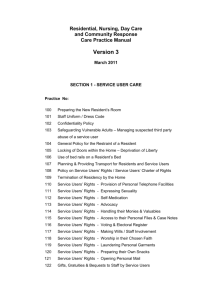
DML Integrated Minimum Data Set
advertisement

DML Integrated Minimum Data Set Resident Assessment Instruments (RAIs), Resident Assessment Protocols (RAPs) & Personalised Care Planning DML Services for Older Persons & Nursing and Midwifery Planning and Development April 2010 Foreword Services for Older people who live in residential care in Ireland are directed by a number of strategies emanating from the Department of Health and Children, from the Corporate Plan of the Health Service Executive and more latterly by the Health Information and Quality Authority (HIQA) through their “National Quality Standards for Residential Care Settings for Older People in Ireland” (HIQA 2009). The provision of care based on an individualised assessment and the development of a personalised care plan is central to these standards. The Nursing & Midwifery Planning and Development Unit in Palmerstown, in conjunction with HSE, DML Services for Older Persons is very pleased to publish this evidence based document which outlines a minimum dataset and supporting documentation tools for use in residential care settings. The minimum dataset comprises Resident Assessment Protocols and Personalised care planning – based on protocols of care and sample care plans. It also includes Resident Assessment Instruments which are included in the appendices. These documents provide nursing staff who work in residential care settings with a comprehensive range of evidence based tools to support them in all aspects of resident assessment and care planning. They assist in the standardisation of documentation across all Health Service Executive residential settings in Dublin Mid-Leinster. I wish to sincerely express our appreciation to the documentation group for their expertise, time and effort over the last eighteen months in the development of this document. Special thanks are extended to Ms Linda McDermott Scales, Chairperson of the DML Documentation Group, - DML Services for Older Persons and Ms Angela Ring former Project Officer; Older Persons services – NMPD for their commitment and drive for the project, thereby ensuring its successful completion. Liz Roche Director NMPD – Palmerstown April 2010 1 Table of Contents Disclaimer . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3 Section 1 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4 1.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4 Section 2 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6 2.1 Personalised Care Planning using the DML Integrated Minimum Data Set . . . . 6 2.2 Resident Assessment Instruments (RAIs) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6 2.3 Resident Assessment Protocols (RAPs) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6 2.4 Lay out of the RAPs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6 2.4.1 Definition . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8 2.4.2 RAI Identifiers of Potential Risk . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8 2.4.3 Risk Factors (intrinsic & extrinsic) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9 2.4.4 Further Assessment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9 2.4.5 Referrals Required . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9 2.5 Personalised Care Planning . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9 2.6 Documenting Personalised Care Planning . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10 2.6.1 Topic Heading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10 2.6.2 Problem/Need Identification . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10 2.6.3 Goal specification . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10 2.6.4 Specific Interventions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10 2.6.5 Evaluation of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11 2.7 Protocol of Expected Standards for Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11 2.8 Sample Care Plan Generic or Personalised . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11 Section 3 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13 Resident Assessment Protocols . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13 RAP 1: Communication, Vision and Hearing . . . . . . . . . . . . . . . . . . . . . . . . . 17 RAP 2: Mood and Behaviour . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28 RAP 3: Cognition and Acute Confusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37 RAP 4: Breathing and Circulation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 44 RAP 5: Nutritional Status . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56 RAP 6: Dehydration and Fluid Maintenance . . . . . . . . . . . . . . . . . . . . . . . . . 65 RAP 7: Urinary Incontinence and Continence Promotion . . . . . . . . . . . . . . . 73 RAP 8: Faecal Incontinence and Continence Promotion . . . . . . . . . . . . . . . . 81 RAP 9: Constipation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 92 RAP 10: Falls Prevention and Risk Reduction . . . . . . . . . . . . . . . . . . . . . . . . 100 RAP 11: Impaired Ability for Personal Care . . . . . . . . . . . . . . . . . . . . . . . . . 107 RAP 12: Pressure Ulcer Prevention and Management . . . . . . . . . . . . . . . . . 115 RAP 13: Skin and Wound Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 122 RAP 14: Psychosocial Welfare . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 137 RAP 15: Activities . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 146 RAP 16: Pain . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 163 RAP 17: Disturbed Sleep and Rest . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 172 RAP 18: Psychotropic Drug Use . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 177 RAP 19: MRSA . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 188 RAP 20: Feeding Tubes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 197 RAP 21: Palliative Care for All . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 214 RAP 22: End of Life Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 223 Section 4 Appendices Appendix 1 Integrated Minimum Dataset and Resident Record - Chart Layout . . . . . 232 Appendix 2 Resident Assessment Instruments . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 234 Appendix 3 Documentation Audit Tools . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 297 Appendix 4 Guidelines for completing "My Day My Way" . . . . . . . . . . . . . . . . . . . . . 306 2 Disclaimer The Resident Assessment Protocols (RAPs) and the Protocols for the Expected Standards of Care in Older Persons designated centres as stated in this document, have been developed based on the best available evidence with expert and peer review. The aim of these instruments is to assist healthcare professionals, carers, residents and their significant other(s) in making decisions about appropriate options or treatments for specific conditions and aspects of care. As with all clinical policies, procedures, protocols and guidelines, the recommendations provided may not be appropriate for use in all circumstances. Decisions to adopt any particular recommendation must be made by the practitioner in the light of: • The resident’s/significant other(s) circumstances and wishes • Available resources • Local services, policies and protocols • Available personnel and support services • Clinical judgement and the experience of the practitioner • Knowledge of more recent research findings 3 DML Integrated Minimum Data Set Resident Assessment Instruments (RAIs), Resident Assessment Protocols (RAPs) and Personalised Care Planning Section 1 1.1 Introduction The ‘National Quality Standards for Residential Care Settings for Older People in Ireland’ and its supporting legislation, set out the standards of the quality in care that older people living in designated centres can expect to receive 1, 2, 3. The provision of these minimum standards in expected care is centred within a model of personalised care planning which is to be delivered within a home-style setting. Personalised care planning is fundamentally based in addressing an individual’s full range of needs and wishes, taking into account their health, personal, social, economic, educational, mental health, ethnic and cultural background and their circumstances4. It recognises that there are other issues in addition to medical needs that can impact on an older person’s total health and well-being. The overarching aims of the care planning process are to: • Put the individual, their needs and choices at the centre of the process to support them in achieving optimal health and well-being • Focus on goal setting and outcomes that residents, their significant others and carers want to achieve • Ensure that there are appropriately planned strategies in place, to address the resident’s potential or actual problems or needs, and that contingency (or emergency) plans are available to better manage crisis episodes (for those with complex needs, such as those with behaviour that challenges) • Ensure that resident choice and control are promoted by putting the person at the centre of the process and facilitating better management of risk • Ensure that people, especially those with more complex needs or those approaching end of life, receive co-ordinated care, reducing fragmentation between disciplines and services • Provide information that is relevant and timely to support residents with decision making in care and lifestyle choices • Provide support for self-care, so that residents can self-care/self-manage their condition(s) and prevent deterioration where possible • Facilitate multidisciplinary team working and inter agency working • Result in an overarching, single personalised care plan that is owned by the resident, but can be accessed by those providing direct care or by other relevant people as agreed by the resident. For example, if a resident is reviewed by a member of the multidisciplinary team (MDT) and specific care instructions are given, the resident’s care plan interventions should be updated to reflect the changes ordered. This ensures a single overarching plan of care is provided to the resident. 4 Note: In designated centers for older people that use an integrated resident record system i.e., where all members of the MDT record in the same resident file, the MDT can record the specific interventions required for achieving personalised care using the Care Plan Template. However, in residential facilities that do not use an integrated resident record system, nurses must update the specific interventions section in the care plan following MDT review. In updating the interventions required, it is not necessary for nurses to re-write all the MDT instructions given. However, MDT reviews must be referenced in the interventions and a copy of the instructions where appropriate should be attached to the care plan. For example, if a resident is seen by a dietitian and detailed instructions for care are given, the care plan interventions need simply record ‘refer to dietitian’s instructions’ and a copy of the dietitian’s instructions should then be attached to the care plan. This will reduce fragmentation of care and ensure that nurses assuming the care of a resident, know exactly what the MDT plan of personalised care is for that specific resident. It is vital to note, the most important part of care provision is that care planning discussions with the resident and/or their significant other(s) has taken place, with an emphasis on goal setting, equal partnership, negotiation and shared decision making4. 5 Section 2 2.1 Personalised Care Planning using the DML Integrated Minimum Data Set The DML Integrated Minimum Data Set is made up of Resident Assessment Instruments (RAIs), Resident Assessment Protocols (RAPs), Personalised Care Planning (based on Protocols of the Expected Standards in Care) and sample care plans. These instruments are guided by professional standards of practice, regulatory requirements and clinical judgement 1, 5, 6, 7, 8 . 2.2 Resident Assessment Instruments (RAIs) The Resident Assessment Instruments are a minimum data set (MDS)9. They ensure that staff collects the minimum, necessary, standardised assessment information for each resident on admission, when the resident’s conditions improves or deteriorates, and at a minimum three monthly. This allows a personalised care plan to be developed and reviewed, based on the individual’s needs, strengths and preferences. However, the Resident Assessment Instruments (RAIs) alone will not provide a comprehensive assessment of all aspects of a resident’s needs. They can be considered as a preliminary screening tool in identifying actual or potential needs. 2.3 Resident Assessment Protocols (RAPs) In certain areas, residents may require further in-depth assessments so that an appropriate plan of personalised care can be developed according to the resident’s needs, preferences and strengths. Resident Assessment Protocols (RAPs) have been designed to meet this need7. They are problem-orientated assessment frameworks which outline the need for additional assessments7. The RAPs are triggered by the symbol when completing the RAIs. In planning personalised care, it is essential that causes or unique risk factors for decline or lack of improvement in the individual are identified. Once identified, the plan of personalised care should address these factors with the goal of promoting the resident’s highest level of functioning, health and well-being. 6 2.4 Layout of the RAPs There are 22 RAPs developed which cover the majority of areas likely to be addressed in a resident’s care plan. RAP 1: RAP 2: Communication, Vision and Hearing RAP 4: Cognition and Acute Confusion RAP 6: Nutritional Status RAP 8: Urinary Incontinence and Continence Promotion RAP 10: Constipation RAP 12: Impaired Ability for Personal Care RAP 14: Skin and Wound Care RAP 16: Activities RAP 18: Disturbed Sleep and Rest RAP 20: MRSA RAP 22: Palliative Care for All RAP 3: Mood and Behaviour RAP 5: Breathing and Circulation RAP 7: Dehydration and Fluid Maintenance RAP 9: Faecal Incontinence and Continence Promotion RAP 11: Falls Prevention and Risk Reduction RAP 13: Pressure Ulcer Prevention and Management RAP 15: Psychosocial Well-being RAP 17: Pain RAP 19: Psychotropic Drug Use RAP 21: Feeding Tubes End of Life Care 7 There are 7 parts to the RAP and Personalised Care Planning Instrument: 1. Definition 2. RAI Identifiers of Potential Risk 3. Risk Factors (intrinsic & extrinsic) 4. Further Assessment 5. Referrals Required 6. Personalised Care Planning 7. Protocols of Expected Standards in Care 8. Sample Care Plan 2.4.1 Definition This provides a definition or description of the identified need, condition, risk or problem affecting the individual. 2.4.2 RAI Identifiers of Potential Risk In the RAIs, the symbol (followed by a number) identifies a potential or actual problem or need that requires further RAP assessment and investigation by the multidisciplinary team. The multidisciplinary team (MDT) includes the resident and their significant other(s), carers, nurses, doctors and allied health professionals. Following RAP assessment, the MDT can determine if a plan of personalised care is needed or on the most appropriate plan which incorporates the resident’s, needs/ strengths and preferences. For example; in the RAIs, if 12 is ticked, this indicates that RAP 12: Pressure Ulcer Prevention and Management has been triggered. The assessor should now refer to this specific RAP for further assessment protocols required in planning appropriate multidisciplinary personalised care. In the RAPs, RAI identifiers of potential risk are listed followed by their corresponding RAI Section letter and number. This identifies where in the RAI the specific RAP was triggered. It is important to note the specific resident’s RAI identifier of potential risk that triggered the RAP in planning personalised care. For example, in RAP12: Pressure Ulcer Prevention and Management, the ‘RAI Identifiers of Potential Risk’ lists ‘Total Assistance required in Repositioning J 4’ and an ‘Inability to Mobilise Independently C11’. This means that when the assessor is completing Section C- Initial Admission Assessment and number 11 is ticked to indicate the resident is dependent in mobilising, RAP 12 is triggered. The assessor should refer to RAP 12 for further assessment protocols while being cognisant of this specific trigger (resident mobility dependence), so that an appropriate plan of personalised can be developed. Similarly, if J4 is ticked indicating the resident requires total assistance in repositioning, RAP 12 is triggered. Again, the assessor should refer to RAP 12 for further assessment protocols while being cognisant of this specific trigger (total assistance required in repositioning) in developing a personalised care plan with the resident and their significant other(s). 8 2.4.3 Risk Factors (intrinsic & extrinsic) This section provides information for evaluating further risks that are not listed in the RAI instrument. These risk factors may cause, contribute to, or exacerbate the problem or need identified. By assessing the risk factors that may contribute to the resident’s problem, the assessor may identify: • Associated causes and effects. Sometimes problems (e.g. constipation) may have a single cause (e.g. inadequate fluid intake). However, more often they have several causes (e.g. new drug, immobility, lack of privacy concerns, etc) • Multiple triggered conditions are related e.g. Vision and Falls • A need for obtaining further information on the resident’s condition from the resident or their significant other(s) or from the multidisciplinary team • A need for expert referral (e.g. Clinical Nurse Specialist in Older Persons Care for Behaviour that Challenges or Psychiatry of Later Life referral) • The basis for care plan goals and specific interventions required for personalised care 2.4.4 Further Assessment This section details further assessments that are needed to undertake a comprehensive assessment of the resident’s needs, which may include multidisciplinary team referral and review. The information listed in the ‘Further Assessments’ section is used to structure and guide the assessment process, so that information needed is not missed. When reviewing the ‘Further Assessments’ section, staff should consider the specific resident’s RAI trigger(s) that caused the RAP to be reviewed. This focuses the review on pertinent information that helps the assessor and multidisciplinary team to determine the nature of the problem identified and to decide if a care plan is necessary or what types of interventions are appropriate. Staff, together with the resident/significant other(s) where possible, then decide whether or not the triggered condition affects the resident’s functional ability or well-being and refer to the Protocols of Expected Standards for Care, if a care plan is warranted. Staff should document key findings following RAP review in the resident’s narrative notes. 2.4.5 Referrals Required Multidisciplinary referrals that may be required in assessing, evaluating and managing a particular resident problem or need are listed under this heading. 2.5 Personalised Care Planning The aim of personalised care planning is to develop a single multidisciplinary tailor-made plan of care to address the individual’s problem(s), concerns or needs and their associated causes or risks. The multidisciplinary team (MDT) includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. This section of the RAPs provides problem-orientated care frameworks for deciding on appropriate personalised interventions for care. Care plan development is centred on discussion with the resident and/or their significant other(s) where possible, to determine their preferences and goals; the best available evidence; MDT review and clinical judgement. Nursing staff should refer to: the resident/significant other(s), the Protocols of Expected Standards for Care and to the Multidisciplinary Team’s specific instructions, when planning appropriate personalised care. This ensures that a single, overarching plan of personalised care is delivered to the resident. 9 2.6 Documenting Personalised Care Planning A Care Plan Template is provided in The DML Integrated Minimum Data Set and Resident Care Record for documenting the resident’s plan of personalised care. The headings on the template include: Topic Heading, Problem/Need Identification, Specific Interventions and Evaluation of Care. 2.6.1 Topic Heading The topic heading outlines the resident’s problem or need. 2.6.2 Problem/Need Identification The resident’s identified problem/need is recorded as an actual or potential problem/need and its associated or related risk factors are documented. 2.6.3 Goal specification The MDT goals of care are recorded. It is important that goals are specific, measurable, achievable, realistic, and time-oriented. The goals of care must reflect the resident’s/family’s care choices and wishes. 2.6.4 Specific Interventions The specific interventions needed to address the resident’s problem or need are recorded under this heading. These specific interventions are based on expected standards of care, the outcome of the MDT RAP review and discussion and clinical judgement. In simple terms, the specific interventions section should address: i. Interventions needed: What we need to do to address the problem, risk or concern. These should include specific MDT interventions based on residents/significant other(s) concerns and care choices, where possible ii. On-going reassessments: What we need to monitor iii. Communication: What, to whom and when we need to communicate back to the MDT/resident/significant other[s] iv. Education: What and who we need to educate/provide information/health promotion advice to in order to improve the problem/need/concern When writing specific personalised interventions in the resident’s care plan, the Protocols of Expected Standards for Care should be reviewed and the following headings used. (Remember the MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals) Record: 1. Specific MDT Interventions to address the resident’s/significant other(s)’ concerns, preferences and care choices 2. Specific MDT Interventions to address the problems or risks identified 3. Monitoring and ongoing reassessments 4. Communication required 5. Information/education/health promotion required 10 2.6.5 Evaluation of Care Personalised care plans should be evaluated when the resident’s condition improves or deteriorates and at a minimum of 3-monthly. A record should be maintained in the “Evaluation of Care” section on the Care Plan Template of all MDT reviews that fall outside the routine 3-monthly reviews, e.g., when the resident’s condition improves or deteriorates or is re-assessed. The Three Monthly Reassessment Form should be used when routinely evaluating resident’s MDT personalised care plans. Three monthly reviews of personalised care plans should be a planned event and where possible an appointment should be made with the resident/significant other(s), to discuss and evaluate their personalised care planning and delivery. 2.7 Protocol of Expected Standards for Care The Protocols of Expected Standards for Care have been developed in a flow chart format and are based on the best available evidence, expert and peer review. These Protocols can be used to assist healthcare professionals, carers, residents and their significant other(s) in making decisions about appropriate treatments for specific conditions and aspects of care. 2.8 Sample Care Plan Generic or Personalised Under specific RAP headings, sample care plans are provided. These are presented in personalised and generic formats. 11 References 1 HIQA (2009) National Quality Standards for Residential Care Settings for Older People in Ireland 2 Department of Health and Children (2009) Health Act 2007 (CARE AND WELFARE OF RESIDENTS IN DESIGNATED CENTRES FOR OLDER PEOPLE) REGULATIONS 2009 3 Department of Health and Children (2010) HEALTH Act 2007(CARE AND WELFARE OF RESIDENTS IN DESIGNATED CENTRES FOR OLDER PEOPLE) (AMENDMENT) REGULATIONS 2010 4 Department of Health UK (2009) Supporting people with long term conditions: commissioning personalised care planning - a guide for commissioners. Accessed on line at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_093354 5 An Bord Altranais, (2000) The Code of Professional Conduct for each Nurse and Midwife, An Bord Altranais, Dublin. 6 An Bord Altranais, (2000) Scope of Nursing and Midwifery Practice Framework, An Bord Altranais, Dublin. 7 An Bord Altranais, (2002) Recording Clinical Practice Guidance to Nurses and Midwives, An Bord Altranais, Dublin. 8 An Bord Altranais, (2009) Professional Guidance for Nurses working with Older People, An Bord Altranais, Dublin 9 Challis., D., Stewart, K., Strudy, D., Worden, A. (2000) UK Long Term Care Resident Assessment Instrument User’s Manual MDS/RAI UK, interRAI UK, York, UK. 12 Section 3 Resident Assessment Protocols 13 RAP 1: 14 RAP 2: Communication, Vision and Hearing RAP 4: Cognition and Acute Confusion RAP 6: Nutritional Status RAP 8: Urinary Incontinence and Continence Promotion RAP 10: Constipation RAP 12: Impaired Ability for Personal Care RAP 14: Skin and Wound Care RAP 16: Activities RAP 18: Disturbed Sleep and Rest RAP 20: MRSA RAP 22: Palliative Care for All RAP 3: Mood and Behaviour RAP 5: Breathing and Circulation RAP 7: Dehydration and Fluid Maintenance RAP 9: Faecal Incontinence and Continence Promotion RAP 11: Falls Prevention and Risk Reduction RAP 13: Pressure Ulcer Prevention and Management RAP 15: Psychosocial Well-being RAP 17: Pain RAP 19: Psychotropic Drug Use RAP 21: Feeding Tubes End of Life Care RAPS Authors Introduction to the DML MDS Linda McDermott-Scales, R.G.N., Post RAP 1: Communication, Vision and Hearing RAP 2: Mood and Behaviour RAP 3: Cognition and Acute Grad Cert Neurological /Neurosurgical Nursing, H Dip Tissue Viability, MSc Nursing. DML Services for Older Persons. Julie Byrne, R.G.N., R.M., CNM2, Education Officer, Cherry Orchard Hospital Edel Carey, RGN, H-Dip L.D., PD / B.C.P, CNS Behaviours that Challenge, Cherry Orchard Hospital Orla Canning, R.G.N., H. Dip Gerontology, Confusion RAP 4: Breathing and Circulation CNS Dementia, Cherry Orchard Hospital RAP 5: Nutritional Status RAP 6: Dehydration and Fluid Linda McDermott-Scales Maintenance RAP 7: Urinary Incontinence and Continence Promotion RAP 8: Faecal Incontinence and Continence Promotion RAP 9: Constipation RAP 10: Falls Prevention and Risk Reduction RAP 11: Impaired Ability for Personal Care RAP 12: Pressure Ulcer Prevention and Management RAP 13: Skin and Wound Care RAP 14: Psychosocial Well-being RAP 15: Activities Anne Marie Payne, R.G.N, Nurse Tutor, St. Mary’s Hospital, Phoenix Park. Linda McDermott-Scales Linda McDermott-Scales Olivia Flattery, R.G.N, Practice Development, James Connolly Hospital Linda McDermott-Scales Olivia Flattery Linda McDermott-Scales Debby Dowd, R.G.N., CNM2, James Connolly Hospital Mary Doyle, R.G.N., R.P.N., R.M., H. Dip Gerontology, CNS Older Persons Peamount Hospital Nicole Nolan, R.G.N., DML Services for Older Persons Linda McDermott-Scales Linda McDermott-Scales Carol Byrne, R.G.N., CNM2 Balltinglass District Hospital Caroline Doran, R.G.N., CNM3, Meath Community Unit Arnel Kidpalos, MSc, H Dip, BSc, R.G.N., RAP 16: Pain RAP 17: Disturbed Sleep and Rest RAP 18: Psychotropic Drug Use RAP 19: MRSA RAP 20: Feeding Tubes RAP 21: Palliative Care for All RAP 22: End of Life Care R.N.T, EdD student, Nurse Tutor- Gerontology, Our Lady's Hospice Ltd. Caroline Doran Luzviminda Montejo, R.G.N., CNM2, Tara Care Centre, Putland Road, Co. Wicklow. Arnel Kidpalos Linda McDermott-Scales Nicole Nolan Anne Murphy, R.G.N., H Dip in Wound Management, H Dip Gerontology, CNS Older Persons Care, Cherry Orchard Hospital Nicole Nolan Nicole Nolan 15 Expert Reviewers • Michelle Bonner, CNS Palliative Care, Bray Palliative Care Team • Sonia Jeffery, CNS Palliative Care, Bray Palliative Care Team • Hazel Bailey, CNS Palliative Care, Bray Palliative Care Team • Mary Gregan, CNS Palliative Care, Bray Palliative Care Team • Dr. Seamus O’Dea, Medical Superintendent, Cherry Orchard Hospital • Dr. Eleanor McNamara, Consultant Microbiologist, Public Health Laboratory, Cherry Orchard Hospital • Laura Dillon CNS Infection Control & The ICS • Gillian O’Brien, CNS Tissue Viability, Naas General Hospital • Fiona Concannon, CNS Tissue Viability, Dublin North East • Mary Doherty, Tissue Viability Nurse, Cherry Orchard Wound Clinic • Mairead Murray, TVN, Midlands • Mary Kehoe, Senior Dietician DML, Clonskeagh Hospital • Grainne Flanagan-Rughoobur, Senior Dietician DML, Mullingar • Anne O’Sullivan, CNM2, A & E Department, Royal Victoria Eye & Ear Hospital • Maeve Murphy, Chairperson of IASLT • Aidan Lawlor ADN, RPN, CBT, St. Loman’s Hospital • Jeremey Jeffreys CNS Behaviour • Continence Promotion Unit, Dr. Stevens Hospital • Lynne Robb, CNS Pain Management and the Pain Nurses at St James’s Hospital • Jean Dunne, RGN, Social Worker, Quality Standards and Governance, HSE DML • Fiona Lyons, Social Worker, Cherry Orchard Hospital • Eimear O’Dwyer, MPSI, Chief II Pharmacist/Supervising Pharmacist, Our Lady’s Hospice Ltd 16 • Alma Joyce, Occupational Therapist Manager, Dublin South City • Pamela Ennis, Occupational Therapist, Meath Community Unit RAP 1: Communication, Vision and Hearing Definitions: Communication is a process, involving a minimum of two people and encompassing any means by which individuals relate experiences, ideas, knowledge and feelings. Communication is the means by which people connect socially, and ensures a person is not isolated. Communication can be verbal (through words) or non-verbal (e.g. gestures/sign language). To communicate effectively, your communication partner must understand your mode of communication.1 Impaired Communication: Decreased, delayed or absent ability to receive, process, transmit and use a system of symbols.2 Expressive Aphasia: is the loss of ability to verbally, express oneself.3 Receptive Aphasia: is the loss of ability to understand language.3 Dysarthia: is a language disorder in which there is difficulty in articulating words due to motor speech impairment.3 Visual Impairment: is a change in the amount or patterning of incoming stimuli, accompanied by a diminished, exaggerated, distorted, or impaired response to such stimuli.2 Hearing impairment: is a change in the amount or patterning of incoming stimuli accompanied by a diminished, exaggerated, distorted, or impaired response to such stimuli.2 Comatosed: Persistent vegative state/no discernable response. RAI Identifiers of Potential Risk: Resident requires an interrupter A11, Unable to express wishes A30, A31, Uses Assistive Devices/Communication Aids - hearing aid A49, I11, Spectacles A50, Communication Aids D5 Speech incoherent or other speech problems D1, Comprehension difficulties D3, Expressive difficulties D4, Inability to verbalise: pain D22, feeling hot or cold I11 Impaired hearing D6, D7, H3 Impaired Vision D8, H3 Restless/agitated (unable to communicate unmet need) D13, D14, History of Behaviour that Challenge (?unable to communicate unmet need) D16, Impaired Communication Skills M7 Other Risk Factors include: Sensory challenges involving hearing and/or vision, ear infection, ear wax accumulation, glaucoma, cataracts, diabetes mellitus, muscular paralysis and weakness, progressive physical, neurological, and psychiatric disorders. C.V.A, vascular dementia, receptive aphasia, expressive aphasia, dysarthia, structural problems e.g. tracheostomy, acute medical conditions e.g. urinary tract infection, pain, medication e.g. psychotropic drugs and narcotics, cultural differences e.g. (speaks a different language), dyspnoea, fatigue, fear/shyness, unfamiliar environment and faces. 17 Further Assessments: Document the following assessment on admission, after 5 days, if the resident’s condition improves or deteriorates and at least 3 monthly. NB: Please note: Prior to carrying out these further assessments ask the resident or their significant other about prior use of assistive devices. Ensure the resident is using these if applicable and that they are working properly. Assistive devices may include: spectacles, hearing aids, magnifying glass, writing pad and pencil, picture board and word/phrase card, assistive technology, including high tech communication devices. In undertaking further assessments of the resident’s communication ability, reduce background noise and ensure privacy. If the resident uses sign language or is an augmentative communication user (e.g. uses a computer or a picture board), ensure the person assessing him/her can use this system of communication or involve someone who can in the process (e.g. family member). Several sources of information should be used in assessing residents with communication difficulties. The resident should be the primary source of this information. However, where marked difficulties exist, significant others and carers will often know the most effective methods of communicating with the resident. Gather and document pertinent information about the resident’s usual mode of communication; this should include verbal / non verbal cues which the resident uses to identify their needs/wants. Assess the Resident’s: 1. Past and present medical history: for any suggestive or actual risk factors for communication. If the resident has already been seen by a Speech and Language Therapist (SLT), Audiologist and /or an Optician prior to admission, record the date of last review and list/attach their recommendations in their personalised plan of care. Consider the resident’s overall risk context for communication e.g. Physical, Neurological, or Mental health disorders, Memory loss, decreased attention span, expressive or receptive aphasia, visual or hearing impairment which may impact on the resident’s ability to communicate. Consider the resident’s medications for possible risks of over sedation, or side effects which may cause or exacerbate communication difficulties4. 2. Level of consciousness: Is the resident alert, orientated, confused, semi-comatose or comatosed? Review clinical records and activity of daily living assessments. 3. Cognitive patterns: conduct a brief interview for mental status (e.g. the Mini Mental State Examination [MMSE] ) 4. Behavioural patterns: behaviours that challenge are frequently the only way that residents have in communicating unmet needs5. Refer to RAP 2 for further assessments required. 5. Hearing: If applicable ensure the resident is using their hearing aid and that it is working correctly before attempting to assess hearing function. Record the use of hearing aids during assessment. Interview and observe the resident. 18 Ask the resident about their hearing function. Be alert to how you communicate with the person in order for them to understand. You may notice that you have to speak louder, more slowly and distinctly. You may have to use gestures or bring the person to a quieter environment. These cues should alert you to the resident having a hearing problem. Select the best description from the list below of the resident’s hearing pattern in the past five days: b) Adequate hearing. The resident has no difficulty in normal conversation, social interaction or in using the telephone. c) Minimal hearing difficulty. The resident finds it difficult to hear in a noisy environment. d) Moderate hearing difficulty. The resident finds it difficult to hear normal conversation. Their communication partner has to speak louder and more distinctly. e) Severe hearing difficulty. The resident demonstrates difficulty in hearing in all situations with an absence of functional hearing. f) No functional Hearing. Document Hearing Assessment findings in the Narrative Notes and ensure appropriate Multidisciplinary referral. 6. Speech Clarity: Select the best description from the list below to describe the resident’s speech pattern in the last 5 days. a) Clear speech. The resident demonstrates distinct intelligible words. b) Unclear speech. The resident’s speech is slurred or with mumbled words. c) Speech unintelligible to unfamiliar conversation partners but can but understood by familiar conversation partners e.g. family/friends d) Speech unintelligible to all listeners, including familiar partners e.g. family/friends e) Speech intelligible in quiet surroundings but poorly intelligible with background noise f) No intelligible speech in any environment. Document Speech Assessment findings in the narrative notes and ensure appropriate multidisciplinary referral. 7. Expression: Interact with the person, observe and listen to his/her attempts to communicate. If the person uses communication devices, encourage their use. These may include: a pad and pen, an alphabet board or a memory book. Record the type of communication device used during assessment. Note the presence of non verbal expressions; these may include e.g. blinking, hand squeezing or gesturing. Select the best description which most closely represents the resident’s ability to make them self understood over the last 5 days. a) Communication partner understands resident always, resident expresses ideas without difficulty b) Communication partner understands resident usually. Resident has difficulty finding words/finishing sentences but can achieve more success when prompted by listener 19 c) Communication partner understands resident sometimes. Resident can make basic needs known e.g. request a drink, but has difficulty with more complex language. d) Resident is rarely/never understood by communication partner. Document Expressive Assessment findings in the narrative notes and ensure appropriate multidisciplinary referral. 8. Comprehension: Interact with the person and consult with other members of the multidisciplinary team and the resident’s significant others. Select the description which corresponds to the most appropriate response for the resident. a) Always Understands. The resident clearly understands the speaker’s message. b) Usually understands. The resident misses some part or intent of the message but understands most of the conversation by responding in words or actions. c) Sometimes understands. The person has difficulty integrating information and responds adequately only to simple direct questions. d) Rarely/never understands. Document Comprehension Assessment findings in the Narrative Notes and ensure appropriate Multidisciplinary referral. 9. Vision: If applicable ensure the resident is using their spectacles before attempting to assess visual function. Record the use of spectacles during assessment. Introduce yourself. Provide adequate light. Always tell the resident with whom they are speaking and when you are moving away, so that they are not speaking to an empty space. Ask the resident if he/she is able to read newsprint, menus, etc. Be sensitive to the fact that some people have literacy difficulties or speech difficulties such as aphasia/dysarthia. To assess for distance visual acuity ask the resident to put on their distance glasses (if appropriate) i.e. what the resident wears for watching telly. If available use a Snellen chart. Check at 6 meters distance, cover one eye and ask the resident to read from the top. All lines on the chart have a number with 6 being the line a normal eye can see at 6 meters and 60 being the line a normal eye can see at 60 meters. The result is written as a fraction with the top number being the distance i.e. 6 and the bottom being the number being the line read. Thus if the result is 6/60 their vision is poor while if the result is 6/6 they have normal vision. If they cannot see the top line you should check if they can count fingers held about 18 inches in front of them or failing that if they can see the hand moving. If not can they distinguish a light shone in their eye. All would be sign of serious visual impairment. To assess near visual acuity, ask the resident to read aloud (if they are able to). Test one eye at a time (cover one eye). Wearing reading glasses (if appropriate), assess if the resident can read different levels of print at normal reading distance which is about 16 inches. Start with the larger print headings and end with the small print. Select the description which corresponds to the list below. e) No visual impairment. Resident sees fine detail including regular print in paper. f) Minimal visual impairment. Resident sees larger print in newspaper g) Moderate visual impairment. Resident is not able to see newspaper headlines but can identify objects 20 h) Severe visual impairment. Resident can not identify object in question but eyes appear to follow objects (especially people walking by). i) No Vision Document Visual Assessment findings in the narrative notes and ensure appropriate multidisciplinary referral. The first point of referral should be an optician as it may simply be a matter of getting new glasses. If there is a necessity to refer to an ophthalmologist the optician will advise. Referrals required: Refer the resident to the multidisciplinary team as appropriate to assessment findings. Referrals should be made as soon as concerns arise e.g. on admission/review. Record all referrals made on the MDT Referral Record. • Refer all residents with communication difficulties to their doctor for assessment and review of their medical condition and current medications. Discuss with the Doctor the resident’s current prescribed medications which may be impacting on the resident’s ability to communicate. • Hearing impairment: minimal, moderate, severe hearing impairment or resident has no functional hearing - check when the resident was last reviewed by an audiologist. Refer residents who have not been reviewed within 1-2 years. Lost or malfunctioning hearing aids - Refer the resident to an audiologist. Some residents who are profoundly deaf may use sign language. It may be necessary to access a certified sign language expert particularly when attempting to get informed consent and for the resident to receive or impart other important medical information. • Speech impairment: speech unclear or resident has no speech. Refer the resident to the Speech and Language Therapist – or make contact with the person’s Speech and Language Therapist if currently under the care of one. • Expressive/comprehension impairments: usually understands, sometimes understands or rarely/never understands- Refer the resident to the Speech and Language Therapist – or make contact with the person’s Speech and Language Therapist if currently under care the of one. • Visual impairment: minimal, moderate, severe or vision absent - check when the resident was last reviewed by an Optician. Refer residents who have not been reviewed within the last 1-2 years. Lost or malfunctioning spectacles – refer the resident to an Optician. • Behavioural Problems: It is essential that any resident who demonstrates challenging behaviour is appropriately assessed - Refer to RAP 2 for the appropriate care and onward referrals required. • Cultural: language barriers/foreign language; access a certified Interpreter to validate information from both sides of dialogue. Interpreters can be sourced through the Interpreting Services (check with Management for the company used). 21 Personalised Care Planning The aim of care planning is to develop a single multidisciplinary MDT plan of personalised care to address the causes or risks of communication difficulties, where possible. The MDT includes the resident/significant other(s), nurses, doctors, carers, and allied health professionals. Problem/Need Identification Record the actual or potential Communication difficulty and its associated or related risk factors. For example; ‘Mary is aware that her hearing has recently deteriorated and reports, “Both ears are bad at the moment. I get this a lot. It’s the wax”. Mary has moderate hearing impairment associated with cerumen build up.’ Or ‘Mary reports “My eyesight is not what it should be, that’s what diabetes does to you”. Mary currently has minimal visual impairment and is at risk of further impairment related to Diabetes associated Macular Degeneration’. Goal Specification Record: realistic, measurable and obtainable goals. For example: ‘To dissolve the plug of ear wax in Mary’s ear and restore her hearing to its normal level within 1 week’ Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential communication, vision and hearing problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: a. Document the specific interventions required to address the resident’s/significant other(s)’ concerns, preferences and care choices e.g. when communicating with a person in a wheelchair, speak directly with the resident not the person pushing the wheel chair. If possible get down to the level of the chair and establish eye contact e.g. by sitting on a chair. b. Document the MDT specific care instructions. This includes the nursing care instructions for addressing and managing impaired communication, vision and hearing and other instructions from the multidisciplinary team, e.g. a speech and language therapist’s specific instructions for communicating with a resident with dysthartia. These should be listed here or a photocopy attached to the care plan. It is important to refer the reader to the attached instructions. The same applies to all instructions from other members of the multidisciplinary team. 22 For residents with Communication difficulties: i. Document the information obtained from the resident/significant others and carers in the development of personalised care plans for effective communication. Detail the verbal/non verbal cues which the resident uses to identify their needs/wants e.g. indicators for thirst, toilet, etc. ii. Document the calming interventions that carers/significant others found most helpful to the resident if they became frustrated in attempting to get their needs across. This includes the sources of comfort/types of reassurance liked. iii. Encourage the use of charts, models and pictures to illustrate messages if appropriate. iv. Maintain eye contact with the resident when communicating. Use gestures and facial expressions to get your message across effectively. v. Be aware of memory impairments, if memory is impaired constant repetition may be required. vi. Pay attention to non verbal cues, encourage the resident’s attempts to communicate vii. Reduce environmental distractions such as TV and radio that compete for attention when conversing with the resident. viii. For identified Hearing and Vision impairments. Ensure all residents assistive device needs are documented to maintain/improve/promote independence e.g. spectacles, hearing aid, memory boards, picture cards. ix. In conversation with residents with expressive dysphasia, avoid verbal testing or questioning beyond the person’s capacity. Give the person ample time to respond. Listen attentively; clarify your understanding of the resident’s communication with the resident or with their significant other if difficulty persists. x. Acknowledge that communication may be a frustrating/difficult experience for both of you. If you need to, take a break to give both of you a short ‘time out’. xi. Do not make assumptions that the resident who has difficulties comprehending language does not understand anything. Explain instructions/ideas simply using jargon free, short sentences and visual aids such as pictures or diagrams. xii. Medication: Some medications e.g. aspirin quinidine, some chemotherapeutic agents and the amino glycosides are known ototoxic agents. If a hearing impairment is noticed after any of these drugs have been commenced, the doctor should be informed as withdrawal of these drugs often allows return to full hearing. 2. Monitoring & Ongoing reassessment: • For residents with cognitive impairment the MMSE should be repeated not less than 3 monthly or if deterioration in the resident’s cognitive status is suspected. Compare their current MMSE score with previous scores, act on findings which are of concern e.g., onward referral to doctor for medication review/CNS in Dementia for further assessment. Refer to Rap 3: Cognition and Acute Confusion. • Ongoing reassessment using a validated tool e.g. HADS should be recorded at least 3 monthly for residents who show signs of depression, anger or withdrawal as these are common responses to communication difficulties. Act on findings, refer to doctor for medication review, CNS in behaviours for further assessment. Refer to Rap 2: Mood and Behaviour. • Conduct regular pain assessments using the Abbey /or Universal Pain Scale Tool. Act on findings. Refer to Rap 16: Pain Assessment and Management • Enquire about and/or observe for signs of infection e.g. eye lid inflammation /discharge, earache /discharge, dizziness. Check ears for ear wax accumulation. Act on findings, refer to doctor. • Monitor the resident’s compliance with the use of assistive devices. 23 3. Communication: • Promptly communicate monitoring concerns to the resident’s doctor and appropriate members of the MDT e.g. SLT, CNS. Update care plan accordingly. • NOTE: Residents MUST BE referred back to the multi-disciplinary team if there is any deterioration in their communication ability despite following MDT advice /instructions. • Communicate the resident’s personalised care plan to all those involved in the residents direct care. Ensure that the resident/significant other(s)/visitors are encouraged to use assistive devices. Ensure the resident /significant other(s) are kept up to date. 4. Information/Education/Health Promotion for the resident, Significant other(s) and care staff. • Educate the resident /care staff on the use and care of assistive devices e.g. hearing aids. Check for age, condition, functional batteries and wax impaction of the equipment. • Provide training for all staff/family members on communicating with people with aphasia. • If a resident uses alternative or augmentative communication such as, sign language or a communication device, make sure staff are all trained in how to communicate effectively with the person. • Demonstrate the proper administration of eye/ear drops or ointments. Allow for return demonstration by resident/care staff. • Teach standard precautions in infection control in relation to maintaining sterility of all eye /ear droppers, medication tubes. • Encourage residents with communication difficulties to socialise with family and friends. Suggest that care staff, significant other/family and visitors engage the resident for short periods at a time and continue talking even if the resident does not respond. • Provide answers and helpful suggestions for what is known while not providing false assurances. • Contact the National council for the blind, Whitworth Road, Drumcondra, Dublin 9. Lo-Call 1850 334353 e-mail info@ncbi.ie or The Irish deaf society, National Association of the deaf, 30 Blessing ton Street, Dublin 7. Phone: 01 8601878. e-mail www.deafhear.ie, www.try-it.ie or www.atdementia.org.uk for up to date information on technical assistive products and services. Evaluation of care (based on goals specified) • Communication care plans must be evaluated when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking if the goals of care are being met e.g. the resident is negotiating their environment safely and participating in ADLs to maximum their potential. • Ensure the resident can use their assistive devices appropriately and effectively. If they are not using their assistive device, discuss with them the reasons for this. • Evaluate if the resident is socialising with family/friends. Refer to the ‘Protocol of Expected Standards for Care’ flow chart and sample ‘Personalised Care Plans’ in documenting personalised care planning and in providing care. 24 25 • • • • • • • • • • • • • • • • • • • Nursing Assessment-Document Past medical history/Co-Morbidities. Risk Factors. Communication abilities /deficits Pain assessment. Cognitive ability assessment. Behaviour and Mood pattern. Expressive language assessment. Comprehension of language assessment. Vision assessment (using his/her spectacles if applicable. Hearing assessment (using his/her hearing aid if applicable). Consider the impact of Psychotropic/Narcotic medications. Acute Infections e.g. U.T.I. Resident’s cultural beliefs. Resident’s/Significant others main concerns. Further Assessments MDT Assessments. Referrals required for e.g. Speech & language therapist, CNS in Dementia/ Behaviour that challenges/ Older Persons Care, Psychiatrist, Audiologist, Optician, Doctor. Assistive device Needs. Dignity, respect and privacy requirements. (On admission, if resident’s condition improves Or deteriorates and at least 3 monthly) Nursing Assessment Reassess when there is a change in the resident’s condition and at a minimum every 3 months. No difficulties in communication identified 1. Identify cause if possible & risk level. 2. Develop a MDT Personalised communication care plan. Difficulty in communication identified Nursing Diagnosis 1. Resident/Significant other discussion in the care planning process where possible 2. The identified resident’s problem(s) / need(s) 3. The resident’s identified Goals of Care 4. The specific interventions including verbal and non-verbal cues. 5. The MDT management plan for any risks identified. Consider MDT referrals required & made & specific communication instructions. 6. Pain risk, refer to RAP 16 7. Psychotropic drug risk, refer to RAP 18. 8. Cognition deficit or acute confusion, refer to RAP 3. 9. Behaviours that challenge risk, Refer to RAP 2. 10. Consider environmental distractions and reduce/remove same. 11. The appropriate assistive devices identified/required. 12. Provide education to residents/significant others & carers on specific communication instructions & on the use & maintenance of assistive devices & on accessing further information from e.g. The National Council for the blind ,or the National association for the deaf. 13. Monitor & address residents/Significant others concerns in relation to communication difficulties. Implement a Communication Care plan Document: Nursing Care Goals & Planning Reassess: Refer back to the MDT should difficulties in communication persist or increase. Goals unmet or Condition Changes Goals met • Resident/carer aware of appropriate communication measures & involved in communication decisions. • Continue with current communication care plan. Measure outcome against specified goals Nursing Evaluation Protocol for Expected Standards in Communication in HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: Communication Care Plan PROBLEM / NEED IDENTIFICATION Number: Date Signature 01/01/10 Mrs Breen’s hearing has recently deteriorated associated with cerumen build up. Mary reports “I can’t hear what you are saying as my ears are full of wax.” Patricia Clarke GOAL SPECIFICATION To dissolve the plug of wax in Mary’s ears and thereby restore her ability to understand speech within 1 week. GOAL SPECIFICATION Date 05/01/10 Signature • • • • • • • • • • • Refer Mary to the doctor for assessment to confirm a plug of ear wax has formed and to prescribe an appropriate ear wax softener. Explain and discuss the procedure with Mary and get her verbal consent to the administration of ear wax softener. Consult her prescription chart and administer the drop(s) as per best practice guidelines as outlined in the Medication Policy. Observe Mary for signs of dizziness, and/or disequilibrium after instilling the ear drops. Reduce background noise when speaking to Mary. Speak distinctly adjusting tone appropriately; use touch to indicate your presence as Mary may not hear you approach. Mary has been given information on the symptoms of ear infection e.g. pain, itchiness, and/or purulent discharge and has been requested to report any symptoms immediately. Monitor effectiveness of treatment. Ask Mary if she can hear her radio, TV, etc and adjust the volume as required. Ask the doctor to re-examine Mary’s ear drum after 5 days to check if the plug of earwax is dissolving & seek Mary’s opinion on her hearing status Mary’s Significant/other / Family/ Visitors & Care Staff have been advised to approach Mary from the front and lightly touch her arm to make her aware of their presence, reduce background noise, speak slowly & clearly & let her know when they are moving away so that she doesn’t continue to speak when they have gone. Communicate monitoring concerns promptly to the Doctor. Patricia Clarke EVALUATION OF CARE (based on goals specified) Date Signature Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 26 Suggested further reading: HSE, (2009) Regional Guidelines for Communication in Older Persons Residential Care Facilities in Dublin Mid-Leinster References 1 Mc Intyre, A. and Atwal, A. (2005) Occupational Therapy and Older People, pages 187192, Blackwell Publishing, Oxford, England. 2 Nanda definition, accessed at http:www.us.elsevierhealth.com/MERLIN/Gulanik/index.cfm?plan=11 3 Zaretsky, H., Richter, E. and Eisenberg, M. (2005) Medical Aspects of Disability, 3rd Edition, A Handbook for the Rehabilitation Profession. Pages 292-293, Springer Publishing, New York. 4 Challis, D., Stewart, K., Sturdy, D., Worden, A., (2000) interRAI UK Long Term Care Resident Assessment Instrument User’s Manual MDS/RAI UK. The JRW Group, Gatley, Cheadle, Cheshire SK8 4BE 5 Kitwood, T, (1997), Dementia reconsidered, the person comes first, p.136 27 RAP 2: Mood and Behaviour Definitions: Mood is a person’s state of mind or emotion. Behaviour is the action or reaction of a person to a stimulus. Stimulus is something that directly or indirectly causes a response in the individual e.g. stimuli can be internal (pain due to infection) or external such as from sound or touch (sense organs). Behaviour that challenges is described as “Behaviour of such an intensity, frequency or duration that the physical safety of the person or others is likely to be placed in serious jeopardy, or behaviour which is likely to seriously limit or delay access to and use of ordinary community facilities”.1 Glossary of terms:2, 3 Functional Analyses (F.A.): Are the observations taken to answer the question, why is the behaviour that challenges occurring. When obtaining information we look at defining the specific behaviour occurring, its rate, intensity or duration and establish a baseline through A-B-C recording (antecedent, behaviour consequence). Antecedent: is what the resident was doing immediately before the behaviour occurred. Behaviour: what the problem behaviour is, clearly define the behaviour. Consequence: what happened immediately after the behaviour occurred? Consider: how staff responded to the resident, what did the resident do? Correlation: a mutual relation identified between factors such as the time of day or specific activities where the incidence of behaviour that challenges occurs. RAI Identifiers of Potential Risk: Resident has behaviours that challenge C20, D15-20, Constipation G11, F23, Pain D22, Depression (mood decline) D11, F23, Altered cognitive state e.g. (confusion,) D11, D13, D14, Communication impairment, D1, D3, D4, D6, Malnutrition F1, Dehydration, F21 Disturbed Sleep Pattern/ Sleep Deprivation, C14, N8, N9, Psychological factors H5 Risk factors: Residents who have behaviours that challenge are often perceived by professionals as challenging. It must be remembered that this may be the resident’s only way of communicating their unmet needs. Risks include all the above RAI Identifiers and Organic disease, (Dementia, Infection, Cancer, Chronic pain), Confusion, Emotional trauma, ABI (acquired brain injury) Mental Health Problems (Delirium, Psychosis, Depression), Immunocompromised, Loneliness, Boredom, Response to environment, Communicative act, Interpersonal interactions, Learnt Behaviours. Further Assessments: The following assessments are to be carried out if the resident is identified as exhibiting behaviour that challenges, if the resident’s behaviour improves or deteriorates and at least two weekly. 1) Assess the resident’s usual behaviour pattern with their significant other(s) and staff working in the unit to establish a baseline. Several sources of information should be 28 used in assessing residents with behaviours that challenge, with the resident being the primary source for this information. However, where marked difficulties exist for residents in communicating their needs, their significant other(s) and carers will often know the most effective methods of communicating with the resident. Gather and document pertinent information about the resident’s usual mode of communication; this should include verbal / non verbal cues which the resident uses to identify their needs/wants. Refer to RAP 1: Communication, Vision & Hearing. 2) Assess for an underlying cause(s) for any new presentations of behaviours that challenge e.g. out rule the presence of: • Pain, use a validated tool to assess e.g. Abbey Pain scale or Numeric Pain Scale. Refer to RAP 16: Pain • Exacerbation of an underlying medical condition causing discomfort/pain e.g. angina, gastric ulcers, arthritis, etc • Constipation • Infection; observe for local/systemic signs and symptoms of infection. Assess vital signs, urinalysis, presence of a cough, etc. If indicated send appropriate samples to the lab for Culture and Sensitivity • Boredom and the need for occupation 3) Assess and observe for signs of agitation, confusion or memory decline using a validated tool e.g. Cohen Mansfield Agitation Inventory or the Mini Mental State Exam, MMSE. Refer the resident to the Doctor for further assessment if required and/or to a specialist in the area e.g. CNS, Psychologist, Psychiatrist as appropriate. 4) Assess nutritional status, refer to RAP 5, hydration status, refer to RAP 6 and constipation status, refer to RAP 9 5) Assess pertinent blood results. Refer to the doctor to reserve bloods for further assessment such as FBC, U&E, ESR etc. 6) Assess each episode of behaviour and or mood decline using a validated tool e.g. ABC Functional Analyses of Behaviour or the Hospital Anxiety and Depression Scale (HADS). Document each episode of behaviour in the accident / incident reporting form, in accordance with the designated centre’s policy. 7) Undertake a full risk assessment where indicated by the behaviour exhibited. Referrals Required: • Refer to the resident’s doctor for a medical assessment and full blood screen to assess for underlying infection and/or dehydration • Refer to the CNS behaviour (if available) or consider referral to the CNS dementia / CNS older persons care if present onsite • Refer the resident to the Occupational Therapist for further cognitive assessment if deemed appropriate • Refer the resident to the dietician if they are identified as being at risk of malnutrition or if malnutrition is evident • Refer the resident to the Physiotherapist for correct positioning to alleviate pain if evident • Refer the resident to the Speech and Language Therapist if communication difficulties are evident • Refer the resident to the Occupational Therapist/Activities Co-ordinator to assist in developing an appropriate, individualised activity/occupation schedule for the resident If behaviours persist consider making a referral to a consultant psychiatrist or to a psychologist. 29 Personalised Care Planning The aim of care planning is develop a single multidisciplinary (MDT) plan of personalised care to address the cause or risks of behaviour where possible. The MDT includes the resident / significant other(s), carers, nurses, doctors and allied health professionals. Problem/Need Identification Record the actual or potential behavioural problem and its associated or related risk factors. For example; “Mary has the potential to display episodes of verbal aggression related to an acquired brain injury or agitation associated with constipation”. Goal Specification Record: realistic, measurable and obtainable goals. For example: “To reduce the number of episodes of verbal aggression exhibited by Mary within a two-week period”. Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential behaviours that challenge. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) Note: The resident’s needs may be physical and/or psychological in nature and if unmet can result in the resident exhibiting the behaviour that challenges. The aim of care is evaluate the RAI Identifiers of Potential Risk that have been triggered during assessment and to consider other risk factors that might be causing the behaviours, so that successful interventions can be identified, implemented and alternate positive behaviours reinforced. Non-pharmacological interventions should be used first before medication in cases of behaviours that challenge4 1. Specific MDT interventions: Record: a) Accurate Assessment of behaviours that challenge: • Record and monitor resident’s behaviour using the ABC functional analyses (antecedent, behaviour, consequence) or the Cohen Mansfield Agitation Inventory. Document the time, location, triggers if noted and the type of behaviour exhibited. Analyse the information to ascertain if any precipitating factors exist, such as a correlation / emerging pattern between the times of day, certain activities, particular staff, etc when an incidence of behaviour that challenges occurs. • Consider: Many residents who experience altered cognitive state may have communication difficulties, thus exhibiting behaviours such as screaming or aggression. The behaviours may also be influenced by the interaction skills of staff • Risk assess the behaviour and implement appropriate risk management strategies e,g. Crisis Prevention Interventions techniques 30 b) Meet with the MDT (Doctor, Psychiatrist, Nurse, CNS, O.T., Physio, Social worker, Activity team, Dietician, Art therapist, Music therapist, Speech and Language therapist) resident and family to develop a multidisciplinary approach and personalised plan of care. c) Treat any identified underlying causes to behaviours such as infection, pain, etc, as directed by the Doctor. Monitor the effects of treatment on the outcome of behaviour. d) Implement a personalised activity schedule based on the information obtained in the meaningful activities assessment. e) Staff should familiarise themselves with the resident as a person, using the information obtained from ‘A Key to Me’, ‘My Day, My Way’ and the resident’s ‘Personal Calendar of Important Events’. Particular emphasis should be noted on the resident’s interests, likes and dislikes. This information may assist staff in de-escalating episodes of behaviours that challenges. 2. Monitoring & ongoing reassessment a) Continue to observe and monitor behaviour to establish a pattern, observing for any new behaviours presenting. Report findings to the MDT b) Document and monitor each episode of behaviours that challenge on the functional analyses form (See Appendix 1). c) Report behaviours that challenge on the Accident / Incident reporting form as appropriate and in accordance with the designated centre’s policy. d) Monitor interventions closely for effectiveness e) Monitor for any underlying causes to behaviour presenting and the treatment outcome. 3. Communication a) Promptly communicate any monitoring concerns to the resident’s doctor and MDT as appropriate. Discuss the issues arising or the need for new interventions. Update and implement personalised care plans accordingly. b) Note: residents MUST BE referred back to the multi-disciplinary team if there is deterioration in their Behaviour despite following behavioural interventions implemented by the MD team. c) Inform all staff of the incidence of behaviour at the commencement of each shift, including agency and relief staff. Ensure staff are aware of resident’s personalised care plan and are informed of any changes in the residents care at the commencement of each shift. d) Communicate with the resident’s significant others / visitors about the resident’s personalised plan of care and inform them of any changes and encourage their involvement. 4. Information / Education / Health promotion for Resident, Significant Other(s) and Carers a) Educate staff around behaviours that challenge. Identify to staff that these behaviours do serve a purpose to the resident who is exhibiting them. This will allow staff to gain an understanding and insight into the behaviour, thus assisting in the treatment outcome. b) Educate the resident’s significant other(s) to allow them to gain an understanding which may in turn alleviate anxiety or fears they may have about their loved one and encourage their involvement. Provide specific written information for them as appropriate. 31 c) Inform staff about the importance to always re-establish communication with the resident after behaviours that challenge are exhibited in a calm reassuring way. d) Educate staff to avoid revisiting the event with the resident, as the resident is unlikely to remember what has happened. This serves no useful purpose. Evaluation of Care, (based on goals specified) a) ‘Behaviour that challenges’ care plans must be evaluated at two weekly intervals. Evaluate the effectiveness of the interventions implemented (care provided) by assessing to see if the goals specified are being met e.g. reduction in the incidences of behaviour that challenge, improved interactions with fellow residents and staff, improved participation in activities of daily living, improvement in the resident’s or their significant other(‘s) self reported quality of life. b) When behaviours that challenge have faded out, observe for replacement behaviours and reinforce alternate positive behaviours. c) If the behaviour has not faded out, meet with the Consultant / Psychiatrist or Doctor to discuss the implementation of Psychotropic / Neuroleptic medication in conjunction with a personalised plan of care. Monitor closely for effects and side effects of medication used. Evaluate as required; “Each resident should benefit from their medication to increase the quality or duration of their life. They should not suffer unnecessarily from illness caused by the excessive, inappropriate or inadequate consumption of medicines”.5 Refer to the ‘Protocol of Expected Standards for Care’ flow chart and sample ‘Personalised Care Plans’ in documenting personalised care planning and in providing care. 32 33 • Past & present medical history including suggestive evidence of behaviours that challenge. • Commence Functional Analyses to determine & assess RAI identifiers / risk factors to behaviour exhibited. • Outrule acute confusional state, mood decline and any RAI identifiers, risk factors identified using a validated tool, continue with F.A. recording. • When / if identified treat causes e.g., pain, UTI. Monitor closely for treatment outcome. • Continue with F.A recording, analyse information to ascertain any precipitating factors, obtain information from resident and or significant other. • Continue to observe and assess behaviour, meet with MDT and family to develop a personalised plan of care incorporating a desired activity schedule, monitor closely. • Undertake a full risk assessment where indicated by the behaviour exhibited. Nursing Assessment-Document (On admission, if the resident’s condition improves or deteriorates and at two weekly intervals) Nursing Assessment Record: realistic, measurable & obtainable goals. For example: to reduce the number of episodes of verbal aggression exhibited within a Two-weekly period. Nursing Goal The resident demonstrates behaviour that challenges e.g. verbal aggression such as shouting & name calling in a threatening manner. Nursing Diagnosis • Accurate assessment: document time, location triggers if noted, type of behaviour. • Close observation of the behaviour is required while also observing for any trigger evident prior to the behaviour by using ABC functional analyses. • Inform all staff of the incidence of behaviour at the commencement of each shift. • Continuous monitoring of the behaviour and document clearly on the FA form and/or the Accident / Incident form in accordance with local policy. Analyse information. • Report findings to the multi-disciplinary team. • Obtain information from the resident /their significant other (s). • Ensure staff, familiarise themselves with the resident (use ‘A Key to Me’, ‘My Day, My Way’, ‘Personal Calendar of Important events’ ) • Meet with the MDT to develop a personalised plan of care incorporating a desired activity schedule, including information obtained. • Implement plan and monitor closely. • Educate staff and the resident’s significant other(s) on their personalised plan of care. • Note: residents must be referred back to the MDT before their scheduled evaluation date should there be a deterioration in their behaviour despite following interventions implemented by the MDT. Care Planning • Behaviour that challenge care plans must be evaluated at two weekly intervals. • Evaluate the effectiveness of the interventions implemented, (care provided) by assessing to see if the goal(s) specified are being met e.g. number of incidences reduced, improved social interactions, self reported improvement in quality of life. • When behaviours that challenge have faded out observe for replacement behaviours and reinforce alternate positive behaviours. • If the behaviour has not faded out meet with consultant / psychiatrist or GP to discuss the use of psychotropic / Neuroleptic medication in conjunction with personalised plan of care, Monitor closely for effects and side effects of drug (s) used, evaluate as required. Evaluation Protocol for Care for Behaviours that Challenge in HSE Older Persons Designated Centres SAMPLE CARE PLAN (to be reviewed in 3 months and re-written in 6 months) Topic Heading: Sample (Behaviour) Care Plan PROBLEM / NEED IDENTIFICATION Number: Date Signature 01/01/10 Mary displays verbal aggression related to acquired brain injury GOAL SPECIFICATION To reduce and / or fade out Mary’s episodes of verbal aggression by 2 weeks SPECIFIC INTERVENTIONS Date 05/01/10 Signature • • • • • • • • • • • • • • All staff must use the same firm approach with Mary when aggressive behaviour is exhibited. Do not respond back to any verbally aggressive statements/behaviours exhibited by Mary. Staff will react in a calm voice and attempt to redirect the conversation, (Use the information obtained in the “A key to Me” to redirect the conversation). Do not revisit the behavioural event, as Mary is unlikely to remember what has happened. This serves no useful purpose. Staff should re-establish communication with Mary after each episode has resolved Always explain to Mary any procedures staff wish to carry out. If Mary becomes agitated when staff are attempting to carry out a procedure walk away and approach again later if safe to do so. (within hour) Ensure routine medications are administered at the correct times. Refer to Mary’s preferred activities see Meaning Activities Care Plan. Mary particularly likes the rummage box and her life story being read to her. Allow time for the Mary to express herself e.g. anxieties, fears. Offer Mary reassurance and encouragement at all times. Monitor / observe and document any verbal/ non-verbal signs of aggression e.g. rigid body, clenched fists or verbally aggressive behaviour using a ABC Functional analyses form. Note any triggers evident prior to the behaviour. Document clearly any incidence of behaviours that challenge in incident / accident report book in accordance with hospital policy Refer Mary back to the MDT before her scheduled evaluation date should there be a deterioration in behaviour despite following interventions implemented by the MDT. Educate resident, significant other and family on interventions implemented Patricia Clarke EVALUATION OF CARE (based on goals specified) Date Time Signature Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 34 Appendix 1: ABC Functional analyses record form Target Behaviour: please complete each time the resident engages in a target behaviour i.e. (the specific behaviour). For example each time the resident is hitting out Time/ Date Antecedents (before) What did the resident do? Name of staff/other residents involved? Target Behaviour Consequences (What is the (After) problem behaviour- What did you do? describe) What did you say to the resident? What did the resident do? Staff please sign and print name 35 References 36 1 Emerson et al, (2000) “treatment and management of behaviours that challenge in residential”, journal of applied research in intellectual disabilities;13;197-215 2 Newman et al, (2003) Behaviour speak, A glossary of terms in applied behaviour analyses; 114-118 3 Miltenberger, R.,G, (2004), third edition, behaviour modification, principles and procedures; 4:71 4 National institute for clinical excellence and social care institute for excellence, (2006) Dementia: supporting people with dementia & their carers in health and social care 5 Health Information and Quality Authority, (2009) National quality standards for residential care settings for older people in Ireland RAP 3: Cognition and Acute Confusion Definitions: Cognition is defined as “the collection of mental processes and activities used in perceiving, remembering, thinking, and understanding, as well as the act of using these processes.” 1 Acute confusion, also known as delirium, is generally a sudden onset of confusion or sudden worsening of a person’s existing confusional state. Delirium is defined as “a transient disorder of cognition and attention accompanied by the sleep-wake cycle and psychomotor behaviour”2 Many residents with acute confusion may have associated cognitive deficits such as altered perception (including hallucinations, illusions and delusions); sleep disturbances; memory loss; language deficits; inattention; altered level of consciousness, disorientation/disorganised thinking; difficulty with calculations, abstraction, insight, judgement and mood disorders e.g. fear, elation, anxiety or depression. Residents with dementia such as vascular, lewy-body, frontal temporal (Picks) and mixed (vascular and Alzheimer’s) dementia may also present with acute confusion. Vascular dementia that presents with a sudden onset of acute confusion, may be associated with a further vascular event occurring. With lewy-body, frontal temporal and mixed dementia, the resident may have a fluctuating decline in cognition and confusion. It is essential not to treat signs of acute confusion as a natural progression of the resident’s dementia. Delirium/acute confusion is a medical emergency. RAI Identifiers of Potential Risks: ■ Constipation G11 ■ Cognitive impairment D3, D4, D11, D13, D14, ■ Hallucinations/delusions D21, ■ Depression N8, ■ Dehydration F21, ■ Malnutrition F1, ■ Vomiting and/or diarrhoea F23, ■ Communication impairment D3, D4 ■ Pain D22 ■ Disturbed Sleep Pattern/Sleep deprivation N9. Other Risks include: ■ Hypoxia, ■ Infection/pyrexia, ■ hyper/hypo glycaemia, ■ Physical restraints, ■ Psychological factors ■ Urinary/chest infection ■ Advanced age ■ Dementia ■ New/unfamiliar environment ■ Alcohol addiction ■ over medication/drug toxicity ■ mental health illness ■ Reduced renal function ■ Post surgery ■ Trauma i.e. head injury following fall ■ Acute stress ■ Immuno-compromised ■ Sensory overload/ deprivation ■ Isolation ■ Relocation ■ Recent loss/bereavement Risk factors for some residents may be compounded further by their inability to give an accurate account of their symptoms associated with their memory problems or cognitive impairment. Therefore it is important for nurses to carefully observe for all triggers and risk factors. Further assessments If a resident is identified as being acutely confused, the following assessments should be carried out. The resident should be reassessed when their confusion improves or deteriorates, and at least once weekly. 37 1. Carry out a health and safety risk assessment to identify any potential risks posed to the acutely confused resident, other residents and staff members. 2. Assess the resident’s falls risk using a validated tool e.g. FRASE (refer to Rap 10: Falls Prevention and Risk Reduction). 3. Assess the resident’s cognition using a validated tool e.g. MMSE 4. Establish the resident’s baseline cognitive status by obtaining information from people who are familiar with the resident e.g. the resident’s significant other(s), carers and staff. 5. Assess for signs and symptoms of infection e.g. urinalysis, assess vital signs and temperature four hourly. 6. Assess the resident’s pressure ulcer risk using a validated tool e.g. Braden (Refer to Rap 12: Pressure Ulcer Prevention and Management). 7. Assess for signs and symptoms of constipation (refer to RAP 9: Constipation). 8. Assess for signs and symptoms of dehydration (refer to Rap 6: Dehydration and Fluid Maintenance) 9. Assess for signs and symptoms of malnutrition (refer to Rap 5: Nutritional Status) 10. Assess for swallowing difficulties which may pose a risk for aspiration. 11. Assess for signs and symptoms of pain (refer to Rap 16: Pain). 12. Assess current medications with the doctor and/or pharmacist as a contributory factor to the resident’s acute confusion (refer to Rap 18: Psychotropic Drugs). 13. Assess each episode of acute confusion using a validated behaviour assessment tool and record e.g. using a mood and behaviour assessment tool (refer to Rap 2: Mood and Behaviour). Referrals required: Referrals should be made as appropriate to assessment findings • Refer to the Doctor promptly for a general physical examination to outrule an underlying pathological cause for the resident’s acute confusion • An onward referral may be required for a psychiatry review if the resident is depressed or anxious and/or has had a recent bereavement • Refer to the doctor and pharmacist for a medication review • Refer to the dietetic services if the resident is at risk of/or has malnutrition • Refer to the physiotherapist if the resident is hypoxic; for recommendations on correct positioning if pain is present and/or for a mobility/gait assessment • Refer to the speech and language therapist for a swallow/communication assessment as appropriate • Refer to Activities for recreational activities • Refer to the Occupational Therapist if the resident has any additional seating/comfort requirements • Refer to the Social Work Department if the resident has had a recent bereavement or loss and/or is struggling to come to terms with their environment • Refer to CNS’s (if available) for education and advice on appropriate management according to current best practice Personalised Care Planning The aim of care planning is to develop a single, multidisciplinary (MDT) plan of personalised care to address the cause or risks of acute confusion where possible. The MDT includes the resident and significant other(s), carers, nurses, doctors, and allied health professionals. 38 Problem/ Need identification Record the actual and /or potential problem and its associated or related risk factors, e.g. Mary has a urinary tract infection and is acutely confused, possibly related to an inadequate oral fluid intake Goal specification Record realistic, measurable and obtainable MDT goals e.g. Mary will drink at least 1.5 litres of oral fluids daily. Mary’s UTI will be resolved within 7 days. Mary’s MMSE score will return to her baseline of 18/30 Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential cognition and acute confusion problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions a) The specific interventions to address the resident’s /significant others concerns, preferences and care choices e.g. A significant other’s concern for the resident’s acute confusion can be addressed by effectively communicating and incorporating their input into the care planning process. b) Specific MDT care instructions: This includes nursing care instructions and other care instructions from members of the MDT e.g. doctors instructions; dietician’s specific instructions on diet and fluids; physiotherapist instructions; CNS instructions. These instructions should be listed here or a photocopy attached to the care plan. It is important to refer the reader to the attached instructions. The specific MDT instructions required will be specific to the underlying cause of the acute confusional state. General interventions include: • Document all incidents of acute confusion using a behaviour diary. Complete an Incident/Accident report form, if required. • Gently orientate the resident to time, place and person, incorporating information obtained from ‘A Key to Me’. • Implement CPI training techniques as deemed appropriate, for the management of agitation and aggressive outbursts. 2. Monitoring and ongoing reassessment: • Monitor the resident’s vital signs at least four hourly • Monitor and reassess the resident’s confusion, mood and behaviour on a Mood and Behaviour Diary. • Continue to monitor and record the resident’s cognition once a week using a validated tool e.g. MMSE. • Monitor for signs of UTI each time the resident passes urine. Note the urine colour, approx volume, presence of malodour, and pain on urination. Check urinalysis and send a urine specimen to the lab for culture & sensitivity if appropriate. 39 • • Monitor for signs and symptoms of dehydration. Maintain a fluid intake and output chart for at least 7 days. Monitor for signs and symptoms of malnutrition and implement interventions as appropriate (Refer to RAP 5- Nutritional Status) 3. Communication: • Communicate any monitoring concerns to the MDT e.g. if the resident’s confusion is worsening. • Communicate the resident’s personalised care plan with all those involved in the resident’s direct care. Ensure the resident and their significant other is kept up to date with the resident’s personalised care plan and with any improvement/deterioration in the resident’s confusion. Ensure that the significant other(s) are involved in and are in agreement with the resident’s plan of care. • Residents must be referred back to the MDT if there is any deterioration in the resident’s acute confusion despite following MDT advice/instructions. 4. Information/ Education/ Health Promotion for resident, significant other and carers • Provide information/education to the resident/significant other(s) and carers on the cause of the resident’s acute confusion, their plan of care and on appropriate strategies in dealing with acute confusion Evaluation of care (based on goals specified) • The personalised plan of care for the resident with acute confusion must be evaluated when the residents confusion improves or deteriorates, and at least once weekly. Evaluate the effectiveness of the interventions provided by assessing to see if the goals of care are being met e.g. is confusion level minimising? Is the MMSE score increasing? Is the resident drinking at least 1.5 litres of fluids daily? Are we providing a safe environment for the resident? • If the resident’s confusion levels are not resolving, refer back to the doctor for further diagnostic assessment and to other members of the MDT, as appropriate. Refer to the ‘Protocol of Expected Standards for Care’ flow chart and sample ‘Personalised Care Plans’ in documenting personalised care planning and in providing care. 40 41 • Past & present medical history including suggestive evidence of previous episodes of acute confusion • Assess the resident’s cognition using a validated tool. Check usual pattern of cognition / confusion with resident’s next of kin, significant other(s) to obtain a base line • Outrule mood decline and treat any RAI identifiers of Potential Risk or other risk factors • Assess for an underlying cause e.g. infection, pain, constipation, dehydration use a validated tool where appropriate • Carry out a health & safety risk assessment to identify any potential risks posed to the acutely confused resident, other residents, visitors & staff • Assess the residents falls risk using a validated tool • Assess current medications with the Doctor and / or the pharmacist which may be a contributory factor to the acute confusion • Assess each episode of acute confusion using a validated tool Nursing Assessment-Document (On admission, if resident’s condition improves Or deteriorates and at once weekly intervals) Nursing Assessment Record: Realistic, measurable & obtainable goals. Nursing Goal Record the identified problem, e.g. acute confusion related to a UTI Nursing Diagnosis Document: • The specific interventions required in the treatment and management of the underlying cause of the acute confusion • Record all incidents of acute confusion using a Behaviour Diary. Complete an Incident/Accident form if appropriate • Document appropriate risk management strategies • Gently orientate the individual to person, place & time. Use the information obtained in the ‘Key to Me’ or the resident’s ‘Life Story’ to assist in re-orientating • Explain any procedures before carrying them out • Monitor vital signs & temperature four hourly • Monitor and reassess the resident’s confusion, mood & behaviour • Monitor for signs and symptoms of local/ systemic infections • Monitor urinary output on an intake/ output chart • Monitor bowel elimination • Monitor for signs & symptoms of dehydration • Monitor for malnutrition • Monitor risks for resident/visitors and staff • Communicate promptly any monitoring concerns to the MDT • Inform the resident/significant other of any proposed changes to their individualised care plan & keep of any improvement and / or deterioration in confusion levels Care Planning • Acute confusion care plans must be evaluated at once weekly intervals • Evaluate the effectiveness of the interventions implemented • If the residents confusion levels are not resolving, refer back to the Doctor for further diagnostic assessment • Refer back to the MDT as appropriate Evaluation Protocol for Care for Acute Confusion in HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: Acute Confusion Care Plan PROBLEM / NEED IDENTIFICATION Number: Date Signature 21/01/10 Mary has a urinary tract infection and is acutely confused, possibly related to an inadequate fluid intake. GOAL SPECIFICATION Mary will be provided with at least 1.5litres of fluids daily. Mary’s UTI will be resolved within 7 days. Mary’s MMSE score will return to her baseline of 18/30. SPECIFIC INTERVENTIONS Date 21/01/10 Signature • • • • • • • • • Administer Ipral 200mgs at 08:00hrs and 18.00hrs daily for 7 days as prescribed. Encourage Mary to drink at least 1.5litres of oral fluids every 24hrs. Maintain a fluid balance chart for 7 days, record the drinks offered/refused and those taken. Mary only likes to drink tea and warm 7UP. Monitor Mary’s urinary output each time she passes urine (note the colour, volume, malodour and assess Mary for any pain on voiding). Document all incidents of acute confusion on a Mood and Behaviour Diary and complete an Incident/Near-miss report form, if required. Record Mary’s vital signs and temperature at least 4 hourly. Gently re-orientate Mary to time, place and person when she is confused. Use the information obtained in the ‘A Key to Me’ document to assist in re-orientating and in communicating with Mary when she is confused. Mary particularly likes talking about her family and looking at their photographs. Always explain any events/interventions/procedures to Mary prior to carrying them out Communicate any concerns regarding Mary’s care promptly to the doctor and other relevant members of the MDT. Inform Mary and/or significant other of any changes to Mary’s individualised plan of care and of any improvement and/or deterioration in confusion levels. Patricia Clarke EVALUATION OF CARE (based on goals specified) Date Time Signature Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 42 References 1 Ashcroft, M, H (2006) Cognition. Fourth Edition: 11. 2 WebMD, (2008) Confusional states and acute memory Disorders. http: // emedicine.medscape.com/article/1135767-overview 43 RAP 4: Breathing and Circulation Definitions: The Cardiovascular System includes the heart together with two networks of blood vessels; these are the systemic circulation and the pulmonary circulation. The cardiovascular system effects the circulation of the blood around the body, which brings about transport of nutrients and oxygen to the tissues and the removal of waste products via arteries and veins. Diseases affecting the cardiovascular system are many and can cause significant morbidity and mortality particularly for older people. Cardiovascular disease (CVD) including coronary heart disease (CHD), Heart failure (HF), stroke (CVA), Peripheral Vascular Disease (PVD) and other circulatory diseases accounts for the most common cause of death in Ireland.2 Because CVD is frequently associated with life-style related atherosclerotic changes, much emphasis is now placed on preventing its occurrence and progression. The aim of which is to modify risk factors, such as: in the treatment of hypertension, controlling cholesterol levels through healthy eating, exercise and/or medication, avoidance of smoking and stress reduction.3 The Respiratory system involves the combination of organs and tissues associated with breathing. It includes the nasal cavity, pharynx, trachea, bronchi, bronchioles, lungs, pleural cavity and the diaphragm, nerves and other muscles associated with breathing movements.4 Diseases affecting the respiratory system range from mild and self-limiting such as a common cold (Respiratory Tract Infection), to life-limiting conditions such as Chronic Obstructive Pulmonary Disease (COPD) or Restrictive Lung Diseases, to life-threatening conditions such as bacterial pneumonia. Modifiable risk factors in the prevention and treatment include: healthy eating, exercise, avoidance of smoking and vaccination (pneumonia/flu). COPD: is a group of respiratory diseases characterised by airway obstruction. The main obstructive airways diseases include: Chronic bronchitis and its subgroup bronchiolitis; Bronchiectasis; Asthma; and Emphysema. Restrictive Lung Diseases: are a group of lung diseases that restrict lung expansion resulting in a decreased lung volume, an increased work of breathing, and inadequate ventilation and/or oxygenation.5 RAI Identifiers of Potential Risks: ■ Has not received Flu / Pneumococcal vaccines A61, A62, ■ Pursed Lipped Breathing E1, ■ Abdominal Breathing E1, ■ Changes in Breathing Pattern E2, ■ Difficulty associated with Breathing C19, E4, ■ History of smoking E7, ■ Trachyeostomy E5■ Cough Present E8, ■ Lower Extremity Oedema E9, ■ Differences in Temperature in Lower Extremities E9, ■ Palliative Care Symptoms of Dyspnoea, Cough, Noisy Breathing, Fatigue O6, ■ End of Life Care Symptoms of Dyspnoea, Cough, Noisy Breathing, Fatigue P5. Other Risk Factors include: 1. Risk Factors and Causes of Respiratory Disease include: a) COPD this includes: • • 44 Chronic bronchitis (associated with hyperplasia and hypersecretion of mucus glands) caused by tobacco smoking and/or air pollutants. Bronchiolitis (associated with inflammatory scarring and bronchiole obliteration) caused by tobacco smoking and/or air pollutants. • • • Emphysema (associated with airspace enlargement and wall destruction) mainly caused by tobacco smoking. Asthma (associated with smooth muscle hyperplasia, excessive mucus and inflammation) results from immunologic or idiopathic causes. Bronchiectasis (dilation and scarring of airways) results from persistent severe infections. b) Restrictive Lung Diseases Causes/risks include 1. Pulmonary fibrosis and hypersensitivity pneumonitis caused by inhalation of environmental or occupational pollutants/allergens e.g. • • • • • • • • Asbestosis (asbestos dust). Silicosis (silica dust [pottery]). Silo-filler’s disease (toxic gas inhalation). Farmer’s Lung (inhalation of thermophilic actinomycetes from fresh-cut hay). Bird Fancier’s Lung (inhalation of avian proteins from bird droppings or feathers). Mushroom Worker’s Lung (inhalation of thermophilic actinomycetes from Mushroom compost). Peat moss worker's lung (caused by Monocillium sp. and Penicillium citreonigrum found in peat moss). Chemical Worker's lung (caused by Trimellitic anhydride found in plastics, resins, and paints). 2. 3. 4. 5. 6. Acute Respiratory Distress Syndrome. Inflammatory Diseases such as sarcoidosis, rheumatoid arthritis. Radiation fibrosis. Certain drugs such as amiodrone, methotrexate, opiates. Neuromuscular disease such as quadriplegia, multiple sclerosis, motor neuron disease, polio and post polio syndrome. 7. Musculoskeletal and chest wall deformities such as kyphosis, severe scoliosis, kyphoscoliosis, kyphosis, fractured ribs. 8. Idiopathic causes. Other risks include: tracheostomy, impaired swallow and aspiration risk (dysphagia/ impaired cough/gag reflex) and bed bound residents. c) Signs and Symptoms of Respiratory Disease These differ depending on the disease. Common symptoms include: • • • • • • General malaise. Shortness of breath or dysponea which usually occurs with exercise and can interfere with daily activities. In severe cases, shortness of breath can occur while resting (Orthopnea). Cyanosis, a bluish discoloration of the lips, tongue or fingers. Abnormal pulse oximetry, peak flow recordings. Cough with or without the production of sputum. Coughing blood (haemoptysis). 45 • • • • • • Chest pain. This may or may not be pleuritic chest pain (that is, pain that worsens with the movements of breathing). Noisy breathing, either wheeze or stridor. Fatigue. Loss of appetite. Weight loss. Cachexia. In some cases respiratory disease is diagnosed without symptoms in the investigation of another disease or through a routine check. 2. Risk Factors for Cardiovascular Disease include: There are many risk factors associated with cardiovascular disease. The major risk factors include: tobacco use, alcohol use, high blood pressure (hypertension), high cholesterol, obesity, diabetes, physical inactivity and unhealthy diets. Old age, gender (men), family history of CVD, ethnic origin (African or Asian ancestry are at higher risks of developing cardiovascular disease than other racial groups), poverty, chronic stress, social isolation, anxiety and depression increases the risk of CVD. Certain medicines such the contraceptive pill and hormone replacement therapy may also increase risks.6 Lower Extremity Peripheral Vascular Disease (PVD) Risk Factors: a) Risk factors for Peripheral Arterial Disease (PAD) include diabetes, hypertension, hyperlipedemia, stroke, transient ischaemia attack, myocardial infarction, angina, intermittent claudication, smoking, a history of arterial surgery and previous or present leg ulceration. b) Risk factors for venous hypertension include multiple pregnancies, Deep Venous Thrombosis, obesity, occupation (standing for long periods), a history of varicose veins, phlebitis, vein surgery or sclerotherapy, fracture, immobility and a family history of leg ulcers or previous/present leg ulceration. Other risks include a history of Intravenous Drug Abuse.7, 8 Cardiovascular Disease Signs and Symptoms9 1. Signs and Symptoms of Coronary Artery Disease • • • • • • • 46 Angina (may be described as a discomfort, heaviness, pressure, aching, burning, fullness, squeezing, or painful feeling in the chest, shoulders, arms, neck, throat, jaw, or back. Pain may mimic heartburn.; fullness, indigestion, or choking feeling). Dyspnoea. Palpitations, arrhythmias and ECG abnormalities. Tachycardia. Weakness or dizziness. Nausea. Sweating. 2. Symptoms of a Myocardial Infarction (MI) Symptoms of a MI typically last 30 minutes or longer and are not relieved by rest or oral medications, these may include: • • • • • • • Chest pain- usually with same distribution as angina above. Atypical pain can also be a feature. Acute shortness of breath, abnormal pulse oximetry recordings. Sweating, nausea, vomiting, or dizziness. Extreme weakness, anxiety, or a sense of impending doom and a feeling of being acutely ill. Tachycardia, arrhythmias and ECG abnormalities. Loss of consciousness. Some people have no signs or symptoms- silent MI. 3. Symptoms of Heart Valve Disease Symptoms may include: • • • • Dysponea which increases with exercise or when lying flat (Orthopnea), abnormal pulse oximetry recordings. Weakness, dizziness or confusion. Chest discomfort with activity or when going out in cold air often described as a feeling of pressure or weight. Palpitations. Valve disease can cause heart failure 4. Symptoms of Heart Failure Symptoms of heart failure can include: • • • • • • • • • • Dysponea-shortness of breath noted during activity (most commonly) or at rest, especially when lying flat (Orthopnea) or paroxysmal nocturnal dysponea (a sudden night-time attack of severe breathlessness, usually several hours after going to sleep also known as ‘Cardiac Asthma’). Cyanosis in late stages due to left-sided heart failure and pulmonary oedema. Abnormal pulse oximetry recordings. Cough that is productive of a white mucus. Quick weight gain due to fluid retention (a weight gain of two or three pounds in one day is possible). Oedema (peripheral-ankles, legs, and ascites-abdomen) associated with right-side heart failure. Nocturia may be a feature due to fluid returning from the legs when elevated. Cool extremities at rest due to inadequate systemic perfusion. Dizziness, confusion due to inadequate systemic perfusion. Fatigue and weakness. Palpitations/Arrhythmias. Other symptoms include nausea, palpitations, and chest pain. Some people may have little or no symptoms yet have a severely damaged heart. 47 5. Symptoms of Heart Muscle Disease (Cardiomyopathy) Symptoms of cardiomyopathy can occur at any age and may include: • • • • • • Chest pain or pressure (occurs usually with exercise or physical activity, but can also occur with rest or after meals). Heart failure symptoms (see above). Oedema (lower extremities). Fatigue. Fainting. Palpitations/Arrhythmias/ECG abnormalities 6. Symptoms of Pericarditis When present, symptoms of pericarditis may include: • • • • • Chest pain. This pain is different from angina. It may be sharp and located in the centre of the chest. The pain may radiate to the neck and occasionally, the arms and back. It is made worse when lying down, taking a deep breath in, coughing, or swallowing and relieved by sitting forward. Dry cough. Fatigue and anxiety. Low-grade fever. Tachycardia. Further assessments Document the following Assessments on admission, if the resident’s condition improves or deteriorates and at least every three months. 1. Consider the resident’s specific risk factors, modifiable risks and previous cardio/pulmonary history. 2. Assess vital signs, weight, BMI and urinalysis and Finger stick blood sugar (document on the Vital Signs, Blood Sugar, Weight, BMI and Urinalysis Chart). 3. Assess if and when Influenza and Pneumococcal vaccine have been administered. 4. Breathing Assessments: • Observe for shortness of breath, wheeze/ stridor or pain while: – Speaking – Eating – Drinking – Exertion – Mobilising – Sleeping / lying flat • Observe the character/type of resident’s breathing pattern. • Assess for the presence of a cough/sputum. • Measure Peak Flow to establish a baseline of the person’s peak expiratory flow rate. • Measure Pulse Oximetry on room air to establish a baseline. Acceptable normal ranges are from 95 to 100 percent. N.B: the limitations of pulse oximetry must be noted. These include: 48 • ➢ Inaccurate recordings due to: – Probe movement e.g. resident shivering or tremor present. – Nail varnish obliterating probe from detecting a pulse. – Room temperature and resident temperature: An environment that is too cold will cause the arterioles to constrict and decrease the blood flow through the digits. – To correct, ensure the resident is warm and any nail varnish removed or rotate the finger probe so that it does not cover the nail. Prevent the resident’s digit from moving during recordings. ➢ Hypoventilation and oxygen therapy; a person suffering from hypoventilation (i.e. poor gas exchange in the lungs) given 100% oxygen can have excellent blood oxygen levels while still suffering from respiratory acidosis due to excessive carbon dioxide. ➢ Insufficient blood flow/anaemia: – If there insufficient haemoglobin in the blood (anaemia), tissues can suffer hypoxia despite high oxygen saturation in the blood. – If there is insufficient blood flow e.g. very ill residents with low BP and poor peripheral perfusion, the finger probe frequently will not pick up a pulse and oximetry reading cannot be recorded. ➢ High blood levels of methemoglobin. Methemoglobin is a form of haemoglobin that cannot carry oxygen. Normally one to two percent of people's haemoglobin is methemoglobin; a higher percentage than this can be genetic or caused by exposure to various chemicals and depending on the level can cause health problems known as methemoglobinemia. A higher level of methemoglobin will tend to cause a pulse oximeter to read closer to 85% regardless of the true level of oxygen saturation.10 Observe the resident’s mucous membranes and nail beds for signs of cyanosis (blueness/greyness). 5. Circulatory Assessments: a) Observe for shortness of breath dysponea, orthopnea, paroxysmal nocturnal dysponea, presence of cyanosis, fatigue, dizziness, confusion. Measure pulse oximetry. b) Observe for dry cough, white sputum. c) Assess for the presence of chest pain, type and characteristics (Refer to RAP 10: Pain). d) Observe pulse for arrhythmias, note: rate, rhythm & volume. e) Assess for presence of palpitations, oedema (peripheral or systemic). In heart failure peripheral oedema is bilateral. 6. Lower Extremity Circulatory Assessments:11 • Assess the resident’s lower extremities for signs and symptoms that are indicative of peripheral arterial disease (PAD): – Observe resident’s extremities note their colour, shape and their temperature. Consider if the temperature is equal between the two extremities. Ensure that both the resident and their environment are warm; a cold environment can cause vasoconstriction in the lower extremities. Note whether feet are cold, pale or blue. 49 – Assess the skin; is it shiny and taut? Note if there are areas of hyperpigmentation (brown staining), presence of varicose veins, and/or eczema. – Assess for blackened or gangrenous toes. – Assess capillary refill in the toes by pressing gently on the nail beds and releasing. Nails beds turn white or blanch when pressure is exerted and resume their normal pink colour within 3 seconds (capillary refill). – Palpate pedal pulses. – Assess for signs of oedema. Note if oedema is bilateral or unilateral. – Calf measurements. – Assess for pain- note the type and nature of the resident’s pain. • Pain Indicative of Arterial disease: • Intermittent claudication on exercise (complaints of pain on walking usually located in the back of the calf muscles, thigh muscles or buttocks, relieved in seconds by ceasing walking). • Relieved by rest. • Rest pain, relieved when foot is placed on the floor (dependent). • Pain Indicative of Venous Disease: • Pain at ulcer site. • Aching or heavy legs. • Night cramps. Indicative of PAD, findings may include: • A pale, cool foot with shiny, hairless skin, thickened toenails and an absence of palpable pedal pulses, delayed capillary refill greater than 3 seconds, intermittent claudication or rest pain and a positive Buerger's Test. To assess using the Buerger’s Test the resident must be supine. Note the colour of the feet/soles. They should be pink. Then elevate both legs to 45 degrees for more than 1 minute. Observe the soles. If there is marked pallor (whiteness), ischemia should be suspected. Next check for rubor on dependency. Sit the resident upright and observe the feet. In normal circulation, the feet quickly turn pink; with arterial insufficiency dependent rubor occurs, this is where the limb presents as ruby red in a sitting position. Indicative of Venous disease, findings may include: • The presence of: varicose veins, brown skin staining, eczema, lipodermatosclerosis (presence of hard woody-type tissue), leg shape (leg of mutton / inverted champagne bottle, shaped leg), ankle flare, atrophe blanche (white spots/areas of avascularisation), oedema, foot pulses present and complaints of night cramps or restless legs. Indicative of Mixed Arterial/Venous lower extremity disease a combination of the sign and symptoms of both arterial and venous disease are present. Oedema Measurements 50 2mm or less = 1+ Oedema 2-4mm= 2+ Oedema ✓ Slight pitting ✓ No visible distortion ✓ Disappears rapidly ✓ Slightly deeper pit ✓ No readable detectable distortion ✓ Disappears in 10-15 seconds 4-6mm = 3+ Oedema ✓ Pit is noticeably deep ✓ May last more than 1 minute ✓ Extremity looks fuller & swollen 6-8mm = 4+ Oedema ✓ Pit very deep ✓ Last as long as 2-5 minutes ✓ Extremity is grossly distorted Referrals required: Refer to the Multidisciplinary Team as appropriate to the Assessment findings: • Doctor: referral is required for baseline assessment and for ongoing concerns e.g. abnormal vital sign measurements, abnormal blood sugars, abnormal character of breathing, shortness of breath, cough, cyanosis, signs/symptoms of Respiratory Disease, CVD, PVD, oedema, unequal calf-measurements, management of pain and for the presence of a leg ulcer. • Physiotherapy: e.g. Cough, decrease endurance, dizziness. • An urgent vascular referral is required for all residents presenting with rest pain or uncontrolled pain and gangrene. • A prompt vascular referral is required for all residents who present with signs/symptoms of PVD. All residents with PAD should be considered for revascularisation devices such as stents, irrespective of their age and co-morbidities. • All residents with lower extremity ulceration should be referred for a leg ulcer assessment by appropriately trained healthcare professionals (Refer to Rap 13: Skin and Wound Care). • Dietician referral may be required to optimise nutritional intake and to advise on appropriate diet e.g. cardiac diet, diabetic diet. • Podiatrist/chiropodist referral will be required for providing nail and foot care for residents with arterial disease. Personalised Care Planning The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care that is specific to the person’s difficulty with breathing and /or circulation. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. Need / Problem Identification Record the specific breathing/circulation problem that has been highlighted following a thorough assessment. This should be written as to address the person’s needs For example: Mrs Peacock states she can only walk a couple of yards and has to stop because of the pain in her right calf muscle. She also reports that her pain is getting progressively worse and that she now has intolerable pain in her right leg at night when she is in bed. Mrs Peacock has signs and symptoms of intermittent claudication, rest pain and progressive peripheral arterial disease. Goal specification Goal: state the desired resident outcome from the nursing interventions. The goal must be measurable, obtainable and reflect the resident’s/families’ desires as much as possible. For example: Mrs Peacock’s leg pain will be controlled to an acceptable level as identified through self reports. Mrs Peacock will have an urgent vascular referral within 1 week to determine her suitability for revascularisation options such as stenting. Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential cardiovascular / respiratory problems. Document: 51 • • • • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) What we need to monitor (on-going reassessments) What we need to communicate (back to the MDT) What/who we need to educate (to improve the problem) 1. Specific MDT interventions a) Specific interventions to address residents/significant other(s) concerns, preferences and care choices e.g. ‘a fear of breathlessness’. This can be addressed by providing psychological support and through education on appropriate MDT management strategies in improving/maximising respiratory status. b) MDT specific care instructions. This includes nursing care instructions for addressing the actual or potential cardiovascular / respiratory problem(s) and other care instructions from members of the MDT. For example: a doctor’s specific instructions for the management of the cardiovascular or respiratory problem. A physiotherapist’s instructions on improving lung capacity and/or the management of the resident’s symptoms. These should be listed here or a photocopy attached to the care plan. It is important to refer the reader to the attached instructions. 2. Monitoring and ongoing reassessment: The monitoring interventions required will be specific to the cardiovascular or respiratory problem identified. Monitoring is aimed at assessing the effectiveness of the treatment/management strategies and in identifying signs of disease progression and its impact on the resident’s life. 3. Communication: • Promptly communicate monitoring concerns to the resident’s doctor and appropriate members of the MDT team. Update care plans accordingly • NOTE: Residents MUST BE referred back to the multi-disciplinary team if there is deterioration in their cardiovascular / respiratory status despite following MDT advice/instructions. • Communicate the residents personalised care plan to all those involved in the resident’s direct care. Ensure the resident’s and their significant others (if the resident so wishes) are aware of the resident’s plan of personalised care and are kept up to date. 4. Information/ Education/ Health Promotion for resident, significant other and carers • Educate residents/significant other(s) on the resident’s specific type of cardiovascular / respiratory problem and their personalised plan of care. Provide written information where possible and/or provide information in a format that suits the resident’s communication requirements. Refer to RAP 1: Communication, Vision and Hearing. Evaluation of care (based on goals specified) • Cardiovascular / Respiratory Care plans must be evaluated when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking to see if the goals of care are being met. e.g. improvement in self reported symptoms and in resident’s self reported quality of life. Refer to the protocols of ‘Expected Standards for Care Flow Chart’ and sample ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. 52 Protocol for the Expected Standards of Care in the Assessment of Breathing and Circulation in Older Persons Designated Centres Does this person have a history breathing and or circulatory problems/ difficulties? Complete admission assessment No Yes Baseline assessment within normal limits No The person has difficulties with: Yes Circulation Both Breathing Assess Assess Assess for modifiable Risk Factors. Assess if & when flu/Pneumococcal Vaccines were given. Further assess: Smoking History Signs & Symptoms of CVD Lower extremities for Signs & Symptoms of PVD Continue to monitor. Requires monthly Observations Yes No. per day Expresses wishes to quit smoking Write a care plan focusing on the specific problem assessed with circulation and address modifiable risk factors Quit No No. of years ago Wishes to continue smoking- risk assess, offer options for smoking cessation Colour of Nail beds, Mucous membranes & skin Write a Plan of Care for the management of smoking/ smoking Cessation Changes in breathing pattern with activities of living Difficulty with inspiration, exertion, expiration, lying down Character of Cough & Pain Write a care plan focusing on the specific problem assessed with Breathing and address modifiable risk factors where possible Document implementation of the interventions on the appropriate Flow Chart or in the Narrative Notes Evaluate the effectiveness of your interventions by referring to the Goal set in the care plan. If the goal is being met continue the care as planned. If the problem is resolved discontinue the care plan, write a narrative note when the care plan is discontinued If the goal has not been met, establish new interventions based on evidence- based, best practice 53 SAMPLE CARE PLAN Topic Heading: Lower Extremity Circulation PROBLEM / NEED IDENTIFICATION Number: Date Signature 01/04/10 Mrs Peacock states she can only walk a couple of yards and has to stop because of the pain in her right calf muscle. She also reports that her pain is getting progressively worse and that she now has intolerable pain in her right leg at night when she is in bed. Mrs Peacock has signs and symptoms of intermittent claudication, rest pain, delayed capillary refill and progressive peripheral arterial disease. Jane Murphy GOAL SPECIFICATION Mrs Peacock’s leg pain will be controlled to an acceptable level as identified through self reports. Mrs Peacock will have an urgent vascular referral within 1 week to determine her suitability for revascularisation options such as stenting. SPECIFIC INTERVENTIONS Date 01/04/10 Signature • • • • • • • • • Mrs Peacock was seen by Doctor O’Brien on admission & commenced on prophylactic Statins therapy (Pravastatin 20ms daily) and antiplatelet therapy (low dose Asprin 75mg daily) according to best practice. Analgesia charted. Administer medication as prescribed.. Dr O’Brien sent an urgent vascular referral and a dietetics referral. While awaiting referral DO NOT apply elastic compression hosiery such as TED Stockings, as these will further reduce Mrs Peacocks arterial circulation Mrs Peacock is at high risk of foot and heel pressure ulcers. Use Heelift boots® while in the bed. Inspect feet daily for signs of pressure ulcer damage and record. Discourage Mrs Peacock from crossing her legs. Encourage Mrs Peacock to wear her soft zip-up slippers while mobilising. Discourage her from wearing her hard leather shoes as these are likely to cause a pressure ulcer. Encourage Mrs Peacock to mobilise as much as possible. Do Not elevate Mrs Peacocks’ legs while in the bed as this will reduce her circulation further and cause pain. If Mrs Peacock complains of right leg pain while in the bed, encourage her to hang her leg out of the bed, so that gravity can assist with her circulation. Review analgesia should this occur. Monitor and record the intensity of Mrs Peacock’s pain using the Numeric Rating Scale 0-10 (with 10 being the worst pain experienced) before and approx 30 minutes after drug administration. Monitor Mrs Peacocks lower extremities at each shift. Note: skin integrity, colour/warmth and capillary refill & document findings Communication: Promptly report monitoring concerns to the Doctor/MDT. Information: Provide information sessions to Mrs Peacock/Significant Others on the Plan of Care to address this problem. Jane Murphy EVALUATION OF CARE (based on goals specified) Date Time Signature Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 54 References 2 Irish Heart Foundation (2010), Facts on Heart Disease and Stroke http://www.irishheart.ie/iopen24/facts-heart-disease-stroke-t-7_18.html 3 Mackay, J., Mensah, G. (2004) Atlas of Heart Disease and Stroke. World Health Organization. Geneva 4 Oxford Medical Dictionary (2005) 7th Edition 5 Kanaparthi, L., Lessnau, K., Sharma, S. (2009), Restrictive Lung Disease, http://emedicine.medscape.com/article/301760-overview 6 J Mackay, G Mensah, (2004) Atlas of Heart Disease and Stroke. World Health Organization. Geneva 7 Meissner, M., Eklof, B., Smith, P., Dalsing, M., DePalma, R., Gloviczki, P., Moneta, G., Neglen, P., O' Donnell, T., Partsch, H., Raju, S. (2007) Secondary chronic venous disorders. Journal of Vascular Surgery, 46 Supplement:S68-S83. 8 Grey, E., Harding, K., (2006) ABC of Wound Healing, BMJ Books, Blackwell Publishing 9 WebMD (2009) Heart Disease Guide http://www.webmd.com/heartdisease/guide/heart-disease-symptoms?page=3 10 Denshaw-Burke, M., Savior, D., Schoffstall, J (2009) Methemoglobinemia, emedicine: http://emedicine.medscape.com/article/204178-overview 11 Kandarpa, K., (2007) Peripheral Vascular Interventions, Lippincott Williams & Wilkins, U.S.A. 55 RAP 5: Nutritional Status Definitions: Nutritional status is the state of a person’s health in terms of the nutrients in his or her diet.1 Malnutrition is a bodily state in which there is a deficiency of nutrients that causes measurable adverse effects on body composition, function or clinical outcome. The term includes under nutrition and over nutrition2, 3. The risk of under nutrition rather than over nutrition is the main cause of concern for older people in residential care.4 Malnutrition has a detrimental impact on a resident’s health and wellbeing, however once identified, it can be effectively treated.5 Body Mass Index (BMI): A measure of body weight relative to height used to determine whether people are underweight, at a healthy weight, overweight or obese.6 RAI Identifiers of Potential Risks: BMI less than 20 C1, Difficulties associated with eating C7, Communication Difficulties C6, D3, D4, Recent unexplained weight loss C9, F1, Modified Diet F5, Difficulties in Swallowing F22, Nausea/vomiting/diarrhoea F23, Presence of Wounds C10, J1, J7, Dietary restrictions C16, Functionally dependent F17, Breathing difficulties C19, E2, Dehydration F21, Potential risk of pressure ulcers J2, Palliative Care Symptoms present- sore mouth, nausea, vomiting, weight loss and anorexia O6, End of Life Palliative Care Symptoms- sore mouth, nausea, vomiting, weight loss and anorexia P5 Other Risk Factors include: • • • Pre-admission risks such as living alone, low income, limited mobility, lack of cooking/shopping ability and a lack of social support.7 On admission to residential care approximately 1 in 3 residents (30%) are at risk of malnutrition.8 Co-morbidities risks may include; behavioural problems, paranoia, depression, oral health problems, medication side effects/sedation and certain underlying medical conditions e.g. Parkinsons disease, dementia, Feeding, Eating, Drinking and Swallowing Disorders (dysphagia), CVA, episode(s) of acute illness (vomiting, diarrhoea, fever), neoplastic and respiratory disease.9 Post-admission risks may include; psychosocial causes e.g. resident’s individual food preferences, palatability (e.g. texture modified diets) and visual presentation of food offered, residents feeling rushed, cultural and religious factors. Biomedical risks include an exacerbation of the resident’s medical conditions and functional decline. Other post-admission risks may include inadequate care practices e.g. a lack of staff awareness of the need for nutritional assessments, poor/inadequate monitoring and documentation of those at risk/or with malnutrition, inflexible timing of meals, lack of assistance while eating.10, 11, 12 Further assessments Document the following assessments on admission, if the resident’s condition improves or deteriorates and at least three monthly: 1. Assess the resident’s past and present medical history for any suggestive or actual risk factors/co-morbidities for malnutrition and for Feeding, Eating, Drinking, and Swallowing Disorders (FEDS disorders/dysphagia). Several sources of information should be used in information/history gathering e.g. discussion with the resident significant 56 2. 3. 4. 5. 6. 7. 8. others, transfer letters, contact with/and discussion with the multidisciplinary team. This is especially important for residents with communication or cognitive difficulties. If the resident has already been seen by a Speech and Language Therapist (SLT) and/or a dietitian prior to admission, record the date of last review and list/attach their recommendations in the nursing care plan. Consider the resident’s medications for possible risks of over sedation or side effects which may cause or exacerbate malnutrition. Assess the resident’s dietary likes/dislikes, preferred portion size, dietary modifications and fluid consistency. Assess if the resident has any cultural or religious practices that might impact on dietary intake. Assess the resident for signs and symptoms of malnutrition e.g. thin/obese, weight loss, loose clothes, loose rings, muscle wasting, prominent bones, poor appetite, feeling cold, low energy levels. Assess and observe the resident for signs and symptoms of FEDS Disorders/dysphagia and associated anxiety/depression13 e.g. reported swallowing problems, drooling, coughing, choking and/or throat clearing when eating /drinking, wet voice after swallowing, recurrent chest infections, pocketing of food in the mouth, unexplained weight loss. Note: Up to 80% of older people may not seek treatment advice for dysphagia prior to admission.14, 15 This highlights the importance of observation in assessing residents. Assess the resident’s; functional ability to self feed, level of assistance required, appropriateness of usual position for eating, need for modified utensils to improve/maintain independence. If a resident is already using modified equipment, record the type used, in the assessment (RAI) and in their care plan. Complete a nutritional risk assessment using a validated tool e.g. MUST or MNA, Record the residents’ weight and BMI. If the resident is at risk or identified with malnutrition they are further at high risk of developing pressure ulcers. Assess the resident’s skin, checking pressure areas. Complete a pressure ulcer risk assessment. Refer to RAP 12: Pressure Ulcer Prevention and Management. Complete an oral cavity assessment and record the date of their last dental check-up. Referrals required: • • Refer the resident to the multidisciplinary team (MDT), as appropriate to their assessment findings e.g. Doctor referral for those identified with/or at risk of malnutrition/FEDS Disorders, Dietetic referral [see protocol below], SLT referral required for those identified with/or suspected of FEDS Disorders, OT/Physiotherapist referral required when advice on correct positioning for feeding/seating assessments are required and Dental referral may be required for oral health needs. Referrals should be made as soon as concerns arise e.g. on admission/review. Record all referrals made on the MDT Referral Record In facilities with no/limited access to SLT, consider the risk of aspiration and urgency for swallow assessment (for residents with suspected FEDS Disorders/Dysphagia). In HSE Units, contact: Resident’s Doctor /Senior Nursing Management/SLT Area Manager/Local Health Manager to arrange an urgent review or to decide on the transfer of the resident to an acute hospital if an urgent review is not possible. In private designated centres contact: Irish Association of Speech and Language Therapists in private practice (IASLTPP) 01-8787959 or IASLT at 085 – 7068707 57 • In facilities with no/limited access to dietetic services, consider the resident’s risk level and urgency of review required. In HSE Units, contact: Resident’s Doctor / Senior Nursing Management/Local HSE Dietitian or Dietetics Area Manager/Local Health Manager to arrange an urgent review if required. In private Units contact: The Irish Nutrition & Dietetic Institute (INDI) on www.indi.ie for a private appointment. Protocol for Dietetic referrals: to be sent when a resident is/has; • At risk/identified with malnutrition (MUST/MNA) or has a BMI < 20kg/m2 or >25kg/m2 • Unintentional weight loss of 10% of body weight since last recorded weight or within 3-6 months. This includes residents whose current BMI falls within 20kg/m2 or >25kg/m2 (normal healthy range) • A diagnosis of Dementia, Feeding, Eating, Drinking and Swallowing Disorders (FEDS disorders/Dysphagia) or whose current co-morbidities place the individual at risk of malnutrition (Carcinoma, COPD, etc) • Currently on a medical diet e.g. diabetic, renal or cardiac diets or is receiving oral or enteral nutritional support i.e. PEG, NG, NJ, JEJ feeding • Wound(s) present e.g. leg/foot ulcers, pressure ulcers including residents with exudating varicose eczema. Refer to RAP 13 - Skin and Wound Care Personalised Care Planning The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to address the cause or risks of malnutrition where possible. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. Problem/Need Identification Record the actual or potential nutritional problem and its associated or related risk factors. For example; ‘Mary reports a difficulty in swallowing and is at risk of malnutrition associated with dysphagia’ or ‘Mary is at risk of malnutrition related to her cognitive impairment and dementia ’. Goal specification Record: realistic, measurable and obtainable MDT goals. For example: ‘Mary will increase her nutritional intake by eating fortified foods. Mary’s weight and BMI will be maintained or improved on monthly reassessment’. Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential nutritional problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 58 1. Specific MDT interventions: Record: a) Specific interventions to address resident’s/significant other(s’) concerns, preferences, care choices and religious/cultural requirements e.g. fear of choking for those with dysphagia. This can be addressed by providing psychological support and through education on SLT strategies to prevent choking. See section below. b) MDT specific care instructions. This includes nursing care instructions for addressing malnutrition risk or management and other care instructions from members of the MDT. For example: a dietitian’s specific instructions for treatment of malnutrition. These should be listed here or a photocopy attached to the care plan. It is important to refer the reader to the attached instructions. The same applies for Speech and Language (SLT) instructions on dietary consistency for safe swallowing and the resident’s position required for safe swallowing. • In facilities with limited access to dietetic services, nurses should implement and document a food fortification plan of care as a first step for residents with / or at risk of malnutrition, unless contraindicated by the resident’s co-morbidities such as residents on medical diets e.g. diabetes, renal disease, etc. If these medical conditions are present consult a dietitian prior to commencing food fortification. Food fortification is the process of increasing the nutrient content of a resident’s diet without increasing the portion size. This includes the addition; of cream, butter, honey or skimmed milk powder to meals where appropriate, and by providing additional nutritious snacks. Refer to the regional guidelines on nutrition and hydration for further information. For residents with dysphagia consider: i. The risks of aspiration and the resident’s position required for safe swallowing e.g. chin tilt, 90° upright and maintain upright for 30minutes after eating/drinking. Ensure the resident is alert to eat. ii. Ensure strategies for safe swallowing which have been provided for an individual resident by the SLT are implemented (e.g. swallow twice, slow down, put your chin down etc). iii. Residents with dysphagia who are prescribed modified consistency diets by a SLT should be provided with clear guidelines on the type of consistency required for safe swallowing e.g. soft, minced and moist, smooth pureed or liquidised. iv. The palatability and visual appearance of food offered. For example, pureed food is more appealing when prepared in food moulds and served in individual portions on the same plate. Residents are likely to eat more if they can taste different flavours, never mash different foods into a bowl. When some vegetables are pureed such as carrots, water separates out onto the plate. The addition of thickener e.g. Thick & Easy®/Nutils® to vegetables before serving can prevent this. v. It may be necessary to avoid food that is difficult to swallow e.g. dry/crumbly foods (toast, brown bread, sponges- moisten first with e.g. syrup/sauces/gravies), mixed consistency foods (e.g. lumpy soups, cornflakes & milk- provide uniform consistency foods e.g. blended soup, porridge etc), stringy vegetables (e.g., green beans), vegetable or fruit with skins (e.g. peas, grapes-remove skins first), foods that can cause choking (e.g. peanuts, popcorn, boiled sweets, sweet corn). Please note: each person with dysphagia must be assessed by a SLT for individual recommendations on safe swallowing. 59 vi. Ensure that any oral nutritional supplements recommended by the dietitian are of the consistency recommended by the SLT. vii. Ensure the resident’s specific equipment needs are documented to maintain/improve/promote independence e.g. beaker/volume control beaker /straw/napkin to protect clothing. Allow sufficient time and support for eating and drinking. viii. Discourage talking while eating or drinking and minimise distractions. ix. Document oral hygiene requirements to prevent the risk of aspiration pneumonia. x. Medication: some medication can help improve swallowing e.g. anti-Parkinsonian medication for those with Parkinson’s disease. Medications prescribed 30-60mins before meals can optimise swallowing and eating. Other medications can make swallowing worse e.g., antipsychotic medication. If swallowing deteriorates when antipsychotic medication is commenced or increased this should be promptly communicated to the resident’s doctor. 2. Monitoring and ongoing reassessment: • Weights should be recorded at least monthly, but may require more frequent monitoring in specific cases. Maintain a weights chart in the Nursing Assessment Tools section. Compare current weight to previous weight and baseline weight. Act on findings which are of concern e.g. onward referral to doctor/dietitian for weight loss. Note: weight loss can be very gradual, therefore the importance of baseline comparisons. • Nutritional Risk reassessments (MUST/MNA) should be recorded at least 3 monthly and BMI indices compared. • Enteral feeding, maintain and monitor a daily intake/output chart. Monitor and record urine colour. Refer to RAP 20- Feeding Tubes. • Accurate food charts/Food diaries should be maintained using agreed descriptions of portion sizes for those at risk/or identified with malnutrition. The duration of this specific record keeping should be agreed with the dietician at local level. If dehydration is present refer to RAP 6- Dehydration and Fluid Maintenance. • Monitor blood reports. • Monitor daily intake of diet using the Daily Record of Care flow chart. The amount taken at each meal is recorded as a %. • Monitor and record daily skin inspections for pressure ulcer development using the Daily Record of Care flow chart. • Monitor for signs/or worsening of dysphagia. If signs of aspiration are observed, document what the person was eating or drinking at the time and promptly communicate findings to the MDT. Further monitor for any evidence of deterioration in respiratory status e.g. recurrent pneumonias and promptly record and report findings to the MDT. 3. Communication: • Promptly communicate monitoring concerns to the resident’s doctor / dietitian / SLT. Update care plans accordingly • NOTE: Residents MUST BE referred back to the multi-disciplinary team if there is deterioration in their nutritional status despite following MDT advice/instructions. • Communicate the resident’s personalised care plan to all those involved in the resident’s direct care. Ensure the resident’s significant others/visitors are aware of any swallowing difficulties. Ensure the resident/significant other is kept up to date. 60 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Educate residents and relatives on the importance of nutrition and the prevention of malnutrition and associated risks if present with FEDS/dysphagia. Provide written information where possible and/or provide information in a format that suits the resident’s communication requirements. Refer to RAP 1 Communication, Vision and Hearing.16 Evaluation of care (based on goals specified) • Nutritional Care plans must be evaluated when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking to see if the goals of care are being met e.g. weight gain, improvement in BMI, improved dietary intake, improvement in biochemical parameters, maintaining skin integrity, improvement in the resident’s self reported quality of life. Refer to the protocols of ‘Expected Standards for Care Flow Chart’ and sample ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. 61 62 • Past & present medical history. Note suggestive or actual risk factors/comorbidities for; malnutrition & FEDS disorders (dysphagia). If resident has already been seen by a SLT and or a dietitian prior to admission, record date of last review & recommendations in the nursing care plan. • Resident’s dietary likes/dislikes- preferred portion size, dietary modifications, fluid consistency, level of assistance required & need for modified utensils. • Weigh resident. • Nutritional Screening using MUST or MNA Tool. Record BMI. • Assess resident’s oral health & record last dental check-up. • Assess resident for signs and symptoms of malnutrition e.g. weight loss, loose clothes, thin/obese, poor appetite, consider MUST/MNA findings. • Assess resident for signs & symptoms of dysphagia e.g. reported swallowing problems, drooling, coughing, choking and/or throat clearing when eating /drinking, wet voice after swallowing, recurrent chest infections, pocketing of food in mouth, unexplained weight loss. • Assess resident’s / significant other(s) concerns in relation to prevention and management of malnutrition. Nursing Assessment-Document (On admission, if resident’s condition improves or deteriorates and at least 3 monthly) Nursing Assessment At Low Risk Reassess when there is a change in the resident’s condition and as per local policy (monthly weights & nutritional screening at least 3 monthly). Consider overall weight loss/gain & refer to the Multidisciplinary Team as appropriate. At Medium-High risk Malnutrition • Identify risk level. • Identify factors for Malnutrition and or Dysphagia (FEDS) disorders Nursing Diagnosis • Refer resident to MDT i.e. Doctor, Dietitian, SLT(If FEDS disorders) & OT for advice on equipment/ positioning. • In units with limited dietetic access, nurses should implement a ‘Foods first, First step approach food fortification plan for those with / or at risk of malnutrition, unless contraindicated by the resident’s co-morbidities. Add cream, butter, honey, skimmed milk powder to meals & provide additional nutritious snacks e.g. Petit Filous, full fat cheese/yogurt, etc. • For units with limited/no access to SLT consider: aspiration risks & urgency for swallow assessment (FEDS Disorders /dysphagia). In HSE Units, contact: GP /Senior Nursing Management /SLT Area Manager/LHM to arrange an urgent review or/ decision to transfer to acute services. In private units contact: IASLTPP 01-8787959 (Private appointment) • Develop & implement a personalised nutritional plan of care, in conjunction with the wishes of the resident/significant other & MDT. • Maintain accurate food/fluid charts using agreed descriptions of portion sizes & monitor intake. • Monitor weights (e.g. weekly), blood results (as necessary) & check skin integrity daily. • Monitor for signs/or worsening of dysphagia/ FEDS e.g. respiratory symptoms Goal- To prevent / manage Risks, FEDS Disorders &/or Malnutrition Nursing Goal & Care planning Malnutrition / FEDS WorseningRefer resident to multidisciplinary team. Malnutrition /FEDS Improving• Continue with care plan. • Continue to monitor intake, weights and BMI. . At Risk or Suffering from Malnutrition / FEDS. • Reassess resident’s progress against care plan goals e.g. improvement in intake, BMI, weight, biochemical parameters, skin integrity maintained. • Document nursing evaluations based on above outcome criteria. Nursing Evaluation Protocol for Care for Nutritional Status in HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: Sample Nutritional Care Plan PROBLEM / NEED IDENTIFICATION Number: Date 01/01/10 Cissy reports a difficulty in swallowing (FEDS Disorder/Dysphagia) and is at risk of malnutrition associated with this. Signature Jane Murphy GOAL SPECIFICATION Cissy wishes to remain as independent as possible and to choose what she would like to eat and drink, while being cognisant of preventing aspiration. Cissy’s weight will be maintained or improved in monthly reassessments. SPECIFIC INTERVENTIONS Date 11/01/10 Signature • • • • • • • • • • • • • • Cissy was reviewed by the dietitian and SLT in St. James’s on 04/01/2010 refer to dietary consistency and food fortification recommendations attached overleaf (or list recommendations here). Cissy must be sitting upright at a 90°angle when eating or drinking and this position should be maintained for at least 30mins afterwards, to prevent aspiration. Mealtimes must be supervised. Ensure Cissy is alert for eating and drinking & do not ask Cissy questions while eating to prevent aspiration. Ensure Cissy has her dentures, modified cutlery, a non-slip mat, clothes protection and plate guard for meals (needs). Provide a choice of menu/drinks and allow Cissy choose. Cissy likes ‘small meal’ portions, ensure food is presented attractively and in the correct consistency. Commence a Food Chart & record for XX days. (State Number) Monitor & record Cissy’s Weight (specify frequency) Monitor & record BMI (specify frequency). Monitor for signs and symptoms of FEDS disorder worsening e.g., silent aspiration (pyrexia, respiratory symptoms). Record Nutritional Risk Assessment (specify frequency) Monitor dietary intake on the Daily Flow Chart of Care. Communicate monitoring concerns promptly to the MDT. Cissy and her family have been given information and advice on the importance of a healthy diet and dysphagia management. Ongoing information is to be provided. Jane Murphy EVALUATION OF CARE (based on goals specified) Date Signature Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 63 Suggested further reading: HSE (2008) Regional PPGs Older Persons ROP066 Nutritional and Hydration Care in HSE Older Persons Residential Care Facilities http://hsenet.hse.ie/Hospital Staff Hub/mullingar/Policies, Procedures Guidelines Midland Area/Care of the Older Persons/Regional PPG's/ROP066 Guideline -Nutritional and Hydration Care in HSE Older Persons.pdf References 64 1 National Cancer Institute (2009) Dictionary of Cancer Terms- Nutritional status http://www.cancer.gov/Templates/db_alpha.aspx?CdrID=463734 2 National Institute for Health and Clinical Excellence (2006) Nutrition support in adults NICE Clinical Guideline no 32. www.nice.org.uk/CGO32 3 Elia, M., Stratton, R., Russell, C., Green, C., Pang, F. (2005) The cost of disease-related malnutrition in the UK and economic considerations for the use of oral nutritional supplements (ONS) in adults. A Report by The Health Economic Group of the British Association for Parenteral and Enteral Nutrition (BAPEN). 4 Milne, A., Potter, J., Vivanti, A., Avenell, A. (2009) Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No.: CD003288. DOI: 10.1002/14651858.CD003288.pub3. 5 Royal College of Nursing (2009) 10 key characteristics of good nutritional care. Royal College of Nursing www.rcn.org.uk 6 National Institute for Health and Clinical Excellence (2006) Nutrition support in adults NICE Clinical Guideline no 32. www.nice.org.uk/CGO32 7 Loser, C., Lubbers, H., Mahlke, R., Lankisch, P. (2007) The involuntary weight loss of the elderly. Der ungewollte Gewichtsverlust des alten menschen, 104(49) A3411-A3420. 8 Russell, C., Elia, M. (2007) Nutrition screening survey and audit of adults on admission to hospitals, care homes and mental health units. Redditch:BAPEN; 2007. 9 Alibhai, S., Greenwood, C., and Payette, H. (2005) An approach to the management of unintentional weight loss in elderly people. Canadian Medical Association Journal, 172 (6):773-80. 10 Caroline Walker Trust (2004) Eating Well for older people. www.cwt.org.uk 11 Suominen, M., Muurinen, S., Routasalo, P., Soini, H., Suur-Uski, I., Peiponen, A., FinneSoveri, H., Pitkala, K. (2005) Malnutrition and associated factors among aged residents in all nursing homes in Helsinki. European Journal of Clinical Nutrition. 59(4):578-583. 12 Voices (1998) Eating well for older people with dementia. Wordworks, London. 13 Eslick G., Talley N. (2008) Dysphagia: Epidemiology, risk factors and impact on quality of life - A population-based study, Alimentary Pharmacology and Therapeutics. 27(10)(pp 971-979). 14 Turley, R., Cohen, S. (2009) Impact of voice and swallowing problems in the elderly Otolaryngology - Head & Neck Surgery. 140(1):33-36. 15 Wilkins T., Gillies R.A., Thomas A.M., Wagner P.J. (2007) The prevalence of dysphagia in primary care patients: A HamesNet research network study. Journal of the American Board of Family Medicine. 20(2)(pp 144-150) 16 HIQA (2009) National Quality Standards for Residential Care Settings for Older People in Ireland RAP 6: Dehydration and Fluid Maintenance Definitions: Dehydration is an abnormal depletion of body fluids.1 It can occur as a result of decreased fluid intake or increased fluid losses or as a combination of both. Dehydration in older adults can result in; constipation, faecal impaction, increased incidence of pressure ulcers, hypotension, increased risk of falls, decreased functional and mental capacity, delirium and infections.2 If untreated dehydration can result in renal failure, shock, seizures, brain damage and death.3 RAI Identifiers of Potential Risks: Drinking difficulties C8 Communication/Comprehension difficulties D3, D4 Functionally dependent F17, Requires thickened fluids F8 Difficulty in swallowing F22 Modified diet F5 Urinary Incontinence G2 Signs & symptoms of dehydration present F21, Nausea, vomiting, diarrhoea F23 Other Risk Factors include: • • Intrinsic risks; e.g. psychological fear of incontinence, diminished sense of thirst, diminished appetite/refusal of food and fluids, excessive output from stoma, medical co-morbidities e.g. dementia, Feeding, Eating, Drinking and Swallowing disorders (FEDS Disorders/Dysphagia), uncontrolled diabetes mellitus, pituitary adenomas and adrenal gland disorders causing diabetes insipidus, internal/external haemorrhage and any acute episode of illness which results in pyrexia, excessive sweating, diarrhoea or vomiting. Extrinsic risks; e.g. medications (over use of sedation/psychotropic drugs / laxatives, drug side effects e.g. nausea, vomiting and diuretic medications). Inadequate care practices such as; inadequate monitoring, documentation and management of residents intake and output for those at risk; inadequate monitoring, documentation and management of residents on fluid restrictions for medical reasons (e.g. renal or heart failure); inaccessibility of fluids for residents or inadequate provision of sufficient fluids.4 Further assessments Document the following assessments on admission, when the resident’s condition improves or deteriorates and at least three monthly. Assess for: 1. The resident’s overall risk context: Bio/psycho/social risks e.g. co-morbidities, medications, malnutrition and pressure ulcer risk, limitations in functional activities, psychosocial, religious and cultural issues6. Several sources of information should be used in information/history gathering e.g. discussion with the resident, significant others, transfer letters, contact with/and discussion with the multidisciplinary team e.g. resident’s doctor, nurses, carers. This is especially important for residents with communication or cognitive difficulties. 2. The cause of dehydration such as infection, fluid refusal, etc. For example: if a resident is repeatedly refusing drinks offered, the reason for this refusal should be explored. Ascertain if the refusal stems from physical conditions such as a sore mouth (e.g. thrush), dental caries, nausea due to fever/viral infections/medication side effects, cognitive difficulties (e.g. dementia), psychological factors (e.g. fluid preferences, depression, behavioural problems, paranoia) or social causes (resident not afforded dignity, feeling rushed, cultural/religious requirements). 65 3. Signs and symptoms of dehydration: dry furrowed tongue and mucous membranes, sunken eyes, dark concentrated/decreased/absent urinary output, increased urine specific gravity, elevated blood urea nitrogen (BUN) to creatinine ratio, increased frequency of urinary tract infections, constipation, confusion, lethargy, muscle cramps, hypotension or othostatic hypotension and tachycardia.5, 6 • Note: Assessment of skin turgor is not a reliable indicator of dehydration in older people due to age related skin changes and a loss of skin elasticity.5 4. Pressure ulcer risk using a validated tool e.g. Waterlow, Braden tools. Refer to RAP 12Pressure Ulcer Prevention and Management. 5. Malnutrition risk using a validated tool e.g. MUST or MNA tools (Refer to RAP 5 Nutritional Status). Referrals required: • • • Promptly refer the resident to his/her doctor if signs or symptoms of dehydration are noted. A prompt referral is further required to a dysphagia trained Speech and Language Therapist (SLT) if a resident is suspected of having FEDS disorders / dysphagia (high risk of aspiration) for swallow assessment. A dietetic referral is required for all residents with FEDS disorders /dysphagia. An Occupational Therapy referral may be required for advice on equipment and positioning in maintaining a resident’s independence. Record referrals made on the MDT Referral Record and document the reason/outcome of the referral in the narrative notes. In facilities with no/limited access to SLT, consider the risk of aspiration and urgency for swallow assessment (for residents with suspected FEDS Disorders/Dysphagia). In HSE Units, contact: Resident’s Doctor /Senior Nursing Management/SLT Area Manager/Local Health Manager to arrange an urgent review or to decide on the transfer of the resident to an acute hospital if an urgent review is not possible. In private designated centres contact: Irish Association of Speech and Language Therapists in Private practice (IASLTPP) 01-8787959 or IASLT at 085 – 7068707. In facilities with no/limited access to dietetic services, consider the resident’s risk level and the urgency of the review required. In HSE Units, contact: Resident’s Doctor / Senior Nursing Management/Local HSE Dietitian or Dietetics Area Manager/Local Health Manager to arrange an urgent review if required. In private Units contact: The Irish Nutrition & Dietetic Institute (INDI) on www.indi.ie for a private appointment. Personalised Care Planning The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to address the cause or risks where possible. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. Need / Problem Identification Record the actual or potential fluid maintenance problem and its associated or related risk factors. For example; ‘Mary reports a difficulty in swallowing and is at risk of dehydration associated with dysphagia’ or ‘Mary has evidence of dehydration related to acute respiratory tract infection’. Goal specification Record: realistic, measurable and obtainable MDT goals. For example: ‘Mary will increase her intake of oral fluids to (specify in millilitres/litres in 24 hours)’. 66 Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential hydration problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: Record: a) Specific MDT interventions to address resident’s/significant other(s’) concerns, preferences and care choices. For example many older people have a fading sense of thirst and forget to drink or they may be unable to consume adequate fluids due to medical co-morbidities such as MS, CVA and end stage dementia. Others may simply be frightened to drink because of the fear of incontinence. Individual considerations should be addressed in the care plan such as by; Providing psychological care/support to address the resident’s; • Fears: e.g. of incontinence, through continence promotion strategies. Refer to RAP 7- Urinary Incontinence and Continence Promotion. • Refusal to take fluids: e.g. residents with dementia who repeatedly refuse drinks from staff will sometimes take it from their loved ones. The importance of touch in this group can further focus a resident’s attention on drinking. Holding hands, giving reassuring touches, singing softly and continuity of care have been found to help overcome resistance to drinking and eating.7 • Fluid maintenance and ethical care choices: The provision of hydration support is not always appropriate. MDT decisions regarding the withholding or withdrawing of nutritional or hydration support require legal and ethical consideration.8 Refer to the Regional Nutritional and Hydration Guidelines. b) MDT specific care instructions. This includes nursing care instructions for addressing dehydration risk or management and other care instructions from members of the MDT e.g. doctor’s specific instructions for increased fluid intake. • Fluid maintenance/ management Record specific MDT instructions to maintain/improve hydration. International consensus is that older adults require 1.5 to 2 litres/day or 6 to 8 cups of fluid daily, unless a fluid restriction has been imposed for medical reasons (e.g. renal or heart failure). Residents who are at medium to high risk of dehydration require 30-35mls/kg of body weight.9 i. Encourage, remind or assist residents to drink small amounts of fluids hourly. Refer to the residents’ specific preferences (likes/dislikes). Residents who are unable to consume adequate oral fluids should be considered for subcutaneous fluids (short term period) or enteral fluids (long term). ii. Ensure fluids are within easy reach of residents and provide a choice of beverages e.g., milk, tea, fruit or vegetable juices, smoothies, soups. Decrease coffee, alcohol and carbonated intake which can contribute to dehydration. iii. Ensure adequate fluid intake for residents on high fibre diets. iv. Ensure the resident is positioned upright and their specific equipment needs are documented to maintain/improve independence e.g. beaker/straw/napkin to protect clothing or for those with dysphagia a volume control beaker (5ml/10ml) can limit how much the person swallows per mouthful. Allow sufficient time and support for eating and drinking. 67 v. Residents with dysphagia who are prescribed modified consistency fluids by their medical practitioner should further be provided with clear guidelines on the daily fluid intake goal (in litres) and the type of consistency required for safe swallowing e.g. syrup/custard/set consistency. For residents with dysphagia consider: vi. The risks of aspiration and position required for safe swallowing e.g. chin tilt, 90° upright & maintain upright for 30minutes post eating/drinking. Ensure strategies for safe swallowing which have been provided for an individual resident by the SLT are implemented (e.g. swallow twice, slow down, put your chin down, etc) vii. The palatability of the fluids offered. For example, warm thickened drinks that are left to stand can be very unpalatable. When thickening tea/coffee, add the milk to the tea to bring the fluid to 200ml and then add the thickener. Thicken minerals, favourite fluids and fruit juices e.g. cranberry, apple and orange are good choices and hold their flavour well. Add squash /fruit juice to water before thickening to increase palatability. viii. The addition of high water foods e.g. soups, jelly, custard and ice cream can further improve hydration levels. 2. Monitoring & ongoing reassessment • At high risk or/with dehydration, measure and document a daily fluid intake/output chart. Record the frequency and types of fluids offered, the amount taken and fluid losses incurred (urine, vomitus, etc). Monitor and record urine colour. • At risk of dehydration, record and monitor urine colour on the Daily Record of Care (use colour code on the flow chart). • Enteral feeding, maintain and monitor a daily intake/output chart. Refer to RAP 20. Monitor and record the urine colour. • Monitor closely any resident who is on thickened fluids or fluid restrictions. • Monitor for worsening of dysphagia/FEDS disorders if present. Monitor signs and symptoms of aspiration, deterioration in respiratory status e.g. recurrent pneumonias • Monitor BUN to Creatinine Ratio and other pertinent lab values (e.g. U & E). • Pressure ulcer risk present refer the reader to the Pressure Ulcer Prevention (Management) Care plan. • Malnutrition (actual or potential problem) refer the reader to Nutritional Care Plan • Pertinent Lab results e.g. U & E, BUN to Creatinine Ratio. 3. Communication • Promptly communicate monitoring concerns to the resident’s doctor / dietitian / SLT. Update care plans accordingly • Communicate the residents personalised care plan to all those involved in the resident’s direct care. Ensure the resident/significant other is kept up to date 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Educate the resident and their relatives on the importance of hydration and the prevention of dehydration and risks associated with FEDS disorders/dysphagia if present. Provide written information where possible and/or provide information in a format that suits the resident’s communication requirements. Refer to RAP 1 Communication, Vision and Hearing.10 68 Evaluation of care (based on goals specified) • MDT Dehydration / Fluid Maintenance Care plans must be evaluated when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking to see if the goals of care are being met Refer to the ‘Protocols of the Expected Standards for Care’ flow chart and sample ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. 69 70 Nursing Assessment-Document • Past & present medical history. Note suggestive or actual risk factors/comorbidities for; dehydration, & FEDS disorders (dysphagia). If resident has already been seen by a SLT prior to admission, record date of last review & Fluid consistency recommendations in the personalised (nursing) care plan. • Assess resident for signs & symptoms of dehydration e.g. dry furrowed tongue, dry mucous membranes, sunken eyes, constipation, concentrated/decreased urinary output, hypotension, tachycardia etc. • Assess resident for signs & symptoms of Dysphagia e.g. reported swallowing problems, drooling, coughing, choking and/or throat clearing when eating /drinking, wet voice after swallowing, recurrent chest infections, pocketing of food in mouth, unexplained weight loss. • Resident’s drinks likes/dislikes- level of assistance required and need for modified utensils (beakers, straws, etc). • Nutritional Screening using MUST or MNA Tool. Record BMI. • Pressure Ulcer Risk assessment using a validated tool e.g. Braden, Waterlow. • Assess resident’s oral health and need for oral care. Record last dental check-up. • Assess resident’s/significant other(‘s) concerns in relation to prevention and management of dehydration. (On admission, if resident’s condition improves or deteriorates and at least 3 monthly) Nursing Assessment At Low Risk • Reassess when there is a change in the resident’s condition. • Monitor the colour of urinary output daily (if incontinent check incontinence pad or ask the resident) • Monitor for signs and symptoms of dehydration daily. At High Risk / has Dehydration • Identify risk factors related to dehydration. • Identify cause(s) associated with dehydration. Nursing Diagnosis • Promptly refer resident to MDT i.e. Doctor, SLT-(If FEDS disorders [Dysphagia] suspected/present) & OT for advice on drinking utensils/ positioning & maintaining or improving resident’s independence. Dietitian referral is required for all residents with dysphagia. • In units with limited/no access to SLT consider aspiration risks & urgency for swallow assessment (FEDS Disorders). In HSE Units, contact: GP /Senior Nursing Management /SLT Area Manager/LHM to arrange an urgent review or/ decision to transfer to acute services. In private units contact: IASLTPP 01-8787959 (Private appointment) • Develop & implement a personalised fluid maintenance plan of care, in conjunction with the resident’s / significant other’s wishes & MDT. • Maintain accurate fluid charts using agreed descriptors (e.g. cup=150mls, beaker=200mls) & monitor intake and output. Record urine colour. • Monitor relevant lab values • Check skin integrity daily. • Provide education/information & psychological support to residents / significant others Goal to Prevent/Manage Risks, Dehydration or FEDS Disorders Nursing Goal & Care planning Dehydration WorseningPromptly refer resident to his/her doctor. Hydration levels Improving• Continue with care plan. • Continue to monitor intake/output, urine colour & lab values . At Risk or Suffering from Dehydration / FEDS. • Reassess resident’s progress against care plan goals e.g. improvement in fluid intake, improvement in biochemical parameters, maintaining skin integrity. • Document nursing evaluations based on above outcome criteria. Nursing Evaluation Protocol for the Expected Standards for Care in Dehydration and Fluid Maintenance in HSE Older Designated Centres SAMPLE PERSONALISED CARE PLAN Topic Heading: Dehydration and Fluid Maintenance PROBLEM / NEED IDENTIFICATION Number: Date 01/01/10 Cissy is at high risk of dehydration associated with a gradual decline in oral intake related to dementia. Signature Jane Murphy GOAL SPECIFICATION Cissy’s oral intake will increase to 1.5 litres/24 hrs. SPECIFIC INTERVENTIONS Date 11/01/10 Signature • • • • • • Reviewed by Dr Johnson today, no evidence of swallowing problems or acute illness. Advised to increase intake to 1.5 litres in 24hrs. Dietetic referral/bloods sent. Encourage Cissy to take at least 100mls of fluids hourly. Cissy likes: pineapple juice, Lilt, 7UP, & Sweet Coffee alternate these drinks & avoid tea, milk, water which she dislikes. Use gentle touch and simple verbal instructions. Let Cissy know that you are about to give her a drink and instruct saying ‘Open your mouth’ ‘swallow’. Cissy likes sweet foods; give high water content foods e.g. soup (add two teaspoons of sugar) & Ice cream / custard. Encourage extra drinks with meals. Monitor & maintain intake/ output chart. Record drinks offered and amount taken. Record urine colour (check Cissy’s incontinence wear). Record if incontinence wear is wet or dry at changes. Monitor blood results. Communicate monitoring concerns promptly to the MDT Information re: prevention and management of dehydration discussed with Cissy’s family, who will further encourage Cissy to take drinks & record amounts taken. Family are to be provided with opportunities to discuss diagnosis and management options. Jane Murphy EVALUATION OF CARE (based on goals specified) Date Time 12/01/10 13.20 Cissy has only taken 900mls of fluid in 24hrs despite best efforts. Doctor contacted, for review this afternoon Signature Jane Murphy Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 71 Suggested further reading: HSE (2008) Regional PPGs Older Persons ROP066 Nutritional and Hydration Care in HSE Older Persons Residential Care Facilities http://hsenet.hse.ie/Hospital Staff Hub/mullingar/Policies, Procedures Guidelines Midland Area/Care of the Older Persons/Regional PPG's/ROP066 Guideline - Nutritional and Hydration Care in HSE Older Persons.pdf References 72 1 Medline (2008) Dehydration. Medical Dictionary. Accessed on line at http://www2.merriam-webster.com/cgiin/mwmednlm?book=Medical&va=dehydration 2 Grandjean, A., Grandjean, N. (2007) Dehydration and cognitive performance. Journal of the American College of Nutrition. 26(5 Suppl):549S-554S. 3 Mentes, J. (2006) Maintaining Oral Hydration in Older Adults: Greater awareness is needed in preventing, recognizing, and treating dehydration. Americian Journal of Nursing, 106(6), 40-50. 4 Allison, S., Lobo, D. (2004) Fluid and electrolytes in the elderly. Current Opinion in Clinical Nutrition & Metabolic Care 7(1):27-33. 5 Pinto, S. (2008) Hydration: Maintaining Oral Hydration in Older Adults, Evidence-Based Care Sheet, Cinahl Informayion Systems, USA 6 Hodgkinson, B., Evans, D., Wood, J. (2005) Maintaining oral hydration in older people: a systematic review, Database of Abstracts of Reviews of Effects, Centre for Reviews and Dissemination -: Systematic reviews 7 Voices (1998) Eating well for older people with dementia. Wordworks, London 8 HSE (2008) Regional PPGs Older Persons ROP066 Nutritional and Hydration Care in HSE Older Persons Residential Care Facilities 9 National Institute for Health and Clinical Excellence (2006) Nutrition support in adults NICE Clinical Guideline no 32. www.nice.org.uk/CGO32 10 HIQA (2009) National Quality Standards for Residential Care Settings for Older People in Ireland RAP 7: Urinary Incontinence and Continence Promotion Definitions: Urinary incontinence is defined as: ‘The complaint of any involuntary urinary leakage’.1 Types: • • • • • • Urge Incontinence/Overactive Bladder: Commonest cause in older persons care. The bladder muscles are overactive and cause a strong sudden urge to void. Urine loss may be equivalent to a full void. Other characteristics include frequency and nocturia.2 Stress incontinence: Small amounts of urine leak through the urethra on effort of exertion or sneezing or coughing.2 Mixed Incontinence: A combination of urge and stress incontinence. Urinary Retention/ Overflow Incontinence: There is dribbling or leaking of urine because the bladder does not empty. Symptoms include frequency, nocturia, reports of dribbling or leaking, and the sensation that the bladder has not emptied. Urine loss is in frequent small amounts.2 Functional Incontinence: This is directly related to the resident’s ability to access the toilet. This ability may be impeded due to physical or cognitive causes. Acute or transient incontinence: Incontinence with a sudden onset often associated with a medical and/or surgical problem, usually resolving with treatment of the underlying problem.3 RAI Identifiers of Potential Risks: ■ Difficulties with urinary management C17, ■ Communication Difficulties D3, D4, ■ Dehydration F21 ■ Urinary Incontinence G2, ■ Constipation G11 ■ Assistance required with Mobility H1 Other Risk Factors include: • Urge Incontinence risks: Diuretic medication, dehydration, glucosuria, or dietary irritants, such as caffeine, fizzy drinks, smoking. Neuropathic causes include CVA, Parkinson’s and multiple sclerosis.4, 2 • Stress Incontinence risks: Pelvic relaxation, obesity, ageing, prostatectomy, chronic cough, multiple pregnancies, menopause and impaired pelvic floor innervations.4 • Mixed Incontinence risks: Combination of risk factors for Stress and Urge Incontinence • Urinary Retention/ Overflow Incontinence risks: Benign prostatic hyperplasia, urethral stenosis / strictures, constipation, neurological conditions such as spinal injury, multiple sclerosis and stroke, diabetic neuropathy, certain medications (anticholinergics, antidepressants, antipsychotics, sedatives, narcotics, alpha-adrenergic agonists, betaadrenergic agonists, calcium channel blockers).5 • Functional Incontinence risks: Physical, cognitive, or motivational impairment, inaccessible toilet or caregiver, inappropriate use of incontinence containment products, drugs e.g. sedatives.3 73 • Transient Incontinence risks: The mnemonic DISAPPEAR identifies the recognised transient causes of incontinence, which are Delirium, Infection, Stool impaction (constipation), Atrophic vaginitis, Pharmaceuticals, Psychological/psychiatric, Excess fluid, Abnormal laboratory values, Restricted mobility.6 Further assessments Document the following assessments on admission, if the resident’s condition improves or deteriorates and at least 3 monthly. Assess For: 1. Asses the resident’s overall risk context (See RAI identifier factors and compare medical history). Several sources of information should be used in information/history gathering e.g. discussion with the resident, significant others, transfer letters, contact with/and discussion with the multidisciplinary team e.g. resident’s doctor, nurses & carers, examination and observation. 2. For residents who are able to communicate use focused questions to establish the type urinary incontinence. • Ask the resident to describe how they pass urine, is it; a steady dribble (retention with overflow); spurts out (stress incontinence); sudden flow (urgency); little, often and sore (dysuria). • Ask the resident how many times do you go to the toilet in 24-hour period? • How often do you wake to go to the toilet during the night? • How often do you feel a strong and sudden urge to urinate during the day? • If you fail to get to the toilet in time, how much urine do you usually leak? • Do you leak urine when you laugh, cough, jump, or run? 3. A physical examination (including a abdomen/pelvis/perineum and focused neurological examination (S2-S4) should be undertaken by the resident’s doctor 4. Laboratory investigations include: renal function, calcium, glucose, PSA, urinalysis and urine culture if indicated 5. Assess the resident’s skin condition in groins (vulva) and anal region to establish baseline data on skin condition and out rule the presence of moisture lesions. 6. Complete an incontinence assessment tool e.g. HSE Continence Promotion Unit Continence Assessment Form for Nursing and Residential Homes 7. Look for signs and symptoms of constipation and urinary tract infections or other causes of transient incontinence. If found treat as necessary, and refer the resident to the multidisciplinary team. 8. Record a frequency volume chart. This should be completed for a minimum of 3 days. 9. Complete a fluid balance chart if it is suspected that the resident is dehydrated. Dehydration contributes to Urge Incontinence. 10. If incomplete bladder emptying is suspected, measurement of post-void residual volume may be required. This should be checked by a bladder scan in preference to catheterization due to the lower incidence of adverse events associated with scans. 11. If conservative treatment has failed further urology referral may be required. Referrals required: Refer to multidisciplinary team as appropriate to assessment findings. A doctor referral is required for baseline assessment and on going management concerns e.g. dehydration, infection, urinary retention/overflow, constipation/faecal impaction, glucosuria, depression and for review of medications associated with incontinence. 74 OT/ Physiotherapist referral may be required for decreased mobility, dexterity problems or for pelvic floor exercises. Optician or Audiology referral may be required if eye sight or hearing impairment is impacting on continence. A Continence Nurse Specialist referral may be required for personalised care planning advice for those with urge, stress, mixed or overflow incontinence (e.g. HSE Continence Promotion Unit phone number: 01-6352775). A consultant urology/specialist referral is required if symptoms do not respond to treatment within 2-3 months, or where haematuria is present without infection on urinalysis, or where symptoms are suggestive of poor bladder emptying (hesitancy, poor stream, terminal dribbling) or where there is evidence of unexplained neurological or metabolic disease. Personalised Care Planning The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care that is specific to the resident and to the type of urinary incontinence being treated. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. Need / Problem Identification Record the specific urinary incontinence problem (refer to the Protocols of Care for Urinary Incontinence) and its associated or related risk factors. For example; ‘Mary is incontinent of urine when she laughs, coughs or moves during the day and is continent at night. Mary has stress incontinence associated with a history of multiple pregnancies’. Goal specification Record: specific (to the type of incontinence), realistic, and measurable Urinary Incontinence and Continence Promotion MDT goals. For example: ‘In 3 months time Mary will have a reduced number of incontinent episodes by using continence promotion strategies’. Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential urinary incontinence problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: Record: a) Specific interventions to address residents/significant(s) concerns, preferences and care choices e.g. educate residents that urinary incontinence is not a normal process of aging and that an overactive bladder is a common and treatable medical condition. Encourage residents to talk about their fears/concerns. If the resident expresses a reluctance to take fluids, provide information on the importance of hydration and on how dehydration can contribute to incontinence. Malodours can be a further cause for concern; provide information/ psychological support on good hygiene practices, continence promotion strategies and on appropriate incontinence products. 75 b) MDT specific care instructions. This includes nursing care instructions/programmes for promoting continence and managing incontinence and other MDT specific care instructions e.g. a doctor’s specific instructions for the treatment of urinary incontinence e.g. specific instructions for faecal impaction treatment or a physiotherapist’s instructions on pelvic floor exercises should be listed here. • Specific Interventions (Programmes) for promoting continence and managing incontinence include: i. Bladder Retraining Programme: This is used to treat Urge Incontinence. It actively involves the individual in attempting to increase the interval between the desire to void and the actual void. A schedule of voiding is strictly adhered to, with a gradual increase in the intervals between voiding. This schedule is based on the results of their frequency volume chart. Bladder training lasting for a minimum of 6 weeks should be offered as first-line treatment to women with urge or mixed incontinence.7 ii. Pelvic Floor Muscle Training Programmes: A trial of supervised Pelvic Floor muscle training of at least 3 months’ duration should be offered as 1st line treatment for stress or mixed incontinence.7 These exercises are initiated by staff who are trained in Pelvic Floor Muscle exercises. iii. Habit Training and Prompted Voiding Programme: These are techniques for restoring continence in residents with Cognitive impairment. The resident is taken to or reminded to void at certain times in order to re-establish and/ or reinforce the habit of voiding. Positive reinforcement techniques are used by staff for the resident on achieving appropriate toileting e.g. by giving praise and positive attention.3, 7 iv. Timed voiding: Promotes conditioned reflexes for residents with neurogenic bladder. Fixed voiding schedule that is unaltered. Times must be adhered to. v. Incontinence Containment Products should only be used when indicated by a comprehensive assessment. Containment products may be necessary either during ongoing treatment or when continence cannot be achieved.8 Refer to local guidelines for choosing the correct type, size and absorbency of incontinence containment products. Document the specific products required. • Specific Interventions for Skin Protection: Following incontinent episodes, cleanse skin with (state product e.g., Clinisan/Water & Silcocks Base). Apply barrier creams sparingly (state product e.g. Petroleum jelly and do not use Sudocrem®/Talc or Powder). Refer to RAP 13: Skin and Wound Care. 2. Monitoring & ongoing reassessment Record the specific types of ongoing reassessments and monitoring requirements in managing the resident’s incontinence problem/need: Consider: a) The types of reassessments/monitoring that may be required for the specific types of incontinence and their associated underlying causes. For example: • Urge Incontinence e.g. if associated with dehydration (refer to RAP 6 Dehydration and Fluid maintenance for specific monitoring and assessments required), glucosuria (monitor blood and urine glucose levels and specify the frequency) or medications (monitor for specific side affects). • Stress Incontinence e.g. if associated with obesity will require weight monitoring (specify frequency) and BMI monitoring (specify frequency). • Mixed Incontinence will require specific monitoring and ongoing reassessment of its associated identified risks. 76 • Urinary Retention/ Overflow Incontinence e.g. if associated with constipation (monitor bowel motions using the Bristol Stool Chart on the Daily Flow Chart of Care and refer to RAP 9 Constipation for further assessments). • Functional Incontinence will require ongoing reassessment and monitoring of the resident’s cognitive and functional status (refer to RAP 3 Cognition and Acute Confusion for further reassessment criteria) • Transient Incontinence will require ongoing reassessment and monitoring for identified transient causes of incontinence (refer to risk factors) b) The types of reassessments/monitoring required, to establish the effectiveness of the MDT Interventions (programmes) in promoting continence and in managing incontinence; • Record and monitor an Intake Output Chart (frequency voiding/volume chart) for residents with urge/stress incontinence. Record for 3-5 days. Document fluid intake, frequency and volume of urine voided (if possible) or frequency of wet/dry incontinent pad. Document urinalysis. Interpretation of monitoring: • Loss of urine during coughing, sneezing or physical exertion is indicative of Stress – usually small amounts, usually dry at night • Frequency (8+ voids per day, or twice or more at night ), and urgency is indicative of Detrusor instability – usually large amounts, usually wet at night • Post micturition dribble, poor stream, hesitancy, straining to void is indicative of outflow obstruction • Continuous wetness may suggest neurogenic/reflex bladder • Reassess resident’s skin daily (groins, [vulva] and anal region) for the presence of moisture lesions, if present update care plan. Refer to RAP 13: Skin and Wound Care. 3. Communication • Promptly communicate monitoring concerns to the resident’s doctor and other members of the MDT as appropriate.Update care plans accordingly. • Communicate the residents personalised care plan to all those involved in the resident’s direct care. Ensure the resident/significant other is kept up to date. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Educate residents/significant other(s) on the resident’s specific type of incontinence and their personalised plan of care. Provide information on the importance of hydration and on the prevention of dehydration. Provide written information where possible and/or provide information in a format that suits the resident’s communication requirements. Refer to RAP 1: Communication, Vision and Hearing.9 Evaluation of care (based on goals specified) • MDT Urinary Incontinence and Continence Promotion Care plans must be evaluated when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking to see if the goals of care are being met. Refer to the ‘Protocol for the Expected Standards of Care’ flow chart and sample ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. 77 78 Protocols of Care Ensure adequate hydration Prevention/treatment of constipation Advise resident to avoid caffeine Bladder retraining Administer Antimuscarinic medication as prescribed Risk Factors Diuretic medication Dehydration Glucosuria Caffeine Neuropathic causes: CVA, Parkinson’s & Multiple Sclerosis Urge Risk Factors & Protocols of Care Combination of those for Urge & Stress Incontinence Mixed Protocols of Care Pelvic Floor Muscle Exercises Programme (to be initiated by staff trained in PFME only) Risk Factors Obesity Ageing Multiple pregnancies Menopause Stress Protocols of Care Treat underlying cause Catheterisation Risk Factors Certain drugs Constipation Benign prostatic hyperplasia MS, CVA Retention Protocols of Care Treat underlying cause Risk Factors Delerium (drugs & bugs) Infection Stool impaction constipation Atrophic vaginitis Pharmaceuticals Psychological Excess fluid Abnormal lab values Restricted mobility Risk Factors Directly related to the ability to access the toilet Protocols of Care Ensure clear access to toilet Ensure adequate lighting & signage Assist resident to the toilet Use aids such as urinals & commodes Use specially designed clothing for dexterity problems Habit training & Prompted voiding Transient Functional Complete a Urinary Incontinence Assessment Tool. Assess for signs & symptoms of constipation, urinary tract infection, & other causes of transient incontinence. If urinary retention is suspected: Assess residual bladder volumes (Palpate bladder). Assessment Protocol for the Expected Care Standards for Urinary Incontinence and Continence Promotion in HSE Older Persons Designated Centres SAMPLE (Personalised) CARE PLAN Topic Heading: Urinary Incontinence and Continence Promotion PROBLEM / NEED IDENTIFICATION Number: Date 01/01/10 Mary is aware that she has “little accidents” (episodes of incontinence) & states “I hate wearing these bulky pads, but sometimes I forget where the toilet is and then it’s too late”. Mary has Functional Urinary Incontinence associated with decreased mobility and mild cognitive impairment Signature Jane Murphy GOAL SPECIFICATION To teach Mary ways in achieving continence. To manage incontinence. Mary’s skin will remain intact and free from incontinence associated dermatitis & moisture lesions. Mary will have reduced episodes of incontinence in 3 months time. SPECIFIC INTERVENTIONS Date 11/01/10 • Provide psychological support by the use of positive coping strategies. These include: listening to Mary’s concerns, giving information/explanation on Mary’s specific plan of personalised care, continence products & choice and information on use, skin care and advice on how to talk (openly) to family/significant others about urinary incontinence and its management if Mary wishes. • Ensure Mary’s privacy and dignity is maintained by ensuring Mary has a call bell close at hand & by walking Mary to the toilet and ensuring doors are closed. • Mary commenced on a Habit Training & Prompted Voiding Programme: Prompt & remind Mary to use her call bell, if she needs assistance in using the toilet. Ensure Mary’s Zimmer frame is within easy reach. Remind Mary of the bathroom location, by pointing out the signage. Walk Mary to the toilet 2 hourly during the day, with her consent, and prompt Mary to void urine. Encourage Mary to void urine prior to settling down for the night. Encourage independent hand hygiene post voiding. Provide positive reinforcement on achieving appropriate toileting/ having dry continence wear. Review toileting intervals in 2 weeks to assess effectiveness • Continence Containment Products: Mary requires: (state product type & absorbency). Do not use fully enclosed products, Mary does not like these. • Skin Protection: Following incontinent episodes, cleanse skin with (state product e.g., Clinisan/Water & Silcocks Base). Apply barrier creams sparingly (state product e.g. Petroleum jelly). • Monitor & record: A daily Frequency Voiding Chart for 3 days (baseline assessment). Record if continence wear is dry/wet & toileting (voided/did not void). Reassess (ongoing) continence wear requirements and check skin daily for moisture lesions. • Monitor Mary’s hydration status daily by observing & recording Mary’s urine colour, use the colour code on the daily Record of Care (to reduce incidence of dehydration/constipation/UTI). • Monitor for constipation & document bowel movements (using Flow Chart). Constipation can exacerbate urinary incontinence. Communication: Promptly report monitoring concerns to the Doctor/MDT. Information: Provide information sessions to Mary/Significant Others on Mary’s specific type of incontinence, continence promotion strategies & progress. Signature Jane Murphy EVALUATION OF CARE (based on goals specified) Date Signature Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 79 Suggested further reading: European Association of Urology (2009) Guidelines on Urinary Incontinence http://www.uroweb.org/fileadmin/tx eauguidelines/2009/Full/Incontinence.pdf References 80 1 Abrams P. Car, Cardozo L, Fall M, et al, (2001), The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society, Neurology and Urodynamics, 21(2): 167-178. 2 Bucci A.T. (2007) Be a Continence Champion: Use the CHAMMP Tool to Individualize the Plan of Care, Geriatric Nursing, 28(2), 120–124. 3 Thompson D., Smith D. (2002), Continence Nursing: A Whole Person Approach, Advanced Nursing Practice: On The Front Lines, 16(2), 14–31. 4 Gross J. (2003) Urinary Incontinence after Stroke: Evaluation and Behavioural Treatment, Lippincott Williams & Wilkins, Inc., 19(1), 43–5 5 Harvey S. (2007) University of Maryland Centre, http://www.umm.edu/patiented/articles/what overflow incontinence 000050 4.htm (accessed 13/08/09) 6 Resnick N.M., Yalla S.V. (1985) Management of Urinary Incontinence in the Elderly, New England Journal of Medicine, 313, 800-804. 7 Zarowitz, B. J., Ouslander, J. G. (2006) Management of Urinary Incontinence in Older Persons, Geriatric Nursing, 27(5), 265–270 8 Wilson L. (2003) Continence and older people: the importance of functional assessment, nursing older people, 15(4), 22-28 9 HIQA (2009) National Quality Standards for Residential Care Settings for Older People in Ireland RAP 8: Faecal Incontinence and Continence Promotion Definitions: Faecal Incontinence is an involuntary loss of solid or liquid faeces.1 RAI Identifiers of Potential Risks: ■ Difficulties with Bowel Management C18, ■ Communication or Cognitive Difficulties D3, D4, ■ Incontinence of faeces G10 ■ Constipation or Loose Stool G11 ■ Difficulties with mobilising H1, ■ Bowel Disease G1. Other Risk Factors include: Further risks associated with causes include: • Primary causes: Childbirth, Menopause, Post Surgery (e.g. haemorridectomy and anal stretch), Trauma (e.g. obstetric), Iatrogenic, Functional bowel disorders, Spinal Injury, Congenital abnormality, Inflammatory bowel disease, Colorectal cancer, Constipation with overflow, rectal prolapse, anal or recto-vaginal fistula, haemorrhoids.2 • Secondary causes: Immobility, frailty and dependence, inaccessibility to toilet facilities, inadequate care/ non available assistance, Mental Health illnesses, Behavioural Problems, Neurological disorders including cognitive impairment, Diabetes, Intellectual disability, Communication difficulties, Infections, Pelvic radiation, Diet and Medications with GIT side effects and excessive use of laxatives.4 NOTE: Faecal incontinence is a sign or a symptom frequently related to several contributory factors, which requires a multidisciplinary approach to individualised assessment and management.1, 3 Further Assessments: Document following assessments on admission, if the residents’ condition improves or deteriorates and at least 3 monthly. 1. Assess the resident’s medical history for possible contributory factors e.g. severe cognitive impairment, terminal illness, communication problems, mobility problems (check RAI Identifiers and risk factors). Several sources of information should be used in information/history gathering e.g. discussion with the resident, significant others, transfer letters, contact with/and discussion with the multidisciplinary team e.g. resident’s doctor, nurses, carers, examination and observation. This is especially important for residents with communication or cognitive difficulties. 2. For residents who are able to communicate assess bowel habit problems by the use of focused questioning: Questions to establish bowel habit history, signs & symptoms: • How long have you had problems with bowel control? Is there any pattern to this or any factors that provoke it? • Has there been any bleeding or mucous from the back passage? • Do the bowel motions vary in consistency and how frequent are they? (use the Bristol stool chart to help residents describe their stool [Figure1]) • Do you have to strain to pass stool? • Are you able to tell the difference between passing wind and a bowel motion? • Do you have a feeling of incomplete emptying after an attempted bowel motion? • Do you experience any bloating or abdominal pain before passing a bowel motion? • Do you ever assist the passage of stool with your finger? 81 • • • 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Are you able to clean yourself after passing stool? Do you have to clean yourself several times after passing stool? Do you ever leak stool without being aware of it? How much leaks? What is the consistency of leaks? Do you get the sensation of the need to empty your bowel before you leak? Is the sensation an urgent need (urge faecal incontinence)? Does soiling occur after a bowel motion has been passed (post defecation soiling)? Do you wear pads (or something else) in your underwear? If so, are they effective in preventing soiling of clothes/furnishings/surroundings?4 Assess the resident for actual or potential risk of dehydration and malnutrition. Assess for signs and symptoms of faecal loading; continuous faecal staining; small bowel motions and for signs/symptoms of constipation, distended abdomen, faeces palpable on abdominal palpation. Measure abdominal girth. Assess the resident’s medications with their doctor and pharmacist and determine if the resident is taking any drugs that might exacerbate faecal incontinence (refer to Table 1) Assess the resident’s diet for foods which might exacerbate faecal incontinence (refer to Table 2) Assess the resident’s skin for excoriation: Ask the resident do you have any itching or soreness around the back passage? Ask permission to examine the skin Assess the impact of faecal incontinence on lifestyle / Quality of life. Enquire sensitively if faecal incontinence impacts on general lifestyle, activities, emotions, self image Assess the resident’s ability to use the toilet. This includes; their mobility, ability to adjust clothing and ability to wash after using the toilet Undertake a cognitive and behavioural assessment if indicated. Refer to RAP 2 Mood and Behaviour and RAP 3 Cognition and Acute Confusion. A general physical examination, including an abdominal assessment and an anorectal examination (Visual inspection of the anus, assessment of perineal descent, digital examination of anal tone; resident should be able to squeeze anal sphincter voluntarily, assessment of faecal loading) should be undertaken by the resident’s doctor. Other assessments that may be required include a vaginal and perineal assessment. If symptoms of faecal incontinence persist after initial management, the resident may require further specialized medical/ surgical assessment e.g. anorectal physiology studies, endoanal ultrasound, MRI, proctography, transit Xray as indicated. Referrals required: Refer to multidisciplinary team as appropriate to assessment findings. • Doctor review will be required for all residents with faecal incontinence for baseline assessment and management. An urgent referral will be required if there is blood or mucus in the stool, recent and significant bowel habit changes or abdominal pain. • Pharmacist and doctor review of medications, refer to Table 1 • Dietician Referral: is required if faecal incontinence is associated with dietary intake or medical conditions e.g. diet related; diarrhoea / constipation / malnutrition / Enteral feeding or co-morbidities such as irritable bowel, inflammatory bowel disease, etc. • Physiotherapy Referral: may be required for faecal incontinence exacerbated by mobility problems and for pelvic floor muscle training, electrical stimulation and biofeedback. • OT referral may be required for faecal incontinence associated with dexterity problems. 82 • • • Continence Specialist Service referral; may be required for specialised management options such as pelvic floor muscle training, bowel retraining, specialised dietary assessment and management, rectal irrigation, advice on anal plugs, collection devices and skin excoriation Behaviour therapy referral e.g. Psychiatry of Later Life or CNS Behavioural Therapy (if available) may be required if faecal incontinence is associated with behavioural problems Medical/ surgical consultant referrals may be required for specialised further assessments Personalised Care Planning The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care that is specific to the resident and to their preferences. The primary aim is to treat the underlying cause of faecal incontinence where possible. The following conditions will require condition-specific interventions: Faecal loading; potentially treatable causes of diarrhoea e.g. infective, inflammatory bowel disease, irritable bowel syndrome; warning signs for lower gastrointestinal cancer; rectal prolapse or third-degree haemorrhoids; acute anal sphincter injury including obstetric and other trauma, acute disc prolapse/cauda equine syndrome. Problem/Need Identification Record the specific faecal incontinence problem (refer to the Protocols of Care for Faecal Incontinence Management) and its associated or related risk factors. For example; ‘Mary states that since she has become immobile she feels she can never completely empty her bowel and has continuous staining which is very upsetting. Mary has faecal Incontinence associated with faecal loading and immobility’. Goal Specification Record: specific, realistic, and measurable Faecal Incontinence and Continence Promotion MDT goals. For example: ‘Mary will establish a predictable bowel pattern with an ideal consistency stool (Type 3-4 on the Bristol Stool Scale)’ within one week. Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential faecal incontinence problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: Record: a) Specific interventions to address residents/significant(s) concerns, preferences and care choices e.g. educate the resident that faecal incontinence is a common problem and that much can be done to treat and manage this condition. Encourage the resident to express their fears/concerns. Provide emotional / psychological support and information on positive coping/continence promotion strategies. 83 Positive coping strategies include: giving information/explanation: on the specific plan of personalised care; continence products & choice and information on use; skin care and odour control; counselling services if needed through the social work department and advice on how to talk openly to family/significant others about faecal incontinence and its management (if the resident wishes this). b) MDT specific care instructions. This includes nursing care instructions/ programmes for promoting continence and managing faecal incontinence and includes MDT specific care instructions aimed at treating the underlying cause and symptom management e.g. a doctor’s specific instructions for the treatment of faecal impaction should be listed here; or a physiotherapist recommendations for improving mobility/pelvic floor exercises. For a dietitian’s instructions for treating constipation/diarrhoea, refer the reader to the Nutritional Plan of Personalised Care. • Specific Initial Interventions for promoting continence and managing incontinence should be based on baseline assessment findings and tailored to the individual’s preferences and circumstances. Include: • Bowel Retraining Programme: Assist or encourage the resident to use the toilet after meals to empty their bowel (to utilise the gastrocolic response which according to Gallagher, et al, [2008] is more pronounced after breakfast). Ensure toilet facilities are accessible, private, and comfortable and can be used safely with sufficient time allowed. Encourage the resident to adopt a sitting or squatting position where possible while emptying the bowel and to avoid straining. Ensure resident is aware of toilet locations and signage. Encourage the resident to use easily removable clothing to reduce the time needed for access. For mobility dependent residents, ensure a call bell is within easy reach. • Incontinence containment products should only be used as indicated by a comprehensive assessment. Containment products may be necessary either during ongoing treatment or when continence cannot be achieved.5 Refer to local guidelines for choosing the correct type, size and absorbency of incontinence containment products. • Skin Care: Encourage resident to/or provide skin care post defecation. Cleanse skin well in the anal region to prevent excoriation (moisture lesions) and record name of products to be used e.g. Clinisan®. Apply barrier products (state products e.g. Vaseline, etc.) Refer to RAP 13: Skin and Wound Care. For residents with moderatesevere anal excoriation, fissures or cracks, consider the addition of a soothing haemorrhoidal preparation (e.g. Hemocane®, Lanacane® cream) apply as directed by the doctor. Use following defecation and cleansing and apply a barrier product over the haemorrhoidal preparation to protect the skin. • Medication management: Review medications with the doctor and pharmacist to identify any drugs which might be causing/exacerbating the problem (Table1). Administer anti-diarrhoeal drugs for loose stools as prescribed (anti-diarrhoeal drugs should only be prescribed once other causes of faecal incontinence have been excluded e.g. excessive laxative use, dietary factors and other medication. The antidiarrhoeal drug of first choice should be loperamide hydrochloride, given in a very low dose to start and gradually increasing until the desired stool consistency is achieved. Loperamide hydrochloride should not be offered to residents with: hard or infrequent stools, acute diarrhoea without a diagnosed cause or an acute flare-up of ulcerative colitis. People unable to tolerate loperamide hydrochloride should be offered codeine phosphate, or co-phenotrope. 84 2. Monitoring & ongoing reassessment Record the specific types of ongoing reassessments and monitoring required in managing the resident’s specific faecal incontinence problem/need: Consider requirements in relation to the identified cause and those required to establish the effectiveness of interventions. • Monitor and record a bowel chart/diary and maintain for one week to provide a baseline of current bowel function. Record the frequency of faecal incontinence, consistency of voided stool (using the Bristol stool chart), presence of mucous/blood.2 ( Note: A bowel chart/diary is a separate document to the Daily Flow Record of Care) • Monitor and record a food and fluid diary/ intake output chart to establish baseline data. Advise resident to modify one food item at a time if attempting to identify potentially contributory factors to their symptoms. See Table 2. • Monitor dehydration/ malnutrition if present refer the reader to the resident’s personalised Dehydration and Fluid Maintenance and Nutritional Care plan. • Monitoring the progress of pelvic floor muscle training requires digital assessment by an appropriately trained healthcare professional who is supervising the treatment. 3. Communication • Promptly communicate monitoring concerns to the resident’s doctor and other members of the MDT as appropriate. Update care plans accordingly • Communicate the resident’s personalised care plan to all those involved in the resident’s direct care. Ensure the resident/significant other is kept up to date 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Educate the resident and their significant other(s) on the resident’s specific type of faecal incontinence and their personalised plan of care. Provide written information where possible and/or provide information in a format that suits the resident’s communication requirements. Refer to RAP 1 Communication, Vision and Hearing.6 Evaluation of care (based on goals specified) • MDT Faecal Incontinence and Continence Promotion Care plans must be evaluated when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking to see if the goals of care are being met. Refer to the ‘Protocol for the Expected Standards of Care’ flow chart and sample ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. 85 86 Bowel Habit: • Encourage bowel emptying after a meal • Ensure toilet facilities are accessible, private, & comfortable & can be used safely with sufficient time allowed • Encourage resident to adopt a sitting or squatting position where possible while emptying the bowel & to avoid straining • Use of easily removable clothing for dexterity problems • Assist the resident to the bathroom. Use aids such as commodes Toilet Access: • Ensure clear access to bathroom Medication Management • Liaise with medical team and pharmacist regarding medication contributing to faecal incontinence (see Table 1) • Administer anti-diarrhoeal drugs as prescribed e.g. Loperamide hydrochloride, codeine phosphate Coping Strategies • Offer the resident emotional / Psychological support • Use of incontinence containment products • Observe and maintain skin integrity Referral to Specialist Continence Service for • Pelvic floor muscle training • Bowel retraining • Specialised dietary assessment & management • Biofeedback • Electrical Stimulation Referral to a Specialist Surgeon for • Specialised assessment e.g. anorectal physiology studies • Surgery If faecal incontinence persists after Initial Management, Resident should be considered for Specialised Management, which may involve Diet: • Assess for malnutrition • Ensure overall diet is balanced • Use a fluid/ food diary/chart. Modify one food at a time • Ensure residents with hard stools &/or dehydration aim for at least 1.5 L daily (unless contraindicated) • Liaise with Medical Team & Dietician regarding modifying type & timing of enteral feed Initial Management Treat: Potential reversible causes of faecal incontinence: faecal loading, treatable causes of diarrhoea, lower gastrointestinal cancer, rectal prolapse and third degree haemorrhoids If Faecal Incontinence persists following Assessment and Treatment of potentially reversible causes commence Protocol for the Expected Care Standards for Faecal Incontinence and Continence Promotion in HSE Older Persons Designated Centres Table 1 Medications associated with Faecal Incontinence as per NICE 2007 Drug (and mechanism) Examples (not an exhaustive list) Drugs altering sphincter tone. • Nitrates • Calcium channel antagonists • Beta-adrenoceptor antagonists (beta-blockers) • Sildenafil • Selective serotonin reuptake inhibitors Broad-spectrum antibiotics (multiple mechanisms). • Cephalosporins • Penicillins • Erythromycin Topical drugs applied to anus (reducing pressure). • • • • Drugs causing profuse loose stools. • • • • Laxatives Metformin Orlistat Selective serotonin reuptake inhibitors • Magnesium-containing antacids • Digoxin Constipating drugs. • • • • • Tranquillisers or hypnotics (reducing alertness). • Benzodiazepines • Tricyclic antidepressants • Selective serotonin euptake inhibitors • Anti-psychotics Glyceryl trinitrate ointment Diltiazem gel Bethanechol cream Botulinum toxin A injection Loperamide Opioids Tricyclic antidepressants Aluminium-containing antacids Codeine 87 Table 2 Food /Drink which may exacerbate faecal incontinence in residents who present with loose stools or rectal loading of soft stool (NICE 2007) Food Type Examples/ Rationale Fibre. Fibre supplements e.g. bulking agents; methylcellulose, ispaghula husk, sterculia or unprocessed bran. Wholegrain cereals/bread (reduce quantities). Porridge/oats may cause fewer problems than whole wheat based cereals. Fruit & Vegetables. Rhubarb, figs, prunes/plums best avoided as they contain natural laxative compounds. Beans, pulses, cabbage & sprouts. Spices. e.g. chilli. Artificial sweeteners. May be found in special diabetic products such as chocolate, biscuits, conserves and in some sugar free items including many nicotine replacement gums. Alcohol. Especially stout, beers and ales. Lactose. A few residents may have some degree of lactase deficiency. Whilst small amounts of milk e.g. in tea or yogurt are often tolerated, an increase in consumption of milk may cause diarrhoea. For more information on lactose intolerance see www.eatwell.gov.uk. Caffeine. Excessive intake of caffeine may loosen stool and thus increase faecal incontinence in some predisposed residents. Vitamin & Excessive doses of vitamin C, magnesium, phosphorous and/or Mineral calcium supplements may increase faecal incontinence. For more Supplements. information see www.eatwell.gov.uk Olestra fat substitute. 88 Can cause loose stool. Figure 1 Types 1 and 2 indicate constipation with 3 and 4 being the "ideal stools" especially the latter, as they are the easiest to pass, and 5–7 being further tending towards diarrhoea or urgency 89 SAMPLE CARE PLAN Topic Heading: Faecal Incontinence and Continence Promotion PROBLEM / NEED IDENTIFICATION Number: Date Signature 01/01/10 Mary expresses fears of never regaining her normal bowel pattern of daily bowel motions after dinner. Mary has faecal Incontinence associated with decreased mobility and faecal loading. Jane Murphy GOAL SPECIFICATION Mary will have a predictable bowel emptying pattern with an ideal consistency stool (Type 3-4 on the Bristol Stool Scale) within one week. Faecal incontinence will be managed & Mary’s skin will remain intact and free from incontinence associated dermatitis & moisture lesions. SPECIFIC INTERVENTIONS Date Signature 01/01/10 • Provide psychological support by use of positive coping strategies. These include: giving information/explanation on the specific plan of personalised care; continence products & choice and information on use; skin care and odour control; counselling services if needed through the social work department and advice on how to talk openly to family/significant others about faecal incontinence and its management (if Mary wishes this). • Mary prescribed Sodium Citrate Micro-enema 5 ml (e.g. Micralax®) 1 daily following dinner for 3 days and 50mls of prune juice twice daily, to clear lower bowel & re-establish bowel pattern. Administer enema as prescribed & ensure Mary is assisted to the toilet and has the call bell. Closely and discreetly supervise Mary while using the toilet post enema, for any signs of weakness, dizziness or nausea and ensure privacy & dignity is maintained. • Commenced on a modified diet (high fibre) to address faecal incontinence associated with faecal loading and overflow. Refer to Mary’s Nutritional Care Plan. • Encourage Mary to do her exercises four times per day as ordered by the physiotherapist. See attached list. To be taken for short walks twice daily. • Continence Products: Mary requires: (state product type & absorbency). • Skin Protection: Following incontinent episodes/defecation, cleanse skin with (state product e.g., Clinisan or Water & Silcocks Base). Apply barrier creams (state product e.g. Petroleum jelly). • Monitor & record: Mary’s tolerance to rectally administered laxatives. • Commenced on an intake/output chart, record consistency of bowel motions/leaks/staining. Monitor amount and consistency of stools evacuated post enema and ask Mary if feels she had a satisfactory bowel clearance. • Check skin at each shift for excoriation / moisture lesions. • Monitor hydration status daily by observing & recording Mary’s urine colour (use the colour code on the daily Record of Care) and encourage at least 8 cups of fluid daily. Record on intake/output chart. • Communication: Promptly report monitoring concerns to the Doctor/MDT. • Information: Provide information sessions to Mary/Significant others on specific type of incontinence, treatment & progress. Jane Murphy EVALUATION OF CARE (based on goals specified) Date Signature 03/01/10 Mary tolerating enemas and had no episodes of faecal incontinence or staining today. Mary is delighted with her progress. Plan continued. Jane Murphy Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 90 Suggested further reading: NICE (2007) Faecal Incontinence The management of faecal incontinence in adults. Methods, Evidence & Guidance www.nice.org References 1 NICE (2007) Quick reference guide. Faecal incontinence. NICE clinical guideline 49 www.nice.org 2 Bardsley, A. (2009) Assessment and management of faecal incontinence, Journal of Community Nursing, 23(4), 4-10 3 Coffey, A., McCarthy, G., McCormack, B., Wright, J., Slater, P., (2007) Incontinence: assessment, diagnosis, and management in two rehabilitation units for older people, Worldviews on Evidence-Based Nursing. 4(4):179-86. 4 NICE (2007) Faecal Incontinence The management of faecal incontinence in adults. Methods, Evidence & Guidance www.nice.org 5 Wilson L. (2003) Continence and older people: the importance of functional assessment, Nursing Older People, 15(4), 22-2 6 HIQA (2009) National Quality Standards for Residential Care Settings for Older People in Ireland 91 Rap 9: Constipation Definitions: Constipation is defined as infrequent bowel movements (typically <3 times per week), difficulty during defecation (straining during more than 25% of bowel movements or a subjective sensation of hard stools), or the sensation of incomplete bowel evacuation.1 RAI Identifiers of Potential Risks: ■ Signs and Symptoms of Dehydration F21, ■ Constipation F23, G11 ■ Difficulty with Bowel Management C18, ■ Bowel disease or overflow G1, ■ Requires assistance to mobilise H1, ■ Palliative care symptoms O6, ■ End of life symptoms P9 Other Risk Factors include: Primary risks/causes: • Dehydration – If there is not enough daily fluid the faeces will become small, hard, dry and difficult to pass. Regular drinks should be offered; approximately eight to ten glasses of fluid a day is required. Unsweetened fruit juices would also help with giving increased fibre. Daily fluid intake is recommended for older persons at 1 ½ litres in 24 hours unless contraindicated by fluid restrictions.2, 3 Fruit juices such as orange and prune juice can help stimulate bowel movements.4 • Lifestyle changes - Issues like reduced privacy, inaccessible toileting facilities and reliance on other people for assistance.5 • Aging may also affect bowel regularity because a slower metabolism results in less intestinal activity and muscle tone. This leads to slack muscles and difficulty in opening the bowels. Encourage residents to have as much regular exercise as possible. Secondary causes: Diseases that cause constipation include neurological and systemic disorders. These disorders can slow the movement of stool through the colon, rectum, or anus as outlined below. • Neurological disorders that may cause constipation include multiple sclerosis, Parkinson’s disease, chronic idiopathic intestinal pseudo-obstruction, stroke, and spinal cord injuries. Systemic disorders include amyloidosis, lupus, and scleroderma. Metabolic and endocrine conditions include diabetes, underactive or overactive thyroid gland, and uremia. • Problems with the colon and rectum. Intestinal obstruction, scar tissue (adhesions), diverticulosis, tumours, colorectal stricture, Hirschsprung's disease or cancer can compress, squeeze, or narrow the intestine and rectum and cause constipation. Many people with irritable bowel syndrome have irregular bowel movements. • Pelvic floor disorders including rectocoeles, pelvic descent, and nonrelaxing puborectalis syndrome may all cause constipation. Iatrogenic causes: This results from various medications and treatments as outlined below: • Pain medications (especially narcotics), antacids that contain aluminum, antispasmodics, antidepressants, iron supplements, diuretics, and anticonvulsants for epilepsy can slow the passage of bowel movements. 92 • • Over time, stimulant laxatives can damage nerve cells in the colon and interfere with the colon's natural ability to contract. Polypharmacy especially with the older person can be associated with constipation. (See Appendix 1). Further Assessments: Document following assessments on admission, if the resident complains of constipation, when the resident’s condition improves or deteriorates and at least three monthly reassess: 1. Assess the resident’s overall risk context (See RAI identifiers and risk factors). 2. Keep bowel records using the flow chart of care to provide a baseline of current bowel function. This should include information on stool consistency. Use the Bristol stool chart to detail consistency. 3. Assess dietary history including fluid intake using a validated tool e.g. MUST or MNA tools. (Refer to RAP 5: Nutritional Status). 4. Refer to the medical practitioner for a general examination. 5. Refer to the pharmacist and the medical practitioner regarding a review of medications, which may be contributing to constipation (See Appendix 1for a table of drugs which may contribute to constipation). 6. If symptoms of constipation persist after initial management, the resident may require further specialized medical / surgical assessment e.g. a digital rectal examination may be required to assess the contents of the rectum and to identify conditions which may cause discomfort such as haemorrhoids or anal fissure.6, 7 7. Develop a multidisciplinary plan of care. Refer to multidisciplinary team as appropriate to assessment findings. Referrals required: Refer to multidisciplinary team as appropriate to assessment findings. • Doctor referral: will be required for all residents with constipation for baseline assessment and management. • Pharmacist and medical review: of medications, refer to Appendix 1. • Dietician referral: is required if constipation is associated with dietary intake or medical conditions e.g. diet related, malnutrition / Enteral feeding or co-morbidities such as irritable bowel, inflammatory bowel disease, etc. • Physiotherapy referral: may be required for constipation exacerbated by mobility problems. • Medical/ surgical specialist consult: may be required for specialised further assessments Record all referrals made on the MDT Referral record and document the reason/outcome of the referral in the narrative notes. Update care plans accordingly. Personalised Care Planning The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to address the cause or risks of constipation, where possible. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. 93 Problem/Need Identification Record the actual or potential constipation problem and its associated or related risk factors. For example; ‘Mary is constipated associated with immobility’. Goal Specification Record: realistic, measurable and obtainable Multi disciplinary team goals. For example; ‘To re- establish Mary’s normal bowel pattern of having bowel movements every second day within 1 week’. Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential constipation problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: The following should be recorded: a) Specific interventions to address the resident’s/significant(s) concerns, preferences, care choices and religious/cultural requirements e.g. the resident may be anxious about the regularity of their bowel movements, or they may have experienced distressful symptoms related to constipation in the past. This can be addressed by providing education and involvement in their plan of care. b) MDT specific care instructions This includes nursing care instructions for addressing constipation and other care instructions from members of the MDT. For example: a dietician’s specific instructions for treatment of constipation associated with nutritional intake. These should be listed here or a photocopy attached to the care plan. It is important to refer the reader to the attached instructions. • Nursing interventions. These may include ensuring that the resident has adequate fluid intake as recommended by the doctor. Ensuring regular exercise as much as is possible depending on the resident’s condition and ability. Ensuring adequate fibre intake. 2. Monitoring and ongoing reassessment • Monitor bowel movements on the Daily Flow Chart of Care • Monitor daily intake of diet using the Daily Flow Chart of Care. The amount taken at each meal is recorded as a %. • Monitor fluid intake using a fluid balance chart. • Monitor specific risk factors as identified for the resident. 3. Communication • Promptly communicate monitoring concerns to the resident’s doctor / dietician or appropriate MDT member. Update care plans accordingly. • Communicate the resident’s personalised care plan to all those involved in the resident’s direct care. Ensure the resident’s significant others/visitors are aware of any problems associated with constipation, if the resident so wishes. Ensure the resident/significant other is kept up to date and involved in care planning. 94 • Educate residents and relatives on the importance of adequate fluid intake, a high fibre diet and regular exercise. The recommended fluid intake is 1 ½ litres in 24 hours unless medically contraindicated. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Educate the resident/significant other(s) on the resident’s specific problem associated with constipation and their personalised plan of care. • Provide written information where possible and/or provide information in a format that suits the resident’s communication requirements (Refer to RAP 1: Communication, Vision and Hearing). Evaluation of Care (based on the goals specified in the care plan) • Constipation care plans must be evaluated when the resident’s condition improves or deteriorates with prevention care plans reviewed at least three monthly. • Evaluate the effectiveness of the care provided by checking to see if the goals of care are being met. Refer to the ‘Protocol for the Expected Standards of Care’ flow chart and sample ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. 95 96 Overall Risk Context Past Medical History Co-morbidities Risk factors Mobility Diet and fluid intake Medication that may be attributing to constipation • Resident’s main concerns • Resident’s goals • Resident’s preferences • Risk Assessments Further Assessments • Keep bowel records using the Flow Chart of Care • Assess dietary history including fluid intake • Refer to medical practitioner for a general examination • Refer to pharmacist and medical practitioner regarding review/assessment of current medications • Further specialized medical/ surgical assessment • Assess needs to maintain Dignity, Respect & Privacy • • • • • • • Nursing Assessment-Document (On admission, if resident’s condition improves or deteriorates and at least 3 monthly) Nursing Assessment No evidence of constipation • Reassess when there is a change in the resident’s condition, if the resident complains of constipation and at a minimum every 3 months Constipated • Identify risk level. • Identify risk factors. • Devise care plan Nursing Diagnosis and their family if the resident so wishes. 11.Level of information given to the resident 10.Privacy and dignity requirements 9. Level of assistance required requirements 8. Recommended daily fluid intake and diet MDT i.e. physio, OT, Dietician etc. 7. Instructions outlined by members of the by the Medical team 6. The medication prescribed for the resident 5. The MDT referrals required & made identified. 4. The Management plan for any risks 3. The Specific Interventions required 2. The identified Goals of care 1. The identified problem(s) / need(s) Implement a “Personal Care” Care plan Document: Nursing Goal & Care planning Goals unmet or Condition Changes • Reassess if condition changes, if the resident complaints of constipation and at least 3 monthly. . Measure outcome against specified goals Goals met • Resident/carer aware of appropriate preventative measures & involved in care decisions. • Resident/carers have Care Plan on Constipation Evaluation, assessment and monitoring Protocol for the Expected Standards in Care for Constipation in HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: Constipation PROBLEM / NEED IDENTIFICATION Number: Date 15/02/10 Mary is constipated associated with immobility Signature Joe Bloogs GOAL SPECIFICATION To re- establish Mary’s normal bowel pattern of daily bowel movements within one week. SPECIFIC INTERVENTIONS Date Signature Joe Bloogs 15/02/10 • Encourage Mary to increase her oral fluid intake to 1 ½ litres over 24 hours and to have 50mls of prune juice twice daily. Record on a fluid balance chart. • May is prescribed 10mls of Lactulose twice daily and Movicol once a day. Monitor the effectiveness of this and review by doctor as required. • Record amount and type of bowel motion on the Daily Flow Chart of Care and enquire with Mary is she feels that her current prescribed treatment is effective. • Liaise with members of the MDT in ensuring that Mary’s medical needs are met • Mary attends physiotherapy every Tuesday and Thursday. Encourage Mary to attend these sessions and establish a regular pattern of mobilisation on the unit with Mary as she can tolerate. Document walks taken in the narrative notes • Mary becomes anxious when she is constipated. Ensure that Mary can call a nurse when required to request assistance • Ensure that Mary’s privacy and dignity are maintained at all times when assisting her with her needs. • Discreetly supervise Mary whilst using the toilet for any signs of weakness. • Monitor the effects of interventions outlined in Mary’s plan of care. • Whilst awaiting dietician review Mary has been commenced on a high fibre diet. Mary enjoys Weetabix and porridge in the mornings. Add linseed to this. Mary practically likes fruit especially apples. • If Mary’s problems persist after initial management refer to medical team. • Monitor hydration status and urine colour. Record urine colour on elimination section on the Daily flow chart of care. EVALUATION OF CARE (based on goals specified) Date Signature Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 97 Appendix 1 Table 1 - Medications associated with constipation Source: World Gastroenterology Guidelines (2007) 98 • Opiates • Anticholinergics • Antidepressants • Antipsychotics • Anticonvulsants • Antacids (aluminum, calcium) • Antihypertensives • Calcium-channel blockers • Diuretics • Ganglionic blockers • Iron supplements • Nonsteroidal antiinflammatory drugs • Cholestyramine Organisation Practice References 1 Basson, M.D (2008) Available at: http:emedicine.medscope.com/article/184704overview 2 Taylor, C. (1997) Constipation and diarrhoea. In: Gastroenterology (eds L. Byrne & T.M.D. Finlay) Churchill Livingstone, Oxford. 3 Day, A. (2001) The nurse’s role in managing constipation. Nursing Standard 16 (8) page 41 – 44. 4 Winney, J (1998) Constipation. Nursing Standard 13 (11) page 49 – 56. 5 Joanna Briggs Institute. Management of constipation in older adults. Best practice: evidence based practice information sheets for health professionals (1999) 3 (1) Page 1 – 6. 6 Hinnriches, M.D & Huseboe, J. (2001) Research based protocol: Management of constipation. Journal of Gerontological Nursing 27 (2) page 17 – 28. 7 World Gastroenterology Organisation Practice Guideline (2007) Page 1 – 10 99 RAP 10: Falls Prevention and Risk Reduction Definitions: A fall is defined as an event whereby an individual comes to rest on the ground or another lower level with or without loss of consciousness.1 RAI Identifiers of Potential Risks: ■ Mobility Impairment C11, H1, ■ Falls History C15, ■ Inappropriate Footwear H3, ■ Impaired Safety Awareness H4, ■ Psychotropic drug use C24, H3, ■ Visual Impairment D8, ■ Cognitive Impairment D11, ■ Low BMI C1 ■ Urinary Incontinence C17, G2 ■ Faecal Incontinence C18, G10 ■ Dizziness H3 ■ Identified Falls Risk H6, ■ Disturbed sleep pattern N9. Other Risk Factors include: ■ Balance deficit, ■ Gait deficit, ■ Fear of falling, ■ Environmental hazards, ■ Number of Medications, ■ Cardiovascular Medications, ■ Muscle weakness, ■ Depression, ■ Orthostatic and postprandial hypotension. The presence of more than one of the above risk factors increases the risk of falling.2 Further Assessments: Document the following assessments on admission, when the resident’s condition improves or deteriorates and at least three monthly: 1. Assess the resident’s past and present medical history for any suggestive or actual risk factors/co-morbidities for falls e.g. history of a falling the last year (resident is classified as high risk if history of recent fall),2 limitations in mobility and functional activities, medications- consider the resident’s medications for possible risks of over sedation or side effects which may cause or exacerbate their fall risk (Refer to RAP 18: Psychotropic Drug Use) 2. Establish if there is a falls history and assess fall risk using a validated tool e.g. STRATIFY, FRASE, FRAT 3. Incontinence assessment (Refer to RAP 7: Urinary Incontinence and Continence Promotion). 4. Assess malnutrition risk using a validated tool e.g. MUST or MNA tools. (Refer to RAP 5P: Nutritional Status) 5. Assess and Observe for signs of confusion or memory decline using a validated tool such as the Mini Mental State Exam, (MMSE) 6. Identify and record manual handling guidelines 7. Assess to ensure the safe use of Bed rails, Lap/safety Belts if their use is indicated (Refer to local policies on Restraint and Bedrail usage) Several sources of information should be used in information/history gathering e.g. discussion with the resident, significant others, transfer letters, contact with/and discussion with the multidisciplinary team. This is especially important for residents with limited mobility or those requiring the use of a mobility aid e.g. Zimmer frame. If the resident has already been seen by a Physiotherapist and/or an Occupational therapist prior to admission, record the date of last review and list/attach their recommendations in the nursing care plan. 100 Referrals required: Residents identified as being at increased risk of falling or present with recurrent falls should be considered for an individualized, multifactoral assessment.2 Refer to the multidisciplinary team as appropriate for further assessment: • Medical referral - cardiovascular examination and medication review, assessment of osteoporosis risk, assessment of visual acuity • Occupational therapy - referral required for seating assessments, environmental hazards assessment and further cognitive assessment • Physiotherapy - assessment of gait, balance and mobility, and muscle weakness, review of current mobility aids • Speech and language - for communication needs • Chiropody/Podiatry /Orthotics referral if specialist foot care and/or specialist footwear is required • Clinical Nurse Specialist in Falls, Behaviour and /or Older person Care • Optician referral may be required if eye sight is impacting on safe mobility • Audiology referral may be required if hearing impairment is impacting on safe mobility • Continence Nurse Specialist referral may be required for assessment of incontinence • Falls Clinic consider a referral to a falls clinic for further assessment and management (Falls Clinics are available in St. James’s Hospital and in the Adelaide Meath incorporating The National Children’s Hospital) Record referrals made on the MDT Referral Record and document the reason/outcome of the referral in the narrative notes. Update care plans accordingly. Personalised Care Planning The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to reduce the risks of falls and fall related injury where possible. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. Problem/Need Identification Record the actual or potential problem and its associated or related risk factors. For example; ‘Linda’s risk of falling is related to her poor safety awareness, cognitive impairment and dementia ’. Goal Specification Record: realistic, measurable and obtainable MDT goals. For example: ‘To reduce Linda’s risk of falls and risk of fall related injuries over a 3 month period’ Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 101 1. Specific MDT interventions: Record: a) The specific interventions to address the resident’s /significant others concerns, preferences and care choices. For example many older people may have a fear of falling and be reluctant to mobilise therefore limiting their level of independence, individual considerations should be addressed in the care plan such as by Providing psychological care/support to address the resident’s fears e.g. fear of falling b) MDT specific care instructions. This includes the nursing care instructions for addressing fall risk reduction for all residents regardless of fall risk: 1) Interventions to reduce fall and injury risk for all residents: • Beds should be maintained at their lowest level • Call bells should be placed within reach of all residents with instructions on their use and constant reminders • Always apply brakes to beds, bed tables, wheelchairs and commodes, etc. • Ensure appropriate footwear • No trailing clothes e.g. dressing gown belts • Encourage residents to mobilise and to participate in functional activities to maintain their abilities and ongoing lifestyle 2) Residents identified as at high falls risk, also consider: • Use of injury prevention devices - ultra low beds • Listening monitor systems • Sensor alarms – chair and bed • Hip Protectors • Record a Falls Diary 3) Physiotherapy instructions for correct use of a specific mobility aid (Individual mobility aids should be labelled and used as recommended) 4) Occupational therapy instructions on appropriate seating for both comfort and mobility 5) Dietitian instructions and ongoing monitoring of nutrition. Refer to RAP 5: Nutritional Status 6) Medical management of: • Osteoporosis risk • Osteoporosis • Regular and ongoing monitoring of medications at least 3 monthly.3 c). Environmental interventions must also be considered: • Prompt management of spillages • Appropriate use of Signage • Avoidance of trailing flexes while cleaning and during maintenance work • Ensure good lighting • Promote a clutter free environment • Appropriate assessment prior to use of bedrails d) MDT specific care instructions in the event of a fall occurring: • Ensure that the resident receives appropriate first aid at the fall site. Assess for shock. • Observe the resident’s neurological status where there is a possible head injury • Refer to the medical team for review 102 • Report and record details of a fall to nursing administration and appropriate other managers • Complete an Incident Report Form and return to the Health and Safety Officer • Record the residents falls in a Falls Diary, this should be maintained in their Resident Care Record • Inform the resident’s significant other of the fall. (With the resident’s consent) • Reassess fall risk • Refer to relevant members of the multidisciplinary team for review • Continue to provide appropriate preventative care 2. Monitoring and ongoing assessment: • Fall risk assessment will be monitored if the improves/deteriorates and at least 3 monthly • Fall risk will be reassessed in the event of a fall occurring • Record a Fall’s Diary resident’s condition 3. Communication: • Communicate the resident’s personalised care plan to all those involved in the resident’s direct care • Promptly communicate monitoring concerns to appropriate members of the MDT and refer the resident to other healthcare professionals as needed • Ensure the resident/significant other is kept up to date and notified promptly (with the resident’s permission) if a fall occurs 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Provide residents/significant others/carers with information (leaflets) on Falls prevention Evaluation of Care (based on goals specified) MDT Fall Prevention and Management Care plans must be evaluated if a fall occurs, when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking to see are the goals of care are being met. Refer to the ‘Protocols of Care Flow Chart’ and Sample Personalised Care Plan in documenting care planning and in providing care. 103 104 At low risk of falls Reassess when there is a change in the residents’ condition and at least 3 monthly. 1. Risk Assessment- Use a fall risk assessment tool FRASE / STRATIFY 2. Consider: • Past Medical History/ Co-morbidities • Falls History • Mobility impairment • Fear of falling • Visual impairment • Cognitive impairment • Urinary Incontinence • Number of Medications-Including psychotropic and cardiac drugs 3. Re-assess 48-72 hours after admission 4. Record level of fall risk on manual handling plan. 5. Assess 24hr equipment needs mobility aids, bed and chair needs (On or within 2hrs of Admission) Nursing Assessment-Document 17. 16. 15. 14. 11. 12. 13. 10. 9. 6. 7. 8. 4. 5. 3. 2. 1. Beds should be maintained at lowest level Call bells should be placed within reach of residents with instructions on their use and constant reminders. Always apply brakes to beds, tables, wheelchairs & commodes, etc. Appropriate footwear No trailing clothes e.g. dressing gown belts Prompt management of spillages Appropriate use of Signage Avoid trailing flexes while cleaning and during maintenance work Encourage residents to mobilise / participate in functional activities and maintain an ongoing lifestyle Individual mobility aids should be labelled and used as recommended Ensure good lighting Promote a clutter free environment Appropriate seating for both comfort and mobility Appropriate assessment prior to use of bedrails Regular and ongoing monitoring of nutrition Regular and ongoing monitoring of medications Advice leaflet on Falls Prevention should be given to all residents/carers on admission Fall / injury prevention for all residents 1. Ensure adherence to fall / injury prevention for all residents 2. Referral to all relevant members of the multidisciplinary team for multifactorial assessment and care planning 3. Encourage compliance with injury prevention devices (low beds, listening monitor systems, sensor alarm – chair and bed) 4. Use of Hip Protectors for residents as indicated and prescribed. 5. Record a falls Diary At high risk of falls Procedure in the event of a fall occurring 1. Ensure that the resident receives appropriate first aid 2. Observe the resident’s neurological status where there is a possible head injury 3. Refer to medical team for review 4. Report and record details of fall to nursing administration and appropriate other managers. 5. Complete Incident Report Form and return to Health and Safety Officer. 6. Update Falls Diary 7. Inform the resident’s significant other of the fall. (With the resident’s consent) 8. Refer to relevant members of the multidisciplinary team for review 9. Continue to provide appropriate preventative care. No falls • Resident/carer aware of appropriate preventative measures & involved in care decisions. • Resident/carers have leaflets on fall prevention/ management. NB: Reassess if condition deteriorate or if a fall occurs Protocol for Fall Prevention and Risk Reduction in HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: Fall Prevention and Risk Reduction PROBLEM / NEED IDENTIFICATION Number: Date 01/01/10 Linda is at high risk of falling, related to reduced mobility, cognitive impairment & impaired safety awareness Signature Jane Murphy GOAL SPECIFICATION To reduce the risk of falls and fall related injury as demonstrated by an absence of falls on three monthly reassessment SPECIFIC INTERVENTIONS Date 11/01/10 • Linda is independently mobile with her Zimmer frame but requires supervision due to impaired safety awareness • Linda needs prompting/ reminding to use her Zimmer frame when mobilising (Individual mobility aids should be labelled and used as recommended) as per physio guidelines -see attached) • Ensure that the call bell is placed within Linda’s reach with instructions on its use and give Linda constant reminders • Encourage Linda to mobilise and participate in functional activities and maintain an ongoing lifestyle • Maintain Linda’s bed at its lowest level at all times • Assessed for safe use of Bedrails - Unsafe to use bedrails on Linda’s bed as due to impaired safety awareness she may attempt to climb over same • Encourage /prompt Linda to wear her hip protector at all times • Encourage /prompt Linda to wear her appropriate footwear when mobilising • Encourage /prompt Linda to use her height adjustable chair when sitting out of bed (as per OT Guidelines- see attached) Monitor & record: ■ Commence recording Falls Diary in the event of a fall occurring ■ Reassess Linda’s fall risk if a fall occurs, if Linda’s mobility level alters and/or 3 monthly Communication: Promptly report monitoring concerns to theDoctor/MDT. Ensure the resident/significant other is kept up to date and notified promp promptly (with the residents permission ) if a fall occurs Information sessions to be provided to Linda & her family. Leaflets on fall prevention given. Signature Jane Murphy EVALUATION OF CARE (based on goals specified) Date 02/01/10 Linda has not had any falls. Plan continued Signature Jane Murphy Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 105 References 106 1 Department of Health and Children (2008) National Strategy for the prevention of falls and fractures in Ireland’s Ageing Population, Summary Conclusions and Recommendations. 2 National Institute for Clinical Excellence 2004 (N.I.C.E) Falls: the Assessment and prevention of falls in Older People Clinical Guideline 21. 3 Health Information and Quality Authority National Quality, HIQA (2009) National Quality Standards for Residential Care Settings for Older people in Ireland. RAP 11: Impaired Ability for Personal Care Definitions: Personal care refers to any care which involves washing, touching or carrying out an invasive procedure that people carry out for themselves. Impaired ability for personal care is defined as being unable to carry out the above for one’s self due to a physical disability, cognitive impairment or emotional status. The elements of Personal Care for this RAP include: • Maintaining the Resident’s functional independence with the activities of living • Maintaining the Resident’s dignity and respect • Personal Cleaning and Dressing • Oral care • Eye Care • Ear Care • Nail care • Hair Care • Foot Care • Self Image • Controlling Body Temperature RAI Identifiers of Potential Risks: Assistance required in Personal Care I1, Cognitive Impairment I2, Hemiparesis I2, Amputation I2, Involuntary Movement I2, Assistance required in choosing appropriate clothing to current temperature I9, Assistance required with Eye Care I10, Assistance required with Ear Care I11, Assistance required with Nail Care I12, Assistance required with Hair Care I13, Assistance required with Foot Care I14, Assistance required with Oral Care F26, Assistance required with Meaningful Activities M1 Other Risk Factors include: Any psychosocial or physical condition that may limit the individual’s ability for personal care such as: 1. Functional / Physical Abilities such as fractures, Arthritis, paresis, tremors, decreased vision, decreased hearing, impaired mobility, etc. 2. Cognitive Abilities such as, Dementia, Acquired Brain Injury, etc. 3. Emotional Abilities such as depression, withdrawal and paranoia. 4. Social/Care practice activities e.g. Any practices which arise from inadequate ongoing assessment and evaluation of the resident’s social, physical and/or clinical need which causes the resident to be deskilled, resulting in a preventable loss of the resident’s functional ability Further Assessments: The focus of further assessments is to identify the resident’s current abilities so that they can be maintained and optimised to prevent loss of independence. The Nurse has a responsibility and a duty of care to adequately assess residents’ ongoing needs and to put appropriate plans in place, which promote the individual resident’s functional abilities and independence. 107 The individual’s ability should be considered and determined in their meaningful activities assessment and weighed against the risks to safety and self identity when planning for their personal care. Document the following assessments on admission, when the resident’s condition improves or deteriorates and at a minimum three monthly: Assess the resident’s: 1. Overall risk context: Bio/psycho/social risks e.g. co-morbidities, medications e.g. sedation level, antidepressants; abilities and limitations in functional activities; psychosocial issues. 2. Functional / Physical Ability assessment using the “Meaningful Activities Assessment”. Residents’ functional level should be identified as: 1. Planned, 2. Exploratory, 3. Sensory, or 4.Reflex. A recognised validated assessment tool such as the Barthel Index can also be used in conjunction with the “Meaningful Activity Assessment”. Assess for the presence of Pain, this may significantly impact on residents’ physical ability. Refer to RAP 16-Pain if present. Assess the resident’s equipment needs; consider what assistive devices may be needed to maximise their functional potential and independence i.e. walking stick, wheelchair, hearing aid, spectacles, modified utensils, non slip mats, long handled shoe horn, shirt buttoner, etc. 3. Cognitive Ability: establish a baseline using a recognised validated assessment tool such as the MMSE. Consider the resident’s abilities to self care and what special requirements may be needed. Assess the resident’s ability for Communication. Consider: Is their ability to communicate impaired? If communication is impaired refer to RAP 1: Communication. 4. Emotional Ability /Status use a recognised validated tool such as the Cohen Mansfield Agitation Inventory. Consider the resident’s Preferences and dislikes for personal care and how best to meet these. Establish from the resident/significant other how they wish their dignity, respect and privacy to be maintained. Consider any Quality of life concerns that the resident may have that may impact on their ability or motivation to participate in self care e.g. pain, social isolation resulting from a depression, malodorous wound causing social embarrassment, continence problems, etc. Refer to the relevant RAPs in these areas to help address the particular issues of concern for the resident. Consider the resident’s self image, is it important to them? How do they like to dress? Which clothes do they favour? Does the resident like to wear make up, perfume/aftershave? 5. Foot care requirements. Consider the resident’s abilities to self care and what special requirements may be needed; Does the resident require the expertise of a chiropodist/ podiatrist? Is the resident a diabetic? Does the resident have a prosthetic device? Can the resident manage their own foot care independently or is minimal assistance/ prompting or total assistance required? 6. Nail care requirements. Consider the resident’s abilities to self care and what special requirements may be needed. Consider: What type of manicure does the resident like? Would the resident like access to a beautician? Would they like their nails painted? What colour would they like? Can the resident manage their own nail care independently or with prompts/minimal assistance? 7. Eye care requirements Consider the resident’s abilities to self care and what special requirements may be needed; e.g. Does the Resident have impaired 108 vision? Does the resident need glasses/contact lenses and are they effective? Can the resident manage their contact lenses, eye drops independently? 8. Ear care requirements: Consider the resident’s abilities to self care and what special requirements may be needed; e.g. Does the resident have impaired hearing? Does the resident need ear syringing to dewax? Do they use a hearing aid that needs maintenance? Do the batteries need to be changed? How much can the resident do for them self? 9. Oral care requirements Consider the resident’s abilities to self care and what special requirements may be needed; e.g. Has the resident been seen by a dentist within the last year? Does the resident wear dentures? Do they fit properly? Do poor fitting dentures impact on their speech or ability to eat/drink? Can they clean their dentures independently? How much assistance is required? 10. Hair Care requirements Consider the resident’s abilities to self care and what special requirements may be needed. Assess how they like their hair styled? Do they have certain accessories they like? How often do they like to see the hairdresser/barber? Consider how much can the resident do for them self? Referrals required: Refer to the multidisciplinary team as appropriate to the resident’s assessment findings. • • • • • • • • OT/Physiotherapist referral required for specialised equipment needs assessments to maximise functioning ability and independence GP/Medical referral for any medical concerns /review of any identified comorbidities that impact on physical, mental and emotional capacity or for a review of medications that may be impacting on functional capacity Speech & Language Therapist referral will be required to maximise impaired communication abilities Chiropody/Podiatry referral required for foot care for residents with diabetes, renal/arterial co-morbidities Ophthalmology referral for any impaired vision Audiologist referral or any impaired hearing Dental referral for any dental issues Doctor, Psychiatry of later life/CNS if available for any mental health issues such as depression, behaviour that challenges, etc. Record all referrals made on the MDT Referral Record and document the reason/outcome of the referral in the narrative notes. Update care plans accordingly. Personalised Care Planning The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to address the cause or risks to the resident’s impaired ability for personal care and to promote the resident’s functional ability and independence, where possible. The MDT includes the resident/significant other(‘s), carers, nurses, doctors and allied health professionals. Problem/Need Identification Record the actual or potential personal care problem and its associated or related risk factors. For example; ‘Joe is at risk of impaired personal hygiene associated with his decreased mobility, diminished manual dexterity and incontinence.’ 109 Goal Specification Record: specific, measurable, realistic, and achievable MDT goals based on assessment of needs. For example; ‘Personal care needs will be demonstrated by Joe having a well groomed appearance daily.” Specific Interventions These are the specific steps taken based on expected standards of care in addressing actual or potential problems associated with impaired ability for personal care. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: Record: a) Specific interventions to address the resident’s/significant(s) concerns, preferences and care choices e.g. Bath, shower, etc and the ways in which the resident’s functional abilities can be maintained and promoted in care b. MDT specific care instructions. This includes the care instructions for addressing any risks associated with the delivery and maintenance of personal care e.g. in the cognitively impaired resident ways to promote their abilities and independence should be explored e.g. if they are handed a bath-mitt instead of a facecloth and their hand is placed on their face, they may be able to wash their own face independently. c. Document any specialised equipment that is required in maintaining/promoting the resident’s independence in personal care e.g., grippers, shirt buttoner, etc. d. Personal Hygiene regime: State the frequency and type of preferred personal hygiene regime. Be specific e.g. shower, bath every day, alternating days etc. Refer to the resident’s functional level and using the appropriate ‘Meaningful Activities’ care plan template, incorporate personal care into the resident’s ‘Meaningful Activities care plan. e. Incontinence present - Refer the reader to the resident’s continence promotion care plan. f. Pain present - Refer the reader to the resident’s pain management care plan. g. Eye care: Outline what residents can do for themselves and any specific instructions given by the optician /Ophthalmologist. h. Ear Care: Outline what residents can do for themselves; include any specific instructions given by the Audiologist. i. Foot Care and Nail Care: Outline what residents can do for themselves and include any specific instructions given by the Chiropodist/Podiatrist based on an ongoing assessment of the needs identified. j. Dental Care Outline any specific instructions given by the Dentist based on an ongoing assessment of the needs identified. k. Hair Care Outline what residents can do for themselves and preferences individual residents may have for their hair style or attending a Hairdresser. l. Self Image Outline any specific instructions given by the Resident or their significant other. m. Controlling Body Temperature Outline any specific action(s) that may be required to monitor and control body temperature. 110 2. Monitoring and ongoing assessment: • Monitor the resident’s ongoing functional ability based on their disease progression and ability to perform tasks • Monitor the resident’s participation and motivation in their care • Monitor the resident’s satisfaction with their care • Monitor the resident’s overall appearance and how well groomed they appear • Monitor any ongoing risk factors associated with co morbidities • Update care plan as appropriate, based on monitoring findings, resident’s satisfaction and their identified needs • Reassess the resident’s needs if there is any change in their overall condition or at a minimum every three months 3. Communication • Discuss and devise the resident’s care plan in conjunction with the resident /significant other. Communicate the resident’s personalised care plan to all those involved in the resident’s direct care. • Ensure any monitoring concerns identified are promptly communicated to all appropriate members of the MDT and refer the resident to other healthcare professionals as needed. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Provide health promotion advice to residents/significant others/carers in order to maximise the resident’s functional independence in their personal care. Evaluation of Care The evaluation of the resident’s care should be based on the goals specified in their individual care plan. All MDT Personal Care Plans must be evaluated when the resident’s condition improves or deteriorates and at a minimum 3 monthly. The effectiveness of the care being provided should be evaluated by checking to see if the goals of care are being met. Refer to the ‘Protocol for the Expected Standards of Care’ flow chart and sample ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. 111 112 • Overall Risk Context • Past Medical History • Co-morbidities • Risk factors • Mobility • Skin Assessment • Pain Assessment • Incontinence Assessment • Resident’s main concerns • Resident’s goals • Resident’s preferences • Risk Assessments • Functional /Physical Ability • Emotional Ability/Status • Cognitive ability • Communication abilities/deficits • Incontinence Assessment Further Assessments • Engagement in Meaningful Activities • Equipment Needs • Preferences /Likes/Dislikes • Foot Care Requirements • Eye Care Requirements • Ear Care Requirements • Oral care Requirements • Quality of Life Concerns • Dignity, Respect & Privacy Requirements Nursing Assessment-Document (On admission, if resident’s condition changes & at a minimum every 3 months) Nursing Assessment Reassess when there is a change in the resident’s condition and at a minimum every 3 months. No Impaired ability for Personal Care 1. Identify risk level. 2. Identify risk factors. 3. Devise a care plan with the resident / significant other which empowers resident’s independence, participation, dignity, choice and self determination. Impaired Ability for personal care Nursing Diagnosis The identified problem(s) / need(s) The identified resident orientated goals of care The Specific Interventions required The Management plan for any risks identified The MDT referrals required & made The MDT Interventions required Refer reader to relevant RAP’s & Care Plans The identified appropriate seating/lifting/specialised equipment identified/required. 9. The Resident’s preferred washing method, and abilities to participate in care. Record preferred frequency for shower, bath, etc 10. The Resident’s preferences in personal care 11. The Resident’s dislikes 12. The Resident’s eye care requirements & their ability to participate in care 13. The Resident’s ear care requirements & their ability to participate in care 14. The Resident’s foot care & nail care requirements & their ability to participate in care 15. The Resident’s dental/oral care requirements& their ability to participate in care 16. The Residents hair care requirements & their ability to participate in care 17. Provide health promotion to residents/significant others & carers in order to maximise functional independence for personal care. 1. 2. 3. 4. 5. 6. 7. 8. Implement a “Personal Care” Care plan Document: Nursing Goal & Care planning Goals unmet or Condition Changes Reassess if condition changes. Measure outcome against specified goals Goals met • Resident/carer aware of appropriate preventative measures & involved in care decisions & care • Resident/carers have Care Plan on Personal Care. Nursing Evaluation Assessment & Monitoring Protocol of the Expected Standards in the Delivery of Personal Care in HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: Personal Care PROBLEM / NEED IDENTIFICATION Number: Page 1 Date Signature 01/01/10 Joe is at high risk of impaired hygiene and personal care related to his immobility, diminished manual dexterity and incontinence Jane Murphy GOAL SPECIFICATION Joe will have a well groomed appearance on daily assessment SPECIFIC INTERVENTIONS Date Signature 01/01/10 • Joe’s main concern(s) for personal care is that he doesn’t like female carers attending to his personal needs so whenever possible a male carer should be assigned to this function. He also experiences a significant amount of back pain on movement Please refer to his Manual Handling & Pain Care Plans. • Joe’s functional abilities Based on Joe’s Meaningful activities assessment, he functions at a planned level. Refer to Joe’s Meaningful Activity Care Plan • Joe’s cognitive ability Joe can be somewhat forgetful and needs to be reminded what he is doing as he becomes easily distracted. • Joe’s preferred method to wash is to have a bath every second day and in between to have an assisted wash. Refer to Joe’s ‘Bathing’ Section in his Meaningful Activity Care Plan and allow Joe to do as much as possible for himself. • Specialised equipment. Joe is unable to mobilise independently and requires two people to walk. Refer to Joe’s Manual Handling Care Plan. • Impaired Manual Dexterity Joe requires assistance with shirt buttons, putting on his shoes and shaving. Please see OT’s instructions attached. • Foot Care - Joe has a number of corns which need attention 3 monthly from the Chiropodist. • Hair Care - Joe likes to have a number 2 hair-cut every six weeks. • Dressing - Joe likes to wear a tie every day with his shirt and trousers. Refer to the ‘Dressing’ Section in Joe’s Meaningful Activity Care Plan. • Pain Assessment/Management: Please refer to Pain Care Plan. • Incontinence: Please see Joes, Continence Promotion Care Plan. • Monitor Joe’s participation and his functional ability in providing self care • Information sessions are to be provided to Joe & his family. Ongoing educational updates are to be provided to Joe’s Carers and significant others. Any alteration in his care needs must be communicated to all carers and significant others. Health promotion will be provided in order to maximise Joe’s independence for his personal care. Jane Murphy EVALUATION OF CARE (based on goals specified) Date Time 02/01/10 13.20 Signature Joe has no problems with the current plan of care and feels all his concerns are being managed well and that he has a good standard of hygiene and is smartly turned out. He has agreed that the current plan of care should remain unchanged. Jane Murphy Discontinued Date: ............../ ............../ 20......... Signature: ................................................ 113 Bibliography The Royal Australian College of General Practitioners (2005) Medical Care of older persons in Residential Care Facilities 4th edition Carnaby, S., Cambridge, P. (2006) Intimate & Personal Care with people with learning disabilities. Chapter 12 Developing Best Practice in Intimate and Personal Care for People with Learning Disabilities. NHS (2009) Common Core Principles to Support Self Care, A Guide to Support Implementation, Skills for Care, Leeds, U.K. www.skillsforcare.org.uk HSE (2008) HSE Transformation Programme- Chronic Illness Framework, HSE Population Health 114 RAP 12: Pressure Ulcer Prevention and Management Definitions: Pressure ulcers (also known as a bed sores, pressure sores and decubitus ulcers) are areas of localised damage to the skin and underlying tissue usually over a bony prominence, as a result of pressure or pressure in combination with shear .1 European Pressure Ulcer Advisory Panel (EPUAP) Categories: (For full definitions of EPUAP/NPUAP categories refer to the EPUAP/NPUAP (2009) Pressure Ulcer Treatment Quick Reference Guide1) Category I Category II Non-Blanchable redness of intact skin. Darkly pigmented skin-colour may differ from surrounding skin. Partial thickness loss of dermis presenting as a shallow ulcer without slough or as a serum filled or sero-sanginous blister. Category III Category IV Full thickness skin loss-Subcutaneous fat may be exposed but bone, tendon or muscles is not. May include slough, undermining or tunnelling Full thickness tissue loss with exposed bone, tendon or muscle, making osteomyelitis or osteitis likely. Slough or eschar may be also present. RAI Identifiers of Potential Risks: Wound Present C10, J1 Impaired mobility H1, Requires prompts, minimal assistance & total assistance in repositioning J4, Pressure ulcer risk identified J2, Pressure Ulcer Present J7, O6, P5 History of a Previous Pressure Ulcer J7, Urinary Incontinence J5, C17, G2, Faecal incontinence C18, G10 Lower extremity oedema E9 Lower extremity circulatory problems E9, Malnutrition C9, F1, Dehydration F21 Other Risk Factors include: Advanced age and age related skin changes, Co-morbidities such as: end stage renal disease, thyroid disease, diabetes mellitus, PVD, hypotension, pyrexia, smoking, stress, using oxygen, having a current fracture2,3,4. Inadequate care practices such as: failure to evaluate the resident’s clinical condition and pressure ulcer risk factors; failure to define and implement interventions that are consistent with the resident’s needs/goals and recognised standards of practice; failure to monitor and evaluate the impact of interventions and failure to revise interventions as appropriate5. 115 Further Assessments: Document the following assessments on admission, when the resident’s condition improves or deteriorates and at least three monthly: 1. Assess the resident’s overall risk context: Bio/psycho/social risks e.g. co-morbidities, medications [e.g., sedation level/steroid use], limitations in functional activities, previous wound history, and psychosocial issues6. 2. Assess Pressure Ulcer risk using a validated tool e.g. Waterlow, Braden tools. 3. Skin inspection. Refer to RAP 13: Skin and Wound Care. 4. Incontinence assessment (Refer to RAP 7- Urinary Incontinence and Continence Promotion). 5. Assess malnutrition risk using a validated tool e.g. MUST or MNA tools. Refer to RAP 5: Nutritional Status. 6. Equipment Assessment (for 24hr period). Consider what is needed for the bed, chair and to protect/offload resident’s heels. Refer to the Regional Guidelines with regard to the Protocol on equipment selection. 7. Repositioning assessment. Assess the level of assistance needed e.g. prompts/staff assistance. Assess the specific frequency of repositioning needed. Pressure Ulcer Present, conduct above assessments and further include: 8. A wound assessment using a formal tool (Refer to RAP 13-Skin and Wound Care). Ensure pressure ulcers are categorised using EPUAP/NPUAP classification system. Assess finger stick blood sugar (to out-rule diabetes), blood pressure, pulse and temperature (check for systemic signs of infection). Assess pertinent blood lab values e.g. FBC. 9. Pain Assessment – using a formal tool. Refer to RAP 16-Pain. Assess quality of life concerns of the resident e.g., insomnia associate with pain, malodour, exudate level, social isolation due to malodour, depression associated with chronic wounds. Referrals required: Refer to the multidisciplinary team as appropriate to assessment findings e.g., Seating pressure ulcers - OT/Physiotherapist referral required for seating assessments. Dietitian referral required for those at risk of/ or with malnutrition and for any resident with a wound. Orthotics referral required for pressure ulcers associated with inappropriate footwear e.g. hammer toes, etc. Vascular referral required for categories III-IV foot ulcers. Plastics referral required for non-healing ulcers. Tissue Viability nurse (if available) for advice on extensive category II pressure ulcers and categories IIIIV pressure ulcers. Record referrals made on the MDT Referral Record and document the reason/outcome of the referral in the narrative notes. Update care plans accordingly. Note: Category II and above pressure ulcers which develop while in residential care must be reported as clinical incidents. Personalised Care Planning: The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to address the cause or risks of pressure ulceration, where possible. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. 116 Problem/Need Identification: Record the actual or potential pressure ulcer problem and its associated or related risk factors. For example; ‘At risk of pressure ulcers associated with immobility’ or ‘High risk of further pressure ulcers related to the presence of an existing category II pressure ulcer’. Goal Specification: Record: realistic, measurable and obtainable MDT goals. For example: ‘To Prevent (further) Pressure Ulcer Development as evidenced by daily skin inspection’. Specific Interventions: These are the specific steps taken based on expected standards of care in addressing actual or potential, pressure ulcer problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: Record the: a) Specific intervention to address the resident’s pressure relief needs, their concerns, and preferences. This includes the nursing care instructions for addressing pressure relief/risk reduction and other care instructions from members of the MDT e.g. a dietitian’s instructions for increased protein intake (pressure ulcer present). Refer the reader to the resident’s Nutritional Care Plan • Record the type of Pressure redistributing equipment required for the resident’s bed, chair and to offload their heels (24 hr period). Record the appropriate settings for manual dial equipment. • Shear/friction reduction/prevention; record the use of profiling beds, the use of ‘knee break’ bed positions when sitting upright (if available) and the use of pressure reducing heel boots. Note: synthetic sheepskin boots or rugs are NOT recommended (they can cause pressure ulcers). Careful manual handling is required. Massaging pressures areas should be avoided (this can cause a pressure ulcer). Refer the reader to the resident’s Manual Handling Care Plan. • Reposition using the 30° tilt method. Record the specific frequency e.g. 2 hourly. Evidence repositioning by the use of a repositioning chart. • Incontinence present - Refer the reader to the resident’s Urinary Incontinence and Continence Promotion Care Plan. 2. Monitoring and ongoing re-assessments: • Pressure Ulcer Present. Record the pressure ulcer category. Monitor the wound and reassess at each dressing change. Refer the reader to the resident’s Wound Assessment and Management Chart. • Pain present. Refer the reader to the resident’s Pain Assessment/Management Care Plan. • Daily skin inspection, assess bony prominences for signs of redness and document findings on the daily Flow Chart of Care. • Pressure ulcer risk reassessment will be reassessed if the resident’s condition improves/deteriorates and at least 3 monthly. 117 • • Malnutrition/dehydration present - Refer the reader to the resident’s Nutritional/Fluid Maintenance Care Plans. Monitor pertinent Lab results. 3. Communication • Communicate the resident’s personalised care plan to all those involved in the resident’s direct care. Ensure the resident/significant other is involved in care planning and is kept up to date. • Promptly communicate monitoring concerns to appropriate members of the MDT and refer the resident to other healthcare professionals as needed. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Provide the resident/significant/carers with information (and leaflets) on pressure ulcer prevention and management7. Evaluation of Care (based on the goals specified in the care plan) MDT Pressure Ulcer Prevention and Management Care plans must be evaluated when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking to see if the goals of care are being met Refer to the ‘Protocol of the Expected Standards of Care’ flow chart and sample ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. 118 119 Nursing Assessment-Document 1. Past medical history/Co-morbidities (e.g. arterial disease increases risk of heel pressure ulcers) and risk factors (pressure [including history of previous pressure ulceration], shear, friction, tissue tolerance, mobility, nutrition & dressing allergies). 2. Pain Assessment & assess resident’s main concerns, goals & preferences. 3. Risk Assessment e.g. Braden, Waterlow Score, Norton Score. 4. Skin Assessment-Inspect pressure areas (bony prominences). 5. Nutritional Risk Assessment e.g. MUST/MNA Score. 6. Incontinence Assessment. 7. Repositioning Assessment. 8. 24 hr Equipment needs assessmentfor bed & chair. Pressure Ulcer Present 9. Remove dressings examine ulcer; size, site, dept, signs of infection & category. Complete a Wound Assessment/ Management Chart. Clinical investigations 10. Investigations to exclude other disorders including; blood pressure, pulse assessment, finger stick blood sugar & blood tests (FBC, U & E, etc) as appropriate. (On admission, if resident’s condition improves or deteriorates and at least 3 monthly) Nursing Assessment • • • 4. 3. 2. 1. Pressure Ulcer Present Requires Pressure Ulcer Prevention & Management Care Plan. Identify factors for delayed healing. Out rule other causes e.g. moisture/ vascular /herpetic lesions etc. Signs of infection present: Swab for C + S Refer to doctor for antibiotics Antimicrobial dressings as appropriate At No Risk Reassess when there is a change in the resident’s condition and at least 3 monthly. At low-high risk 1. Identify risk level. 2. Identify risk factors. 3. Pressure Ulcer Prevention Care Plan required. Nursing Diagnosis Goal: Pressure Ulcer Prevention No Pressure Ulcer Present but resident at risk of Pressure Ulcers. Document: 1. Management plan for risks identified. 2. Skin Inspections (document daily), hygiene & continence care. 3. Nutritional risk reassessment; Low- high risk of malnutrition- follow local policy, guidelines. 4. Select appropriate pressure redistributing equipment for 24hr period. Consider: bed, chair & heels (Use Equipment protocol to guide selection). Consider Seating (immobile residents)refer to OT/Physiotherapist as appropriate 5. Repositioning Regime, record frequency on a repositioning chart. 6. Provide information/education to residents / significant others & carers. Goal: Pressure Ulcer Prevention & Management Pressure Ulcer Present-Resident at High Risk of further Pressure Ulcers. (Include all prevention points mentioned above) 7. Categorise Pressure Ulcers 1-IV-EPUAP Tool & complete Wound Assessment/Management Chart. 8. Monitor pain and provide pain relief 9. Appropriate dressing choice & management of complications e.g. Infection, Necrotic Tissue. 10. Refer all residents with wounds to the doctor and dietitian. Further multidisciplinary referral as appropriate e.g. OT, physiotherapist, orthotics, surgical/ vascular /plastics consult. 11. Refer extensive category II & category III, IV ulcers to the tissue viability nurse if available. 12. Category II and above pressure ulcers which develop while in residential care should be reported as clinical incidents. Nursing Care Goals & Planning Goal unmet ulcer fails to heal or make progress despite MDT input- Referral for surgical/vascular/plastics consult. Goal met ulcer heals• Reassess equipment needs and downgrade if appropriate. • Continue to provide appropriate preventative care. Goal met develops no pressure ulcers • Resident/carer aware of appropriate preventative measures & involved in care decisions. • Resident/carers have leaflets on pressure ulcer prevention/ management. NB Reassess if condition deteriorates. Nursing Evaluation Protocols for Care in the Prevention and Management of Pressure Ulcers in HSE Older Persons Designated Centres SAMPLE (Personalised) CARE PLAN Topic Heading: Pressure Ulcer Prevention & Management Care Plan PROBLEM / NEED IDENTIFICATION Number: Page 1 Date Signature 01/01/10 Cissy is at high risk of pressure ulcer development (or further pressure ulcers), related to immobility & malnutrition (or presence of an existing pressure ulcer) Jane Murphy GOAL SPECIFICATION To prevent (further) pressure ulcer development as evidenced by daily skin inspection. To treat malnutrition. To provide appropriate pressure ulcer prevention and management care strategies. SPECIFIC INTERVENTIONS Date Signature 01/01/10 • • • • • • • • • Cissy’s main concern(s) for pressure ulcer prevention is that she doesn’t like sleeping on her sides. Information given re: repositioning using the 30° tilt method. Cissy states she will “give it a try”. Assess Cissy’s comfort level at each change of position. Cissy is unable to reposition herself independently. Reposition Cissy carefully to prevent shear and friction (state frequency, e.g. 2 hourly) using a 30° tilt while in bed and ½ hourly while sitting out. Refer to Manual Handling Care Plan. Pressure relieving equipment. Cissy to be nursed on: Bed surface - e.g. An alternating overlay (record make/model & settings for manual dial products). Chair - A pressure relieving cushion record make/model). Heels Offload Cissy’s heels (in the bed using e.g. pillows, Heelift Boots®). Cissy is at risk of malnutrition - Refer to Cissy’s Nutritional Care Plan for specific care instructions. Pressure ulcer risk assessments (Waterlow, Braden) must be reassessed (Specify frequency, e.g. 3 monthly) or sooner if Cissy’s Condition improves/deteriorates. Cissy will have a skin inspection for signs of pressure ulcer development recorded & monitored at each nursing shift. Pressure Ulcer Present (record category) - Cissy’s wound will be reassessed at each dressing change and any deterioration will be promptly reported to her doctor/tissue viability nurse. Refer to Cissy’s Wound Chart. Pain Assessment/Management - Refer to Pain Care Plan. Information sessions are to be provided to Cissy & her family. Leaflets on pressure ulcer prevention have been given to them. Ongoing educational updates are to be provided to Cissy’s carers. Jane Murphy EVALUATION OF CARE (based on goals specified) Date Signature 02/01/10 Cissy has no problems with the 30° tilt repositioning regieme. Plan Jane Murphy continued Discontinued Date: …..... / ……… / 20…… Signature: ………………………………………….. 120 Suggested further reading: • • • • HSE (2009) National best practice and evidence based guidelines for wound management European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel (2009) Treatment of Pressure Ulcers: Quick Reference Guide. Washington DC: National Pressure Ulcer Advisory Panel. www.epuap.org European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel (2009) Prevention of Pressure Ulcers: Quick Reference Guide. Washington DC: National Pressure Ulcer Advisory Panel www.epuap.org HSE (2008) Pressure Ulcer Prevention and Management in HSE Older Persons Residential Care Facilities http://hsenet.hse.ie/Hospital_Staff_Hub/mullingar/Policies,_Procedures_Guidelines_ Midland_Area/Care_of_the_Older_Persons/Regional_PPG's/ROP067_Guideline__Pressure_Ulcer_Prevention_and_Management.pdf References: 1 European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel (2009) Treatment of Pressure Ulcers: Quick Reference Guide. Washington DC: National Pressure Ulcer Advisory Panel. www.epuap.org 2 Bryant, A., Nix, D. (2007) Acute & Chronic Wounds, 3rd Eds, Mosby, USA 3 Grey, J., Harding, K. (2006) In ABC of Wound Healing, Oxford, Blackwell publishing 4 Heast, D., Parslow, N., Houghton, P., & Norton, L. (2007) Best Practice Recommendations for the Prevention and Treatment of Pressure Ulcers, Advances in Skin and Wound Care; 20:447-60 5 Rijswijk, L., Lyder, C. (2005) Pressure ulcer prevention and care: implementing the revised guidance to surveyors for long-term care facilities. Ostomy Wound Management, (4): 51-57, (suppl). 6 National Institute for Health and Clinical Excellence (2005) CG29 Pressure ulcer management: RCN guideline, http://www.nice.org.uk/page.aspx?o=cg029fullguideline 7 HSE (2009) National best practice and evidence based guidelines for wound management 121 RAP 13: Skin and Wound Care Definitions: Wounds are defined as an injury resulting in tissue damage, which may or may not result in a loss of intact skin e.g. Category 1 pressure ulcer1. Chronic wounds are wounds of over 4 weeks duration, that have failed to heal2. Wound infection is a bacterial imbalance within or extending from the wound bed3. Diagnosis of wound infection is made on the presenting clinical signs and symptoms of infection, in the local wound bed, deeper structures and in the surrounding skin and not on swab reports4,5. Swab reports guide treatment decision making. Infection can be systemic, regional or local. Signs and symptoms of wound infection may include; • Local signs and symptoms e.g. increased pain/change in the nature of pain, spreading peri-wound erythema, increased exudate, malodour, friable/dark /dusky red granulation tissue (bleeds easily), increased wound dimensions, wound healing becomes static, pocketing of the wound base, bridging of the epithelium and oedema. Treatment with systemic antibiotics is dependent on clinically diagnosed infection and swab results. Local wound infection restricted to the wound bed without infiltration of the surrounding tissues may be treated successfully with antimicrobial dressings alone. Topical antibiotics are generally not recommended in wound care, due to the development of antimicrobial resistance and an increased incidence of sensitivity reactions. • Regional signs and symptoms e.g. cellulitis, myositis, fasicitis, lymphangitis, abscess formation and osteomyelitis. Treat urgently with systemic antibiotics and antimicrobial dressings. • Systemic signs and symptoms of bacteraemia i.e. fever, tachycardia, tachyponea, altered mental state, hypotension and leukocytosis. Treat urgently with systemic antibiotics and antimicrobial wound dressings. RAI Identifiers of Potential Risks: Wound present J1, J7, J6, C10, I14, O6, P5 Other Risk Factors include: Intrinsic risks • Advanced age and age related skin changes. • Co-morbidities e.g. PVD (Venous insufficiency/Arterial Disease), diabetes, end stage renal disease, rheumatoid arthritis, malignancy, anaemia, immobility, cardiac and respiratory conditions increase the risk of chronic wounds such as leg ulcers and pressure ulcers. These medical conditions may further affect systemic and peripheral oxygenation and tissue nutrition, prolonging the healing process5,6. • Acute episodes of illness/medical conditions such as UTIs, respiratory and viral infections, malnutrition, and dehydration further create significant risks for wounds such as pressure ulcers. • Therapies received as part of a prior health condition e.g. radiation therapy, immunosuppression may further impede wound healing2. • Negative psychosocial factors can further impair wound healing e.g. stress/ anxiety/depression associated with altered body image/malodor/healing status. 122 Extrinsic risks8,9 • Medications such as non steroidal anti inflammatories (NSAIDs) and steroids reduce the inflammatory response and delay wound healing. • Smoking impedes wound healing. • Inadequate care practices. For example: – Moisture lesions caused by inadequate hygiene care practices (i.e. inadequate cleansing, drying and skin protection practices) – Avoidable pressure ulcers (inadequate pressure ulcer prevention practices). – Avoidable leg ulcers (non compliance of staff/residents with the use of prescribed compression hosiery for healed venous leg ulcers). – Negative attitudes of staff to treatment and healing. – Failure of staff to identify and correct the underlying cause of the wound where possible. – Use of inappropriate treatment modalities. Further Assessments: Holistic wound assessment is needed to: • Identify the cause of the wound • Provide a clear picture of what the wound looks like (baseline information) • Provide a comprehensive picture of the resident • Identify contributory factors • Communicate findings to other health care professionals • Allow for continuity of care • Have a centralised location for wound care information • Identify what specific personalised care planning is required • Identify complications as they arise Assess 1. The resident’s overall risk context: Consider the resident’s bio/psycho/social risks which may be treatable e.g. co-morbidities, medications, blood profiles, limitations in functional activities (immobility), malnutrition risk, pressure ulcer risk, previous wound history, known dressing allergies and psychosocial issues6. 2. Skin Assessment: A thorough, head to toe nursing assessment/examination is required • Assess all skin areas and pressure points for signs of tissue damage/wounds. • Note the presence of existing wounds and old scars. • Note the appearance of the skin, nail and hair on the extremities (in arterial disease, lower limbs may be hairless, with shiny skin and thickened toenails). • Note the presence of bruises (e.g. senile purpura [aged related], steroid or anticoagulant induced) which indicates the resident’s skin is very fragile and at high risk of skin tears. • Assess feet and note the presence of wounds and/or callus formation (thickened, hard skin which can result in pressure related, ulcer formation underneath the callus). To prevent foot ulcers especially in diabetics, it is essential that calluses/corns are promptly removed or reduced by a podiatrist/chiropodist. • Evaluate skin colour, temperature, capillary refill, pulses and oedema. 123 3. Wound Assessment (use a Wound Assessment/Management Chart). Record the: • Type and identified cause of the wound e.g. Venous Leg ulcer, Arterial Leg ulcer, pressure ulcer. Categorise all pressure ulcers using the EPUAP / NPUAP classification system. Refer to RAP 12: Pressure Ulcer Prevention and Management. • Location. • Duration of the wound (days/weeks/months/years). • Size- measure width, length and depth or trace wound. In cavity wounds assess for sinus/fistula formation and/or undermining of the wound edges. • Type of tissue in the wound bed. Record in percentages – epithialisation %, granulation %, slough %, necrotic %. Refer to the Wound Bed Descriptions chart. • Condition of wound edges and surrounding skin. • Amount and type of exudate. – Low exudate levels: is understood as requiring dressings once per week. – Moderate exudate levels: is understood as requiring dressings twice weekly. – A high exudate level: is to be understood as requiring three or more dressings per week. • Record the type of exudate: serous, serous sanguineous, purulent, haemopurulent. • Odour: Note type e.g. foul (may indicate the presence of anaerobic bacteria- select antimicrobial dressings), sweet smelling (may indicate the presence of pseudomonas especially if it is associated with a bright blue-green exudate). • Pain, soreness or discomfort associated with the resident’s wound; assess using a formal pain assessment tool. Refer to RAP 16: Pain. • Signs of Infection refer to the definitions section for expected standards in care. Referrals required: Assess the resident’s specific referral needs in relation to their specific wound type. Consider: the cause of the wound and the MDT members that are likely to be needed to improve or maintain the resident’s quality of life. • A doctor and dietetics referral is required for all residents with a wound. Repeat referrals are required if the wound deteriorates or stops healing (becomes static). • A vascular referral and assessment by a competent practitioner (e.g. Nurse-led Leg Ulcer Services or a Vascular Consultant) is required for residents with below knee leg wounds that are at high risk of developing leg ulcers e.g. residents with diabetes, renal disease, arterial disease, evidence of venous disease such as varicose veins, brown staining on legs, or for all residents whose below knee wound fails to heal within 4 weeks. • A plastics consult, vascular or tissue viability nurse consult (if available) is required for residents with non- healing, static wounds (no decrease in wound dimensions for 6 weeks) or wounds that are deteriorating. • A dermatology consult is required for wounds originating from primary skin conditions e.g. carcinomas, eczema. • Physiotherapy/OT referrals may be required for seating assessments e.g. pressure ulcers related to inappropriate chair/seating equipment. • Orthotics referral may be required for special footwear e.g. wounds originating from footwear (e.g. foot deformity/hammer toes and footwear causing pressure). 124 • Other referrals may be required to improve/stabilise the resident’s underlying co-morbidities or to treat risks. For example an Endocrinology referral is required for diabetic foot ulcers. A Podiatry referral is required for callus removal and advice on the treatment of diabetic foot ulcers (such as offloading using total contact casts/boots). A Rheumatology referral is required for vasculitic or rheumatoid leg ulcers, etc. Personalised Care Planning: In providing care to residents with wounds it is firstly essential to identify the type of wound being managed. Different wound types require different therapeutic management e.g. compression therapy for venous leg ulcers, offloading heels with pressure ulcers. The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to treat the underlying cause of the wound and address actual or potential risks, where possible. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. Problem/Need Identification: Record the actual or potential wound problem and its associated or related risk factors. For example; (‘Joe is at high risk of skin tears associated with age-related skin changes’ or ‘Mary has a venous leg ulcer related to long standing venous hypertension’ or ‘Tim has an inoperable malodorous cancerous wound on his left lower arm’). Goal Specification: Record: realistic, measurable and obtainable MDT goals. For example: ‘Joe will not develop skin tears’ or ‘Mary’s will have reduced wound dimensions by 6 weeks’ or ‘To manage Tim’s wound exudate and wound odour and to maintain Tim’s comfort. This will be demonstrated by an odour free wound within two weeks and by Tim expressing his pain/comfort levels as acceptable to him’. Specific Interventions: These are the specific steps taken based on expected standards of care in addressing actual or potential wound problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: Record: a) Specific interventions to address residents/significant(s) concerns, preferences and care choices; For example: Pain (must be assessed and addressed refer to RAP 16: Pain), Malodour (identify the cause and treat appropriately e.g. necrotic tissue, refer to Section: Wound Bed Descriptions, Treatment Aims & Dressing Selection), Fears/worries (provide psychological support using positive coping strategies. This includes the provision of: • Information/explanation to the resident on their specific plan of personalised care. • Information and choice on the use of wound care products. • Advice on skin care and odour control. • Accessing counselling services if required by the resident. 125 b) MDT specific care instructions. This includes the nursing care instructions for addressing the specific wound risks/problems and other MDT care instructions e.g. A dietitian’s specific instructions, refer the reader to the resident’s nutritional personalised care plan. • Skin Care for Older People i. Avoid soap in older persons’ care5,6. Soaps can dehydrate the skin causing dryness, affect pH balance and may impair bacterial resistance6. Use an emollient for washing residents such as Aqueous Cream or Silcock’s Base. Ensure each resident has their own individual tube of emollient. Apply emollients in the direction of hair growth; rinse skin and pat dry (never rub the skin vigorously). Re-apply emollient as a moisturiser to the skin twice daily. ii. Apply barrier products sparingly to groin/anal region for those who are incontinent or in skin areas likely to have high moisture (skin folds, under breasts). Example of barrier products include: Vaseline®, Petroleum jelly, Sprilon Spray®, Triple Care®. Refer to Moisture lesions in Wound Bed, Dressing Selection and Treatment section for further information. iii. Avoid dusting powders and talc. Dusting powders should not be applied to moist areas because they can cake and abrade the skin6. Talc is a lubricant and does not absorb moisture; it is not a barrier product and should be avoided. • Equipment required specific to the wound type. Consider: • Pressure relieving/redistributing equipment required. Refer to RAP 12- Pressure Ulcer Prevention and Management. • Dressings required, refer to section: Wound Bed Descriptions, Treatment Aims and Dressing Selection. • Prevention of skin tears: consider: i. Equipment risks and remove where possible e.g. lockers, etc. ii. Need for padded bed rails, shin protectors, long sleeve clothing. iii. Careful use of hoists/slings and careful manual handling practices. iv. Consider staff manual handling practices. The wearing of engagement rings, watches jewelry, false nails or having long nails must be avoided. 2. Monitoring and ongoing reassessment • Reassess the resident’s wound at each dressing change. Refer the reader to the resident’s wound assessment and management chart. Measure wounds at least weekly. • Record a finger stick blood sugar for all residents who have a wound. • Pressure ulcer risk present; refer the reader to the pressure ulcer prevention care plan. • Malnutrition/dehydration present; refer the reader to Nutritional, Fluid Maintenance Care Plans. • Incontinence present; refer the reader to the resident’s Incontinence and Continence Promotion Care Plan. • Pertinent Lab results e.g. FBC, U&E. 3. Communication • Promptly communicate monitoring concerns to the resident’s doctor and appropriate members of the MDT. Update care plans accordingly. • Communicate the resident’s personalised care plan to all those involved in the resident’s direct care. Ensure the resident/significant other is involved in care planning and is kept up to date. 126 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers. • Provide information to the resident/significant other(s) if they so wish on: – Their wound type, monitoring and progress. – Strategies to promote healing, prevent reoccurrence and maintain comfort e.g. offloading/repositioning for pressure ulcers. – Care of Older Persons’ skin. – The importance of nutrition and hydration in wound healing. • Information should be given in a suitable format that meets the resident’s communication requirements and in written format where possible7. Refer to RAP 1: Communication, Vision and Hearing. Evaluation of care: (based on goals specified) • • Wound Prevention Care plans must be evaluated when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the wound at each dressing change. Compare the current wound assessment to the previous assessment and to the initial baseline assessment, to evaluate the effectiveness of care Refer to the ‘Protocol of Expected Standards in Wound Care, Wound Bed Descriptions, Treatment Aims and Dressing Selection’ and sample ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. Please note: • In the following section “Wound Bed Descriptions, Treatment Aims and Dressing Selection” deals with the main wound types encountered in Older Persons Care. Refer to RAP 13 for Pressure Ulcer Prevention and Management. • Products listed are in alphabetical order and are given as examples of generic product types. The HSE does not endorse any specific wound products. • Dressings are classified as medical devices and do not require a doctor’s prescription. In ordering products from HSE Central Pharmacy please ensure that similar generic dressings on contract are ordered. • Never apply a dressing in ignorance. Always read the manufactures instructions and contra-indications, this is especially pertinent for antimicrobial dressings such as Iodine based dressings. 127 128 Nursing Assessment-Document 1. Past medical history/Co-morbidities. • Assess risks for wounds: e.g. PVD (increase risk of arterial/venous leg ulcers), diabetes (increase risk of leg/foot ulcers), history of recurrent wounds, assess pressure ulcer risk & incontinence. • Assess risks for delayed healing: e.g. psychosocial factors (e.g. stress) comorbidities (e.g. anaemia), medications (e.g. steroids), smoking, dressing allergies & mobility. Assess hydration status and nutritional risk. 2. Skin Assessment: Check all skin areas, pressure points & feet. Note: presence of wounds, scars, bruises (Senile, steroid or anticoagulant induced purpura), calluses/corns, appearance of the skin, nails & hair on extremities (shiny/hairless/ thickened toenails suggestive of arterial disease). Assess skin colour, dryness, fragility, temperature, capillary refill, pulses and oedema. 3. Wound Assessment: Assess: duration, site, size, wound bed tissue type, exudate, odour & signs of infection. Complete a Wound Assessment/ Management Chart. 4. Investigations to exclude other disorders e.g. ABPI, B/P, pulse, finger stick blood sugar & blood tests e.g. FBC, U & E, as appropriate. (On admission, remove dressings, assess Wounds at each dressing change) Nursing Assessment Wound Present 1. Identify the type of wound 2. Identify risk factors for delayed healing. 3. Requires a Wound Assessment & Management Care Plan. 4. Clinical Signs of infection present: • Swab for C + S • Refer to doctor for antibiotics • Antimicrobial dressings as appropriate At No Risk of Further Wounds Reassess when there is a change in the resident’s condition and at least 3 monthly At Risk of Further Wounds 1. Identify risk factors. 2. Develop a MDT Wound Prevention Plan of personalised Care Nursing Diagnosis Goal-Wound Prevention No wound present but resident at risk of wound e.g. skin tears/leg ulcer. Document: 1. MDT management plan for identified risks, Consider MDT referrals required & specific care instructions. 2. Skin/feet inspections (document daily). 3. Skin Care: Avoid soap & talc. Wash with an emollient e.g. Silcocks Base, Aqueous Cream, rinse & pat dry skin. Moisturise skin twice daily. 4. Incontinence care/continence promotion, refer to RAPs: 6 & 7. 5. Pressure Ulcer Risk -Refer to RAP 12. 6. Nutritional Risk - Refer to RAP 5. 7. Select appropriate preventative equipment, devices & products for the 24hr period. Consider: specific resident needs in relation to their wound type e.g. compression hosiery for venous leg ulcer prevention. 8. Consider environmental hazards & remove if possible. 9. Provide information/education to residents/significant others & carers. Goal- Wound Prevention & Management (Wound present-Include all prevention points above) 10. Complete a Wound Assessment/Management Chart. Measure wound at least weekly. 11. Monitor & address resident’s pain, if in doubt assume all wounds are painful. 12. Monitor & address resident’s/significant other(‘s) specific wound related concerns. 13. Use appropriate dressings & manage complications e.g. Infection, Necrotic Tissue. Refer to Wound Bed Descriptions, Treatment Aims & Dressing Selection. 14. Refer all residents with wounds to the doctor and dietitian. Further MDT referral as appropriate to specific wound type e.g. TVN, OT, Physiotherapist, Orthotics, Surgical/ Vascular/Plastics consult. Nursing Care Goals & Planning Goal unmet-Wound Fails to Heal or make progress despite multidisciplinary input- Referral for Surgical/ Vascular/ Plastics consult. Goal met-Wound heals • Reassess equipment needs and downgrade if appropriate. • Update Care Plan. • Continue to provide appropriate preventative care. Goal met-Develops no Wound • Resident/carer aware of appropriate preventative measures & involved in care decisions. • Continue with Wound Prevention Care Plan. • NB Reassess if condition deteriorates. Nursing Evaluation Protocol for Expected Standards in Wound Care in HSE Older Persons Designated Centres Wound Bed Descriptions, Treatment Aims & Dressing Selection Epithealialising Wound Bed Healthy Granulating Wound Beds Wound Bed Treatment Aims To protect from infection and injury, promote complete epithialisation and comfort. Pain must be assessed/addressed. Wound Bed Treatment Aims To protect from infection and injury, promote further granulation tissue/epithelialisation, manage exudate and provide comfort. Pain must be assessed & addressed. Dressing Selection Low/non-adherent dressing e.g. Adaptic, Atramun, Tricotex (requires secondary dressing) or a foam adhesive e.g. Allevyn, Biatain, Mepilex Tegaderm, or Thin Hydrocolloid e.g. Duoderm. For Fragile skin consider Silicone dressing e.g. Allevyn Gentle®, Mepilex®. Dressing Selection Low to moderate exudate: Foam adhesive e.g. Allevyn, Biatain Tegaderm or for Fragile skin consider a Silcone dressing e.g. Allevyn Gentle®, Mepilex® High exudate: Use a primary dressing first such as a hydrofibre e.g. Aquacel or an alginate e.g. Algisite M/ Kaltostat, Sorbsan. Secondary dressings: Use a foam adhesive e.g. Allevyn, Biatain, Tegaderm. For fragile skin consider Silicone-based dressings e.g. Allevyn Gentle®, Mepilex®. Sloughy Wound Bed Necrotic Wounds Wound Bed Treatment Aims To remove slough through autolysis and promote granulation and wound closure. Pain must be assessed/addressed. Wound Bed Treatment Aims Identify cause of necrosis & determine vascular status of wound (i.e. an adequate blood supply). Vascular assessment/referral required for all below knee necrotic wounds. Pain must be assessed & addressed. For healable wounds, debridement is the aim. Dressing Selection Low Exudate: hydrogel e.g. Granugel, Intrasite Gel, Nu-Gel & secondary dressing. Moderate-High Exudate: alginates e.g. Algisite M/Kaltostat or a hydrofibre dressing such as Aquacel. Secondary dressings: Use a foam adhesive e.g. Allevyn, Biatain, Tegaderm. For fragile skin consider Silicone-based dressings e.g. Allevyn Gentle®, Mepilex® Dressing Selection Awaiting vascular consult Keep all necrotic leg wounds clean and dry. Apply a dry dressing e.g. Inadine, Betadine spray, low non adherent dressing & bandage loosely with absorbent padding roll e.g. Soffban, Surepress. This can be held in place with a loose retention sock e.g. Netelast or loose cling bandage. Hydrogels are contraindicated due to the risk of ‘wet’ gangrene & sepsis. For wounds with a good blood supply & Low exudate: consider a hydrogel e.g. Granugel, Intrasite gel & secondary dressing. Moderate-High exudate: consider an alginate e.g. Algisite M, Sorbsan or a hydrofibre dressing e.g. Aquacel [GMS].Sharp debridement should be considered and executed by an experienced person. 129 Wound Bed Descriptions, Treatment Aims & Dressing Selection Cavity Wound 130 Wound Infection Wound Bed Treatment Aims Management of exudates. Protection of surrounding skin. Removal of devitalized tissue. Promotion of granulation from the base of the wound. Assess wound edges for presence of undermining, fistula or sinus formation (measure depth in all angles). Pain must be assessed/addressed. Wound Bed Treatment Aims To address local & systemic treatment of infection. (Assess resident for signs of systemic infection e.g. pyrexia, nausea, confusion etc., ensure a prompt Medical review and antibiotic cover [may need IV antibiotics & surgical debridement], send swab for culture). Manage wound exudate/odour. Pain must be assessed & addressed. Dressing Selection Dry granulating cavity: Fill cavity loosely with a hydrofibre ribbon e.g. Aquacel ribbon moistened with a hydrogel or fill cavity with hydrogel first. Low to moderate exudate: Fill cavity loosely with a dry hydrofibre e.g. Aquacel ribbon, if exudate very low consider the addition of a hydrogel. Heavy exudate: Use an alginate rope e.g. Algisite M rope/Kaltostat/ Sorbsan cavity or hydrofibre ribbon e.g. Aquacel. Infected cavity: silver dressing e.g. Aquacel Ag Ribbon or a silver alginate e.g. Acticoat absorbent rope. Secondary dressings: Use a foam adhesive e.g. Allevyn, Biatain, Tegaderm. For fragile skin consider Silicone-based dressings e.g. Allevyn Gentle®, Mepilex®. Dressing Selection Low to moderate exudate: use an antimicrobial dressings e.g. Iodine-based (Inadine, Iodoflex) or silver-based e.g. Acticoat, Aquacel Ag Contreet Ag, or hospital grade mannuka honey & a secondary dressing as for sloughy wounds. Moderate to heavy exudate: use antimicrobial dressings e.g. Iodine- based (Iodoflex) or silver based (Acticoat absorbent, Aquacel Ag) or hospital grade Mannuka honey & cover with dressing as for primary dressings in sloughy wounds. Secondary dressings: Use a foam adhesive e.g. Allevyn, Biatain, Tegaderm. For fragile skin consider Silicone-based dressings e.g. Allevyn Gentle®, Mepilex®. Wound Bed Descriptions, Treatment Aims & Dressing Selection Skin Tear Moisture Lesions Treatment Aims Stop bleeding. Prevent infection. Minimise pain & discomfort. Recover skin integrity. Prevent reoccurrence. Assess environment. Pain must be assessed/addressed. Treatment Aims To treat underlying cause e.g. diarrhoea, etc. To promote resident comfort & treat pain. To promote good skin care protocols. To prevent further skin damage. Treatment & dressings Identify category of skin tear using Payne Martin Classification System (1993): Category I: Skin tear fully approximates the wound. Category II: Skin tear with partial thickness skin loss. Category III: Skin tear with complete tissue loss. Local Wound Treatment: Cover wound with a sterile pad and apply light pressure until bleeding stops. If flap rolled up & dried out remove aseptically. If flap viable or partially viable, cleanse with saline/potable water & roll flap back into place to achieve optimum cover. If edges approximate secure flap over wound using: adhesive wound closure strips, skin glue, silicone-on-adhesive dressings & apply an appropriate secondary dressing for fragile skin e.g. Mepilex® range or Allevyn® Gentle range or a non adherent dressing, padding and a loose bandage. If flap partially covers wound, treat open wound as per wound bed presentation and only apply a fragile skin dressing as above. All other dressings, adhesive tapes should be avoided. Provide ongoing assessment & evaluation of healing. Other Consideration: Determine cause & remove if possible e.g., use padded bed rails, move lockers, etc. Skin Care Regime- avoid soap, wash and moisturise with emollient e.g. Silcocks Base, Use long sleeves, careful & gentle manual handling, use of padded shin protectors. Document Prevention & Management Plan. Treatment & dressings • Document incontinence assessment & skin condition. Consider secondary fungal infection (presence of satellite spots) swab if present & send for fungal cultures. Refer resident to the doctor for anti fungal treatment. If skin is ‘burned’ in appearance (as above) consider addition of a corticosteroid such as Daktacort. • Develop & implement individualised program of skin/incontinence care & continence promotion. Consider temporary urinary catheterisation for extensive moisture lesions • After each incontinent episode cleanse skin with a pH balanced cleanser e.g. Clinisan®, Silcocks Base, do not rub skin vigorously. Avoid soap & talc. • Gently apply a barrier ointment/ cream such as Emulsifying Ointment, Triple Care®, Zinc Ointment or Cream. For wet, weeping areas a light coat of skin barrier powder e.g. Orahesive powder® applied first may increase adherence of the moisture barrier ointment/cream. • For moisture lesions in skin folds; twice daily skin care is recommended. Cleanse as above, pat dry and thinly apply a barrier cream. Separate skin folds with cotton wound pads to prevent friction & moisture. • Moisture lesions in the groin area require skin care post defecation & after voiding urine. • Encourage fluids & diet. • Assess and address pain. 131 Wound Bed Descriptions, Treatment Aims & Dressing Selection 132 Venous Leg Ulcer Arterial Leg Ulcers Wound Bed Treatment Aims Vascular Assessment to establish if the leg has an adequate blood supply to support compression therapy i.e. Ankle brachial Pressure Index (ABPI) >0.8. Following a holistic vascular assessment by a competent health professional, compression therapy will be advised. Wound treatment is aimed at managing venous insufficiency through compression therapy by improving venous return and managing oedema. Local wound treatment aims are the same as those listed in ‘Wound Bed Descriptions’. Pain must be assessed/addressed. Wound Bed Treatment Aims Revascularisation of the limb (Vascular Consult). While awaiting vascular consult dress wound according to necrotic wound bed presentation. For those where revascularisation or amputation is not a viable option, the Vascular team may decide on Palliative Care. The aim here is to maintain resident’s comfort, disturb dressing as little as possible, provide good pain relief, manage odour & exudate & provide resident/significant other with psychological support. Pain must be assessed & addressed, if pain is uncontrolled despite best efforts residents must be referred to the local Palliative Care Team/Pain Consultants for analgesia advice. Skin Care & Dressing Selection • Good skin care is essential. Wash leg(s) with an emollient e.g. emulsifying ointment (steep legs in warm [drinking] water or shower with potable water if available). Gently remove any loose, flaky, skin scales. Rinse skin and pat dry. Moisturise from below knee to toes using an emollient e.g. Paraffin gel, emulsifying ointment. • Assess bony prominences for signs of pressure damage from bandages e.g. tibial crest, heel, malleoli etc. These areas may require extra padding. • Assess for signs of allergy to bandages; itchy, red rash from below knee to toes. If noticed apply a cotton sock (e.g. Tubiton 78) underneath compression bandages (below knee to base of toes). • Assess wound bed & apply dressing according to wound bed description. • Measure ankle circumference. • Apply compression therapy as advised & provide frequent circulation checks. Please note: compression therapy requires training; inappropriately applied compression therapy can lead to tissue necrosis and may result in amputation. Contact company reps for onsite training. Post Healing: Compression hosiery as advised to prevent reoccurrence. Dressing Selection in Palliative Care • The aim of care is to keep the wound dry. • Ensure pain relief is provided at least 1 hr before dressing. These wounds are extremely painful. • If eschar (necrotic area) is intact and dry, keep area dry & apply a non-adherent dressing such as Tricotex & a secondary dressing (see below). • If eschar is separating from the sides, use a dry antimicrobial dressing such as Inadine, Betadine spray, Acticoat. Iodoflex (paste dressing) is not recommended. Please note in some individuals Iodine causes pain.Do not use for these residents. • If necrotic area is wet, malodorous and exudating, apply a non-adherent antimicrobial dressing such as Acticoat, Inadine Or an activated charcoal (absorbs odour) e.g., Actisorb® Silver 200. Consider use of Metronidazole (Metrotop® (prescription only)-only use in wet, malodorous, necrotic wounds. Do not use in dry necrotic wounds). Consider use of plug in ‘Air Fresheners’ in resident’s room. • If wound continues to be painful despite analgesic interventions or while awaiting review by Palliative Care Team/Pain Consultant, consider applying Instillagel® (prescription only & only suitable for wet, wounds. Do not use on dry, necrotic wounds) or use Biatain-Ibu dressings (releases ibuprofen). • Secondary dressings: bandage loosely with absorbent padding roll e.g. Soffban, Surepress. Cover with a loose retention sock e.g. Netelast or a loose cling bandage. Dress weekly or sooner if exudate breakthrough. SAMPLE: Wound Assessment and Management Chart Initial Assessment Details Type of Wound: Venous Leg Ulcer Name: Margaret (Cissy) McDermott Duration of Wound: Ward: The Aspens 2 months Location of Wound: Right Medial Gaiter Date: 11/01/2010 Nutrition: MUST Score: 4 Please state: 1) Is a dietician available to refer this resident to? Yes 2) Referred to Dietician: Yes 3) No dietician Available. Hospital/ Community guidelines dietary plan for resident: Yes/No D.O.B.: 08/08/1932 M.R.N. No: 00124x G.P./C.O.H.: Dr. McEvoy Community Hospital: The Burren Factors Which May Delay Healing (Tick If Present) This is Not a Definitive List Rheumatoid Arthritis Diabetes Mellitus Cardiac Disease Anaemia Reduced Tissue Perfusion Chronic Breathing Difficulties Malabsorption Syndrome Wound Infection Present Foreign Body Radiotherapy Immobility Allergies: Drugs Steroids N.S.A.I.D.S Cytotoxic Immunosuppresents Anticoagulants Smoker Other Dressing Allergies: None Known Finger Stick Blood Sugar: B.P.: 130/90mmhg Braden Scale: No No No No No No No No No No No No Yes No No No No No Adhesive Tapes 4.5mmols/L 16 Ankle Brachial Pressue Index: Date: 24/11/09 Signature of Assessing Nurse: Right: 1.1 Left: 1.2 Jane Murphy 133 Sample Wound Assessment Chart Resident Name: Margaret (Cissy) McDermott Wound: Right Medial Gaiter Venous Leg Ulcer DATE 11/01/2010 SIZE (cms) Length Width Depth Trace: Yes/No 4cms 2cms Superficial Yes Wound Bed % (Chart Letter) A. Granulation (Red) B. Epithelialisation (Pink) C. Slough (yellow) D. Necrotic (Black) 80% 10% 10% 0% Exudate A. What Colour B. Amount Mild/Moderate/Severe C. Odour (1) None (2) Some (3) Offensive D. Maceration Yes/No Infection (Chart Letter) A. Nil B. Suspected-Swab sent C. Confirmed D. Doctor notified Yes/No Surrounding Skin A. Cellulitis Yes/No B. Eczema Wet/Dry C. Erythema (measure distance from wound Oedema A. Mild B. Moderate C. Severe D. None Pain Severity (0-None 10=Extreme) A. Continuous B. Intermittent C. Increased at dressings D. Unable to verbalise, demonstrates pain by facial expression (Use Pain Faces Score) or by moaning, crying etc. Signature of Nurse 134 MRN No: 00124x Serous Mild 1 None A A=No B=None C=0.5cms B B=1 to 2 Jane Murphy Page No: ___ Sample Wound Assessment Chart Resident Name: Margaret (Cissy) McDermott Wound: MRN No: 00124x Page No: ___ Right Medial Gaiter Venous Leg Ulcer Date:11/01/2010 Treatment Objective Date: Date: To address venous insufficiency. To debride slough and promote granulation tissue. Type of Cleansing Solution Wash legs (shower) with potable water. Treatment of Surrounding Skin Wash with emulsifying ointment, remove loose skin scales atraumatically, pat dry & reapply emulsifying ointment in direction of hair growth. Type of Primary Dressing Aquacel. Type of Secondary Dressing Profore size 1825cms. Method of Securing Dressing to Skin Not applicable. Type of Compression Profore Multilayer Compression. Frequency of Dressing Changes Weekly. Removal of Sutures/Staples/Steristrips Not applicable Patient Education (Briefly outline topics covered) Benefits of Compression, Leg Exercises. Complications of compression. Information Leaflets Given (State Type) Leaflet on Leg Ulcers given. Pain Addressed: State how Refuses to take analgesia despite education. Dr XX & family aware Signature Jane Murphy 135 Suggested further reading: HSE (2009) National best practice and evidence based guidelines for wound management References: 136 1 Collier, M. (2006) Understanding the principles of wound management, Journal of Wound Care, Supp; 15(1): S7-S10 2 Baranoski, S., Ayello, E. (2008) Wound Care essentials: practice principles. Second Edition. Lippincott, Williams and Wilkins, USA 3 European Wound Management Association, (2005), Position Document. Identifying Criteria for Wound Infection. London: MEP Ltd. 4 European Wound Management Association, (2006), Position Document. Management of Wound Infection. London: MEP Ltd. 5 Bryant, A., Nix, D. (2007) Acute & Chronic Wounds, 3rd Eds, Mosby, USA 6 British National Formulary (2008) BNF 2008 Pharmaceutical Press, UK 7 HIQA (2009) National Quality Standards for Residential Care Settings for Older People in Ireland RAP 14: Psychosocial Well-being Definitions: Psychosocial is defined as “of or relating to the interrelation of social factors and individual thought and behaviour.1 Well-being is the state of being comfortable, healthy or happy. Psychosocial Well-being refers to feelings about self and social relationships. RAI Identifiers of Potential Risks: Admission Concerns A65, Communication Impairment C6, D3, D4, Difficulties with eating C7, F22, Modified Diet F5, Difficulties with drinking C8, Thickened Fluids F8, Dehydration F21, Wounds C10, J1, J8, Impaired Mobility C11, H1 Impaired ability for Personal Care C12, C13 Disturbed Sleep Patterns C14, N9 Urinary Incontinence C17, G2 Faecal Incontinence C18, G10, Constipation G11, Stoma G12, G13, Breathing Problems C19, E4, Behaviours that Challenge C20, D16, Pain C22, Emotional state: Anxious, Low Mood, Tearful, Nervous D11, H5, Hemiparesis I2, Cognitive Impairment I2, Amputation I2, Involuntary Movements I2, Altered Body Image I15, Communication, Mood & Behaviour Concerns D23, Breathing & Circulation Concerns E10, Nutrition & Hydration Concerns F24, Continence & Elimination Concerns G16, Mobility & Safety Concerns H10, Personal care, Controlling Body Temperature and Self Image Concerns I16, Skin Condition, Wounds & Pressure ulcer prevention Concerns J8, Sleep, Rest & Spiritual Needs Concerns N18 Palliative Care Concerns O9, End of Life Concerns P12, Unresolved grief, unresolved inter-personal relationships, feelings of loss as identified in “A Key To Me” K1-38, Section L- Events which are likely to impact on psychosocial well-being, Events likely to impact on psychosocial well-being as identified in “My Day, My Way”. Other Risk Factors include: Individual: • Feelings of loss, for example: in lifestyle, place of residence, independence, autonomy/control, disease progression, functional decline • Change in individual’s expectations and daily routines or the affects of moving residence/institutionalisation • Interpersonal relationships e.g. conflict with family, friends or staff, unresolved grief issues, unresolved bereavement, lack of integration in the community prior to entering residential care, lack of family support and a lack of appropriate support in the preparation and transition to long term care • Uncompleted personal affairs- e.g. End of Life planning Environmental: • Lack of privacy and dignity • Unhappy with shared facilities • Unhappy with surroundings • Unhappy with other residents • Unhappy with residential daily routines 137 Co- morbidity risks: • Loss of Independence • Functional decline • Organic disease (e.g. Dementia, Underlying infection, Cancer, Chronic Pain). • Mental health disorders (e.g. delirium, psychosis, depression). • Emotional trauma (e.g. loneliness, boredom). (The above list is not exhaustive.) Further Assessments: Where possible document the resident’s/significant other(s) concerns in each of the assessment areas on the Resident Assessment Instruments (RAIs). Further assessment in specific areas may be required to fully explore the resident’s/significant others concerns. A key worker should be identified i.e., one who has developed a good relationship with the resident. Identify where possible, the origins of the resident’s negative psychosocial well-being. Negative psychosocial well-being may be related to: 1. Psychosocial Causes: Assess and explore all areas that have been identified during RAI assessment as impacting negatively on the resident’s psychosocial well-being e.g. the resident may have several issues of concern identified in the RAIs. These should be collated together to give an overall picture of the resident’s psychosocial well-being. 2. Environmental Causes: Ask the resident what specific environmental issues are impacting on their psychosocial well-being e.g. privacy, dignity, routines and expectations, dining facilities, bathroom facilities, availability of quiet area, social facilities and interaction with residents, staff. For residents who have difficulty with, or are unable to communicate refer to RAP 1: Communication, Vision and Hearing. 3. Physiological causes: Physiological causes that may impact on a resident’s psychosocial well-being may include delirium, malnutrition, pain, infection. If relevant assess: • Mood and Behaviour changes e.g. complete ABC analyses of behaviour. Refer to RAP 2: Mood and Behaviour • Cognitive impairment, dementia and the impact of disease progression on psychosocial well-being e.g. complete M.M.S.E. or Cohen Mansfield Agitation Inventory. Refer to the Doctor for further assessment if required and/or specialist in the area e.g. C.N.S., Psychologist, Psychiatrist as appropriate • Functional decline- Complete a validated functional assessment tool e.g. Barthel score. • Level of depression- Complete a H.A.D.S. (Hospital Anxiety & Depression Scale). • Assess pain status- Complete a validated pain assessment tool e.g. Abbey Pain Scale, numeric pain scale, refer to RAP 16: Pain Assessment and Management • Communication difficulties. Refer to RAP 1: Communication, Vision and Hearing • Nutritional status, refer to RAP 5: Nutritional Status. Assess hydration status, refer to RAP 6: Dehydration and Fluid Maintenance. Assess constipation status, refer to RAP 9: Constipation. (The above lists are not exhaustive.) 138 Referrals Required: Refer to the multidisciplinary team with the resident’s/significant other(s’) consent and as appropriate to the individual’s assessment findings and specific needs: • • • • • • • • • • • • GP/Medical referral for any medical concerns and to aid identification of underlying causes which may be treatable Where there is a social work service available, referral should be prioritised to this service so that appropriate expertise is accessed for psychosocial issues O.T./Physiotherapy referral to record baseline of physical ability/activity level & address an appropriate plan of personalised care/specialised equipment needed Speech & Language assessment to maximise communication abilities, etc. C.N.S. Dementia/Behaviour/Older Persons Care if available Consultant Specialist services as required e.g. neurologist, psychiatry of later life Counselling service Spiritual Advisor Complementary therapy Advocacy services Addiction services Psychology/ Psychiatric services (The above list is not exhaustive) Personalised Care Planning: The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to address the cause or risks of negative psychosocial well-being, where possible. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. Problem/Need Identification: Record the actual or potential psychosocial well-being problem and its associated or related risk factors. For example: ‘Mary displays anger towards her family members related to her recent admission to extended care’. Goal Specification: Record: realistic, specific (to the cause of negative psychosocial well-being), measurable and obtainable MDT goals. For example: ‘To help Mary cope with issues that are triggering her feelings of anger as evidenced by a reduction in angry outbursts directed towards Mary’s family within six weeks’. Specific Interventions: These are the specific steps taken based on expected standards of care in addressing actual or potential psychosocial well-being problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 139 1. Specific MDT interventions: Record • The specific MDT care instructions for addressing any risks /needs /underlying causes associated with the resident’s problem of negative psychosocial well-being. Specific care instructions are aimed at reducing/addressing negative psychosocial well-being feelings where possible, by treating/managing the underlying causes and by promoting positive ways for the resident to regain/restore their usual pattern of psychosocial wellbeing. Specific care instructions will be based on the individual’s assessment findings and interests e.g. ‘Mary would like to attend the Day Care Centre she has always attended. This has been organised for Monday, Wednesday and Friday from 10:00-14:00hrs. Day Care Centre transport is arranged, pick up at 09:30hrs’. • A named key worker(s) should be identified i.e., one who has developed a good relationship with the resident. This key worker should encourage the resident to express their fears/concerns and provide emotional/psychological support and information on positive coping strategies. Positive coping strategies include: giving information/explanation/choice on all aspects of care and encouraging the resident to discuss their feelings/choices and goals in relation to their lifestyle and active participation in care. Encouraging residents to talk about their previous life in the community and their present worries and fears may help some residents in coming to terms with feelings of loss. Offer and access social work services/counselling / advocacy services to empower/enable residents to seek further help in discussing and resolving their feelings if they so wish. In undertaking the above tasks it is important that the key worker is aware of their reporting accountability i.e. to their unit nurse manager and that they are further aware of the designated centre’s policy on confidentiality and on Elder Abuse. It is further essential that key workers are aware of their own limitations and know when they need to refer the resident on for specialist advice. • Record the MDT specific interventions to treat any underlying cause(s) identified e.g. low mood associated with infection / pain. Monitor closely the treatment outcome and its impact on the resident’s psychosocial well-being. Consider each area in the RAIs where the resident has reported a concern in conjunction with the risk factors outlined. An MDT meeting may be required where these services are available to draw up MDT interventions in Care Planning, that are time specific, measurable and that outline areas of specific responsibility, if the resident’s needs are sufficiently complex. • While it is essential that a key worker provides psychosocial support for specific residents, all staff should familiarise themselves with the resident needs including their past and current interests, previous life and present wishes using the information obtained from the resident/significant other in the assessments ‘A Key to Me’ (Resident profile), the resident’s ‘Diary of Important Events’ and ‘My Day, My Way’ document. This will assist staff in better knowing the resident and in providing care to those with negative psychosocial feelings. • Devise an activity schedule or refer the reader to the resident’s ‘Meaningful Activity Care Plan’. This must be based on the resident’s identified meaningful activities. Encourage the resident’s participation on an ongoing daily basis with all staff members. Further encourage participation with planned onsite activities e.g. weekly visit to library (based on the specific interests of the individual). Take account of the resident’s previous lifestyle, their priorities and the issues that matter to them. 140 2. Monitoring and ongoing assessment: Monitor psychosocial well-being, mood and behaviour by assessment of: a. Participation and interest in his/her care. b. Interpersonal relationships e.g. record the frequency/intensity of episodes of angry outburst towards significant other(s). c. Resident’s participation in activities of choice. d. If underlying physiological conditions are impacting on the resident’s psychosocial wellbeing, these need to be monitored and treated where possible e.g. pain. e. Monitor effectiveness of specific interventions recorded and evaluate at weekly intervals unless otherwise indicated e.g. the degree of negative psychosocial wellbeing gets worse rather than improves. f. Report monitoring concerns to appropriate members of the MDT. 3. Communication: • Discuss and agree the resident’s care plan and their wishes in conjunction with the resident where possible and /or their significant other/advocate. Inform them of any proposed change to the plan of personalised care and encourage/enable/empower them to be involved. • Plan regular MDT meetings with the resident’s consent e.g. Doctor, Psychiatrist, Nurse, CNS, O.T., Physiotherapist, Social Worker, Activity team, Dietician, Art Therapist, Music Therapist, Speech and Language Therapist, resident/significant other(s) to discuss monitoring findings and the effectiveness of the Multidisciplinary plan of personalised care. • Communicate the resident’s preferences and wishes with their consent to all those involved in the resident’s direct care. Residents must be referred back to the MD team if there is deterioration in psychosocial wellbeing, despite implementing the MDT plan of agreed care. Ensure staff are informed of any changes in the resident’s care/wishes at the start of each shift. • Ensure any changes are recorded as agreed by the resident to their individualised plan of care and that these are communicated to the appropriate M.D.T members. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and carers: Provide information and education to the resident, significant other(s) and all staff involved in individualised care giving regarding: • Understanding the resident’s identified individual and diverse psychosocial needs. • Empowering and enabling residents by listening to their concerns and offering choices and autonomy in decision making regarding their care. • Ensuring residents are involved in communication and are not isolated. • Understanding the impact of change and its affect on lifestyle and personal routine. • Understanding that the ‘timescales’ of adjustment required for adapting to change is different for each individual resident. 141 Evaluation of care: Evaluate care, based on the goals specified for improving the resident’s psychosocial wellbeing. Psychosocial well-being care plans must be evaluated when the resident’s condition improves or deteriorates and at least three monthly. Evaluate the effectiveness of the care provided by checking if the goals of care are being met e.g. improved mood, resident demonstrates increased interest in Activities of Living / participation in onsite activities, improved social interest in other resident’s, significant other and staff. Encourage self reporting of improved feelings of well-being. Refer to the ‘Protocol of Expected Standards in Care for Psychosocial Wellbeing’ and ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. 142 143 A. Psychosocial Causes 1. Any section of RAIs identified by the resident or significant other(s) as being an issue of concern 2. Past social relationship & lifestyle assessment. Complete ‘A Key to Me’, ‘Diary of Important Events’, ‘My Day, My Way’ & ‘Meaningful activities’. 3. Assess usual behaviour pattern. Ask resident/ significant other- complete ABC Functional Analyses or H.A.D.’s (Hospital Anxiety & Depression Scale) if appropriate. 4. Identify a Key Worker to further explore the areas of concern with the resident B. Physiological Causes 5. Assess physiological conditions which may impact negatively on the resident’s psychosocial wellbeing e.g. delirium, malnutrition, pain, infection which may be treatable once diagnosed 6. Baseline cognitive status, complete M.M.S.E. (Mini Mental Score Examination) within 48 hours of admission. 7. Assess pain status. 8. Complete Functional Assessment e.g. Barthel Score. 9. Complete Nutritional risk assessment M.U.S.T. D. Environmental Causes 10. Ask the resident about what specific environmental issues that are impacting on their psychosocial well-being e.g. issues with regard to privacy/dignity/routines & expectations. Refer to RAP 1 for those with communication problems. (on or within 5 days of admission, if the Residents condition improves or deteriorates and at least 3 monthly Nursing Assessment Identify specific need for individual risk and develop a personalised plan of care with the resident/ significant other. At Risk Reassess when there is a change in the resident’s condition & at least 3 monthly. At No Risk Nursing Diagnosis 1. Empower and enable the resident and/or their significant other/advocate to be involved in all aspects of multi -disciplinary personalised care planning, having first sought the resident’s consent where possible. 2. With the resident’s consent, decide on specific goals of care. 3. Ensure an identified Key Worker is appointed to work with the resident 4. Interact positively with resident to their identified needs. 5. Refer to multi-disciplinary team with the resident’s consent and as appropriate e.g. Social Worker, O.T., Physiotherapist, Psychiatrist / Psychologist. 6. Include M.D.T specifics care instructions 7. Offer resident personal choices in everyday activities. 8. Implement personalised plan & closely monitor. Implement an Enteral Feeding Care plan Document: Nursing Care Goals & Planning 4. Update care plans as appropriate. 3. Liaise with M.D.T. and discuss changes, monitoring findings, improvement or deterioration in psychosocial well-being. 2. Communicate with the resident to assess a verbal improvement in their psychosocial well-being, if possible. 1. Continuous observation is required to assess the resident’s progress/ condition. Refer to the resident’s goals to assess if they are being met. Nursing Evaluation Protocol of Care for Psychosocial Well-being in H.S.E. Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: Psychosocial well-being PROBLEM / NEED IDENTIFICATION Number: Date Signature 11/01/10 Mary displays anger towards her family members related to her recent admission to extended care. C. Byrne GOAL SPECIFICATION To help Mary cope with the issues that are triggering her feelings of anger as evidenced by a reduction in angry outbursts towards Mary’s family within six weeks. SPECIFIC INTERVENTIONS Date Signature 11/01/10 1. Mary particularly likes to talk to Ann (night carer). Ann has been assigned as Mary’s Key worker and will encourage Mary to discuss her feelings/anger towards her family and explore her feelings with her. 2. Establish permission from Mary to discuss Mary’s angry outbursts with her significant other(s) and explore their feelings if appropriate. 3. Provide education/information to both Mary and her family on adjustment to change/loss and on the importance of maintaining Mary’s normal routines and personal choices in all aspects of care and lifestyle 4. Mary wishes to talk to her family about her feelings and would like to talk to an advocate first and for them to be present when she is talking to her family. Advocacy referral sent. Awaiting a date for a meeting. 5. Mary and her family do not want an onward referral to counselling services at present. Monitor situation and approach topic of counselling at a later date if needed. 6. Refer to Mary’s-A Key to Me, Diary of Important Events & My Day, My Way to familiarise with Mary’s interests and previous life 7. Encourage Mary’s participation in her Meaningful Activity Care Plan and to participate in daily organised activities of her choice. 8. Mary likes to sit beside Ann during mealtimes / evenings 9. Mary’s daughter will take her mother out every Saturday afternoon- returning at approx. 20.00 hrs & her friend Peg will visit on Tuesday mornings and accompany her to mass. Mary is happy with this arrangement. 10. Monitor Mary’s angry outburst, mood & behaviour. Record on a mood and behaviour diary. 11. Monitor Mary’s participation and interest in ADL’s and interpersonal relationships. Record a daily narrative note 12. Report monitoring concerns to the MDT as appropriate C. Byrne EVALUATION OF CARE (based on goals specified) Date Signature Discontinued Date: …..... / ……… / 20…… Signature: ………………………………………….. 144 Bibliography: Cantwell, L. (2008) An Exploration of the Psychosocial needs of The Older Person in Extended Care Services Health Information and Quality Authority, (2009), National quality standards for residential care settings for older people in Ireland Corey.G (2005) Theory and Practice of Counselling and Psychotherapy, Brooks/Cole: U. S. A. Perroto, R. & Culkin, J. (1993). Exploring Abnormal Psychology, Harper: New York References: 1 Oxford dictionary 10th edition (edited by Judy Pearsall) 145 RAP 15: Activities In our lives our leisure activities are just as much a part of our identity and quality of life as any other pursuits. Individually planned activities programme not only facilitate the leisure interests and enjoyment of residents, but are also beneficial to their potential physical, emotional, social and psychological outcomes. Through enjoyable, purposeful activities, individual programmes must aim to achieve maximum independence, choice and selfdetermination, while enabling and motivating residents to reach their highest potential. Meaningful activities provide the potential for improved function, mobility, dexterity, pain reduction, diminished helplessness and isolation, release of tension, promotion of self esteem and social interaction. Definitions: • Activity: is the execution of a task or action by an individual. An activity can be anything we do from the moment we get up in the morning, to when we go to bed at night. • Meaningful Activities: The term ‘Meaningful Activities’ is to be understood as any endeavour, including activities of daily living in which a resident participates, where the intention is to enhance the resident’s sense of well-being and to promote or enhance physical, cognitive and emotional health. Meaningful activities also include leisure activities that promote quality of life, self-esteem, pleasure, comfort, education, creativity, success and independence. • Activity therapy: is a holistic person centred practice. It is concerned with the promotion of recreation and leisure opportunities, in addition to functional an psychological wellbeing of people of all ages who experience barriers to participation in the ‘fullness of life’ due to health problems, disability, ageing or frailty. Many staff may think that activities are not a part of their role and consider ‘activities’ as an event such as running a group or organising an outing. However, if we accept that everything a resident does in a day is an ‘activity’ which can be participated in a meaningful way by the resident, then all staff have a part to play in the provision of Meaningful Activities. Helping a person to remain active and socially engaged is the job and responsibility of every member of the team. The types of activities which provide meaning in our lives include all of the following: • 146 Physical Activities – Are activities that can help to improve a person’s mobility, coordination, respiration and circulation. Examples include exercise and movement, ball games, engaging in different household tasks and daily life in their place of residency. • • • • • • Mental Activities – Include activities that stimulate thinking and memory which further encourages and enhances orientation. Examples include reading newspapers or having newspapers read to them, social discussions between staff and residents on current news events, providing opportunities for residents to participate in meaningful mental activities appropriate to their level of cognition, so that residents can achieve a feeling of self worth e.g. ‘the sequences involved in setting the table for meals’, gardening, bingo, quizzes, word games and crafts. Personal Care Activities such as enabling and promoting independence in washing, dressing, brushing one’s teeth or brushing one’s hair, mealtimes, etc Social Activities – encourage communication, interaction and involvement and can enhance self-esteem, reduce boredom and stress and provide fun and relaxation. Examples include; meals and mealtimes, chatting with residents or staff, shopping, card games, participation in on-site and off-site Older Persons groups, sing along, dancing, outings, parties, bingo, story telling and poetry. Creative Activities – can help develop self-expression. Examples include; enabling and promoting choice in daily life such as choice in clothing/jewellery/perfume/ aftershave, Menu planning and developing pictorial menus, enabling residents to personalise their rooms/living area, arts and craft, music, drama. Spiritual Activities enabling residents to carry out their usual pre-admission spiritual routines such as night time prayers or attending religious services, singing hymns participating in or listening to prayer groups Vocational Activities, residents may have a vocational role that they want to continue at some level Activity is essential to human wellbeing and will help maintain a person’s sense of self worth and give purpose and enjoyment to the day. Activities may be structured or unstructured see Appendix 1. RAIs identifiers of Potential Risk that may impact on the resident’s activities include: Mobility Problems C11, H1 Impaired ability for Personal Care C12, C13 Behaviours that Challenge C20, D16 Impaired Communication D3, D4, Impaired Hearing D6, Impaired vision D8, Pain D22, Cognitive & Emotional State D11, D13, D14, Impaired Safety Awareness H4, Resident’s Likes and Dislikes K27-38, ‘My Day, My Way’ Assessment Findings ‘Meaningful Activities’ Assessment findings M1-10. Other Risk Factors include: Other risk factors which may impact on residents’ activities include: 1. Cognitive impairment 2. Sensory impairment 3. Cardiac problems 4. Medications – i.e. Psychotropic drugs, Antidepressants, Cardiac Medications 5. Limitations in functional capabilities 6. Communication difficulties 7. Low Mood 8. Behaviour that challenge 147 Further Assessments: Assess the resident’s overall ability; this assessment must include assessment of their lifestyle and leisure preferences, their needs, strengths, weaknesses, ability to perform a range of tasks and their ability to interact positively with others. The challenges of ageing affect each person in different ways and in varying degrees of intensity. In order to propose suitable activities to older people it is important to be aware of the unique physical and sensory challenges they may have. Learning the specific physical and sensory needs of the resident can help to better determine which activities are most suited for them e.g. the needs of cognitively intact residents will differ from those with cognitive impairment. Similarly immobile, bed bound or chair bound residents will have different activity needs. Residents who have capacity to decide what their level of involvement in the activities programme must have their choices respected. When a person says no to being involved in an activity, we have to think of different ways of engaging their interests. Ask them what activities they enjoy and would like to do with you, rather than trying to decide for them. Allow residents to tell you about activities they enjoy and they will likely suggest ideas that you can do together. Identifying Interests: In finding out how best to assist a person to become involved in recreational and leisure activities, it is important to begin by getting to know the person. This involves spending time with the person and possible with others who know him/her well, in order to learn about the resident’s family, their background, experiences, their cultural and ethnic identifications, cultures, traditions, strengths, likes or dislikes etc. Plan a personalised activity programme with the resident/significant where possible with consideration to the following: 1. Is resident suitably challenged/over stimulated a. Available activities should correspond to resident lifetime values, attitude, expectations and wishes. b. Establish if the resident considers “leisure activities” a waste of time- he/she never learned to play, or to do things just for enjoyment. c. Consider the resident’s wishes and prior activity interests. d. What was the resident’s preadmission routine for activities? e. Consider how activities requiring lower energy levels may be of interest to the resident – i.e. reading a book, talking with families, friends, other residents and staff. f. Does the resident have cognitive/functional deficits that either reduce options or preclude involvement in all/most activities that would otherwise have been of interest to the person? 2. Health Related factors may affect participation in activities. a. Assess if the resident is suffering from an acute health problems. b. Assess if the resident is hindered because of embarrassment / unease due to the presence of health-related equipment e.g. catheter bags, etc. c. Assess if the resident has just recovered from an illness and is well enough to actively participate in any activities. d. Assess if the resident has some degree of disability. 148 3. Recent decline in resident health status – cognition, communication, function, mood or behaviour. a. Staff should be aware of the current health status of the resident. b. Assess the resident retained skills and capacity to learn new skills to ascertain the level of participation. c. Consider life history of the resident (what was the resident like prior to the most recent decline). d. Assess if the resident has the interest to learn new activity. 4. Environmental factors a. Physical space limitation for the activity. b. Residential care setting policy (Safety) 5. Availability of staff and family support Activities for Residents with Cognitive Impairment: The most important thing we have to give people with cognitive impairment is our time and our attention – if we remember this we can then bring activity into all parts of the day. A vital consideration when selecting and presenting activities are ‘knowing the person’ and analyzing the activity. It is vital to ‘match’ the resident’s level of ability and interest with a meaningful activity of the correct degree of challenge; too easy may be boring and too difficult may be frustrating. The Meaning Activities Assessment (based on the Pool Activity level (PAL) instrument), ‘My Day, My Way’ and ‘A Key to Me’ are tools which have been developed for residential care staff to develop a profile of a person’s likes and dislikes. The PAL tool provides a simple checklist that reveals the level of ability of an individual. This information can then be used to plan how to present activities to the person at just the right level. Knowing the person: There are two aspects to this. Firstly gather information about the person’s life (A Key to Me) their background, family and social networks, past interests and hobbies. It is not sufficient to list the persons interests, what was it about the interest that the resident valued? Secondly, it is important to understand how dementia affects the individual’s ability to ‘do’. The PAL checklist is an assessment of the activity level the resident is functioning at. The outcome of the Meaningful Activities Assessment will indicate to staff the ability of a resident with cognitive impairment to engage in different activities. The tool broadly indicates four levels of functioning: Planned, Exploratory, Sensory and Reflex levels. It is not possible to be prescriptive about suitable activities as activity preference is very individual. However, the stages in the PAL can give a good indication of the level of ability of the resident with dementia. It is important that activities are risk assessed and that staff are aware of the risks for each resident. The resident’s activity plan should be reviewed with the resident/significant other at least every 3 months or sooner if necessary. 149 Referrals required: Onward referrals to the multidisciplinary team should be made as appropriate to the resident’s RAIs findings, to ensure each resident can achieve their full potential in all activities. For example: • Physiotherapists are the experts on mobility problems and can advise on activities which maximise functional ability, gait, circulatory and breathing problems. • A speech and language therapist can advise on activities, techniques, assistive technologies and aids to help improve overall communication. • Occupational therapists can provide an assessment of the residents’ ability to carry out activities of living such as eating, drinking, bathing and dressing and will advise on appropriate adaptations and assistive aids to facilitate independence in activities of living. Occupational therapists can also provide advice on leisure activities that will promote physical and mental wellbeing. • Activities co-ordinators can advise on activities appropriate to the residents holistic needs. • Other referrals may include hairdresser, massage therapist, resident’s spiritual advisor, etc. Personalised Care Planning: The aim of the care plan is to develop a single multidisciplinary team (MDT) plan of personalised care that will facilitate the resident to participate in activity or activities that will empower the resident to have a meaningful day. The MDT meeting is an opportunity for all the members of the team to match their assessment information to the interview information and for the team to plan activities which accurately reflect the resident’s needs/interests and current ability to participate. Need/Problem Identification: Care planning for activities should be interest or need led and not necessarily problem based. For example: Following Mrs Smith’s Meaningful Activities Assessment her Activity level Profile is identified at a Planned Activity Level. Goal Specification: Goal: Record desired outcome/s that is specific, measurable, attainable, realistic and time bound. For example: To enable Mrs Smith to take control of the activity being performed and to master the steps involved within 3 months. Specific Interventions: These are the specific steps taken based on expected standards of care in addressing actual or potential needs/problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem/need) 150 1. Specific MDT interventions: This includes MDT and nursing care instructions and interventions to promote participation of the resident in meaningful activity/activities. The following should be recorded in the interventions: • Appropriate activities which are based on the findings of the resident’s comprehensive assessments • The interventions must specify the individual’s interests and needs and these should reflect past and present interests • The interventions should specify meaningful activities that enable the resident to meet their highest level of functioning • Structured and unstructured activity interventions should be recorded For example Mrs Smith is able to plan what to wear and select her own clothes from the wardrobe, encourage her to dress herself, be available to assist if required. 2. Monitoring and ongoing reassessment: Continuous monitoring and assessment of the planned interventions is needed to evaluate the effectiveness of the meaningful activity approach in enhancing the resident’s sense of well being and in promoting or enhancing the resident’s physical, cognitive and emotional health. For example • Observe and document the resident’s participation and response to the activity. • Determine the resident’s perception of the causes of problems which may arise • Monitor participation of unstructured/structured activities where possible in the daily flow sheet or in the narrative notes. 3. Communication Discuss and plan the resident’s meaningful activity care plan in collaboration with the resident and their significant others. Inform or discuss with the members of the MDT the residents personalised meangiful activity care plan. Discuss what activities the resident really enjoyed or engages in and identify if they match the care plan. Meaningful activities must be discussed among the ward/unit team at least daily, it is important that all members of the care team are involved in this process. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers Educate and provide advice to the resident and their significant others regarding the resident’s personalised meaningful activity care plan. Provide written information or a copy of the Meaningful Activities care plan to the resident/significant other if they so wish. Evaluation of Care Meaningful Activity care plans should be evaluated to determine the effectiveness of the MDT interventions. Care plans should be evaluated at least every three months or sooner if there is a change in condition. In evaluating care the ward/unit team members should reflect on the resident’s responses and progress to determine the effectiveness of the interventions in meeting the resident’s goals of care. Refer to the Protocols of Care Flow Chart and Sample Personalised Care Plan in documenting care planning and in providing care. 151 152 2. Develop activity promotion care plan incorporating the following: a) Identify problem/need b) Goal specification (SMART) c) Specific intervention • Specific MDT interventions • Monitoring and ongoing assessment. • Communication • Information/education/health promotion for resident, significant other and carers. 3. A Key to Me 5. Identify the resident’s holistic needs 4. My Day, My Way 3. Evaluation of care 1. Nursing goals focus is to reduce the effect of inactivity, promote optimal physical activity, and assist the person to maintain a satisfactory life style. 1. Personal likes and dislikes 2. PAL Establish resident goals and devise care plan Document: Nursing Care Goals & Planning (Goals of care are based on the resident’s goals and wishes) Nursing Assessment (Within one week of admission, if the resident’s condition improves or deteriorates & at least 3 monthly) 2. Unmet Goals Reassess and review nursing care plan. Consider are the activities being offered suitable? What would the resident like to do? Reassess Establish effectiveness of nursing and MDT interventions 1. Goals met Evaluate the need for progression in the activity to maintain or progress gained physical and psychological conditioning. Establish effectiveness of nursing and MDT interventions Nursing Evaluation Protocol of Care for Meaningful Activities in DML, HSE Older Persons Designated Centres Addressograph Label or complete the following Name: ...............................….....................… D.O.B .…..............................……………….… MRN: ……........................………..…………… Ward/Unit: …........................……..................… Nurse’s Signature: … ........................................ Date: .................................. Page no: .............. Meaningful Activities Programme Residents Activity Level Profile Pool Activity Level (PAL) Profile© Sample Personalised Care Plan for: Planned Activity Level Likely Abilities Can explore different ways of carrying out an activity. Can work towards completing a task with a tangible result. Can look in obvious places for any equipment. Likely Limitations May not be able to solve problems that arise. May not be able to understand complex sentences. May not search beyond the usual places for equipment. Method of engagement Activity objectives To enable…Mary… to take control of the activity and to master the steps involved. Position of tools Ensure that equipment and materials are in their usual, familiar places. Verbal directions Explain task using short sentences by avoiding using connecting phrases such as “and”, “but”, “therefore”, or “if”. Demonstrated directions Show …Mary… how to avoid possible errors. Working with others ..Mary.. is able to make the first contact & should be encouraged to initiate social contact. Activity characteristics There is a goal or end product, with a set process, or “recipe”, to achieve it. An element of competition with others is motivating. For dressing, bathing and dining please refer to the plan of care on the next page, please record and reassess Mary’s activity level of function on a daily basis while assisting her with these meaningful activities of daily living. Suitable Activities (based on knowledge of the person’s life history ‘A Key To Me’&‘My Day, My Way’) • Mary really enjoys baking. Organise with the OT for Mary to attend the weekly baking group on Wednesdays. Referral to OT sent on xx/xx/2010. • Mary enjoys reading the daily newspaper preferably the Irish Independent with her morning tea, ensure that Mary receives the paper each morning and chat with her throughout the day on what is currently in the news. • Mary enjoys watching old movies, her favourite actors are Humphrey Bogart and Cary Grant; her favourite movies of all time are Casablanca, Key Largo and To Catch a Thief. • Mary likes to wear some make up every day and hates going out without at least her lipstick on. • She was very active in her local church and sang in the choir, and wishes to be included in all Church of Ireland activities, her spiritual representative is Rev Malone contact no. 01 xx………… • Mary’s family are very involved in her care and enjoy bringing their Mum out regularly, ensure that they are involved in all activity planning. 153 Addressograph Label or complete the following Ward/Unit: …........................……..................… Name: ...............................….....................… D.O.B .…..............................……………….… MRN: ……........................………..…………… Nurse’s Signature: … ........................................ Date: .................................. Page no: .............. Planned Activity Level Activity: DRESSING • • • • Encourage Mary to plan what to wear and to select own clothes from the wardrobe Encourage Mary to put on her own clothes, be available to assist if required Point out labels on clothing to help orientate the back from the front Encourage Mary to attend to grooming such as brushing hair, putting on make-up, cleaning shoes Activity: BATHING • • • Encourage Mary to plan when she will have the bath, to draw the water and select toiletries from the usual cupboard or shelf. Ensure a slip resistant bath mat is in the bath and on the floor Encourage Mary to wash her own body, be available to assist if required Encourage Mary to release the water afterwards, and to wipe the bath Activity: DINING • • • Encourage Mary to select when and what she wishes to eat Encourage Mary to prepare the dining table and to select the cutlery, crockery and condiments from the usual cupboards or drawers Encourage Mary to clear away afterwards Note: Consideration of National Infection Control Guidelines and HSE Health & Safety Guidelines is required in undertaking the above. 154 Addressograph Label or complete the following Name: ...............................….....................… D.O.B .…..............................……………….… MRN: ……........................………..…………… Ward/Unit: …........................……..................… Nurse’s Signature: … ........................................ Date: .................................. Page no: .............. Meaningful Activities Programme Residents Activity Level Profile Pool Activity Level (PAL) Profile© Sample Personalised for: Exploratory Activity Level Likely Abilities Can carry out very familiar tasks in familiar surroundings. Enjoys the experience of doing a task more than the end result. Can carry out more complex tasks if they are broken down into 2-3 step stages. Likely Limitations May not have an end result in mind when starts a task. May not recognise when the task is completed. Relies on cues such as diaries, newspapers, lists and labels. Method of engagement Activity objectives To enable…Peter…to experience the sensation of doing the activity rather than focusing on the end result. Position of tools Ensure that equipment and materials are in the line of vision. Verbal directions Explain task using short simple sentences. Avoid using connecting phrases such as “and”, “but”, or “therefore”. Demonstrated directions Break the activity into 2-3 steps at a time. Working with others Others must approach…Peter and make the first contact. Activity characteristics There is no pressure to perform to a set of rules, or to achieve an end result. There is an element of creativity and spontaneity. For dressing, bathing and dining please refer to the plan of care on the next page, please record and reassess Peter’s activity level of function on a daily basis while assisting him with these meaningful activities of daily living Suitable Activities (based on knowledge of the person’s life history ‘A Key To Me’&‘My Day, My Way’) • Peter loves talking about his family, occasionally he forgets some of their names and this upsets him, encourage him to talk about his family using his photo album which has his family’s names under each picture and where it was taken, encourage his family to continue to build this photo album. • Peter enjoys exercise refer to the physiotherapist for inclusion in the exercise class referral sent xx/xx/2010, he also enjoys Tai Chi on Wednesdays • His favourite type of movies are westerns and he enjoys listening to country and western music particularly Johnny Cash and Hank Williams 155 Addressograph Label or complete the following Name: ...............................….....................… D.O.B .…..............................……………….… MRN: ……........................………..…………… Ward/Unit: …........................……..................… Nurse’s Signature: … ........................................ Date: .................................. Page no: .............. Exploratory Activity Level Activity: DRESSING • • • • Encourage discussion about the clothing to be worn for the day: is it suitable for the weather or the occasion, is it a favourite item Spend time colour matching items of clothing and select accessories Break down the task into manageable chunks: help lay the clothes out in order so that underclothing is at the top of the pile. If Peter wishes to be helped, talk Peter through the task: “put on your underclothes” “now put on your shirt and cardigan” Encourage Peter to check his appearance in the mirror Activity: BATHING • • • • • Ensure a slip resistant bath mat is in the bath and on the floor Break down the task into manageable chunks: suggest that Peter fills the bath, then when that is accomplished suggest that he gathers together items such as soap substitute (e.g. Silcock base®), shampoo, flannel, and towels When Peter is in the bath, suggest that he washes and rinses his upper body, and when that is accomplished, then suggest that he washes and rinses his lower body Ensure that bathing items are on view and that containers are clearly labelled Have attractive objects around the bath such as unusual bath oil bottles or shells and encourage discussion and exploration of them. Activity: DINING • • • Store cutlery and crockery in view and encourage Peter to select own tools for dining Offer food using simple choices Create a social atmosphere using table decorations, music, and promote conversation Note: Consideration of National Infection Control Guidelines and HSE Health & Safety Guidelines is required in undertaking the above. 156 Addressograph Label or complete the following Name: ...............................….....................… D.O.B .…..............................……………….… MRN: ……........................………..…………… Ward/Unit: …........................……..................… Nurse’s Signature: … ........................................ Date: .................................. Page no: .............. Meaningful Activities Programme Residents Activity Level Profile Pool Activity Level (PAL) Profile© Sample Personalised Care Plan for: Sensory Activity Level Likely Abilities Is likely to be responding to bodily sensations. Can be guided to carry out single step tasks. Can carry out more complex tasks if they are broken down into one step at a time. Likely Limitations May not have any conscious plan to carry out a movement achieve a particular end result. May be relying on others to make social contact. Relies on cues such as diaries, newspapers, lists and labels. Method of engagement Activity objectives To enable Ann to experience the effect of the activity on the senses. Position of tools Ensure that Ann becomes aware of equipment and materials by making bodily contact. Verbal directions Limit requests to carry out actions to the naming of actions and objects e.g. “lift your arm”, “hold the brush”. Demonstrated directions Show Ann the action on the object. Break the activity down into 1 step at a time. Working with others Others must approach Ann and make the first contact. Use touch and Ann’s name to sustain social contact. Activity characteristics The activity is used as an opportunity for a sensory experience. This may be multi-sensory and repetitive. For dressing, bathing and dining please refer to the plan of care on the next page, please record and reassess Ann’s activity level of function on a daily basis while assisting her with these meaningful activities of daily living. Suitable Activities (based on knowledge of the person’s life history ‘A Key To Me’&‘My Day, My Way’) • Ann enjoyed music and dancing throughout her life; she won a prize for waltzing and jiving in her younger years, encourage her to take an active part in the weekly dance class. Her favourite music for dancing to is jive music from the 1960’s. She enjoys singing and will actively take part in sing –a-longs. • Ann worked as a dressmaker and has lots of fabrics, lace and buttons in her rummage box, she is a very sensory person and also enjoys the feel of soft toys • Ann responds well to therapeutic massage and has a weekly massage session on Tuesdays. However, she enjoys a hand massage other days using scented hand creams. 157 Addressograph Label or complete the following Ward/Unit: …........................……..................… Name: ...............................….....................… D.O.B .…..............................……………….… MRN: ……........................………..…………… Nurse’s Signature: … ........................................ Date: .................................. Page no: .............. Sensory Activity Level Activity: DRESSING • • • • • • Offer a simple choice of clothing to be worn Spend a few moments enjoying the sensations of the clothing: feeling the fabric, rubbing the Ann’s finger up and down a zip fastener, or smelling the clean laundry Break down the task into one step at a time: “put on your vest” “now put on your pants” “now put on your stockings” “now put on your dress” Activity: BATHING Prepare the bathroom and run the bath water for Ann Make the bathroom warm and inviting - play music, use scented oils, have candles lit on a safely out of reach shelf. Ensure a slip resistant bath mat is in the bath and on the floor Break down the task into one step at a time and give Ann simple directions: “rub the soap (e.g. Silcocks Base®) on the cloth, rub your arm, rinse your arm, rub your chest, rinse your chest......” Activity: DINING • • • Serve food so that it presents a variety of colours, tastes and textures Offer Ann finger foods, encourage her to feel the food Offer Ann a spoon, place it in her hand and direct her to “scoop the potato” “lift your arm” open your mouth” Note: Consideration of National Infection Control Guidelines and HSE Health & Safety Guidelines is required in undertaking the above. 158 Addressograph Label or complete the following Name: ...............................….....................… D.O.B .…..............................……………….… MRN: ……........................………..…………… Ward/Unit: …........................……..................… Nurse’s Signature: … ........................................ Date: .................................. Page no: .............. Meaningful Activities Programme Residents Activity Level Profile Pool Activity Level (PAL) Profile© Sample Care Plan for: Reflex Activity Level Likely Abilities Can make reflex responses to direct sensory stimulation. Can increase awareness of self, and others, by engagement of senses. May respond to social engagement through the use of body language. Likely Limitations May be in a subliminal or subconscious state. May have difficulty organising the multiple sensations that are being experienced. May become agitated in an environment that is over stimulating. Method of engagement Activity objectives To arouse……Michael…… to a conscious awareness of self. Position of tools Stimulate area of the body being targeted e.g. stroke ……Michael’s arm before placing it in a sleeve. Verbal directions Limit spoken directions to movement directions i.e. “Lift”, “Hold”, “Open”. Demonstrated directions Guide movements by touching the relevant body part. Working with others Maintain eye contact, make maximum use of facial expressions, gestures and body posture for non-verbal conversation. Use social actions which can be imitated e.g. smiling, waving, shaking hands. Activity characteristics The activity is in response to direct selective sensory stimulation. For dressing, bathing and dining please refer to the plan of care on the next page, please record and reassess Michael’s activity level of function on a daily basis while assisting her with these meaningful activities of daily living. Suitable Activities (based on knowledge of the person’s life history ‘A Key To Me’ & ‘My Day, My Way’) • Michael always had a dog and he still responds well to animals, ensure that the visitor from PEATA spends extra time with Michael on the visits on Monday and Thursday. • Make sure Michael can always see your face when you are speaking to him, he responds well to smiles. • Involve Michaels family in his care and ensure they are aware of his level of activity • Michael enjoys the snoozelum room when he becomes agitated, with just the soft music playing. • Ensure that he is not in an environment which may over stimulate him and cause agitation. 159 Addressograph Label or complete the following Ward/Unit: …........................……..................… Name: ...............................….....................… D.O.B .…..............................……………….… MRN: ……........................………..…………… Nurse’s Signature: … ........................................ Date: .................................. Page no: .............. Reflex Activity Level Activity: DRESSING • • • • • • • Prepare the clothing for Michael, ensure the dressing area is private and that a chair or bed at the right height is available for sitting Talk through each stage of the activity as you put the clothing onto Michael. Use a calm tone, speak slowly and smile to indicate that you are non threatening Stimulate a response in the limb being dressed by using firm but gentle stroking. Ask Michael to assist you when necessary by using one word requests: “lift” “stand” “sit” At the end of dressing, spend some time brushing Michael’s hair using firm massaging brush strokes Activity: BATHING Prepare the bathroom and run the bath water for Michael, put in scented bath products (lavender will aid relaxation) Ensure that the bathroom is warm and inviting, and feels secure by closing the door and curtains. Provide a slip resistant bath mat in the bath and on the floor. Clear away any unnecessary items which may be confusing Use firm, massaging movements when washing and rinsing Michael. Wrap him securely in a towel when he is out of the bath Activity: DINING • • • Use touch on Michael’s forearm to make contact, maintain eye contact, and smile to indicate the pleasure of the activity Place a spoon in Michael’s hand. Close your hand over Michael’s and raise the spoon with food on it to his mouth As the food reaches Michael’s mouth say “open” and open your own mouth to demonstrate. Touch Michael’s lips gently with the spoon Note: Consideration of National Infection Control Guidelines and HSE Health & Safety Guidelines is required in undertaking the above. 160 References: Gulanick M. & Myers J. (2007) Nursing Care Plans: Nursing Diagnosis and Intervention (6th ed). Mosby Elsevier, United States of America. Kenny J., O’Donnell M., Greehan N. & McDermott-Scales L. (2009) Guidelines on the Provision of Activities for Older People in Residential Care. Health Executive Service, Dublin, Ireland Linton A.D. & Lach H.W. (2007) Matteson & McConnell’s Gerontological Nursing, Concepts and Practice (3rd ed). W.B. Saunders Company, St. Louis Missouri. United States of America. Pool J. (2008) The Pool Activity Level (PAL) Instrument for Occupational Profiling: A Practical Resource for Carers of People with Cognitive Impairment (3rd ed). Jessica Kingsley Publishers, United Kingdom. Redfern S. & Ross F.M. (2006) Nursing Older Person (4th ed). Elsevier Church Hill Livingstone, United Kingdom. Ulrich S.P. & Canale S. W. (2005) Nursing Care Planning Guides for Adults in Acute, Extended, and Home Care Settings (6th ed). Elsevier Saunders, United States of America. Cohen-Mansfield J, Werner P. Environmental influences on agitation: An integrated summary of an observational study. American Journal of Alzheimer’s Disease. 1995;10(1),32-39. 161 162 Large Group 8 + People Small Group 2 – 8 People Individual 1:1 Type of Activity Music groups Concerts in community Group quizzes Bingo Bus trips ‘Parachute’ activity Exercise group Bean bag games/skittles Mass/Church services Balloon/Ball/Throwing games Requires staff planning and leading. Residents need to be able to follow social rules like the ability to remain seated and have a degree of concentration. Examples: Card playing/games Oratory/Rosary/Adoration English Literature Laundry sorting Reminiscence Watching a film/DVD. Visiting musicians/entertainers. Watching RTE/T.V. Set up a larger space for participation by those who are already there and those who may wander in. Examples: Laundry sorting by basket Place 2 or 3 chairs around a fire. Place chairs looking out onto the garden. Rosary or Reminiscence DVD’s. Relaxation or soft music CD. Sports programmes/matches on T.V. Busy tablecloth Workshop boards Prayer books Sorting laundry. Newspapers/Books Baking group Art/Craft Group Gardening Afternoon tea Sonas Enhanced Dining Busy aprons/overlays Informal chats; staff/volunteers Rosary beads Lacing cards Place chairs facing a fire Set up the environment so that two or more people can join. Examples: Hairdressing Spirituality/Oratory Looking at Life Bright Light SIMS (Individual Sonas) Requires the environment to be ‘set up’ to encourage unprompted participation. Leave ‘half done’ activities within reach, or ‘position’ seating. Examples: Unstructured Usually a prepared group, led by a staff member. These groups have a set ‘goal’. Examples: Dressing Showering Hand Massage Relaxation Aromatherapy These are what we usually call “one to one” They are directed and monitored by the staff. Examples: Structured Appendix 1: Meaningful Activities of Daily Living; for Residents with Cognitive Impairment in HSE, DML Older Persons Designated Centres Activities can be structured or unstructured, and can be carried out with individuals, small groups or large groups. Setting-up the environment creatively will maximise the residents’ abilities to participate in activities (Meredith Gresham OT Australia) RAP 16: Pain Assessment and Management Definitions: Pain is a subjective, personal experience only known to the person who suffers. The experience of pain is multidimensional and may be described at several levels, sensory dimension, affective dimension and impact.1 Chronic pain: is defined as ‘pain without apparent biological value that has persisted beyond normal healing time,’ usually taken to be 3 months.2 Acute pain: pain of recent onset and probable limited duration, usually having an identified temporal and causal relationship to injury or disease. RAI Identifiers of Potential Risks Pain Present C21, D22 Communication Impairment D3, D4, Emotional State: Tearful, Low Mood D11, Behaviours that Challenge (? unmet pain need) D16, Restlessness/Agitation D13, D14, Difficulty with breathing E4, Wound Present J1, J7, J6, Disturbed Sleep Pattern N9, Palliative Care pain symptoms O6, End of Life pain symptoms P5. Other Risk Factors include: Cognitive impairment, Presence of chronic disease associated with pain e.g. arthritis, post stroke pain, peripheral vascular disease, diabetic neuropathy, Social diversity (e.g. educational levels, cultural, ethnic and linguistic differences), Being over 65 and resident attitudes (e.g. pain is sometimes incorrectly considered as an expected part of ageing) Staff practices (inconsistent and inadequate pain identification, assessment and treatment). Further Assessments: Document the following assessments on admission, when the resident’s condition improves or deteriorates, any time pain is suspected, if the resident displays any of the signs or symptoms of pain and at least three monthly. Pain has been referred to as the Fifth Vital Sign™3, this emphasises the importance of considering, measuring and monitoring the presence of pain systematically.3 Self reporting of pain is the gold standard method for identifying pain.4 1. Assess the resident’s overall risk context: bio/psycho/social risks e.g. comorbidities, medications, limitations in functional activities, psychosocial issues. 2. Assess for signs and symptoms associated with pain. Signs and Symptoms: Observational assessment is essential for assessing the signs and symptoms of pain in older people with cognitive impairment or for those with impaired communication. Observe for: • Autonomic changes; pallor sweating, tachyponea, altered breathing patterns, tachycardia, hypertension 163 • Facial expression; grimacing, frowning, rapid blinking, brow raising or lowering, cheek raising, eyelid tightening, nose wrinkling, lip corner pulling, chin raising, lip puckering. Body movements; altered gait, pacing, rocking, hand wringing, repetitive movements, increased tone, guarding (an abnormal stiff rigid or interrupted movement while changing position), bracing • Verbalisation/vocalisation; sighing, grunting, groaning, moaning, screaming, calling out, aggressive/offensive speech • Interpersonal interaction; aggressive, withdrawn, resisting • Changes in activity pattern; wandering, altered sleep, altered rest patterns • Mental status changes; confusion, crying, distress, irritability • Self reporting Note: In some neurological conditions, facial expressions are absent e.g. Parkinson’s and end stage Alzheimer’s, residents who have a neurological impairment may not demonstrate the signs and symptoms of pain. If pain is suspected it should be treated. When it has been established that there is pain present5 3. Assess the multidimensional aspects of pain including; • A sensory dimension which describes the intensity and nature of pain. The resident should be asked about pain in a broad and open ended way using at least two questions phrased in different ways, such as: ■ Does it hurt anywhere? ■ Do you have any aching or soreness? ■ Do you have any ache, pain or discomfort? ■ Is your pain a big problem, a medium sized problem or a small problem? ■ Describe the pain; is it crushing, throbbing, sharp, burning, etc? • An affective/evaluation dimension which describes the emotional component of pain and how pain it is perceived e.g. dangerous, exhausting, frustrating, frightening. • Impact on life including physical, functional and psychosocial effects. Impact of pain on the activities of daily living, spontaneous movement, evidence of activity, avoidance of activity, comfort on movement, functional assessment, the resident’s coping resources, their belief about the cause of pain, the resident’s cognitive state, their family’s belief and expectations about pain and stress/distress, presence of anxiety and/or depression, effect on sleep, suicidal thoughts; impact on relationships, impact on social activities. 4. Factors relevant to a pain assessment include: Pain history When pain began Site Severity Quality Aggravating and relieving factors Radiation General Medical History Relevant diseases (e.g. dementia, arthritis, vascular, neurological, gastrointestinal, renal) Associated symptoms (e.g. nausea). Allergies Physical examination Comprehensive examination covering and including: Sites of reported pain and referred pain The musculoskeletal and neurological systems Signs of arthritis Sensory changes 164 Physical impact of pain Impact of pain on activities of daily living Spontaneous movement Evidence of activity Comfort on movement Functional assessment Psychosocial situation Resident’s coping resources Resident’s belief about the cause(s) of pain Resident’s cognitive state Family expectations and beliefs about pain and stress Presence of anxiety and/or depression Effect on sleep Suicidal thoughts Social impact of pain Impact on relationships Impact on social activities Review of medications and other treatments Treatments that have been tried (list dates and reasons for discontinuation if known) Effectiveness of current treatments 5. Baseline assessment for residents able to self report A multi dimensional pain assessment instrument is the best choice for the initial assessment of communicative people and subsequent formal reviews at weekly or longer as appropriate intervals e.g. the “Resident’s Verbal Brief Pain Inventory” (RVBPI). Ongoing assessment Uni-dimensional assessments can be performed daily, or more frequently if the information gained will help to guide treatment. This can be done using either a numeric rating scale (NRS) or a verbal descriptor scale (VDS). One or the other may be chosen on the basis of resident preference and understanding. It has been suggested that the vertical form of the NRS may be preferable and more easily understood by older people with impaired abstract reasoning skills. 6. Baseline assessment for residents unable to report pain The two structured procedures to assess pain in residents who are unable to report pain, mostly due to dementia, dysphasia or delirium are staff observation and informant report. With both procedures it is important to record, if the identified pain occurs at rest (and over what time) or only in relation to a certain activity (e.g. being turned) or in conjunction with another activity (moving a certain part during dressing or bathing). Staff observation Staff should formally observe and document both the known kinds of pain related behaviours seen in people who are not cognitively impaired, as well as other behavioural and clinical changes that could indicate pain in people suffering from dementia. These are outlined in the signs and symptoms. 165 Informant report This involves obtaining and documenting a report from people familiar with the resident including family members, carers and others who know the resident well. Once pain has been identified as a significant issue the use of an observational instrument such as the Abbey pain scale and the PAINAD, will help indicate the presence and intensity of pain in these residents. Referrals Required: Refer to the multi disciplinary team as appropriate to the assessment findings e.g. The doctor should be informed and a full examination carried out, a comprehensive examination covering and including; the site of the reported pain, the musculoskeletal and neurological systems, signs of arthritis, sensory changes. A referral should be made to the physiotherapist if the pain is musculoskeletal in nature, to the dietician and tissue viability nurse for wounds, to the pharmacist for review of medications and other treatments; assess what has been tried and how did it work. Consider music therapy, occupational therapy, diversional therapy, social worker, counselling services or pastoral care team for residents with psychosocial issues which may be aggravating pain. Psychotherapy may be beneficial based on the premise that pain is a sensory and emotional experience with psychological factors contributing to the pain. It may be necessary to refer outside to a specialist pain clinic. Record all referrals made on the MDT referral record and document the reason/outcome in the narrative notes, remember to update care plans accordingly. Personalised Care Planning: The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care. The MDT includes the resident/significant other (if appropriate), carers, nurses, doctors and allied health professionals. The primary aim is to treat the pain where possible, however, it is also very important to reduce the risks of exacerbating pain during delivery of care e.g. manual handling may exacerbate pain by stimulation of tissue which has an increased sensitivity to pain and movement that exceeds the impaired range of joints and muscles. Problem/Need Identification: Record the actual or potential pain problem and its associated or related risk factors. For example; Mary has pain associated with a pressure ulcer on her sacral area, or Mary is at high risk of pain associated with the pressure ulcers on her sacrum. Goal Specification: Record: realistic, measurable and obtainable MDT goals. For example, ‘Mary reports pain severity less than when previously assessed. Mary’s pain will be assessed at each interaction with Mary’. Or, ‘Mary’s level of pain will be at an acceptable level as defined by Mary herself following the planned interventions. Mary reports a level of pain that allows her to participate in activities. Pain will be assessed at each interaction with Mary’ (The score can be measured using a pain scale e.g. NRS or VDS). 166 Specific Interventions: These are the specific steps taken based on expected standards of care in addressing actual or potential problems/needs. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: Record a) Specific interventions to address resident/significant others concerns, preference and care choices e.g. educate the resident/significant others that pain is not a normal process of ageing and that pain is a common and treatable condition. Encourage the resident to talk about their fears. Often residents are afraid to tell anybody about their pain as they think it may be a symptom of something more sinister or they fear developing an addiction to medication. b) MDT specific care instructions This includes the nursing care instructions /programmes for assessing, reducing and managing pain and other MDT specific care instructions. Establish a plan for management in collaboration with the multidisciplinary team that is consistent with the resident’s and family/significant other’s goals for pain relief, taking into consideration the following factors; assessment findings baseline characteristics of pain physical, psychological and socio-cultural factors shaping the experience of pain aetiology most effective pharmacological and non-pharmacological strategies Pharmacological approach advocate for use of the simplest analgesic dosage schedules and least invasive pain management plans. Non pharmacological approach For residents with significant cognitive impairment superficial heat (mild) superficial cold (mild) vibration (mild) Complementary and alternative medicine therapies (CAM) mobilising exercise passive relaxation For residents with no significant cognitive impairment, all treatments listed above plus educational approaches biofeedback/relaxation guided imagery coping skills problem solving behaviour reactivation transcutaneous electrical nerve stimulation (TENS) mind body CAM strengthening exercise aerobic exercise 2. Monitoring and ongoing reassessments Pain is reassessed on a regular basis according to the type and intensity of pain and the treatment plan. • Pain is reassessed: at each new report of pain; new procedure; when the intensity increases; when pain is not relieved by previously effective strategies and when a resident complains or shows any indicators of pain. • Pain is reassessed after the intervention has reached its peak effect (15-30 minutes after parenteral drug therapy, 1 hour after immediate release analgesic, and 4 hours after sustained release analgesic or transdermal patch, 30 minutes after non-pharmacological intervention). • Monitor for medication side effects e.g. constipation if using opoid analgesics. 167 3. Communication • Communicate the resident’s pain assessment findings to MDT members, by describing the parameters of pain based on the tool used, the relief or lack of relief obtained from treatment methods, the person’s goals for pain treatment and the effects of pain on the person. Update care plans accordingly. • Communicate the resident’s personalised care plan to all those involved in the resident’s direct care. • Ensure the resident/significant other is kept up date. 4. Information/Education/ health promotion for resident significant other(s) and carers • Educate the resident/significant other(s) on how best to manage pain and what the personalised plan of care involves. Provide information on what they can do to assist in the pain management plan. • Provide written information where possible and/or provide information in a format that suits the resident’s communication requirements. Refer to RAP 1: Communication, Vision and Hearing. Evaluation of care: Care plans must be evaluated every time the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking to see if the goals are being met. 168 169 Reluctant to complain of pain • • • • • Take a detailed pain history Examine the resident Treat cause Treat symptoms if cause is not identifiable Consider referral Yes • Assess pain intensity using a simple scale such as a verbal rating scale (VRS) or numeric rating scale (NRS). • Ask the person to show you where their pain is (pointing to the area) Is pain present? Yes • Ask whether the person has pain at rest or on movement. Use alternative descriptors such as sore, hurting or aching. • Observe for potential indicators of pain. • Is pain reported/apparent? Yes Can the person communicate successfully? No No No No immediate action needed. Continue to monitor. • No immediate action needed. • Continue to monitor and treat as required. Yes Treat morbidity Do potential pain indicators persist? Yes Is there evidence of morbidity that may be causing pain? Yes Observe for potential indicators of pain: • Facial expression. • Verbalisation/vocalisation. • Body movements. • Altered interpersonal interactions. • Changes in activity patterns or routines. • Mental status changes. • Physiological changes. Yes • Consider empirical analgesic trial or other pain-relieving intervention. • Monitor response carefully. Yes No • No immediate action needed. • Continue to monitor. Yes • Attempt to interpret meaning of behaviour with help of caregivers familiar with the person. Provide individualised care. • Ensure basic comfort needs are met. • Provide reassurance if behaviour suggests fear. • Consider providing analgesics prior to movement. • No immediate treatment needed • Continue to monitor Protocol for Care for the Assessment and Management of Pain in HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: Pain PROBLEM / NEED IDENTIFICATION Number: Page 1 Date Signature 11/01/10 Mary has pain on movement associated with her osteoarthritis GOAL SPECIFICATION Mary will be pain free or that pain will be at an acceptable level so that Mary can keep her independence as much as possible as evidenced by self report and by Mary maintaining her personal care with minimal assistance and attending her favourite recreational activities. SPECIFIC INTERVENTIONS Date Signature 11/01/10 • • • • • • • • Record Mary’s initial comprehensive assessment using the RVBPI and the NRS in order to establish a baseline characteristic of the pain. Record the intensity of Mary’s pain using the NRS before and after every intervention in order to build up an accurate pain history. Mary reports her pain to be worse in the mornings with her knees experiencing the highest level of pain – she enjoys a bath and finds that this loosens up her joints and thus decreases the pain- Offer Mary a bath every morning. Administer analgesia as prescribed approx 30 minutes before Mary’s favourite activities start to allow it time to take effect. Mary finds that some cream rubbed into her skin in the evenings helps the pain to settle enough so she can have a good nights rest – use gentle touch when carrying out this procedure, Mary’s daughters also like to do this for her, encourage and facilitate this. Monitor and assess Mary at each contact throughout the day and offer analgesia as prescribed – record the intensity of the pain using the NRS before and approx 30 minutes after drug administration to monitor the effectiveness. Reassess pain at each new report of pain. Provide information sessions to Mary and her family on the importance of reporting and monitoring pain, so that effective pain management can be achieved. Allow them the time and the opportunity to discuss her diagnosis and management options. Educate them further on the other non- pharmacological strategies used to manage pain such as relaxation, diversional therapy. EVALUATION OF CARE (based on goals specified) Date Signature 11/01/10 Outcomes were partially met; Mary is now enjoying her activities but feels her pain is now waking her during the night. For referral to the MDT to review her care plan. Discontinued Date: …..... / ……… / 20…… Signature: ………………………………………….. 170 Suggested further reading: Weiner, et al (1999) Pain in nursing home residents; an exploration of prevalence, staff perspectives and practical aspects of measurement, Clinical Journal of Pain: 15(2): 92-101. Kane, et al (2004) Pain management in older adults in care, Nursing and Residential Care, 6(5): 226-231. WHO analgesic step pain management ladder. References: 1 The British Pain Society, The assessment of pain in older people. National Guidelines http://www.bgs.org.uk/Publications/Clinical%20Guidelines/pain%20concise%20gui delines%20WEB.pdf 2 International Association for the Study of Pain (1986) 3 Pain the Fifth Vital Sign ™ http://www.ampainsoc.org/advocacy/fifth.htm 4 The Australian Pain Society (2005) Pain in Residential Aged Care Facilities; Management Strategy 5 The American Geriatrics Society (AGS) panel guidelines on persistent pain in older persons, Clinical practice Guidelines P211, Table 3. 171 RAP 17: Disturbed Sleep and Rest Definitions: Sleep – a condition of body and mind such as that which typically recurs for several hours every night, in which the nervous system is relatively inactive, the eyes closed, the postural muscles relaxed, and consciousness practically suspended Disturbed Sleep – sleep that is interrupted. Rest – the repose of sleep that is refreshing to body and mind and is marked by a reduction in metabolic activity. – a state or period of refreshing freedom from exertion RAI Identifiers of Potential Risks: ■ Disturbed Sleep Pattern C14, N9, ■ Individual Reported Symptoms N8, ■ Difficulties with Urinary Management C17, ■ Difficulties with Bowel Management C18, ■ Breathing Difficulties C19, E4, ■ Behaviours that Challenge C20, D16 ■ Pain C21, D22, ■ Cognitive & Emotional State D13, D14 ■ Wound C10, J1, J7, J6 Other Risk Factors include: • • • • • • • • • Pain/Discomfort/Impaired skin integrity e.g. sunburn, pruritus, arthritis, etc. Environmental changes/stimuli (too noisy, too bright, etc) Anxiety/Fear Depression Medications Caffeine Excessive or inadequate stimulation Abnormal physiological status or symptoms (e.g. urinary frequency, dyspnoea, hypoxia, or neurological dysfunction) Normal changes associated with aging Further Assessments: Document the following assessments on admission, if the resident’s condition improves or deteriorates and at least three monthly: 1. Assess past patterns of sleep in normal environment: amount, bedtime rituals, depth, length, positions, aids, and interfering agents. 2. Assess the resident’s perception of cause of sleep difficulty and possible relief measures to facilitate treatment. 3. Document nursing or caregiver observations of sleeping and wakeful behaviours. Record number of sleep hours. Note physical (e.g. noise, pain or discomfort, urinary frequency) and/or psychological (e.g. fear, anxiety) circumstances that interrupt sleep. 4. Identify factors that may facilitate or interfere with normal patterns. 5. Evaluate timing or effects of medications that can disrupt sleep. 172 Personalised Care Planning: The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to promote optimal amounts of sleep as evidenced by rested appearance, verbalization of feeling rested and improvement in sleep pattern. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. Problem/Need Identification: Record the actual or potential nutritional problem and its associated or related risk factors. For example: “Maureen expresses difficulty of falling asleep following her transfer to the residential home”. Goal Specification: Record: realistic, measurable and obtainable MDT goals. For example: “In two weeks time, Maureen will report that she finds it easier to get to sleep and expresses feelings of being rested” or “Maureen achieves optimal amounts of sleep as evidenced by rested appearance.” Specific Interventions: These are the specific steps taken based on expected standards of care in addressing actual or potential disturbed sleep and rest problems. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: Record: a) Specific interventions to address the resident’s/significant other(s’) concerns, preferences, care choices and religious/cultural requirements e.g. anxiety related to transfer to a residential unit. This can be addressed by providing reassurance that it is quite a common feature that during the settling-in period, a new resident often finds it difficult to sleep, this can be associated with the change in environment, bedding, disruption to normal bedtime routines, worries, fears, etc. It is important to ask the resident about their specific concerns that may be affecting their normal sleep patterns and address these where possible or to refer the resident on to the MDT where concerns fall outside the scope of practice of nurses, e.g., Social Work services for counselling, etc. b) MDT specific care instructions. This includes the nursing care interventions to enhance sleep such as: • Advise the resident to follow as consistent a daily schedule for retiring and arising if possible. • Instruct the resident to avoid large fluid intake before bedtime. • Increase daytime physical activities as indicated, but instruct the resident to avoid strenuous activity before bedtime. • Discourage pattern of daytime naps unless deemed necessary to meet sleep requirements or if part of one’s usual pattern. 173 • • • • • • • • • • • • Consider the following to promote an environment conducive to sleep or rest (e.g. quiet, comfortable temperature, ventilation, darkness, closed door). Suggest use of earplugs or eyeshades as appropriate. Suggest engaging in a relaxing activity before retiring (e.g. warm bath, calm music, reading an enjoyable book, relaxation exercises). Explain the need to avoid concentrating on the next day’s activities or one’s problems at bedtime. Encourage the resident to keep a journal or write down their problems or activities before going to sleep. Suggest hypnotics or sedatives as ordered; evaluate effectiveness. If unable to fall sleep after 30 to 45 minutes, suggest getting out of bed and engaging in a relaxing activity. Provide nursing aids (e.g. backrub, bedtime care, pain relief, comfortable position, relaxation techniques) Eliminate nonessential nursing activities. Prepare the resident for necessary anticipated interruptions and disruptions. Attempt to allow for sleep cycles of at least 90 minutes. Move the resident to a room father from the nursing station if noise is a contributing factor. Post a “Do not disturb” sign on the door. 2. Monitoring and ongoing reassessment • Assess individual’s sleep pattern and changes, naps, amount of activity, awakenings and frequency, and complaints of lack of rest. 3. Communication • Discuss further with the individual as they may have an insight into the aetiological factors of the problem (e.g. depression over the selling of their property, fear of not being able to get out of the unit for family outings). • Promptly communicate monitoring concerns to the resident’s doctor and appropriate members of the MDT team. Update care plans accordingly. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Provide the individual with information on non-pharmacological sleep enhancement techniques such as relaxation techniques, guided imagery, muscle relaxation, meditation, etc. Evaluation of Care (based on goals specified): • Based on the time frame specified, the care plan must be evaluated when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking to see if the goals of care are being met. Refer to the Sample Personalised Care Plan in documenting care planning and in providing care. 174 SAMPLE CARE PLAN Topic Heading: Sleep Enhancement Care Plan PROBLEM / NEED IDENTIFICATION Number: Page 1 Date Signature 01/01/10 Maureen expresses difficulty in falling asleep following her transfer to the residential home. Jane Doe GOAL SPECIFICATION Maureen will report that she finds it easier to get to sleep and expresses feelings of being rested within 2 weeks, or Maureen achieves optimal amounts of sleep as evidenced by daily self report and by her rested appearance. SPECIFIC INTERVENTIONS Date Signature 02/01/10 • • • • • • • • • • Instruct Maureen to avoid stimulants, such as caffeinated drinks (e.g. tea, cola, coffee), stressful activity, prior to sleep Provide nursing aids (e.g. backrub, bedtime care, pain relief, comfortable position, relaxation techniques). Maureen particularly finds a back rub helpful in getting to sleep Provide soft music, and other relaxation techniques Provide ritualistic procedures of warm drink, night prayers, extra covers, and/or warm bath prior to bedtime Promote an environment conducive to sleep or rest (e.g. quiet, comfortable temperature, ventilation, darkness, closed door). Suggest use of earplugs or eyeshades as appropriate. Eliminate non-essential nursing activities Administer medications as ordered to promote normal sleep patterns and monitor their effectiveness If unable to fall sleep after 30 to 45 minutes, suggest getting out of bed and engaging in a relaxing activity Record & monitor the effectiveness of the specific interventions in the Narrative Notes Communicate monitoring concerns to Maureen’s Doctor Provide Maureen with opportunities to discuss her concerns and provide information to help address these where possible or refer to the MDT as appropriate Jane Doe EVALUATION OF CARE (based on goals specified) Date 11/01/10 Maureen verbalizes she had a good night’s sleep and feels rested when asked in the morning. Signature Jane Doe Discontinued Date: …..... / ……… / 20…… Signature: ………………………………………….. 175 References: 176 1 Encarta World English Dictionary (1999), Bloomsbury Publishing Plc 2 The Oxford Pocket Dictionary of Current English (2009) 3 Gulanick, M., Myers, J., Nursing Diagnosis and Intervention, Nursing Care Plans 6th Edition 4 Comer, S., Delmar’s Geriatric Nursing Care Plans 3rd Edition RAP 18: Psychotropic Drug Use Definitions: Psychotropic drugs are substances that act directly on the central nervous system, affecting mood, cognition and behaviour. When used appropriately and judiciously and in accordance with their licensed indications, these medications can enhance the quality of life of residents who need them. It should be noted that most anti-psychotic drugs are not licensed for use of behavioural problem associated with dementia. Risperidone is the only anti-psychotic agent, which is licensed for use with behavioural problem associated with dementia.1 RAI Identifiers of Potential Risks Note: The resident must be prescribed with psychotropic drug under the classification of antipsychotic, antidepressant, antianxiety/hypnotics and mood stabilisers C23, (See list of psychotropic drugs Appendix 1) Potential RAI risks (unwanted effects of psychotropic drugs) that may be triggered include: Impaired Verbal Communication D1, D3, D4, Cognitive impairment and confusion D11, Restless and agitated, D13, D14 Aggressiveness D16, Depression N9, Delusions, Hallucinations, Anxiety D21, Insomnia N9, Dehydration F21, Nausea and Vomiting F23, Urinary Retention G4, Constipation G11, Dizziness H3, Fatigue H3, Falls Risk H6. Special Considerations: Age (65 and above) in relation to prescribed dosage, history of renal, hepatic, respiratory and cardiac conditions; a non-existent ability to communicate and a hypersensitivity to the drug. Unwanted/Side Effects: 1. Presence of movement disorders- Primarily associated with anti-psychotic agents and mood stabilisers. 2. Signs of over sedation 3. Fainting. 4. Unsteady gait. 5. Fall in the past month. 6. Period of altered perception or awareness. 7. Periods of disorganised speech. 8. Mental function varies over the course of the day. 9. Changes in mood. 10. Increased hostility and aggression (may occur as a paradoxical effect of benzodiazepines). 11. Change in behaviour 12. Changes in cognitive function. 13. Alterations in weight and glucose tolerance 14. Hypo or Hyperthermia. 15. Signs of neuroleptic malignant syndrome with antipsychotic drugs: a rare but potentially life threatening acute side effect of some psychotropics: Hyperthermia, sweating, alterations in blood pressure, tachycardia, muscle rigidity. 177 Other Adverse Reactions: • Antipsychotic agents – Residents on long-term anti-psychotic medicines are at increased risk of stroke. However, this risk must be balanced against the drugs positive effect on well being. • Anxiolytics and hypnotics – Dependence and tolerance develop to these agents, which may result in increasing anxiety or insomnia requiring increasing doses. Sudden withdrawal after prolonged use of these medicines is not recommended in older people. Side effects to sudden withdrawal includes: acute confusion, psychosis and convulsions. Note: It is important to consider whether the side effects observed could be related to centrally acting drugs prescribed for other co-morbidities, for example analgesics, antiemetics, antihistamines, anti-cholinergics, medicines for Parkinson’s disease, dementia or epilepsy. Further Assessments: • • • • • • Assess for adverse/unwanted/side effects, note what RAI identifiers were ticked in completing these assessments. Assess for indications of postural hypotension, increasing incidents of falls, dizziness, ataxia or staggering gaits, unsteady movements and lack of co-ordination. Observe for the presence of movement disorders such as Parkinsonism (any combination of tremors, postural unsteadiness and rigidity of muscles in the limbs, neck or trunk), Akinesia (marked decrease in spontaneous movement, often accompanied by non-participation in activity or self-care), Dystonia (marked by holding of the neck or trunk in a rigid, unnatural position. Head is either hyperextended or turned to the side), Akathisia (inability to sit still, person is driven to constant movement, including pacing, rocking or fidgeting which can persist for weeks) and Tardive Dyskinesia (Persistent, sometimes permanent movements induced by long term anti-psychotic drug therapy. Most typical are thrusting movement of the tongue, movements of the lips, or chewing or puckering movements. Other variations include abnormal limb movement, such as peculiar and recurrent posture of the hands and arms, or rocking or writhing trunk movements). Observe for signs of over sedation, drowsiness, delirium and paranoia. Observe for signs of decreased concentration, memory impairment or the person being easily distracted. Complaints of dry mouth and blurred vision. Note: If any suspected adverse reactions or unwanted/side effects are observed, the resident’s Doctor/prescriber must be contacted urgently, to facilitate prompt action in the need for any treatment alterations. A narrative note must be recorded. Suspected adverse reactions are reported to the Irish Medicine Board as per designated centre’s policy. Referrals Required: The medical doctor/prescriber and pharmacist to review medication administration record at least every three months or sooner if side effects are noted. 178 Protocols of Care: 1. Before initiating prescribing, or changing a resident’s medication, due attention should be given to the possibility of the resident’s behaviour resulting from other causes, for example, urinary tract infection, tooth ache, ear ache, constipation, need for change of incontinence pads, leg cramps or other precipitating pain, discomfort, need or stimulus. 2. Assess complaints reported by the resident and observation reported by the staff. Each resident on long-term medication is reviewed by his/her medical practitioner on a three monthly basis, in conjunction with nursing staff and the pharmacist. Special consideration is given on to the use of: - Antipsychotic Medication. - Sleeping tablets and other sedating medication. - Anticonvulsant medication. - Medication for management of depression. - Analgesic medications (pain management). - Medication for the management of constipation. - Antiplatelet and anticoagulant medication (prevention of stroke). - Influenza and pneumococcal vaccines. - Non-steroidal anti-inflammatory drugs. 3. Review medication administration record. This review should involve input from the following people: the resident and their significant others, the nurse, a pharmacist and medical doctor/prescriber. The potential drug related problem should be recorded: a. Drug – drug interaction. b. Drug – disease interaction. c. Contraindication for one or more drugs. d. Evidence of an adverse drug event/ side effect of a drug. e. Assess appropriateness of drug selection. f. Review of dose/ frequency. g. Assess compliance/ concordance problems. h. Problems for safe administration of drug. i. Assess the need for investigations, refer to British National Formulary for recommended routine blood test specific to the psychotropic drug being taken by the resident such as Liver Function Test, Full Blood Count, Urea & Electrolytes, therapeutic drug levels, thyroid function tests and others. 4. Following review of medication and discussions, actions taken should be recorded or documented, such as: a. Discontinue medication. b. Reduce dose. c. Substitute an alternative drug. d. Discuss drug regimen with the resident and their family. e. Discuss side effects with the resident and their family. f. Continue. 5. Assess the resident’s medical condition and identify factors that may impair drug metabolism (i.e. metabolic disorders like renal and hepatic conditions, fluid and electrolytes imbalance-dehydration). 179 6. Assess the resident’s behaviour/mood/overall mental status with recommended assessment tools and his/her current behavioural management if appropriate (i.e. MMSE) (Refer to RAP 2: Mood and Behaviour). 7. Document recommended changes in the resident’s narrative notes and update care plan as appropriate and its rationale. 8. Develop appropriate care plans for other identified needs in collaboration with the resident and their significant others. 9. Inform relevant members of the staff about the changes in the resident’s medication management and nursing care plan. 10. All medication errors, suspected adverse reactions and incidents are recorded, reported and analysed within an open culture of reporting. Learning is fed back to improve resident safety and to prevent reoccurrence. Personalised Care Planning: The aim of the care plan is to develop a single multidisciplinary team (MDT) plan of personalised care that is specific to the management of problems identified with the use of psychotropic drugs. Need/Problem Identification… Record the specific problem and the related factors you have identified relating to the use of psychotropic drugs. For example: John is showing signs of over sedation from his prescribed risperidone medication as diagnosed by his medical doctor. Goal Specification: Record desired outcome/s that is specific, measurable, attainable, realistic and time bound (SMART). For example: John will demonstrate improvement in his thought processes as evidenced by orientation to person, place, time and situation within two days. Specific Interventions: These are the specific steps taken based on expected standards of care in addressing actual or potential problems in psychotropic drug use. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: The following should be recorded: a. Specific interventions to address the resident’s/significant(s) concerns, preferences and care choices. Explain the plan of care, the interventions and the implementation process to manage the identified cognitive problem associated with psychotropic drug use. Encourage the resident and their significant others to ask questions and clarify any information that is not clear. 180 b. MDT specific care instructions. This includes MDT and nursing care instructions and interventions to improve the person’s cognitive function. It also includes the assessment of the person’s cognitive function and management of the identified cognitive problem. Develop a personalised care plan in collaboration with the MDT, the resident and their significant others. 2. Monitoring and ongoing assessment: Continuously observe and assess for signs and symptoms of psychotropic drug toxicity or adverse reaction. For Example: Assess for the resident’s degree of disorientation to time, place, person and situation. Monitor pertinent lab results for signs of drug toxicity as appropriate. 3. Communication Discuss and plan the resident’s care plan with the MDT, the resident and the significant others. Inform or discuss with the members of the MDT, resident and significant others about any changes in the care plan or improvement in the resident’s condition. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers Educate and provide advice to the resident and their significant others regarding the personalised care plan for identifying and managing cognitive problems associated with psychotropic drug use. For example: Disorientation. Provide written information regarding the use of psychotropic drugs and its adverse reaction. Evaluation of Care: Nursing care plans must be evaluated on a regular basis to ascertain if the resident’s condition is improving, deteriorating or if there is no change. Evaluating the nursing care plan determines the effectiveness of the formulated nursing interventions. It is recommended that the nursing care plan must be evaluated every three months or sooner if needed. Refer to the Protocols of Care Flow Chart and Sample Personalised Care Plan in documenting care planning and in providing care. 181 182 10. Behaviour and mood. 9. Functional ability. 8. Level of cognitive ability. 7. Communication difficulties. 6. Current medications. 5. Presence of sign & symptoms of adverse reactions. 4. Presence of conditions stated in the risk category and further assessments. 3. Medical & Social history 2. Observations of staff 1. Complaints of the resident. Document: Nursing Assessment 3. Identify defining characteristics (sign & Symptoms) 2. Identify the common related factors (Cause) 1. Identify the problem Nursing Diagnosis 3. Evaluation of care a. Identify problem/need b. Goal specification (SMART) c. Specific intervention - Specific MDT interventions - Monitoring and ongoing assessment. - Communication - Information/education/health promotion for resident, significant other and carers. 2. Develop nursing care plan incorporating the following: 1. Nursing goals should focus on maximising the resident’s functional potential and well being while minimising the hazards associated with drug side effects. Establish nursing goals and devise care plan Nursing Care Goals & Planning 2. Unmet Goals - Reassess and review nursing care plan Establish effectivity of nursing and MDT interventions 1. Goals met - Sign off the nursing care plan Establish effectivity of nursing and MDT interventions Nursing Evaluation Protocol of Care in the Delivery of Personal Care in HSE Older Designated Centres SAMPLE CARE PLAN Topic Heading: Disorientation PROBLEM / NEED IDENTIFICATION Number: Page 1 Date Signature 01/01/10 John has disturbed thought processes related to unwanted side effects of psychotropic drug Risperidone as diagnosed by the doctor. Jane Murphy GOAL SPECIFICATION John will demonstrate improvement in his thought processes as evidenced by orientation to person, place, time and situation within two days. SPECIFIC INTERVENTIONS Date Signature 01/01/10 • • • a) b) c) d) • a. b. c. d. e. • • • • • Assess John’s degree of disorientation to time, place, person and situation at each shift, record on the flow chart of care. John’s medication has been reviewed with his significant others, medical doctor and pharmacist. It has been agreed to gradually reduce Risperidone therapy under close monitoring to avoid the risk of acute withdrawal syndrome. Administer reduced dose as prescribed. Monitor for other signs and symptoms of psychotropic drug toxicity or adverse reaction. Monitor vital signs 4 hourly x 48hours, observe for: Postural hypotension- Record Blood Pressure lying and standing, twice daily. Tachycardia Assess finger stick blood sugar Record all episodes of disturbed thought processes using a Mood and Behaviour diary (ABC Functional Analysis Chart) Orient John to surroundings and reality as needed: Use John’s name when speaking to him. Speak slowly and clearly. Refer to time of day, date and recent events when interacting with John. Encourage John’s wife Jean to bring familiar personal belongings into the residential care setting. Provide reality orientation with respect and sensitivity when correcting John’s misperceptions of reality. Use the words “You” and “ I” instead of We when talking to John. Maintain a consistent fairly structured routine. Encourage John to participate in activities (Refer to John’s Meaningful Activities care plan). Have John perform only one activity at a time and allow adequate time for performance of activities. Assist John to problem solve if necessary. Involve his wife Jean to participate in helping John with his ADL’s. Communicate monitoring concerns to the doctor or if disturbed thought processes worsen. Jane Murphy EVALUATION OF CARE (based on goals specified) Date Signature John is now able to tell the time, place and identify person but still Jane Murphy 02/01/10 requires assistance in problem solving situational events. John is for review by the doctor tomorrow. Care plan to be updated following review Discontinued Date: …..... / ……… / 20…… Signature: ………………………………………….. 183 References: Medicines and Healthcare Regulatory Agency (2010) Antipsychotic drugs http://www.mhra.gov.uk/Safetyinformation/Generalsafetyinformationandadvice/Prod uct-specificinformationandadvice/Antipsychoticdrugs/index.htm 2 British Medical Association and Royal Pharmaceutical Society of Great Britain, British National Formulary. 3 Culhane C. (2005) A Guide to Psychotropic Drugs. Mental Health Research Institute, Melbourne, Australia. 4 Health Information and Quality Authority (2009) National Quality Standards for Residential Care Settings for Older People in Ireland. Health Information and Quality Authority Dublin, Ireland. 5 Irish Medicines Board (2009) Drug Safety Newsletter, 30th Ed, Update on safety of antipsychotic medicines – Risk of stroke and increased risk of mortality in elderly patients treated for dementia. Pharmacovigilance section, Irish Medicine Board, Dublin. 6 Linton A.D. & Lach H.W. (2007) Matteson & McConnell’s Gerontological Nursing, Concepts and Practice (3rd ed). W.B. Saunders Company, St. Louis Missouri. 7 Nursing Home Ireland (2009) Medication management template: standards for practice in residential care. Nursing Home Ireland, Dublin Midleinster. 8 Redfern S. & Ross F.M. (2006) Nursing Older Person (4th ed). Elsevier Church Hill Livingstone, United Kingdom. 9 Stone J.T., Wyman J.F. & Salisbury S.A. (1999) Clinical Gerontological Nursing, A guide to advanced practice (2nd ed.) W.B. Saunders Company, Philadelphia. 10 Voyer P., Cohen D., Lauzon S. & Collin J. (2004) Factors associated with psychotropic drug use among community dwelling older persons: A review of empirical studies available on line http://www.biomedcentral.com/1472-6955/3/3. 11 www.medicines.ie (The IPHA website contains the summary of product characteristics and patient information for most licensed drug in Republic of Ireland. 1 184 Appendix 1: Psychotropic Drugs What are Psychotropic drugs? Psychotropic drugs can be described as any drug capable of affecting the mind, emotions and behaviour. This group of drugs act primarily on the CNS (Central Nervous System) where it alters brain function resulting in temporary changes in perception, mood, consciousness and behaviour. Psychotropic drugs are used in medical day to day practice but are also substances of abuse. Some substances of abuse include Caffeine, Alcohol, Cocaine and Cannabis. The most common groups of drugs classified as psychotropic are; • Hypnotics • Anxiolytics • Antipsychotic: – Typical – Atypical • Mood Stabilisers – some of which are anti-epileptic drugs • Antidepressants: – Tricyclic – MAOI’s – SSRI’s – Others • CNS stimulants and drugs used in ADHD • Drugs used in substance dependence DRUG GROUP DRUG NAME INDICATIONS FOR USE Hypnotics (Mainly Benzodiazepines) Nitrazepam Flunitrazepam Flurazepam Loprazolam Lormetazepam Temazepam Zaleplon Zolpidem Zopiclone Chloral Hydrate Triclofos Sodium Clomethiazole Promethazine Triazolam Treatment of insomnia 185 186 DRUG GROUP DRUG NAME INDICATIONS FOR USE Anxiolytics (Mainly Benzodiazepines) Diazepam Alprazolam Chlordiazepoxide Lorazepam Buspirone Meprobamate Barbiturates Prazepam Clobazam Bromazepam Pregabalin (Lyrica) Hydroxyzine Alleviating anxiety states Pregabalin is an antiepileptic drug indicated for use in generalised anxiety disorder. Antipsychotics (Typical - Older) Chlorpromazine Flupentixol Haloperidol Levomepromazine Pericyazine Perphenazine Pimozide Prochlorperazine Promazine Sulpride Trifluoperazine Zuclopenthixol Schizophrenia Relieve symptoms such as thought disorder, hallucinations, delusion and also prevent relapse. Antipsychotics (Atypical - Newer) Amisulpride Ariprazole Clozapine Olanzapine Paliperidone Quetiapine Risperidone Sertindole Zotepine Schizophrenia Relieve symptoms such as thought disorder, hallucinations, delusion and also prevent relapse. Mood Stabilisers Lithium Carbamazepine Lamotrigine Sodium Valporate Lithium used in mania to control acute attacks and to prevent their recurrence. Also used in the prophylaxis of bipolar disorder (manicdepressive disorder). All other drugs are anti-epileptic agents used in bipolar disorder. DRUG NAME INDICATIONS FOR USE Amitriptyline Clomipramine Dosulepin Doxepin Imipramine Lofepramine Nortriptyline Trimipramine Mianserin Trazadone Moderate to severe depression. Also used in the management of panic disorders and neuralgia. Antidepressant drugs (Monoamine-oxidase inhibitors) MAOI’s Phenelzine Isocarboxazid Tranylcypromine Moclobemide (reversible MAOI) Depressive illness unresponsive to other antidepressants. Have high food and drug interactions. Antidepressant drugs (Selective serotonin reuptake inhibitors) SSRI’s Citalopram Escitalopram Fluoxetine Fluvoxamine Paroxetine Sertraline Depressive illness, also used for panic disorder, obsessivecompulsive disorder, generalised anxiety disorder, social anxiety disorder and bulimia nervosa. Antidepressant drugs (Others) Duloxetine Flupentixol Mirtazapine Reboxetine Tryptophan Venlafaxine Depressive illness, also used for diabetic neuropathy (duloxetine), stress urinary incontinence (duloxetine) and generalised anxiety (Venlafaxine) CNS stimulants and drugs used in ADHD Atomoxetine Dexamfetamine Methylphenidate Modafanil Treatment of attention deficit hyperactivity disorder – Atomoxetine, dexamfetamine and methylphenidate. Treatment of daytime sleepiness associated with narcolepsy- Modafanil. Drugs used in substance dependence Acamprosate – alcohol Disulfiram – alcohol Bupropion – nicotine Nicotine – nicotine Varenicline – nicotine Buprenorphine – opioid Lofexidine – opioid Methadone – opioid Naltrexone – opioid Drugs used to help in the withdrawal of alcohol, nicotine and opioids. DRUG GROUP Antidepressant drugs (Tricyclics and related) 187 RAP 19: MRSA (Methicillin Resistant Staphylococcus Aureus) Colonization and Decontamination Protocol This protocol deals only with MRSA colonization which requires a multidisciplinary team (MDT) approach to assessment and management. If MRSA is present with signs of infection, then advice on such infections must be sought from the resident’s doctor and the Infection Control Team. Definitions: MRSA stands for methicillan-resistant Staphylococcus aureus. Staphylococcus aureus live harmlessly on the skin and in the nose of approximately a third of the population. Some strains of Staphylococcus aureus have developed resistance to Methicillin (a type of penicillin) and other common antibiotics. These resistant strains of Staphyloccous aureus bacteria are called MRSA.1 MRSA colonization means that MRSA is present on the body or in the nose of an individual but is not causing any ill effects or infection. MRSA infection means that the MRSA is causing clinical signs and symptoms of local or systemic infection, which require prompt medical intervention. Systemic signs of infection may include: elevated temperature (fever), general malaise, nausea/vomiting, tachycardia, acute confusional state/delirium (Refer to RAP 3: Cognition and Acute Confusion), hypotension and leukocytosis. Local signs of infection may include: pain/soreness, spreading skin redness (erythema) or tracking as for IV sites; for signs and symptoms of local wound infection refer to RAP 13: Skin and Wound Care. RAI Identifiers of Potential Risks: MRSA positive, A59 Other Risk Factors for MRSA colonization include: Advanced age, the very ill, open wounds or sites such as skin lesions, leg ulcers, pressure ulcers, PEG sites, I.V. sites, tracheotomy and urinary catheters. While inadequate care practices e.g. inadequate hand hygiene, lack of Standard Precautions in Infection Control or a history of recent hospitalisation (within previous 6 months of admission), a history of multiple courses of antibiotics, excessive antibiotic duration or under-dosing create further risks.1 Further Assessments: A. Screening for MRSA Residents should be screened on first admission only, to identify the presence of MRSA. Respite residents need not be screened on subsequent admissions unless they have been exposed to a possible risk of contracting MRSA (i.e. they have been resident in another healthcare facility between respite admissions). MRSA screening sites: • Nasal (anterior nares), one swab only • Perineum or groin, one swab only • All sites where the resident has a break in skin, e.g. wounds, I.V., PEG sites. 188 • • PLEASE NOTE: Throat, Axilla, Sputum and CSU/MSU’s are not routinely screened. Urine samples are only to be sent if there are signs of a Urinary Tract Infection (UTI). When sending a urine sample, please record the reason for sending the sample on the lab form, e.g. pyrexia, frequency, dysuria, clinical signs/symptoms of UTI. Note: The presence of a urinary catheter is not an indication for sending a urine sample. Each sample must be accompanied by its own individual laboratory form fully completed. B. Risk Assessment of MRSA Positive residents A multidisciplinary team risk assessment (e.g. doctor, infection control nurse/team, ward nurse) must be undertaken on all residents who screen positive for MRSA to determine: (i) Is the resident colonized or infected (ii) The appropriateness of ward/room allocation for the resident. Residents who are MRSA positive must not share bedrooms with residents who have any of the following conditions: • Eczema/skin lesions/open wounds • Chronic respiratory problems, tracheotomy • PEG, urinary catheters or IV lines • Immunosuppressed (ii) If a decontamination protocol is required. For example: • Decontamination is recommended for residents who are planned for elective surgery • MRSA positive residents maybe cohorted together or isolated (if appropriate), after discussion with the Infection Control Team If in doubt of risks posed, seek advice from your local Infection Control Team. If the MRSA screen is positive or it is identified on admission that the resident has MRSA, an “MRSA positive resident check sheet” should be completed and inserted into the resident’s care record (Appendix 1). Referrals required: Refer the resident to the multidisciplinary team (Doctor, Infection Control Team) to determine the risk with regard to the appropriateness of room allocation and whether or not a decontamination protocol is required. Further referrals should be made as soon as concerns arise e.g. on daily review, concerns on re-screening results following MRSA decontamination, etc. Record all referrals made on the MDT Referral Record. Personalised Care Planning: The aim of care planning is to develop a single multidisciplinary team (MDT) plan of personalised care to address the actual or potential risks of MRSA colonization or infection. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. 189 Problem/Need Identification: Record the resident’s MRSA status and its associated or related risk factors. For example; ‘MRSA identified on nasal and groin Swab 12/01/10 which creates a potential risk of crossinfection’. Goal Specification: Record: realistic, measurable and obtainable MDT goals. For example: ‘To eradicate MRSA skin and nasal carriage within a five day period and to prevent MRSA cross contamination/infection’ Specific Interventions: These are the specific steps taken based on expected standards of care in addressing MRSA colonization and in preventing cross contamination/infection. Document: • What we need to do (specific interventions based on the resident’s/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 190 1. Specific MDT interventions Record the: a. Specific interventions to address the resident’s/significant others(s) concerns, preferences and care choices. Encourage the resident/significant other(s) to voice their concerns. Provide psychological support and information on MRSA colonization to the resident and their significant others. Discuss and address where possible the resident’s/significant other(s’) concerns. Where it is not possible to address the resident’s/significant other’s concerns, seek advice from the local Infection Control Team and inform the resident/significant other of the Infection Control Team’s advice. b. MDT specific care instructions. This includes nursing care instructions for addressing MRSA colonization and for the control and prevention of infection. Other specific MDT care instructions should be listed here. For example: a Doctor’s specific instructions for MRSA decontamination or the Infection Control Team’s specific instructions for care. • Contact Precautions in addition to Standard Precautions must be used in caring for residents with MRSA. i. Hand hygiene, before and after every contact with the resident or their immediate environment is essential. Encourage the resident to practice good hand hygiene and be assisted with this if their physical or cognitive condition makes this difficult (Refer to SARI Hand Hygiene Guidelines).2 ii. Disposable aprons/ gloves should be worn if contact with body fluids or dressings are expected and hands should be washed after removing the gloves. Use a fluid-shield mask with visor if splashing to the face is likely. iii. The resident’s physical environment should be kept clean and dust free. Chemical disinfection is not required for equipment with which the MRSA colonized resident has been in contact e.g. a commode, cleaning with detergent and hot water is recommended. However, where there is a risk of heavy shedding (e.g., MRSA positive urine, MRSA throat colonization with the resident spitting, etc,) it is advisable to follow routine cleaning with disinfection with a suitable disinfectant such as chlorine (e.g. Presept, Actichlor). Clothes and bedding should be machine-washed, preferably on the hottest wash that the fabric will allow and where possible to follow this with tumble drying. Clothes may dry-cleaned if unsuitable for machine washing. • • • Residents colonized with MRSA may join other residents for therapeutic care and social activities in the sitting room, dining room and other communal areas. Isolation of residents is generally not required, other than in exceptional circumstances. These include where a resident poses a risk of shedding large numbers of bacteria (e.g. heavily exudating wounds not contained by dressings or tracheostomy with frequent coughing), or where resident’s have been implicated in the development of infection in other residents. Due to the negative impact of isolation on residents’ psychosocial well-being, advice on whether isolation is truly necessary must be sought from the Infection Control Team (ICT). Complete an MRSA positive resident check sheet and maintain this in the resident’s care record. MRSA Decontamination Process (5 Day Protocol)- if indicated after a risk assessment; for some residents colonized with MRSA, decontamination may be indicated. This protocol is to be attempted once only, unless otherwise specified by the ICT. Please ensure that staff who perform the MRSA protocol, (if indicated by the risk assessment) adhere strictly to the protocol guidelines, in order to provide the resident with the best chance of achieving a successful decontamination and to avoid future resistance. The decontamination preparations must be used for a full 5 days as follows: A) MRSA Nasal colonization: i. Apply Mupirocin Ointment to the nasal cavity three times a day as prescribed. Method for applying Mupirocin: • Ask resident to blow his/her nose into a disposable tissue. • Squeeze a pea size amount of ointment onto a cotton bud and apply to inside of the nostril. • Repeat for other nostril. • Spread the ointment inside each nostril by pressing the nose together for a moment. Do not use Mupirocin on: • Residents who do not have MRSA carriage in their nasal cavity or • Where the MRSA identified is known to be resistant to Mupirocin, seek the advice of the Infection Control Team B) MRSA Skin colonization: i. Wash hair with Triclosan (EPI WASH) or Chlorhexidine on the first and the third day of treatment. ii. Each of the 5 days wash body all over with Triclosan (EPI WASH) or Chlorhexidine using a disposable cloth. NOTE: SOAP/SOAP SUBSTITUTES MUST NOT BE USED DURING THE 5 DAY PROTOCOL. iii. Clothes day/night, underwear and bed linen should be changed daily after shower/wash. C) MRSA Throat colonization: i. Chlorhexidine mouth wash (CORSODYL) if prescribed should be gargled three times a day. D) MRSA wound colonization: i. Wounds to be cleaned with normal saline and an appropriate impermeable dressing applied. 191 Supply and use of following products for residents, must be prescribed by the doctor and obtained through a pharmacy: • Triclosan (EPI WASH) or Chlorhexidine 250mls for each individual resident • Mupirocin • Corsodyl mouthwash. All the above products are for single resident use only. The protocol is discontinued after 5 days. 2. • • • Monitoring and ongoing reassessment: 48 hours following the last protocol day, the resident is re-screened for MRSA. Monitor the resident’s skin for any signs of allergies to the decontamination products. Monitor the resident for signs and symptoms of infection. 3. Communication • Promptly communicate any monitoring concerns to the resident’s doctor, or Infection Control Team. Update care plans accordingly • Communicate the resident’s personalised Infection Prevention and Control care plan to all those involved in the resident’s direct care. Ensure the resident’s significant others/visitors are aware of the required infection control precautions. Ensure the resident/significant other(s) is kept up to date on their plan of personalised care. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Communicate and educate residents and relatives on the importance of hand washing and contact precautions in preventing the spread of MRSA. Support this with resident information leaflets on MRSA (available from www.hspc.ie) or provide information in a format that suits the resident’s communication requirements (Refer to RAP 1: Communication, Vision and Hearing).3 Evaluation of Care (based on goals specified): • MRSA Care Plans must be evaluated when the resident’s condition improves or deteriorates and at least 3 monthly. Evaluate the effectiveness of the care provided by checking to see if the goals of care are being met e.g. results of re-screening. Refer to the ‘Protocol of Expected Standards for Care’ flow chart and sample ‘Personalised Care Plan’ in documenting personalised care planning and in providing care. 192 193 1. Assess MRSA status on admission. 2. Screen all residents on first admission only. 3. Respite residents need not be re-screened on subsequent re-admissions unless they have been resident in another healthcare facility in the interim period between respite admissions. 4. MRSA screening sites: • Nasal (anterior nares), one swab only. • Perineum or groin, one swab only. • All sites where there is a break in the skin, e.g. wounds, I.V./PEG sites. • NOTE: Throat, axilla, sputum, CSU/MSU are not routinely screened unless there are signs & symptoms of infection. Nursing AssessmentDocument (On admission) Nursing Assessment MDT Risk Assessment to decide: 1. If the resident is Infected or Colonized 2. Decide on bed allocation. MRSA positive residents should not share a bedroom with residents who have: • Eczema/skin lesions/open wounds. • Chronic respiratory problems, tracheotomy. • PEG, urinary catheters or I.V. lines. • Immunosuppressed. 3. Following a risk assessment to decide on whether decontamination is required i.e. • Decontamination is recommended if the resident is for elective surgery. • If Infection Control Team Recommend MRSA identified on admission or following screening Nursing Diagnosis Goal: Prevention and Control of MRSA 1. Encourage resident/significant other(s) to voice concerns. Provide psychological support & information to address concerns where possible or seek advice from local Infection Control Team (ICT). Provide education on hand hygiene & infection control to residents / significant other(s), visitors & carers. Support with MRSA information leaflets. 2. Use Standard Precautions & Contact Precautions in providing care. Chemical disinfection of communal equipment (e.g. commodes) is not required. Clean all equipment with hot water & detergent after use. 3. MRSA colonised residents do not normally require isolation & can participate in therapeutic & social groups. In exceptional cases (e.g. tracheostomy with frequent coughing) ICT advice should be sought before decisions on isolation are made. 4. Monitor for signs of infection. Goal: Sleeping arrangements: cohort MRSA Positive Residents *(ward/unit) & provide standard and contact infection control measures as outlined above Goal: MRSA Decontamination-(5 day Protocol) (Include all Infection Control measures as above) 5. Nasal carriage: Apply Mupirocin ointment as prescribed (do not use for residents with NO MRSA nasal carriage or for Mupirocin resistant MRSA). 6. Skin carriage: Wash daily head to toe (hair- 1st / 3rd day) with Triclosan (Epi Wash®) or Chlorohexidine. 7. Throat carriage: Gargle with Chlorhexidine mouth wash (Corsodyl®) 3 times daily as prescribed. 8. Wound carriage: use appropriate impermeable dressing Nursing Care Goals & Planning Refer to the Infection Control Team & Resident’s doctor for advice. Goal not met -MRSA not eradicated • Resident/carer is aware of appropriate infection control measures and have been given leaflets on MRSA (available from www.hspc.ie ). • Continue to provide appropriate infection control measures (standard precautions). NB Reassess MRSA status if concerns arise. Goal met MRSA carriage eradicated • Continue to provide standard and contact infection control measures & monitor for signs of infection Goal met- MRSA colonized residents Cohorting Nursing Evaluation Protocols for Care in the Control and Prevention of MRSA in HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: MRSA Care Plan PROBLEM / NEED IDENTIFICATION Number: Page 1 Date Signature 02/02/10 Margaret has MRSA skin and nasal colonization as identified by swab results on the 30/01/10. Margaret with the multi-disciplinary team has identified a need for decontamination. Jane Murphy GOAL SPECIFICATION To prevent Margaret from developing MRSA infection and eradicate MRSA skin and nasal carriage within 5 days. To control and prevent MRSA cross infection. SPECIFIC INTERVENTIONS Date Signature 02/02/10 • • • • • • • • • • • • Margaret was very upset hearing that she had MRSA, her main concern is that she is afraid of ‘passing it on’ to her family and fellow residents. Provide Margaret with opportunities to discuss her worries and reinforce information/education on MRSA. MDT risk assessment carried out. Specific instructions; commenced on 5 day MRSA decontamination protocol. Apply Mupirocin ointment to nasal cavity as prescribed. Method: ask Margaret to blow her nose into a disposable tissue. Squeeze a pea sized amount of Mupirocin onto a cotton bud and gently apply to inside of nostril. Repeat for other nostril. Ask Margaret to gently press her nose together to spread the ointment inside her nose. Ensure Margaret has a daily shower using Triclosan, encourage Margaret to wash her hair with Triclosan on the 1st & 3rd day. Change Margaret’s day & night clothes, underwear & bed linen daily for 5 days. Infection control contact precautions and standard precautions are to be used in care delivery. MRSA positive check list completed-update document following the 5day decontamination protocol. Margaret is to be encouraged to participate in social activities Monitor daily for signs of skin allergies to Triclosan and for signs & symptoms of infection. Re-screen for MRSA 48hours post last protocol day. Communicate monitoring concerns promptly to Margaret’s doctor/Infection Control Team. Information/education sessions to be provided to Margaret & her family on the importance of hand washing and the control & prevention Jane Murphy of infection. Resident Information Leaflets on MRSA given to Margaret and her family. EVALUATION OF CARE (based on goals specified) Date 03/02/10 No skin allergies noted. Plan continued. Signature Jane Murphy Discontinued Date: …..... / ……… / 20…… Signature: ………………………………………….. 194 Suggested Further Reading: Health Protection Surveillance Centre (2005) Guidelines for Hand Hygiene in Irish Health Care Settings http://www.hpsc.ie/hpsc/A-Z/Gastroenteric/Handwashing/Guidelines/File,1047,en.pdf Health Protection Surveillance Centre (2005) The Control and Prevention of MRSA in Hospitals and in the Community http://www.hpsc.ie/hpsc/AZ/MicrobiologyAntimicrobialResistance/EuropeanAntimicrobi alResistanceSurveillanceSystemEARSS/ReferenceandEducationalResourceMaterial/Saureu sMRSA/Guidance/ References 1 SARI (2005) The Control and Prevention Of MRSA in Hospitals and in the Community, HSE Health Protection Surveillance Centre 2 Health Protection Surveillance Centre (2005) Guidelines for Hand Hygiene in Irish Health Care Settings http://www.hpsc.ie/hpsc/A-Z/Gastroenteric/Handwashing/Guidelines/File,1047,en.pdf 3 HIQA (2009) National Quality Standards for Residential Care Settings for Older People in Ireland 195 Appendix 1: MRSA Positive Resident Checklist Forms should be completed on all residents who return a positive culture for MRSA and checklist to be maintained in the resident’s Care Record NAME Dates Samples Sent Site/Sites Positive Mupirocin Resistance MRN DATE OF BIRTH 1st 2nd (Circle As Appropriate) If yes: High Level resistance Low Level Resistance Yes/No Yes/No Yes/No Risk Assessment see protocol (Circle As Appropriate) • • (i) Does resident require isolation (ii) Does resident require cohorting Yes/No Yes/No Is Decontamination If Yes indicated Yes /No Date commenced Resident/Next Of Kin Informed Yes /No Information leaflet given Yes /No Action: Isolated / Cohorted / Other (Circle As Appropriate) Any Further Action or comment: 196 Signature WARD/UNIT RAP 20: Feeding Tubes Definitions: A feeding tube is a medical device used to provide nutrition to residents who cannot obtain nutrition by swallowing. The state of being fed by a feeding tube is called enteral feeding or tube feeding. Placement may be temporary for the treatment of acute conditions or lifelong in the case of chronic disabilities. A variety of feeding tubes are used in medical practice. They are usually made of polyurethane or silicone. The diameter of a feeding tube is measured in French units (each French unit equals 0.33 millimetres). They are classified by the site of insertion and intended use. Re-feeding syndrome: residents that have eaten nothing for more than 7 days are at high risk of this phenomenon. ‘Re-feeding syndrome’ usually occurs within four days of starting to feed again and can occur with parental, enteral and oral re-feeding. It is caused by an intracellular loss of electrolytes, in particular phosphate due to starvation. Serum phosphate concentrations of less than 0.50 mmol/l (normal range 0.85-1.40 mmol/l) can produce the clinical features of re-feeding syndrome, which includes: rhabdomyolysis (release of muscle fibre contents-myoglobin into the bloodstream resulting in kidney damage), leucocyte dysfunction, respiratory failure, cardiac failure, hypotension, arrhythmias, seizures, coma, and sudden death (Hearing, 2004). Types of Feeding Tubes: 1. Nasogastric Tube A naso-gastric (NG) feeding tube is passed through the nares (nostril), down the oesophagus and into the stomach. It is generally not recommended for long term use. 2. Gastric feeding tube A gastric feeding tube (or "G-tube," or "button") is a tube inserted through a small incision in the abdomen into the stomach and is used for long-term enteral nutrition. The most common type is the Percutaneous Endoscopic Gastrostomy (PEG) tube. It is placed endoscopically: the resident is sedated, and an endoscope is passed through the mouth and oesophagus into the stomach. The tube is kept within the stomach either by a balloon on its tip (which can be inflated / deflated) or by a retention dome which is wider than the tract of the tube. Gastric tubes are suitable for long-term use; they last about six months, and can be replaced through an existing passage without an additional endoscopic procedure. 3. Jejunostomy Tubes (J Tube): Jejunostomy tubes are useful for residents with contraindications to gastrostomy tubes e.g, gastrectomy, and bowel obstruction proximal to the jejunum. However, these tubes do not pose less risk of tracheo-bronchial aspiration than gastrostomy tubes, as is often thought. Jejunostomy tubes are easily dislodged and are not usually recommended for long term use. 197 Indications for enteral nutrition include the following: • Prolonged anorexia. • Severe protein-energy under-nutrition. • Coma. • Liver failure. • Inability to take oral nutrition due to head or neck trauma or neurological disorders resulting in impaired gag reflexes. • Critical illnesses e.g. burn injury, causing metabolic stress. Other indications may include bowel preparation for surgery in seriously ill or seriously undernourished resident’s, closure of entero-cutaneous fistulas, and small-bowel adaptation after intestinal resection or in disorders that may cause malabsorption e.g. Crohn's disease. RAI Identifiers of Potential Risks: Enteral Feeding F4 Risks/Complications associated with having a feeding tube include: 1. Mechanical complications • Tube blockage: this results from deposition within the tube and may be addressed by following instructions under Flushing tubes. • Tube displacement. • Tube dysfunction/malfunction. • Tube leakage. 2. Infective complications • Infection- this can occur due to contamination of the feed or aspiration pneumonia. 3. Gastrointestinal complications • Gastro - oesophageal reflux: this can lead to aspiration if not addressed. • Diarrhoea: this is characterised by frequent loose, watery stools (3 or more episodes in a day). It is rarely due to the feed type. • Constipation: this is characterised by few bowel movements (absence of bowel movement for longer than 3 days) with hard stools causing pain and discomfort. Determine cause of constipation, refer to RAP: 9 Constipation. The enteral feed should only be stopped if faecal impaction is suspected or the resident has overflowing diarrhoea. If possible eliminate cause of constipation in conjunction with the resident’s doctor and dietician re: feed regimen and/or need for medication (laxatives). • Nausea/Vomiting: This may not be due to the feed type. 4. • • • 198 Metabolic complications Over/under hydration Raised blood glucose levels. Bio-chemical/electrolyte imbalances. 5. Drug/Nutrient interactions Interactions between enteral feeds and drugs can occur. The bioavailability/ absorption of drugs may be affected by enteral feeding, so it is important to check for this with the pharmacist before administering any medication via the enteral feeding tube. 6. • • • • Stoma Related complications Overgrowth of granulation tissue. Infection at stoma site Stoma leakage. Buried Bumper Syndrome (Buried bumper syndrome is a complication of PEG tubes where the disc becomes buried in the wall of the stomach. Preparation of the resident prior to transfer to an acute setting for PEG insertion: 1. A multidisciplinary team meeting should be organised to discuss the resident’s nutrition/hydration status and available options with the resident/significant other/advocate. The decision for PEG tube insertion should be based on the resident’s/significant other(s) wishes/ care preference where possible. 2. Nursing staff and the dietician must document a formal nutritional screening and assessment using a validated tool e.g. MNA, MUST. 3. A PEG feeding regimen is drawn up by the dietician and must accompany the resident on transfer to the hospital performing the procedure. 4. Prevention of “Re-Feeding syndrome” should be a priority. 5. Residents will need to fast for 12 hours prior to PEG insertion Post PEG insertion: 1. On return to the Older Persons designated centre the resident is kept fasting as per post operative instructions. 2. Assess the resident for signs and symptoms of pain or discomfort using a validated tool (refer to RAP 16: Pain) and appropriately address pain/discomfort where present. 3. Ensure all equipment required i.e. feeding pump/appropriate feed/giving sets, etc, as per dietician’s instructions are available. 4. PEG Feeding should not commence for the first 6-10 hours (refer to post-operative sheet). • Evaluate all enterally fed residents for risk of aspiration. • Assure that the feeding tube is in the proper position before initiating feedings (See section below titled: Procedure for checking correct positioning of an enteral tube). • Keep the head of the bed elevated at 30°-45° at all times during the administration of enteral feedings. • Check gastric residuals every 4 hours during the first 48 hours for gastrically fed residents. After enteral feeding goal rate is achieved, gastric residual monitoring may be decreased to every 6-8 hours in non-critically ill residents. However, every-4-hours measurements are prudent in critically ill residents. 199 If the Gasrtic Residual Volume (GRV) is ≥ 250mL after a second gastric residual check, a promotility agent should be considered. Contact the resident’s Doctor and Dietician to discuss the plan of care. Document the referrals made on the resident’s MDT referral record and in the resident’s narrative notes. • A GRV ≥ 500mL should result in holding the enteral feed and reassessing resident tolerance by the Doctor/Dietician to include a physical assessment, GI assessment, evaluation of glycemic control, minimization of sedation, and consideration of promotility agent use, if not already prescribed. • Consideration of a feeding tube placed below the ligament of Treitz when GRVs are consistently measured at > 500mL. (American Society for Parenteral and Enteral Nutrition [2009]). • Note: Aspiration of small bore tubes is not recommended. GRV of < 500mL should be returned unless contra indicated by resident risk i.e. resident retching, vomiting, complaining of nausea, etc. Following the first 48 hours, the frequency of GRVs should be as per dietician’s instructions. 5. Site care: Following the initial tube insertion, a channel of scar tissue forms between the gastric wall and the abdominal wall. This process takes between 10 -14 days. During this time there is a risk of cellulitis and peritonitis. Always wash hands with soap and water, dry with a disposable paper towel or use alcohol gel on visibly clean hands before and after contact with the stoma site and feeding apparatus. Wear gloves if in contact with body fluids and follow standard infection control precautions. Discuss care and management with the resident, supporting and encouraging them to manage their own care if possible. • 200 Care Immediately postplacement (up to 48hrs ) PEG tube site Care (day 3 until stoma is healed). Long term PEG tube site care (after stoma site has healed, 14 – 21 days). • Treat the entry as a surgical wound for the first 48hrs. • Do not touch the site & tube for 8-12 hrs after placement. • After 12 hours remove dressing, observe site for signs of swelling,bleeding or infection. • Cleanse site & fixation device with sterile normal saline using an aseptic technique. • Apply a thin dry sterile dressing only if required to absorb exudate. Do not release the fixation device. • After 48hrs non-sutured tubes must be rotated 360 degrees daily to avoid infections related to buried bumper syndrome. • Tube should be pushed in by 5mm & gently pulled back to prevent buried bumper syndrome. • Tubes that are sutured should be rotated following removal of the suture. • A clean technique using sterile equipment e.g. dressing pack with non woven gauze should be used until the tract has healed. • Do not release the fixation device • No dressings required • Residents may shower but should not have a plunge bath until tract is healed Ensure that daily PEG tube observation chart is updated (Appendix 1) • Inspect the site daily. • Wash with warm water and rinse daily, dry thoroughly with a clean dry towel. • The fixation device should be separated from the base to allow further cleaning on a daily basis. • Ensure the tube is replaced to the correct position in relation to the fixation device when cleaning is completed • Ensure the tube is secured (tapped) without pressure to the abdominal wall to prevent friction and the development of granulomas at the stoma site. • Apply a dressing if there is a discharge. • Do NOT apply antiseptic creams to the site as they may damage the tube. Plunge baths are permitted once the stoma site has healed. 5. Checking the Balloon (For CORFLO Gastostomy tube only) The balloon volume should be checked weekly and documented in the resident’s care plan. Prior to the procedure the nurse should check the resident’s care plan to: • • • • • • • • Establish the amount of water in the balloon. Equipment required: • 2x 10ml syringes one to withdraw the water and one with the correct amount of sterile water to re inflate the balloon. • Sterile Gloves. • Sterile water. Dispose of syringes in sharp disposal container. Using a syringe to withdraw the contents of the balloon, while carefully holding the tube in place to avoid displacement. Observe the amount of fluid withdrawn and re insert the correct amount. Observe the resident for any pain, discomfort or pressure around the site during and after the procedure. Report any concerns to the doctor. Document that the procedure has been carried out in the narrative notes and document the date of when the next weekly check is due. Procedure for the administration of a Tube Feed: Equipment required: • Drip Stand/ attachment for bed, feeding pump, feed and giving set. Note: Feeding pumps and drip stands must be cleaned daily with a detergent. They should be disinfected where required with hypochlorite 1:1000 e.g. Presept when contaminated with body fluids or when used by residents who are in source isolation. • 50ml syringe, sterile water. Note: Syringes used for aspiration, flushing, administering medication and bolus feeding are for ‘single use’ only. Therefore, they must be discarded following use as per disposal of sharps guidelines. Syringes may be discarded into sharps safe bin, 50ml syringes used for feeding may be discarded into household waste (provided it is NOT contaminated with blood). • Disposable Gloves / paper towel • Sterile Scissors (if required) • Waste disposable bag • PEG observation chart • Enteral feeding pumps should be serviced annually in line with the manufacturer’s recommendations. • Bottle openers if used should be dedicated for use with enteral feeding products only. Prior to use clean with a mediswab and allow to dry. After use, wash in a dishwasher or wash with hot water and detergent, dry with a paper towel. Store covered in a clean place. • Administration sets and feed containers are for single use and must be discarded after each feeding session, maximum of 24 hours. • Ready-to-use feeds can be given for a whole administration session, up to a maximum of 24 hours. Please ensure hanging times are adhered to. • Select a system that minimises the risk of contamination, use the minimum number of connections and use giving sets with recessed spikes. 201 Procedure: • Explain the procedure to the resident. • Ensure that they have privacy when setting up the feeding regime. • Check feeding regime as per dieticians regime in the resident’s care plan • The head of the resident’s bed should be elevated at least 30 degrees while feeding in order to prevent oesophageal reflux resulting in aspiration pneumonia. Do not lay the resident flat after the feed is finished. Administration of Feeds: • Prior to preparing/setting up a feed, hands must be washed and dried thoroughly or alcohol gel may be used on visibly clean hands. Hand hygiene is the single most important procedure in the prevention and control of infection. Wear gloves if in contact with body fluids and if the resident presents a risk for infection. • Connect the feed container to the administration set using a non-touch technique. This involves ensuring that no part of the equipment, which comes into contact with the feed, be allowed to touch the hands, skin or clothing, etc. Prime the set and ensure there are no kinks. • The feed container should be clearly labelled with a grey enteral feeding tube, the date and start time of the feed. • Check the position of the fixation device daily, in relation to the markings on the tube and adjust to the correct position if necessary. This position should be confirmed before feeding is commenced to ensure that the tube has not been displaced. • Prior to commencing the feed, explain the procedure to the resident and ensure that there is a call bell within reach to enable them to call for assistance if required. • Prior to feeding check for correct placement by aspirating the gastric contents. Procedure for checking correct positioning of an enteral tube: • Wash Hands as per infection control policy on hand hygiene. • Apply non sterile gloves. • Explain procedure to the resident. • Using a sterile syringe (large tip) aspirate a small amount of fluid from the feeding port with gentle suction. • Place a drop of aspirate on pH indicator strips and check for an acidic reaction (wait for approx 10 seconds) • Match the colour change of the pH indicator strips with the colour code on the box to determine the pH of the aspirate: • A pH of 5.5 indicates correct gastric placement of tube and feeding can be recommenced as ordered • If the pH reading is 6 or above, consider repeating the test in one hour. Do not commence feeding. If the repeat test remains high, seek medical advice. Reasons for a high pH reading: • Dilution of gastric aspirate by enteral feed, wait an hour to allow the stomach to empty and pH to fall (most common reason). • Resident is receiving antacids/H2 receptor antagonists and proton pump inhibitors may have an unusually high pH. Timing of pH testing is crucial. • Tube displacement outside of the stomach. 202 During administration: • Ideally feeds should not be interrupted once they are in progress. If it is necessary to disconnect the feed use a non-touch technique, flush the tube and cap the giving set with a sterile cap or one supplied by the manufacturer with the set. Once the cap from the distal end of the giving set has been removed from the giving set, it should be stored in a clean covered container, at the resident’s bedside until required. Clean as per manufacturer’s instructions and discard the cap after 24hours. A non-touch technique should be used when reconnecting the giving set to the enteral tube. • Avoid unnecessary handling of ports or connections as this increases the risk of introducing bacteria into the system, from hands or the environment. • Document the feed and volume on the resident’s fluid intake/output chart, stating the time and date the feed was commenced. Tube Flushing: • Feeding tubes must be flushed with sterile water before and after feeding and before and after administration of each medicine. • Follow the dietician’s instructions on the feeding regimen to ensure that the resident’s calculated fluid requirements are met. Note: Sterile Water must be used during enteral feeding e.g. for flushing the tube, reconstituting powder feeds, administering medication or for hydration. Use sterile water only and discard any that may be remaining after 24 hours. Record the following information on the bottle: the date and time when the bottle was opened. Do not decant the sterile water into a non sterile container. Flushing the tube is essential to: • Reduce the risk of microbial colonisation of the surfaces of the enteral feeding tube. • Prevent blockage - the tube should be flushed before and after feeding, before and after drug administration, when more than one drug is being administered (flush with 510ml of water between each drug), if the feed is stopped / interrupted. MERCK recommend flushing the tube every four hours to reduce the risk of blockage. Equipment: • A 30ml or larger syringe should be used, as the pressure from smaller syringes may cause the tube to rupture. • 50 mls of sterile water should be used to flush each time unless the resident is on a restricted fluid intake. • Non sterile gloves . • Sterile Water. Precautions required during Feeding: • Feeds should be administrated at room temperature. • Never force any feed through the tube. • Feeding tube should be flushed with 50mls of sterile water before and after every feed. • Feed reservoirs are for single use only. Giving sets should be changed every 24hrs, with the time changed documented on the PEG observation sheet. • If PEG feeding is the sole source of nutrition it should be administrated over 20 hours with a fast period. This is to allow the gastric pH to fall and therefore reduce bacterial overgrowth and potential infection. • If the PEG is used for supplemental feeding this may take the form of overnight or bolus feeding. 203 Bolus Feeding: The resident’s nutritional needs and life style will determine their method of feeding i.e. continuous feeding or bolus feeding. Bolus feeding is delivering a bolus of feed by a syringe as a gravity feed, using a sterile 50ml syringe. Do not use the plunger of the syringe to force the feed. Raise the syringe above the resident and allow it to siphon in slowly. Repeat this process for the flushing of the tube. Some residents may prefer to use the pump to administer their bolus feed. It is important to liaise with the dietician regarding planning of an individual regime. The syringe must be discarded after single use. Document feeding regime in the daily PEG observation chart. After Feed Administration: • Giving sets should be changed every 24 hours or as per manufacturer’s instructions. • Always flush the enteral tube with sterile water at the end of a feed using a syringe. • Document the procedure in the resident’s intake/output chart and complete the PEG observation sheet • Report any adverse reactions to the doctor and consult the dietician. Replacement of a Gastrostomy Tube for residents with an already established tract by an appropriately trained and competent healthcare professional. Equipment Required: • Clinically clean trolley, Sterile Dressing Pack, Sterile Gloves 2 pairs, Alcohol Gel • Normal Saline 0.9% to cleanse stoma area • Silicone Replacement Gastrostomy Tube • Pre-filled syringe which comes in each initial pack, 5 mls for the 12, 14, 16 and 18fr balloons. Only the 20fr & some specially requested 16fr will need 20mls of sterile water • Syringe for obtaining gastric aspirate • Water Soluble Lubricating Gel • pH Indicator strips • Small black bag for waste disposal Procedure: • Explain the procedure to the resident and gain verbal consent. Allow time to answer any questions the resident/significant other(s) may have. Provide privacy. • Wash hands and wear sterile gloves adhering to National SARI Guidelines. • Using an aseptic technique, open inner cover of the dressing pack. Pour saline into the receptacle. Open the replacement kit and contents and open the syringe from its outer packaging and place it in the sterile field. • Inspect the replacement tube prior to insertion. Using a syringe inflate the balloon with 5mls of sterile water. Remove the syringe and observe the balloon for a symmetrical shape, if necessary roll the balloon gently between the thumb and the index finger to achieve a uniform shape. • Check the retention bolster to see that it slides up and down the shaft of the tube. • Close the feeding port. • Thoroughly cleanse the stoma area with normal saline 0.9%. • Remove gloves and decontaminate hands with alcohol gel. • Put on a new pair of sterile gloves. • Lubricate the tip of the replacement tube with water soluble lubricant. • Gently guide the lubricated tip of the replacement tube through the stoma, until the entire balloon has passed through the tract and into the stomach. • Hold the tube in position and inflate the balloon with the recommended amount of sterile water. 204 • • • • • • • • • • Position the balloon against the stomach by pulling the tube up and away very gently until resistance is felt. Check for the correct placement by aspirating gastric contents with a syringe and testing aspirate on pH indicator strip. Wipe away any fluid or lubricant from the tube and stoma. Inspect the stoma for gastric leakage; if there is leakage add an additional 1-2mls of water until the leakage stops. Do not exceed the maximum volume of the balloon. Remove gloves, dispose of waste and decontaminate hands. Prior to the commencement of each feed, check for correct placement by aspirating gastric contents with a syringe and testing aspirate on pH indicator strip. pH 5.5 or below confirms stomach placement . Document procedure in the resident’s narrative notes with details of the size of the tube, the amount of water in the balloon and the date and time of the procedure, and a confirmation of the correct tube placement via a pH indicator test. Schedule date for next replacement if appropriate. Adhere to An Bord Altranais guidelines on Recording Clinical Practice (2002). If a resident complains of undue pain or displays non verbal signs of discomfort, stop the procedure and refer to the Doctor immediately. Never exceed the manufacturer’s recommendations on the maximum volume of sterile water to be inserted into the balloon. Specific Considerations for residents receiving enteral feeding: All relevant baseline assessments and care plans should be reviewed as this is essential to their ongoing management. Document the following assessments on determination that enteral feeding is required and when the resident’s condition changes. Assess the resident’s: 1. Physical Care Requirements: These will incorporate: 1. The resident’s nutritional status and needs and how they should be managed. This should incorporate their nutritional status e.g. weight/BMI, nutritional requirements (as assessed by the dietician), swallowing status & recommendations: in dysphagic/aphagic residents, following assessment by a Speech and Language Therapist. The resident’s recommended nutritional intake including their oral intake (if permitted) and tube feeding regime should be recorded. The quantity, frequency and consistency of oral fluid and food allowed should be noted.These should be explained to the resident and /or their significant other(s). Record all intake and output on a Fluid Balance chart (In the first 48 hours post tube insertion, record gastric residual volumes (GRVs) aspirated and returned. Record further GRVs as ordered by the dietician on the intake/output chart). 2. Positioning: Residents requiring enteral feeding should be in a sitting position during feeding to prevent aspiration, where possible. If this is not possible a semi-recumbent position should be used. The person should be nursed at a 30° angle or more and this position should be maintained for 30 minutes following feeding. Residents who are at risk of aspiration should not have a continuous feed overnight. 3. Pain assessment and management Refer to RAP 16-Pain. 4. Communication Ability and how to best communicate with the resident, refer to RAP 1 Communication, Vision and Hearing. 205 5. Equipment needs Consider what is needed to maximise the resident’s comfort, privacy and dignity, and to facilitate the feeding regime i.e. pump type and serial number. 6. Stoma care requirements: condition of stoma and surrounding site (peri-stomal skin condition). 7. Tube details – date of insertion, make of tube, batch number, French gauge, length of external tubing visible, and the volume of water in the retention balloon, if appropriate and method of fixation. Record the date the tube is to be replaced. 8. Oral hygiene needs Refer to RAP 11: Impaired ability for Personal Care. 9. Medications prescribed; the method of administration and drug interactions require consideration. Phenytoin interaction with enteral feeds is well described. It is recommended that Phenytoin is given as a single dose where possible, and the enteral feed is stopped two hours before and restarted two hours after administration. Quinolone antibiotics are further examples of drugs that interact with enteral feeds. All medication should be reviewed by the doctor and pharmacist for possible interaction with the enteral feed. Any recommendations subsequently made should be documented and implemented. 10. Monitoring requirements for potential complications with any details concerning the resident’s clinical condition and/or any biochemical abnormalities. 2. Psychological Care Requirements: Consider the resident’s: • Quality of life: residents on enteral feeding have various factors that can impede on their quality of life. Mealtimes can be particularly difficult for residents; the smells of food/cooking, watching others eating and missing being able to eat or drink can be very distressing for the person. Time constraints in feeding can also present challenges to the resident’s normal life-style, resulting in immobility and infringements of their activities. Consideration should be given to the individual especially around the timing of meals and planned activities for the person, to ensure the resident does not feel socially excluded. Other factors include: disturbed sleep and a restricted choice of clothing. • Preferences and dislikes should be accommodated especially for residents who can tolerate and are permitted a small amount of food/fluid orally. • Dignity, Respect and Privacy Requirements: establish from the resident/significant other how the resident wishes their dignity, respect and privacy to be maintained. • Decision making ability e. g. consider the resident’s advanced care directives or wishes for withholding or withdrawing enteral feeding. Consider who can legally make these decisions if the resident cannot or has not already done so. Refer to the Regional DML Guidelines on Nutrition for further advice in this area. • Information that the resident / their loved one and carers may request e.g. what are the risks/complications associated with feeding tubes? How long is the resident expected to need this type of feeding? • Support Services that the resident/significant others may require e.g. what are the ways that caregivers can best provide emotional/ psychological comfort to the resident/their significant other(s)? Is there a need for additional resources such as counselling services? 3. Social/cultural Care Requirements: Establish what the resident’s and their significant other’s wishes are regarding tube feeding and how these can be respected e.g. Food and eating are an important part of the social and emotional life of a person. It is important to provide time and support to enable the resident to come to terms with their nutritional regime and for the nurse/carer to be sensitive around general mealtimes. It is important that where possible the resident is offered a choice of leaving the dining area at meal times. 206 Multidisciplinary Team Referrals required: Refer to the multidisciplinary team as appropriate to the resident’s assessment findings. • Dietician: for further nutritional assessment, screening, and for review of the resident’s feeding regime as appropriate e.g. in delayed gastric emptying, the volume of feed/fluid administration will need to be reviewed, and altered accordingly. • Speech and Language Therapist: for swallow reassessment and positioning advice for safe feeding. • Medical Doctor must review a resident if he/she shows signs of abdominal discomfort or distension or signs of complications as outlined earlier. • Dentist: to assess the resident’s oral health and to advise on appropriate mouth care. A dental review should be carried out at a minimum on an annual basis. • Pharmacist: to review medications prior to the commencement of enteral feeding and to supply any liquid drug preparations necessary as an alternative to oral drug medications that cannot be administered via the PEG tube. • Infection Control Team: as required for recommendations and advice on specific treatment e.g. MRSA detected at the stoma site. • Consultant Specialist Care: as required. • Counselling Services: as required. • Pastoral Care Team: as required. • Clinical Nurse Specialist: in relevant specialties e.g. wound care, stoma nurse specialist as appropriate. Record all referrals made on the MDT Referral Record and document the reason/outcome of the referral in the narrative notes. Update care plans accordingly. Personalised Care Planning: The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to address the prevention of risks and management of enteral feeding. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. Problem/Need Identification: Record the actual or potential feeding tube problem/need and its associated or related risk factors. For example; “Mary has a very poor gag reflex following her CVA and is unable to tolerate anything by mouth. A PEG tube was inserted on 07/03/2010 to address nutritional and hydration needs.” Goal Specification: Record specific, measurable, realistic, and achievable MDT goals based on the assessment findings of the resident’s needs. For example; ‘Mary will receive all her nutritional and hydration needs and medication via her PEG tube without the development of any complications.” Specific Interventions: These are the specific steps taken based on expected standards of care in addressing actual or potential problems/needs. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem/need) 207 1. Specific MDT interventions: The following should be recorded: a. Specific interventions to address the resident’s/significant(s) concerns, preferences and care choices e.g. the resident may be deeply distressed at not being able to eat or drink. Provide appropriate psychological support and assess the need for onward referral for counselling /psychological supports if necessary. b. MDT specific care instructions. This includes care instructions for addressing any risks associated with the delivery and maintenance of the resident’s feeding regime and nutritional care .e.g. Speech and Language Therapist instructions regarding positioning of the resident for safe feeding; the specific instructions form the dietician, these should be listed here or attached to the care plan. Refer the reader to the instructions. c. Oral hygiene d. Specialised equipment – Feeding solution, giving set etc. Refer the reader to the resident’s Nutritional Care Plan. e. Pain present – Refer the reader to the resident’s Pain Management Care Plan f. Advanced Care Directives/Plans 2. Monitoring and ongoing assessment: • It is essential that residents receiving PEG feeds are adequately monitored. Monitoring should place emphasis on fluid balance, biochemistry and haematology and changes in the resident’s clinical condition. • Baseline bloods should be taken i.e. FBC, U&E, Serum Proteins, Serum Magnesium, and Blood Sugars. These results should be documented and tracked in the resident’s medical notes. • It is important to check and document glucometer readings as instructed by the dietician, as the resident can develop hyperglycaemia/ hypoglycaemia. If a blood sugar reading is not within normal range it should be reported to the doctor. • The resident should be monitored closely for both the outcome of the prescribed nutritional support and for any potential side effects from the administration of a feed e.g. intestinal obstruction and delayed gastric emptying; nausea, vomiting, constipation, diarrhoea, aspiration, or side effects of medication. This should be managed accordingly under medical supervision. • The resident’s weight should be checked and documented prior to insertion of the PEG tube. The resident should be weighed weekly to monitor any weight changes associated with the tube feeding regimen. Any changes in their weight should be reported to the dietician and the outcome documented in the resident’s narrative notes.The care plan should be updated as appropriate. • Abdominal discomfort and bloating may be caused by excessive air/gas in the stomach. Venting or decompression (allowing air to escape) should be performed prior to each feed or medication administration. • The resident’s hydration status should be monitored and managed accordingly under medical supervision. Observe for signs of dehydration e.g. dry mucous membranes; sunken eyes; low/absent or concentrated urinary output; increase in urinary tract infections; constipation; confusion; lethargy; muscle cramps; hypotension, tachycardia & seizures. Record all intake and output on a fluid balance chart. • Observe for signs and symptoms of aspiration, symptoms include coughing/choking, wet/gurgly voice, alterations in breathing pattern e.g. shortness of breath, fever, acute or increasing confusion, chest pain, and respiratory arrest. Some residents who aspirate have no overt symptoms, they may just present with a low grade temperature i.e. silent aspiration. 208 • • • Monitor ongoing risk factors associated with co morbidities. Update care plan as appropriate based on monitoring findings, resident’s satisfaction and emerging identified needs. Reassess the resident’s needs if there is any change in their overall condition. 3. Communication Discuss and devise the resident’s care plan in conjunction with the resident/significant other(s) where possible and based on the resident’s wishes. Communicate the resident’s preferences and wishes to all those involved in the resident’s direct care. Ensure any monitoring concerns identified are promptly communicated to all appropriate members of the MDT and refer the resident to other healthcare professionals as needed. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers Provide education / information on the care of feeding tubes to residents, to promote self care where possible. Provide education on the plan of personalised care to the resident/significant other. All carers should receive training appropriate to their role in providing care to residents on enteral feeding. Evaluation of Care: The evaluation of the resident’s care should be based on the goals specified in their individual care plan and must be evaluated when the resident’s condition improves or deteriorates and at a minimum 3 monthly. The effectiveness of the care being provided should be evaluated by checking to see if the goals of care are being met. Please refer to the “Protocols of Care” flow chart and sample “Personalised Care Plan” in documenting care planning and in providing care. 209 210 Nursing Assessment-Document • Overall Risk Context • Past medical history • Co-morbidities • Risk factors: aspiration • Peri-stomal Skin assessment • Pain Assessment • Fluid balance Assessment • Resident’s main concerns • Resident’s goals • Resident’s preferences • Cognitive ability • Communication abilities/deficits • Resident’s cultural beliefs • Resident’s religious beliefs Further Assessments • Assess ongoing needs • Assess for signs & symptoms of complications of enteral feeding • Assess for the need of MDT referrals / assessments /management • Feeding tube care needs & ability to self care • Functional /Physical /Cognitive/Emotional Ability/ Status • Equipment needs • Preferences /Likes/Dislikes • Wound Care Requirements • Quality of Life Concerns • Dignity, Respect & Privacy Requirements On admission, if resident’s condition changes & at a minimum every 3 months Nursing Assessment 1. Identify Physical, Psychological, Social & Spiritual Care Needs 2. Devise Resident Centred care plan Need for Feeding Tube Care Plan Nursing Diagnosis 12. 13. 9. 10. 11. 6. 7. 8. 5. Reassess if condition changes. Goals unmet or Condition Changes Goals met • Resident/carer aware of appropriate preventative measures & involved in care decisions. • Resident/carers have care Plan for feeding tube care 1. 2. 3. 4. The identified problem(s) / need(s) The identified goals of care The Specific interventions required The management plan for any risks identified. The Care Plan for all identified problems and goals The MDT referrals required & made Refer reader to relevant care plans The identified appropriate specialised equipment identified/required and specialised care required Symptom management Monitoring requirements Steps to prevent the development of complications The Resident’s preferences Provide education to residents/significant others & carers in care of Residents with feeding tubes Measure outcome against specified goals Nursing Evaluation Implement an Enteral Feeding Care plan Document: Nursing Care Goals & Planning Protocol of Care for Feeding Tubes in HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: Feeding Tube Care PROBLEM / NEED IDENTIFICATION Number: Page 1 Date Signature 01/01/10 Mary has a very poor gag reflex following her CVA and is unable to toler- ate anything by mouth. GOAL SPECIFICATION Jane Murphy Mary will receive all her nutritional and hydration needs and medication via her PEG tube without the development of any complications” SPECIFIC INTERVENTIONS Date 01/01/10 Signature Identify the type of feeding tube and stoma Mary has in place and the type of feeds to be administered Gastrostomy Tube Details Name of tube: ______________________________________________________ Size of tube: ___________ G/Fr Measurement at skin: _________cm Type of tube: G-tube/PEG J-tube/PEJ Low Profile Stoma: Yes No • For stoma care refer to Wound Management Care Plan. Identify the type of feeding that Mary requires Method of feeding: Gravity-drip Pump Syringe Schedule of feeds: Continuous Intermittent • Refer to Mary’s Nutritional Care Plan for the feeding regime. • Identify the methods of gastric decompression to be used Venting / Decompression prior to each feed. • Highlight the importance of positioning for the feeding regime. Tube feeds must only be given when the Mary is sitting upright, standing, or half seated with the head raised 30° or more. Never allow Mary to lie flat during a feed, and wait for 30 minutes or longer before lying down. Medication Administration • Most of Mary’s medications can be given via her PEG feeding tube. It is recommended that: Liquid medication is used whenever possible (suspensions/elixirs). If a tablet must be crushed, it must be ordered by the doctor and local policy followed. • Mary’s main concern(s) for her feeding tube care is that she will experience discomfort and hunger and that her PEG tube will be accidentally dislodged while she is being moved. Offer Mary plenty of reassurance and explain all procedures to her. • Pain Assessment/Management. Mary’s preferred method of pain control is to take oral medication as she does not like needles. Explain to Mary that she can have her medication given to her via her PEG tube and that she will not be left in pain. Refer to Mary’s Pain Care Plan. • Dieticians Referral: Please see attached Feeding regime and recommendations from the Dietician. • Speech & Language: Pease see attached recommendations from the SLT. • Monitoring: Monitor lab results as ordered by the Doctor. • Mary’s Weight and BMI are to be monitored on a weekly basis as per the attached Dietician’s recommendations. Mary’s Blood sugars are to be monitored on a 4 hourly basis. Observe for complications such as agitation, depression, mood disorders, self-extubation (removal of the tube by the resident), infections, aspiration, misplacement of tube in trachea or lungs, pain, and tube dysfunction/malfunction, tube obstruction, tube displacement, tube leakage, over/under hydration, raised blood glucose levels, biochemical/ Electrolyte Imbalances –Overgrowth of Granulation tissue, stoma leakage. Report monitoring concerns to Mary’s doctor or other members of the MDT as appropriate. • Information sessions are to be provided to Mary & her family. Ongoing educational updates are to be provided to Mary’s Carers and significant others. Any alteration in her care needs must be communicated to all carers and significant others as per Mary’s wishes. Jane Murphy EVALUATION OF CARE (based on goals specified) Date Signature Jane Murphy 02/01/10 Mary and her family report that they are very happy that Mary’s PEG tube/wound care and feeding regime are being well managed and that she is content. They do not wish to have any changes made in her care plan at this time and will notify staff in the event that they wish any adjustments to be made to her plan of care. No complication to enteral feeding noted. Discontinued Date: …..... / ……… / 20…… Signature: ………………………………………….. 211 Bibliography: American Society for Parenteral and Enteral Nutrition (2009) Enteral Nutrition Practice Recommendations, Journal of Parenteral and Enteral Nutrition, 33, 2:122-167. An Bord Altranais (2000) Scope of Nursing and Midwifery Practice Framework, An Bord Altranais, Dublin Anderton A (1995) Reducing Bacterial Contamination in Enteral Tube Feeds British Journal of Nursing Vol 4 no 7 pp 368-375 Arrowsmith, H., (1996) Nursing Management of Residents receiving gastrostomy feeding, British Journal of Nursing 5(5) 268-273 Fieldhouse( 1995) Parental nutrition. British Journal of Nursing Vol 7 no 9 1998. Cummins, C., Marshall T., Buris, A. (1997) PEG Feeding in the Enteral nutrition of Dysphagic Stroke Professional Nurse Vol.13 No 1 NICE (2006) Nutritional Support for Adults, Oral Nutrition Support, Enteral Tube Feeding and Parental Nutrition. http://www.nice.org.uk/nicemedia/pdf/cg032fullguideline.pdf Hearing, S. (2004) Refeeding syndrome Is underdiagnosed and undertreated, but treatable. BMJ: 328(7445): 908–909. Irish Nutrition & Dietetic Institute (2002) – ‘Nutrition support Reference Guide’ Irish Nutrition & Dietetic Institute (2007) – 'Home enteral feeding resource pack' HSE SOP (2008) Management of Enteral Feeding Care in Older Persons Residential Care Centres http://hsenet.hse.ie/Hospital_Staff_Hub/mullingar/Policies,_Procedures_Guidelines_Midland_Area/Care_of_the_Older _Persons/Regional_PPG's/ROP045_Guideline_Management_of_Enteral_Feeding_Care_in_Older_Persons_Residential_ Care_Centres.pdf 212 Sample Feeding Regime To be completed by a Dietician or Medical Practitioner FORMULA PREPARATION Powder Formula Thoroughly mix ____ cups, or ____ scoops of “___________________” powder with ____ mL of water in a large, clean container. Use a standard measuring cup and follow the manufacturer’s instructions. Ready-to-Use Formula Shake the can or container well. Wipe the top of the container with a clean cloth before opening, following the directions on the label. Use a standard measuring device to measure the amount of formula required. Do not add water to ready-touse formulae. FEEDING SCHEDULE Continuous Feeding Place ________ mL of formula in the feeding container every _______ hours. Set the flow rate at: Gravity: ________ drops/minute Pump: ________ mL/hour Give the feed for ______ hours, starting at _____:_____ and finishing at _____:_____. Give ________ mL of water every _______ hours. Intermittent Feeding Number of feeds per day: __________________________________________________________________________ Time(s) of feeds: __________________________________________________________________________ For each feed, place ______ mL of formula in the feeding container. The feed should be given over _______ minutes, or _______ hours. 213 RAP 21: Palliative Care for all Definitions: Palliative Care is the care of residents with active, progressive, far advanced disease, for whom the focus of care is relief, prevention and management of symptoms while maintaining their quality of life. It is considered active Palliative Care management in accordance with the resident’s and their carers’ wishes. When death appears imminent, an end of life assessment and care plan is completed. Palliative care is described by WHO as an approach that improves the quality of life of people and their families facing problems associated with life threatening illness through the prevention and relief of suffering. This is achieved by means of early identification, impeccable assessment and treatment of pain and other symptoms that may be physical, psychosocial and spiritual. The introduction of palliative care can be appropriate early in the course of the disease and may be applicable with other therapies that are intended to prolong life. Levels of Palliative Care Services: Level one – Palliative care approach Palliative care principles should be practiced by all health care professionals. The palliative care approach should be a core skill of every clinician at hospital and community level. Many residents with progressive and advanced disease will have their care needs met comprehensively and satisfactorily without referral to specialist palliative care units or personnel. The palliative care approach aims to promote both physical and psychosocial well-being. It is a vital and integral part of all clinical practice, whatever the illness or its stage, informed by a knowledge and practice of palliative care principles. Level two – General palliative care At an intermediate level, a proportion of residents and families will benefit from the expertise of health care professionals who, although not engaged full time in palliative care, have had some additional training and experience in palliative care, perhaps to diploma level. Such intermediate level expertise may be available in hospital or community settings. Level three – Specialist palliative care Specialist palliative care (SPC) services are those services whose core activity is limited to the provision of palliative care. These services are involved in the care of residents with more complex and demanding care needs, and consequently, require a greater degree of training, staff and other resources. SPC services, because of the nature of the needs they are designed to meet, are analogous to secondary or tertiary health care services. SPC services are those services with palliative care as their core speciality and which are provided by an inter-disciplinary team, under the direction of a consultant physician in palliative medicine. SPC services are available within primary care settings, acute general hospital settings and specialist inpatient units. 214 RAI Identifiers of Potential Risks: Section O Decision to Adopt a Palliative Care Approach: Chronic diseases and terminal diseases are the common reason for adopting a palliative care approach. However, people with life-limiting, non-malignant diseases can experience a range of physical and psychological symptoms throughout the course of their disease. Their symptom burden has been shown to equal that of people dying with cancer. In addition, their disease trajectory can be more complex and often of a much longer duration. These aspects of non-malignant disease demonstrate the need for a palliative care approach to be incorporated as part of their routine care. Some life-limiting diseases that require particular consideration for palliative care include: • • • • • • • • Dementia Heart failure Advanced respiratory disease such as COPD Chronic kidney disease Scleroderma Motor neurone disease Cardio-vascular accident Multiple sclerosis Further Assessments: Palliative care responds to physical, psychological, social and spiritual needs, and extends to support in bereavement. The goal of palliative care is to allow the highest possible quality of life for both the resident and their family by identifying the resident’s needs in relation to their • • • • • Physical Needs Psychological Needs Social Needs Spiritual Needs Family Support required All relevant baseline assessments and care plans should be reviewed with a view to maintaining the resident’s comfort, dignity and choice. Document the following assessments on determination that Palliative care is required and when the resident’s condition changes Assess the resident’s 1. Physical Care Requirements – This will incorporate: a) The resident’s symptoms as identified in Section O assessment and how best they should be managed. b) Palliative Care Needs – These should be explained to the resident and /or their significant other. c) Pain Management. Refer to RAP 16: Pain. 215 d) Communication ability and how to best communicate with the resident, their significant other and carers. Refer to RAP 1: Communication, Vision and Hearing. e) Equipment needs: consider what is needed to maximise the resident’s comfort, privacy and dignity. 2. Psychological Care Requirements. These will include the resident’s: a) Preferences and dislikes. b) Dignity, Respect and Privacy Requirements. Establish from the resident/significant other how they wish their dignity, respect and privacy to be maintained. c) Decision making ability e.g. for resuscitation, advanced directives and who can legally make these decisions if the resident cannot or has not already done so. d) Information provision-that the resident, their loved one and carers may request e.g. how long the resident is expected to live? What are the signs that death is approaching? e) Support Services that the resident their loved one and carers may require e.g. ascertain the ways that caregivers can provide emotional comfort to the resident? Consider what additional resources are needed and available. Provide information about palliative care issues as appropriate to the resident’s wishes. 3. Social Care Requirements Family Issues and Interventions a) Establish with the resident and their significant other(s) what their wishes are and how these can be respected e.g. their desire for advanced care or specific aspects of advance care options. b) Conflict Resolution Ability and how to best resolve any conflicts that may arise or that already exist. 4. Cultural Beliefs/Practices – ascertain how the resident and/or their significant other would like these exercised 5. Any potential Legal implications e.g. Life support being withheld or withdrawn 6. Spiritual Care Requirements, Religious beliefs and wishes and how the resident and/or their significant other(s) would like these incorporated into their palliative care approach. Referrals required: Refer to the multidisciplinary team as appropriate to assessment findings. • • • • • • • • • 216 OT/Physiotherapist referral required for specialised equipment needs assessments to maximise functioning ability and comfort GP/Medical referral for any medical concerns Speech and Language referral to maximise communication abilities, etc Rehabilitation Services (physiotherapy / OT therapy / Social Work Services) in order to maximise physical abilities, promote independence and adapt to their condition Specialist Palliative Care Teams for symptom management Consultant Specialist Care as required Counselling Services as required Pastoral Care Team Clinical Nurse Specialist in relevant specialties • • Bereavement Counsellors Alternative/Complementary Therapists for relief of physical symptoms and psychological distress Record all referrals made on the MDT Referral Record and document the reason and outcome of the referral in the narrative notes. Update care plans accordingly. Personalised Care Planning: The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to address the cause, symptoms or risks where possible. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. Problem/Need Identification: Record the actual or potential palliative care problem and its associated or related risk factors. For example; “Mary is frightened that she will remain in pain” Goal Specification: Record: specific, measurable, realistic, and achievable MDT goals based on the resident’s assessed needs. For example; ‘Mary will be free from pain as evidenced by Mary’s self report during assessment at each interaction with Mary’. Specific Interventions: These are the specific steps taken based on expected standards of care in addressing actual or potential problems in palliative care. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem) 1. Specific MDT interventions: The following should be recorded: a. Specific interventions to address the resident’s/significant other(‘s) concerns, preferences and care choices e.g. the resident may not wish to see anyone outside of their immediate family. b. MDT specific care instructions. This includes care instructions for addressing any risks associated with the delivery and maintenance of the resident’s palliative care e.g. Palliative Care Team instructions re: symptom management. c. Specialised equipment – Syringe driver, prosthetics, etc. Refer the reader to the resident’s Manual Handling & other care plans. d. Pain present – Refer the reader to the resident’s Pain Management Care Plan. 217 e. Symptom Management. Record any intervention used to help relieve the individual’s pain, discomfort or other negative experiences that arise as either a direct or indirect result of their medical condition or the ageing process. This may include medication, physical therapy, social activities, or spiritual support. It should be an integral element of the care plan, focusing on identifying and managing the individual’s symptoms. It may concentrate on managing pain or other psychosocial or physical problems that the individual identifies as being significant to them. Person-centred symptom management assesses and responds to the individual’s needs, taking account of the wider context within which they live, their priorities, and the things that matter to them. f. Resident’s/Significant other(‘s) understanding of their illness and prognosis g. Resuscitation Status h. Advanced Care Directives/Plans/wishes i. Need for Counselling /psychological supports 2. Monitoring and ongoing assessment: • Monitor the resident’s symptoms and assess the effectiveness of the interventions implemented • Monitor the resident’s pain using a validated tool. (Refer to RAP 16: Pain) • Monitor the resident’s mental status • Monitor the resident’s overall appearance and how comfortable they appear • Monitor ongoing risk factors associated with co morbidities • Update care plan as appropriate based on monitoring findings, the resident’s satisfaction with the plan of care and on further identified needs • Reassess the resident’s needs if there is any change in their overall condition There are tools available to help audit and improve the quality of palliative care for residents in the End of Life/terminal phase. Complete an End of Life assessment and consider the use of The Liverpool Care Pathway (see template- Appendix 1). This incorporates 11 goals covering care of the dying patient, as well as the use of education and resources. 3. Communication • Discuss and devise the resident’s care plan (based on their wishes) in conjunction with the resident where possible and/or their significant other(s). Communicate the resident’s preferences and wishes to all those involved in the resident’s direct care, with the resident’s permission. • Ensure any monitoring concerns identified are promptly communicated to all appropriate members of the MDT and refer the resident to other healthcare professionals as needed with the resident’s consent (where possible). 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers • Provide education on palliative care approaches to residents/significant others/carers. • Staff members need to be educated in relation to the provision of palliative care approaches. Evaluation of Care: The evaluation of the resident’s care should be based on the goals specified in their individual care plan and must be evaluated when the resident’s condition improves or deteriorates and at a minimum 3 monthly. The effectiveness of the care being provided should be evaluated by checking to see if the goals of care are being met. Refer to the ‘Protocols of Care Flow Chart’ and Sample ‘Personalised Care Plan’ in documenting care planning and in providing care. 218 219 Overall Risk Context; Assess: Past Medical History Co-morbidities Risks Mobility Skin Assessment Pain Assessment Incontinence Assessment Resident’s main concerns Resident’s goals Resident’s preferences Cognitive ability Communication abilities/deficits Residents cultural/religious beliefs & requirements Further Assessments • Assess for signs & symptoms of palliative care needs: Functional /Physical/ Cognitive/Emotional/Spiritual • Specific MDT referrals/assessments as per identified need • Equipment Needs • Preferences /Likes/Dislikes • Personal Care Requirements • Quality of Life Concerns • Dignity, Respect & Privacy Requirements • • • • • • • • • • • • • • Document On admission, if resident’s condition changes & at a minimum every 3 months Nursing Assessment Assessment & Monitoring Reassess when there is a change in the resident’s condition No need for Pallaitive Care identified 1. Identify Physical, Psychological, Social & Spiritual Care Needs 2. Devise Resident Centred care plan Need for Pallaitive Care identified Nursing Diagnosis 9. 10. 11. 12. 13. 6. 7. 8. 5. 1. 2. 3. 4. The identified problem(s) / need(s) The identified Goals of care The Specific Interventions required The Management plan for any risks identified. The Care Plan for all identified problems and goals The MDT referrals required & made Refer reader to relevant MDT instructions The identified appropriate seating/lifting/specialised equipment required Symptom management Any advanced directive/plans The resident’s choice, preferences for care The resident’s dislikes Provide education to residents/significant others & carers in palliative care approaches Implement a Palliative Care Care plan Document: Nursing Care Goals & Planning Reassess if condition changes. Goals unmet or Condition Changes Goals met • Resident/carer aware of appropriate preventative measures & involved in care decisions. • Resident/carers have Care Plan for Palliative Care Measure outcome against specified goals Nursing Evaluation Protocol for Palliative Care Approaches in HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: Palliative Care PROBLEM / NEED IDENTIFICATION Number: Page 1 Date Signature 01/01/10 Mary is frightened that the pain she has will have continue to get worse and that she will note be able to cope Jane Murphy GOAL SPECIFICATION Mary will be free from pain as evidenced by Mary’s self-report during assessment at each interaction with Mary. SPECIFIC INTERVENTIONS Date Signature 01/01/10 • • • • • • • Mary’s main concern(s) for her palliative care is that she will remain in pain as she is aware that she will need to be repositioned at a minimum at two hourly intervals and she experiences a significant amount of back pain on movement. Please refer to Manual Handling & Pain Care Plan. Specialised equipment. Mary has poor hearing in her left ear and needs to have her hearing aid in place at all times. Please refer to her Personal Care Plan. Pain Assessment/Management. Mary’s preferred method of pain control is to take oral medication as she does not like needles. Please refer to her Pain Care Plan Incontinence Mary is incontinent of urine and needs frequent toileting/ attention. Please see Incontinence Care Plan Information sessions are to be provided to Mary & her family. Ongoing educational updates are to be provided to Mary’s Carers and significant others. Any alteration in her care needs must be communicated to all carers and significant others as is Mary’s wish. Resuscitation status: Mary is not for active resuscitation as per her own wishes. Please refer to resuscitation orders in Palliative Care assessment and ensure all care staff are aware of this decision and directive Spiritual Care Needs. Mary is a practising Roman Catholic and would like prayers said with her at night time or for her in the event that she cannot say them herself. Mary received the Sacrament of the Sick (Jan 3rd Jane Murphy 2010) EVALUATION OF CARE (based on goals specified) Date Signature Mary and her family report that they are very happy that Mary’s pain is Jane Murphy 02/01/10 being well managed and that she is pain free. They do not wish to have any changes made in her care plan at this time and will notify staff in the event that they wish any adjustments to be made to her plan of care Discontinued Date: …..... / ……… / 20…… Signature: ………………………………………….. 220 Bibliography: Department of Health and Children DOHC, Report of the National Advisory Committee on Palliative Care. 2001 Irish Hospice Foundation, A Baseline Study on the provision of Hospice/Specialist Palliative Care Services in Ireland. 2006: Dublin World Health Organisation, Palliative Care, The Solid Facts, ed. E. Davies and I. J. Higginson. 2004 The Marie Curie Palliative Care Institute Liverpool (MCPCIL) The Liverpool Care of the Dying Pathway The NICE clinical guidance on supportive and palliative care (CSG) NICE Guidance on Cancer Services Improving Supportive and Palliative Care for Adults with Cancer www.who.int/cancer/palliative/en Marie Curie Cancer Care Spiritual and Religious Care Competences for Specialist Palliative Care National End of Life Care Programme/University of Nottingham “Advance Care Planning: A guide for Health and Social Care Staff” 221 222 As required subcutaneous medication written up as per protocol (eg. pain, agitation, nausea and vomiting, emergency orders, Goal 2 Summary GP and other key people in the primary care team are aware of patient's condition Goal 11 Family/others express understanding of plan of care Goal 10 Plan of care explained and discussed with patient/family Goal 9 Family given relevant RACF, funeral and bereavement information Goal 8 Communication with primary health care team Identify how family/other are to be informed of patients impending death Communication with family/other Religious/spiritual needs assessed with patient/family Goal 7 Goal 6 Insight into condition assessed Goal 5 Religious/Spiritual Support Ability to communicate in English assessed as adequate Psychological Insight when necessary, routine turning regimens/vital signs discontinued) Discontinue inappropriate interventions (routine blood tests, antibiotics, subcutaneous fluids, not for resuscitation documented Goal 4 Goal 3 Current medications (via appropriate route) assessed, nonessentials discontinued Goal 1 respiratory tract secretions Comfort measures Goals Appendix 1: The Liverpool Care of the Dying Pathway RAP 22: End of Life Care Please note that when ‘resident/significant other’ is referred to in the course of this document, information to or from the resident’s significant other is made with the resident’s consent or when the resident cannot communicate their wishes. Definitions: End of Life Care is defined here as the care provided to a person in their final stages of life where death is imminent. It is considered to be the period of time marked by disability or disease that is progressively worse until death. Symptoms of imminent death may include an altered mental status, decreased socialisation and withdrawal, decreased need for food and fluids, increased challenges in controlling pain/increased need for analgesia, skin becomes cool to the touch, breathing becomes laboured with rattling or gurgling sounds, involuntary movements (Myoclonus), tachycardia, hypotension, etc. End of life care involves: Physical Care: effective symptom control/prevention such as: pain, discomfort, agitation, fatigue, dyspnoea, respiratory tract secretions, constipation, nausea, vomiting and/or loss of appetite, constipation, pressure ulcer prevention. Physical care further includes personal care activities and activities of living which promote the resident’s comfort, dignity and autonomy. It should also include empowering the resident by discussing and agreeing their plan of care with them and/or their significant other where the resident is no longer able to do so. Psychological Care: assessing individual needs and providing referral to appropriate supports e.g. social work services for counselling, etc. Psychological Care also includes the provision of emotional support to the resident and those who care about them; giving time to listen and understand their concerns and by expressing sympathetic presence with the resident and their family/friends. Where desired by the resident, their family and friends should be included in decisions about their care and provided with the necessary information about their individual care plan. Social Care: giving support and advice on practical matters such as getting their affairs in order or onward referral of the resident to appropriate members of the multidisciplinary team where matters fall outside of the nurses’ scope of practice. Social care also includes allowing the resident time and space to spend in private with their family and friends e.g. the provision of appropriate accommodation such as a single room where possible. Consideration should also be given to ensuring that staff understand how to communicate sensitively and appropriately with the resident and their family so that dignity, comfort and choice is always respected by staff members caring for the resident and their family. Spiritual Care: some people may have a need to explore thoughts about the meaning of life, or concerns about what happens after death. Most people are likely to have spiritual needs and some may also have practical things they need to do because of their religious beliefs. A spiritual needs assessment should be undertaken to identify individual needs. 223 RAI Identifiers: Section P End of Life Quality of Life Risk Factors: Risk factors that may negatively impact on residents’ quality of life in their end of life days may be associated with the impact/exacerbation of co-morbidities/disease progression and related symptoms on the resident’s life, and unfulfilled/unmet psycho-social needs. It should be noted that during the final stages of terminal care emphasis should not be placed on actively treating symptoms that will not improve the resident’s quality of life. The emphasis should be on comfort care. This will require focussed assessments of all the various components. Focussed Assessments: The focus of assessment is to identify the resident’s/ significant other(s) needs so that they/their loved one can be afforded a death with dignity in their place of choice with whom they wish. Their dignity should be promoted and maintained at all times. All relevant baseline assessment and care plans should be reviewed with the resident and/or their loved one with a view to maintaining the resident’s comfort, choice and dignity. Document the following assessments on determination that end of life care is required and when the resident’s condition changes. All documentation should evidence a person centred approach to care. Assess the resident’s 1. Physical care requirements: this incorporates: The resident’s symptoms and how they should be managed. a) End of Life symptoms: these should be identified through RAI Section P End of Life Assessment. Discuss symptoms identified and the resident’s/significant others wishes in managing these symptoms. Provide appropriate advice where possible or refer the resident/significant other to appropriate MDT members for advice/discussion. b) Pain management: it should be noted that 25% of people, who die; die in pain. A strong emphasis is required on pain assessment and management. Refer the reader to RAP 16: Pain. c) Communication Ability and how to best communicate with the resident, their significant other and carers. Communication may include sensitive breaking of bad news, respectful discussion about how the resident feels about dying, how the family are coping with the resident’s imminent death, etc. d) Equipment needs: consider what is needed to maximise their comfort, privacy and dignity 2. Psychological Care Requirements: these will include the resident’s: a) Wishes regarding their place of death and whom they would like to be present, as far as possible. b) Dignity, Respect and Privacy Requirements. Establish from the resident/ significant other how they wish their dignity, respect and privacy to be maintained. c) Decision making ability e.g. for resuscitation, advanced directives and who can legally make these decisions if the resident cannot or has not already done so. 224 d) Information provision-that the resident, their loved one and carers may request e.g. how long the resident is expected to live? What are the signs that death is approaching? What are the signs that the patient has died? e) Support Services that the resident their loved one and carers may require e.g. ascertain the ways that caregivers can provide emotional comfort to the resident? Consider what additional resources are needed and available. Provide information about end of life issues as appropriate to the resident’s wishes. 3. Social Care Requirements Family Issues and Interventions a) Establish with the resident and their significant other(s) what their wishes are and how these can be respected e.g. their desire for advanced care or specific aspects of advance care options. b) Conflict Resolution Ability and how to best resolve any conflicts that may arise or that already exist. 4. Cultural Beliefs/Practices and how the resident and/or their significant other would like these exercised. 5. Any potential Legal implications e.g. Life support being withheld or withdrawn. 6. Spiritual Care Requirements Religious beliefs and wishes and how the resident and/or their significant other would like these incorporated into their end of life care. Referrals required: Refer to the multidisciplinary team as appropriate to their assessment findings. • • • • • • • • • OT/Physiotherapist referral required for specialised equipment needs assessments to maximise functioning ability and comfort GP/Medical referral for any medical concerns Speech and Language therapist Referral to maximise communication abilities etc Palliative Care Teams for complex pain management beyond the scope of the team Consultant Specialist Care as required Counselling Services as required Pastoral Care Team Clinical Nurse Specialist in relevant specialties Bereavement Counsellors Record all referrals made on the MDT Referral Record and document the reason/outcome of the referral in the narrative notes. Update care plans accordingly. Personalised Care Planning: The aim of care planning is to develop a single multidisciplinary (MDT) plan of personalised care to address the cause, symptoms or risks where possible along in conjunction with the resident’s expressed wishes and preferences. The MDT includes the resident/significant other(s), carers, nurses, doctors and allied health professionals. 225 Problem/Need Identification: Record the actual or potential end of life care problem and its associated or related risk factors. For example, ‘Mary is frightened that she will die in pain’. Goal Specification: Record specific, measurable, realistic, and achievable MDT goals based on assessment of the resident’s needs. For example; ‘Mary will die comfortably and peacefully free from pain’. Specific Interventions: These are the specific steps taken based on expected standards of care in addressing actual or potential End of Life problems/needs. Document: • What we need to do (specific interventions based on residents/significant other(s) care choices where possible) • What we need to monitor (on-going reassessments) • What we need to communicate (back to the MDT) • What/who we need to educate (to improve the problem/need) 1. Specific MDT interventions: The following should be recorded: a. Specific interventions to address the resident’s/significant(s) concerns, preferences and care choices e.g. the resident may not wish to see anyone outside of their immediate family. b. MDT specific care instructions. This includes the care instructions for addressing the resident’s identified problems or needs in their end of life days, this section should make reference to: • Symptom Management. Any intervention used to help relieve the individual’s symptoms or negative psycho-social well-being should be detailed here or refer the reader to the resident’s appropriate care plan e.g. pain present - Refer the reader to the resident’s Pain Management Care Plan for the Palliative Care Team instructions regarding pain management /syringe driver etc. • Resident’s/Significant other(s) understanding of illness and prognosis. • Resuscitation status • Advanced Care Directives/Plans • Counselling /Bereavement supports/interventions 2. Monitoring and ongoing assessment: • Monitor the resident’s mental status for signs of distress, anxiety and diminishing ability to communicate verbally • Monitor the resident’s pain using a validated tool • Monitor the resident’s symptoms and manage accordingly in line with the resident’s/significant others expressed wishes • Monitor the resident’s overall appearance and how comfortable they appear • Monitor ongoing risks associated with co morbidities e.g. constipation, etc • Update care plan as appropriate based on monitoring findings and resident’s satisfaction with care and emerging identified needs • Reassess the resident’s needs if there is any change in their overall condition 226 There are tools available to help audit and improve the quality of residents’ End of Life care. The Liverpool Care Pathway template (Appendix 1) incorporates 11 goals covering care of the dying resident, as well as use of education and resources. 3. Communication Discuss and devise the resident’s care plan and their wishes sensitively in conjunction with the resident where possible and/or their significant other. Communicate the resident’s preferences and wishes to all those involved in the resident’s direct care. Ensure any monitoring concerns identified are promptly communicated to all appropriate members of the MDT and refer the resident to other healthcare professionals as needed. 4. Information/Education/Health Promotion for Resident, Significant Other(s) and Carers Provide education on diagnosis, current phase of illness, attitudes, actions, awareness and advice to residents/significant others/carers as appropriate. All carers should receive training in dealing with the dying resident and/or their significant other and in the breaking of bad news as appropriate to their role. Staff need to be educated in relation to what procedures need to be adhered to following the death of a Resident and where their individual responsibilities lie i.e. who does what? Evaluation of Care: The evaluation of the resident’s care should be based on the goals specified in their individual care plan and must be evaluated with the resident when the resident’s condition improves or deteriorates and at a minimum 3 monthly. The effectiveness of the care being provided should be evaluated by checking to see if the goals of care are being met and that this in turn is having a positive impact on the resident and their significant other. Please refer to the Protocols of Care Flow Chart and Sample Personalised Care Plan in documenting care planning and in providing care. 227 228 • Overall Risk Context • Past Medical History • Co-morbidities • Risk factors • Mobility • Skin Assessment • Pain Assessment • Resident’s main concerns • Resident’s goals • Resident’s preferences • Risk Assessments • Cognitive ability • Communication abilities/deficits • Incontinence Assessment • Residents cultural , religious needs Further Assessments & ongoing • Assess for signs & symptoms of imminent death • MDT referrals & assessments • End of Life Care Needs • Functional /Physical /Cognitive/Emotional Ability/ Status • Equipment Needs • Preferences /Likes/Dislikes & wishes • Personal Care Requirements • Quality of Life Concerns • Dignity, Respect, Choice & Privacy Requirements Nursing Assessment-Document On admission, if resident’s condition changes & at a minimum every 3 months Nursing Assessment 1. Identify Physical, Psychological, Social & Spiritual Care Needs 2. Devise personalised care plan Need for End of Life Care identified Nursing Diagnosis Implement an End of Life Care plan Document: The identified problem(s) / need(s) The identified abilities of the resident The identified resident’s goals of care The Specific Interventions required in the management/prevention of risks identified. 5. Symptom management: refer reader to relevant care plans 6. Complete Care Plans for all identified problems with goals based on the resident’s wishes, choice, comfort & preferences 7. The MDT referrals required & made 8. Advanced directive/plans 9. Monitoring interventions required 10. Communication interventions required 11. Provide education to residents/significant others & carers in care of the dying and breaking bad news as appropriate. 1. 2. 3. 4. 0 Nursing Care Goals & Planning Reassess if condition changes & update care plan accordingly. Goals unmet or Condition Changes Goals met • Resident/carer aware of interventions & are involved in care decisions. • Resident/carers have Care Plan on End of Life Care • Outcomes are evaluated based on the specified goals Measure outcome against specified goals Nursing Evaluation Protocol of Care for End of life Care in the DML, HSE Older Persons Designated Centres SAMPLE CARE PLAN Topic Heading: End of Life Care PROBLEM / NEED IDENTIFICATION Date Number: Page 1 Signature 01/01/10 Mary is frightened that she will die in pain Jane Murphy GOAL SPECIFICATION Mary will die comfortably & peacefully free from pain SPECIFIC INTERVENTIONS Date Signature 01/01/10 • • • • • • • Mary’s main concern(s) for her end of life care is that she will die in pain. Mary’s experiences a significant amount of back pain on movement. Please refer to Manual Handling & Pain Care Plan. She is also concerned about her catheter being accidentally dislodge while being moved. Please refer to continence & Manual Handling care plan Pain Assessment/Management. Mary’s current preferred method of pain control is to take oral medication as she does not like needles. Please refer to her Pain Care Plan Specialised equipment. Mary has poor hearing in her left ear and needs to have her hearing aid in place at all times. Please refer to her Personal Care, care plan Mary is at high risk of developing pressure ulcers: refer to Mary’s Pressure Ulcer Prevention care plan Information sessions are to be provided to Mary & her family by a staff member. Ongoing educational updates are to be provided to Mary’s Carers and significant others in accordance with Mary’s expressed wishes. Any alteration in her care needs must be communicated to all carers and significant others. Resuscitation status: Mary is not for active resuscitation as per her own wishes. Please refer to resuscitation orders in her medical notes and ensure all care staff are aware of this decision and directive Spiritual Care Needs Mary is a practising Roman Catholic and would like prayers said for her in the event that she cannot say them herself. She has indicated specifically which prayers she would like said. Please see Jane Murphy attached list. Mary has been anointed (Nov 3rd 2009) EVALUATION OF CARE (based on goals specified) Date 02/01/10 Time Signature Mary and her family report that they are happy that Mary’s level of pain Jane Murphy is controlled and constantly reviewed. They do not wish to have any changes made in her care plan at this time. Discontinued Date: …..... / ……… / 20…… Signature: ………………………………………….. 229 Bibliography: HIQA (2009) National Quality Standards for Residential Care Settings for Older Persons, Health Information and Quality Authority HSE NMPDU (2009) End of Life Care Guideline Department of Health (2008) End of Life Care Strategy Department of Health October (2004) The NHS Knowledge and Skills Framework (NHS KSF) and the Development Review Process The Marie Curie Palliative Care Institute Liverpool (MCPCIL) The Liverpool Care of the Dying Pathway National Institutes of Health State-of-the-Science Conference: Statement on Improving End-of-Life Care. 6-8 December 2004. 4 November 2006. The NICE clinical guidance on supportive and palliative care (CSG) NICE Guidance on Cancer Services Improving Supportive and Palliative Care for Adults with Cancer Executive Summary Common core competences and principles for health and social care workers working with adults at the end of life http://consensus.nih.gov/2004/2004EndOfLifeCareSOS024html.htm http://www.skillsforcare.org.uk/publications/publications_c.aspx www.who.int/cancer/palliative/en Marie Curie Cancer Care Spiritual and Religious Care Competences for Specialist Palliative Care National End of Life Care Programme/University of Nottingham “Advance Care Planning: A guide for Health and Social Care Staff” Institute for Health Research Lancaster University (2008) Advanced care planning in care homes for older people; A survey of current practice International observatory on end of life Care 230 231 As required subcutaneous medication written up as per protocol (e.g. pain, agitation, nausea and vomiting, emergency orders, Goal 2 Summary GP and other key people in the primary care team are aware of patient's condition Goal 11 Family/others express understanding of plan of care Goal 10 Plan of care explained and discussed with patient/family Goal 9 Family given relevant RACF, funeral and bereavement information Goal 8 Communication with primary health care team Identify how family/other are to be informed of patients impending death Communication with family/other Religious/spiritual needs assessed with patient/family Goal 7 Goal 6 Insight into condition assessed Goal 5 Religious/Spiritual Support Ability to communicate in English assessed as adequate Psychological Insight when necessary, routine turning regimens/vital signs discontinued) Discontinue inappropriate interventions (routine blood tests, antibiotics, subcutaneous fluids, not for resuscitation documented Goal 4 Goal 3 Current medications (via appropriate route) assessed, nonessentials discontinued Goal 1 respiratory tract secretions Comfort measures Goals Appendix 1: The Liverpool Care of the Dying Pathway Appendix 1 Integrated Minimum Dataset and Resident Record Chart Layout 232 Chart Layout Doc 1 DML Cover Page and Index 1 - Care Plan Instructions Doc 2 Signature Bank Doc 3 Index 2 - Guidelines for Completing Personal Details and Assessments Doc 4 Consent for Photography Doc 5 Section A: Personal Details Doc 6 Section B: Missing Persons Profile Doc 7 Section C: Initial Admission Assessment & Discharge Potential Doc 8 Section D: Communication, Mood & Behaviour Doc 9 Section E: Breathing and Circulation Doc 10 Section F: Nutrition and Hydration Doc 11 Section G: Continence and Elimination Doc 12 Section H: Mobility and Safety Doc 13 Section I: Personal Care, Controlling Body Temperature, Self Image Doc 14 Section J: Skin Condition, Pressure Ulcer Prevention and Wounds Doc 15 Section K: A Key to Me Doc 16 Section L: Personal Calendar of Important Dates Doc 17 Section M: Meaningful Activities Assessment Doc 17.1 Meaningful Activities Care Planning- Planned Activity Level Doc 17.2 Meaningful Activities Care Planning- Exploratory Activity Level Doc 17.3 Meaningful Activities Care Planning- Sensory Activity Level Doc 17.4 Meaningful Activities Care Planning- Reflex Activity Level Doc 18 Section N: Sleep and Rest Doc 19 Section O: Palliative Care Doc 20 Section P: End of Life Doc 21 Index 3 - Nursing Assessment Tools Doc 22 Vital Signs, Weights, BMI, Urinalysis Chart Doc 23 Index 4 - Guidelines on completing the: MDT Referral Record, Care Plans, Daily Flow Charts and Narrative Notes Doc 24 Multidisciplinary Referral Record Doc 25 Out Patients Appointments Doc 26 My Day, My Way Doc 27 Care Plan Template Doc 28 Daily Flow Chart of Care Doc 29 Daily Flow record of Care Doc 30 Narrative Notes Doc 31 3 Monthly Reviews Doc 32 Readmission (Respite) Form 233 Appendix 2 Resident Assessment Instruments 234 DML Integrated Minimum Data Set & Resident Care Record 2010 Affix Residents’ Photograph This Care Record belongs to:.................................................................... Medical Records Number (MRN): ...................................................... Ward/Unit:............................................................................................... Room:...................................................................................................... Bed Number: ........................................................................................... Allergies (Food [bananas, nuts, avocado, kiwi], Latex [balloons, rubber gloves, plasters, etc], Medications, Dressings: .................................... ................................................................................................................ (If a latex allergy is suspected / present complete a latex screening assessment) Private and Confidential Access allowed for the Resident, their Significant Other (as permitted by resident) and the Healthcare Team only. HSE Print (01) 626 3447 Ordering Code DML 01 Index 1 Specific Instructions for Using this Care Record 1. Writing must be legible. 2. Write in black ink. 3. Nurses must sign entries using their name as entered on the Register of Nurses and Midwives maintained by An bord Altranais (ABA, 2002). 4. Signatures must be legible. Sign your name in the Signature Bank Form. The signature bank should be updated on a 6-monthly basis. 5. Resident’s name and medical records number must be on all nursing documentation, and should be transcribed correctly. Ensure you have the correct chart / record before you begin writing. 6. Chart promptly as soon as possible after you make an observation or provide care, when details are fresh in your memory. 7. Entries must be in chronological order. 8. Use appropriate spelling and grammar. Write clear, concise, factual, non-judgmental sentences. 9. Date and time all entries. Broad times, e.g. 8am – 8pm or ‘nocte’ are not acceptable. Use the 24-hour clock as it precisely identifies the time of day. 10. Full titles/names to be given to residents and personnel on all documentation e.g. instead of writing Dr. informed, document the doctor’s name. 11. Avoid the use of abbreviations. If necessary, use hospital-authorised abbreviations as identified in the individual facility’s Abbreviation Policy. 12. Entries made in error should be bracketed and have a single line drawn through them so the original entry is still legible. Errors should be signed and dated (ABA, 2002). 13. No attempt should be made to alter the entry in error. Erasure fluid should never be used. 14. If you need to make an addition to the nursing record, date and time the entry and write ‘late entry’ beside it. Do not leave any blank spaces or spare lines in nursing records. 15. Avoid using terms or phrases that can be open to misinterpretation or that are unclear such as: some, a lot, enough, every so often, now and then, etc. 16. Avoid phrases as in ‘resident is comfortable’- instead describe his/her comfort. 17. Accepted grading systems should only be used. Urinalysis results (+++) are an example of official grading system. (ABA, 2002). Pitting oedema can be described with the 1+, 2+, 3+, 4+ following the guideline at the end of the Breathing & Circulation Assessment. Symbols like ++, , < > are not acceptable in nursing documentation. Use terms such as mild/moderate/severe, increased/decreased as appropriate. 18. Read your notes to ensure they are accurate. Read your colleague’s entries. 19. Strict adherence to the principle of confidentiality must be maintained in relation to all nursing records. 20. Any delegated recording in any document of the care record must be countersigned by a registered nurse. HSE Print (01) 626 3447 Ordering Code DML 01 Addressograph Label or complete the following Ward/Unit: ....................................................... Name: ...................................................... D.O.B.: ..................................................... MRN: ........................................................ Date Commenced: …… /…… / 20…… Page no.: ............. Signature Bank Date HSE Print (01) 626 3447 Print Name Initials Signature Witnessed by Ordering Code DML 02 Addressograph Label or complete the following Ward/Unit: ....................................................... Name: ...................................................... D.O.B.: ..................................................... MRN: ........................................................ Date Commenced: …… /…… / 20…… Page no.: ............. Signature Bank Date HSE Print (01) 626 3447 Print Name Initials Signature Witnessed by Ordering Code DML 02 Index 2 Guidelines on Completing PERSONAL DETAILS and ASSESSMENTS The Assessment Sections are broadly based on the Activities of Living Model: A. Personal Details – to be completed on or within 2 hours of admission. B. Missing Person Profile – to be completed on or within 2 hours of admission. C. Initial Admission Assessment and Discharge Potential – to be completed on or within 2 hours of admission. Important: attach a copy of the resident’s medication prescription D. Communication, Mood and Behaviour. E. Breathing and Circulation. F. Nutrition and Hydration. G. Continence and Elimination. H. Mobility and Safety. I. Personal Care / Controlling Body Temperature / Self-Image. J. Skin Condition / Pressure Ulcer Prevention and Wounds. K. A Key to Me (Personal History Profile) – complete 5 days following admission. L. Personal Calendar of Important Dates. M. Meaningful Activities – complete 5 days following admission. N. Sleep and Rest / Spiritual Needs. O. Palliative Care. P. End of Life. Guidelines on Completing the Documentation. (This documentation is completed using resident’s self-report assessment) 1. Ensure the resident’s privacy is maintained when sharing personal information. 2. Explain the nursing assessment process to the resident and their significant other. Clarify that assessments may take up to 2 hours to complete. Make arrangements with the resident and their significant others if the assessment process is to be staggered. 3. Complete Personal Details and Initial Admission Assessment on or within two hours of admission. HSE Print (01) 626 3447 Ordering Code DML 03 4. A photocopy of the resident’s medication prescription must be maintained with the Initial Admission Assessment. The Initial Admission Assessment will help prioritize assessments that need to be completed immediately and those which can be deferred to within the 7-day period. 5. Three photographs of the resident should be taken with resident’s consent on admission. These are to be attached to the Prescription Sheet, Resident’s Care Record and the Missing Person’s Profile. If a resident refuses to have their photograph taken, this needs to be documented in the narrative notes. 6. An explanation should be provided to the resident and their significant other on the necessity of undertaking specific detailed nursing examinations. For example, when undertaking an examination of the resident’s skin, pressure areas and feet; shoes, socks and clothes must be removed and the skin inspected. It is not sufficient merely to ask the resident. It is therefore vital that an explanation is provided and the resident’s dignity is maintained during examination. 7. Ensure that each part of every form is completed; do not leave any blank spaces. 8. Ensure appropriate tick box is recorded. 9. Be specific when recording information. For example, in the Nutrition and Hydration Assessment under Food Likes, be specific when recording likes / dislikes e.g. ‘likes all food but particularly likes sausage, beans and chips, etc’. Do not write statements that provide little information such as ‘likes all food’ or ‘no preferences’. 10. Be cognisant of the potential of the resident tiring during the assessment process. It may be more appropriate to complete the assessments within several short sessions. 11. The Meaningful Activities Assessment should not be completed before day 5 so that an overall assessment of the resident’s cognitive and functional ability and need may be obtained. 12. Activities of Living Assessments should be evaluated at least three-monthly using the Three-Monthly Review form or sooner if there is a change in the resident’s condition. Acknowledgements The DML Documentation Sub Group would like to acknowledge & thank the following for permission to use and / or adapt their care planning documentation: St. Mary’s Hospital (Phoenix Park), The HSE Midlands, The HSE South, NMPDU, Jackie Poole and Birr Community Nursing Unit. HSE Print (01) 626 3447 Ordering Code DML 03 Addressograph Label or complete the following Ward/Unit: ................................................... Name:................................................... Nurse’s Signature: ......................................... D.O.B.:.................................................. Date Commenced: …… /…… / 20…… MRN:..................................................... Page no.: ............. Consent for Photography I hereby confirm that I give consent for photographs to be taken for the purposes of identification in my: • Prescription Sheet • Care Record • Missing Person’s Profile • Wound Assessment/Management: Yes Yes Not applicable Yes Yes No No No No Consent given by/on behalf of the Resident (signed): ……….............…………..................… I understand that photographs of my wound have educational value. I consent to my wound photographs being used for educational purposes and to be shown to appropriate professional staff. I understand that efforts will be made to conceal my identity during educational session, but full confidentiality is not guaranteed. Yes No Not applicable Consent given by/on behalf of the Resident (signed): …………………..............................… I confirm that the purpose for which the photographs will be used has been explained to me in terms, which I have understood. Refusal to consent will in no way affect my right to medical or nursing care Consent given by/on behalf of the Resident (signed): ………............……….....…..………… Print Name: ………………………………………………………..........….................………… Date: ………………………………………………………………...........…........……......……... HSE Print (01) 626 3447 Ordering Code DML 04 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section A: PERSONAL DETAILS 1. 21. Next point of contact: Legal Name: ……………......…………….........................…..... Name: …………….......……………….....………… 2. Likes to be known as: …......………………....….. Address: …….......………………….....…….……… 3. Address: …………………......……...…..…....…… ………….......……………………………….......….. ……………......…………….........................…..... Telephone No: ….......……………...……………… 4. Telephone No: ………......…………...….....…..… Relationship: …...…………….......…...…………… 5. Religion: ……………......…..………..…….....…… Contact at night: 6. Date of Birth: …… /…… /20…..... 7. 8. Age: ………………......………..…………..........… 23. Does the resident wish to manage their own finances: Yes No Marital Status: ……………......……..……….....… 9. Occupation: ……….......…......…..……………..... 22. Ward of Court: 10. 1st Language: ………...……..…......……......…… Yes1 11. Does the resident want/need an interpreter No 12. Date of admission: …… /…… /20…...... (day/month/year) 13. Time of admission: (24 hr. clock) ......….….…..... 14. Admitted from: …………………......…......…...… 15. Type of admission: …………….........…......…….. 16. Admitted under the care of:…….......…….....….. ……………......…………….........................…..... 17. Significant other aware of admission: Yes No 18. Accompanied by: ……......…………......………… 19. Who is to be contacted first? Address: ……………......…….………….....……… ……………......…………….........................…..... Telephone No: ..………......………………........… Relationship: .……………......…………….....…… Yes Yes No No If No - record the name of the resident’s appointed financial representative: ….......……… 24. G.P: ………………………………….......….....…… Telephone No: .…………….........………...……… Address: .…….......………………………..……….. 25. Public Health Nurse: ….......……………….……… 26. Health Centre: ………….......……………...……… Telephone No: ….....…….......……...……….……. 27. Medical Card No: …….......………………….……. 28. P.P.S. No: ………….......………………………....… 29. Health Insurance: …….......………….………….… 30. How much information do you want to be told regarding your care? all none would like to have a significant other present unable to express wishes 1 when being told Name: ………………......…………….....………… Contact at night: Yes No 20. Next point of contact: 31. How much information is given to Significant other(s)? all none must be consulted each time information is unable to express wishes 1 given Name: ……………………......………………....…. 32. Name(s) of person/people permitted to Address: ...………………......………….…….….... receive information: ……...............………….. ……………......…………….........................…..... ………………………….......……………….......….. Telephone No: …......……..……………........…… 33. What is the extent of family involvement? (specify):…..………….......…........………………… Relationship: ……......…………………………...… Contact at night: HSE Print (01) 626 3447 Yes No ………….......……………………………….......….. Ordering Code DML 05 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. 34. Admitting Doctor informed of admission: Yes No Date & Time: …......…………….. 54. Resident’s Property List completed: Yes No 35. Doctor’s Name: …………..........…………..…… 55. Valuables Sent to: Administration office: 36. Health History: ............................................... Yes No Yes No ……………....…………….........................….......... 56. Home (with whom): ………....……….......…….....……… ……………....…………….........................….......... ……………....…………….........................….......... Signature: ………...………….......………………… ……………....…………….........................….......... 57. Resident informed: ……………....…………….........................….......... 58. Relatives informed: Yes No Yes No ……………....…………….........................….......... 59. MRSA: Positive19 Negative ……………....…………….........................….......... ……………....…………….........................….......... Unknown19 Date confirmed: ……… /……… /20……… N/A Yes No 37. Respite form: N/A Yes No 38. Nursing letter: N/A Yes No 39. Doctor’s letter: N/A Yes No 40. Prescription: 41. Reviewed by Psychiatry of Later Life? N/A Yes No 42. Home Situation/Support Network: Lives Alone With Spouse/ Partner With other (specify) ……….......……….……… 43. Type of accommodation: ………......……………. Yes No 44. Meals on Wheels: Yes No 45. P.H.N. visits: 60. C. Diff.: Positive Negative Unknown No4 Date confirmed: ……… /……… /20……… 61. Flu Vaccine: Yes No4 Date received: ……… /……… /20……… 62. Pneumococcal Vaccine: Yes Date received: ……… /……… /20……… 63. Communicable Diseases: ……..........………… 64. Care Plan required for Communicable Diseases: Yes No concerns for admission14: 65. Resident’s understanding of reason/ ………….......…………………………......…........ 46. Day Care: Yes No ………….......…………………………......…........ Yes No ………….......…………………………......…....... 48. Physiotherapy: 47. Occupational therapy: Yes No Assistive Devices: 49. Hearing Aid: Yes1 No Left Right Yes No 50. Spectacle(s): number of pairs ...................... 51. Dentures: upper lower 52. Walking Frame: Yes No partial Yes10 No ………….......…………………………......…........ 66. Significant other’s understanding/ concerns over admission: ……......………….. ………….......…………………………......…........ ………….......…………………………......…........ ………….......…………………………......…........ 67. Information obtained from: .……….......…...…… 68. Date: ……… /……… /20……… 69. Time :(24 hr. clock) ………………… 70. Referred to Social Worker: Yes 53. Other: .................................................................. 71. Referred to Interpreter: HSE Print (01) 626 3447 Yes No No Ordering Code DML 05 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section B: MISSING PERSON PROFILE (to be reviewed in 3 months and re-written in 6 months) Name: …………………………….......….................................. Date of Admission: ……… /……… /20…….. Known as: ……………………………...........…… D.O.B...……….. Age on Admission: .………………………….. Previous Home Address: ………………………..........……………………........................................................… ………......…………………...............……………………………………………………………………………………… Is this resident likely to attempt to leave the unit without staff knowledge? Yes No If Yes, where is the resident most likely to attempt to go: ............................................................................... ………......…………………...............……………………………………………………………………………………… What disability does this resident have that would increase their vulnerability, whilst absent from this unit e.g. hearing, sight, cognitive impairment? ...................................................................................................... Has this resident got a history of leaving the unit without staff knowledge? Is a care plan required for an unanticipated absence of this resident? Description Male Female Yes No Yes No Photograph Height: …………….................……… Weight: …………………… kg Build: ....................………………………………………………………… Hair Colour and Style: ……………..................………….....…………… Eye Colour: ..................…………………………………..............……… Outstanding features: ......…..................……………………………...... …………….................……..……………………………………………… Yes No (specify) ……………...........……………………………………........ Glasses: Yes No (specify) ……………...........……………………………………........ Hearing Aid: Yes No (specify) ……………...........……………………………………........ Mobility Aid: Communication problems: Yes No (specify) ……………...........……………………………………........ In the event that the resident is missing; complete the following: LAST KNOWN DETAILS Reported absent at: ……………………………………………...........………………...… (use the twenty-four hour clock) Last seen at: ……………………………………………………………………...............… (use the twenty-four hour clock) Clothing description: ………………………………………………....................................…………………........... ……………………………………………………………………………………...........……………………………...… Location where he/she was last seen: …………………………………………..............................………............. He/she is alert He/she is confused HSE Print (01) 626 3447 Yes Yes No No He/she is agitated He/she may be aggressive Yes Yes No No Ordering Code DML 06 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section C: INITIAL ADMISSION ASSESSMENT Must be completed on or within two hours of admission 1. BMI5,10: ….……......… Admitting Observations: BP: ..….... / …...... O2 Sat: ……….… Wt: …….….. kg Temperature: …........ Pulse: …........ Respiration: …........ Blood Sugar: ….......……........................... Urinalysis: ……………………….……........................................................................................................................ 2. 3. 4. 5. Resident introduced to the staff on duty: Yes No Resident/Significant other given the CNM’s name and contact details: Yes No Information Handbook given: Yes No The resident/significant other given a brief introduction/tour of the environment: Yes No If ‘No’ is ticked for any item(s) above, the reason must be documented in the Admission Notes Resident’s Assessments: If ‘no’ is ticked, there must be a full assessment carried out following the completion of this form 6. 7. 8. 9. 1, 14 No 5, 14 No 6, 14 No 5, 12 No 5, 12, 13, 14, 17 No 10, 12, 15, 14 No 11, 15, 14, No 11, 15, 14 No 2, 14, 17 Can verbally communicate without any difficulties ................................................. Yes No Able to eat without any difficulties ......................................................................... Yes Able to drink without any difficulties ...................................................................... Yes Weight has been stable for the past 6 months ........................................................ Yes 10. Skin has been inspected and is intact and healthy ................................................... Yes 11. Able to mobilise independently .............................................................................. Yes 12. Able to maintain hygiene independently ................................................................ Yes 13. Able to dress independently ................................................................................... Yes 14. Able to sleep without any problems ....................................................................... Yes If ‘yes’ is ticked, there must be a full assessment carried out following the completion of this form 10 No Has dietary restrictions ....................................................................................... Yes 5, 14 No Has difficulty with urinary management ............................................................. Yes 7, 10, 12, 14, 17 No Has difficulty with bowel management ............................................................... Yes 8, 9, 10, 12, 14, 17 No Has problem with breathing ............................................................................... Yes 4, 5, 14, 17 No Has behaviours that challenge ............................................................................ Yes 2, 15, 14, 17 No Has pain ............................................................................................................. Yes 16, 14, 17 No 15. Has fallen in the past year ................................................................................... Yes 16. 17. 18. 19. 20. 21. 22. Any additional issues that require immediate attention: ………………………............…………...............….. …………………………………………………………………….............……………………………………………………..........… HSE Print (01) 626 3447 Ordering Code DML 07 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. 23. Affix a copy of current medication prescription/list current medications: 24. Is the resident prescribed psychotropic drugs: Yes 10,17,18 No (Examples of psychotropic drugs include antipsychotics, antidepressants, antianxiety/hypnotics, mood stabilisers such as Haloperidol [Serenace], Olanzapine [Zeprexia], Citalopram [Cipramil], Diazepam [Valium]; Alprazolam [Xanax], Carbamazepine [Tegretol], Lithium Carbonate [Camcolit or Priadel]) 25. List 24. List non-prescribed medicinal products that the resident is currently taking: …………………………………………………………………...........…………………………………………………… …………………………………………………………………...........…………………………………………………… …………………………………………………………………...........…………………………………………………… …………………………………………………………………...........…………………………………………………… 26. Doctor informed of non-prescribed medicinal products: 27. Discharge potential: Within 1 month: Within 1-3 months: Yes No Yes No Yes No No Discharge Status uncertain-not planned: HSE Print (01) 626 3447 Yes Yes No Ordering Code DML 07 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. 1. Section D: COMMUNICATION 1, MOOD AND BEHAVIOUR 2, 3 15. Time of the day behaviour is exhibited2: Speech: Clear Incoherent1, 18 Morning Afternoon Evening Other1, 2 Previously seen by a: N/A Speech & Language Therapist Yes No If yes, please attach written instructions to care plan 2. Yes1, 2 , 3, 14, 15, 16, 17, 18 16. History of behaviours that challenge: 17. Physical: Yes No Describe (i.e. slurred, indistinct): …..........……….... 18. Verbal: …………….............………………………………..... 3. 1, 2, 3, 5, 6, 7, 8, 10, 14, 15, 16, 18: Comprehension: Any difficulty understanding what is being said No specific time Night (specify) …...................……..............………...…… No Yes No If yes, describe: ……..........……….........…………… …..………....................……………...……………… 19. What triggers behaviour: .…..….......……………… …..………....................……………...……………… …………….............………………………………..... 20. What interventions decrease behaviour: 4. needs/wants1, 2, 3, 5, 6, 7, 8, 10, 14, …..………....................……………...……………… Expression: Any difficulty expressing their 15, 16, 18: (specify) ..……........…...........…........……………… Uses communication aids: Yes1 No If yes, specify …................................................…………. …..………....................……………...……………… …………….............………………………………..... 6. Hearing: Normal Impaired1, 2, 15 left Uses hearing aid: Yes1 8. Vision: Normal Impaired1, 10, 15 Blind left Spectacles: Distance Varifocals No right both Reading None 10. Disease of the eye: Yes No If yes, specify: (Glaucoma, Cataracts, etc.) …………….............………………………………..... Confused10, 18, 2, 3 11. Cognitive / Emotional State: Alert Orientated Semi Comatosed18 Deep Coma Anxious14 Tearful14,16 Low mood 14,16, 2 Content No 1, 2, 3, 15, 16, 17, 18 12. MMSE: Score: …… /30 Date: ….../…../20….. 13. Restless: Yes 14. Agitated: Yes HSE Print (01) 626 3447 …..………....................……………...……………… If yes to any above, refer to Doctor/OT for a FULL Mental State Examination 22. Pain: Yes 2, right 7. 9. Yes If yes, specify: ….…….…......................…………… …………….............………………………………..... 5. phobias/depression: Yes2, 3, 18 21. History of delusions/hallucinations/fears or No1, 2, 3, 15, 16, 17, 18 No Unsure2, 16 Difficult to assess2, 16 3, 14, 15, 16, 17 Unable to verbalise1, 16 If yes to any above, complete a pain assessment chart 23. Resident’s / Significant Other’s concerns14 …..………....................……………...……………… …..………....................……………...……………… 24. Information obtained from: …...............…………. …..………....................……………...……………… 25. Referral required for: CNS: Audiology: Optician: SLT: Doctor: Yes No Yes No Yes Yes Yes No No No 26. Care Plan required for: Communication: Yes Behaviour that challenges: Yes No No Ordering Code DML 08 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section E: BREATHING & CIRCULATION4 1. Character of Breathing: 7. Yes4 Rhythm: .…………….........……………..…………… Yes4 Pursed Lipped Abdominal Breathing No No Quit……………… years ago Speaking Yes No Cough: Yes4 Mobilizing Yes No 8. Yes No Sleep Yes No …..…………………............……………...........…… No Frequency ...…….........……………………...……… When? …….........….....……………………………… Other: …..….............................………………… Productive cough: Yes No …..……….........………………………………………. Sputum: Amount: ….....….… Colour: ….......…… Colour: Specimen sent: Yes No Skin: …............................………………………….… Date: …. /…. /20.… Nail Bed: …........................…………………………. Ineffective Cough: Yes No Mucous Membrane: …...................………………… 9. Lower Extremities: Colour: .….........…………… Yes4, 14, 16, 17 Difficulty associated with breathing: Exertion Expiration Yes Yes Yes Yes No No Left - warm cool4, 12 cold4, 12 Temperature to touch: Right - warm cool4, 12 cold4, 12 Oedema: Yes4, 12 No, if yes: No No left No 1+ 2+ 3+ 4+ right 1+ 2+ 3+ 4+ Tracheostomy: Yes4 No Lying down 6. Expresses wish to stop smoking Yes No Changes in breathing pattern when4, 5: Inspiration 5. ………/day Support required Yes No Details: Drinking Yes No 4. Yes4 …..……….........………………………………………. Eating 3. Smokes: Never No. of years smoking ……...…….…………… Other: ..…...............……………………………… 2. Smoking History: 10. Resident’s / Significant Other’s concerns 14: Date: .…/.… /20.… …..…………………............……………...........…… If yes, requires Separate Care Plan …..…………………............……………...........…… Equipment: Nebuliser (see prescription sheet) Continuous O2 Pacemaker Humidified O2 >4 litres Yes Yes Yes Yes No No No No 11. Information obtained from: .……........…………… …..…………………............……………...........…… 12. Referral required for: Doctor: Physiotherapy: Yes No Breathing and Circulation Yes No Other, specify: .…………............………………… 13. Care Plan required for: ………...……………….........………………………… 2mm or less = 1+ Oedema Slight pitting No visible distortion Disappears rapidly HSE Print (01) 626 3447 2-4mm= 2+ Oedema Slightly deeper pit No readable detectable distortion Disappears in 10-15 seconds Yes No 4-6mm = 3+ Oedema Pit is noticeably deep May last more than 1 minute Extremity looks fuller & swollen 6-8mm = 4+ Oedema Pit very deep Last as long as 2-5 minutes Extremity is grossly distorted Ordering Code DML 09 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section F: NUTRITION 5 & HYDRATION 6 1. 2. Recent Unexplained Weight Loss: Yes2, 3, 5 , 12 No Previously seen by a: Speech & Language Therapist Yes No Dietician Yes No If yes, please attach written instructions to care plan 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. Diet: Normal Yes No Diabetic Yes No High Protein Yes No Renal Yes No Enteral feeding: Yes20 No If yes, see Care Plan Modified: Yes5, 6, 14 No specify: …........................................................…………… Other: Yes No specify: …........…....…… …........................................................…………… Fibre (must have >1500mls fluid each day) Yes No Thickened Fluids: Yes No (If yes6, 14) syrup custard set Food fortification required: Yes No Oral nutritional supplements required: Yes No Normal fluid intake: (approx.) ……….........… mls Preference of Serving Size (Food Portion Size) Small Medium Large Extra-Large Preferred Beverage: (specify) ……............….… …........................................................…………… …........................................................…………… Food Allergies: (specify) ……........……....……… …........................................................…………… Food Likes: …………………...…........…………… …........................................................…………… …........................................................…………… Food Dislikes: …………..………........…………… …........................................................…………… Level of Assistance: Independent Verbal Cues Set Up Minimal Assistance14 Total Assistance5, 6, 14 Details: ………........……....………………………… …........................................................…………… Willing to share a table with other residents at mealtimes: Yes No Where does the person like to eat? …........................................................…………… Requires position for safe swallowing: Yes No (e.g. Upright, chin tilt, etc) …........................................................…………… HSE Print (01) 626 3447 21. Any signs/symptoms of dehydration: (e.g. dry mucous membranes; sunken eyes; low/absent or concentrated urinary output; increase in urinary tract infections; constipation; confusion; lethargy; muscle cramps; hypotension & tachycardia). Yes2, 3, 5, 6, 7, 9, 12, 14, 18 No Specify: ....….…………….…………........………… …..............………………………………………....... 22. Any difficulty in swallowing: Yes4,5, 6, 14 No If yes, tick the box: Coughing/choking Throat clearing Residue in mouth Recurrent chest Holding food in mouth infection Hoarse/gurgly voice after swallowing Alterations in breathing pattern Other: (specify) ........……….…….........………… 23. Influencing Factors: None Constipation2, 9 Nausea/Vomiting2, 3, 5, 6,18 Flatulence Depression2 Diarrhoea 3, 5, 6 Heartburn Pain/Discomfort2 Anxiety2 Absent Gag Reflex Other: (specify) ……..……………………… 24. Resident’s/Significant Other’s concerns14 …..............………………………………………....... …..............………………………………………....... …..............………………………………………....... 25. Information obtained from: ...…........…......……… …..............………………………………………....... 26. Assessments completed: Oral Cavity Yes No Assistance required with Oral Care: Yes11 No Nutritional Risk Yes No 27. Referral required for: Dentist Yes No Dietician Yes No Speech & Language Yes No Doctor Yes No 28. Care Plan required for: Oral Care Plan Yes No Nutrition/Hydration Yes No PEG Care Yes No Ordering Code DML 10 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section G: CONTINENCE & ELIMINATION 7, 8 1. Influencing Factors: (i.e. mobility, bowel surgery, to urinary infections, prostatic symptoms) 8, 9 Continent: Specify: ……....……........…………………....………… …...……….................……………………………..... Crohn’s Disease, carcinoma obstetric history or prone 2. Continent Day Time: Yes No6, 7, 10, 12, 14 Occasional Incontinence: Yes No If incontinent, continence promotion programme Yes No initiated Incontinence Wear required: Yes No Conveen Usual pattern: ..……........................………………. Constipated2, 3, 7, 8, 9, 14, 18 Loose Stool8 11. Individual Reported Symptoms: Micturition: Continent Night Time: Yes No6, 7, 10, 12, 14 3. Yes No8, 10, 12, 14 10. Faecal Elimination: Incontinence pad Discomfort Flatulence Uses Laxatives (type) .……...........……………… Changes in bowel pattern No symptoms 12. Stoma: Yes 14 No Type: colostomy ileostomy ileo-conduit Appliance type: .………......….......………………… Size: .…......…...……………………………………… Size: …......………… 13. Level of Assistance required for Stoma Care: Night wear: ….……….… Size: …......………… Independent Minimal Assistance 14 Individual Reported Symptoms: Total assistance14 Day wear: .……….......… 4. Frequency Yes No Burning Yes No Discomfort Yes No Urgency Yes No Stress Retention 5. Yes No Nocturia Yes No Yes No18 Other Yes No 7. Continence Assessment required: Yes No Level of Assistance required for Toilet Use: Independent Minimal Assistance Total Assistance 8. Equipment/Aids Used: Bedpan Yes No Toilet If yes, document details in the Narrative Notes Contact details: ..……………………….......……..… Commode at bedside Catheter: Yes No Independent Minimal Assistance Total Assistance 16. Resident’s/Significant Others concerns14: …...……….................……………………………..... …...……….................……………………………..... 17. Information obtained from: …..….......……….....… …...……….................………………………………… Urinal Yes No Yes No Grab rails Yes No Raised toilet seat 9. Yes No admission: (specify) ...…..…….......……………………………… 15. Level of assistance required for hand washing How is desire to use toilet communicated: ………………........................................................... 6. 14. Instructions from Stoma Nurse prior to Yes No Yes No …...……….................……………………………..... 18. Referral required for: Continence Specialist: Doctor: Stoma Nurse: Dietician: Specify type of catheter: ...………........…....……… 19. Care Plan required for: Reason for insertion: ……...........……………...…… Continence & Elimination: Product type: ......….....….. Size: ….....……… Stoma: Date last changed: ……… /……… /20……… Catheter: HSE Print (01) 626 3447 Yes No Yes No Yes No Yes No Yes No Yes No Yes No Ordering Code DML 11 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section H: MOBILITY & SAFETY 10 1. Mobility Status: 6. Independent Falls risk: Yes10, 18 No Score………………… Requires supervision/prompts to mobilise independently 10, 14, 15 Minimal Assistance (1 person)7, 8, 9, Total Assistance7, 8, 7. Other (specify) ………………………………….. 2. 8. Safety System Required: Bed Rails: Yes No Safety Belt: Yes No ………………………………………………............. Hoist: Yes No Devices Used: Monitoring System: Yes No Crutches: Yes No Tripod: Yes No ………......………………………………….………… Cane: Yes No Zimmer frame: Yes No Other (specify):.………...………………………… If using bed rails or safety belt, complete a Risk Other (specify)…………..……………………….. Assessment and document the rationale for use in the ………………………………………………............. Narrative Notes with a review date • Visual Status: Yes1, 10 Do the following factors affect mobility: No No • Medication: Yes10, 17, 18 No • Pain: • Dizziness: Yes16 No Yes10, 17,18 No • Amputation: Yes No • Fracture: Yes No Arthritis: Yes No • Hemi paresis: Yes No 9. Risk of mobility / safety discussed with: Resident: Family/ Significant other: Left Right • Fatigues: Yes18 No Time of day: …....… 10. Resident’s / Significant Other’s concerns14: ………......………………………………….………… 11. Information obtained from: .………………..……... ………......………………………………….………… 12. Referral required for: • Appropriate footwear: Yes No10 Safety Status: OT: Impaired10, 15 Good Yes2, 3, 16 No Influencing factors affecting safety: Psychological: Nervous: Anxious: Smoker: Yes14 Yes14 Yes Yes No Document details in the Narrative Notes Doctor: Safety awareness: Yes No ………......………………………………….………… • Contracture(s): Yes No 5. Yes No Call Bell: Yes No Hip Protectors: Yes No • Aural Status: Yes1 4. Moving and Handling Risk Assessment ………………………………………………............. Grabber: Yes No Wheelchair: Yes No 3. Date: ……/… /20……… completed: 10, 12 , 14, 15 9, 10, 12, 14, 15 Falls Risk Assessment completed: Yes No No Physiotherapy: 13. Care Plan required for: Mobility & Safety Restraint Yes No Yes No Yes No Yes No Yes No No No Other (specify): .…….…………………………… HSE Print (01) 626 3447 Ordering Code DML 12 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section I: PERSONAL CARE/CONTROLLING BODY TEMPERATURE/SELF-IMAGE 11 Personal Cleansing & Dressing 13. Hair Care: Assistance required: Yes11 No 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Level of Assistance required: Independent Minimal Assistance11, 14 Total Assistance 11, 14 Associated factors: Cognitive impairment: Yes11, 14 No Hemiparesis: Yes 11, 14 No left right Amputation: Yes11, 14 No Specify ..……………………………………………… Involuntary movement: Yes11, 14 No Other (specify) …….….………………..………… Preferences for intimate care: None Female Male Preferences for: Bath Shower Bed bath History of sensitivity to hygiene products No (e.g. creams, soaps etc.) Yes13 Specify ……....……………………………………..… Personal clothes clearly labelled: Yes No Carer informed of laundry arrangements: Yes No Carer will take laundry home for washing: Yes No Controlling Body Temperature Assistance required in choosing clothing appropriate to current temperature: Yes11 No Able to communicate feeling hot or cold: Yes No 1 Likes blanket on knees while in chair: Yes No Socks (non-slip soles) preferred in bed: Yes No Eye Care Eye Care needed: Yes No Assistance required: Yes11 No Specify ……....……………………………………..… ………………........………………………………… ………………........………………………………… Ear Care Assistance required: Yes11 No Yes No Hearing Aid1: Left Right Yes No Usual cleaning schedule for de-waxing hearing aid: Specify ……....……………………………………..… ………………........………………………………… ………………........………………………………… Nail Care: Assistance required: Yes11 No ………………........………………………………… ………………........………………………………… HSE Print (01) 626 3447 Hairstyle preferred: (comment) ………….………… Would like to attend a hairdresser: Yes No Beard: Yes No Moustache: Yes No Hair removal/shaving preference: Wet shave: Yes No Electric Razor: Yes No Hair removal cream Yes No 14. Foot Care: Assistance required: Yes11 No Associated Factors: (e.g. Diabetic, PVD, Neuropathy) Specify: ….….………………………………………… Right Left Dry skin13: Yes No Yes No Cracks & fissures: Yes No Yes No Calluses/Corns: Yes No Yes No Toe nails ingrown/long: Yes No Yes No Hammer/Overlapping toes: Yes No Yes No Wounds12, 13: Yes No Yes No If wound is present, complete a wound care chart 15. 16. 17. 18. Uses preventative/protective foot wear: Yes No Specify: ….….………………………………………… ………………........………………………………… Self Image Altered body image (e.g. amputation) Yes14 No Specify: ….….………………………………………… ………………........………………………………… Preferred clothes or colours (specify) .…….……… ………………........………………………………… Resident’s/Significant other’s concerns 14 (e.g. Privacy, dignity)………………………………… ………………........………………………………… Information obtained from: …......………………… ………………........………………………………… Referral required for: Audiologist Yes No Doctor Yes No Orthotics Yes No O.T. Yes No Vascular Consult Yes No Chiropody Yes 19. Care Plan required for: Personal Care: Yes Eye/Ear Care: Yes Foot Care: Yes No No No No Ordering Code DML 13 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section J: SKIN CONDITION/ WOUNDS13 & PRESSURE ULCER PREVENTION12 1. Intact Yes No5, 13 Moist Yes No Healthy Yes No13 Dry Yes No13 Bruising Yes No Rashes Skin Condition: Scars Yes No 6. N.B. Remove all dressings on admission. A wound assessment/ management chart and a pain Yes No assessment chart must be completed on admission. Wound present: Yes5, 13, 14, 16, 17 No All residents with wounds require a dietetic referral. Yes No If yes, is this area blanchable? Yes No12 Area of redness On antibiotics for wound infection: Yes No Other skin conditions noted 13 (specify) Date commenced: ..……….………………..……… Type (specify): ..……………………………………… 12, 13, 14, 16, 17 ……….……...............……………………………… Skin not intact No. of courses of antibiotics in last 6 months …… Wound Location/s:.…………....…………………… Pressure Ulcer Risk Assessment5, 12: (complete a wound assessment/ management chart) 2. Tool used (specify) ……….....……………...………. Score: …...…… 3. ………………………...……………………………… Duration of wound: .…..…………………………… 7. Risk Level: ……...……………… Yes No Category of Pressure Ulcer: .……….....…………… If yes, please specify equipment needed for: (Use EPUAP/NPUAP (2009) Classification to Categorise Bed: ………......…………..………………….……… Chair: …….....…………...………………..………… Heels: …......……………………………………….… 8. Repositioning Assessment: Level of assistance required: Independent Independent but requires prompts 12 Minimal Assistance (1 Person)12 Total Assistance12 Frequency of repositioning required: (specify) ………………………...……………………………… 9. Information obtained from: .…............................. ………………………...……………………………… 10. Referral required for: Yes No Dietician Yes No Podiatrist Yes No Doctor Yes No Physiotherapist Yes No Bed: ……......……………………….………..……… Tissue Viability Nurse Incontinent: Yes7, 12, 13 No Occupational Therapist Vascular Consult If yes; state cleansing and barrier creams/products (Leg/Foot ulcers- unknown cause) Chair: ……......………………….…………………… 5. (malodour, pain16, etc): .…………….....…..…… ………………………...……………………………… pressure): …….....……………………………...…… 4. Resident’s / Significant Other’s concerns14 Pressure Ulcers) Resident’s equipment (e.g. static, alternating ……….……...............……………………………… Yes5, 12, 13, 14, 16, 17 No Pressure Ulcer Present: History of Previous Pressure Ulcer: Yes12 No Pressure Relieving/Redistributing Devices required: Wounds: Yes No Yes No required (Sudocrem is not recommended. CREST, 1998): 11. Care Plan required for: Pressure Ulcer Prevention/Management Yes No ……….……...............……………………………… ……….……...............……………………………… HSE Print (01) 626 3447 Wound Yes No Ordering Code DML 14 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section K: A Key to Me 14 (Adapted from the Pool Activity Level (PAL) Personal History Profile© Poole [2008]) Childhood 1 Where were you born? 2 What are your family members’ names? 3 Where did you grow up? 4 Which schools did you attend? 5 What was your favourite subject? 6 Did you have any family pets? What were their names? Adolescence & Adulthood 7 When did you leave school? 8 Any special teenage memories? 9 Did you have any special training? (e.g. college, apprenticeship) 10 What did you work at? 11 What special memories do you have of workdays? 12 Do/did you have a partner? Partner’s name/occupation? 13 Where and when did you meet? 14 Where and when did you marry? 15 What did you wear? What flowers did you have? 16 Where did you go on honeymoon? 17 Where did you live? 18 Any children- what are their names? HSE Print (01) 626 3447 Ordering Code DML 15 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Adulthood 19 Any grandchildren- what are their names? 20 Did you have any special friends? What are their names? 21 When and where did you meet? 22 Are they still in touch? 23 Did you have any pets? What were their names? Retirement 24 When did you retire? 25 What are your hobbies and interests? 26 What are the biggest changes for you? Likes and Dislikes 15 27 What do you enjoy doing now? 28 What do you like to read? 29 Do you like to celebrate your birthday? 30 What is your favourite time of year? 31 What is your favourite colour? 32 What kind of music do you like? 33 Is there anything that you definitely do not like to do? 34 Do you have any special routines to your day? 35 Do you want people to help you with anything? 36 Do you want people to leave you to do anything on your own? 37 What are you good at? 38 Is there anything else you would like to tell us about you? HSE Print (01) 626 3447 Ordering Code DML 15 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section L: PERSONAL CALENDAR OF IMPORTANT DATES Which dates are important to you e.g. birthdays, Christmas, dates that make you feel happy and sad 14 or dates that you like to celebrate January July February August March September April October May November June December HSE Print (01) 626 3447 Ordering Code DML 16 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section M: MEANINGFUL ACTIVITIES ASSESSMENT 15 Pool Activity Level (PAL) Checklist © The term meaningful activity includes Activities of Living & leisure activities that promote quality of life, self-esteem, pleasure, comfort, education, creativity & independence. Each registered nurse assessing a resident is accountable for designing, co-ordinating & implementing an individualised Meaningful Activity Programme to meet the resident’s psychological and social needs. Completing the checklist: For each activity, the statements refer to a different level of ability. Tick the statement that represents the resident’s ability in each activity. Assessment centres on 4 levels of ability & suitable meaningful activities: P= Planned, E= Exploratory, S= Sensory & R= Reflex. There should be only one tick for each activity. If in doubt about which statement to tick, choose the level of ability that represents the average performance over 5 days. Make sure you tick only on one statement for all of the activities. 1. 2. Risk Assessment for Meaningful Activities 4. Mobility Status Independent Supervised Minimal assistance Total assistance Falls Risk: Yes No Safety Awareness: Poor Intermittent Good Risk of Wandering: Yes No Mental Test Score: ..……………………..……………….. Alarm System: Yes No specify: .…….…………… On-site Activities: Yes No 1:1 assistance needed: Requires assistance as part of a group: Yes No Off-site Activities: 1:1 assistance needed: Yes No 5. Requires assistance as part of a group: Yes No Bathing/Washing • Can bathe/wash independently, sometimes with a little help to start • Needs soap put on flannel & one-step at a time directions to wash • Mainly relies on others but will wipe own face & hands if encouraged • Totally dependent & needs full assistance to wash or bathe P E S R 6. 3. Getting Dressed • Plans what to wear, selects own clothing from cupboards; dresses in correct order • Needs help to plan what to wear but recognises items & how to wear them; needs help with order of dressing • Needs help to plan and with order of dressing, but can carry out small tasks if someone directs each step • Totally dependent on someone to plan, sequence & complete dressing; may move limbs to assist HSE Print (01) 626 3447 P E S R Eating • Eats independently & appropriately using correct cutlery • Eats using a spoon &/or needs food to be cut up into small pieces P E • Only uses fingers to eat food S • Relies on others to be fed R Contact with Others • Initiates social contact & responds to needs of others • Aware of others & will seek interaction, but may be more concerned with own needs • Aware of others but waits for others to make the first contact • May not show an awareness of the presence of others, unless in direct physical contact Group Work Skills • Engages with others in a group activity, can take turns with the activity/tools • Occasionally engages with others in a group, moving in and out of the group at whim • Aware of others in the group and will work alongside others although tends to focus on own activity • Does not show awareness of others in the group unless close 1:1 attention is experienced P E S R P E S R Ordering Code DML 17 7. 8. Communication Skills • Is aware of appropriate interaction, can chat coherently and is able to use complex language skills • Body language may be inappropriate and may not always be coherent, but can use simple language skills1 • Responses to verbal interaction may be mainly through body language: comprehension is limited 1 • Can only respond to direct physical contact from others through touch, eye contact or facial expression1 P 9. E S R Practical Activities (craft, domestic chore, gardening) • Can plan to carry out an activity, hold the goal in mind and work through a familiar sequence; may need help solving problems • More interested in the making or doing than in the end result, needs prompting to remember purpose, can get distracted • Activities need to be broken down & presented one step at a time, multi-sensory stimulation can help to hold attention • Unable to “do” activities, but responds to the close contact of others & experiencing physical sensations 10. P E S R Use of Objects • Plans to use and looks for objects that are not visible: may struggle if objects are not in usual/familiar places (toiletries in a cupboard below washbasin) • Selects objects appropriately only if in view (i.e. toiletries on a shelf next to washbasin) • Randomly uses objects as chances upon them, may use inappropriately • May grip objects when placed in the hand, but will not attempt to use them P Looking at a Newspaper/Magazine • Comprehends and shows interest in the content, turns the pages and looks at headlines and pictures • Turns the pages randomly, only attending to items pointed out by others • Will hold and may feel the paper, but will not turn the pages unless directed and will not show interest in the content • May grip the paper if it is placed in the hand but may not be able to release grip or may not take hold of the paper P E S R E S R Total amount of ticks in each box below: Planned TOTAL: Exploratory11 Sensory11 Reflex11 Now, select the appropriate ‘Meaningful Activities Programme - Residents Activity level Profile’ to act as a general guide to engaging with the resident in a variety of meaningful activities. Then, complete an individualised ‘Meaningful Activities Programme’ to act as a specific guide to facilitating personal activities. HSE Print (01) 626 3447 Ordering Code DML 17 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Meaningful Activities Programme-Residents Activity Level Profile Pool Activity Level (PAL) Profile © Planned Activity Level Likely Abilities Can explore different ways of carrying out an activity. Likely Limitations May not be able to solve problems that arise. Can work towards completing a task with a tangible result. May not be able to understand complex sentences. Can look in obvious places for any equipment. May not search beyond the usual places for equipment. Method of engagement Activity objectives To enable…………………………………………… to take control of the activity and to master the steps involved. Position of tools Ensure that equipment and materials are in their usual, familiar places. Verbal directions Explain task using short sentences by avoiding using connecting phrases such as “and”, “but”, “therefore”, or “if”. Demonstrated directions Show ………………………………………… how to avoid possible errors. Working with others …………………………………… is able to make the first contact & should be encouraged to initiate social contact. Activity characteristics There is a goal or end product, with a set process, or “recipe”, to achieve it. An element of competition with others is motivating. Suitable Activities (based on knowledge of the person’s life history ‘A Key To Me’) ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ HSE Print (01) 626 3447 Ordering Code DML 17.1 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Planned Activity Level Activity: DRESSING • Encourage ......................................................... to plan what to wear and to select own clothes from the wardrobe • Encourage ......................................................... to put on their own clothes, be available to assist if required • Point out labels on clothing to help orientate the back from the front • Encourage ......................................................... to attend to grooming such as brushing hair, putting on make-up, cleaning shoes Activity: BATHING • Encourage ......................................................... to plan when they will have the bath, to draw the water and select toiletries from the usual cupboard or shelf. Ensure a slip resistant bath mat is in the bath and on the floor • Encourage ......................................................... to wash their own body, be available to assist if required • Encourage ......................................................... to release the water afterwards, and to wipe the bath Activity: DINING • Encourage ......................................................... to select when and what they wish to eat • Encourage ......................................................... to prepare the dining table and to select the cutlery, crockery and condiments from the usual cupboards or drawers • Encourage ......................................................... to clear away afterwards Note: Consideration of National Infection Control Guidelines and HSE Health & Safety Guidelines is required in undertaking the above. HSE Print (01) 626 3447 Ordering Code DML 17.1 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Meaningful Activities Programme-Residents Activity Level Profile Pool Activity Level (PAL) Profile © Exploratory Activity Level Likely Abilities Can carry out very familiar tasks in familiar surroundings. Likely Limitations May not have an end result in mind when starts a task. Enjoys the experience of doing a task more than the end result. May not recognise when the task is completed. Can carry out more complex tasks if they are broken down into 2-3 step stages. Relies on cues such as diaries, newspapers, lists and labels. Method of engagement Activity objectives To enable…………………………………………… to experience the sensation of doing the activity rather than focusing on the end result. Position of tools Ensure that equipment and materials are in the line of vision. Verbal directions Explain task using short simple sentences. Avoid using connecting phrases such as “and”, “but”, or “therefore”. Demonstrated directions Break the activity into 2-3 steps at a time. Working with others Others must approach …………………………………… and make the first contact. Activity characteristics There is no pressure to perform to a set of rules, or to achieve an end result. There is an element of creativity and spontaneity. Suitable Activities (based on knowledge of the person’s life history ‘A Key To Me’) ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ HSE Print (01) 626 3447 Ordering Code DML 17.2 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Exploratory Activity Level Activity: DRESSING • Encourage discussion about the clothing to be worn for the day: is it suitable for the weather or the occasion, is it a favourite item. • Spend time colour matching items of clothing and select accessories. • Break down the task into manageable chunks: help lay the clothes out in order so that underclothing is at the top of the pile. If the person wishes to be helped, talk ......................................................... through the task: “put on your underclothes” “now put on your dress and cardigan”. • Encourage ......................................................... to check (his/her) appearance in the mirror. Activity: BATHING • Ensure a slip resistant bath mat is in the bath and on the floor. • Break down the task into manageable chunks: suggest that ......................................................... fills the bath, then when that is accomplished suggest that he or she gathers together items such as soap substitute (e.g. Silcock base®), shampoo, flannel, and towels. • When ......................................................... is in the bath, suggest that (he/she) washes and rinses (his/her) upper body, and when that is accomplished, then suggest that (he/she) washes and rinses (his/her) lower body. • Ensure that bathing items are on view and that containers are clearly labelled. • Have attractive objects around the bath such as unusual bath oil bottles or shells and encourage discussion and exploration of them. Activity: DINING • Store cutlery and crockery in view and encourage ......................................................... to select own tools for dining. • Offer food using simple choices. • Create a social atmosphere using table decorations, music, and promote conversation. Note: Consideration of National Infection Control Guidelines and HSE Health & Safety Guidelines is required in undertaking the above. HSE Print (01) 626 3447 Ordering Code DML 17.2 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Meaningful Activities Programme-Residents Activity Level Profile Pool Activity Level (PAL) Profile © Sensory Activity Level Likely Abilities Is likely to be responding to bodily sensations. Can be guided to carry out single step tasks. Can carry out more complex tasks if they are broken down into one step at a time. Likely Limitations May not have any conscious plan to carry out a movement to achieve a particular end result. May be relying on others to make social contact. Relies on cues such as diaries, newspapers, lists and labels. Method of engagement Activity objectives To enable…………………………………………… to experience the effect of the activity on the senses. Position of tools Ensure that ……………………………… becomes aware of equipment and materials by making bodily contact. Verbal directions Limit requests to carry out actions to the naming of actions and objects e.g. “lift your arm”, “hold the brush”. Demonstrated directions Show ………………………………………… the action on the object. Break the activity down into 1 step at a time. Working with others Others must approach…………………………………… and make the first contact. Use touch and …………………’s name to sustain social contact. Activity characteristics The activity is used as an opportunity for a sensory experience. This may be multi-sensory and repetitive. Suitable Activities (based on knowledge of the person’s life history ‘A Key To Me’) ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ HSE Print (01) 626 3447 Ordering Code DML 17.3 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Sensory Activity Level Activity: DRESSING • Offer a simple choice of clothing to be worn. • Spend a few moments enjoying the sensations of the clothing: feeling the fabric, rubbing the person’s finger up and down a zip fastener, or smelling the clean laundry. • Break down the task into one step at a time: “put on your vest” “now put on your pants” “now put on your stockings” “now put on your dress”. Activity: BATHING • Prepare the bathroom and run the bath water for ......................................................... • Make the bathroom warm and inviting - play music, use scented oils, have candles lit on a safely out of reach shelf. Ensure a slip resistant bath mat is in the bath and on the floor. • Break down the task into one step at a time and give ......................................................... simple directions: “rub the soap substitute (e.g. Silcocks Base®) on the cloth, rub your arm, rinse your arm, rub your chest, rinse your chest......”. Activity: DINING • Serve food so that it presents a variety of colours, tastes and textures. • Offer ......................................................... finger foods, encourage (him/her) to feel the food. • Offer ......................................................... a spoon, place it in (his/her hand) and direct (him/her) to “scoop the potato” “lift your arm” open your mouth”. Note: Consideration of National Infection Control Guidelines and HSE Health & Safety Guidelines is required in undertaking the above. HSE Print (01) 626 3447 Ordering Code DML 17.3 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Meaningful Activities Programme-Residents Activity Level Profile Pool Activity Level (PAL) Profile © Reflex Activity Level Likely Abilities Can make reflex responses to direct sensory stimulation. Can increase awareness of self, and others, by engagement of senses. May respond to social engagement through the use of body language. Likely Limitations May be in a subliminal or subconscious state. May have difficulty organising the multiple sensations that are being experienced. May become agitated in an environment that is over stimulating. Method of engagement Activity objectives To arouse…………………………………………… to a conscious awareness of self. Position of tools Stimulate area of the body being targeted e.g. stroke …………….........................…………’s arm before placing it in a sleeve Verbal directions Limit spoken directions to movement directions i.e. “Lift”, “Hold”, “Open”. Demonstrated directions Show ………………………………………… the action on the object. Break the activity down into 1 step at a time. Working with others Maintain eye contact, make maximum use of facial expressions, gestures and body posture for non-verbal conversation. Use social actions which can be imitated e.g. smiling, waving, shaking hands. Activity characteristics The activity is in response to direct selective sensory stimulation. Suitable Activities (based on knowledge of the person’s life history ‘A Key To Me’) ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ ........................................................................................................................................................................................ HSE Print (01) 626 3447 Ordering Code DML 17.4 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Reflex Activity Level Activity: DRESSING • Prepare the clothing for ........................................................., ensure the dressing area is private and that a chair or bed at the right height is available for sitting. • Talk through each stage of the activity as you put the clothing onto ......................................................... Use a calm tone, speak slowly and smile to indicate that you are non threatening. • Stimulate a response in the limb being dressed by using firm but gentle stroking. Ask ......................................................... to assist you when necessary by using one word requests: “lift” “stand” “sit”. • At the end of dressing, spend some time brushing ......................................................... hair using firm massaging brush strokes. Activity: BATHING • Prepare the bathroom and run the bath water for ........................................................., put in scented bath products (lavender will aid relaxation). • Ensure that the bathroom is warm and inviting, and feels secure by closing the door and curtains and providing a slip resistant bath mat in the bath and on the floor. Clear away any unnecessary items which may be confusing. • Use firm, massaging movements when washing and rinsing ......................................................... Wrap (him/her) securely in a towel when (he/she) is out of the bath. Activity: DINING • Use touch on ......................................................... forearm to make contact, maintain eye contact, and smile to indicate the pleasure of the activity. • Place a spoon in ......................................................... hand. Close your hand over ......................................................... and raise the spoon with food on it to (his/her) mouth. • As the food reaches ......................................................... mouth say “open” and open your own mouth to demonstrate. Touch ......................................................... lips gently with the spoon. Note: Consideration of National Infection Control Guidelines and HSE Health & Safety Guidelines is required in undertaking the above. HSE Print (01) 626 3447 Ordering Code DML 17.4 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section N: SLEEP AND REST17 SLEEP and REST 1. Usual Sleep Environment Type of bed: ……………….…….…..……………… Type of bedding: …………….……………………… Sleep attire preferred: ………………………….…… Shared bedroom Sleeps alone Shared bed Light on Light off Door opened Door closed Quiet Noise (type) .…..…… ……………………………………………........……… 2. Temperature preference: Warm Cool Other ………...…………………………………… 3. Preferred time to get up: …………………………… 4. Preferred bed time: ………………….……………… 5. Pre-Sleep Routine: (describe) .…….………………… ……………………………………………........……… ……………………………………………........……… 6. Hours of sleep per night: …………………………… 7. Do you need assistance to get into bed? Yes No If yes, specify: ………......…………….……………… ……………………………………………........……… ……………………………………………........……… 8. Resident’s Perception of Own Night-time Sleep2, 3, 17: (tick as appropriate) Good Mood on waking Difficulty going to sleep Refreshed on waking Restless Disturbed sleep Early morning wakening Requires medication Other (specify) .….………………………….…… ……………………………………………........……… SPIRITUAL NEEDS SPIRITUAL NEEDS 11. Religion: .…………………..………………………… Yes No 12. Wish to partake in services: 13. Informed of services available: Yes No 14. Do you need assistance to access services? Yes No If yes, specify: .………..……………………………… * If resident is unable to communicate wishes, ask significant other* 15. Any specific spiritual beliefs, requirements, or daily practices (dress, diet, place to meditate, daily prayers, etc): ............................................................................... ............................................................................... ............................................................................... 16. Name of Spiritual Advisor:.………………………… Contact details/ number: ....…............…………… ............................................................................... ............................................................................... ............................................................................... 17. If Roman Catholic, has the resident received the Sacrament of the Sick: Yes No 18. Resident’s /Significant Other’s concerns14 .…… ............................................................................... Date received: ……… /……… /20……… ............................................................................... ............................................................................... ............................................................................... ............................................................................... 19. Information obtained from:.…….....……………… Note: Early morning wakening, difficulty going to ............................................................................... sleep, tired/low mood on waking - assess for ............................................................................... Depression using a validated tool e.g. HADS 20. Referral required for: Disturbed sleep pattern: Doctor (Sleep and Rest) Yes2, 3, 10, 14, 17, 18 No Spiritual Advisor: Associated factors: 21. Care Plan required for: None Anxiety Depression18 Sleep and Rest Apprehension Boredom Pain16 Spiritual Needs Confusion Snoring Sleep Apnoea Muscle cramps Lack of activity Other (specify) ………………...………………… 10. Daytime Rest: (no longer than 2hours) Yes No 9. Yes No Yes No Yes No Yes No Time: ..…………….....……………………….……… HSE Print (01) 626 3447 Ordering Code DML 18 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section O: PALLIATIVE CARE 21 Palliative Care is the care of residents with active, progressive, far advanced disease, for whom the focus of care is relief, prevention and management of symptoms while maintaining quality of life. It is considered active Palliative Care management in accordance with the resident’s and their carers’ wishes. When death appears imminent, an end of life assessment and care plan is completed. However residents’ wishes regarding their end of life days should be completed as appropriate to the individual. 1. 2. Decision to move to a palliative the following there must be an Assessment and Plan of By: .…..……….....…………………………….. Care to alleviate the symptom) ..……….....…..................................……… Reddened Pressure Areas/Wound Date: ……… /……… /20……… Dry / sore mouth This decision was discussed with: Dehydration Significant Other MDT Date: …../..… /20..… Nausea / vomiting Date: …../..… /20….. Weight loss / Anorexia Date: ..… /..…/20..… Constipation Drowsiness Awareness of Prognosis: Yes No Resident : Significant other : 4. Fatigue Insomnia Yes No MDT at Case Conference : Yes No For CPR : For blood tests / procedures: On-Site Off-Site Yes No Yes No 10. Antibiotic therapy : I.V. Yes No Oral Artificial Nutrition: Artificial Hydration: Yes No Yes No Level of Consciousness: Alert 7. 8. 9. Yes No Orientated Confused Semi-Comatose 11. Deep Coma 12. HSE Print (01) 626 3447 Yes12, 13 No Yes5 No Yes5 No Yes6 Yes5 Yes6, 9 Yes Yes4 Yes Dyspnoea/Cough/Noisy breathing Yes4 Depression / low mood / anxiety Yes The following issues were discussed with the Resident /Significant Other & 5. Frequent Palliative Care Symptoms21: (If yes to any of approach to care was taken: Resident 3. 6. No No No No No No No No Pain: Yes16 No • Syringe pump: Yes No Break through pain /comfort/palliative medications prescribed: Yes No Current medications reviewed by MDT: Yes No Psychosocial care: • Resident’s concerns14: Narrative Note pg…… • Significant Other’s Concerns: Narrative Note pg…… Resident’s wishes: • Visit by Priest/Religious person Yes No • Visit by Solicitor/Legal Advisor Yes No • To be Alone Yes No • Family involvement in decisions: Narrative Note pg…. • Place of Death: Narrative Note pg …. • Funeral Arrangements: Narrative Note pg…. Referral required for: Specialist palliative care service Yes No MDT Yes No Counselling Services Yes No Religious Advisor Yes No Chaplaincy Team Yes No Care Plan commenced: ……… /……… /20……… Ordering Code DML 19 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... Nurse’s Signature: .............................................. D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. Section P: END OF LIFE ASSESSMENT 22 1. Resident aware of his/her condition: Yes No 2. Emotional status: Client expresses – Fear Anxiety Anger Depressed Resident’s wish: Alone Friends Others With Family Unable to express Cafeteria/Kitchen/Refreshment facility Bereavement Counselling Resident’s preferred Religious, Spiritual and Religious symbols and rituals e.g. altar, candle, Bible Anointing / Sacrament of the Sick 11. Person to contact in the event of the resident’s condition changes: …………………………………………………. Visit by Priest / Religious Advisor …………………………………………………. Frequent Palliative Care Symptoms: (If yes to any …………………………………………………. of the following, there must be a plan of care to alleviate …………………………………………………. the symptoms) • Pain: Yes16 No • Syringe driver: Yes No • Dry/Sore Mouth: Yes5 No • Reddened Pressure Areas/Wound: Yes12,13 No • Dehydration: • Nausea and Vomiting: • Constipation: • Weight Loss/Anorexia: • Insomnia: • Fatigue: Yes6 No Yes5 No Yes9 No Yes5 No Yes No Yes4 No Yes No • Dyspnoea/Cough/Noisy Breathing: Yes4 No • Depression/Low Mood/Anxiety: Resident’s wish regarding their place of death: Wish to go to home Single Room No preference 7. Information obtained from: .………………... Family room Cultural practices: 6. 9. No 10. Significant other aware of: ......…………......………………………………………… 5. Yes …………………………………………………. Specific wishes: .……………………………..…………… 4. Significant other aware of resident’s condition: Acceptance Other: .……..………………………………………… 3. 8. 12. Resident’s concerns14: …………………………………………………. …………………………………………………. …………………………………………………. …………………………………………………. …………………………………………………. …………………………………………………. …………………………………………………. …………………………………………………. …………………………………………………. 13. Significant other’s concerns: …………………………………………………. …………………………………………………. …………………………………………………. Resident’s wish regarding care after death: …………………………………………………. Personal Dress: ………………...………………………… …………………………………………………. …………….……………………………………………… …………………………………………………. Jewellery: ………………………………………………… …………….……………………………………………… Wish to go to home Wish to remain in church over night HSE Print (01) 626 3447 Ordering Code DML 20 Index 3 Nursing Assessment Tools On admission the following assessments must be recorded for all residents: • A pressure ulcer risk assessment with the score documented. • A nutritional risk assessment using a validated screening tool with a BMI recorded. • An oral cavity assessment • A falls risk assessment • A manual handling assessment • Vital Signs, Weights, BMI, Blood Sugar & Urinalysis Additional assessments which may need to be carried out include: (This list is not intended to be exhaustive) • Pain Assessment • Dependency Scale • Assessment for the use of restraint • Wound Assessment and Management chart • Behavioural and Mental State Checklist • Dementia Care mapping • Bed rails Assessment • Continence Assessment HSE Print (01) 626 3447 Ordering Code DML 21 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... D.O.B.:....................................................... Page no.: ............. MRN: ......................................................... Vital Signs, Weights, BMI, Blood Sugar and Urinalysis DATE/TIME TEMP PULSE HSE Print (01) 626 3447 RESP. B.P. WEIGHT BMI BLOOD URINALYSIS SUGAR NURSE SIGNATURE Ordering Code DML 22 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... D.O.B.:....................................................... Page no.: ............. MRN: ......................................................... Vital Signs, Weights, BMI, Blood Sugar and Urinalysis DATE/TIME TEMP PULSE HSE Print (01) 626 3447 RESP. B.P. WEIGHT BMI BLOOD URINALYSIS SUGAR NURSE SIGNATURE Ordering Code DML 22 Index 4 Guidelines on completing: the Multidisciplinary Referral Record, ‘My Day, My Way’, ‘A key to Me’, a resident’s ‘Personal Calendar of Important Dates’, Care Plans, Daily Flow Charts and Narrative Notes Multidisciplinary Referral Record • All referrals to the Multidisciplinary Team (MDT) must be recorded on the Multidisciplinary Referral Record • The Multidisciplinary Referral record should be updated each time an MDT referral is made and a narrative note written. The accompanying narrative note should accurately record the time, date, method/mode of referral and the reason for the referral • All significant observations on a resident's condition that are made to members of the MDT by nursing staff must be recorded in the nursing Narrative Notes • Care plans should be updated to reflect the MDT decisions ‘My Day, My Way’, ‘A key to Me’ and a ‘Personal Calendar of Important Dates’ The importance of getting to know the resident as a unique person is the cornerstone to providing personalised care. ‘My Day My Way’, ‘A key to Me’ and the resident’s ‘Personal calendar of important dates’ were developed to help staff get to know the resident as an individual. These ‘getting to know the resident’ exercises can be carried out before a resident is admitted to the unit, when they are admitted as part of their admission procedure or now as part of their ongoing assessment. • My Day, My Way can be completed with the resident, by a family member, care staff or named nurse • It is important to note that the document ‘A Key to Me’ is not designed to be used in an interview format but to be completed by all staff as they interact with the resident through the activities of daily living, i.e. washing, dressing, chatting, etc. Staff may find it useful to fill in the form as they learn the information through chatting with the individual, their family and their visitors • These living documents should be kept in the resident’s care plan which is accessible to the resident and all staff • They should be updated as part of the ongoing evaluation of the residents care and life choices • All new staff should familiarise themselves with these documents Care Plans Care plans must be discussed, agreed and drawn up with the involvement of the Resident or their Significant Other and recorded under the following headings • Problem identification - Any residents needs or problems identified are recorded in this section • Goal specification - The goals or aims of care are recorded. Goals must be realistic, obtainable and measurable, for successful evaluation of care HSE Print (01) 626 3447 Ordering Code DML 23 • Specific Interventions - The interventions recorded should provide sufficient information to provide appropriate care • Evaluations of Care are based on measurable outcome criteria as outlined in the Goal specification. Evaluation must be documented on the flow chart as a NN (Narrative Note) and a narrative note must be written. All care plans must be evaluated at least three monthly using the Three Monthly Care Plan Review form or sooner if the residents condition indicates, using the Evaluation Section on the Care Plan Template. All Care plans are to be re-written six monthly irrespective of change to the resident’s condition Note: If the resident or their significant other is unable or unwilling to participate in care planning, a narrative note must be recorded. Daily Flow Records of Care Daily flow records of care are recorded: • During the morning (M), evening (E) and night (N). Times; M= 08.00-12.00, E= 12.01=20.00 N=20.01-07.59 • Accurately record the appropriate code as outlined on the Daily Flow Chart of Care Narrative Notes Narrative notes should be accurately recorded and updated: • Following Daily Assessment if any changes occur • When significant observations on a resident's condition are made • When referrals are made to the multidisciplinary team. The reason for the referral requested should be recorded • MDT reviews/ case reviews or family meetings should be recorded • When care changes due to new medical treatments/requirements e.g. when IV or Subcutaneous fluids or enteral feeding are commenced • When PRN medication is administered and the reason for/outcome of the PRN medication administration • When the resident’s condition improves or deteriorates • When problems/needs identified, are resolved • Following evaluation of the specific resident’s need/psycho-social wellbeing • Following evaluation, updating or changes to care plans • Refer to Index 1 for further instructions on recording the Narrative Notes Note: Where HCA’s are filling in documentation as part of nurse/HCA delegation of tasks e.g. recording Food/Fluid charts, Flow Charts of Care, etc, it is recommended that the HSE National Guidelines on Delegation are followed and that nurses co-sign the documents. HSE Print (01) 626 3447 Ordering Code DML 23 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... D.O.B.:....................................................... Page no.: ............. MRN: ......................................................... MULTIDISCIPLINARY REFERRAL RECORD REFERRAL DATE REFERRED TO HSE Print (01) 626 3447 REFERRED BY Page number of Narrative Notes where the reason for the referral must be documented REVIEW DATE REVIEWED BY Ordering Code DML 24 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... D.O.B.:....................................................... Page no.: ............. MRN: ......................................................... MULTIDISCIPLINARY REFERRAL RECORD REFERRAL DATE REFERRED TO HSE Print (01) 626 3447 REFERRED BY Page number of Narrative Notes where the reason for the referral must be documented REVIEW DATE REVIEWED BY Ordering Code DML 24 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... D.O.B.:....................................................... Page no.: ............. MRN: ......................................................... Out Patients Appointments DATE APPOINTMENT TYPE DATE OF E.g. Wound, Vascular, Cardiac, Orthopaedic APPOINTMENT HSE Print (01) 626 3447 CONSULTANT/ NURSE LOCATION SIGNATURE Ordering Code DML 25 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... D.O.B.:....................................................... Page no.: ............. MRN: ......................................................... Out Patients Appointments DATE APPOINTMENT TYPE DATE OF E.g. Wound, Vascular, Cardiac, Orthopaedic APPOINTMENT HSE Print (01) 626 3447 CONSULTANT/ NURSE LOCATION SIGNATURE Ordering Code DML 25 Addressograph Label or complete the following Ward/Unit: ......................................................... Name:........................................................ Nurse’s Signature: ............................................... D.O.B.:....................................................... Date: ……… /……… / 20……… MRN: ......................................................... Page no.: ............. My Day, My Way 14 I would like to share with you what is important to me when caring for me What makes me happy? What makes me unhappy? HSE Print (01) 626 3447 Ordering Code DML 26 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... D.O.B.:....................................................... Page no.: ............. MRN: ......................................................... CARE PLAN (to be reviewed in 3 months and re-written in 6 months) Topic Heading …………………………………………………………… This Care Plan has been discussed, agreed and drawn up with the involvement of the Resident or their Significant Other: Yes No Signed…………………………………… (Resident/Significant Other) (If the resident/significant other is unable or unwilling to participate a narrative note must be recorded) PROBLEM / NEED IDENTIFICATION Date Number: .................... Signature GOAL SPECIFICATION SPECIFIC INTERVENTIONS Date HSE Print (01) 626 3447 Signature Ordering Code DML 27 Addressograph Label or complete the following Ward/Unit: ........................................................ Name: ....................................................... D.O.B.:....................................................... Page no.: ............. MRN: ......................................................... SPECIFIC INTERVENTIONS (Continued) Date Signature EVALUATION OF CARE (based on goals specified) Date Signature Discontinued Date: …..... / ……… / 20…… Signature: ………………………………………….. HSE Print (01) 626 3447 Ordering Code DML 27 HSE Print (01) 626 3447 Ordering Code DML 28 1. 2. Pain Continence & Elimination Snacks given Fluids given 8. 9. 1. 2. 3. 0. Bowels not opened. (If the resident is independent, the nurse must ask the resident) 6. Stoma care given 4. 5. Bristol Stool Chart in 7. Bed rails in place brackets & add sm., med., or and checked as lg per care plan Safety 6. Monitoring systems in place & checked as per care plan 5. Mobilising as per care plan 4. Total Assistance required, interventions implemented as per manual handling care plan 3. Minimal Assistance 2. Mobilising with Supervision / prompts / aids Mobility 1. Independent Mobility & Safety 6. Activities & Location 7. 1. Self-caring a) Shover b) Bath c) Wash d) Shave 8. 1. Pressure Areas On-site intact & 1. Meaningful healthy activities as per care plan 2. Pressure ulcer 2. In bed present, care 3. Bedside 2. Asisted care implemented 4. Dayroom a)Wash as per care 5. Therapy b)Shover plan 6. Bingo c)Bath 3. Pressure 7. Cooking d)Bed Bath ulcer/wound 8. Music therapy e)Shave present 9. Sing along 3. Refused personal (wound chart 10. Out door care-record in recorded) activities narrative note 11. Exercise 4. Wound care session Care Attended: carried out as 12. T.V. 4. Oral Hygiene: per wound 13. Reading a) Independent chart 14. Butterfly b) Assisted 5. Repositioned Moments see (see chart) 5. Perineum care repositioning 15. Others chart 6. Eye Care (record NN) 6. Heels offloaded Off-site 7. Ear Care as specified in 8. Finger Nail Care 11. Trips/Tours care plan 12. Special event 9. Toe nail Care 13. Out with 10. Foot Care significant other for part 11. Hair Care of the day 12. Skin Care Skin Condition/ Pressure Ulcer Prevention & Wounds If the colour of the urine is 5 or greater for more than two days, commence Fluid Monitor Chart 12. Refused meal/feed 11. Refused fluids 10. Nil by mouth Supper record (%) taken Food fortification provided Urinary Elimination 1. Incontinent of urine. Insert corresponding number in brackets to urine colour & Dietary record daily to assess for modification dehydration & add sm., provided as per med., or lg dietician’s/SLT 2. Continence promotion orders attended to as per care plan Enteral feeding instructions Recorded on 3. Continent of urine Fluid Insert corresponding number Monitoring in brackets to urine colour & Chart record daily to assess for Breakfast record dehydration (%) taken 4. Catheter care given. Insert Lunch/Dinner corresponding number in record (%) brackets to urine colour & taken record daily to assess for dehydration Tea/Evening Meal record Bowel Elimination (%) taken 5. Insert number from the Nutrition & Hydration 7. 6. 5. 4. a) Alert 2. b) Orientated c) Confused d) Semi-comatosed e) Deep Coma f) Anxious g) Low Mood 3. h) Tearful i) Content j) Restless/ Agitated 1. Cognitive/ Emotional State: Narrative Any complaints or notes must signs of pain? be written if a) Yes there is any b) No cause for concern for If yes, the resident complete a Pain and/or a Assessment change in Chart their condition Insert NI when there is no interaction. Insert NN when a Narrative Note is written. When recording on the Daily Record of Care: Communication Personal Care/ Controlling Body Temperature/ Self-Image DAILY FLOW CHART OF CARE 7. Visited by Spiritual Advisor 6. Prayers 5. Attended Mass/ Religious Service Spiritual Needs 4. Disturbed Sleep pattern, care given as per care plan 3. Restless 2. Eyes open and restful 1. Eyes closed & restful Sleep & Rest Sleep & Rest/ Spiritual Needs HSE Print (01) 626 3447 Ordering Code DML 29 M E N M E N M E N M E N M E N Date Communication Nutrition & Hydration MRN: ......................................................... D.O.B.:....................................................... Name:........................................................ Addressograph Label or complete the following Continence & Elimination Mobility & Safety Personal Care/ Controlling Body Temperature/ Self-Image Skin Condition/ Pressure Ulcer Prevention & Wounds DAILY FLOW RECORD OF CARE Activities Sleep & Rest / Spiritual Needs Page no.: ............. HCA’s Signature Nurse’s Signature Ward/Unit: .................................................. HSE Print (01) 626 3447 Ordering Code DML 29 M E N M E N M E N M E N M E N Date Communication Nutrition & Hydration MRN: ......................................................... D.O.B.:....................................................... Name:........................................................ Addressograph Label or complete the following Continence & Elimination Mobility & Safety Personal Care/ Controlling Body Temperature/ Self-Image Skin Condition/ Pressure Ulcer Prevention & Wounds DAILY FLOW RECORD OF CARE Activities Sleep & Rest / Spiritual Needs Page no.: ............. HCA’s Signature Nurse’s Signature Ward/Unit: .................................................. Addressograph Label or complete the following Name: ....................................................... Ward/Unit: ...................................................... D.O.B.:....................................................... MRN: ......................................................... DATE & Time (24 Hour clock) Topic Heading HSE Print (01) 626 3447 Page no.: ................ Narrative Notes Signature & Grade Ordering Code DML 30 Addressograph Label or complete the following Name: ....................................................... Ward/Unit: ...................................................... D.O.B.:....................................................... MRN: ......................................................... DATE & Time (24 Hour clock) Topic Heading HSE Print (01) 626 3447 Page no.: ................ Narrative Notes Signature & Grade Ordering Code DML 30 Three-Monthly Reassessment Date: ……… /……… /20……… Resident’s Name: …………………....…....……… MRN: ……………....…………… Ward/Unit: …..….......…………………… Yes No Resident/Significant other participated: If No, document in Narrative Notes Resident/Significant other signature: .……………....………………....……........…………....………………....………………....… Using the Resident Assessment Instruments (RAIs) listed below, are any changes noted from the resident’s last assessment? Record: No NN=Narrative Note written below CP= Care Plan initiated Please ✓(tick) in appropriate box No NN CP No NN CP No NN CP Communication, Mood / Behaviour Skin Condition, Pressure Ulcer Prevention / Wounds Meaningful Activities Breathing / Circulation Nutrition / Hydration Mobility / Safety Personal Care A Key To Me Psychosocial Well-Being Sleep / Rest Palliative Care Continence / Elimination Reassessments completed: Nutritional Continence Observations: Temp: °C, BP: / Blood Sugar Oral Pain Pressure Ulcer Risk mmHg, Pulse: /min, Resp: Falls Manual Handling /min, Weight: Kgs , Urinalysis: Referrals sent: Occupational Therapy Physiotherapy Speech & Language Therapist Nutrition Tissue Viability Nurse Audiology Activities Other: ………........……………………… MDT Referral Record updated and Narrative Note written in the main record Narrative Notes on Assessment Findings All Care plan’s reviewed and care plan initiated/ rewritten for the following problems/needs: Topic Heading Problem/need (Describe the resident’s need/identified problems in the resident’s own words, where possible) Nurse’s Signature: HSE Print (01) 626 3447 Ordering Code DML 31 Three-Monthly Reassessment (continued) Date: ……… /……… /20……… Resident’s Name: …………………....…....……… MRN: ……………....…………… Ward/Unit: …..….......…………………… Resident/Significant other participated: Yes No If No, document in Narrative Notes Resident/Significant other signature: .……………....………………....……........…………....………………....………………....… Topic Heading Problem/need (Describe the resident’s need/identified problems in the resident’s own words, where possible) Nurse’s Signature: HSE Print (01) 626 3447 Ordering Code DML 31 Respite Readmission Form Resident’s Name: ……………........…...........…..…… MRN: ……………........……… Ward/Unit: …….......…………………… Date of Readmission: ……… /……… /20……… Time: ……......………………… Admitted from: …………..............………………………… Accompanied by: ……………………………………………………. Medications with resident: Yes (see Prescription) No Aids: Hearing aid: left right Dentures: upper lower Walking Frame Wheelchair Mattress 7. Valuable List completed: Yes No Glasses: number of pairs ……..............………… partial Cane Other: …………..………………………………… Activity of Living Any changes noted from last assessment? NN=Narrative Note written CP= Care Plan initiated Please ✓(tick) in appropriate box No NN CP No NN CP No NN CP Communication, Mood / Behaviour Skin Condition, Pressure Ulcer Prevention/ Wounds Meaningful Activities Breathing / Circulation Mobility/Safety Psychosocial well being Nutrition/ Hydration Personal Care Sleep/Rest Continence/Elimination A Key To Me Palliative Care Observations: Blood Pressure: Blood Sugar: Pulse: O2 Sat: Skin Integrity: Intact See Narrative Note See Wound Care Plan Temperature: BMI: Respirations: Weight: Urinalysis: kgs Referrals sent: Occupational Therapy Physiotherapy Nutrition Audiology Activities Speech & Language Therapist Tissue Viability Nurse Other: ………........……………………… MDT Referral Record updated and Narrative Note written Reassessments completed: Nutritional Oral Pressure Ulcer Risk Falls Manual Handling Continence Admitting Nurse’s Signature: Discharge Form Resident’s Name: ……………........…...........…..…… MRN: ……………........……… Ward/Unit: …….......…………………… Date of discharge: ……… /……… /20……… Time: ……............………………… Discharged to: …………..............………………………… Accompanied by: ……………………………………………………. Medications with resident: Yes No Aids: Hearing aid: Valuable List returned: Yes No left right Glasses: number of pairs ……..............………… Dentures: upper lower Walking Frame Wheelchair Mattress partial Cane Other: …………..………………………………… Skin Integrity: Intact See Narrative Note 10. IV discontinued: Yes Not applicable Discharge Letter sent: Doctor’s letter Yes Not required Nurse’s letter Yes No Referrals: Public Health Nurse Community Health Team General Practitioner Other: ..................................................................................... Prescriptions sent: Yes No Significant other given information on the resident’s status at discharge: Yes Further details in Narrative Notes: Yes Discharging Doctor: No (see Narrative Notes) No Next Planned Admission Date: ………….....…………………. Time: Admitting Nurse’s Signature: HSE Print (01) 626 3447 Ordering Code DML 32 Appendix 3 Documentation Audit Tools 297 MINI Clinical Audit of Care Record Name of Auditor: _________________ Ward/Unit ______________ Date: __/__/20___ Yes Are the following completed: Name Ward/Unit On each page MRN Front &Back Completed and Up-to Date as per guidelines: Pain Assessment Pressure Risk Assessment Nutritional Risk Assessment Oral Cavity Assessment Falls Risk Reduction Assessment Manual Handling Assessment Weights Is there a care plan written when indicated by the RAI assessments MDT Referral Record up-to-date Three Monthly Reassessments Narrative Notes: Give a clear picture of the resident’s progress All entries are: Signed Dated Timed using the 24 hour clock Care Plans: Is there evidence of resident and / or significant other involvement in care planning? Care Plans are written within the last six months Resident’s Problem written Goal is measurable, obtainable & realistic Interventions provide sufficient information to provide care The flow charts are without gaps, using the appropriate codes Totals Not No Applicable Score % Comments: _________________________________________________________________________ ____________________________________________________________________________________ ____________________________________________________________________________________ ____________________________________________________________________________________ ____________________________________________________________________________________ Scoring: Number of ‘yes’ ticked divided by the number answered (23 (total number of questions) minus the number of ‘not applicable’ ticked) then multiply this number by 100 and this will give you the percentage Sample: 16 (total yes) ÷ 23 = 0.69 x 100= 69% compliance Full Audit of Care Plan to be carried out 6 monthly HSE Print (01) 626 3447 Ordering Code DML 33 HSE Print (01) 626 3447 Ordering Code DML 34 Number of Care Records Audited: Documentation Particulars 1 2 Audit Date: Total Scores for N/A Total Scores for Yes 14. A Pressure Ulcer Risk Assessment has been completed within the last three months 13. The Resident Assessment Instruments are signed 12. The Resident Assessment Instruments are dated 11. There is evidence that all Resident Assessment Instruments have been assessed 10. The Initial Admissions Assessment is completed within two hours of admission 9. The Personal Details Form is signed 8. The Personal Details Form is dated 7. The Resident’s vital signs have been recorded on admission 6. The Personal Details Form is timed within two hours of admission time 5. The Personal Details Form is completed without omissions 4. The resident’s medical record number is on every page of the record 3. The resident’s name is on every page of the record 2. Every staff member who has documented in the care record has signed the Signature Bank 1. All documentation is in black ink Auditor Name: Ward/Unit: 3 4 5 Chart Score 6 Methodology: Please insert 1 for Yes, if the item is found in the resident’s care record. Record 0 for No, the item is not present or N/A (Not applicable) Care Record Audit Tool HSE Print (01) 626 3447 Ordering Code DML 34 Total Scores for N/A Total Scores for Yes 34. A Manual Handling Assessment has been completed within the last three months 33. There is evidence that the Care Plan is updated when the Continence Assessment Score changes 32. The Continence Assessment is signed 31. The Continence Assessment is dated 30. A Continence Assessment has been completed within the last three months 29. There is evidence that the Care Plan is updated when Oral Cavity Assessment Score changes 28. The Oral Cavity Assessment is signed 27. The Oral Cavity Assessment is dated 26. An Oral Cavity Assessment has been completed within the last three months 25. There is evidence that the Care Plan is updated when the Falls Risk Assessment score changes 24. The Falls Risk Assessment is signed 23. The Falls Risk Assessment is dated 22. A Falls Risk Assessment has been completed within the last three months 21. There is evidence that the Care Plan is updated when the Nutritional Assessment score changes 20. The Nutritional Assessment is signed 19. The Nutritional Assessment is dated 18. A Nutritional Assessment has been carried out within the last three months 17. There is evidence that the Care Plan is updated when the Pressure Ulcer Risk Assessment Score changes 16. The Pressure Ulcer Risk Assessment is signed 15. The Pressure Ulcer Risk Assessment is dated Documentation Particulars 1 2 3 4 5 Chart Score 6 HSE Print (01) 626 3447 Ordering Code DML 34 54. All narrative notes are written as the care is given 53. The flow charts are complete without any gaps 52. The nursing interventions state when it will be done 51. The nursing interventions state how often it will be done 50. The nursing interventions state how it will be done 49. The nursing interventions state what will be done 48. The goals are realistic 47. The goals are obtainable 46. The goals are measurable 45. The goals of care are aimed to solve/ alleviate /help the resident cope 44. Resident’s identified needs/problems are written as a resident problem Total Scores for N/A Total Scores for Yes 43. There is evidence that the Activities Assessment is completed within seven days 42. There is evidence that the Activities Assessment has commenced after five days 41. Each section of the Care Plan provides information to provide individualised care 40. All problems identified have a corresponding care plan 39. There is evidence of the resident/significant other involvement in care planning than at three-monthly intervals (Standard 11.6: The residents care plan – HIQA) 38. All Care Plans are updated as indicated by the resident’s changing needs and no less frequently 37. The Manual Handling Plan is completed 36. The Manual Handling Assessment is signed 35. The Manual Handling Assessment is dated Documentation Particulars 1 2 3 4 5 Chart Score 6 HSE Print (01) 626 3447 Ordering Code DML 34 Documentation Particulars 1 2 3 4 evidence to support this Total Scores for N/A Total Scores for Yes 72. Restraint that requires removal is being removed every two hours and there is documentary 71. The use of restraint is re-assessed every 24 hours by two nurses 70. The decision to use restraint has been made by at least two members of the Healthcare Team 69. The Restraint Assessment is completed in full (with corresponding documentation in notes) 5 Chart Score Has the resident been identified as requiring restraint If yes: answer 69 – 72: If no mark with N/A 68. All student nurses’ / healthcare assistants’ entries have been co-signed by a registered nurse 67. There is evidence that the resident is reviewed after referral to Multidisciplinary Team 66. The Multidisciplinary Referral Record is current 65. Members of the healthcare team are identified by name 64. Errors are corrected according to policy 63. All symbols / grading used is An bord Altranais approved 62. All abbreviations used are from the approved list 61. Entries are made without gaps / lines between entries 60. All entries are in chronological order 59. All entries are signed 58. All entries use the twenty-four hour clock 57. All entries are dated 56. All written records are legible 55. All narrative notes are factual Documentation Particulars 6 HSE Print (01) 626 3447 Ordering Code DML 34 1 Chart Score 2 3 4 5 A minimum of 20% of the Care Records or (a minimum of 4 care records) must be randomly selected to undertake an audit. Total Scores for N/A Total Scores for Yes 80. Would you be confident to take over this resident’s care using the care plan without a handover 79. Care records are updated according to policy 78. The reassessments are signed 77. The reassessments are dated (i.e. Pressure ulcer Risk Assessment, Weights, Nutritional Assessment) 76. Reassessments are done according to local Policy 75. The Infection Care Plan is discontinued once the infection is cleared 74. There is evidence that the interventions from the care plan have been implemented 73. An Infection Care Plan is iniated once the infection is noted Has the resident been identified as having an infection; If yes answer 73 – 75: If No mark with N/A Documentation Particulars 6 HSE Print (01) 626 3447 Ordering Code DML 34 Chart 2 References: An bord Altranais (2002) Recording Clinical Practice: Guidance to Nurses and Midwives, An bord Altranais Payne, A.M. (2005) Nursing Care Plan Policy, St. Mary’s Hospital Policy Committee Chart 1 Audit Scores Chart 3 Chart 4 The target score is 100% = 80% compliance for chart 1 56 70(Total questions 80 – 10 ‘N/A’) X 100 Chart 5 For Example Total number of ‘Yes’ scores in chart 1 = 56 Total number of questions answered in chart 1 = 80 Total number of ‘Not Applicable’ questions in chart 1 =10 Chart 6 To score the audit, first total the number for ‘Yes’ scores on each page. Then add the ‘Yes’ totals from each page together, to give the total ‘Yes’ scores for each chart audited. Next total the number of ‘Not Applicable’ scores using the same format. For each chart subtract the total number of ‘Not applicable’ scores from the total number of audit questions (80 questions). The audit is scored by the following formula: Total number of ‘Yes’ scores per chart, divided by the Number of questions answered, minus ‘Not Applicable’ answers X 100 Appendix 4 Guidelines for completing “My Day My Way” 298 “My Day My Way “ Towards Developing Person Centred Care for Our Residents The Importance of getting to know the person not just the resident and what is important to them in their daily care is kernel to the concepts underpinning PCC. How can we help staff be more person- centred in their care for the individual person? As part of a National Older Persons Centred Care Programme an innovative way “My Day My Way” was developed by participants. • This getting to know me exercise can be carried out before a resident is admitted to the unit, when they are admitted as part of their admission procedure or now as part of their ongoing assessment. • This can be completed with the resident by a family member care staff named nurse. • It should be kept in the residents care plan which is accessible to all staff. • It should be reviewed and updated as part of the ongoing evaluation of the residents care. • All new staff should familiarise themselves with the plan HSE Print (01) 626 3447 My Day My Way (Example ) I would like to share with you what is important to me when caring for me Name: Mary Kelly Suite: Sandymount What makes me Happy ? • I like to put my own makeup on in the morning please don’t rush me. If you leave the mirror and the makeup bag I will work away at it. I am not in a hurry. • I love to get fresh air every day, if you can assist me to go to the garden. • I love a lie in on a Saturday morning I always did it at home. If you can put my radio on and put RTE 1. I love the chat on the radio. • I don’t like to eat my meals with other people. Please let me sit on my own to have my meals. I eat better that way. What Makes me Unhappy? • Tea. I hate tea, always have and I am not going to change now, please let staff know that. • Trousers, I have never worn a pair and I would prefer not to at this stage of my life. • Loud music and the TV on at the same time. If you bring me in to the day room, keep the noise level down please! • Not to be consulted when planning my care. I hate when people talk over me like I am not there! HSE Print (01) 626 3447