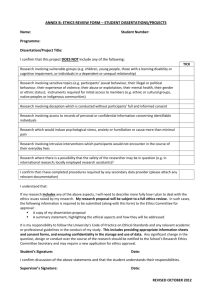
introduction 1. ethical responsibilites
advertisement

INTRODUCTION In this document we have sought to make recommendations on how ethical issues in relation to research involving human participants should be dealt with. On the great majority of issues, our recommendations are in keeping with those of other parallel bodies and, where relevant, we make reference to their reports. In all instances, we have paid careful attention to legal requirements but there are several difficult issues in which the legal situation remains ambiguous or uncertain and a very small number in which, in our view, the law appears to operate on principles that run counter to either ethical standards or good practice, or both. When that is the case, we draw attention to the discrepancies currently involved but, nevertheless, outline what we regard as the desired ethical practice. Similarly, at the time of our report, discussions are taking place on a possible revision of the Declaration of Helsinki and European bodies are considering the revision of requirements on data protection. Again, we draw attention to possible discrepancies but focus on the ethical principles. Guideline recommendations are displayed in purple text throughout this document. 1. ETHICAL RESPONSIBILITES This document is aimed at both researchers and research ethics committees for human participants (hereafter referred to simply as ethics committees). The responsibility for the ethical conduct of research rests firmly on the principal investigator (and, for legal reasons, therefore on his or her employer), and not on either the research ethics committee or the funding body, although both have a concern that the principal investigator exercises those ethical responsibilities in an appropriate fashion. We specifically note that, although there is a requirement to obtain the consent of participants1 in the research (we make no distinction in that connection between patients and volunteers), the responsibility remains with the principal investigator and is not shared with the participant. The responsibility for the ethical conduct of research rests firmly on the principal investigator. 1. Or, in the case of people who are incompetent to give consent, those who can give consent on their behalf – see paragraph 5. 1 ROYAL COLLEGE 2. RISKS AND BENEFITS OF RESEARCH OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS 2.1 Definition of research Research can be defined in a number of ways. For purposes of ethical review, the Royal College of Physicians (1996) defined the difference between research and practice as one of intent. In medical practice the primary intention is to benefit the individual patient. In research the primary intention is to advance scientific knowledge so that patients in general may benefit. In considering whether a procedure is research or not, local research ethics committees and researchers are referred to the Royal College of Physicians (1996) guidelines, paragraph 6.4: “The distinction between medical research and innovative medical practice derives from the intent2. In medical practice the predominant intent is to benefit the individual patient consulting the clinician, not to gain knowledge of general benefit, though such knowledge may emerge from the clinical experience gained. In medical research the primary intention is to advance knowledge so that patients in general may benefit: the individual patient may or may not benefit directly.” 2.2 Value of research Many advances in clinical practice have been crucially dependent on the findings of research. In some cases the gains have come from bringing together, over time, the results of basic research, which have led to a much better understanding of causal processes and of how they may be prevented or treated effectively. In other cases the gains have come from systematic evaluations that have shown which interventions are effective and which ones ineffective; or which patterns of service delivery are most beneficial for the most people. Sometimes, too, the benefits have derived from systematic descriptions of the experiences, perceptions or opinions of consumers or of staff. The benefits of research, however, are crucially dependent on it having been of high quality. Poor research, or biased research, by contrast, may impede improvements in health services, and is unethical. A key issue with respect to the advances in clinical practice that should derive from research is that it would be unethical to have a system that meant that individuals from certain segments of the population could not participate in research that focused on the disorders from which they suffered or for which they were specifically vulnerable. The criterion that is relevant in this connection, however, must be the needs of that segment of the population and not the needs of the researcher. In paragraph 5 we consider the protections that need to be employed in that connection. 2 2. In the Royal College of Physicians’ guidelines the phrase was ‘sole intent’. Although that is correct in most instances of medical practice, and although the benefit to the individual patient predominates in all cases, there are important circumstances throughout medicine in which it cannot be the sole intent. Thus, there are legal requirements to notify certain diseases because of the risk to others; similarly, compulsion may be necessary in psychiatric practice because of risks to others as well as to the individual. The key difference between clinical practice and research is that the chief focus in practice revolves around needs arising from the individual, whereas in research the focus is on extending knowledge that will provide benefits to groups of people. It is also the case that, although the aim of research is to advance knowledge, the conduct of any trial must be undertaken in a manner that is responsive to patient needs. Thus, if during the trial it becomes evident that the patient is at risk, the patient will need to be withdrawn from the study because the interests of the individual have to take precedence over the research interests. It is in the interests of everyone that high quality research should be fostered and supported. Ethics committees need to check that the research they approve is of adequate quality. Because of the immense value of research, it is unacceptable that individuals from any segments of the population be disallowed, by virtue of their being members of that group, from participation in research that is necessary to improve the understanding of disorders from which they are particularly likely to suffer. The difficulties that must be faced in this connection with groups whose capacity to consent is limited are considered further below in paragraph 5. Nevertheless, it is a basic ethical principle that psychiatric patients, like all other patients, must be able to benefit from the fruits of research and, hence, they must have the opportunity to participate freely in sound research. RISKS AND BENEFITS OF RESEARCH 2.3 Risks of research Regrettably, history shows that some research, even that which is otherwise scientifically sound, has put participants in the research at levels of risk that are unacceptable, sometimes without the participants being aware that it has been so (Beecher, 1966; Pappworth, 1967; Fienberg & Resnick, 1997). Ethics committees should be required to assess the levels of risk in all research that they review and they should not approve projects in which the risk is regarded as excessive when considered in the light of all the circumstances, and of the potential benefits. With research regarded by the ecthics committee as within an acceptable risk level, there is the additional requirement that all participants should be adequately informed about the nature of the research, its possible risks and potential benefits, so that they can make up their own minds, on an informed basis, with respect to whether or not they are willing to take part in the study. 2.4 Misuse of research Equally regrettably, history tells us that some funding bodies have sought to misrepresent or suppress the results of research (Barnes et al, 1995; Bero et al, 1995; Glantz et al, 1995, 1996; Hanauer et al, 1995; Slade et al, 1995; Hilts, 1996; Ong & Glantz, 2000). It is clear that, in some instances, such bodies have sometimes supported, without constraint or censorship, other reputable research, apparently in an attempt to conceal or downplay the examples in which they have misused research findings. Ethics committees should refuse to approve research where the funding body is of a kind that raises serious doubts about its track record on abuses of research findings. 2.5 Censorship of research It is not in the interests of the community to participate in research that is censored, subject to suppression/distortion of some findings, or for which publication is refused or unduly delayed by the funding body. Ethics committees should ensure that such constraints do not exist3. Particular difficulties arise in three main circumstances. Government departments sometimes require that they approve publications because of the policy 3. Throughout this report, we have assumed that our guidelines apply to researchers/clinicians employed by universities, charities, governmental research funds, the National Health Service (NHS) or other bodies in which the conditions of employment do not contain clauses requiring secrecy or other imposed controls. Thus, for example, our remit does not cover employees of pharmaceutical companies or governmental defence establishments. Their ethical issues are comparable but they must fall outside the remit of university/NHS ethics committees because the conditions of employment clash with our guidelines. Nevertheless, we recommend that no research should be conducted without there being an ethics committee to which research proposals must be submitted. 3 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS considerations that may arise. It is reasonable, and acceptable, that they can require the opportunity to comment and make suggestions in advance of publication. Nevertheless, it cannot be ethically acceptable that they suppress or alter findings. If they do not accept particular findings, or the interpretations put on them, it is acceptable that they require some explicit statement to that effect to be included in the report, but this must not involve prevention of publication (or unreasonable delay in publication). The second circumstance arises when the findings are commercially sensitive because of the potential financial benefits for the funding agency (such as could be the case with pharmaceutical companies). A reasonable short delay in publication may be required to allow commercial exploitation but it is not acceptable that findings be kept out of the public arena for other than a strictly defined, previously agreed, time period. The third circumstance is when Government departments consider that the publication of findings could involve national security risks. Although it is accepted that this could be a reality in some circumstances (rarely so in the field of biomedical research), the same principle as that relevant to commercial interests applies. A reasonable, previously agreed, delay in publication is acceptable, but prevention of publication is not acceptable. Ethics committees should require applicants to state whether the funding body (or any other interested party) places any constraints on publication. If any such constraints exist, the ethics committee must satisfy itself that they are reasonable in type and degree, that they are explicit and time-limited and that they do not involve risk of censorship or distortion of findings or prevention of publication. 4 3. SCOPE OF ETHICS COMMITTEES AND VARIETIES OF RESEARCH We take it as given that the role of ethics committees is to facilitate good research and that the prime purpose of ethical guidelines is to protect those who participate in research as ‘subjects’ and, in addition, to protect the researchers who undertake the research. All employing institutions have an obligation to ensure that the research undertaken by its staff meets expected ethical requirements; this obligation has implications for the remit of ethics committees. 3.1 Scope of ethics committees’ remit In order to provide the protection needed for participants, researchers and institutions, the scope of the remit of ethics committees necessarily has to be broad. The question of how the remit is dealt with in relation to different types of circumstances is considered further below. All research that involves human subjects directly or indirectly, and that is undertaken by the staff of any discipline (paid, honorary or emeritus) of an institution4, comes within the remit of its relevant ethics committee, irrespective of whether or not the participants are its patients, and irrespective of where the research is undertaken. Similarly, irrespective of who undertakes the research, all research that involves the institution’s patients, clients, students or staff as participants in the research falls within the ethics committee remit. 3.2 Clinical audit Clinical audit is now a required routine in National Health Service (NHS) practice as a set of procedures designed to ensure that the requisite standards of clinical care, notemaking, reporting, timeliness of communication and the like are being met. In so far as they have a focus on advancing knowledge (about patient care, note-taking, etc.) rather than the care of an individual, they fall within our definitions of research. As such, it is the responsibility of ethics committees to ensure that they are conducted in an ethical manner. Ordinarily, all regular clinical audits in a particular institution follow an accepted routine, and once this has been agreed and established, it should not be necessary for further ethical consideration unless and until it is proposed to alter the routine. In addition, however, there is a range of other forms of audit that go beyond these routines because they involve asking patients or staff to complete questionnaires or be interviewed. For example, this would apply to studies to determine patient satisfaction with the care they have received, or staff views on the handling of risk situations. Similarly, studies comparing different ways of giving patients information or different forms of preparation for clinical procedures constitute specific research projects. All such special forms of non-routine audit constitute research that needs to be dealt with in the same way as any other form of research. Routine clinical audit solely based on perusal of records must be conducted in an ethical manner and it is the responsibility of ethics 4. We recognise that non-medical employing bodies that are concerned with research that is not funded by either biomedical charities or research councils may not have ethics committees and procedures of a kind that we consider in this document. We regard this as unsatisfactory but its consideration falls outside the scope of our working party. Nevertheless, as noted in footnote 3, we recommend that all research should be subject to ethics committee approval. 5 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS committees to ensure that this is the case5. This will require them to obtain written details of the procedures to be followed. It is up to the committee to decide whether to delegate this responsibility to someone acting on their behalf (such as the clinical director), or to consider the procedures in committee. Either way, however, the ultimate responsibility lies with the ethics committee and it is their duty to ensure that the necessary ethical needs have been met. Patient information sheets and consent forms should not be required for such case note audit and, once a set of procedures has been agreed, it should not be necessary to reconsider the procedures until it is proposed to change them. Research into audit that involves any form of new information from patients or staff (such as by questionnaire or interview), any form of intrusion into routine procedures (such as by video- or audiotape recording or observation by researchers) or any form of participation in a comparison of procedures (whether or not by random allocation) should be subject to the same form of individual application as required for other research applications to the ethics committee. Patient information and consent forms should ordinarily be required. 3.3 Other forms of research using records and archived samples Archived records have proved invaluable in a wide range of research that has led to important advances in the understanding of risk and protective processes for disease and disorder (see Medical Research Council, 2000 for a discussion of the range of ethical issues to be considered in relation to their use). In recent years, concerns over data protection have raised the possibility that legislation might be introduced (although it has not happened so far) to require individual consent for such use of records or to restrict their use (Walton et al, 1999); this would effectively stop such research because of the impracticality of contacting people on the basis of records that may have been obtained as long as half a century ago (Melton, 1997). In any case, contact in order to ask for consent could only be obtained through the use of the very records the use of which is the subject of the consent being sought! There are many reasons to preserve the availability of archived records and samples for research, there is no possible harm to the individuals provided the necessary safeguards are maintained, and there is no reason to treat this use of archived data differently from clinical audit. However, there are four rather different uses that require some variations in approach (see paragraphs 3.3(a) to 3.3(d)). As with any other type of research involving human subjects, approval of research using records and archived samples must be sought from the appropriate ethics committee, which will need to consider the usual ethical issues with respect to purposes, reputability of researchers, lack of inappropriate constraints on publication, source of funding and the other matters outlined in this document. In addition, as also recommended by the Royal College of Physicians (1999)6, the ethics committee should have specifically agreed to exempt the research from the general requirement for individual consent from each research subject. In that respect, our recommendation on research using records and archived samples follows the same principles as those that apply to clinical audit. 3.3(A) GROUP ANALYSES USING ANONYMISED DATA In cases in which the sole intention is to undertake group analyses of anonymised data, the ethics committee should be satisfied that the required anonymisation has been 6 5. Currently, in the UK, the use of medical records and samples for audit does not require ethical approval, despite the fact that it cannot be differentiated from research in any clear and unambiguous fashion (Choo, 1998). We agree that individual consent should not be required but, despite the fact that it may not be required by law, we consider that ethical consideration of the audit procedures should be undertaken. undertaken before the data are made available to the researchers seeking to use the archived data. When the archived information involves pooled data-sets (as would be the case with many DNA or brain tissue banks), the organisation having custodianship of the databank should have its own ethics committee to review the purposes to which the analyses are to be put, and the reputability of the researchers and the funding agency. This is not currently standard practice and we recommend that it should become so. SCOPE OF ETHICS COMMITTEES AND VARIETIES OF RESEARCH Individual consent should not be necessary for group analyses of anonymised data but the ethics committee should ensure that the required anonymisation has been achieved before the data are made available. Custodians of pooled data-sets should have their own ethics committees review applications for use of those sets. 3.3(B) ANALYSIS OF PERSONALISED RECORDS In some instances it may be necessary for the analysis of archived samples or records to include access to personalised data either because of the need to derive information from patients’ case notes of a kind that is not or could not really be computerised, or because of a need to link data-sets. In keeping with the Royal College of Physicians’ (1994) Working Group, we agree that this is ethical without individual patient consent provided that: (a) access to the records be controlled by their custodian (who must not be the investigator – in order to avoid the conflict of interest entailed in someone granting themselves research access to the records of patients under the care of another consultant) who must be a senior clinician who takes the necessary steps to be satisfied on the bona fides, professional standing of the investigator and the ability of the investigator to handle the identifiable data securely in such a way as to maintain confidentiality; (b) the custodian ensures that the investigator is an appropriate senior professional person who is bound by a code of ethical standards set by a professional licensing body, and who could be subject to disciplinary action in the event of a break of confidentiality; (c) the publication of research information in no circumstances directly or indirectly identifies individuals. Individual consent should not be necessary for analyses of personalised records provided that no contact with participants is envisaged, that access to records is controlled by a custodian (who must not be the investigator) who has the responsibility for checking the details of what is proposed and that no data will be published that could directly or indirectly identify individuals. 6. The Royal College of Physicians (1999) went on, however, to recommend that, in the future, patients and healthy volunteers be made aware that the information and samples they provide may be used for research and they should be given the opportunity to dissent from such use and that such dissent would prohibit the use of their information and samples from future research, unless an ethics committee later ruled that it was in the public interest that their objection be overruled. We agree with the recommendations that all patients be made aware that their records may be used for research, but we also agree with Professor Wald’s minority view that this opportunity to dissent is illogical, would serve no useful purpose, lacks credibility and carries the risk of distorting research findings by making samples biased (Royal College of Physicians, 1999). It seems unsatisfactory to appear to give people a choice when that choice can be rescinded later without their knowledge or involvement in the decision-making. If there are no risks and if the relevant ethics committee has agreed that it is in the public interest for the research to be undertaken, there seems no point in the introduction of a meaningless constraint that would not apply to existing data-sets. Moreover, as such constraints on the use of anonymised data do not apply to clinical audit, it seems illogical to apply them to research use as these involve the same considerations. It also seems unreasonable to expect people to agree or disagree with research usage in the future when they have no idea what purpose that will serve. It is likely to be the case that some people will dissent on the basis of their views at the time the information or samples are obtained but, if asked some decades later, would give agreement freely for a purpose that they could see was valuable (or vice versa). 7 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS 3.3(C) USE OF ARCHIVED DATA FOR TRACING In other instances, archived data may have to be used as the starting point for studies because they require contact with individual patients or volunteers. This would be the case, for example, with follow-up studies. In these circumstances, the archived data may be used, without individual consent, in order to trace and make contact with the potential participant in the research, provided the requirements above (paragraph 3.3(b)) are met, and provided the safeguards noted for follow-up studies (see paragraph 4.13) are used. However, at the time of contact with the potential participant, all the usual requirements for an information sheet and informal consent should apply. The dispensing with individual consent applies only to the use of records for tracing (or for group analyses of archived data) and participants should have their usual freedom to agree or disagree to taking part in any research that requires further information, samples or any other form of personal involvement. Archived data may be used without individual consent to trace individual patients or volunteers in order to ask if they are willing to participate in a study. However, the planned study must have received ethical approval and all the usual expectations of individual informed consent apply to participation in any aspect of the research required for individual contact or new information/samples from individuals. 3.3(D) USE OF OTHER PERSONAL RECORDS FOR TRACING A related issue to that considered above is the use of other personal records (such as NHS identification numbers) in order to trace individuals in order to ask whether they are willing to participate in a particular study. Currently, practice on this issue seems inconsistent and dependent on the varying views of individuals, but it is evident that practice is becoming more restrictive. Because of the proven great importance of followup studies, and because scientific findings are likely to be seriously misleading if followup is based on incomplete biased samples, we recommend that the principles outlined above (paragraph 3.3(c)) be extended to the use of other personal records for tracing. The use of personal records for tracing, when the records are not themselves the basis for identification of potential participants in research, should be dealt with in the same way as the use of archived records for tracing. For this to be generally possible, the legal acceptability of this procedure under data protection rules will have to be made explicit. Ethics committees should ensure that the method of tracing to be used is discrete (see paragraph 4.13). 3.4 Therapeutic v. non-therapeutic research 8 The distinction between therapeutic and non-therapeutic research was included in the original Declaration of Helsinki (World Medical Association, 1989). It has particular relevance to the inclusion of some vulnerable groups in ‘non-therapeutic’ research, for example children, those with learning disabilities, some patients with dementia and others without the capacity for consent to research (also see paragraph 4). However, the Declaration of Helsinki has recently been revised (in 2000) and the therapeutic v. nontherapeutic distinction is no longer maintained. The distinction continues to be adopted in most research ethics guidelines (British Paediatric Association, 1992; Medical Research Council, 1992; Royal College of Psychiatrists, 1990; Royal College of Physicians, 1996). However, it has increasingly been criticised for excluding ‘vulnerable’ patients from benefiting from research and sometimes for thwarting potentially valuable research altogether. There is also a growing recognition that it tends to disguise the fact that therapeutic research (for example, a trial of a new drug) may often be considerably more hazardous than non-therapeutic research. Hence, although carrying ethical and legal weight, we recommend that the distinction between therapeutic and non-therapeutic research should be dropped in favour of a general provision that all research, whether or not potentially benefiting individual research subjects directly, should be considered with respect to its costs and benefits. Local research ethics committees and researchers should be aware of the continued ethical and legal relevance of the therapeutic v. non-therapeutic distinction as embodied in a number of current guidelines. However, rather than relying on the distinction as made, they should assess each research project on its merits according to the general principles outlined above, having regard in particular to the risks and benefits to potential participants. We recommend that steps should be taken to remove the distinction between therapeutic and non-therapeutic research. SCOPE OF ETHICS COMMITTEES AND VARIETIES OF RESEARCH 3.5 Non-intrusive or non-invasive research Although terms such as non-intrusive or non-invasive research and minor or ethically trivial research still appear in many guidelines and codes, they are now generally considered to be most unsatisfactory as guides to the ethical aspects of research. We agree. There are three main problems with such distinctions. First, what is deemed non-intrusive by professionals (because the procedures are routine and very low risk) may not be viewed in the same way by the lay public. Such differences of perception might apply, for example, to venesection or magnetic resonance imaging. Similarly, questionnaires that are poorly designed may give rise to distress that was not anticipated by researchers. Second, the distinctions are dimensional rather than categorical; that is, procedures vary in the degrees to which they are intrusive, invasive, major or ethically problematic. It has not proved possible, or helpful, to try to define these terms in a meaningful dichotomous fashion that applies in a comparable way to all forms of research and all kinds of participants. The degrees necessarily depend on a wide range of patient-related (or participant-related) and research-related considerations. Third, there is a danger that definitions that classify certain types of research as ‘minor’ or ‘ethically trivial’ will prove to be over inclusive, so allowing significant ethical issues to be overlooked. Ethics committees need to consider, for example, whether the use of non-standard interviews or questionnaires involves unacceptable intrusion or psychological risk. Each research proposal should be assessed on an individual basis with respect to its individual merits and risks. The details of all procedures should be considered with regard to their possible intrusiveness, invasiveness or distress-provoking properties in relation to the target group of participants. Researchers should be expected to have taken appropriate steps to keep all of these potentially negative features to a minimum. 3.6 Pilot studies All good research is likely to require the use of some form of pilot study to develop new tests or measures, to assess the likely relevance of particular approaches, to determine the applicability of established measures for use in new groups (differing, for example, in age, gender or sociocultural background from those previously studied) or to determine the timing or acceptability of combinations of measures. In practice it is often difficult to draw a clear line between clinical innovation and pilot studies for research. The criterion we apply is the one with which the document started, namely whether the main intent is to help the individual or to gain knowledge applicable to groups. When the new development constitutes a pilot study for research, it necessarily requires ethical consideration, regardless of whether one participant or 100 are involved. This means that the risks and benefits in relation to the kinds of participants and to the overall circumstances need to be considered in relation to the criteria applicable to any form of research. It should become a routine for researchers to obtain a second opinion on the level of risk from someone who is not associated with the pilot research but who has the relevant expertise to assess what is involved. It should also be mandatory for participants to be informed that the procedure is research and not ordinary clinical care, and that informed consent be obtained in an explicit fashion. Although we consider that pilot studies of all kinds, and at all stages, fall within the remit of ethics committees, there is a dilemma with respect to when a formal application for approval needs to be made. Clearly it would be impractical to expect application for 9 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS the first initial exploratory steps. On the other hand, it is important that the ethical issues be considered seriously. It is for that reason that we recommend that a second opinion should be sought at the outset. If, in the view of that external reviewer, the pilot study involves either ethical concerns or risks that might be viewed by participants (not just researchers) as more than minor, formal application for approval by the ethics committee should be required before proceeding further. If, however, the second opinion is that the risks are minor, the pilot study is being handled ethically and proper informed consent is being obtained from participants, it is acceptable that the second opinion gives approval on behalf of the ethics committee. It is up to the ethics committee to set criteria for who is able to act in this way. However, once there is a formulated plan for a pilot study, application to the ethics committee should be made in the usual way. The second opinion should have the right to specify that this must occur after a particular time period, or a particular number of cases or after some early objective have been reached. All pilot studies, at all stages and of all kinds, fall within the remit of the ethics committees. It is acceptable, however, for the early stages of pilot work to proceed without formal application provided that a second opinion (by someone approved by the committee to act on its behalf) is obtained and that the view is taken that the risks are trivial (as likely to be viewed by participants), the study is being ethically undertaken and satisfactory informed consent is being obtained from all participants. 3.7 Complaints Anyone who has valid and serious concerns over possibly unethical research has a duty to bring these concerns to the attention of the proper authority, the individuals who do so should be protected and it should be the responsibility of ethics committees to investigate all such complaints in a dispassionate manner in whatever detail seems appropriate in the circumstances. Ethics committees should be prepared dispassionately to investigate any complaints over possibly unethical practice in relation to any research falling within their area of responsibility. 3.8 Scientific fraud Fraudulent research is unethical and, hence, concerns over possible fraud fall among the responsibilities of ethics committees. Whether or not they constitute the most appropriate body to investigate allegations of possible fraud is a separate matter, but they should ensure that the organisations to which they are answerable have set up appropriate mechanisms for dealing with concerns over fraud and that the individuals who raise such concerns are protected. A key issue with respect to possible fraud is that researchers must be expected to make proper records of all steps in the research and that such records be retained for later scrutiny if required because queries about the integrity of the science have been raised. We understand that the National Academies Policy Advisory Group (NAPAG) is currently conducting a study of scientific fraud and a draft set of guidelines is peing prepared. It is the responsibility of ethics committees to ensure that appropriate mechanisms for dealing with concerns over possible fraud are available and are operated in a fair and efficient manner. 10 4. RESEARCH GOVERNANCE AND CLINICAL CARE SCOPE OF ETHICS COMMITTEES AND VARIETIES OF RESEARCH 4.1 Research quality Necessarily, consideration of the quality of research has to be a concern of ethics committees; bad or biased research is, in itself, unethical. That is because it wastes participants’ time, it creates a false impression for participants that the findings will be useful, it may lead to inappropriate policies or practice and in many cases it will also waste public monies. We consider below (see paragraph 6.5) the practical implications for ethics committees that arise from this ethical principle, but here we consider the expectations that should be placed on researchers. In all cases, there should be a recognised, named research leader who has the skills and experience to undertake well the particular study proposed, and who has the time and resources necessary to provide the supervision required. The measures used should be well designed for their purpose and should involve no more risk (including distress) than is essential for the proper, good standard conduct of the research. Appropriate informed consideration of statistical power should have been undertaken so that the sample is not so small as to be useless in meeting the stated aims of the research, or so large as to be unacceptably wasteful. When the research is of a kind that might give rise to occasional clinical risks (such as side-effects of drugs, discovery of child abuse or significant homicidal/suicidal risk) the organisation of the research team operation must provide for the availability at all times of a senior clinician who can advise on any action needed. It can never be acceptable for junior researchers to have to take such decisions on their own without the opportunity for consultation (except when essential because of the extreme urgency of the situation). It must be expected that untoward incidents arising during the course of a study (irrespective of the researcher’s judgement on whether the research procedures caused the incidents) are routinely reported to the ethics committee for it to decide on their significance and on whether there are any implications for the further continuation of the study. There must also be a commitment to publishing the results of the research (see paragraph 2.5). Quite appropriately, much research is of an exploratory or hypothesis-generating nature and often the main purpose of a study is to train a student in research methods, rather than to obtain a definitive answer to a research question. This is both scientifically necessary and ethically acceptable. Nevertheless, all such studies should be undertaken with appropriate skilled supervision; they should meet at least minimal scientific requirements in relation to the experience of the researchers, the goals of the study and the risk involved; and all the usual ethical requirements should be fulfilled. It is reasonable, however, for the degree of scientific scrutiny to be proportional to the risks for both the participants and the researchers. Ethics committees must consider the scientific quality of the study they are asked to approve and the adequate provision of expert advice within the research team on the handling of risk situations. The degree of scientific scrutiny should be proportional to the risks involved. Untoward incidents arising during the course of a study should be reported to the ethics committees, as a matter of routine. 4.2 Clinical care It is a standard ethical requirement that a person’s clinical care must not be affected by his or her unwillingness to take part in a study, or by his or her withdrawal from the study during its course. Moreover, they must have the right to decline to take part, or to withdraw, without giving a reason. It is also a standard expectation that participation in a study should not result in a person receiving a worse standard of care than would ordinarily be expected on the basis of the knowledge available at the start of the study. We consider that these are fundamental ethical principles that must be maintained. 11 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS A person’s clinical care should not be affected by his or her unwillingness to take part in a study, or his or her withdrawal from the study during its course. No reason for non-participation or withdrawal need be given. The ethics committee needs to determine that, in these circumstances, it is practical for normal care to be provided. Participation in a study, similarly, should not result in a person receiving a worse standard of care than would ordinarily be expected; the ethics committee should determine that the research design will not have that adverse effect. 4.2(A) COMPARISON GROUPS AND PLACEBO CONTROLS The general principles outlined in paragraph 4.2 can give rise to possible difficulties in seven main circumstances concerned with comparison groups and placebo controls. First, all evaluations of treatment require some form of comparison. It is therefore necessary to ensure that the control or comparison condition should not involve a quality of care below that which would be expected if the research were not taking place. This means, for example, that if the control is provided by a baseline period without active treatment, this period should not be substantially longer than the usual waiting list time in that clinical service. Similarly, if the control is provided by random allocation to a pattern of care other than that involved in the ‘experimental’ treatment to be evaluated, that other pattern of care must be at least as good as that ordinarily available locally. This means, for example, that ethically it is not acceptable for there to be a placebo control condition if a treatment of proven efficacy is already available and would ordinarily be provided. Occasionally, concerns are expressed that this brings about an undesirable interference with scientific design. We do not agree. If there is already an effective treatment, the relevant scientific question is whether the new treatment is more advantageous in any sense (e.g. in reducing symptoms or impairment, in being less likely to produce side-effects or in providing the same benefits in a more pleasant way) and not whether the new treatment is better than no treatment. In any case, we consider it ethically unacceptable that one arm of a treatment trial provides inferior care. If there is reasonable doubt over the efficacy (and/or risks) of standard treatments, the use of a placebo condition gives rise to no ethical problems. In that connection, it is up to the investigator to make the case that there is doubt and it is up to the ethics committee to decide whether that argument is valid. We accept that the case on doubt needs to be based on the evidence as a whole (and not just one isolated study) and it needs to consider the risks and benefits in the long-term as well as short-term. Second, the scientific question may focus on the immediate pharmacological effects of a new drug or psychological effects of a new psychological intervention, rather than on the clinical benefits. In this circumstance the science may require a placebo control for the period during which immediate effects are being examined. This is ethically acceptable provided that: (a) the science requires a placebo control; (b) the time period is short; (c) there is a demonstrated need to use patients rather than volunteers; (d) the participant is fully informed of the details (including the withholding of an active treatment) and agrees to take part. The ethics committee should require a reasoned argument on the science (including reasons why a placebo condition is required) and should satisfy itself that the study is ethical in the light of the overall circumstances, including the current state of knowledge. Third, there are practical difficulties in deciding during the course of a study when sufficient evidence has accumulated to demonstrate a clear advantage of one treatment over another (DeMets et al, 1999). History makes clear that some trials have been terminated prematurely, whereas others have continued for an unreasonably long time after it became obvious that one treatment was ineffective. An even more difficult situation arises when the findings show a clear short-term benefit, but doubts remain on long-term risks (this often applies with respect to preventive measures) – or vice versa. There is not (and cannot be) a simple rule of thumb to apply in these circumstances. 12 Researchers have an obligation to consider carefully the balance between the scientific and ethical considerations, and to present to the ethics committee in a fair fashion the pros and cons of different courses of action. Data monitoring committees have a key role in this connection. Fourth, a dilemma arises when the clinical research team providing the experimental and comparison treatments is not resourced to provide treatment outside the confines of the research. In these circumstances there is an obligation on the researchers to make explicit how ordinary clinical care will be provided if the individual refuses to take part in the study or withdraws from it. There can be no expectation that the research approach will enable special services outside of the research to be made available, but it must be practical to operate the clause that participants can withdraw from the study without detriment to their clinical care. Fifth, there is also an ethical dilemma if (the study having been completed), when it is demonstrated that one treatment has been effective for an individual participant and needs to continue, there are no resources for the effective treatment to continue to be provided after the research comes to an end. We recognise that there are cost issues involved and that the way these are dealt with is outside the control of the researchers. Nevertheless, we regard it as ethically dubious to stop an effective treatment that needs to continue and we recommend that the relevant health authority considers in advance how this eventuality would be dealt with. If there can be no expectation that an effective treatment can continue after the end of the research, this should be made explicit in the information sheet. There is a particular problem with research undertaken by UK researchers in other countries where the expectation for all participants is that free services are not available and it is unlikely that participants will be able to pay for the treatment themselves (Nuffield Council on Bioethics, 1999). We recommend that the issue be raised explicitly in advance with whatever pharmaceutical company is involved, asking for continuing free treatment provision for research participants if the treatment proves effective for the individuals and will need to be continued. Parallel issues arise with respect to treatments other than those involving the use of drugs. Sixth, in the course of follow-up studies it is common for research assessments to reveal unmet clinical needs and equally common for participants to request clinical help. By the nature of the research agreement between researchers and participants, there can be no expectation that clinical services can be provided. Nevertheless, as a matter of good clinical research governance, it is reasonable to expect the research team to be as helpful as they can in informing participants how they may obtain services. The senior clinician referred to in paragraph 4.1 should be expected to ensure that such advice is available. Seventh, there are some circumstances in which scientific requirements would seem to require a design in which a comparison group is subject to more than minimal risks and that these are risks that they would not experience in the absence of the research. The issues have been debated in relation to the clinical acceptability or otherwise of certain forms of sham surgery (Freeman et al, 1999; Macklin, 1999). We recognise that opinions are divided on this matter but, on the principle that a risky procedure would be against the best interests of the individual, we recommend that the use of a risky procedure as a control would not be ethically acceptable if it falls outside the scope of ordinarily expected treatment. However, often it may be possible to devise sham procedures that serve the scientific needs and yet are not risky; these may be acceptable if the participants are offered the active treatment at a later date should it prove successful. RESEARCH GOVERNANCE AND CLINICAL CARE Comparison groups are an essential part of research designs to evaluate the efficacy of treatment. When a treatment known to be effective is ordinarily available, this treatment should usually be chosen as the comparison for the new treatment being investigated; this is both scientifically and ethically appropriate. Placebo controls may, however, be justified and ethically acceptable if the science requires it and their use is not against the best interests of the individual. 4.2(B) TERMINATION OF THERAPEUTIC TRIALS As discussed in the previous section, there are real dilemmas in decisions on when a therapeutic trial should be terminated. These arise because of uncertanties over when 13 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS there is acceptable sufficient evidence that a treatment either is or is not effective, and over the balance between risks and benefits (in the short-term and long-term) of the new treatment being evaluated. Nevertheless, however diffucult the individual decision may be, the ethical princlple is clear. Therapeutic trials must be terminated when it is clear that one of the treatments being evaluated is ineffective or when a treatment is associated with an unacceptable risk of harm. Therapeutic trials must be undertaken with attention to the necessary steps required to provide adequate assessment of risks and benefits. Trials must be terminated when findings show either that a treatment is ineffective or that it is associated with an unacceptable risk of harm. For the latter to be apparent, there must be a systematic monitoring of untoward effects; these must be reported to the ethics committee. 4.3 Payment to research participants Although there has been a good tradition of altruism in clinical research, it is appropriate that research participants should be reimbursed for their time, travel/subsistence expenses and inconvenience. It is also appropriate that there be parity between payments made to patients and payments made to non-patient participants. Nevertheless, it would be unethical for such payments to be at such a high level that they either are, or could be interpreted to be, inducements to take part in research to which participants would not otherwise agree. In order to safeguard propriety, ethics committees should consider the size of reimbursements made to participants. There is a lack of consensus in the scientific community on the principles to be considered in deciding when and in what manner it is ethical to pay research participants. The pros and cons of different models are helpfully discussed by Dickert and Grady (1999) and we follow the approach that they recommend as providing the best balance. That is, payment should cover expenses and should recompense people for their time and inconvenience but, in order to avoid differing levels of payment according to earning power, this should be at a standard unskilled labour level. It is reasonable that participants in research should be reimbursed for their time, expenses and inconvenience. Ethics committees, however, need to ensure that the payments are not at such a high level that they constitute an inducement to participate. 4.4 Payment to researchers There are no ethical problems in research workers being employed (full-time or part-time) on research grants or contracts. There is also no ethical objection to research workers whose salaries are otherwise covered being reimbursed for their time, expenses and inconvenience; the situation is directly comparable with payment to research participants. However, some pharmaceutical companies have offered very substantial payments per patient recruited (or per patient who completes the trial), the level being so high that it can only be interpreted as being intended to provide an inducement. Similarly, unduly lavish entertaining may serve a similar purpose. Application forms to ethics committees should include a specific question on the level and nature of all payments to researchers, and ethics committees should satisfy themselves that these are in keeping with the guidelines of the relevant professional bodies. It should be a standard requirement that there are explicit statements on how much researchers are being paid per patient, whether the payment is to the individual researcher or the institution and what use is being made of the money. The guideline on payment to researchers is the same as that on payment to participants. 14 4.5 Deception of research participants RESEARCH GOVERNANCE It is unethical for patients or other participants to be included without their knowledge and agreement in a study involving personal contact of any kind. Also, it is a standard expectation that participants should be informed about the overall purpose of the research. This need not always specify the hypothesis to be tested or the details of the sampling because such information could create bias in reporting. If the study is a randomised controlled trial, it is, however, essential that the information sheet provided to participants be explicit that there will be random allocation to conditions, including a clear explanation of what this involves and why it is scientifically necessary. Ordinarily it is ethically unacceptable to deceive participants deliberately about the nature or purpose of a study. Nevertheless, there are some types of research in which the essence of the experimental design requires participants to be misled for the brief periods required for the experiment. Care needs to be taken in giving approval to such studies but there are circumstances in which this is both scientifically necessary and ethically acceptable. However, in order to be acceptable, it is required that the participants be appropriately debriefed after the experiment has been completed. It is never justifiable to deceive participants without discussing with them afterwards what was done and why it was necessary. AND CLINICAL CARE Participants should not be included without their knowledge or agreement in a study involving personal contact (see paragraph 3.3 regarding the exceptions with respect to group analyses of archived data). Ordinarily, participants must also be informed about the purposes of the research in which they are being asked to participate. There are occasional cases in which the essence of the scientific design requires a degree of deception. Such research needs to be carefully considered with regard to its ethical acceptability, but it may be acceptable if scientifically essential and if there is appropriate debriefing at the conclusion of the experiment. 4.6 Safety of participants The broad issue of confidentiality is discussed in paragraph 4.8 and paragraph 4.12, below, but specific consideration needs to be given to whether or not the patient’s general practitioner (or hospital or clinic professional if ongoing care is provided there) should be informed about either their participation in a study or findings from the research that have medical implications. We consider that all personal medical information belongs to the patient and it is ethically unacceptable to pass on such information without the patient’s consent. Permission may be withheld unreasonably but there are valid reasons why patients may consider that they will be disadvantaged if information is passed on. Either way, the responsibility for the decision on disclosure of information lies with the patient. The issue is somewhat different when the research involves an intervention (such as drug treatment) that could be dangerous if other medical treatments were given in ignorance of the research intervention. When this is a significant risk, it would be unethical to include the person in the study if permission to disclose the information on the research participation was withheld. It is the responsibility of the ethics committee to decide whether the risk is sufficient to require that the patient should not enter the trial. All personal medical information belongs to the patient who has the right to refuse this information (either with respect to participation in a study or to findings from the research) being passed on to his or her medical carer unless the safety of others is in jeopardy (see paragraph 4.8). If such refusal constitutes a sufficient danger to the participant (because of other treatments given in ignorance of the research intervention), it would be unethical to put the patient at risk by inclusion in the study. 15 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS 4.7 Safety of researchers It is unethical to undertake research that puts research staff under avoidable, or unreasonable, risk. The ethics committee needs to make clear to researchers that they have a responsibility for the safety of their research staff. All good research teams should have written guidelines and set procedures for dealing with whatever risks are likely to arise in the context of the particular type of research being undertaken. Acceptable research governance requires that research teams have agreed procedures for minimising the risks to staff involved in the research. 4.8 Safety of others The confidentiality of research findings should be regarded as directly comparable with the confidentiality of clinical findings. This means that, in all ordinary circumstances, findings should not be passed on to anyone else without the participant’s explicit permission. There are, however, legal limits, so that, for example, if evidence is obtained that there is current child abuse, researchers are required by law to inform social services. When this occurrence is at all likely because of the nature of the research, the information sheet should be explicit that confidentiality can only be maintained in so far as the law allows. In practice, if such evidence is dealt with sensitively by experienced clinical researchers it is extremely rare for it to be necessary to break confidentiality without the participant’s consent. A more common situation, posing a difficult ethical dilemma, is when genetic information about the participant has serious risk implications for other members of the family (Nuffield Council on Bioethics, 1993). In these circumstances, the seriousness of the situation must be discussed between the participant and a senior clinician (either within or outside the research team) knowledgeable about the specifics of the risk. If the participant still refuses permission for relevant information to be given to other family members, consideration needs to be given to whether the risks are such that the confidentiality should be breached. In these circumstances it would be good clinical practice to seek the advice of experienced colleagues and, if appropriate, of the ethics committee. The criteria to be applied should be regarded as exactly comparable to those expected if the same information arose in the course of clinical care. Exactly the same applies with respect to very serious risks of other kinds (such as homicidal threats). In practice, it is exceedingly rare not to be able to handle the risks effectively without breach of confidentiality (through discussion with the participant), but both the law and good clinical and ethical practice recognise that there can be situations in which confidentiality must be breached. When the nature of research means that it is likely that findings relevant to other family members could arise (as would be the case with some types of genetic studies), the contingency should be discussed at the point of obtaining informed consent with the aim of obtaining agreement for disclosure. If this is refused, the researcher needs to consider whether it is ethically justifiable to include that participant in the research. Research findings, like clinical findings, should in all ordinary circumstances be regarded as confidential and should not be passed on to others without the participant’s explicit permission. There are, however, rare circumstances in which the law (and/or good clinical and ethical practice) requires that confidentiality be breached. The criteria for when this rare occurrence can be considered to arise are the same in research as in clinical practice. When the nature of the research means that it is likely that findings could have implications for other family members, this contingency should be discussed at the point of obtaining informed consent, with the aim of obtaining agreement for disclosure. 4.9 Safety of children in relation to researchers 16 Currently, it is an expectation that university and NHS employed researchers working directly with children have a police check before starting such work. This is not, so far, required of those employed by the Medical Research Council (MRC) or any of the charities. The police check is focused exclusively on crimes related to children and the only information passed to the employing authority is whether or not there is a relevant risk. Clearly, this provides a highly imperfect screening, but, in our view, it is better than no screening and we recommend that it should be mandatory for all researchers working with children. Ordinarily, the personnel department should have the responsibility for monitoring that the police check has been made. RESEARCH GOVERNANCE AND CLINICAL CARE All researchers working directly with children should have a police check for crimes relating to children before starting such work. 4.10 Feedback of general research findings to participants Participants in research have the right to expect to be informed about the general results of research in which they have participated. The practice of providing feedback in the form of succinct newsletters (written in readily understandable language) summarising the key findings from the research and their implications is growing and should be strongly encouraged. It would be reasonable for this to become a standard requirement for all major studies in the future. Researchers should be strongly encouraged to provide feedback to participants on the general findings and implications of research in which they have participated. 4.11 Feedback of specific research findings applicable to the individual When research involves clinically skilled individual assessments, or when tests giving rise to individually valid findings are undertaken, it should ordinarily be expected that participants will be informed of findings that have substantial medical significance for them as individuals. This would apply, for example, to the discovery of hitherto undetected diseases such as a brain tumour revealed on a scan obtained for some other research purpose. It is essential that when feedback on specific research findings is provided that this be done in person (and not by letter), that the professional giving the feedback understands the clinical implications and that the information be given in a clinically sensitive manner with time available for discussion. There are two main circumstances, however, in which it might well be unethical to provide feedback. First, feedback would be inappropriate when the clinical significance of the ‘abnormalities’ found is unknown or uncertain. This would apply, for example, to some forms of chromosomal anomaly for which there is no known functional consequence, or some laboratory test findings that are outside the supposed normal range but appear to have no clinical significance. In many instances further testing will resolve the uncertainties but, when this is not the case, it is not clinically appropriate or helpful to tell the participant that they have some ‘abnormal’ finding but it is not known what it means. Second, in many large scale epidemiological studies the testing is undertaken by people who are not clinically trained and/or the tests used are satisfactory for detecting group differences but not satisfactory for individual diagnosis. It has become standard practice in many such studies to make it explicit on the information sheet provided at the time of obtaining informed consent that individual findings will not be fed back to participants. That is sound ethical practice. When research involves clinically valid assessments relevant for individual diagnosis, it should be expected that participants will be informed on all findings that have substantial medical significance for them as individuals. This must be done by someone who understands the clinical implications of the findings and the information must be given in a clinically sensitive manner. However, when the findings are of unknown significance or when they have meaning only at a group level, feedback should not be expected. For studies from which the findings are likely to be of this kind, the information sheet should be explicit that individual feedback will not be provided. 17 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS 4.12 Data protection and sharing Data collected during the course of research should be protected and held securely and confidentially under the control and supervision of the research group originally acquiring the data. These requirements apply equally to written records, video- or audiotaped recordings, biological samples and computerised data; the expectations with respect to security and confidentiality are the same as those that apply to clinical information (Caldicott Committee, 1998). There should be a record of the name of a given patient/participant that is linked to their data; this is necessary for the purpose of corroborating data and also in case of an urgent need to contact the person if information is obtained on a condition requiring intervention. So far as possible, however, all records (in whatever form) should be stored using identification numbers, rather than names, with the link between number and name kept separately. Ethics committees have a responsibility to ensure that research leaders for all studies are aware of their responsibilities with respect to data protection, and operate systems that provide adequate safeguards with respect to security and confidentiality. At the time of recruitment into a study, participants are (through the information sheet and consent form – see paragraph 5.3) entering into an agreement on the use of the data they provide. This involves two key elements: (a) the purpose of the research (and the uses to which information will be put); (b) the research group to whom responsibility for the data is being given. So far as the latter is concerned, the agreement is, and needs to be, with a research group; the composition of the group may change over time, but there must be a leader and contact person (with work address and telephone numbers) specified on the information sheet. Much research now is, and needs to be, collaborative and, hence, research data will need to be shared with a broader range of researchers at other centres, some of which may be abroad. In most cases, the sharing can be of anonymised data, and where this is possible, it should be the rule. In some cases, however, the sharing of personalised data may be necessary (as, for example, in order to check the reliability of ratings). This is ethically acceptable, under the concept of extended confidentiality (Wald et al, 1994) provided that: (a) the research leader exercises scrupulous research governance regarding data security and confidentiality; (b) the fact that this may happen is made explicit in the information sheet; (c) the data are shared with researchers working in a country with a data protection regime at least as rigorous as that in the UK. The expectation that the consent agreement is on the basis of a known defined purpose poses more problems when archived data of any kind may, for very good reasons, be used for purposes not envisaged at the time consent was obtained. This is particularly likely in the case of databanks that pool data-sets and make them available to a wider group of researchers. We consider that this is ethically acceptable provided that: (a) it is made explicit in the information sheet; (b) the databanks operate ethics committees to check both the bona fides of researchers applying to use databanks and the scientific legitimacy and ethical propriety of the proposed research use. Research data should be subject to the same safeguards on security and confidentiality as clinical data. The custodianship of the data should be the responsibility of the named lead researcher for the study that collected the data initially but, given appropriate safeguards, the data may be shared with collaborating researchers under the concept of extended confidentiality. 4.13 Letters and telephone calls to participants 18 Researchers need to assume that initial letters and telephone calls to potential participants (particularly in follow-up studies based on addresses and telephone numbers that are long out of date) may be intercepted by third parties and, therefore, that such communications should not implicitly or explicitly provide personal information. Thus, for example, postal franking and letter heading should not be such as to identify the communication as coming from a psychiatric facility (or any other sensitive source) and the content of the letter should not provide any information about individuals that could be regarded as confidential. RESEARCH GOVERNANCE AND CLINICAL CARE Researchers need to be aware that letters and telephone calls to potential participants, especially when using addresses and telephone numbers that may no longer be applicable, may be intercepted by third parties. This possibility requires attention to the need to avoid initial communications that, implicitly or explicitly, include personal information that could inadvertently provide a breach of confidentiality. 4.14 Biological samples Permission to use biological samples of any kind should be obtained in the same way as for any other form of research information, and the materials (and associated identifying data) should be subject to the same safeguards. It is an ethical requirement that consent for research use be obtained at the time of sample collection if research use is expected or intended, and that this is required even if most of the sample needed is to be obtained anyway for clinical purposes. Reference should be made to the MRC guidelines for collection of human tissue samples (Medical Research Council, 2001)for details on handling. Situations arise, however, when unused portions of samples obtained with the sole intention of clinical use are kept and an unanticipated research possibility arises later. The issues that pertain to this situation were discussed in paragraph 3.3. Informed consent must be obtained if it is envisaged that a portion of a biological sample obtained for a clinical purpose may also be used for research. 4.15 Avoidance of overload on participants Particularly in very active research centres, there is a potential danger that some participants may be overloaded with research requests. In some cases, this may involve significant risks – such as the repeated exposure to radiation (as a result of people being in several studies with this feature, without the researchers being aware of the other investigations). In other instances, it may involve no more than an unreasonable imposition with respect to time and inconvenience. It is part of good research governance to ensure that such overload does not occur. It would not be feasible to expect ethics committees to monitor load on participants, but they can expect their organisations (trusts, universities, etc.) to seek to ensure that researchers coordinate their studies in relation to load on participants, and they can (and should) alert lead researchers to their responsibilities in this connection. Also, when significant potential risks are involved (such as through repeated irradiation) they should require appropriate questions on past exposure to be included on the information sheet. In some instances, it may be appropriate to ask participants for permission to inform their general practitioner about their research involvement so that the general practitioner can serve as a check on possible over-involvement. Ethics committees should emphasise to their organisations and to the applicants asking for ethical approval of studies the need to avoid undue overload on research participants. 4.16 Collaboration and consultation with participant groups It is good research (and ethics) practice to consult members of the community to be studied prior to finalising research plans (Patel, 1999). Such consultation might, as appropriate to the individual study, involve consumer groups, or professional groups (who will be asked to provide information or participate in other ways), or community groups (including religious or ethnic minority groups). The several purposes of consultation 19 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS include the likelihood of better participation rates if consumer concerns have been addressed, alerting to research issues relevant to measurement and to the meaning of measures, and attention to sensitivities regarding possible misinterpretations or misuses of the research project or its findings as they apply to groups as well as to individual participants. It is good research (and ethics) practice to consult members of the community to be studied when planning studies. As appropriate to the individual study, such consutation might involve consumers, professionals, community members or ethnic/religious groups. 20 5. INFORMED CONSENT, CAPACITY AND COMPETENCE RESEARCH GOVERNANCE AND CLINICAL CARE The ethical acceptability of research requires that it be based on the freely given informed consent of participants (exceptions in relation to archived data were discussed in paragraph 3). This is no different in the case of participants who may suffer from psychiatric disorder, but the presence of mental disorder or impairment raises certain special issues of ethical concern. The ethical acceptability of research also resides on the premise that it has a sound methodological basis, uses methods that are adequate to provide valid results, is undertaken by researchers with the necessary skills and experience and involves a degree of risk that is commensurate with the benefits and that has been kept as low as possible in relation to the scientific needs. 5.1 Opting in and opting out of participation Ordinarily, it is necessary that participants should actively opt in to research, rather than have researchers assume their agreement provided that they do not actively opt out. This provides a problem, however, in the case of large scale epidemiological studies (which may require samples of tens, or even hundreds, of thousands) when parents are consenting on behalf of children. Experience shows that opting in on the basis of a posted letter (or letter sent via the child) often results in very low response rates, which is likely to bias or even nullify the research. Furthermore, when samples of non-responders have been contacted personally it has been evident that the great majority were quite happy for their children to be involved; it was just that they had not got round to replying or had mislaid the letter of invitation. It has become accepted now in several major studies in the UK that an ‘opt out’ strategy is ethically acceptable and practically feasible provided that: (a) all parents are sent an information sheet about the study and are given full details of whom to contact if they do not wish their child to take part, or if they wish for further information before deciding; (b) the research procedures are of a kind that are a normal part of ordinary routine practice (such as the use of educational tests) or involve no significant risk (such as the use of a well tested questionnaire or interview); (c) the children are given appropriate information about the study, are able themselves to give or withhold their consent and that their refusal is respected; (d) the details of the study have been scrutinised and approved by the appropriate ethics committee. An opt out strategy is not ethically or legally acceptable for any medically intrusive procedures (such as venesection) even if the risks are minimal. Ordinarily, it is necessary that potential participants actively opt in to a study. Opt out procedures with respect to parents consenting on behalf of children may be ethically acceptable, however, for large scale studies involving routine type procedures carrying no significant risk so long as certain safeguards are provided and the details of what is proposed have been approved by the appropriate ethics committee. It will always be necessary for the children to be given appropriate information, for them to give or withhold their consent, and their refusal should be accepted. 5.2 Vetoing of access to patients It is a fundamental principle that patients should have the freely exercised right to participate in sound research. Accordingly, family doctors, or other professionals, do not 21 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS ‘own’ patients on their lists and should not be able to refuse access if the potential participants are known to the researcher through some other route (such as through membership of a user organisation, attendance at some other facility or a case register). Similarly, the issue applies to the provision of addresses to enable potential participants to be contacted to ask if they are willing to take part in a study (see paragraph 3.3). An exception to this guidance arises when the patient is currently receiving treatment and when the carer considers that the research could jeopardise the care being provided. Participants should ordinarily have the right to decide for themselves whether or not they wish to participate in a study, and professionals should not have the right to refuse access when the potential participant is known to the researcher through some other route. An exception arises when the patient is currently under active treatment and the carer considers that the research could jeopardise the care being provided. 5.3 Information sheets 22 It is crucial that respondents’ agreement (or otherwise) to participate in research be based on an adequate understanding of the purpose of the study and what will be entailed if he or she agrees to take part. The research purpose and procedures must be expressed in terms that have meaning to a lay person, must be in a language that is likely to be understandable to all respondents and specific aims must be made reasonably explicit. General lofty aspirations (such as ‘to find the causes of schizophrenia’ or ‘to learn about the best treatment for depression’) are not acceptable. Similarly, the information sheet should be explicit about what is required of the participants with respect to procedures (e.g. complete questionnaires, be interviewed, have a blood test, etc.) and give a reasonable estimate of the time likely to be involved. It is not necessary to give details of all questions to be asked in a questionnaire or interview, but a clear notion of the types of topics to be covered should be given. Significant risks must be noted, together with an indication of how they will be dealt with. The information is given for the potential participant to come to an informed decision on whether to agree to take part; it is not intended as a legal protection for the researcher in relation to unlikely hazards. Thus, for example, if a treatment is thought to carry an important risk, this must be stated, but it is not necessary (or desirable) to list all possible remote or minor side-effects that could occur. Researchers should, however, be ready and willing to provide more detailed information if the participant requires it. The guiding principle is that the consent be based on a full and frank disclosure of the relevant facts. The information sheet should provide a succinct summary but it should not be a substitute for personal discussion between the researcher and the prospective participant (see paragraph 5.4). It is helpful to all concerned for the ethics committee to develop a set of recommended standard descriptions of standard procedures and their risks. Thus, these might be made available for the different types of brain scan, for randomisation and for the various forms of genetic study. Some illustrative examples are given in Appendix 1. The form of words should have been checked with user representatives. Jargon terms should always be avoided. Care should be taken to ensure that the language used is neither discriminatory nor derogatory. Applicants should be instructed to have checked the reading level required for the information sheet (using appropriate computer software). The information sheet should have a readily understandable title for the study and should give the name, work address and contact telephone numbers of the lead researcher responsible for the study and the person to contact with respect to queries or practicalities (if different). Application forms should include a mandatory question on possible conflicts of interests (these go beyond the source of funding of the particular study that is the subject of the application) and this should be parallel to the same issue with respect to committee members (see paragraph 6.7). They should also include questions on payments to researchers and to participants. If some of the sample require special consideration, there should be separate versions of the information sheet tailored to their needs (but what is said must always be compatible across versions). Thus, if the sample includes children, there should be consideration of whether there should be separate versions of the information sheet for parents and children. Similar considerations may apply when some of the sample are patients and some are recruited as volunteers. In multi-centre studies, the information sheet and consent form should be standardised in their important details in order to ensure comparability in samples and procedures across centres. The information sheet must state explicitly that respondents have a choice on whether or not to participate and that declining to take part will not affect the availability of normal treatment. Similarly, it should be stated that participants may withdraw from the study at any stage and need not give a reason for doing so. Despite the need for the information sheet to provide key details about the study, it is essential that it be in a form, and of a length, likely to be read and understood by the respondent. Thus, it must be a succinct statement and not a discussion essay. Ordinarily it should be confined within a single page of A4 paper. INFORMED CONSENT, CAPACITY AND COMPETENCE Researchers have a responsibility to ensure that all respondents have a clearly written, readily understandable information sheet that is explicit on the purpose of the study, the procedures involved, what is required of the participants, details of the lead researcher and contact person, any significant risks and the right to decline to take part (or to withdraw during the study) without giving a reason and without detriment to normal treatment. 5.4 Consent forms It is a requirement that participants have the opportunity to ask questions or raise concerns and that consent be obtained only after the person is satisfied that they have received the information they want, have understood what is involved and have been satisfied that their concerns have been addressed and dealt with to their satisfaction. Usually, the discussion and the obtaining of consent can be dealt with on the same occasion. However, it is good clinical practice to allow potential participants the time and circumstances to consider their decision and they should be allowed to think over the issues if they wish to do so before deciding whether or not to consent. Ordinarily, there should be a signed and dated consent form that is stored with the individual research record. When video- or audiotapes are used the recording should include a question and the respondent’s answer about the fact that the interview/test/ observation is being recorded, and that the participant is willing for that to be done. The consent form need not repeat the information in the information sheet, but it should include a statement that the information sheet has been provided and that the participant has been able to have his or her queries answered. If a written consent is not to be obtained, the ethics committee should be satisfied that verbal consent is sufficient and that the reasons for not obtaining written consent are valid and ethically acceptable. If oral consent is used, a record must be kept of the relevant circumstances (including the information given, how consent was obtained and who was present). Ordinarily, a written consent should be obtained; this should specify that the information sheet has been given, read and understood and that what is involved has been explained to the satisfaction of the participant. 5.5 Inducements and undue influence to participate The GMC (1998) has stressed that there must be no coercion placed upon potential participants to agree to take part in research. There are three main situations in which there may be particular concerns. First, whereas it is appropriate to reimburse participants (see paragraph 4.3), the level of reimbursement must not be such that it could act as an inducement to agree to participate. Second, hierarchical relationships within organisations can place undue pressure on people to participate. This may arise if patients wish to please their doctor by participating and if they fear that non-participation may jeopardise their medical care or the time they have to wait for it. It may also arise with non-patient 23 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: samples if the respondents are students or employees, who may feel that their careers will be fostered by participation in the research (see paragraph 5.6(g)). Two safeguards are needed: (a) an explicit statement in the information sheet (see paragraph 5.3); ETHICS (b) discussion with potential participants on whether or not they wish to participate, which should be undertaken by someone other than the person in a hierarchical relationship with the respondent. Third, detained persons (either patients or prisoners) may feel under pressure to consent to participate or may think that participation will afford them more favourable treatment or will make early release more likely. These groups are considered more fully in paragraphs 5.6(e) and 5.6(f), but the safeguards to be employed comprise: (a) relevant explicit statements in the information sheet; (b) discussions on whether to participate by a researcher who is not in a position (real or perceived) to influence detention; (c) an independent opinion on participation from someone with relevant experience. Scrupulous care must be taken by researchers to avoid undue influence on potential participants to agree to take part in research. Attention is particularly necessary with respect to payments to participants, the dangers of pressure implicit in hierarchical relationships and the pressures (and opportunities) that may be perceived by detained persons. 5.6 Competence and capacity to consent Of all the ethical issues regarding research with psychiatric patients, those surrounding competence and capacity to consent are the most problematic for both practical and legal reasons7. Competence is a legal concept that, by its nature, has to be categorical. That is, in order to decide whether a person can or cannot provide consent, it is necessary to determine whether a particular individual is or is not competent to consent to a given procedure at a specific time. Capacity is a clinical term that is generally taken to mean that a person has the cognitive and other psychological skills/understanding necessary to be capable of coming to an informed decision on whether or not to consent. At one time, this used to be thought of in ‘status’ or categorical terms, meaning that an individual either did or did not have the capacity to consent. Research findings and clinical experience have made it clear that that is a mistaken approach because skills/understanding constitute a graded dimensional phenomenon (rather than something that is categorically present or absent). Moreover, it is likely to be influenced by training and by how the issues are expressed. Also, it may fluctuate over time according to mental state and circumstances. In addition, the level of capacity will vary according to the complexity of particular decisions and the person’s experience of the related features, and according to context (see Appendices 2 and 3). The need to consider capacity in dimensional functional terms, together with the recognition that individuals can be helped to have the capacity necessary for specific decisions in specific contexts, mean that researchers are under an obligation to seek to enable potential participants to achieve the capacity required. This requires that the issues be put in practical concrete (rather than abstract) terms; that steps should be taken (if necessary, over several sessions) to help the person understand what is involved in the 24 7. The Medical Defence Union (1997) guidance and the British Medical Association and the Law Society publication (1995) to which it refers, are reasonably clear and helpful, but the therapeutic/ non-therapeutic distinction, which we reject, is used. The Law Commission (1995) report adopts a broadly functional approach. The legal situation remains somewhat ambiguous because the key issue of the true meaning of capacity and how to measure it remains unresolved (see Kennedy, 1997). decision and in its consequences; when appropriate, reference should be made to parallel situations that the person has already experienced; and the discussion should use language appropriate to the person’s understanding. Irrespective of the categorical decision on competence that is legally required, it is always clinically desirable for respondents to be helped to understand what is involved and to participate in decision-making at whatever level is possible8. INFORMED CONSENT, CAPACITY AND COMPETENCE The capacity to give consent is task- and time-specific, it constitutes a graded dimension of understanding, and it is something that can be influenced to some degree. Researchers should seek to help respondents achieve the capacity needed for the specific decision needed. Although, legally, a categorical decision on whether a person is competent to give consent is required, individuals whose capacity falls below that level should be helped to understand what is involved and to participate in decision-making. Ethics committees should satisfy themselves that the materials and process used to facilitate understanding are adequate. 5.6(A) CHILDREN The issues already outlined (paragraph 5.6) with respect to the need to aid understanding of the research participation issues, and to include in decision-making respondents whose capacity falls short of that required for competence, apply to children (Smyth & Weindling, 1999). Researchers should start with the assumption that, until proved otherwise with a particular child, all children are able to achieve some degree of understanding (however partial). Even when the child lacks the capacity to give consent, it is good research practice to engage the child in the decision-making process and to seek to achieve the child’s assent to whatever is required. At one time the criterion for including children in research was that it was therapeutic and, therefore, in the child’s personal best interests. That is no longer regarded as an ethically acceptable criterion because it would serve to exclude children from research that could lead to major advances in the treatment or prevention of diseases that are a substantial source of morbidity or mortality in early life. Rather, the criterion is that the research needs to be done with children because it concerns disorders or diseases of childhood and because answers to the scientific questions could not equally well be obtained using adult participants who are competent to give consent for themselves. Also, it is necessary that the research should not be against the child’s best interests. In this circumstance, parents are able to authorise children’s participation in a study (and should sign an appropriate consent form making that explicit) provided it presents no more than minimal risks9. On that criterion, it would be permissible, for example, to agree to venesection or a low radiation dose X-ray or scans (such as magnetic resonance imaging) that do not involve a radiation risk. Steps should always be taken through adequate preparation and specific interventions (such as anaesthetic cream for venesection) to reduce the distress of the child. Videotapes and demonstrations have been found to be very helpful in gaining children’s participation in procedures such as scans. The situation is not quite as straightforward when the research (therapeutic or nontherapeutic) involves risks that are more than minimal. Provided that the scientific need is sufficiently great, specifically applies to children and could not be met with research on competent adults, the research may still be ethically acceptable10. We emphasise that the scientific need must be judged strictly in terms of the potential benefits with respect to 8. There is a growing literature on semi-standardised approaches to the assessment of capacity/ competence, but there are no widely accepted instruments even for use in the clinical context and the validity of attempts to seek to develop a standard tool are highly dubious, given that capacity is task-specific. 9. In the USA, minimal risks have been defined as those no greater than the risks normally encountered during routine physical or psychological examinations or tests (Federal Policy for the Protection of Human Subjects, 1991). Although this has no legal standing in the UK, this seems a sensible, workable definition to use. 10. The legal situation in the UK regarding such research on children remains unclear. 25 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS the disorders from which the children suffer (or to which they are at risk) and not in terms of the scientific interest as viewed from the perspective of the researcher. However, we recommend that a strong case would need to be made and, in addition to obtaining parental assent, it would be essential to obtain an independent professional opinion on both the scientific needs and ethical acceptability. The research should be approved only if that opinion is unambiguously supportive. Parents are ordinarily the best judges of what is acceptable for their children but there may be occasions when, in their fully reasonable concern to achieve a solution to the disease/disorder from which their child suffers, they may be too ready to give assent. Parental assent is a necessary but not a sufficient criterion for approval for a child to be included in research involving more than minimal risk. Two situations require specific consideration. First, there is the question of what is acceptable when a child expresses (verbal or non-verbal) refusal to participate, despite parental assent having been obtained. We advise that, when the procedures are more intrusive than those required for ordinary clinical care, the child’s refusal should be accepted as a sufficient reason not to proceed. The child’s perception of what is intrusive should always be considered. Second, there is the question of whether parental refusal can be overridden. Clearly, there are circumstances (such as when there has been child abuse or neglect) in which it cannot be assumed that parents will act in the child’s best interests. The legal situation is clear that when the child has been removed from parental care, the parental responsibilities are then transferred to some other person or body. When that has not happened, it would be unethical to proceed without the assent of the parent. Ordinarily, the expectation is that both parents should assent, but if the child is living with just one parent who is exercising decision-making in other aspects of the child’s life, the assent of that one parent may be sufficient. Given the complications of the many permutations on child care that are possible, each case will need to be decided on its own merits. Great caution should be exercised before proceeding when the parents disagree over the child’s participation in a study. It is good research practice to engage children in the decision-making process even when they lack the capacity to give consent. The issues with respect to assessing capacity outlined in paragraph 5.6 apply to children. Parents should be able to authorise children’s participation in research provided it presents no more than minimal risks. If the research involves risks that are greater than minimal, it could be ethically acceptable if the scientific need is sufficiently great, specifically applies to children and could not be met with research on competent adults. A strong case would need to be made in this circumstance and, in addition to parental assent, it would be essential for there to be unambiguous support from an independent professional with respect to both scientific needs and ethical acceptability. With procedures that are more intrusive than required for ordinary clinical care, a child’s refusal should be accepted as a sufficient reason not to proceed, irrespective of parental consent. 5.6(B) ADULTS INCOMPETENT TO CONSENT TO RESEARCH 26 Despite extensive legal and ethical discussion, it remains the case that, in the UK, the law does not recognise proxy consent for adults. The issue of obtaining informal consent with adults suffering from a psychiatric disorder is not a problem in most instances. Many patients do not have an impaired capacity (Appelbaum & Grisso, 1995; Grisso & Appelbaum, 1996; Wong et al, 1999, 2000) and, even when initially they appear to lack capacity, it is often possible to improve understanding through the provision of appropriate information, discussion and education; the improvement may often be sufficient for informed consent to be obtained (Appelbaum, 1998). This may be the case, for example, in the early stages of dementia – a common condition in the psychiatric care of older people. Nevertheless, there are important common situations requiring research in which potential participants are not competent to consent. This applies, for example, to the more severe forms of dementia or learning difficulties and to some cases of schizophrenia or bipolar affective disorder, to mention a few examples. In these circumstances it is important to have a way of proceeding in order to ensure that individuals from these groups are not prevented from profiting from the benefits of research simply because of their membership of a group likely to have impaired capacity. We recommend, following the same principles as those discussed in relation to children, that it is ethically acceptable to include in research (therapeutic or non-therapeutic), without informed consent, adults who are incompetent to consent provided that: (a) the study is concerned with the disease, disorder or disability from which the patient suffers; INFORMED CONSENT, CAPACITY AND COMPETENCE (b) the research cannot be undertaken with validity in less vulnerable groups with the same disorder who are capable of giving consent; (c) adequate steps have been taken to help the individual gain sufficient understanding so that informed consent could be obtained; (d) the individual’s closest relative or cohabiting partner has given assent on the basis of adequate information and discussion; (e) the patient’s professional carer (medical or non-medical, as appropriate) is of the firm opinion that the risks and benefits for the individual, taken in consideration with the relevance of the research, warrant the person being included in the study; (f) this opinion is reviewed and ratified by an appropriately experienced clinician who is independent from the study; (g) the risks are minimal (using the criteria as we have defined them above); (h) the research is not against the individual’s best interests; (i) the study as a whole has been reviewed and approved by the appropriate ethics committee. No individual should be disqualified, by virtue of his or her group membership, from participating in research (as a result of incompetence to give consent or other reason) that could be of benefit in relation to the disease, disorder or disability from which he or she suffers. It is ethically acceptable to proceed without personal informed consent provided that a specified set of conditions has been met. These include the relevance of the research, the fact that the research cannot be undertaken with validity in less vulnerable groups with the same disorder, the assent of the individual’s closest relative or cohabiting partner, the support of both the person’s professional carer and an independent clinician, minimal risks and approval by the appropriate ethics committee. However, as with children, the patient’s refusal should be accepted as sufficient reason not to proceed, irrespective of other consents. 5.6(C) EMERGENCY RESEARCH WITH ADULTS INCOMPETENT TO CONSENT There are some further considerations that apply to circumstances in which research decisions need to be taken very quickly. This would be the case, for example, with patients who are in a state of severely impaired consciousness following head injury or stroke (see Appendix 4). This is a life-threatening situation requiring emergency action but in which existing treatments are unsatisfactory. In this circumstance, the research is in the patient’s best interest because the emergency necessitates intervention, and the research risk may be reasonable compared with the risks of existing therapy, or the expected outcome without therapy. The patient is incompetent to give consent at the time the research intervention needs to be introduced and, in most instances, it would not be feasible to contact a close relative (or they may be in too distressed a state for their consent to be truly informed and dispassionate). In keeping with the decisions of a local or multi-centre research ethics committee with respect to a specific randomised controlled trial of treatment in such an emergency situation, we recommend that it is ethical to proceed without consent if eight conditions are met: (a) the existing treatment is of dubious or limited effectiveness; (b) the research treatment is promising but unproven; 27 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS (c) the research risk is reasonable compared with the risks of the existing treatment or natural outcome (but not necessarily minimal in the ordinary sense); (d) the doctor dealing with the emergency treatment of the patient considers that the balance of risks and benefits for the individual patient warrant going ahead with inclusion in the study; (e) the decision to include the patient in the randomised trial (or other type of study) is reviewed and ratified by an appropriately experienced clinician who is independent of the research; (f) there is no objection from any available relative or cohabiting partner; (g) the study as a whole has been reviewed and approved by the appropriate ethics committee; (h) in keeping with Food and Drug Administration (1999) recommendations, we advise that, in addition and whenever possible, waived consent should be followed by deferred consent. That is, as soon as possible, the patient, family or guardians should be informed about the research (British Paediatric Association, 1992) and given the option of continuing in the trial or withdrawing from it. It is ethical to waive consent in the study of emergency treatments for life-threatening situations affecting individuals who are incompetent to give consent, provided the principles outlined in paragraph 5.6(b) have been followed. The specifics in such emergency situations differ, however, in two respects. It is acceptable to proceed without the assent of a relative if that cannot be obtained in time (but not ethical to proceed in the face of a relative’s objection) and the risks and benefits should be judged in relation to those associated with existing treatments or outcomes (rather than minimal risks in an absolute sense). In planning research that deals with these circumstances, there should be appropriate consultation with the relevant user groups (see paragraph 4.16). 5.6(D) PEOPLE WITH LEARNING DIFFICULTIES 28 The same general principles outlined in paragraphs 5.6 to 5.6(g) apply to individuals with learning difficulties (see Appendix 3). It should not be assumed that people with learning difficulties are incompetent to give consent; active steps should be taken to enable them to achieve sufficient understanding to give informed consent; and the level of decisionmaking ability required should be less for research without significant risks but with potential benefits. Research involving people with learning difficulties is ethically acceptable provided that: the research is of major relevance to learning difficulties; the risks are minimal; the individual does not object or appear to object either verbally or nonverbally; the research does not intrude unreasonably on the person’s privacy or freedom of action; appropriate assent is obtained (see below); and the study has been considered and given approval by the relevant ethics committee. Two specific issues need consideration. First, the minimal risk criterion, if regarded as an absolute, would rule out certain types of research that might be crucial for an understanding of the causes of severe learning difficulties and that could not be undertaken validly in less vulnerable groups. Thus, for example, some investigations might require the person to be heavily sedated (which might also be viewed as above a minimal risk). We advise that such research would be ethical provided that its quality was high, its potential value in relation to learning difficulties was great, the absolute level of risk for the individual was low and that the assent of a close relative and approval of an independent professional was obtained (as in paragraphs 5.6(a) and 5.6(b)). In the case of an individual without close relatives, it would be appropriate to obtain assent from a primary non-professional carer who is well known to the individual and apparently trusted by them. It would also be important to obtain the views of relevant user group representatives. However, the risk–benefit ratio of such research would have to be clearly favourable for ethics approval to be justified. The second point derives from the first. UK law at present does not recognise the parents of adults with learning difficulties as having any rights in relation to their care. This is widely resented by the families and is seen as inappropriate, and very insensitive, by most professionals. We recommend that consideration needs to be given to a change in the law on this issue. In most ordinary circumstances parents are the people most likely to look after the benefits of the individual in relation to treatment or research. We recognise that there are circumstances in which this might not be the case (see paragraph 5.6(a) above) and, hence, the procedures we propose require the support of an independent professional (approved by the ethics committee), as well as the assent of the closest relative. INFORMED CONSENT, CAPACITY AND COMPETENCE Active steps should be taken to help individuals with learning difficulties to achieve sufficient understanding for them to give informed consent. Even when this is not possible, the individuals should be helped to be involved in the decision-making process. When the competence to give consent is lacking, research may be ethically acceptable if it is relevant to learning difficulties, it is not against the individual’s best interests, it does not intrude unreasonably on the person’s privacy or freedom of action, appropriate assent has been obtained from a close relative, the procedures have been approved by an independent professional, the study has the support of relevant user group representatives and the study as a whole has been approved by the relevant ethics committee. 5.6(E) STAFF AND STUDENTS There is a good tradition of researchers trying out procedures on themselves before asking participants in studies to undergo them. Also, there are situations in which control data may be obtained most appropriately from the researchers themselves (e.g. in scanning studies), although attention will always need to be paid to comparability in features that could affect findings. Researchers, however, need to be very sensitive to the problems inherent in asking others (such as staff and students) to volunteer for research. When there is an implicit or explicit hierarchical relationship with those individuals who are being recruited as participants, there is a substantial risk of a perception that covert coercion is present (because there may be a concern that agreement to take part in a study will be favorable to career progression and a refusal will put progression at risk). We advise that these risks must always be carefully considered whenever staff or students are to be used as research participants. It is usually undesirable for researchers to use staff or students with whom they have a hierarchical relationship, and if this is intended, the application to the ethics committee must provide a reasoned explanation of why it is necessary and how the coercion risk will be dealt with. The risks are somewhat less, but still present, for staff and students in the same institution but outside the responsibility of the research group. The risks are least with staff and students at other institutions. In all cases, however, scrupulous attention must be paid to the risks of perceived covert coercion, and thought needs to be given to the possibility of using other sources of volunteers. In addition to the issue of possibly perceived coercion in a hierarchical situation, there are ethical issues involved in asking colleagues (i.e. staff or students) highly personal questions. In research where this is involved, we recommend that staff or students should not be asked to participate. There are risks of perceived covert coercion if staff and students who are in a hierarchical relationship with the researcher are approached to volunteer to participate in research. It is usually desirable to avoid the use of such groups in research and, if their use is needed, there must be a reasoned case included in the ethics committee application; this must specify how the coercion concern will be dealt with. 5.6(F) DETAINED PATIENTS The obtaining of fully informed consent is an especially sensitive issue in relation to patients detained under the Mental Health Act, mainly because of the actual or perceived problem of coercion, but also because they are likely to be seriously ill (with the consequent 29 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS uncertainties over their ability to give informed consent). The general principles already outlined in earlier paragraphs of section 5.6 apply, but particular care should be taken to ensure that the process of gaining informed consent should be as transparent as possible to the patient and that it should be obtained by someone other than the medical officer who is seen by the patient as having a decision-making role in relation to the detention. As advised in earlier paragraphs, it should be essential to obtain the opinion of an independent professional; an approved social worker or legal representative might well be the most appropriate person. When the patient is incompetent to give consent, the same procedures as outlined in paragraph 5.6(b) apply. When the patient is competent, the procedures should be those that apply to any patient except that especial care is needed to ensure that there is no possibility of perceived coercion and, because of that, an independent professional opinion should always be obtained. The minimal risk criterion applies in the case of incompetent patients but not detained patients capable of giving informed consent. For detained patients the general principles of paragraph 5.6 apply, but especial care is needed to ensure that there is no possibility of perceived coercion and that an independent professional opinion has been obtained. For research on detained patients to be ethically acceptable, the focus of the research must be relevant for their disorders, it must not be possible for the research to be undertaken in a valid and generalisable fashion with less vulnerable groups, it must not be against their individual best interests and particular care must be taken to ensure that the informed consent is real. Ordinarily, too, it should be expected that the research procedures should be non-invasive. Invasive research may be ethically acceptable but particularly strong justification with respect to risks and benefits would be essential (see paragraph 5.6(a)). 5.6(G) PRISONERS Prisoners, or offenders under community detention orders, may be approached to take part in two main sorts of research: (a) that which pertains to their status as offenders, in order to further an understanding of the nature of antisocial behaviour or its effective prevention or management; (b) that designed to further the understanding or treatment of some disorder to which they may be particularly vulnerable. In the latter case they should not be approached to take part in any research that would not be appropriate for their peers in the wider community. As with other groups, it is important that they not be excluded from research that is relevant in relation to the problems they experience or the disorders from which they suffer. Equally, it is crucial that researchers are aware of the many opportunities for perception that there is covert coercion, or the opportunity for gain, both of which could invalidate consent procedures. Particular care should be taken to ensure that prisoners and supervised offenders understand that their decision whether or not to participate in research will not affect their sentence or conditions. This should be made explicit in the information sheet. For prisoners the same general principles as those outlined for detained patients apply with respect to possibly perceived coercion, but in most cases there is not the same issue with respect to competence. In the few instances where that is relevant, a comparable set of procedures should be followed at the individual level. When competence is not in doubt, the main concern is to ensure that the research, and the procedures of obtaining consent, provide adequate protection to the individual. Ethics committees should consider whether, given the nature of a particular study, independent advice should be sought regarding the ethical acceptability of the study. 30 6. OPERATION OF ETHICS COMMITTEES INFORMED CONSENT, CAPACITY AND COMPETENCE Ethics committees vary greatly in the types of research that they cover. Some serve wide areas of NHS research, with very few projects concerned with mental health issues. Some serve teaching hospitals, medical schools or universities, with many proposals dealing with pilot projects by students, but also many that deal with complex high technology research, much of which is inter-disciplinary. A few are concerned with postgraduate psychiatric research and teaching centres with a very high throughput of psychiatric, psychological, nursing and social work research concerned with psychopathological questions, dealing with both patient and general population samples. It is inevitable, therefore, that such committees will vary in their mix of expertise and experience, as well as in the applications that they have to assess. This has unavoidable implications for the details of the ways in which they operate. In this report, we concentrate, therefore, on the basic principles that we wish to see applied. 6.1 Legal framework Ethics committees review protocols, make recommendations on the ethical acceptability of specific studies and advise on broader issues. Currently, however, they do not, even vicariously, have responsibility for the implementation and conduct of any study, or for the behaviour of any individual researchers. Those responsibilities remain firmly with the principal investigators and their employers. We recommend that clearer lines of responsibility need to be established. At present, institutions vary greatly in their rules regarding ethical review of studies carried out by their employees and/or carried out on their patients or staff. We advise that it is desirable that there be uniformity in expectations and that these follow the lines of paragraph 3.1. It is also not always clear whether individual researchers have the right to disregard the recommendations of ethics committees. We suggest that employing authorities make it explicit that research undertaken without ethical approval will not be supported by them and that undertaking unethical research is automatically a justification for disciplinary action. If an individual believes that an ethics committee decision is mistaken, there should be a right to appeal against the decision, and ethics committees need to decide how they operate such an appeals system. We recognise the unacceptability of an arrangement whereby the body that came to the initial decision also assesses the appeal. We advise that in the event of such an appeal, the ethics committee should as a matter of course have the appeal assessed by a different ethics committee, the choice of committee being agreed with the person making the appeal. The decision should lie with that second committee and not with any individual (such as a dean or clinical director) who has been outside the group with experience in considering ethical issues. Uniformity should be sought on expectations regarding which studies need to be submitted to ethics committees. The legal implications of disregarding ethics committee decisions should also be clarified. 6.2 Composition of ethics committees Ethics committees face complex issues, and it is essential that their membership provides the expertise and experience required for the task (see National Bioethics Advisory Commission, 1998). This has to include knowledge on the relevant scientific issues, and it is essential that membership includes mental health specialists if research in this field is to be considered. At present, that is sometimes not the case, and it needs to be remedied. Expertise should also be available on those aspects of research that are relevant to many studies in the psychiatric field such as: epidemiology; statistics; experimental methods; randomised control trials; pharmacology; imaging methods; genetics; the design and use of research interviews and questionnaires; and the clinical issues involved in caring for 31 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS 32 vulnerable groups whose ability to give informed consent is an issue to be considered. Experience in these areas may well be provided by researchers who do not themselves work in the mental health field. We recognise that often it may not be practicable to have a membership with all the relevant research skills; when this is the case it should be a matter of routine to seek expert advice on the relevant clinical or research issues (such as drug effects or radiation hazards). Much research into mental disorders is inter-disciplinary, and this should be reflected in the ethics committee membership; clinical psychology expertise is particularly relevant. There is a similar need for membership to cover the relevant areas of clinical experience. Clearly, this has to include psychiatry if applications are likely to deal with research into mental disorders. In addition, however, the coverage should provide for experience with age groups presenting special issues that need consideration; childhood and old age are obvious examples. If applications are likely to include these groups, the committee should have clinicians whose practice is relevant to them. The same applies to learning disabilities if they are included in the applications covered by the committee. Clinical research will often impinge on care outside hospital, and it should be routine to have a general practitioner on each committee. With psychiatry, care frequently involves other disciplines, and there is a comparable need to have a nurse and/or a social worker included in the membership. Ethical issues involve far more than scientific and clinical considerations, and it is essential that the membership includes several lay (meaning non-clinical) people who are not employees of the trust or university served by the committee. However, if lay people are to have an effective role, it is important that they have some relevant experience such as through holding (or having recently held) a non-clinical role in hospital or community services or in a medical charity. It is also important that patients, their families and non-statutory bodies that represent them should also be able to provide input to ethics committees. Ordinarily, however, it is preferable for such members not to be patients of the trust served by the committee (to avoid their having too personal a view – either positive or negative). A further consideration is that the committee should be sensitive to possible special considerations arising from differences in gender or variations in ethnicity, and this should be reflected in its membership. Although it is necessary for the committee membership to cover a wide range of interests and experience, it is also essential that it works as a cohesive group and that members respect the complementary expertise of others. Accordingly, we advise that members should be chosen for their personal qualities as effective committee members with an interest in ethical issues, and not as advocates or representatives of particular interests. It should also be explicit that they accept that all discussions in the committee are confidential, although the decisions of the committee should be made available in appropriate reports. In order to ensure that the relevant expertise is available at all committee meetings, it should be acceptable for members to have previously agreed alternates. It is necessary that ethics committees are trusted for their dispassionate consideration of ethical issues and not be open to the perception that they are there to defend research interests. For this reason, we recommend (in line with Department of Health advice, see NHS Management Executive, 1991) that it is highly desirable for either the chair or vicechair of ethics committees to be a lay person and we advise that, in time, it might be desirable for this to become a mandatory requirement. We do not, however, recommend that now because of the practical difficulties some ethics committees have experienced in getting lay people with both sufficient knowledge of the clinical and research issues and the time and commitment to consider many varied applications. As evidenced by the need for the present working party, ethical issues in the mental health field are becoming increasingly complex. Training in research ethics is becomingly increasingly widely available and committee members should be strongly encouraged (and financially supported) to obtain such training. Ethics committees need to consider whether they should specify a minimum level of training that is expected of each committee member. When ethics committees only rarely receive applications dealing with mental health issues, it may be reasonable not to include in their membership either professionals or user group representatives with experience in this area of work. However, when they do receive an application on mental health issues it should be a standard expectation that either they obtain expert advice through coopted membership or they should pass the application on to be dealt with by another ethics committee that does have the necessary expertise. OPERATION OF ETHICS COMMITTEES Committee membership should reflect the range of research and clinical skills relevant to the applications that they consider and the range of disciplines involved in the case of patients with disorders in the field covered, and should include both lay members and people who reflect the interests of patients and their families. It is highly desirable that the chair or vice-chair be a lay person. Sufficient experts in clinical and research aspects of mental health should be included in the membership of committees to cover the range of research topics they are likely to have to deal with. 6.3 Resourcing of ethics committees Experience has shown that the time needed by committees to deal with applications can be very greatly reduced if applications have been processed efficiently first by an experienced and skilled administrator with the necessary training in ethical issues and the committed time to do what is required. The administrator should be able to vet all applications and seek clarification or further details from applicants whenever this seems to be needed. Ethics committees should have a properly resourced professional administration. 6.4 Application forms The ease and thoroughness of ethical scrutiny of studies is greatly influenced by the quality of the design of application forms. It should be mandatory for the purpose and procedures of the study to be described succinctly and accurately, using language that can be easily understood by committee members without either scientific or clinical training. The details should always include the nature, size and method of recruitment of the sample, funding source, payments to be made, research design (how the study will achieve its objectives), procedures or measures to be used (if non-standard they should be included with or described in the application, as appropriate) and an explicit statement of the risks and the ethical considerations. The information sheet and consent form should always be provided. The name, professional position and employing authority of the senior researcher (who must be of consultant/senior lecturer level or their equivalent) must be specified, as well as the same details for the researcher concerned with the day to day running of the study. The source of funding must be specified and details of payments to researchers and participants provided. The application must indicate how informed consent and data protection issues will be dealt with, and whether (and in which form) research findings will be fed back to participants. Attention should be paid to the design of application forms to ensure that all necessary details of the study and ethical issues are provided in a standard way. 6.5 Scientific review As noted above, ethical issues require consideration of the scientific quality of the proposed research. That need is reflected in our recommendations on committee membership (paragraph 6.2). The degree of scientific scrutiny should always be proportional to the potential risks to participants or researchers. When the scientific merits of studies have already been considered by peer review prior to seeking ethical approval, ethics committees should not normally make further suggestions on the science unless it is clear that a major issue has not been addressed. Many funding bodies, however, do not undertake peer review, so scientific quality cannot be assumed on the basis that funding is provided. 33 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS In addition, many of the major funding bodies (such as the MRC and the Wellcome Trust) require ethical review before they consider funding. As, currently, such a small proportion of applications get funded, clearly this means that ethics committees have to review many studies that never get undertaken. The rationale of funding bodies is that they would be unwilling to fund unethical research, so this has to be a prior consideration. Also, if the ethical review leads to a change in design, the scientific appraisal will be based on the wrong design. Equally, however, if peer review leads to a change in research strategy or tactics, the ethical review will have been based on an inappropriate design. There is no entirely satisfactory way out of this impasse but we accept that, unless the funding system changes, ethics committees will need to undertake some form of scientific scrutiny prior to peer review. We recommend that ethical approval should always be contingent on the science receiving peer review approval, if that is being obtained, and that it should be mandatory for applicants to inform the ethics committee of any changes in research design or procedures (including sampling), as well as any changes in the source of funding or payments to be made to researchers or participants. It is usual for studies to undergo some changes during their course, as a result of practical or scientific difficulties encountered. We recommend that it should be a routine for researchers to be asked once per year to provide details of any changes in the research, and in the research personnel, as well as of any ethical difficulties experienced. Continuation of ethical approval should be contingent on this information being provided and the changes in protocol agreed by the ethics committee. Ethical review of studies must include an appropriate degree of scientific scrutiny and continuation of ethical approval should be made contingent on the researchers providing information on any changes in design, funding or personnel involved. 6.6 Multi-centre studies Increasingly, research is based on samples from more than one hospital or clinic and on large epidemiological samples that are widely spread geographically. In the past this has posed a major problem to researchers who have had to seek separate ethical approval from multiple ethics committees, each of which uses a different style of application form, and may raise contradictory scientific or ethical issues. Multi-centre research ethics committees have been set up in the UK to obviate these difficulties (NHS Executive, 1997). There are no issues specific to research in the mental health field that apply to their operation, and we make no recommendations about their operation. It should be noted that studies involving five or more recruitment centres must go to the multicentred research ethics committees before going to the local committee. However, these were primarily set up to deal with large multi-centre randomised control trials and other clinical research presenting similar coordination issues. They appear well designed for that purpose but their operation does not map well onto large scale epidemiological studies based on non-patient samples or on samples of patients obtained through voluntary registers or membership of support groups. In these circumstances it is appropriate for the study to be considered by the local ethics committee serving the employing institution of the lead researcher. It is imperative, however, that the committee has the necessary expertise to review the study. If it does not, they should seek advice from one that does. In addition to large scale multi-centre studies, there are many more studies based on just a few collaborating clinical facilities. According to present arrangements, these still need to be considered by several separate local ethics committees. In these circumstances, we recommend that the lead review should be undertaken by the committee with the most appropriate expertise to undertake the assessment of that particular type of study. The other committees must consider any ethical issues that are specific to their clinical facility, and must have the right to raise serious ethical concerns if they consider that they were overlooked by the lead committee. Nevertheless, ordinarily, it should be expected that the same application form should be accepted by all committees, and that the recommendation of the local committee should be followed. It should also be a requirement, however, that the separate committees share and consider any expert external advice that any of the committees have obtained regarding the study or its procedures. 34 Studies of non-patient samples or samples of patients obtained from registers separate from local centres should ordinarily be considered by the appropriate local ethics committee, rather than being passed on to a multi-centre ethics committee. When research involves several centres (but below the number requiring referral to a multi-centre committee), the relevant local ethics committees should decide on which one should take the lead, with the expectation that the other committees would accept their decision unless there were some special additional considerations to be taken into account. OPERATION OF ETHICS COMMITTEES 6.7 Conflicts of interest Increasingly it is becoming standard practice to require members of all committees to make a formal declaration of potential sources of conflict at the time of joining the committee and to update these once a year. We recommend that this should be expected of all members of ethics committees. It is accepted that it is entirely proper for members to have affiliations with organisations that have interests relevant to some applications coming to the committee; what is improper is for this not to be known to other members of the committee. It should also be obligatory for members to make overt any such possible conflicts of interests in relation to individual applications, and to withdraw from the room if the conflict is felt by the member or the rest of the committee to make it inappropriate to remain present during discussions. The chairman’s ruling on this matter should be absolute. Potential conflicts concern any links (including paid or unpaid consultancies, membership, office holding and other connections) that have possible financial, lobbying or hierarchical implications. Formal declaration of potential conflicts of interest should be expected of all members of ethics committees, and if these create a possible problem in relation to individual applications, affected members should withdraw during their discussion. 35 ROYAL COLLEGE REFERENCES OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS Appelbaum, P. S. (1998) Missing the boat: competence and consent in psychiatric research. American Journal of Psychiatry, 155, 1486–1488. ––– & Grisso, T. (1995) The MacArthur Treatment Competence Study: 1. Mental-illness and competence to consent to treatment. Law & Human Behavior, 19, 105–126. Barnes, D. E., Hanauer, P., Slade, J., et al (1995) Environmental tobacco smoke. The Brown and Williamson documents. Journal of the American Medical Association, 274, 248–253. Beecher, J. K. (1966) Ethics and clinical research. New England Journal of Medicine, 274, 1354– 1360. Bero, L., Barnes, D. E., Hanauer, P., et al (1995) Lawyer control of the tobacco industry’s external research program. The Brown and Williamson documents. Journal of the American Medical Association, 274, 241–247. British Medical Association & The Law Society (1995) Assessment of Mental Capacity: Guidance for Doctors and Lawyers. London: BMA. British Paediatric Association (1992) Guidelines for the Ethical Conduct of Medical Research Involving Children. London: British Paediatric Association. Caldicott Committee (1998) Report on the Review of Patient-Identifiable Information. London: Department of Health. Choo, V. (1998) The line between research and audit. Lancet, 352, 337–338. DeMets, D. L., Pocock, S. J. & Julian, D. G. (1999) The agonising negative trend in monitoring of clinical trails. The Lancet, 354, 1983–1988. Dickert, N. & Grady, C. (1999) What’s the price of a research subject? Approaches to payment for research participation. New England Journal of Medicine, 341, 198–202. Food and Drug Administration (1999) Informed Consent: Exception for Emergency Research. http://www.fda.gov/cder/present/dia698/diafda4 Federal Policy for Protection of Human Subjects (1991) Federal Register, June 18; 56: 28012-8. Fienberg, S. E. & Resnick, D. P. (1997) Reexaming the bell curve. In Intelligence, Genes, and Success: Scientists Respond to The Bell Curve (eds B. Devlin, S. E. Fienberg, D. P. Resnick et al), pp. 3–18. New York: Copernicus. Freeman, T. B., Vawter, D. E., Leaverton, P. E., et al (1999) Use of placebo surgery in controlled trials of a cellular-based therapy for Parkinson’s disease. New England Journal of Medicine, 341, 988–992. General Medical Council (1998) Seeking Patients’ Consent: The Ethical Considerations. London: GMC. Glantz, S. A., Barnes, D. E., Bero, L., et al (1995) Looking through a keyhole at the tobacco industry: the Brown and Williamson documents. Journal of the American Medical Association, 274, 219–224. –––, Slade, J., Bero, L. A., et al (1996) The Cigarette Papers. Berkeley, California: University of California Press. Grisso, T. & Appelbaum, P. S. (1996) Values and limits of the MacArthur Treatment Competence Study. Psychology, Public Policy and Law, 2, 167–181. Hanauer, P., Slade, J., Barnes, D. E., et al (1995) Lawyer control of internal scientific research to protect against products liability lawsuits. The Brown and Williamson documents. Journal of the American Medical Association, 274, 234–240. Hilts, P. J. (1996) Smokescreen: The Truth Behind the Tobacco Industry Cover-up. Reading, Massachusetts: Addison-Wesley. Kennedy, I. (1997) Consent: Adult, Refusal of Consent, Capacity. Commentary on ReMB[1997]2 F.L.R. 426. Medical Law Review, 5, 317–325. Law Commission (1995) Mental Incapacity (Law Commission Report No. 231). London: HMSO. Macklin, R. (1999) The ethical problems with sham surgery in clinical research. New England Journal of Medicine, 341, 992–996. Medical Defence Union (1997) Consent to Treatment. London: Medical Defence Union. Medical Research Council (1992) Responsibility in Investigations of Human Participants and Material and on Personal Information. MRC Ethics Series. London: MRC. ––– (2000) Personal Information in Medical Research. MRC Ethics Series. London: MRC. ––– (2001) Human Tissue and Biological Samples for Use in Research. Operational and Ethical Guidelines. MRC Ethics Series. London: MRC. Melton, I. J. (1997) The threat to medical-records based research. New England Journal of Medicine, 337, 1466–1470. 36 National Bioethics Advisory Commission (1998) Research Involving Persons with Mental Disorders that may Affect Decisionmaking Capacity: Vol. I. Report and Recommendations of the National Bioethics Advisory Commission. Rockville, Maryland: National Bioethics Advisory Commission. NHS Executive (1997) Ethics Committee Review of Multi-centre Research: Establishment of Multi-centre Research Ethics Comittees, HSG(97)23. NHS Management Executive (1991) Local Research Ethics Committees. Health Service Guidelines. London: Department of Health. Nuffield Council on Bioethics (1993) Genetic Screening: Ethical Issues. London: Nuffield Council on Bioethics. ––– (1999) The Ethics of Clinical Research in Developing Countries. London: Nuffield Council on Bioethics. Ong, E. K. & Glantz, S. A. (2000) Tobacco industry efforts subverting International Agency for Research on Cancer’s second-hand smoke study. Lancet, 355, 1253–1259. Pappworth, M. (1967) Human Guinea Pigs: Experimentation on Man. London: Routledge. Patel, N. (1999) Getting the Evidence: Guidelines for Ethical Mental Health Research Involving Issues of ‘Race’, Ethnicity and Culture. London: Mind. Royal College of Physicians (1994) Independent ethical review of studies involving personal medical records. Report of a working group. Journal of the Royal College of Physicians of London, 28, 439–443. ––– (1996) Guidelines on the Practice of Ethics Committees in Medical Research Involving Human Subjects (3rd edn). London: The Royal College of Physicians. ––– (1999) Research based on archived information and samples. Journal of the Royal College of Physicians of London, 33, 264–266. Royal College of Psychiatrists (1990) Guidelines for Research Ethics Committees on psychiatric research involving human subjects. Psychiatric Bulletin, 14, 48–61. Slade, J., Bero, L. A., Hanauer, P., et al (1995) Nicotine and addiction. The Brown and Williamson documents. Journal of the American Medical Association, 274, 225–233. Smyth, R. L. & Weindling, A. M. (1999) Research in children: ethical and scientific aspects. Lancet, 354 (suppl. 2), 21–24. Wald, N. J., Law, M., Meade, T. M., et al (1994) Use of personal medical records for confidential research purposes. British Medical Journal, 309, 1422–1424. Walton of Detchant, Lord, Doll, R., Asscher, W., et al (1999) Consequences for research if use of anonymised patient data breaches confidentiality. British Medical Journal, 319, 1366. Wong, J. G., Clare, I. C. H., Gunn, M., et al (1999) Capacity to make health care decisions. Its importance in clinical procedures. Psychological Medicine, 29, 437–446. –––, –––, Holland, A. J., et al (2000) The capacity of people with a ‘mental disability’ to make a health care decision. Psychological Medicine, 30, 295–306. World Medical Association (1989) The Declaration of Helsinki (1964, revised 1989) The World Medical Association Handbook of Declarations. Ferney-Voltaire, France: World Medical Association. REFERENCES 37 ROYAL COLLEGE APPENDIX 1 – EXAMPLES OF POSSIBLE STANDARD OF PSYCHIATRISTS RESEARCH DESCRIPTIONS GUIDELINES: ETHICS Example of medical term Suggested alternative Analgesia Animal studies Assigned Auditory hallucinations (Brain) scan Claustrophobia Combined treatment arm Pain killer In the laboratory Put/allocated/placed Hearing voices Picture of your (brain) Fear of enclosed spaces Part of the study in which patients will receive both/all treatments Genetic material Difficulty in breathing Involve/mean Every 3 months The first treatment you had/would have Studying how common Affecting the way Treatment/care Psychiatric problems/mental ill health Feeling sick Tablets The way your body handles the drug An inactive substance Before you come into hospital Allocated by chance Treatment plan/programme Make you Stop taking part in the study DNA Dyspnoea Entail Every 3/12 First line treatment Investigating the incidence Jeopardising Management Mental illness Nausea Oral medication Pharmacokinetics Placebo Prior to your hospitalisation Randomisation Regime/Regimen Render you Terminate your participation 38 APPENDIX 2 – CHILDREN’S LEVEL OF UNDERSTANDING OF MEDICAL DECISIONS By M. Rutter The issue of children’s capacity to understand what is involved in research closely parallels the queries regarding their understanding of decisions about their own treatment. Accordingly, in this appendix, the topic is considered first in the latter context because decisions on how research consent should be dealt with ought to follow good clinical practice. Discussions about children’s consent to medical treatment tend to be dominated by the twin issues of whether children are competent to make informed decisions and whether, even if they are competent, it is right to allow them to make serious and difficult choices (Alderson & Montgomery, 1996). The questions are normally posed in this way because the really tricky legal, medical and ethical problems arise when there is a clash between the expressed views of parents and of children, and where one or other of those also clashes with professional opinion. The evidence on these points is considered further below but they do not constitute the most appropriate initial basis for discussion. Very few decisions about treatment are of the life and death variety, very few involve such stark clashes and very few have to be decided in a hurry. Accordingly, the starting point needs to be the more everyday question of whether or not, in the course of ordinary medical practice, young children should be involved in discussions about their medical problems and about how such problems should be dealt with. INDIVIDUALS’ RIGHTS TO PARTICIPATE IN HEALTH CARE DECISIONS The basic principle is an assumption that all people, of whatever age and whatever degree of handicap, should be able to be properly informed about medical matters that pertain to them and be involved in decision-making about their care and treatment. This means that the onus needs to be placed on the justification for not doing this in individual cases. That could arise either because the individual’s level of understanding was so extremely limited that it would be obviously pointless to do so, or because of evidence that it would be damaging. So far as the first possibility is concerned, everyone would accept that there is a point when it would be absurd to try to have a discussion. Thus, it would be ridiculous to try to engage a neonate in discussions about treatment, to take an extreme example. Equally, however, the same would apply to a profoundly retarded individual whose level of understanding of language was, say, below the age of 6 months. The question then becomes one of asking at what chronological or mental age children begin to have sufficient understanding to engage in a meaningful conversation about medical matters. We consider the evidence on the growth of understanding further below but, at this point, it is sufficient to note that detailed naturalistic studies of young children’s conversations in the home make it quite clear that even 3- and 4-year-old children can and do discuss matters of moment and engage in decision-making (Dunn, 1988). Obviously, the ways in which they do so, and their capacity to deal with complex matters, is very much less than that of adults, but it is far from zero. The implication is that health care professionals should be expected to talk with children, even during the preschool period, about medical matters that involve them. This needs to be done in ways that the children can understand but that are no different in principle from the exactly 39 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS comparable need to do so with respect to adults. Thus, most adults can scarcely be expected to understand all the complex considerations that go into decisions about different forms of medical treatment, or different surgical procedures, for specific conditions. It would make no sense to present the patient with the sort of technical evidence that would be taken into account by an expert in the field. On the other hand, it would be generally accepted that it is the duty of health professionals to provide the patient with as much understanding of these issues as possible and to engage them in the decision-making. Exactly the same applies in childhood. The other reason for withholding information or leaving people out of decisionmaking is that it would be harmful to them to do otherwise. Once more, it seems appropriate to start with the adult case. There was a time when some doctors would ‘protect’ their patients from the worry of knowing that they have cancer or some other life-threatening disease by concealing this information from them or giving them information that was misleadingly optimistic. The assumption seems to have been that if you did not tell people about terrible things, they would not think about them themselves. It is now obvious that is not the case. Indeed, often, people’s fantasies about what might be wrong with them and about the chances of successful treatment are worse than the reality. Rather, it has become clear that the appropriate approach is to discuss these matters honestly with patients but with a sensitivity to individual wishes on the extent to which they want to discuss matters in detail. That is, the opportunity for discussion should always be made available, and deliberate misinformation is not acceptable, but there needs to be an appreciation that there are valid individual differences between people in the extent to which they wish to be involved in detailed decision-making and in learning about all the specifics of what is entailed. The maintenance of hope and of a positive attitude is important, particularly because there is good evidence that attitudes of mind may influence the course of somatic disease. There is a parallel with parents’ desire to protect children in the occasional requests from families that their loved one (an adult) should not be told that they have cancer. It would now be accepted that although health professionals need to pay attention to what families say about patients’ sensitivity, feelings and wishes, nevertheless, the starting point has to be the rights of individuals to be properly informed and to be able to participate in decision-making. It follows that there should be a similar starting point with respect to children. The question is whether there are circumstances in which the needs of children, and the potential damage brought about by engaging them in decision-making, is of a degree that an exception should be made to this general principle that people should be informed and engaged in decision-making. Such exceptions should have a clear, well justified, basis. GROWTH IN CHILDREN’S LEVEL OF UNDERSTANDING In considering children’s level of understanding, we need to be guided by well established empirical research findings rather than by theories, either outmoded or contemporary (Rushforth, 1999). The evidence is clear-cut that people’s mental abilities, social understanding and emotional appreciation do indeed increase greatly over the course of development (Keating, 1990; Rutter & Rutter, 1993; Ceci et al, 1994a,b; Walden & Garber, 1994). Thus, at about the age of 2 years, children first develop a capacity to make inferences about the causes of events and to appreciate the psychological state of other people (Kagan, 1981). Over the next couple of years or so their ability to understand what other people are thinking increases markedly (Baron-Cohen et al, 1993). However, strategic thinking of a planful goal-oriented nature does not become well established until later childhood or early adolescence (Kail, 1990). At all ages there are marked individual differences in the extent to which children are suggestible but, on the whole, younger children are more prone to be misled by leading questions and by a wish to please adults (Ceci & Bruck, 1993; Bruck & Ceci, 1999). The growth in mental abilities continues through the teenage years (Justice, 1996). Thus, in early adolescence, young people’s thinking tends to become more abstract, multi-dimensional, self-reflective and self-aware, with a better understanding of relative concepts. They are better able to hold in mind several different dimensions of a topic at the same time, and so generate more alternatives in their decision-making. In addition, 40 they become better able to monitor their own thinking for inconsistency, for its gaps in information and for the accuracy of its logic. This greater mental sophistication that comes during the teenage years is accompanied by related developments in the ways in which young people think about themselves. During adolescence, there is a marked increase in emotional introspection, together with a growing tendency to look back with regret and to look ahead with apprehension. That is, not only do young people become increasingly able to consider the long-term consequences of their own actions, and of what happens to them, but also they tend to think about such consequences more in terms of their own sense of responsibility and better awareness of the effects of what they do on other people. These developments in intellectual capacities and emotions derive, in part, from continuing brain development (which extends into the teenage years and beyond), and, in part, from life experiences. However, it would be a mistake to view the changes as just a growth in the power of information-processing. The increase in mental abilities reflects several different features including the knowledge base, an ability to use more of the information available, more sophisticated mental planning capacities in order to decide how best to tackle decision-making and an increased flexibility in the use of mental strategies (Sternberg & Powell, 1983). The evidence that children’s understanding, and their ability to make difficult decisions, increases greatly over the age period between infancy and adulthood is overwhelming. At first sight, it would seem a straightforward matter to determine when young people’s cognitive capacity has reached a point when they are competent to take decisions on health care and medical treatment themselves without the need for parents to decide things on their behalf. Unfortunately, it is evident that several crucial features much complicate that assessment. To begin with, decision-making is influenced by both cognitive capacity and emotional understanding and these two aspects of functioning do not necessarily develop with the same timing. Also, however, there is huge individual variation both in the time taken to reach particular mental levels and in the ultimate levels attained. This is, as it were, the mental equivalent of the enormous individual variation in the age at which children acquire their permanent teeth or reach puberty. It would be misleading to make a general claim that girls reach sexual maturity at, say, 12 years, when some have their menarche at 9 years but others not until 15. The same applies to cognitive maturity. Equally, not all adults have the same level of understanding. This is apparent, for example, in the spread of IQ scores, some 2.5% have an IQ below 70 but an equal proportion have one above 130. That analogy makes it seem tempting to search for a good test for the skills involved in decision-making. Of course, a test of general intelligence does provide a rough and ready guide to the likely level of relevant mental skills, but it is highly fallible for three different reasons. First, standardised tests of children’s understanding may underestimate what children can and do achieve in more ordinary day to day situations, as well illustrated by the findings on children’s ability to ‘mentalise’ or appreciate what other people are likely to be thinking (Dunn, 1988). Second, this variation in mental performance is even more marked when people’s everyday experiences are unusual. Thus, there is much evidence of the contextspecificity of knowledge (Ceci et al, 1994a). People tend to be very much better at solving problems when they concern issues well familiar to them than when exactly the same problem is presented in an unfamiliar fashion. Third, failure on a mental task does not necessarily mean that the relevant cognitive skill is missing. If children can be helped with remembering different facets of a decision-making task, or if they can be shown how to adopt a different mental strategy, they may solve problems that are not ordinarily possible for children until a much older age (Bryant, 1974; Goswami, 1991). Much the same applies in the field of emotional understanding. Thus, quite young children express mixed feelings, but it is not until middle childhood that they gain much insight into their own emotional lives and realise when there is emotional ambivalence. Also, over the same age period, children learn a range of thinking techniques to control their emotions. But this capacity is influenced by circumstances. Thus, Harris (1989) found that children experiencing distress in hospital were less able than other children of the same age to appreciate mixed feelings. APPENDIX 2 41 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS ASSESSMENT OF COMPETENCE TO TAKE DECISIONS It follows from these considerations that any assessment of a particular child’s competence to take a specific decision regarding health care or treatment needs to be based on how they deal with that specific decision rather than on any standardised tests (although these may be useful in alerting professionals to the possibility that the child is unusually mentally advanced or delayed in comparison with others of the same age). Furthermore, the assessment needs to be based on how the child deals with the matter after discussion and help with understanding and with ways of thinking about the issues. First impressions can be misleading. But, even with the most detailed and skilled of assessments, it will still be the case that capacity needs to be considered as a graded dimension and not as something that is either present or absent. Even pre-schoolers are likely to have some appreciation of what is involved in their health care but they will have a quite limited capacity to appreciate long-term consequences and will be restricted on their capacity to balance competing considerations. WHEN, IF AT ALL, SHOULD CHILDREN BE PROTECTED FROM DECISION-MAKING? The final issue concerns the question of whether there are circumstances in which it is damaging for children to be expected to make difficult decisions. The query needs to be split into two parts. First, at least after the early pre-school years, it is never acceptable for children to be excluded totally from participating in decision-making on matters of health care that concern them. The weight given to their views should properly be influenced by the level of their understanding, but their wishes should not be disregarded as of no consequence. Second, that does not necessarily mean that children, or even young adolescents, should be expected to be the final arbiter on a serious decision. They are used to turning to parents for advice and guidance and most young people continue to do so on serious matters right through adolescence, despite rebellion on more everyday concerns such as hair style, dress and time in at night (Rutter, 1979; Rutter & Rutter, 1993). Shared decision-making will be the preferred option in most instances. Perhaps the most obvious circumstance when it is particularly damaging to force (or expect) children to take the final decision is when one parent argues for one course and the other parent presses for the opposite. Inevitably, such decisions will be felt by the child as having an element of conflict over loyalty. The closest parallel is provided by decisions over which parent should look after the child when there is a parental divorce or separation. It would be usual nowadays to seek to understand the child’s feelings and wishes and to give them considerable weight, and that ought to apply equally to health care decisions. Ordinarily, children are not, and should not be, expected to choose between their parents, but, equally, there ought to be grave hesitation before taking a decision that runs counter to a child’s firmly and consistently expressed opinion when that is judged to be based on an adequate (not necessarily complete) understanding of the issues, and when it does not appear to be the result of undue influence exerted by one or other parent. The same should apply to health care decisions. EXTRAPOLATIONS TO CAPACITY TO CONSENT TO RESEARCH 42 Several key principles that are pertinent to the capacity to consent to research participation derive from the findings on children’s development and their application to clinical decision-making. First, a child’s ability to understand constitutes a graded phenomenon and not something that appears in categorical fashion at some particular age. Even quite young children can understand some of the relevant issues and it should be a standard expectation that every effort is made to help children appreciate what is asked of them and to participate in the decision-making process in so far as they are able. Second, even with an individual child, the level of understanding is not a fixed feature. It will be influenced by the socio-emotional context, the extent to which past experiences are relevant to the particular decision, it can be increased by discussion and education and its evaluation will be much influenced by whether questions are put in an abstract or reallife familiar way. Third, although legal considerations require that categorical decisions on capacity have to be taken, it needs to be appreciated that this requirement derives from practical considerations (in situations in which people may differ on whether there should be research participation, someone’s view must prevail) and not from the underlying psychological reality. The situation parallels that in clinical decision-making. The severity of psychopathology varies in a continuous fashion but at some point a categorical decision has to be taken on whether or not to treat or whether or not to admit to hospital. Fourth, a child’s ability to understand may change over time according to alterations in mental state, increased biological maturation or as a result of new experiences. This possibility will need to influence the way in which children are dealt with over time in research participation. Fifth, because children can understand to some degree, it should require special justification to override a child’s clear and sustained objection to any research procedure that carries significant risk. Finally, children are much influenced by the views of those whom they love and respect. This means that they are likely to be influenced by their parents’ attitudes. In most circumstances, this is likely to be protective, but care needs to be taken in the unusual situation in which parents seem to be seeking to influence children against the children’s own best interests. APPENDIX 2 REFERENCES Alderson, P. & Montgomery, J. (1996) Health Care Choices: Making Decisions with Children. London: Institute for Public Policy Research. Baron-Cohen, S., Tager-Flusberg, H. & Cohen, D. (1993) Understanding Other Minds: Perspectives from Autism. Oxford: Oxford University Press. Bruck, M. & Ceci, S. J. (1999) The suggestibility of children’s memory. Annual Review of Psychology, 50, 419–439. Bryant, P. E. (1974) Perception and Understanding in Young Children. London: Methuen. Ceci, S. J. & Bruck, M. (1993) Suggestibility of the child witness: a historical review and synthesis. Psychological Bulletin, 113, 403–439. –––, Bronfenbrenner, U. & Baker-Sennett, J. G. (1994a) Cognition in and out of context: a tale of two paradigms. In Development Through Life: A Handbook for Clinicians (eds M. Rutter & D. Hay), pp. 239–259. Oxford: Blackwell Scientific. –––, Baker-Sennett, J. G. & Bronfenbrenner, U. (1994b) Psychometric and everyday intelligence: synonyms, antonyms and anonyms. In Development Through Life: A Handbook for Clinicians (eds M. Rutter & D. Hay), pp. 260–283. Oxford: Blackwell Scientific. Dunn, J. (1988) The Beginnings of Social Understanding. Oxford: Blackwell. Goswami, U. (1991) Analogical reasoning: what develops? A review of research and theory. Child Development, 62, 1–22. Harris, P. L. (1989) Children and Emotion: The Development of Psychological Understanding. Oxford: Basil Blackwell. Justice (1996) Children and Homicide: Appropriate Procedures for Juveniles in Murder and Manslaughter Cases. London: Justice. Kagan, J. (1981) The Second Year: The Emergence of Self-Awareness. Cambridge, Massachusetts: Harvard University Press. Kail, R. V. (1990) Memory Development in Children (3rd edn). San Francisco: Freeman. Keating, D. P. (1990) Adolescent thinking. In At the Threshold: The Developing Adolescent (eds S. S. Feldman & G. R. Elliott), pp. 54–89. Cambridge, Massachusetts/London: Harvard University Press. Rushforth, H. (1999) Communicating with hospitalised children: review and application of research pertaining to children’s understanding of health and illness. Journal of Child Psychology and Psychiatry, 40, 683–691. Rutter, M. (1979) Changing Youth in a Changing Society: Patterns of Adolescent Development and Disorder. London: Nuffield Provincial Hospitals Trust (1980, Cambridge, Massachusetts: Harvard University Press). ––– & Rutter, M. (1993) Developing Minds: Challenge and Continuity Across the Lifespan. Harmondsworth, Middlesex: Penguin and New York: Basic Books. Sternberg, R. J. & Powell, J. S. (1983) The development of intelligence. In Cognitive Development, Vol.3, Mussen’s Handbook of Child Psychology (eds J. H. Flavell & E. M. Markman),4th edn, pp. 341–-419. New York: Wiley. Walden, T. & Garber, J. (1994) Emotional development. In Development Through Life: A Handbook for Clinicians (eds M. Rutter & D. Hay), pp. 403–455. Oxford: Blackwell Scientific. 43 ROYAL COLLEGE APPENDIX 3 – DECISION-MAKING AND ASSESSMENT OF OF PSYCHIATRISTS RESEARCH COMPETENCE IN INDIVIDUALS WITH A LEARNING DISABILITY GUIDELINES: ETHICS By W. I. Fraser BACKGROUND CONSIDERATIONS Although the distinction between therapeutic and non-therapeutic research is becoming less tenable, this distinction has often guided ethics committees in relation to research on learning disability. In the past, people with learning disability have frequently been automatically excluded from participation in non-therapeutic research. Supporters of normalisation now generally consider this devalues people with learning disabilities. Also, researchers know this detracts from the representativeness of research when samples do not include the ‘lowest’ range of IQ distribution. A good example is provided by current research into the neurodevelopmental origins of schizophrenia, in which it is only recently that schizophrenia in individuals with learning disability have begun to be included. Ethics committees have to weigh the same benefits, discomforts and risks for individuals with learning disability as for any other group of participants, and this need applies equally to therapeutic and non-therapeutic research. People with learning disability have been excluded unthinkingly and automatically from many non-intrusive surveys that do not affect their privacy, simply because there were uncertainties about their ability to give or withhold consent. Research with persons with learning disability can be justified when: (a) it attempts to provide knowledge about the care and treatment of people with such clinical conditions; (b) it cannot be carried out without their involvement; (c) it does not expose them to more than negligible risk, is not unnecessarily invasive or restrictive and does not unduly interfere with their freedom and privacy. Minimal risk can be defined as the situation in which the probability and magnitude of harm or discomfort are no greater than those encountered in ordinary life or during the performance of routine physical or psychological examinations or tests (Council for International Organisations of Medical Sciences & World Health Organization, 1993). Research journals in learning disability now use the above as an ethics framework for publications. Researchers in learning disability, like researchers in other fields, are faced with guidelines listing questions about every project involving people with learning disability. These include: How much information is to be given to the subjects? What could prevent the subjects from understanding the information? Will the subjects have acquired appropriate information to decide freely to take part? What detail of explanation is required? (Informed consent in clinical practice has not required detailed understanding.) Information may not be sufficiently clear. It may be given too quickly or under conditions where the subject is unable to concentrate. The individual may have difficulties in understanding because of anxiety, depression and dementia on top of low intelligence. Although serious mental illness may impair understanding, it does not necessarily have this effect. A recent study by Wong et al (2000) of capacity in groups with mental illness, learning disabilities and dementia showed that capacity was significantly impaired in the learning disabled and dementia groups, but not in the mental illness group. With the exception of the dementia group, the other groups benefited from more information. In the learning disabled group, simplification of information increased the capacity to make decisions. Those with learning disabilities are particularly likely to be suggestible in their decision-making. Most people with learning disability will fail suggestibility tests and even when they pass on oral vignette tests of vulnerability, the validity of such 44 tests in real situations, where wishes to please override common sense, may be very low. They may say what they believe is expected of them. In individuals of all ages with learning disability, explanations should be in language and terms that are appropriate to the person’s stage of development. It may be helpful to use pictorial information to aid communication and, where appropriate, use should be made of augmented communication symbolics (such as BLISS) or of signing (such as by Makaton). Learning disability does not necessarily imply incompetence, and an inability to make one kind of decision does not necessarily mean a general incompetence. It is good practice to get the views of close relatives and an independent person who knows the subject (such as an advocate) but, whatever their views, the decision of the subject is paramount in most circumstances. The various approaches to the assessment of capacity in learning disability were reviewed by Wong et al (1999). Traditionally, reliance used to be placed on either the outcome of individual decision-making (capacity being determined on whether the decision met some external criterion) or on the status of the person as belonging to a class of low IQ that automatically meant a lack of competence. Both approaches have been rejected on empirical and conceptual grounds. Instead, a functional approach is now preferred (Hoggett, 1994; Arscott, 1997). This focuses on the person’s relative abilities and the extent to which these meet the demands for a particular decision-making task. As in other groups, so also for those with learning disabilities, the following are necessary: retaining and understanding information about the procedure; appreciating that the information is of personal relevance; weighing up the information to reach a decision; and communicating the decision (Appelbaum & Grisso, 1995; Grisso & Appelbaum, 1996; Law Commission, 1995). This functional approach (President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioural Research, 1983; Law Commission, 1995; Scottish Law Commission, 1995), is based on the extent of the person’s understanding, knowledge, skills and abilities to meet the demand for the task involved in making a particular decision. It is decision-making and time specific. While evidence from standardised assessments of mental states is essential background, this should not replace a specific evaluation of decision-making abilities in relation to the particular procedure. The way in which relevant information is presented to the subject is crucial. Regardless of whether or not the person has a ‘mental disability’, material seems easier to understand when it is presented in simple language and separate elements, rather than in an uninterrupted text (Grisso & Appelbaum, 1998). Consideration should be given to the possibility of improving relevant functional abilities by education, treatment or simplifying the task by presenting it in simpler language or by use of pictures or by augmented or alternative communication systems (Tymchuk et al, 1986). There is an obligation to take all practical steps to improve communication in learning disability. The status and functional approaches are usually combined so that a functional assessment is only carried out when status places the presumption of capacity in doubt. APPENDIX 3 ABILITIES RELEVANT TO DECISION-MAKING Wong et al (1999) listed the following as relevant abilities: (a) communicating a choice; (b) understanding relevant information; (c) retaining the information; (d) appreciating the purpose and significance of the information; and (e) reasoning, and rational manipulation of information to arrive at a decision (Appelbaum & Grisso, 1988; Berg et al, 1996). With respect to the fourth requirement, dealing with appreciation of the situation and its consequences, it is necessary for the person to recognise that he or she has a disorder. Todd and Shearn (1997) pointed out that carers are sometimes reluctant, for political correctness, to inform these people that they have a learning disability. The fifth requirement of handling information rationally centres on the process by which the individual reaches a decision, not its outcome. It focuses on whether the person’s decision was a rational product of his or her underlying beliefs and, in the case of people with learning disability, not simply an intention to preserve face or to please. 45 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS 46 LEARNING DISABILITY ADULTS WITHOUT CAPACITY Substitute judgement (requiring the proxy to decide which is the best estimate of a person’s choice) has been much employed in the past by practitioners in learning disability to make treatment decisions. This was in accordance with the practice accepted at the time by a responsible body of appropriately skilled medical opinion. This was most recently challenged following the admission to hospital, without using the Mental Health Act 1983, of a person who lacked capacity but was not objecting. The Court of Appeal found against Bournewood Community and Mental Health NHS Trust (L v Bournewood Community and Mental Health NHS Trust decision by the House of Lords in the appeal, 1998). The House of Lords in June 1998 overturned the Court of Appeal’s decision but the issue will undoubtedly arise again. It is being considered by the European Court of Human Rights. In Scotland (although very rarely employed) there is a court provision to appoint someone to have the power to give consent on behalf of an adult – a tutor dative. Enquiry should, therefore, be made as to whether there is a tutor dative and if there is, what is the extent of power to consent given by the appointing court. Presumably, the law would permit this to apply to research but no examples of this use are known. For any non-therapeutic procedure involving people with learning disability, more systematic assessments of what constitutes ‘best interest’ will be required. A general rule is that the capacity required should increase as the risk–benefit ratio goes down (American Psychiatric Association, 1998; Hansson, 1998; Clegg, 1999). Potential proxies show lack of agreement on health care decisions for people who lack capacity (Ouslander et al, 1989). Large differences exist among and within professional groups and carers as to the legal capacity of clients (Biesaart & Hubben, 1999). Conflicts of interest make parental caregivers and independent advocates of limited use as proxies. The most serious ethical concerns are raised by higher risk studies offering no prospect of direct benefit to incapable subjects. The Nuremberg Codes and the Declaration of Helsinki do not authorise this form of research: “It should be permitted only after vigorous ethical review or public notice and opportunity for comment”. The criteria for capacity now widely accepted in learning disability are those suggested by the Law Commission (1995) for England and Wales, adopted in the proposed Mental Incapacity Bill (Wong et al, 2000). The best example of decision-making assessment is that of Wong et al (2000), drawing on the methodology used in the MacArthur Treatment Competence Study (Grisso & Appelbaum, 1995). This comprises an information sheet providing the necessary elements of information, including: (a) the purpose of the test; (b) the nature of the procedure; (c) the risks of having the test; (d) the risk of not having the test; and (e) voluntariness – the principle of free choice. These should be written in simple language, employing a readability measure to check this, and printed in large font. Wong et al (1999) provided a useful flow chart for consent to health care interventions, indicating what is ethically and legally defensible for people with learning disability. This has value for research consent. This decision assessment to elicit valid responses of capacity to make a decision tested by Wong et al (2000) has a satisfactory inter-rater reliability. It comprises a spontaneous account, involving participants relating what in their view is a blood test, before any information disclosure, to establish a baseline. In their study, an information sheet was then presented in its entirety under two conditions: uninterrupted disclosure and elements disclosure. The sheet was read out to the individuals and given to them in writing. Participants were then asked for paraphrased recall and a recognition task was used to identify whether a series of statements matched the information. For learning disabled people, as for people with mental illness, the best understood item was the procedure, followed by the purpose, voluntariness and then risk. People with dementia, in contrast, found voluntariness less difficult than purpose. As Wong et al (1999) pointed out, participants who need support in their everyday lives are not used to considering the consequences of their decisions. Wong and colleagues are currently investigating a strategy that may make these more abstract elements more concrete, such as by using pictures. The simplification of decision-making tasks significantly increased capacity for the learning disabled by presenting information in this uninterrupted form and then by constituent elements and by amending the response to include recognition and non-verbal demonstration. Most adults with moderate disabilities who have a research project explained twice understand what the research is about and how often the researcher wishes to meet them, but less than half know they can withhold consent at any time (Arscott et al, 1998). APPENDIX 3 ASCERTAINING THE LEARNING DISABILITY PERSON’S PERSPECTIVE Advocacy organisations in learning disability, such as People First, are already guided by the Green Paper, Who Decides (Lord Chancellor’s Department, 1997). Best interest is decided by the following factors: (a) ascertainable past and present wishes and feelings of the person concerned and the factors that the person would consider, if able to do so; (b) the need to permit a person to participate as fully as possible in any decision affecting him or her; (c) the views of other persons, if appropriate and practical to consult about the person’s wishes and feelings, and what would be in his or her best interests; and (d) the purpose for which any action or decision required can be as effectively achieved in a manner least restrictive of a person’s freedom of action (i.e. an attempt has to be made to make some assessment of the preferences, hopes and values). Clearly this is a complex task, which is generally not carried out in the treatment of learning disabled persons and may well have a significant impact and different perspective for patients with backgrounds that differ from those of the researcher. The speciality of learning disability has a tradition of individuals with that condition being thought of as belonging to a dependent category, an attitude that is not value-neutral. They may even be regarded as not necessarily entitled to life (e.g. use of the severe handicap as a justification for termination of pregnancy in the Abortion Act) and less entitled to contribute to society (Edwards, 1997). Sometimes, too, they may be thought not to have a degree of ethical or moral development sufficient to enable them to take part for altruistic reasons and, therefore, not to be able to take part in non-therapeutic research. The lack of opportunity to take part is disenfranchising them and disproportionately excludes them from sharing the burdens and benefits of ordinary people (Edwards, 1997; Arscott et al, 1998; Clegg, 1998, 1999). Acknowledgements This Appendix draws heavily on the papers by Wong et al, provided by Dr. A. J. Holland, one of the authors, and I am much indebted to him for making them available at a time that was prior to publication. REFERENCES American Psychiatric Association (1998) Guidelines for assessing the decision-making capacities of potential research subjects with cognitive impairment. American Journal of Psychiatry, 155, 1649–1650. Appelbaum, P. S. & Grisso, T. (1988) Assessing patients’ capacities to consent to treatment. New England Journal of Medicine, 319, 1635–1638. ––– & ––– (1995) The MacArthur Treatment Competence Study: 1. Mental-illness and competence to consent to treatment. Law & Human Behavior, 19, 105–126. Arscott, K. (1997) Assessing the capacity of people with learning disabilities to make decisions about treatment. Tizard Learning Disability Review, 2, 17–28. –––, Dagnan, D. & Kroese, B. (1998) Consent to psychological research by people with an intellectual disability. Journal of Applied Research in Intellectual Disabilities, 11, 77–83. Berg, J.W., Appelbaum, P. S. & Grisso, T. (1996) Constructing competence: formulating standards of legal competence to make medical decisions. Rutgers Law Review, 48, 345–396. Biesaart, M. C. I. & Hubben, J. H. (1999) Incompetence in practice in health care in the Netherlands: Report of a study. Journal of Intellectual Disability Research, 43, 454–460. Clegg, J. A. (1998) Critical Issues in Clinical Practice. London: Sage. ––– (1999) Ethics in intellectual disability. Current Opinion in Psychiatry, 12, 537–541. 47 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS 48 Council for International Organisations of Medical Sciences (CIOMS) & World Health Organization (1993) International Ethical Guidelines for Biomedical Research Involving Human Subjects. Geneva: WHO. Edwards, S. D. (1997) The moral status of intellectually disabled individuals. Journal of Medicine & Philosophy, 22, 29–42. Grisso, T. & Appelbaum, P. S. (1995) Comparison of standards for assessing patients’ capacities to make treatment decisions. American Journal of Psychiatry, 152, 1033–1036. ––– & ––– (1996) Values and limits of the MacArthur Treatment Competence Study. Psychology, Public Policy and Law, 2, 167–181. ––– & ––– (1998) Assessing Competence to Consent to Treatment. Oxford: Oxford University Press. Hansson, M. O. (1998) Balancing the quality of consent. Journal of Medical Ethics, 24, 182–187. Hoggett, B. (1994) Mentally incapacitated adults and decision-making. The Law Commission’s project. In Decision-Making and Problems of Incompetence (ed. A. Grubb), pp. 27–40. Chichester: John Wiley & Sons. Law Commission (1995) Mental Incapacity (Law Commission Report No. 231). London: HMSO. Lord Chancellor’s Department (1997) Who Decides: Making Decisions on Behalf of Mentally Incapacitated Adults. A Consultation Paper issued by the Lord Chancellor’s Department. London: The Stationary Office. L v Bournewood Community and Mental Health NHS Trust decision of the House of Lords in the appeal (1998) Health Service Circular, series number 122. London: Department of Health. Ouslander, J., Tymchuk, A. & Rahbar, B. (1989) Health care decisions among elderly long-term care residents and their potential proxies. Archives of Internal Medicine, 149, 1367–1372. President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research (1983) Making Health Care Decisions. Washington DC: US Government Printing Office. Scottish Law Commission (1995) Report on Incapable Adults. Scottish Law Commission Report No. 151. Edinburgh: HMSO. Todd, S. & Shearn, J. (1997) Family dilemmas and secrets: parents’ disclosure of information to their adult offspring with learning disabilities. Disability & Society, 12, 341–366. Tymchuk, A.J., Ouslander, J.G. & Rader, N. (1986) Informing the elderly: a comparison of four methods. Journal of the American Geriatrics Society, 34, 818–822. Wong, J.G., Clare, I.C.H., Gunn, M., et al (1999) Capacity to make health care decisions. Its importance in clinical procedures. Psychological Medicine, 29, 437–446. –––, –––, Holland, A.J., et al (2000) The capacity of people with a ‘mental disability’ to make a health care decision. Psychological Medicine, 30, 295–306. APPENDIX 4 – WAIVED CONSENT FOR RESEARCH INTO ACUTE GRAVE ILLNESS, INCLUDING UNCONSCIOUS PATIENTS, UNDER EMERGENCY CONDITIONS APPENDIX 3 By J. Pickard 1. CLINICAL CARE It is generally accepted that when a patient presents acutely with a depressed level of consciousness because of injury or illness the clinician may undertake whatever treatment is necessary to ensure the patient’s life or health, without waiting to obtain consent. A note should be made in the clinical records to explain the absence of formal consent. It is good practice to involve relatives or other carers in the decision-making, but in an emergency, the desirability of this should not delay the clinician taking such actions as the best interest of the patient demands. It is important that the clinician confine himself to providing only necessary treatment (Council of Europe, 1997; Medical Defence Union, 1997). 2. NEED FOR RESEARCH INTO ACUTE GRAVE ILLNESS AND UNCONSCIOUS PATIENTS There is general agreement that research is necessary if emergency medical, surgical and neonatal care are to be improved. Some currently accepted treatments may prove to be counterproductive and new treatments require critical evaluation. This is an international view. For example, the proposed Maryland Law on research involving decisionally incapacitated individuals emphasises that research may be essential if science is to understand and ultimately combat disease of the brain, including Alzheimer’s disease, severe psychiatric disorders, severe trauma, stroke, other causes of decisional incapacity and the medical problems that are associated with these conditions and disorders (British Paediatric Association, 1992; Council of Europe, 1997; Anonymous, 1998). 3. CONSENT TO RESEARCH The General Medical Council (GMC, 1998) recommends that a practitioner should seek further advice where research involves children or adults who are not able to make a decision for themselves. The GMC emphasises that in these cases the legal position is complex or unclear and there is currently no general consensus on how to balance the possible risk and benefits for such vulnerable individuals against the public interest in conducting research. However, the GMC goes on to note that a number of public consultation exercises are underway and guidance should be sought from bodies such as the Medical Research Council (MRC) and Medical Royal Colleges, as well as the relevant research ethics committees. Such bodies generally agree that exceptions are required to the need for informed consent for research provision equivalent to those governing that of medical care in an emergency. On many, but not all, such occasions it may be impractical, or meaningless, to attempt immediately to obtain consent for a proposed research study from relatives, parents or guardians before proceeding. To require such an attempt always to be made would also inhibit much potentially valuable research. Provided, therefore, that the specific approval of a local research ethics committee has been obtained for the project overall, it would be ethical to carry out research on unconscious and decisionally incapacitated individuals including children without obtaining consent on such occasions of extreme urgency. The World Medical Association , as part of its revision of the World Medical Association (1999) Declaration of Helsinki, notes in its paragraph on waiver of consent: “When permitted by applicable law, the requirement for informed consent may be waived by the independent research ethics 49 ROYAL COLLEGE OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS committee. It may be justified in research and emergency situations in which patient-subjects of temporary or enduring loss of decisional capacity and interventions or procedures must be initiated before informed consent can be obtained from patient-subjects through legally authorised representatives. In the latter case the research ethics committee may require special procedures to protect the rights and welfare of the research subjects.” The proposed revision of the Declaration of Helsinki has attracted some controversy, but not with regard to this section (paragraph 25) (Brennan, 1999; Levine, 1999). The MRC (1998) guidelines for good clinical practice and good clinical trials state that situations do exist in which fully informed consent may not be possible (e.g. emergency settings). In these cases procedures agreed in the existing guidelines should be followed, provided a favourable opinion has been given by the appropriate independent ethics committee. Similar guidelines are provided by the Council of Europe (1997). The Food and Drug Administration (FDA, 1997) notes that, in emergency situations, when prior consent by the subject is not possible, the consent of the subject’s legally acceptable representative, if present, should be requested. When prior consent of the subject is not possible, and the subject’s legally acceptable representative is not available, enrolment of the subject should require measures described in the protocol and/or elsewhere with documents of approval/favourable opinion by the ethics committee to protect the right, safety and well-being of the subjects and ensure compliance with applicable regulatory requirements. Previously the FDA had specified that such waived consent applied only in the very restrictive circumstances of testing investigational therapies for life threatening emergency medical conditions and for whom available treatments were unproven or unsatisfactory. It added four additional safeguards or additional protection: (a) Consultation with representatives of the communities from which the subjects will be drawn. (b) Public disclosure prior to the commencement of the study sufficient to describe the study and its risks and benefits. (c) Public disclosure of sufficient information following completion of the study to apprise a community in the research to the study and its results. (d) The establishment of an independent data and safety monitoring board. However, it has been pointed out that some of the special precautions may be counterproductive (Mariner, 1995). There is a problem with defining the appropriate community for consultation. Lindley (1998) suggested that the appropriate community may be the patients and relatives who have personal experience of the particular illness. Communities should be informed that entry into placebo controlled randomised control trials offers patients, who are in the randomised placebo group, some benefits. First, they are not exposed to the risks of novel treatment and second, they have the benefit of being treated by a better-educated and interested team with better records, follow-up and ancillary treatments. 4. WHAT SHOULD BE THE MECHANISM OF WAIVED CONSENT? (a) A local or multi-centre research ethics committee needs to be convinced that the prospective subjects have a life threatening situation, available treatments are unproven or unsatisfactory and clinical research is required to determine which intervention is most beneficial. In addition, obtaining informed consent is not feasible. The research is in the patient’s best interest because the emergency necessitates intervention and the research risk is reasonable compared to the risks of existing therapy. Clearly in the context of potential treatments for head injury and stroke, for example, it is not reasonable to expect that treatment risks are minimal in relation to the standard of available treatment. Existing treatments may be 50 dangerous and have indeed proven to be so. Some treatments may be beneficial but certainly carry a risk, for example, thrombolysis for stroke and myocardial infarction. Hence it has been recommended that a better guideline would be that such a trial is ethical if the treatment is promising but unproved, provided that the potential risks are considered acceptable by the public. APPENDIX 4 (b) Rather than vague review by the community, which is already explicit in the composition of ethical committees that include lay members, the opinions of patients and their families who have personal experience of a particular condition should be sought. (c) Four tiers of decision making have been discussed by various law commissions including advanced statements, family members, patientselected proxy decision-makers and court-appointed guardians. In the absence of any of these the doctor must make the decision (Luttrell, 1997). The problem with advanced statements is that the incompetent patient has become a different person and hence there is a need for both physicians and surrogates to focus more on the incompetent patient’s current condition rather than on previous preferences (Fletcher & Spencer, 1995). (d) Much discussion centres on the best interest test and the substituted judgement test. The two tests may not be mutually exclusive and the Law Commission in 1993 recommended the use of the test based on best interest with a strong element of substituted judgement (see also Lord Chancellor’s Department, 1997). (e) The FDA (1999) have led the way in auditing the use of exceptions from informed consent for emergency research and have published the results on the internet. Patients with head injury and impaired consciousness may be unable to give properly informed consent, and in this emergency situation it may not be medically appropriate to delay the start of treatment until proxy consent can be obtained. Hence, the doctor in charge should take responsibility for entering such patients, just as he or she would take responsibility for choosing other treatments. However, the requirements of the relevant research ethics committee must be adhered to at all times. An information leaflet on the study for patients and their friends and relatives will be available in all drug packs (http://www.CRASH.ucl.ac.uk). 5. DEFERRED CONSENT It is generally agreed that the patient, the family or the guardian(s) should be informed about the research as soon as possible both for reasons of ethics and courtesy (British Paediatric Association, 1992). However, there remains discussion about the notion of ‘deferred consent’ (Mariner, 1995). The Royal College of Physicians (1996) considers that the local research ethics committee should advise on what, if anything, the patient or family should be told later. Informing the patients that they are participants in a trial, after entry, even if offering the possibility of withdrawal, may not prevent their inclusion as contributors to the data in an ‘intention to treat’ design. This does not appear to be a major ethical issue, whereas the right to withdraw from an act of involvement clearly is. Somberg (1996) noted that in his experience patients and their families were thankful to have the option to be told, and to go along with the research project as it continued or to withdraw from the project once they could be presented with the information and make a choice of their own volition. The FDA (1997) noted “The subject or the subjects legal representative should be informed about the trial as soon as possible and consent to continue and other consents as appropriate should be requested.” Deferred consent should not stand alone as a mechanism but it is simply the final step in a well-regulated mechanism of waived consent. 51 ROYAL COLLEGE REFERENCES OF PSYCHIATRISTS RESEARCH GUIDELINES: ETHICS Brennan, T. A. (1999) Proposed revisions for Declaration of Helsinki: Will they weaken the ethical principles underlying human research? New England Journal of Medicine, 341, 527– 531. British Paediatric Association (1992) Guidelines for the Ethical Conduct of Medical Research Involving Children. London: British Paediatric Association. Anonymous (1998) Research and the incompetent. Bulletin of Medical Ethics, 141, 22–24. Council of Europe (1997) Convention of Human Rights in Biomedicine. Articles 1–22. Food and Drug Administration (1997) International Conference on Harmonisation: Good Clinical Practice: Consolidated Guidelines. www.fda.gov/cder/guidance/iche6.htm. ––– (1999) Informed Consent: Exception for Emergency Research (22 June 1998). www.fda.gov/ cder/present/dia698/diafda4. Fletcher, J. C., & Spencer, E. M. (1995) Incompetent patient on the slippery slope. Lancet, 345, 271–272. General Medical Council (1998) Seeking Patients’ Consent: The Ethical Considerations. London: GMC. Levine, R. J. (1999) The need to revise the Declaration of Helsinki. New England Journal of Medicine, 341, 531–534. Lindley, R. I. (1998) Thrombolytic treatment for acute ischaemic stroke: consent can be ethical. British Medical Journal, 316, 1005–1007. Lord Chancellor’s Department (1997) Who Decides: Making Decisions on Behalf of Mentally Incapacitated Adults. A Consultation Paper issued by the Lord Chancellor’s Department. London: The Stationary Office. Law Commission (1993) Mentally Incapacitated Adults and Decision-Making: A New Jurisdiction. Consultation Paper No. 128. London: Stationery Office. Luttrell, S. (1997) Making decisions about medical treatment for mentally incapable adults in the UK. Lancet, 350, 950–953. Mariner, W. K. (1995) Research and emergency care without consent: new proposed FDA rules. Lancet, 346, 1505–1506. Medical Defence Union (1997) Consent to Treatment. London: Medical Defence Union. Medical Research Council (1998) Guidelines for Good Clinical Practice in Clinical Trials. Clinical Trials Series. London: MRC. Royal College of Physicians (1996) Guidelines on the Practice of Ethics Committees in Medical Research Involving Human Subjects (3rd edn). London: The Royal College of Physicians. Somberg, J. C. (1996) Research and emergency care without consent: New proposed FDA rules. Lancet, 347, 475–476. World Medical Association (1999) Proposed revision of the World Medical Association Declaration of Helsinki (WMA document:17.C/Rev 1/98). Ferney-Voltaire, France: World Medical Association. 52