File
advertisement

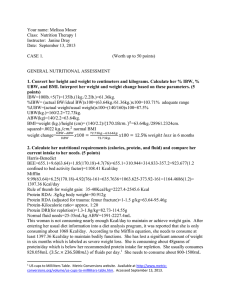
Miska Upton Medical Nutrition Therapy 1 Case Study #1 Dr. Alireza Jahan-mihan September 8, 2014 Clinical Case Studies for the Nutrition Care Process Case 1: General Nutrition Assessment Learning Objectives 1. Recognize anthropometric, biochemical, clinical, and dietary factors that impact on nutritional status. 2. Calculate and interpret weight change and body mass index. 3. Determine adequacy of dietary intake. 4. Apply the Nutrition Care Process to an elderly patient. Case Description Background Adequate nutrition can be viewed as a state of balance between intake, requirements, metabolism, and losses of nutrients. The term malnutrition usually refers to a state of undernutrition, and has been associated with increased morbidity and mortality in the clinical setting (1-4). The accurate identification and patients at risk for malnutrition and its associated complications is both an art and a science; subjective and objective data are interpreted along with clinical judgment to evaluate nutritional status. From the dietary standpoint, a full evaluation considers not only calorie and protein intake but also vitamin and mineral status. Surrogate markers of visceral protein stores such as serum albumin and prealbumin have traditionally been measured for nutritional assessment. These parameters are now known to be affected by many factors, including hydration, physiological stress, and inflammation. Particularly during metabolic stress, serum proteins more specifically reflect severity of illness than nutritional stores (1-7). While a low serum albumin is associated with an increased morbidity and mortality, it cannot be used alone to measure nutritional status or repletion. Conversely, a normal serum albumin cannot be used in isolation to rule out malnutrition. Serum protein levels by themselves do not form the basis for nutrition diagnosis or intervention. Individual assessment parameters should be considered as part of the biggest picture of nutritional equilibrium. The client is a 76-year old woman with a history of hypertension admitted to the hospital after tripping over her cat and falling at home. She is admitted for a femur fracture. She is currently confined to bed. Nutritional Assessment Data 1. Anthropometric Measurements. Height: 67’ Weight: 140lb Usual weight: 160lbs 6 months ago. She has been unmotivated to cook since the loss of her husband during the previous 6 months. 2. Biochemical Data, Medical Tests, and Procedures. a. Labs Parameter Value Sodium 140 mEq/L Normal Ranges* (may vary by age, sex, and lab) 135-147 mEq/L Potassium 3.2 mEq/L 3.5-5.0 mEq/L Chloride 103 mEq/L 98-106 mEq/L Carbon dioxide 29 mEq/L 21-30 mEq/L BUN 19 mg/L 8-23 mg/L Creatinine 1.0 mg/L 0.7-1.5 mg/L Glucose 108 mg/L 70-110 mg/L Hemoglobin 12.0 g/L 12-16 g/L (female) Hematocrit 38.1% 36-47% (female) Albumin 3.2 g/dL 3.5-5.5 g/L Prealbumin 11mg/dL 16-40 mg/L b. Test results, if pertinent X-ray indicates fracture of left femoral neck. 3. Nutrition-Focused Physical Findings Blood pressure: 128/65 mm Hg Oral mucosa dry. Has upper and lower dentures which are poorly fitting. Skin turgor decreased. 4. Client History Social Hx: No smoking or alcohol Husband diet 6 months ago and patient has lost weight since this time Family Hx: N/A 5. Food/Nutrition-Related History Usual Diet Breakfast: 1 cup (8oz) decaffeinated tea with 1 tbs half and half and 1 tsp sugar 1 slice white toast with 1 tsp margarine and 1tsp jelly or 1 frozen pancake with 1 tbs syrup ½ cup orange juice Lunch: Canned soup, usually chicken noodle, 1 cup 4 unsalted crackers with 2 tbs peanut butter ½ cup sliced peaches in light syrup Sweetened iced tea, 1 cup Dinner: Chicken thigh with skin, stewed ½ cup rice or potato with 1 tsp margarine ½ cup spinach or carrots 1 cup (8oz) decaffeinated tea with 1 tbs cream and 1 tsp sugar Notes: Rarely eats or drinks between meals. Avoids eggs and milk due to food preferences. Medications Furosemide 20 mg daily Supplements None Questions: 1. Convert her height and weight to centimeters and kilograms. Calculate her % IBW (1 point), % UBW (1 point), and BMI (1 point). Interpret her weight and weight change based on these parameters (2 points). 2. Height: 170.18cm 1 3. Weight: 140lb/2.2kg/lb= 63.63 kg 1 4. IBW: (63.64 kg/ 60.09 kg) x 100 = 104 % 1 5. The patient has lost 20lbs in six months, resulting in a 12% wt loss. 6. BMI: 21.9 1 7. UBW= (63.64 kg/72.73 kg) x 100 = 87.5%. 1 8. Calculate her nutritional requirements (calories, protein, and fluid) (3 points) and compare her current intake to her needs (2 points). 9. Mifflin St Jeor: 10. 10 x 63 (630) + 6.25kg x 170cm (1062.5)-5 x 76(380)-161=1151.5 11. Harris-Benedict Equation: 12. 447.593+ (9.247 x 63kg) + (3.098 x 170)- (4.330 x 76)=1227.7 cal 13. Total Carbohydrate: 130.0g 2 14. Dietary Fiber: 21.0g 2 15. Protein: 1g/kg BW= 64 g/d 1 16. Fluid intake: 30ml/kg BW= 1910 ml/d 1,2 17. The pt fluid intake is very low. She is only taking in, on average around 1000 ml/d of fluid, none of which is water. 18. Based off the patients food history, an example day of eating provides her with an estimated 1000 kcal, which is only around 65% what her caloric intake should be. 19. The protein requirements for the patient is 64g/d, though she is roughly only taking in about 40g/d.1,2 20. Are any major food groups and nutrients obviously missing from her diet? Explain your answer. 21. Even though the patient is not fond of milk, there is a need for dairy products (yogurts or cheese) in order to increase her calcium intake. Her protein intake is low due to only a small amount of proteins in the diet. And the patients fruit and vegetables are not in the amounts that they should be.3 22. Do you think she could be experiencing any drug–nutrient interactions? (2 points) If so, what dietary suggestions would you make? (3 points) 23. The patient is taking 20 mg of Furosemide daily, which is an antihypertensive loop diuretic. This calls for an increase in potassium as well as magnesium and calcium. Furosemide interacts with many minerals, which leads to loss of minerals in the urine. I would recommend that the patient eat foods like sweet potatoes, beans, bananas, yogurt, or green leafy vegetables. Furosemide also can increase the risk of anorexia. This will need to be particularly monitored for risk of inadequate nutrient intake. 4 24. Interpret her serum albumin and prealbumin. (2 points) In addition to nutritional intake, what factors can cause these indices to drop? (2 points) What factors would cause them to be elevated? (1 point) The normal ranges for albumin are between 3/5-5.5 g/dL and for prealbumin 16-40mg/dL. 1,5 The patients albumin levels are at 3.2 g/dL and her prealbumin level is 11 mg/dL. Her low levels or albumin and prealbumin levels indicate that her protein intake is too low. Decreased albumin levels can also indicate low levels of iron, vitamin A and zinc deficiencies. 1 It could also decrease from malnutrition, kidney disease, liver disease and gastrointestinal malabsorption syndromes. 5 Elevated levels of albumin can occur when the patient is dehydrated. 1 Low levels of prealbumin levels can occur if the patient is deficient in zinc, has acute stress reactions, liver disease or hemodilution. 5 Elevated levels of prealbumin can be due to renal failure. 1 25. Describe how factors in her anthropometric, biochemical, clinical, and dietary nutritional assessment data all fit together to form a “picture” of her nutritional health. (5 points) 26. Anthropometric Ax: The patient is an elderly, 76 year old woman who’s BMI is in the normal range. However, she has lost nearly twenty pounds in the last 6 months, causing concern.1 Biochemical Ax: The woman’s albumin and prealbumin levels are both very low, which could indicate a number of deficiencies or risk factors. 1,2 The patients low levels most likely are related due to inadequate amounts of protein in her diet. 2 Because the patient is taking furosemide, she needs to increase her amounts of potassium. Currently the patients potassium levels are around 3.2 mEq/L, which is below the normal ranges of 3.5-5.0 mEq/ L. Clincal Ax: Though the patient has no family history of hypertension, the patient’s blood pressure is 128/65 which is pre-hypertensive. 3 Some causes of hypertension might be high levels of sodium intake, insufficient calcium, potassium and magnesium consumption, kidney disease, or stress. Dietary Ax: The patient clearly is not taking in enough calories to sustain a healthy diet. Her protein requirements are also not being met, which is leading to low levels of albumin and prealbumin. The patients lack of calcium, due to the patients preference to not have milk, is low. There is a need for the patients to increase her protein, dairy, and whole grains in her diet. Her fluid intake is also low and should be increased. 1,3 27. Write a PES statement based on the nutritional assessment data available. (5 points) Inadequate amounts of protein related to low intake as evidence by low albumin and prealbumin levels. Inadequate amounts of potassium in the diet related to inadequate intake of fruits, vegetables and whole grains and supplementation of furosemide as evidence by patients diet recall and biochemical test. 28. What dietary and social changes would you suggest to improve her nutritional intake? (5 points) 29. For dietary changes, I would suggest that the patient increase her calorie intake by 200-300 calories. I would stress the importance of adding protein sources like beans, lean meats and fish into her diet as well as the importance of adding whole grains, fruits, and dairy. Because of her medications, I would explain the need for potassium and how she could easily raise her levels by incorporating fresh produce into the diet. Because of her fracture and lack of milk consumption, I would encourage the client to look for other sources of calcium like leafy greens, broccoli, nuts, and beans. 1,3 30. For social changes, I would ask the client if she had any family near by that could help prepare and enjoy meals with. According to the patients assessment, the client has lost twenty pounds since the death of her husband, indicating decreased amounts of food as well as a possible sign of depression. 1 31. What are your nutritional goals for her (2 points), and how would you monitor the effectiveness of your interventions from question #8? (3 points) 32. My nutritional goals for the client would be an increase in protein, calcium and potassium within 3 days. I would also like to see her increase her fluid and caloric intake by 25% within the next 42 hours. 33. I would monitor the effectiveness of my intervention by asking how the patient is feeling in regards to cooking and preparing meals with family members or friends and follow up on this to see if she initiated any meal time fellowships within the last week. 34. 35. Write a note documenting your assessment in SOAP or ADIME format. (5 points) S: Inadequate diet, inadequate fluid intake, inadequate protein intake. Lives and eats alone since husbands passing. PMH-HTN. 1 O: Patient is 5’7. Admitted into hospital for femur fracture. PMH-HTN. BMI= 21.9. IBW=60. Low K. ALB: 3.2 g/dL. Taking furosemide for HTN. 1-5 A: Pt is a at normal BMI. severe wt loss since husband passing in 6 months. Needs to increase fluid intake, calories, protein. Drug-nutrient interactions with furosemide could possibly be leading to anorexia, need for K, Ca, and Mg. 1-5 P: Counseling on ways increase fluid and calories needed. Recommending social meal times to enjoy eating meals more. Schedule snacks throughout the day and set goals to achieve fluid intake. Follow up with pt in 2 weeks to check levels of Ca, K, and Mg as well as albumin and prealbumin to check for adequate dietary changes. 1-6 References: 1. Mahan LK, Escott-Stump S, Raymond JL. Krause’s Food and the Nutrition Care Process. St. Louis, Mo: Elsevier Saunders; 2012. 2. SuperTracker Web site. http://supertracker.usda.gov. Accessed September 10, 2014. 3. Nelms M, Sucher K, Long S. Thomson/Wadsworth, Nutrition Therapy and Pathophysiology Australia, Third Edition, 2010- 2011. 4. Pronsky ZM, Crowe JP. Food-Medication Interactions. Birchrunville, Pa: FoodMedication Interactions; 2010: 110. 5. WebMD Website. http://www.webmd.com/a-to-z-guides/total-serum-protein?page=2. Accessed September 10, 2014. 6. Emery EZ. Clinical Case Studies for the Nutrition Care Process. Burlington, Ma: Jones & Bartlett Learning; 2012: 3-7.