Decannulation Protocol For Patients with Adequate Peak Flow
advertisement

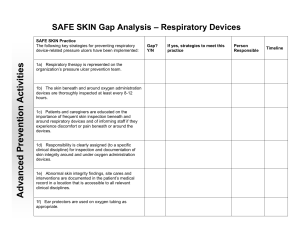
Gaylord Hospital Respiratory Care Protocol RCPRO 6 Decannulation Protocol For Patients with Adequate Peak Flow All patients undergoing decannulation will need to be evaluated by a Pulmonary or Critical Care Medicine (CCM) consultant. The consultant will document the patient is ready to go ahead with the decannulation protocol. For patients unable to perform cough peak flow procedure, refer to the protocol designated for inadequate peak flow. Daily progress of the decannulation process will be documented by the Respiratory Care Practitioner (RCP) and conveyed to covering therapists during change of shift report. The RCP will maintain daily communication with the Licensed Independent Practitioner (LIP) and/or consultant of the progress of the decannulation process. Once the decannulation protocol has been completed, the RCP will notify the LIP of completion of the protocol, and the LIP will enter the decannulation order in Meditech. Please refer to the section on trach removal. 1. LIP enters order for Decannulation Protocol into Clinical Information System. a. Criteria for Initiation of Protocol: i. All patients must meet the following criteria: 1. Afebrile 2. Hemodynamically stable 3. Clear or stable Chest X-ray 4. Controlled Secretions 5. Peak Cough Flow ≥160 l/m 6. Satisfactory on-going nutrition (low risk of aspiration) 7. No clinical evidence of tracheal obstruction 8. Ability to tolerate a speaking valve All patients must have a Morning ABG immediately upon completion of the Noctural Oxygen Therapy (NOT) study. The Respiratory Care Practitioner will determine that the above criteria have been met. If the patient fails to meet the criteria, the LIP will be notified and the protocol cancelled. 2. Initiation of Decannulation Protocol a. For all patients, Respiratory Care Practitioners/Registered Nurses: i. Decrease trach size to ≤ 6mm inner diameter. ii. Monitor vital signs including O2 Sat and EtCO2 every 4 hours for 24 hours with each tracheostomy change. iii. Observe tracheostomy site for bleeding. iv. RCP does tracheostomy change and documents same in the Clinical Information System. Gaylord Hospital Respiratory Care Protocol RCPRO 6 v. RCP/RN will notify LIP if vital signs become unstable &/or O2 Sat < 92% Note: The first tracheostomy change, post initial surgical insertion will be done by an ENT, Pulmonary or CCM physician 3. Plugging Trials a. Criteria to begin plugging trials i. Vital signs stable (within 15% of baseline) ii. For patients with no underlying lung disease: 1. O2 sat 92% or > and 2. EtCO2 < 50 mmHg iii. For patients with underlying lung disease: 1. Stable Blood Gases 2. PaCO2 <60 mmHg 3. O2 saturation ≥ 92% on Room Air or Oxygen b. Day 1 i. Plug tracheostomy (Note: Patients that require supplemental oxygen will be placed on the Vapotherm Precision Flow with nasal cannula.) ii. Monitor vital signs every 4 hours iii. Monitor O2 sat and EtCO2 every 4 hours iv. Plug up to 16 hours, remove for sleep 1. Criteria for unplugging sooner than 16 hours (Any of the following): a. Change in hemodynamics (BP 15% above or below baseline) b. Increased respiratory (15% above baseline) c. O2 Sat < 92% d. Increase in EtCO2 of > 20% over baseline e. Increased HR (15% above baseline) f. Temperature > 100.8 F°/ 38.2C g. Increase in pulmonary secretions Note: RCP will notify LIP and obtain an ABG if plugging trial fails. v. RCP will document plugging trial in the decannulation protocol and document intervention and patient response/compliance in notes section of Clinical Information System. c. Day 2 i. If successful for 16 hours of plugging over first day, then, on day 2, plug trach and leave plugged for 24 hours. (Note: Patients that require supplemental oxygen will be placed on the Vapotherm Precision Flow with nasal cannula.) ii. Monitor vital signs every 4 hours Gaylord Hospital Respiratory Care Protocol RCPRO 6 iii. Monitor O2 sat and EtCO2 every 4 hours iv. Obtain Overnight pulse oximetry v. Obtain early AM ABG according to criteria in section II 1. Criteria for unplugging before 24 hrs is any listed under Day 1, Section 1 above. Note: RCP will notify LIP if plugging trial fails. vi. RCP documents plugging trial and if appropriate that patient meets criteria for removal in notes section of the Clinical Information System. Any unsuccessful decannulation requiring replacement of the tracheostomy tube will require an ENT consult. If a patient is moved to another unit as part of the decannulation process, RT staff will complete bedside hand-off of report. 4. Decannulation a. Criteria for tracheostomy removal i. Decannulation will take place prior to 5 PM. ii. Stable vital signs (within 15% of baseline) iii. Oxygen saturation ≥ 92% iv. EtCO2 remains stable (within 5% of baseline) v. Overnight Oximetry results without suggestion of sleep apnea: vi. Overnight Oximetry results with suggestion of sleep apnea: 1. RCP will leave trach in place and discuss further action with the LIP b. If decannulation is decided, then the RCP will decannulate patient and place securely taped sterile gauze over the patient’s stoma c. RCP will then document procedure and patient response in the clinical information system. 5. Post decannulation a. For all patients, the RCP and Nurse will: i. Will monitor patient with pulse oxymetry for the first 24 hours post decannulation, with vital signs taken every 4 hours for the next 24 hours. If the patient is on telemetry during the decannulation process, he/she will be maintained on telemetry. b. The LIP will be notified if patient experiences: i. Change in hemodynamics (BP 20% above or below baseline) ii. Increased respiratory (15% above baseline) iii. O2 Sat < 92% iv. Increase in EtCO2 of >5% above baseline v. Increased HR (15% above baseline) vi. Temperature > 100.8 F°/ 38.2C vii. Increase in pulmonary secretions Gaylord Hospital Respiratory Care Protocol RCPRO 6 c. If stable, patient may be discharged 48 hours after decannulation. Original: 2/05 Reviewed and Revised: 6/06, 6/07, 6/08, 7/09, 7/10,12/11, 09/04/12, 4/14 Approved by: Approved by: _______________________________ Lorraine Trow, MD Medical Director ________________________ Peggy Bartram, Director Respiratory Services