the patients with cardiovascular system disorders. Inspection and palpation of the heart region and peripheral vessels. Percussion of the heart: determination of the borders of the relative and absolute cardiac dullness. Configuration of the heart. Diagnostic value. Type of a lesson – theoretical consideration, practical (bedside). Contents: 1. Functional and clinical anatomy of the cardiovascular system. 2. Specific and nonspecific complaints in the cardiovascular disease. 3. Characteristics of the pain in cardiac ischemia. Atypical forms of the pain in cardiovascular disease. 4. Heart rhythm disorders. 5. Dyspnea, orthopnea and other respiratory symptoms in cardiovascular disease. 6. Syncope. 7. General inspection of the patients. 8. Posture of the cardiac patients. Orthopnea. 9. Skin and visible mucosa color. 10.Inspection of the face and neck. 11.Specificity of the edema in cardiovascular disease. Methods of edema revelations. 12.Inspection of the heart region. 13.Palpation of the heart region. The apex beat. 14.Percussion of the heart. Relative and absolute cardiac dullness. Configuration of the heart. Interrogations: 1. What are specific and nonspecific complaints in the cardiovascular disease? 2. What is typical to the heart pain? 3. What is difference between intermissions and palpitation? 4. What types of the dyspnea do you know? 5. Please describe the dyspnea as a symptom of left heart failure. 6. Due to what pathological process patients with cardiovascular disease can have cough and hemoptysis? 7. What are specific sings of the edema in cardiovascular disease? 8. What causes of the syncope do you know? 9. What forced postures in patients with cardiovascular disease are distinguished? 10.What changes of skin and visible mucosa color in patients with cardiovascular pathology are distinguished? 11.What special features can be found in the inspection of the face in patients with cardiovascular pathology? 12.What are mechanisms of edema formation in patients with cardiovascular pathology? 13.What methods of edema revelation can be used in patients with cardiovascular pathology? 14.What signs can be detected during the inspection area of the heart? 15.Please describe technique of palpation of heart region. Where is found a normal apex beat? 16.What are causes of the apex beat displacement? 17.What are apex beat properties? 18.What is examination plan of percussion of the heart? 19.How to determine relative and absolute cardiac dullness, configuration of the heart. 20.What types of heart configuration do you know? 21.How to determine transverse length of the heart and borders of the vascular bundle? Sample Multiple Choice Questions 1. Prolonged retrosternal pain above 20 min that does not response to nitrates is specific to: A. angina pectoris; B. myocardial infarction; C. pericarditis; D. cardiomyopathy. 2. Orthopnea is: A. sitting or standing posture of the patient due to worsening dyspnea in lying posture; B. acute dyspnea waking the patient from sleep; C. dyspnea results after less than ordinary physical activity; D. none of the above. 3. Hemoptysis is: A. persistent dry cough; B. cough during exertion; C. coughing up blood; D. foaming sputum. 4. Cardiac edema: A. has ascending character; B. is warm; C. more pronounced in the evening; D. all of the above. 5. Normal apex beat is found in: A. 4th intercostals space 1-1,5 cm toward to the sternum from the left midclavicular line; B. 4th intercostals space 1-1,5 cm laterally from the left midclavicular line; C. 5th intercostals space 1-1,5 cm laterally from the left midclavicular line; D. 5th intercostals space 1-1,5 cm toward to the sternum from the left midclavicular line. Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с. Topic 8 Auscultation of the heart. Technique and points of auscultation. Diagnostic value. Type of a lesson – theoretical consideration, practical (bedside). Contents: 1. The plan of examination. 2. The technique of the auscultation of the heart. 3. Points of projection of heart valves on the chest wall. 4. Standard listening points of the heart. 5. Normal heart sounds. Different sings of the first and second sound. Components of heart sounds. 6. Cardiac rhythm. 7. Heart rate. 8. Loudness of heart sounds. Decreasing and increasing of heart sounds. 9. Reduplication and splitting of the heart sounds. 10.Cardiac murmurs. Organic cardiac murmurs. Systolic and diastolic murmurs. Interrogations: 1. What is plan of auscultation of the heart? 2. Where are the sites of valves projection on the chest wall? 3. Where are points of auscultation of heart valves? Why we separate sites of valves projection and sites of auscultation? 4. Please describe characteristics of two heart sounds and two pauses between them. 5. Please describe changes of heart sounds in physiological and pathological conditions. 6. What is a cause of reduplication and splitting of the heart sounds? 7. In what conditions we can observe physiological splitting of the heart sounds? 8. What additional sounds can be auscultated over heart? Describe three-sound rhythms and systolic clicks. Sample Multiple Choice Questions 1. S1 is produced during: A. systole B. diastole C. systolic pause D. diastolic pause 2. The point of projection of mitral valve is: A. to the left from the sternum at the level of the 3rd costosternal articulation B. in the middle of the sternum at the level of the 3rd costosternal articulation C. in the 2nd intercostal space 1-1.5 cm to the left of the sternum D. base of the xifoid process 3. The point of auscultation of aortic valve is: A. The heart apex B. 2nd intercostal space to the left of the sternum C. base of the xifoid process D. 2nd intercostal space to the right of the sternum 4. Sings of S2 A. listening point – heart apex B. follows the long pause C. synchronous with apex beat D. nothing from all of the above 5. Both heart sounds increasing in all listening points in case of A. thyrotoxicosis B. anemis C. fever D. all of the above Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с. Topic 9. Auscultation of the heart. The mechanisms of cardiac murmurs. Diagnostic value. Phonocardiography and echocardiography. Type of a lesson – theoretical consideration, practical (bedside). Contents: 1. Functional and organic murmurs. 2. Systolic and diastolic murmurs. 3. A configuration of the cardiac murmurs. 4. The duration of the cardiac murmurs. 5. The location and radiation of the cardiac murmurs. Best auscultatory areas of a cardiac murmurs. 6. Clinical application of the phonocardiography. 7. Echocardiography: modalities, standard positions. Clinical application of the echocardiography. Interrogations: 1. How can you explain the mechanisms of cardiac mutmurs? 2. What is difference between decrescendo murmur, crescendo murmur, diamond-shaped and plateau murmur? 3. What is systolic and diastolic murmur? Which types of duration of murmurs do you know? 4. Please describe the specificity of duration and radiation of cardiac murmurs. 5. Which valves disorders can cause the systolic and diastolic murmurs? 6. Which positions of the transducer can be useful to examine the heart? 7. What is ejection fraction of the left ventricle? What methods of the assessment of the ejection fraction of the left ventricle do you know? 8. How do you understand diastolic function of the left ventricle? Sample Multiple Choice Questions 1. Systolic heart murmur A. terminates between S1 and S2 B. begins instead or after S2 C. terminates before the subsequent S1 D. nothing from all of the above 2. According to the Levine scale the heaert murmurs of Grade I A. are of loud intensity B. with a palpable thrill C. are audible by all listeners D. are of lowest intensity, difficult to auscultate by expert listeners 3. Auscultatory characteristics of mitral regurgitation are: A. auscultatory area is at the heart apex B. sustolic murmur C. no radiation D. A and B answers are correct 4. The murmurs in aortic stenosis radiate A. B. C. D. 5. A. B. C. D. to the left axillary region don’t radiate to the heart apex to the carotid arteries Diastolic murmurs are listened in: aortic stenosis aortic regurgitation mitral stenosis A and C answers are correct Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с. Topic 10. Assessment of the blood pressure and arterial pulse. Clinical electrocardiography. Interpretation of the ECG. Examination of waves, intervals. Determination of electrical axis of the heart. ECG-signs of atrial and ventricular hypertrophy. Type of a lesson – theoretical consideration, practical (bedside). Contents: 1. Study of arterial pulse: palpation, symmetry, rhythm, rate, tension, volume. 2. Blood pressure measurement. Classification of hypertension by blood pressure level. 3. Basic physiological principles of ECG. 4. Physiology of cardiac conduction system, cardiac automaticity, Cardiac conductivity function. 5. Graduation of the ECG paper. Speed of ECG paper. 6. The ECG leads. 7. The triangle of Einthoven. The electrical axis of the heart. 8. The waves and intervals on ECG. 9. The algorithm of reading of normal ECG. 10.Diagnostic ECG sings of atrial and ventricular hypertrophy. Interrogations: 1. On which arteries pulse can be assessed? Demonstrate the technique of pulse examination. 2. Describe the characteristics of the pulse: symmetry, rhythm, rate, correlation of the pulse and heart rate, tension, filling, size, speed and pulse wave shapes. 3. What causes of an irregular pulse do you know? 4. What can you estimate indirectly according to the pulse tension? 5. What is diagnostic value of characteristics of pulse? 6. What can be causes of tachycardia and bradycardia? 7. What method of using for measuring of blood pressure? 8. What reading is systolic and what is diastolic BP? 9. What is optimal and high normal BP? 10.What structures can be pacemaker of the heart? 11.Why refractoriness is important mechanism of preventing of heart from lifethreatening arrhythmias? Sample Multiple Choice Questions 1. If an ECG is recirded at speed of 50 mm/s, one small box (1 mm) represents A. 0,04 ms B. 0,01 ms C. 0,02 ms D. 0,05 ms 2. The standard bipolar limb leads are A. Leads I, II and III B. Leads aVF, aVR, aVL C. Leads V1-V6 D. all of the above 3. In horizontal position of heart electrical axis voltage of R is: A. RI>RII>RIII B. RII>RI>RIII C. RIII>RII>RI D. RI=RIII 4. The normal PQ-interval duration is: A. 0,08-0,10 sec. B. 0,12-0,2 sec. C. 0,06-1 sec. D. 0,35-0,04 sec. 5. The normal Q wave characteristics are: A. amplitude not more than 1/4 of the R wave B. its duration is 0,03 sec. C. may be deep and wide in the aVR lead D. all of the above Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с. TOPIC 11. Cardiac Arrhythmias. ECG in abnormalities of the impulse formation Type of a lesson – theoretical consideration, practical (reading of ECG). Contents: 1. Abnormalities of the Impulse Formation. Sinus tachycardia, bradycardia, arrhythmia, sick sinus syndrome. 2. Increasing of automaticity of an ectopic pacemaker: atrial rhythm, junctional rhythm, idioventricular rhythm, wandering pacemaker. 3. Ectopic arrhythmias: premature heart contraction, paroxysmal tachycardias, atrial and ventricular flutter and fibrillation. Interrogations: 1. List ECG-sings of sinus tachycardia. 2. What is sinus bradycardia and what diagnostic ECG sings of sinus bradycardia do you know? 3. What is sinus arrhythmia and has patient any clinical sings of sinus arrhythmia? 4. Which diagnostic ECG sings of junctional rhythm do you know? 5. What is idioventricular rhythm and what is difference on ECG in sinus bradycardia and idioventricular rhythm? 6. What ECG-sings of supraventricular premature contractions do you know? 7. What ECG-sings of ventricular premature contractions do you know? 8. What is compensatory pause? What is complete and incomplete compensatory pause? Sample Multiple Choice Questions 1. The cause of heart rate less than 40 beats per minute may be: A. ventricular rhythm B. sinus baradycardia C. heart sick syndrome D. all of the above 2. Wave P is hidden in QRS in A. sinus premature contraction B. an upper nodal extrasystole C. an midnodal extrasystole D. an lower nodal extrasystole 3. Does P-wave precede to QRS-complex in case of ventricular premature contraction? A. yes, always B. no C. if ventricular premature contraction generates in upper part of ventricular septum 4. Sings of wandering pacemaker are: A. changes of P-wave configuration from cycle to cycle B. PQ-interval duration is not constant, depend on the site of pacemaker C. the morphology of QRS-complex is normal D. all of the above 5. Brady-tachy syndrome is typical to A. idioventricular rhythm B. sinus arrhythmia C. sick sinus syndrome D. heart blockades Recommended literature: Kovalyova O., Ashcheulova T. Propedeutics to internal medicine. Part 1. – Вінниця: Нова книга, 2006. – 424 с.