Final Check Off Guidelines
advertisement

GEORGIA BAPTIST COLLEGE OF NURSING
Of
Mercer University
NUR 211 Health Assessment
Guidelines for Physical Assessment Performance Laboratory
Examination
A. The nursing history will be completed and turned in to the lab instructor prior to
the final physical exam. The checklist for the history and physical assessment is to be
turned in with the completed history. This is found in the syllabus.
B. Guidelines:
1.There will be one instructor evaluating one student.
2.The student will be evaluated using the performance checklist.
3.Laboratory testing will take place in the nursing skills lab.
4.Each student will have 45 minutes to complete the designated physical examination.
5.The instructor will function in the role of evaluator. The instructor will not answer questions
or assist with the examination.
6.The student is allowed to use note cards during the exam.
7.The student is expected to arrive for the exam at the designated time. If student arrives
late for exam, a grade of "O" will be given for performance examination and the student may
request another opportunity for performance with faculty within 24 hours.
8.Students failing to achieve 75% on the final physical assessment performance or
documentation of the final physical assessment performance will be allowed one additional
attempt to achieve a satisfactory score. (The maximum possible grade on a repeat final
physical assessment performance or a repeat documentation of the final physical
assessment performance will be 75).
Failure to achieve a satisfactory rating on either of the above will result in failure in the
course, necessitating retaking the entire course.
9.The student is expected to be able to perform a complete physical examination.
10.On completion of the laboratory exam, the instructor will have the student sign the
completed performance checklist.
11.Written documentation of the physical examination will be completed and turned in to the
lab instructor within 24 hours of completing the examination. Five points will be deducted
each day the documentation is late.
12.If the student receives a grade below 75 on the documentation of the final
performance examination, the student may submit a second documentation within 24 hours
of being notified of the unsatisfactory grade - no written feedback will be provided.
12/91/VDD
Reviewed 7/95 DL
Revised 6/97/DD; 6/97
Revised 4/02 CTH
Georgia Baptist College of Nursing
of
Mercer University
NUR 211 Health Assessment
Grading Form for Total Health Database
Student: ________________________________
Date: ________
Faculty: ________________________________
Grade: _______
Total Health Database
Points
P
Earned
o
s
s
i
b
l
e
Points
Biographical Data
5
Reason for visit (chief complaint)
5
Present health Status/Present Illness (History of present illness,
including seven dimensions of a symptom)
10
Past Health Data:
Childhood illnesses
5
Serious accident or injuries
Hospitalizations
Operations
Current Health Data:
Allergies
Immunizations
Habits
Medications
Exercise Patterns
Sleep Patterns
5
Family History
5
General State of Health
5
Total Health Database (continued)
Review of Physiological Systems
Integumentary
Head & Face
Eyes
Ears
Nose, nasopharynx, & sinuses
Oral cavity
Neck & lymph nodes
Breasts
Chest & Respiratory
Cardiovascular & Peripheral vascular
Gastrointestinal
Genitourinary
Musculoskeletal (extremities & back)
Central Nervous System
Hematologic
Endocrine
Possible
Points
30
Points
Earned
Total Health Database
Review of sociological system
Family relationships
Occupational history
Economic status
Daily profile
Educational level
Pattern of health care
Environmental data
Review of Psychological system
Cognitive abilities
Response to illness
Response to care
Cultural implications
Possible
Points
10
5
Developmental Data
2.5
Nutritional Data
2.5
Format & style (spelling, grammar, & sentence structure)
10
TOTAL
Revised 11/01 SHM
100
Points
Earned
Georgia Baptist College of Nursing
Of
Mercer University
TOTAL HEALTH DATABASE
BIOGRAPHICAL DATA
Client’s initials
Student Name
City, State
Birthdate
Age
Sex
Race
Religion
Marital Status
Informant
Education
Occupation
I.
Reason for Visit [Chief Complaint(s)}:
II.
Present/Health Status/Present Illness Status {History of Present Illness &
seven dimensions of the symptoms]:
Student Initials
III.
Past Health Data:
Childhood illnesses:
Serious accidents or injuries
Hospitalizations:
Operations:
Other major illnesses:
IV.
Current Health Information:
Allergies (food, drugs, environmental, latex):
Immunizations:
Habits:
Medications:
Exercise patterns:
Sleep patterns:
Student Initials
V.
Family Health History: relevant information regarding client’s blood relatives,
spouse, and children (to include client’s maternal and paternal grandparents,
aunts, and uncles) related to Alzheimer’s disease, cancer, diabetes, heart
disease, hypertension, epilepsy, mental illness, alcoholism, endocrine
diseases, sickle cell anemia, kidney disease, genetic defects and other
chronic or communicable diseases. (CIRCLE POSITIVE FINDINGS.
COMPLETE A FAMILY TREE CHART UTILIZING TRADTIONAL
GNEOGRAM NOTATIONS. SEE SAMPLE IN TEXTBOOK).
VI.
General State of Health to include information regarding description of current
health status; fatigue patterns; exercise tolerance; episodes of weakness;
fever; sweats; frequency of colds, infections, or illnesses; ability to perform
ADL.
Student Initials
VII.
Review of Psychological Systems: (CIRCLE POSITIVE FINDINGS;
EXPLAIN ANY POSTIVE FINDINGS UTILZING THE SEVEN DIMENSIONS
OF A SYMPTOM)
Integumentary:
skin, (lesions, growths, dryness, sweating, odors, pigment changes, pruritus, texture
or temperature changes, sun screen use, bathing habits, skin care products)
hair (changes in amount, texture, character, use of dyes, hair care products, perms,
hair care)
nails (changes in appearance, texture, artificial nails, use of polish)
Head & Face: headache, trauma, vertigo, dizziness
Eyes: discharge, visual problems, pain, edema, use of corrective lenses, eye
exams, excessive tearing, itching
Ears: pain, hearing loss, tinnitus, discharge, infection
Student Initials
Nose, nasopharynx, and sinuses: discharge, epistaxis, allergies, pain, sneezing,
olfactory ability
Oral cavity: lesions, pain, bleeding, hoarseness, prosthetic devices, problems
chewing or swallowing, hygiene practices, dental care
Neck and Nodes: nodes, masses, tenderness, limitation of movement
Breast: pain or tenderness, swelling, discharge, lumps or dimples, pattern and
frequency of self exam
Chest & Respiratory: asthma, sputum production, hemoptysis, cough, shortness
of breath, night sweats, wheezing or difficulty breathing
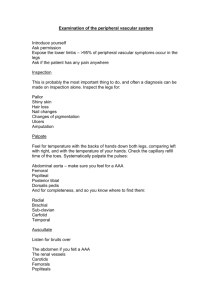
Cardiovascular: palpitations, murmur, hypertension, heart disease, chest pain,
shortness of breath, orthopnea, paroxysmal nocturnal dyspnea; Peripheral
vascular (coldness, discoloration, peripheral edema, varicose veins, intermittent
claudication).
Student Initials
Gastrointestinal: dysphagia, food, intolerance, pain, indigestion, nausea,
vomiting, ulcer, hematemesis, jaundice, ascites, bowel habits, stool
characteristics, hemorrhoids, use of laxatives or antacids
Genitourinary: dysuria, frequency, urgency, hesitancy, incontinence nocturia,
force of stream, bleeding, stones, pain, polyuria, oliguria, pyuria, lesions,
discharge, odor, pain, veneral disease, satisfaction with sexual activity, birth
control methods practices, sterility; Males: prostate problems; Females:
menstrual history, amenorrhea, menorrhagia, dysmenorrheal
Musculoskeletal (Extremities & Back): weaknesses, pain, swelling, redness or
stiffness, deformity, cramping, crepitus, twitching, gait, limitation of movement,
prostheses or braces
Central Nervous System: fainting, seizures, memory, orientation, phobia,
hallucinations, coordination of movement, paralysis, tic, tremors, spasm,
parethesia, tingling sensation
Student Initials
Hematologic: lymph node swelling, excessive bleeding, anemia, transfusions,
bruising, exposure to radiation
Endocrine: intolerance of heat or cold, goiter, polydipsia, polyphagia, polyuria,
anorexia, weight, or height change, change in hair distribution, change in
pigmentation or texture of hair or skin
VIII. Review of Sociological System
Family relationships:
Occupational history:
Economic status:
Daily profile:
Educational level:
Patterns of health care:
Environmental data:
Student Initials
IX.
Review of Psychological System
Cognitive abilities:
Response to illness:
Response to care:
Cultural implications:
X.
Developmental Data (use Erikson’s stage)
XI.
Nutritional Data:
Revised 4/02/CTH
Student's Name _______________
Physical Examination
NUR 211
Client's initials: _____
Date: _____
Vital Signs: _____ T _____
P _____
R _____
Height _____
Weight _____
General Survey:
Integument:
Head:
Eyes:
Ears:
Nose and paranasal sinuses:
Mouth and pharynx:
BP (R) arm _____
BP (L) arm _____
Student's Name: ___________________
Neck and Lymphatics:
Breast and axilla:
Thorax and Lungs:
Heart and Peripheral Vascular System:
Pulses:
Carotid
Brachial
Radial
Femoral
Popliteal
Dorsalis pedis
Posterior tibial
0
1
Absent
Abdomen:
Genitalia:
Genitourinary:
Musculoskeletal:
Markedly
Impaired
Right
2
3
Moderately
Impaired
Slightly
Impaired
Left
4
Normal
Student Name _________________
Neurological:
Mental status and speech:
Cranial Nerves:
Cranial
Nerve:
I
II
III, IV, VI
V
VII
VIII
IX, X
XI
XII
Evaluation Comments:
Student Name __________________
Motor:
Sensory:
Reflexes:
R
L
Biceps
Triceps
Brachioradialis
Patellar
Ankle
Plantar
0
Absent
Revised 10/01KH
PHYSEXAM
1
Diminished
2
3
Average
Brisker than
Normal
4
Very Brisk
Student name: ___________________________________
Faculty name:_______________________
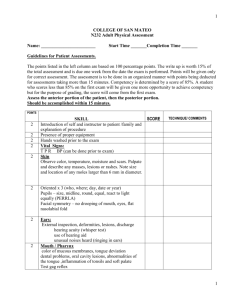
NUR 211 Health Assessment Final Check-Off Evaluation Form
Performance
Written Record
General Inspection
Done
Done Incorrectly
Points
Recorded
Recorded
Correctly
Or not done
Earned Accurately &
Incompletely
Completely
General appearance and state of
*Points for this
Is not included in
health; estimation of height &
The Performance
Portion of the
weight
Evaluation. This
Information must,
Estimation of somatic age (older,
Younger, same as stated age)
Patient's speech
However, be
The written
Included when doing
record
Points
Earned
Points
Possible
2
1
1
SKIN
Assess skin for color, temperature
& turgor
HEAD
Inspect head
Inspect scalp/hair
Palpate scalp
Inspect face noting facial
Muscle movement (CN VII)
Masseter compression & facial
sensation (CN V)
EYE
Determine visual acuity (CN II)
(Rosenbaum)
Determine e.o.m.'s
(CN III, IV, & VI)
Inspect external ocular structures
Observe pupillary response to light
& accommodation
3
1
1
1
3
3
2
2
2
2
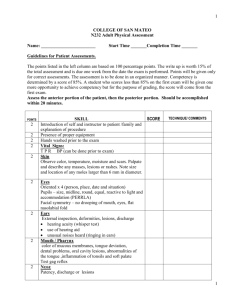
NUR 211 Health Assessment Final Check-Off Evaluation Form
Performance
General Inspection
EAR
Inspect external canal
Inspect ear canal and T.M.
Assess hearing with whisper test
NOSE/MOUTH
Inspect nose/nasal mucosa
Inspect mouth (lips, buccal mucosa,
gums, teeth, roof & floor of mouth)
Inspect tongue movement(CN XII)
Inspect pharynx
Observe movement of soft palate
(CN IX, X)
NECK
Inspect neck
Palpate lymph nodes (occipital, pre
& post auricular, cervical chain,
submental, submaxillary, supra &
infraclavicular)
ROM of cervical spine
Determine strength and contraction
of sternocleidomastoid & trapezius
(CN XI)
Done
Correctly
Done Incorrectly
Or not done
Written Record
Points
Earned
Recorded
Accurately &
Completely
Recorded
Incompletely
Points
Earned
Points
Possible
2
2
1
2
2
2
2
2
1
2
2
2
NUR 211 Health Assessment Final Check-Off Evaluation Form
Performance
General Inspection
BREAST
Inspect breast in sitting positions,
inspect nipples
Palpate axillae in sitting position
Palpate breasts supine position
Done
Correctly
Done Incorrectly
Or not done
Written Record
Points
Earned
Recorded
Accurately &
Completely
Recorded
Incompletely
Points
Earned
Points
Possible
2
1
3
THORAX/LUNGS
Inspect rate, rhythm and effort
3
Auscultate all lung fields
3
CARDIOVASCULAR
Auscultate heart
(using bell & diaphragm)
Auscultate carotids
Assess capillary refill and nail bed
color
Palpate all pulses bilaterally and
Simultaneously (radial, brachial,
femoral, posterior tibial, & dorsalis
pedis)
ABDOMINAL
Inspect abdomen including flanks &
groin
Auscultate for bowel sounds
Palpate abdomen
3
2
1
3
2
2
2
NUR 211 Health Assessment Final Check-Off Evaluation Form
Performance
General Inspection
MUSCULOSKELETAL
Inspect and palpate spine
Inspect and palpate upper and lower
extremities
Determine ROM of upper and lower
extremities
Determine strength of upper and
lower extremities
NEUROLOGICAL
Sensory
Test vibration
Test light touch and pain
Reflexes
Test deep tendon reflexes (triceps,
biceps, brachioradialis, patellar, &
achilles, plantar)
Motor
Test coordination (finger-nose, heelshin, rapid alternating movements)
Test proprioception (Romberg)
Observe gait
Mental
Assess orientation
Done
Correctly
Done Incorrectly
Or not done
Points
Earned
Written Record
Recorded
Accurately &
Completely
Recorded
Incompletely
Points
Earned
Points
Possible
2
2
2
2
2
2
2
2
2
2
2
NUR 211 Health Assessment Final Check-Off Evaluation Form
Relationship to patient
Most
About half the time
Seldom
Points earned
performance
Possible points this
section
Did student give appropriate
explanation to client prior to starting
assessment?
Did student preserve client's modesty
throughout exam?
Did student integrate performance of
assessment in an efficient manner?
2
Did student present self in professional
manner both in verbal and nonverbal
behavior?
2
2
3
Performance write-up
Format &style (spelling, proper use of medical terminology and phrasing)
5
Total possible points performance = 100
Total points earned performance = _____
Total possible points written record = 100
Total points earned written record = ____
* Points for the above shaded area are not included in the written portion of the evaluation
* Minus 5 points for turning performance documentation in past 24 hours after performance demonstration