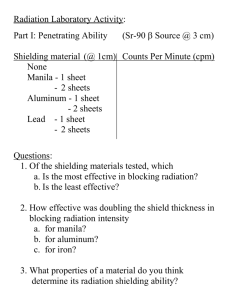
The Shielding of Radiographic Facilities at Diagnostic Energies
advertisement

The Shielding of Radiographic Facilities at Diagnostic
Energies
1.
Preface
2.
Introduction
2.1.
Scope of this report.
2.2.
Definition of Dose
2.3.
Design criteria.
2.4.
Sources of radiation
2.5.
Occupancy Factors
2.6.
Use of reference doses.
2.7.
Room Layouts
3.
Building Materials
4.
Dealing with secondary radiation
4.1.
Leakage Radiation
4.2.
Scattered Radiation
5.
Transmission through building materials
6.
Assessment of shielding
7.
Methodologies and worked examples
7.1.
Radiographic facilities
7.2.
Mammographic facilities
7.3.
R&F
7.4.
C Arm
7.5.
CT
7.6.
Dental
7.7.
Mobile
7.8.
Bone Densitometry
8.
Appendix
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
1
2 INTRODUCTION
2.1 Scope Of This Report
This will be a small section outlining what the aims of the report are and how things
are structured.
2.2 Definition of Dose
When using dose limitation and calculating shielding requirements, it is important to
be clear about what is meant by the term ‘dose’. The constraint refers to the effective
dose to the person who may be irradiated. However, this report considers the need to
shield the individual from radiations which are generally measured in terms of air
kerma. It should also be recognised that individual doses, as recorded on a personal
dose monitor, are assessed in terms of the operational quantity, personal dose
equivalent, Hp(d). Hp(d). is assessed at depths (d) of 0.07 and 10 mm.
The relationship between the derived quantities and air kerma is complex, depending
on radiation spectrum, and, in the case of effective dose, distribution of photon fluence
and the posture of the exposed individual. In fact, whilst air kerma represents a
significant overestimate of effective dose due to self shielding within the body it is
actually less than Hp(10) by 20 to 70% in the energy range used for diagnostic
radiology,
It is neither practical nor realistic to use effective dose when calculating shielding
requirements. All calculations in the report are therefore based on air kerma which,
to retain clarity, is expressed in units of mGy and µGy.
2.3
Design Criteria
The Ionising Radiations Regulations 1999 require that work involving exposure to
external radiations should be performed in rooms which are provided with adequate
shielding. If there is public access to the surrounding area or access is permitted to
employees who are not directly involved in the work, the shielding should be designed
to reduce dose rates to the lowest level that is reasonably practicable. It is therefore
necessary to formulate design criteria to ensure that this requirement is met.
A design limit based on the annual dose limit for members of the public (1 mSv) does
not comply with the needs of the legislation and certainly does not represent an ‘as
low as reasonably practicable’ (ALARP) solution.
There is considerable weight of advice suggesting that dose optimisation procedures
can be performed by the adoption of constraints. However, the legislative framework
is not prescriptive as to the actual value of the constraint to be applied.
In their advice following the publication of ICRP Report 60, the NRPB recommended
that the constraint on optimisation for a single source of radiation should not exceed
30% of the dose limit, in this case 0.3 mSv per annum (NRPB 1993 a, b). They also
emphasise that the introduction of dose constraints does not replace the requirement
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
2
on operators to optimise their use of sources or their management of practices to
ensure that exposures to members of the public are kept as low as reasonably
achievable.
Dose constraints, therefore, represent an upper bound on the outcome of any
optimisation procedure. However, there is also an acceptance that on-site exposures
to members of the public should not be assessed in terms of either continuous
occupancy or exposure. In terms of shielding, therefore, the application of the dose
constraint must be made using realistic assumptions.
The Working Party considered the application of alternatives to the 0.3 mSv per
annum dose constraint as recommended by NRPB. One such alternative was to base
the criterion on the minimum amount of radiation detectable by a personal radiation
monitor. It can be argued that such an approach may represent an ALARP solution.
However, this concept was rejected because of its arbitrary nature, given for example
the potential for changes in the detection limits of radiation monitors.
The conclusion of the Working Party was that any design would have to be based on
the dose limit for members of the public of 1mSv per annum and that the principle of
optimisation left no alternative but to utilise the concept of a dose constraint of 30%.
The ALARP design criterion for all examples was therefore chosen as 0.3 mSv per
annum. However, it should be stressed that in order to use this criterion effectively, it
is essential that realistic allowances be made for mitigating factors such as
occupancy.
In designing shielding one further dose constraint may need to be considered. Film
may be stored in a room adjacent to the x-ray room and some attention may need to
be given to inadvertent blackening of unexposed film. Film itself is relatively
insensitive to radiation requiring doses in excess of about 10 µGy to cause any
significant increase in fog. The period of storage in the department may be several
months so that it is prudent to aim to restrict doses further in those areas where long
term film store is planned and an annual design limit of 30 µGy (?100µGy) is
recommended.
Film in cassette is much more sensitive. By definition, exposure of 400 speed film to
2.5 µGy will produce a density of 1.0 above base plus fog and perceptible fog will be
produced at a dose which is one-tenth of this. In a busy department it is unlikely that
a film cassette will remain unused for more than one day which means that shielding
should be designed to reduce the dose to 0.25 µGy per day or 60 µGy per year
based on a five day week. This only applies to those areas where film cassettes are
to be kept and is of most significance when considering the specification of the screen
in radiography or R&F rooms.
2.4 Sources of Radiation.
The three sources of radiation which need to be considered in any examination of the
shielding problem can be grouped into two distinct types, primary and secondary
radiation. Secondary radiation has two components, scatter and leakage. The three
sources are briefly discussed below.
Primary Radiation.
The primary beam consists of the spectrum of radiation emitted by the x-ray tube prior
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
3
to any interaction with the patient, grid, table, image intensifier etc. The fluence of the
primary beam will be several orders of magnitude greater than that of either of the
secondary radiations discussed below.
In the majority of all radiography, the primary beam will be collimated so that the entire
beam interacts with the patient. Exceptions include extremity radiography and are
confined to low kVp, low mAs exposures..
Interactions within the patient results in considerable attenuation of the primary
radiation. Whilst typical entrance doses are of the order of mGy, exit doses are
measured in µGy. The exit beam is however considerably more penetrating than the
entrance beam. Take the simple example of an 85 kVp constant potential primary
beam with a total filtration of 3.5 mm Al. The half value layer of this radiation is 3.66
mm Al and it has an effective energy of 47 keV. After passing through 16 cm of tissue
equivalent material and 2 cm of bone, its fluence is reduced by a factor of
approximately 330, but the exit beam has an effective energy of 62 keV and an HVL
of 8.93 mm Al.
Scattered Radiation.
Scattered radiation is inevitable in diagnostic radiology and is a direct result of the
Compton effect. The fluence of scattered radiation depends on the volume of the
patient irradiated, the spectrum of the primary beam and the field size employed.
Both the fluence and quality of the scattered radiation are dependent on angle at
which they are measured. A simple generalisation is that the scattered kerma is
between 10-5 and 10-6 of the incident kerma per cm2 of the incident beam.
Figure 2.1 shows data measured by the working party indicating how the scatter
kerma varies with angle for three different accelerating potentials. This data is
consistent with other published data used in section 4.2 (Williams 1996) Figure 2.2
shows how the HVL, (i.e. beam quality) varies with angle of scatter for an 85kVp
primary beam incident on the pelvis of a rando phantom. The primary beam has a
constant wave form and a half value layer of 3.7 mm Al. It will be seen from the figure
that for angles below approximately 120 degrees, the scattered radiation will be
harder than the primary radiation.
Leakage Radiation.
Leakage radiation arises because x-rays are emiited in all directions by the target.
The outer shell of the tube housing is generally constructed of a light alloy with
adequate mechanical properties. Evidently, such an alloy will not absorb enough of
the radiation to reduce the kerma of the unwanted radiation to the legal maximum.
The housing is therefore lined with lead where appropriate. Any radiation transmitted
through this protective shield is termed leakage radiation. Manufacturers often protect
tubes well beyond the legal minimum with the possible exception of those used in
mobile radiography, where weight is especially important. Because it generally
passes through two or more mm of lead, leakage radiation will be considerably
harder than radiation in the primary beam.
Leakage is usually defined at the maximum operating potential of an x-ray tube /
generator combination and is specified at the maximum continuous tube current
possible at that potential (the leakage technique factors). Consider the example of a
constant potential x-ray tube with an inherent filtration of 1.2 mm Al and leakage
technique factors of 3mA at 150 kVp. To reduce the leakage radiation to the legal
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
4
maximum of 1mGy at 1 metre in 1 hour requires the addition of between 2.1 and 2.5
mm of lead. As a result of the hardening effect of the lead the HVL of the 150 kVp
leakage radiation will be of the order of 14 mm Al. However, with the exception of
high kVp chest techniques, where mAs values are in any event low, the majority of
conventional radiography is carried out at less than 100 kVp. The measureable
leakage will therefore be a lot lower than the legally defined maximum. For example,
assume that the tube housing has indeed been shielded as required by the above
example and that 1mGy is measurable at 1 metre at 150 kVp. At 80 kVp the leakage
radiation will have an HVL of about 12 mm Al. However, the kerma of the leakage
radiation will be of the order of 14 µGy, i.e. it will be reduced by a factor of about 70.
Variation of scatter factor with scattering angle
scatter factor (uGy/(Gy.cm^2))
9
8
7
6
5
4
3
2
1
0
0
20
40
60
80
100
120
140
160
scattering angle
Figure 2.1 Variation of scatter factor with scattering angle
. _____ 105 kVp ------- 85 kVp ......... 50 kVp.
HVL in mm of Al
HVL variation with angle of scatter
6.5
6
5.5
5
4.5
4
3.5
3
2.5
0
50
100
150
angle of scatter
Figure 2.2 Variation of HVL with angle of scatter.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
5
2.5 Occupancy factors
As stated in 2.2 above, the application of the dose constraint must be made using
realistic assumptions regarding the occupancy of areas which are relevant in terms of
the shielding problem. To be realistic, the occupancy factor for an area should not be
considered as being an indication of the time during which it is occuppied by a
generic group of people (such as patients in a waiting room). Instead, it is the
fraction of time spent by the single person who is there the longest. In this context, it
is most likely that the critical groups for shielding purposes will not be patients or
patients' visitors but non radiation workers employed by the hospital. Given this
assumption, the occupancy factor is best defined as being the fraction of an 8 -hour
day or 2000 hour year for which a particular area is occupied by a single person.
NCRP 49 contains examples of suggested occupancy factors and Dixon (1997) has
made more recent suggestions. For ease of reference, extracts from both sets of data
are reproduced in table 2.1. The data in the table do not represent hard and fast
requirements for occupancy factors; rather they are for indicative purposes only and
are intended for use only when no realistic data is available. It will be noted that the
minimum occupancy factor in the table is 1/40. This is a result of a US requirement
that persons who are not occupationally exposed should not, on average, receive
more than 2mR (20 µGy) from any one source in any one week. It is not
recommended that either set of occupancy factors in table 2.1 be used without serious
consideration being given to the specific task in hand. Rather, it is considered that a
more appropriate course of action is to make an informed assessment of the particular
installation being considered. The assessment should be made in terms of the 0.3
mSv constraint and should involve detailed appraisal of available architectural
drawings. The drawings consulted should not only be of the room to be shielded itself,
but should also encompass the surrounding area.
Whilst making such an assessment, it is important to bear in mind the fact that the use
to which a particular room is put may change with time. It is also important to
consider all of the surrounding rooms, not just those adjacent to the area being
shielded. For example, although a corridor may have low occupancy, an office
accross the corridor may be occupied on a full time basis and this must be taken into
account when specifying the construction of the corridor wall.
Above : The Americans have a max of 2mR per week hence 1/40. Do we have a
basis for a minimum occupancy factor ?
2. 6 Estimating workload : use of reference doses and other
data.
A prerequisite to designing shielding for any x-ray facility is a knowledge of the use to
which the room is going to be put and of the number of patients that are expected to
be imaged in a year. This information will allow estimates of workload to be made.
Without doubt, the best estimates of workload are those which take into accouint local
practice, rather than generic figures which represent 'busy departments', 'DGH
departments' and so on. Accordingly, whichever technique is adopted for estimating
shielding requirements, the recommendation made in this publication is that the
design be based on workload data extracted from audit of present practice.
For example, in much of this report it is recommended that DAP is used as the
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
6
measure of workload. In the UK most fluoroscopy sets have dose-area product (DAP)
meters fitted . They are also becoming increasingly common on fixed radiographic
units. In addition, most physicists who are involved in shielding calculations will have
been involved in patient dose audits and will have their own data. It is therefore
relatively simple to estimate total DAP from the projected clinical workload of the
proposed x-ray facility. Similarly the number of CT slices performed in any one year
should be easily accessible in any site where there is a existing CT facility
If workload cannot be extracted from locally available data, for example in the case of
the implementation of a new technique, then there are several alternatives open to the
person making the calculation. For example, DAP values have been published for
some common examinations(ref) and for high dose interventional procedures (ref)
and are reproduced at appropriate points in this publication. Alternatively, and
probably more conservatively, there are the reference doses produced by the NRPB
following their 1984 survey (NRPB 1984) and adopted by the CEC. More up to date
information is available such as the 1995 review of doses to patients undergoing
medical examinations in the UK (NRPB 1995). . Paediatric data can be found in the
CEC guidelines on quality criteria in paediatric radiography (CEC 1996) CT reference
levels ?? CEC CT quality criteria ??
New NRPB report on trends in radiography etc. One assumes we can include data
from this publication when it comes out
2.7 Room Layout
The official UK guidance on the design of radiological facilities ({Scottish} Health
Building Note 6) suggests that general, specialised (including angiographic) and CT xray rooms should be designed to a minimum dimension of 38 m2 . No specific
recommendation is given for mammography facilities. It is accepted that these
recommended dimensions do not necessarily reflect the situation encountered in
practice, where rooms may be considerably smaller. Nevertheless given that there is
no other available recommendation, the majority of examples in this document will be
based on x-ray rooms having a floor area of 38m2.
References
CEC 1996 European guidelines guidelines on quality criteria for diagnostic
radiographic images in paediatrics. Euopean Commission , Luxembourg.
Dixon RL 1997. Application of new concepts for radaiation shielding of medical
diagnostic x-ray facilities. Presented at RSNA Chicago, November, 1997.
National Council on Radiation Protection and Measurements (1976) Structural
shielding design and evaluation for medical use of x rays and gamma rays of energies
up to 10 MeV. NCRP Report No 49
NRPB 1984 A National survey of doses to patients undergoing a selection of routine
x-ray examinations in UK hospitals.
NRPB 1993 a
NRPB 1993 b
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
7
NRPB (1995) Doses to patients undergoing medical examinations in the UK - 1995
review. NRPB report R-289 , NRPB Chilton, Oxfordshire
Scottish Health Building Note 6.Radiology Department. The Scottish Office 1994
Williams JR (1996) Scatter dose estimation based on dose-area product and the
specification of radiation barriers. Br J Radiol, 69, 1032-7.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
8
Table 2.1 Some suggestions for occupancy factors when no other data is available.
LOCATION
T Dixon
T NCRP49
1
1
1
-
Employee Rest Area
1
1
Film Reading Area
1
-
Laundry
1
-
Nuclear Medicine Scanning Room
1
1
Offices, shops, living quarters, children’s indoor play areas,
occupied space in nearby buildings
1
1
Ultrasound Scanning Room
1
-
X-ray Control Room
1
1
Barium Kitchen
1/2
-
Cafeterias
1/2
-
Kitchens
1/2
-
Nurses stations
1/2
1
Patient Dressing Rooms
1/2
-
Patient Examination and Treatment rooms
1/2
-
Corridors
1/8
1/4
1/8
-
Patient rooms
1/8
-
Toilets or bathrooms
1/8
1/16
Outdoor areas with seating
1/20
-
Storage rooms
1/20
-
Unattended vending areas
1/20
-
Attics
1/40
-
Outdoor areas with only transient pedestrian or vehicular traffic
1/40
1/16
Patient Dressing room
1/40
-
Stairways
1/40
1/16
Unattended elevators
1/40
-
Unattended parking lots
1/40
1/4
Unattended waiting rooms
1/40
1/16
Vehicular drop off areas (unattended)
1/40
1/16
Adjacent x-ray room
Attended waiting room
c
Employee lounge
b
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
9
3 Building Materials
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
10
4 Dealing With Secondary Radiation
Secondary radiation comprises of a scatter component and a leakage component.
Both components must be taken into account when considering the transmission of
secondary radiation. It is often assumed that the scattered radiation will have the
same transmission properties as the primary beam whilst the leakage component will
be harder. As exemplified in section 2.4, the first assumption will only be true at
specific scattering angles.
One approach which has been used to allow for the two types of secondary radiation
is that of NCRP 49 and is based on work done in the 1950s. The foundation of the
method is that the contribution of leakage and scattered radiation can be assessed
separately and barrier requirements for each determined independently. The larger of
the two is taken to be the final result, unless they have the same magnitude, in which
case the ‘add one half value layer’ approach is adopted. This concept is significantly
flawed as has been pointed out by several authors (Archer 1983, Simpkin 1987,
Simpkin 1998).
4.1 Leakage Radiation
In the traditional treatment of leakage radiation, it is usual to assume that it is all
generated at the maximum potential of the generator / tube combination. This can
lead to extremely conservative design parameters given that much radiography is
performed at potentials below 100 kVp whilst leakage parameters are frequently
specified at 150 kVp. Simpkin and Dixon (1998) have reworked the issue of the
transmission of secondary radiation to take this fact into account. In doing so, they
have demonstrated that that the NCRP49 approach to leakage radiation can result in
solutions which are up to 8300 times too conservative.
Table 2.1 shows data extracted from the work of Simpkin and Dixon and
demonstrates the ratio of leakage to scatter at 90 degrees for a range of accelerating
potentials. Figure 2.1 is a graph showing this ratio plotted against the kVp. The data
are for a field size of 1000 cm2 and are specified at 1 metre from the sources of the
scatter and leakage. The assumption is also made that protection against leakage
radiation is only sufficient to ensure an air kerma of 1 mGy/hour at 1 metre with
leakage factors of 150 kVp and 3.3 mA. As has been pointed out previously the
majority of x-ray tubes have more protection than this in place.
Even making this conservative assumption it is evident that there will be considerably
less leakage radiation than scatter at commonly used energies. Consequently, in this
publication the ‘add one half value layer’ approach is rejected. Instead, secondary
radiation transmission curves which take into account the variation of leakage
radiation with kilovoltage are provided. See section 5.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
11
4.2
ASSESSMENT OF SCATTER DOSE
Scatter dose is a function of kVp, scattering angle, entrance surface dose, and the
area of the x-ray beam. This principle was the basis of the standard equation used for
scatter dose calculation given in NCRP Report 49 (NCRP 1976). This equation can
be written as:
K s = a ⋅ Ku .
F
400
(4.2.1)
in which Ks is the scatter air kerma at 1 m, Ku is the kerma free in air at the beam entry
point, F cm2 is the x-ray beam area at the image receptor and a is an experimentally
determined constant which is a function of kV and scattering angle. Values for a
given in NCRP 49 were based on data from Trout and Kelley (1972).
More recently, Williams (1996) proposed that DAP be used for scatter dose estimation
DAP meters are calibrated in terms of area-kerma product which is essentially the
same as Ku.F in equation 4.2.1. The only difference is that F is defined at the image
receptor and not at the position at which air kerma is specified. Williams measured
scatter dose as a function of angle and kV. He defined the scatter factor, S, as:
S=
Ks
DAP
(4.2.2)
Experimental values of S are plotted as a function of angle for a range of kVps in
Figure 4.2.1. It can be approximated by the equation:
S = (a ⋅ θ 4 + b ⋅ θ 3 + c ⋅ θ 2 + d ⋅ θ + e)∗ (( kV − 85)∗ f + 1)
(4.2.3)
for which the fitting constants are given in Table 1.
It is recommended that where possible, scatter dose is calculated from DAP using the
scatter factor given by equation 3. The examples in this report follow this suggestion.
Where it is not possible to do so, for example, in mammography, other methods of
deriving scatter dose are presented.
It is important to note that for a surface parallel to the central axis of the x-ray beam, it
can be shown that the maximum scatter dose is at an angle of 117° . This is the most
common geometry for shielding calculations on room walls. It corresponds to vertically
directed x-ray beams and to non-vertical beams when the axis of rotation from the
vertical is perpendicular to the wall. This generally applies to tilting tables and to
chest radiography, for example. With this geometry it can be shown that the
maximum wall scatter (Smax) at 1 m is given by:
Smax = (0.031 kV + 2.5) µGy (Gy.cm2)-1
(4.2.4)
For distances greater than 1 m, the inverse square law can be applied.
It should be noted that scatter factors were also assessed by Simpkin and Dixon
(1998). They used Trout and Kelley’s original data with certain modifications. In
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
12
particular they changed the low kV (50 and 70 kV) data which were originally
measured in x-ray beams with very low filtration. The data were modified on the basis
of measurements by Dixon (1994) for one scattering angle (90° ). In their re-analysis
of Trout and Kelley’s data, Simpkin and Dixon adopted a more conservative method
for dealing with the variations in scatter due to variations in scatter path length in the
phantom arising from differences in field area and the position of the beam centre.
The revised scatter factors (a’) were normalised to 1 cm2 rather than to a 400 cm2
beam, i.e. a ' = a
400 .
Their data may be compared with that used here. Figure 4.2. 2 shows the scatter
factors at 85 kV. It can be seen that, although there is good agreement between 90°
and 120° , the shape of the curves is very different. The ratio of maximum to minimum
scatter factor is 3.7 and 1.5 as assessed by Williams and Simpkin & Dixon
respectively
References
Archer BR , Thorny JI, Bushong SC. (1983) Diagnostic x-ray shielding design based
on an empirical model of photon attenuation. Health Physics 44 , 507-517.
Dixon RL (1994) On the primary barrier in diagnostic x-ray shielding. Med Phys, 21,
1785-93.
Hart D, Jones DG and Wall BF (1994) Estimation of effective dose in diagnostic
radiology from entrance surface dose and dose-area product measurements. NRPB
Report R262.
Hart D, Hillier MC, Wall BF, Shrimpton PC and Bungay D (1996) Dose to patients
from medical x-ray examinations in the UK - 1995 review. NRPB Report R289.
Legare JM, Carrieres, PE, Manseau A et al. (1977) Blindage contre les grands
champs de rayons x primaires et diffuse des appareils triphase au moyen de
panneaux de verre de gypse et de plomb acoustique. Radioprotection 13 79-95
National Council on Radiation Protection and Measurements (1976) Structural
shielding design and evaluation for medical use of x rays and gamma rays of energies
up to 10 MeV. NCRP Report No 49.
Simpkin DJ and Dixon RL (1998) Secondary radiation shielding barriers for diagnostic
x-ray facilities: scatter and leakage revisited. Health Physics, 74, 350-65.
Trout ED and Kelley JP (1972) Scattered radiation from a tissue-equivalent phantom
for x-rays from 50 to 300 kVp. Radiology, 104, 161-9.
Williams JR (1996) Scatter dose estimation based on dose-area product and the
specification of radiation barriers. Br J Radiol, 69, 1032-7.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
13
kVp
50
70
100
125
150
Table 4.1
angle.
Ratio of scatter to leakage
3.45 x108
2 x 104
22.6
14.6
13.5
Ratio of scattered to leakage radiation at a 90 degree scattering
a
b
c
d
e
f
Table 4.2
-1.042 x 10-7
-5
3.265 x 10
-3
-2.751 x 10
-2
8.371 x 10
1.578
5.987 x 10-3
Factors required for the calculation of the scatter factor, S, from kV and
scattering angle using equation 3. These data were derived from
measured values over a kV range of 50 to 125 kV and scattering
angles between 30° and 150° .
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
14
1.00E+09
1.00E+08
1.00E+07
Ratio
1.00E+06
1.00E+05
1.00E+04
1.00E+03
1.00E+02
1.00E+01
1.00E+00
40
60
80
100
120
140
160
kVp
Figure 4.1 The ratio of scatterd to leakage radiation at 90 degree scattering angle.
Scatter factor, S
2 -1
µGy.(Gy.cm )
12
125 kV
100 kV
85 kV
70 kV
50 kV
10
8
6
4
2
0
0
30
60
90
120
150
180
Angle of scatter
Figure 4.2
Variation of scatter with angle from Williams (1996)
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
15
Scatter factor µGy/(cGy.cm 2)
10
9
Williams
8
Simpkin & Dixon
7
6
5
4
3
2
1
0
0
Figure 4.3
30
60
90
120
Scatter angle
150
180
Comparison of scatter factors at 85 kV from Williams (1996) and
Simpkin and Dixon (1998)
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
16
5. Transmission of X-rays through Shielding Materials
5.1 Unattenuated Primary Radiation
The most commonly available publications in the UK containing information which
Medical Physicists can use to derive the characteristics of shielding materials are
HPA Report 41 (HPA 1984) and the Radiological Protection Handbook (HMSO 1971).
The first was published in 1984 and the second in 1971; both are now out of print.
Another potential reference source is the publication NCRP 49 (NCRP 1976) Much of
the transmission data in all three sources is based on single phase measurements or
was derived under narrow beam conditions and can therefore be discounted for use in
a pragmatic situation..
In 1983, Archer et al (1983) developed an empirical model (equation 1) to describe
the broad beam attenuation of x-rays through a material provided that the parameters
α, β, λ could be determined for the particular medium.
β
β
B = 1 + exp. (αλx ) −
α
α
−
1
λ
5.1)
.
In the above equation, B is the broad beam transmission, x is the thickness of material
and α, β, λ are the fitting parameters.
The equation can be inverted to enable the calculation of the amount
required to provide the desired transmission thus :
−λ β
1 B + α
x=
ln
αλ 1 + β
α
material
5.2)
Work by Archer (1994), Rossi et al (1991) , Simpkin (1995), Christensen and
Sayeg(1979) amongst others has resulted in a body of data for three phase and
constant potential transmission through a variety of materials. based on empirical
measurement and theoretical modeling. As a result the parameters α, β, λ have also
been determined for these materials. Simpkin (1995) has published a compendium of
available data and has also demonstrated how relatively simple techniques can be
used to fit α, β and λ to experimentally obtained transmission measurements.
Tsalaffoutas et al (1998) have recently applied this procedure to an aerated concrete
building material. The working party have done the same for barium plaster using
data supplied by the manufacturer, British Gypsum (1991). Table 5.1 gives fitting
parameters for a selection of materials at representative constant potential energies.
A more comprehensive collation of fitting parameters can be found in Simpkin (1995).
Equation 5.2 has been used to predict transmission values for a selection of
commonly used shielding materials at differing kVps using the available data. Table
5.2 shows the density assumed for each material. Figures 5.1 and 5.2 show derived
transmission curves through lead and concrete, for radiation arising from a Tungsten
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
17
target at 50, 60, 75, 90 and 120 kVp. Also shown in these figures are transmission
curves for 30 kVp Mo/Mo radiation. Figure 5.3 shows transmission curves for Ba
plaster at 50, 75 100 and 125 kVp . Figure 5.4 shows transmission through wood
and gypsum for 30 kVp Mo/Mo radiation. All data are plotted for B=1 to B=10-6.
Figure 5.5 demonstrates a plot of thickness vs transmission for lead, concrete,
barium plaster , plate glass, steel wood and gypsum at 75kVp. Such curves are
instructive and can be generated at other potentials using the coefficients provided in
table 5.2
Inspection of curves like those in figure 5.5 shows that there is an obvious correlation
between the transmission provided by differing materials at any accelerating potential.
It is possible to fit polynomial equations to the data and thus relate the quantities of
the different materials required to provide the same transmission. Table 5.3 goves the
coefficients of cubic polynomial fits using thickness of lead as the dependent variable
and concrete, glass, gypsum, steel, wood and barium plaster as the independent
variables. The polynomial fit was applied over transmission values 1 to 10-8. Also
shown (Table 5.4) are the coefficients where concrete thickness is the independent
variable and equivalent thickness of lead is the dependent variable. The cubic
polynomials fitted have no intercept and are of the form y = b1x + b2x2 +b3x3 . A cubic
fit was performed in all cases for consistency even though in some cases a linear fit
provided almost as good a result. The tendency towards linearity is increasingly
pronounced as the kVp increases In all cases r2>0.999. A typical example is given in
figure 5.6 which shows the equivalence between concrete and lead at 60 kVp.
The coefficients in tables 5.1, 5.3 and 5.4 can easily be incorporated into spread
sheets and used to evaluate either the required thicness or the equivalent thickness'
of material. Two example are given below :
1) Suppose that calculation had shown that the requisite shielding could be provided
by 2.2 mm lead at 75 kVp.
Use of Table 5.3 shows that the same degree of
protection can be obtained using
87.63 × 2.2 + 1.1509 × 2.2 × 2.2 + .1787 × 2.2 × 2.2 × 2.2 = 200.25 mm concrete
2) Suppose that calculation showed that a transmission factor of 0.002 was required
to achieve the desired specification and that the majority of radiography in the room
was carried out at 75 kVp or lower. Equation 5.2 shows that the required shielding
can be provided with 6 mm Ba plaster.
When considering equivalent thickness of concrete, it is worth recalling that HPA
report 41(1984) points out that in the UK ordinary concrete has a density of 2200 kg m
-3
whilst in the US the standard specification has a density of 2350 kg m -3 . The data
presented here is based on the US specification but, provided that the material is not
loaded with granite or other aggregates, the data can just be scaled appropriately. So
for example, if the transmission curves and / or equations presented here are used to
derive a desired thickness of concrete, and the actual material to be used has a
density of 2200 kg m-3, then the answer should be scaled by a factor of 2.35/2.2.
5.2 Unattenuated primary radiation
As outlined in section 2 of this report, primary radiation is significantly attenuated and
hardened following transmisssion through a patient. It is not unreasonable and also
conservative to treat this radiation as being of constant HVL. It is easy to use equation
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
18
5.1 to show that
1 β
ln(B) = −αx − ln1 +
λ α
5.3)
As x becomes large the second term in this equation becomes increasingly
insignificant and the transmission equation tends to a simple exponential with a
constant equal to α Thus, one can treat the primary, attenuated radiation as having a
constant (or assymptotic) HVL of (ln 2)/α. The final column of table 5.1 shows typical
high attenuation HVLs calculated in this manner. The validity of this approach can be
seen by inspecting the transmission curves (figs 5.1 - 5.4). It can be seen that for
transmission less than 10-3 the form of the logarithmic plot is effectively linear. In
cases such a chest radiography, where the transmiussion through the patient is such
(< 10-3) that the 'high attenuation' assumption is probably not valid, the result of
adopting it will be a conservative design since the true transmitted beam will not be as
prenetrating as that modelled.
5.3 Secondary Radiation
5.3.1 Radiography.
Simpkin and Dixon (1998) have used equation 5.1 above and applied it to the
secondary radiation problem. They have made the simplifying assumption that the
scattered and primary beams have the same attenuation. Values of α, β, and λ have
been derived for secondary radiation transmitted through various media at a 90
degree angle and for a field size of 1000 cm2 at an FFD of 1m. The leakage
technique factors assumed, and then modified to reflect the operating potential being
considered, were 5 mA at 50 kVp for radiography below 50 kVp and 3.3 mA at 150
kVp for radiography above 50 kVp.
The data of Simpkin and Dixon have been used here to produce secondary
transmission curves. Although they have not considered the variation of scatter quality
with angle experimental measurements performed by the working party suggest that
at 117 degrees, which is the angle for maximum scatter dose (see section 4.2) , the
primary and scattered radiation have very similar HVLs (figure 2.2). The use of the
data is therefore considered to be justifiable. As in the case of primary radiation,
equation 5.2 has been used to predict transmission values for a selection of
commonly used shielding materials at differing kVps using the available data..
Figures 5.7 and 5.8 show derived transmission curves through lead and concrete, for
secondary radiation arising from a primary beam (Tungsten target) at 50, 70, 100 and
125 kVp. Also shown in these figures are transmission curves for seconary radiation
arising from a 30 kVp Mo/Mo primary beam. Figure 5.9 shows transmission of
secondary through wood and gypsum for a 30 kVp Mo/Mo primary beam. All data are
plotted for B=1 to B=10-6. Selected fitting factors at representative energies are given
in table 5.5 as is the high attenuation Half Value Layer. A more comprehensive
collation of fitting parameters can be found in Simpkin and Dixon (1998).
The equivalence of materials has also been determined, using the cubic polynomial
approach outlined above. The equations of each fitted curve are given in tables 5.6
and 5.7. It will be seen from the figures and equations that, as expected, the
secondary radiation requires more shielding than the corresponding primary radiation.
This is especially the case especially at higher values of kVp.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
19
Hopefully can put some Monte Carlo results in here - i.e. what the effect of
scattering angle really is and when Simpkin & Dixon's work can be used. Need
to determine what the effect of the HVL variation is.
The penetrating ability of the scattered radiation decreases as the scatter
fraction increases - (I don't think this is at all remarkable) - . In the experiment
performed as part of this work, it was lower than the primary beam at angles
greater than about 120 degrees. The question is : is it in fact all stopped by
about the same amount of shielding since as the fluence goes down, the
penetrating ability goes up and one balances the other out.
5.3.2 Computed Tomography
The spectrum of scattered radiation which is produced as a result of CT scanning will
be considerably harder than that observed in general radiogrpahy. Allowance must
be made for this when designing computed tomography suites. There is very little
data available on the transmission characteristics of such radiation. Simpkin (1990)
has used Monte Carlo tehniques to simulate CT scatter spectra and has modelled the
transmission characteristics of a variety of commonly used materilals but has made
no allowance for leakage. radiation His results are given in table 5.6 in the form of
coefficients for equations 5.1 and 5.2. Figure 5.10 is a demonstration of the use of this
table, and shows predicted transmission through concrete at 120 and 140 kVp.
5.4 References.
Archer BR , Thorny JI, Bushong SC. (1983) Diagnostic x-ray shielding design based
on an empirical model of photon attenuation. Health Physics 44 , 507-517.
Archer BR, Fewell TR, Conway BJ & Quinn PW. (1994). Attenuation properties of
diagnostic x-ray shielding materials. Medical Physics 21 1499-1507
British Gypsum (1991) Thistle x-ray. Technical Information leaflet.
Chritensen Rc & Sayeg JA. 1979 Attenuation characteristics of gypsum wallboard.
Health Physics 36 595-600.
HMSO 1971 Handbook of Radiological Protection. HMSO London.
HPA 1984 Report no 41 :Notes on Building Materials and Reference Data on
Shielding Data for use below 300 kVp. HPA (now IPEM) , York
Legare JM, Carrieres, PE, Manseau A et al. (1977) Blindage contre les grands
champs de rayons x primaires et diffuse des appareils triphase au moyen de
panneaux de verre de gypse et de plomb acoustique. Radioprotection 13 79-95
National Council on Radiation Protection and Measurements (1976) Structural
shielding design and evaluation for medical use of x rays and gamma rays of energies
up to 10 MeV. NCRP Report No 49.
RossiRP, Ritenour R, Christodoulou E. 1991 Broad beam transmission properties of
some common shieldin materials for use in diagnostic radiology. Health Physics 61
601-608
Simpkin DJ 1989 Shielding requirements for constant potential diagnostic x-ray
beams determined by a monte carlo calculation. Health Physics 56 151-164
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
20
Simpkin DJ 1990 Transmission of scatter raduiation from computed tomography (CT)
scanners determined by a monte carlo calculation. Health Physics 58 363-367
Simpkin DJ 1995 Transmission data for shielding diagnostic x-ray facilities. Health
Physics 68 704-709
Simpkin DJ and Dixon RL (1998) Secondary radiation shielding barriers for diagnostic
x-ray facilities: scatter and leakage revisited. Health Physics, 74, 350-65.
Tsalafoutas A, Yakoumakis A, Manetou A & Flioni-Vyza A. 1998 The diagnostic x-ray
protection characteristics of Ytong, an aerated concrete based building material. BJR
71 944-949
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
21
1.0E+00
1.0E-01
Transmission
1.0E-02
Tx
Tx
Tx
Tx
Tx
Tx
1.0E-03
30
50
60
75
90
120
1.0E-04
1.0E-05
1.0E-06
0.0
1.0
2.0
3.0
4.0
5.0
mm
Figure 5.1 Transmission of primary radiation through Lead
.
1.0E+00
1.0E-01
Transmission
1.0E-02
Tx 30
Tx 50
Tx 60
Tx 75
Tx 90
Tx 120
1.0E-03
1.0E-04
1.0E-05
1.0E-06
0.0
50.0
100.0
150.0
200.0
250.0
300.0
350.0
400.0
mm
Figure 5.2 Transmission of primary radiation through concrete.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
22
.
1.0E+00
1.0E-01
Transmission
1.0E-02
Tx
Tx
Tx
Tx
1.0E-03
50
75
100
125
1.0E-04
1.0E-05
1.0E-06
0.0
10.0
20.0
30.0
40.0
50.0
60.0
70.0
80.0
mm
Figure 5.3 Transmission of primary radiation Through Barium Plaster
1.0E+00
1.0E-01
Transmission
1.0E-02
Wood
Gypsum
1.0E-03
1.0E-04
1.0E-05
1.0E-06
0.0
100.0
200.0
300.0
400.0
500.0
600.0
mm
Figure 5.4 Transmission of primary radiation Through Wood & Gypsum 30 kVp
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
23
1.0E+03
1.0E+02
Lead
1.0E+01
Thickness
Steel
Gypsum
Plate Glass
Concrete
Ba Plaster
1.0E+00
1.0E-01
1.0E-02
1.0E-06
1.0E-05
1.0E-04
1.0E-03
1.0E-02
1.0E-01
1.0E+00
1.0E+01
Transmission
Figure 5.5 Transmission of primary radiation at 75 kVp.
CONCRETE
200
100
Cubic fit
Observed Data
0
0.0
.2
.4
.6
.8
1.0
1.2
1.4
1.6
LEAD
Figure 5.6 Equivalence between concrete and lead at 60 kVp.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
24
1.0E+00
1.0E-01
Transmission
1.0E-02
Tx 30
Tx 50
Tx 70
Tx 100
Tx 125
1.0E-03
1.0E-04
1.0E-05
1.0E-06
0.0
1.0
2.0
3.0
4.0
5.0
6.0
mm
Figure 5. 7 Transmission of secondary radiation through lead.
1.0E+00
1.0E-01
Transmission
1.0E-02
Tx
Tx
Tx
Tx
Tx
1.0E-03
30
50
70
100
125
1.0E-04
1.0E-05
1.0E-06
0.0
50.0
100.0
150.0
200.0
250.0
300.0
350.0
400.0
mm
Figure 5.8 Transmission of secondary radiation through concrete.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
25
1.0E+00
1.0E-01
Transmission
1.0E-02
Gypsum
Wood
1.0E-03
1.0E-04
1.0E-05
1.0E-06
0.0
50.0
100.0
150.0
200.0
250.0
300.0
mm
Figure 5.9 Transmission of secondary radiation for 30 kVp primary
1.00E+00
1.00E-01
Transmission
1.00E-02
120 kVp
140 kVp
1.00E-03
1.00E-04
1.00E-05
1.00E-06
0.00
50.00
100.00
150.00
200.00
250.00
300.00
350.00
400.00
450.00
500.00
Barrier Thickness (mm)
Figure 5.10 Transmission of scattred CT radiation through concrete.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
26
30 kVp
α
β
λ
∆ = β/ α
Lead
Steel
Gypsum
Plate glass
Concrete
wood
50 kVp
Lead
Steel
Gypsum
Plate glass
Concrete
Ba Plaster
60 kVp
Lead
Steel
Gypsum
Plate glass
Concrete
Ba Plaster
75 kVp
Lead
Steel
Gypsum
Plate glass
Concrete
Ba Plaster
90 kVp
Lead
Steel
Gypsum
Plate glass
Concrete
120 kVp
Lead
Steel
Gypsum
Plate glass
Concrete
38.8
5.716
0.1208
0.3061
0.3173
0.02166
178
43.41
0.7043
1.599
1.698
0.03966
0.3473
0.3959
0.3613
0.3693
0.3593
0.3732
Assymptotic
HVL =( ln 2)/α
α
4.58763 0.017865
7.59447 0.121264
5.8303
5.737973
5.22378 2.264447
5.3514
2.184517
1.831025 32.00125
8.8014
1.817
0.03883
0.09721
0.09032
0.447049
27.2737
4.845
0.08732
0.1798
0.1712
1.222173
0.2956
0.4024
0.05106
0.4912
0.2324
0.263357
3.09879
2.66648
2.24878
1.8496
1.89548
2.73387
0.078754
0.381479
17.85082
7.13041
7.674349
1.550496
6.951
1.183
0.02985
0.07452
0.06251
24.89
4.219
0.07961
0.1539
0.1692
0.4198
0.4571
0.6169
0.5304
0.2733
3.58078
3.56636
2.667
2.06522
2.70677
0.099719
0.585923
23.22101
9.301492
11.08858
4.666
0.5793
0.2066
0.5291
0.04797
0.609028
22.69
3.629
0.6649
1.28
0.1663
2.357352
0.6618
0.5908
0.775
0.6478
0.4492
0.582836
4.86284
6.26446
3.2183
2.4192
3.46675
3.870677
0.148553
1.196525
3.35502
1.310049
14.4496
1.13812
3.067
0.3971
0.01633
0.0455
0.04228
18.83
2.913
0.05039
0.1077
0.1137
0.7726
0.7204
0.8585
0.8522
0.469
6.13955
7.33568
3.08573
2.36703
2.68921
0.226002
1.745523
42.44624
15.234
16.39421
2.246
0.2336
0.01235
0.03758
0.03566
8.95
1.797
0.03047
0.06808
0.07109
0.5873
0.8116
0.9566
1.031
0.6073
3.98486
7.69264
2.46721
1.8116
1.99355
0.308614
2.96724
56.12528
18.44458
19.43767
Table 5.1 Selected coefficients to generate primary
(equations 5.1, 5.2 & 5.3)
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
transmission curves
27
Material
Density
Lead
11350 kgm-3
Concrete
2350 kg m-3
Steel
7400 kgm-3
Gypsum
705 kgm-3
Plate Glass
2560 kgm-3
Wood
550 kgm-3
Table 5.2 Density of Materials
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
28
30 kVp
CONCRETE
GLASS
GYPSUM
STEEL
WOOD
Ba Plaster
50 kVp
CONCRETE
GLASS
GYPSUM
STEEL
BA PLASTER
60 kVp
CONCRETE
GLASS
GYPSUM
STEEL
Ba Plaster
75 kVp
CONCRETE
GLASS
GYPSUM
STEEL
BA PLASTER
90 kVp
CONCRETE
GLASS
GYPSUM
STEEL
BA PLASTER
125 kVp
CONCRETE
GLASS
GYPSUM
STEEL
BA PLASTER
b1
112.096
120.829
277.034
5.1375
3103.48
-
b2
51.0661
42.2184
207.506
8.7427
-5936.3
-
b3
-78.89
-74.817
-309.99
-13.859
8776.53
-
120.679
150.514
203.376
6.2303
20.3472
-30.717
-47.992
-113.94
-0.7349
-1.6765
11.2057
13.2935
42.8306
.1146
.7105
105.721
138.504
337.873
6.2363
-
-9.9460
-33.431
-72.798
-0.1632
-
4.2142
7.9825
16.5428
0.0228
-
87.6303
116.682
296.416
6.2954
7.7994
1.1509
-15.916
-37.643
0.837
-0.1512
.1787
2.6675
6.134
-0.1226
0.0322
76.0696
99.6588
258.95
6.6.17
-3.0833
-11.927
-26.028
.3716
.4431
1.3144
2.8502
-0.0386
91.3923
103.422
290.882
9.9312
12.8985
-6.9006
-10.843
-25.812
.2880
.0098
.5278
.8456
1.9735
-.0303
.0003
Table 5. 3
Cubic coefficients relating lead thickness with that of other material
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
29
30 kVp
LEAD
50 kVp
LEAD
60 kVp
LEAD
70 kVp
LEAD
80 kVp
LEAD
90 kVp
LEAD
100 kVp
LEAD
110 kVp
LEAD
125 kVp
LEAD
b1
.0089
b1
.0080
b1
0.0095
b1
0.0109
b1
0.0119
b1
0.013
b1
0.0136
b1
0.0127
b1
0.0101
b2
-3e-05
b2
2.9E-05
b2
9.0E-06
b2
-2E-06
b2
9.7E-07
b2
8.9E-06
b2
1.6E-05
b2
1.8E-05
b2
1.8E-05
b3
3.9e-07
b3
-1.E-07
b3
-4.E-08
b3
-3.E-09
b3
-5.E-09
b3
-2.E-08
b3
-3E-08
b3
-3.E-08
b3
-2E-08
Table 5. 4
Cubic coefficients relating concrete thickness with that of lead
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
30
30 kVp
Lead
Steel
Gypsum
Plate glass
Concrete
wood
50 kVp
Lead
Steel
Gypsum
Plate glass
Concrete
70 kVp
Lead
Steel
Gypsum
Plate glass
Concrete
100 kVp
Lead
Steel
Gypsum
Plate glass
Concrete
125 kVp
Lead
Steel
Gypsum
Plate glass
Concrete
α
β
λ
∆ = β/ α
HVL (=ln(2)/α
α)
38.79
7.408
0.1198
0.306
0.3174
0.02159
180
42.49
0.7137
1.62
1.725
0.03971
0.356
0.4021
0.3703
0.3793
0.3705
0.03971
4.64037
5.73569
5.95743
5.29412
5.43478
1.83927
0.017869
0.093567
5.78587
2.265187
2.183829
32.10501
8.801
1.817
0.0388
0.09721
0.0903
27.28
4.84
0.0873
0.1799
0.1712
0.2957
0.4021
0.5105
0.4912
0.2324
3.09965
2.66373
2.25
1.85063
1.8959
0.078758
0.381479
17.86462
7.13041
7.676049
5.369
0.7149
0.023
0.05791
0.0509
23.49
3.798
0.0716
0.1357
0.1697
0.5883
0.5381
0.73
0.5968
0.3849
4.37512
5.31263
3.11304
2.34329
3.33399
0.129102
0.969572
30.13683
11.96939
13.61782
2.507
0.3424
0.0147
0.04279
0.0395
15.33
2.456
0.04
0.08948
0.0844
0.9124
0.9388
0.9752
1.029
0.5191
6.11488
7.1729
2.72109
2.09114
2.13671
0.276485
2.024378
47.15287
16.19881
17.54803
2.233
0.2138
0.012
0.03654
0.0351
7.888
1.69
0.0267
0.0579
0.066
0.7295
1.086
1.079
1.093
0.7832
3.53247
7.90458
2.225
1.58456
1.88034
0.310411
3.242035
57.76227
18.96955
19.74778
Table 5.5 Selected coefficients to generate secondary transmission curves at
90 degrees(equations 5..1 & 5.2).
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
31
30 kVp
CONCRETE
GLASS
GYPSUM
STEEL
WOOD
50 kVp
CONCRETE
GLASS
GYPSUM
STEEL
70 kVp
CONCRETE
GLASS
GYPSUM
STEEL
100 kVp
CONCRETE
GLASS
GYPSUM
STEEL
125 kVp
CONCRETE
GLASS
GYPSUM
STEEL
b1
112.351
121.035
277.503
4.9526
2028.45
b1
120.675
150.465
355.969
6.2303
b1
91.6283
123.435
310.695
6.2219
b1
69.1344
85.3562
229.377
7.0278
b1
81.9378
90.6395
257.496
10.1464
b2
51.7292
41.8356
217.189
2.5928
-6270.3
b2
-30.657
-47.944
-93.493
-0.7366
b2
1.3991
-19.366
-45.936
0.6853
b2
-2.6302
-8.0393
-17.588
0.0908
b2
-4.6953
-7.5868
-18.028
0.1501
b3
-81.807
-74.904
-324.34
-4.9301
10390.8
b3
11.2004
13.2771
23.3248
0.1155
b3
0.4601
3.7135
8.4881
-0.1175
b3
0.2774
0.7137
1.5571
-0.0082
b3
0.3615
0.5849
1.3748
-0.0150
Table 5.6
Cubic coefficients relating lead thickness with that of other material for
secondary radiation
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
32
30 kVp
LEAD
50 kVp
LEAD
70 kVp
LEAD
100 kVp
LEAD
125 kVp
LEAD
b1
.0089
b1
.0080
b1
0.0109
b1
0.0143
b1
0.0117
b2
-3e-05
b2
2.9E-05
b2
-2E-06
b2
1.1E-05
b2
1.5E-05
b3
4e-07
b3
-1.E-07
b3
-3.E-09
b3
-2.E-08
b3
-2E-08
Table 5.7
Cubic coefficients relating concrete thickness with that of lead for secondary
radiation
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
33
α
β
γ
∆=β
∆=β/ α
Pb
120-kVp
140-kVp
2.70214
2.86862
6.2227
4.6590
0.7721
0.7921
2.303
1.624
Concrete
120-kVp
140-kVp
0.03829
0.03359
0.0142
0.0122
0.6582
0.5185
0.371
0.363
Gypsum wallboard
120-kVp
140-kVp
0.00100
0.01177
0.0268
0.0167
0.4125
1.3910
26.800
1.419
Steel
120-kVp
140-kVp
0.27957
0.19215
1.5191
0.9519
1.2357
0.9649
5.434
4.954
Plate glass
120-kVp
140-kVp
0.03213
0.03544
0.0146
.00975
0.2280
0.9450
0.454
0.275
Table 5.8 Coefficients which can be used to generate transmission of scattered
radiation from CT installations.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
34
6 PRACTICAL ASSESSMENT OF SHIELDING
6.1 INTRODUCTION
When an X-ray facility is complete, it is necessary to check the integrity of the
shielding provided and ensure that it fulfils the design criteria. This is one element of
the critical examination required by the Ionising Radiation Regulations. Such checks
can be carried out through discussions with the builder and visual inspection of all
parts during the construction phase. However, a complete inspection of all parts of the
facility at this stage may not be practicable, in which case it is necessary for checks of
the shielding to be made when the construction is complete. Use of a radiation
source and detector during the critical examination allows the integrity of all parts of
the shielding in a completed installation to be checked. The most suitable type of
source is a sealed source of 241Am as the main γ -ray has an energy of 60 keV which is
within the upper part of the photon energy range of an X-ray beam (Hewitt 1982). A
vial of 99mTc may be used as an alternative to determine the thickness of lead used to
provide protection if an 241Am source is not available. However, a knowledge of
shielding materials employed is essential for interpretation of results, because the
energy of the main 99mTc γ -ray (141 keV) is significantly higher than the normal X-ray
range and relative attenuation properties of shielding materials at this energy differ
from those at X-ray energies. An alternative method is to make the assessment using
radiographic exposures. However, this method is more time consuming and less
flexible and so will only be considered briefly in this report.
6.2 METHODOLOGY
6.2.1 Radioactive source method
There are two main aims of the practical assessment of shielding:
1) to detect any places where there are gaps in the shielding provided
2) to check that the protection is of the level specified.
The apparatus consists of a source, a detector and positioning rod, a tape
measure and calibration charts. Two persons are required to carry out the tests, both
for practicality of making the measurements and for purposes of ensuring security of
the radioactive source and minimising exposure of other staff. Procedures must be in
place to comply with current Ionising Radiation Regulations and ensure effective
supervision of the source. One person is required to position and control the source
and the second to determine the location of the beam on the far side of the barrier
using a suitable detector. A tape measure is useful for defining the approximate
location of the source, in order to assist the second person in locating the radiation
beam. Persons carrying out the assessment may choose to use the source and
detector on whichever side of the boundary is better both for access and for safety
purposes. It is easier to locate the source at fixed points on the side of a wall to which
access is limited and leave areas of wall on the other side where more space may be
available to allow the person using the detector more space to search for the radiation
beam. Other things being equal, positioning of the source on the inside of the X-ray
room will simulate more closely the situation in practice. It will be necessary to move
the detector back and forth over the wall surface to locate the position of maximum
response.
Detector
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
35
The detector used should have a rapid response to facilitate location of the
radiation beam on the far side of the barrier from the source. A scintillation detector
such as a Mini Instruments 900 Monitor with a Type 44A probe, which has a 32 mm
diameter x 2.5 mm thick sodium iodide scintillation crystal, is suitable. <For situations
in which the expected degree of protection is less than 1mm Pb equivalent, an end
window geiger tube such as a Mini Instruments Type E probe can be used.>> A rigid
measuring bar with 1 cm graduations attached to the probe housing is useful to
enable the probe face to be positioned at a fixed distance of 1 to 15 cm from the wall
surface (figure 6.1).
Sources
As already mentioned, the source may be 241Am or 99mTc. The source must be
housed in a shielded container having a window or cap which can be readily
removed, so that the aperture can be placed against the barrier to be tested. A design
for a lockable container with a safety shutter for an 241Am source (Hewitt 1982) is
shown in figure 6.2. A spring loaded rotating lead shutter may be held open when the
container is positioned against a barrier and closes automatically when the container
is moved away from the barrier. This minimises the exposure to scattered radiation of
the person handling the source.
241-Americium
241
Am emits a gamma ray of energy 60 keV which is close to the peak of the
photon energy spectrum for a diagnostic X-ray unit. Plots of count rate against source
detector separation are given in figure 6.3 for barriers made from different materials.
Results are normalised with respect to the count rate obtained with a source detector
separation of 30 cm with 1 mm of lead in the beam.
In order to obtain a high enough radiation level for the check to be made, a source of
15-40 GBq must be used. This requires the use of a type A transport container and
associated procedures under the Radioactive Material (Road Transport) (Great
Britain) Regulations 1996 including consignment note, labelled vehicles and carrying
of a fire extinguisher. In addition the Radiation (Emergency Preparedness and Public
Information) Regulations require the operator holding and using an 241Am source of
activity more than 300 MBq to carry out a hazard assessment and risk evaluation for
the Health and Safety Executive. Sources with a valid special form certificate are
exempt from this requirement.
99m- Technetium
For hospitals which do not possess an 241Am source, a vial of 99mTc provides
an alternative. 99mTc is readily available in Nuclear Medicine departments, is
inexpensive and the potential hazard is low because of the short half-life. As a result,
a vial of 99mTc can be carried as an excepted package. Activities required are typically
50 MBq or 100 MBq. It is recommended that standard activities are used for which
calibration charts can be prepared. If the amount of liquid is much smaller than the
volume of the vial, the position of the activity will depend on the inclination of the vial.
It is therefore recommended that a volume of liquid is used which is sufficient to fill the
majority of the vial.
The disadvantage of 99mTc is that the γ -ray has an energy of 141 keV, which is
significantly higher than the photon energies in most diagnostic X-ray beams. As a
result the relative attenuation by different shielding materials such as lead, concrete
and X-ray plaster is not the same for 99mTc as for an X-ray beam. The attenuation by
lead is high because the K absorption edge for lead is at 88 keV, but attenuation by
other materials used for shielding is much lower than that for diagnostic X-ray beams.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
36
Thus the attenuation for a beam of 99mTc γ -rays can be used to determine the amount
of lead protection, but is seldom satisfactory for assessing barriers of other materials.
Plots of normalised count rates versus source detector separation for different
thicknesses of lead and other materials are given in figure 6.4.
Checks for gaps in shielding
Checks for gaps in protection should be made with the detector in contact with
the wall. It will be necessary to move the detector back and forth over the wall surface
to locate the position of maximum response. This will normally be the position where
source and detector are directly opposite each other on either side of the wall, but in
places where there is a gap in the protection in a cavity wall, this may not necessarily
be the case. Places where gaps are more likely to occur are where different forms of
shielding meet. These include:
Frames of shielded windows and doors
Joins between two parts of a shield
Where sockets, etc, breach the integrity of the wall.
Practical assessment of level of protection
The source container with the window or lid open is held against the wall for
the measurements (figure 6.1). A tripod and baseplate are useful for holding the
source in a fixed position. An option to include an additional 1 mm of lead in the beam
is useful to increase the range of attenuation that can be assessed. In order to make a
shielding assessment it is necessary to know the thickness of the wall, so that the
separation of the source and the detector can be set. If there is a door in the wall, this
can be determined with relative ease, but if not, it may be necessary to measure
distances along a number of walls to determine the wall thickness, as illustrated in
figure 6.5. Where several measurements are required the accuracy of the distance
may be limited. Values for the thickness may also be available from plans of the
facility or from measurements made during the construction phase. Where the wall is
some distance from any door to the room, these may be the only thicknesses
available.
The results of the measurement depend upon the separation of the source and
detector. A separation between 20 cm and 50 cm is recommended. If a shorter
distance is employed, error due to inaccuracy in the distance becomes large, while if
the distance is too large count rates may be too low to obtain an accurate
measurement. As already discussed, it is necessary to know what shielding materials
were used if a realistic result is to be obtained. The data in figures 6.3 and 6.4 allow
results to be converted to thicknesses of different shielding materials
Normalised count rates are plotted as a function of separation of source and detector
to allow flexibility in the configuration used. It is suggested that the user make a
measurement of the count rate obtained at 30 cm through 1 mm lead using their
choice of activity This measurement could be used to calibrate the user’s monitor and
a set of curves of count rate versus distance determined from the figures. Variations in
the measurements relating to the relative position of the source, detector and barrier
were ±15%.Experimental results indicate that use of a type E geiger as opposed to a
type 44 monitor will not alter the magnitude of this error See Daves figure at the end
6.2.2 Measurements using X-ray equipment
Assessments of shielding may be made using X-ray equipment, although this method
tends to be more time consuming and requires a radiation detector with good dynamic
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
37
range. The measurements may be performed with the unit installed in the room, if
there is sufficient flexibility in positioning of the X-ray tube, or a mobile radiographic
unit may be used. The energy of the X-ray beam can be chosen to match that of
examinations performed in the room and so used to obtain the wall attenuation
directly. An ionisation chamber of appropriate sensitivity should be used to measure
air kerma for an exposure using standard factors on either side of the barrier to be
tested. The attenuation can then be determined directly from the ratio of the two
measurements with an inverse square law correction applied to allow for the different
positions. Alternatively the air kerma at the distance to be used for the assessment
could be determined from measurements made in the room. The use of X-ray
equipment and film can be useful for direct demonstration of gaps in shielding
detected using the source method.
References
Hewitt JM (1982) A self-contained method for assessing the lead equivalence
of protective barriers in diagnostic X-ray departments. J. Soc. Radiological
Protection 2, 22-26.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
38
Figure 1
Arrangement for assessment of shielding using a source and
scintillation detector. Thickness of the wall = A + B.
Figure 2
Shielded container for 241Am source. (N.B. Awaiting information
from Graham Ramsden, NRPB, Leeds on design)
Figure 3
Graphs of normalised count rate from a 241Am source versus
distance between probe and source for different thicknesses of a)
lead and b) barytes plaster and brick. Data are normalised with
respect to the count rate with 1 mm lead at a source probe
distance of 30 cm.
Figure 4
Graphs of normalised count rate from a 99mTc source versus
distance between probe and source for different thicknesses of a)
lead and b) barytes plaster. Data are normalised with respect to
the count rate with 1 mm lead at a source probe distance of 30
cm.
Figure 5
Determination of wall thickness A from distances along intervening
walls.
Last
Figure
Dave Sutton results
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
39
Wall
A
B
Scintillation Contamination Monitor
Source
Measuring Bar
Figure 6.1
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
40
Americium-241 Lead Attenuator
100
Normalised Count Rate (c/s)
10
1
0.5 mm
1.0 mm
1.5 mm
0.1
2.0 mm
3.0 mm
0.01
0.001
0
10
20
30
40
50
60
70
Source Detectro Distance (cm )
Figure 63a
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
41
Americium-241 - Barium Plaster Attenuator
10
Normalised Count Rate
1
0.1
10 mm
20 mm
30 mm
0.01
0.001
0
10
20
30
40
50
60
70
Source Detector Distance (cm )
Figure 6.3 b
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
42
Technetium-99m - Lead Attenuator
100
Normalised Count Rate
10
0.5 mm
1.0 mm
1.5 mm
1
2.0 mm
2.5 mm
3.0 mm
0.1
0.01
0
10
20
30
40
50
60
70
Source Detector Distance (cm )
Figure 6.4a
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
43
Technetium 99m Ba Plaster Attenuator
10
10 mm Barytes
1
20 mm Barytes
30 mm Barytes
10 cm Brick
21.5 cm Brick
0.1
0.01
0
10
20
30
40
50
60
70
Figure 6.4 b
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
44
A
C
B
D
Wall thickness A = D - B - C
Figure 5
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
45
scint & geiger com parison
10 00 00
100 00
10 00
sc in t il lat ion p r ob e
g eig er t u be
100
10
1
0 .0 0
0 .50
1.00
1.5 0
2 .0 0
2.50
3.0 0
3 .5 0
4 .00
4.50
Daves Figure to show the similarity - counts are normalised.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
46
7 Methodologies and Worked Examples
7.1 RADIOGRAPHIC FACILITIES
Radiographic rooms are used in a more versatile manner than most other x-ray installations.
Generally there are two main imaging stations – a table and a vertical bucky stand used
principally for chest radiography. Examinations on the table most commonly involve the
radiation beam firing downwards with the cassette either in the bucky tray or on the table top
(generally for extremities). For these locations protection is required for the secondary
radiation and for the transmitted primary radiation. The area of the wall or floor exposed to the
latter component being both limited and predictable. However, other parts of the floor or walls
may be exposed to transmitted primary due, for example, to lateral views taken with the patient
on the table and examination of patients on trolleys.
7.1.2 Methods
1. NCRP
The conventional method of calculating barrier thickness is to use the
recommendations in NCRP Report 49 (NCRP 1976). The NCRP method considers
the three components of radiation (primary, leakage and scatter) separately and has
the following features:
•
•
•
•
•
Workload is expressed in mA.min
A single, high kVp is assumed for the total workload
Primary barrier thickness is designed on the assumption that there is no
attenuation in the beam directed towards the wall or floor
Leakage radiation is assumed to be at the maximum specified rate, i.e. 1 mGy h-1
Scatter radiation is computed on the basis of equation 4.1.1 using scatter factors
based on single phase, low filtration sets.
Changes in the methodology for primary shielding were proposed by Dixon and Simpkin
(1998) and for secondary barriers by Simpkin and Dixon (1998) which retained the use of
mA.min as the unit of workload.
For the specification of primary barriers, the biggest changes made by Dixon and Simpkin
(1998) are concerned with more realistic assumptions regarding primary attenuation and
workload spectra. They provide the following data:
•
•
•
•
transmission through the patient, image receptor, and supporting structures based on work
by Dixon (1994);
tube output at 1 m per mA.min;
workload spectrum based on a survey by Simpkin (1996);
use factors, i.e. proportion of the workload for which the beam is directed at the floor or
specific walls.
The data can be used to specify shielding for any workload spectrum and pattern of usage.
However, they give a general equation for calculating transmission B through a barrier of
thickness, x , in association with pre-shielding in the patient, image receptor, etc. which is
assumed to have an equivalent thickness, xpre:
P d2
B( x + x pre ) =
T D1 (0 ) N
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
(1)
47
in which P is the dose constraint, T is the occupancy factor, d is the focus to barrier distance,
D1(0) is the unshielded primary dose per patient at 1 m for the standard workload spectrum,
and N is the number of patients per week.
Values of these parameters are given by Dixon and Simpkin (1998) and reproduced in Table
1. For cross-table radiography, they recommend the use of xpre = 0.3 mm lead or 30 mm
concrete.
For secondary radiations, Simpkin and Dixon (1998) recommended that scatter and leakage
radiations are combined and used with modified transmission data to account for the
hardening of the leakage spectrum. This approach was discussed in Section 4. They provide a
simplified equation for the calculation of the secondary barrier based on the same workload
data as given above combined with the assumption that all vertical bucky work including chest
2
radiography is with a 35 x 43 cm cassette and that the average field area for table
2
radiography is 1000 cm . The total secondary dose per patient at 90° and distance of 1 m
( D1sec ) is given in Table 1 for the standardised workload.
The unshielded secondary dose is given by:
D sec (0) =
D1sec N
d 2sec
(2)
in which dsec is the distance to the area to be shielded and N is the number of patients.
2. Working party
Alternative methods are proposed here for shielding calculations. For primary
radiation it is proposed that film dose is used and secondary radiation shielding should
be assessed from workload in terms of DAP as outlined in Section 4 of this report.
This approach is described in more detail.
400 speed radiographic film requires, by definition, a dose of 2.5 µGy to produce a
density of 1.0 plus base plus fog. Some areas of the film will have higher densities
because a) radiologists generally prefer somewhat darker films, b) the beam may be
larger than the body part (for example for extremities), and c) there are density
variations across the film. In addition slower films may be used for extremities
(although for protection purposes, these are associated with low kVps and are
therefore of much less relevance). It is proposed to use a value of 10 µGy as the
average for the maximum dose on any part of the film. This represents significant
attenuation of the primary which may vary between about 10-3, e.g. for a lateral view
of the lumbar spine with an entrance skin dose of 10 mGy to 0.1 for a chest
radiograph with an ESD of 0.1 mGy.
Making the assumption that the beam is fully collimated to the area of the cassette,
there is then further attenuation produced in the cassette itself and in the structure of
the cassette holder and the table base or vertical bucky stand.
Attenuation needs to be estimated for three geometries:
Table radiography with attenuation in the cassette plus table assembly
Cross table radiography with attenuation in the cassette alone
Vertical bucky radiography with attenuation in the cassette plus bucky assembly
Ø
Ø
Ø
Dixon (1994) measured primary attenuation in 8 types of film cassette. Average values are
shown in Table 2. However, these data cannot be applied to the primary transmitted through
the patient because of beam hardening. To estimate this effect, the primary transmission
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
48
factors can be used to estimate lead and concrete equivalence of the cassette. These values
are shown in the Table. The equivalent thicknesses can then be used to calculate the
transmission of the filtered spectrum in lead (A) and concrete (B) using the limiting values of
HVL for the primary beam derived as for the data in Table 5.1. It can be seen that the
transmission of the filtered beam is much greater and it is recommended that 50%
transmission is assumed at all energies.
Transmission through a table assembly with a cassette in place was given by Dixon
(1994).
This included transmission through the tabletop and grid. Primary
transmission through these components are given separately. The data are shown in
Table 3. Using primary transmission data the lead equivalence of the complete
assembly and of the tabletop plus grid can be calculated. From these values the
transmission of the filtered beam through the cassette plus the table base can be
calculated using the limiting values of HVL.
Dixon (1994) measured primary transmission through 3 models of vertical bucky stand
at 125 kVp. The same type of analysis as for the table has been made for the model
with maximum transmission. The result shown in Table 3 indicates that the
transmission of the filtered beam is 0.25.
For secondary radiation, the working party recommend that the methods described in
Section 4 are used with workload based on DAP.
7.1.3 Workload
Primary radiation
For primary radiation it is necessary to know which examinations may involve the use
of a horizontal beam. Most commonly horizontal beams are used with the vertical
bucky with the patient standing or lying on a trolley. The vertical bucky may be used
for the following examinations:
Ø
Ø
Ø
Ø
Ø
Chests – kVp depends on local practice and may vary over virtually the full
diagnostic range (60 to 150 kVp). It is advisable to design shielding on the basis
that practice may change to the upper end of this range since this has been
recommended in a number of publications both for patient dose reduction and
image quality.
Shoulders, cervical spines (at between 60 and 75 kVp).
Abdomens (70 to 90 kVp) –required for erect patients in rare circumstances.
Standing knees, femur (60 to 70 kVp) and erect spines (70 to 90 kVp) generally in
rooms serving orthopaedics.
Skulls, sinuses, facial bones (60 to 75 kVp) – may preferably be done in rooms
with isocentrically mounted skull units.
The examinations of the skull, etc. may also be done on the table with the film
propped up. There are other cross-table radiographic views but these are relatively
rare except with seriously injured patients. It is also possible that the radiographic
workload will include ‘sky-line’ views of the knee. However, this is with the tube
pointing towards the patient who will be protected by a lead coat and will effectively
provide local shielding.
In A&E horizontal beams are more common particularly for seriously injured patients.
Examinations include: skull; spine; hips; and extremities. The film may be taken using
a vertical bucky, if that is available, or with the film propped up or held.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
49
Scatter
For scatter calculations workload is required in terms of DAP. There are few
publications of DAP for radiographic doses. However, it is possible to infer typical
values using average entrance skin doses (ESD) from NRPB (1996) and the ratio of
ESD and DAP to effective dose conversion factors from NRPB (1994). These values
are given in Table 4 with upper limit values calculated from the reference doses. A
large proportion of the workload in terms of the numbers of films will be for
extremities. However, the DAPs for these examinations will be low (in the range 0.01
to 0.1 Gy.cm2) so that they make a relatively small contribution to scatter and the
kVps are also relatively low (50 to 70 kV) requiring less shielding.
For a busy radiographic room, the workload will be in the region of 500 Gy.cm2 but
this will depend on case mix. The average DAP weighted kVp will be in the range 80
to 90 kVp. This will be determined by the relative proportion of examinations in the
pelvic and abdominal regions which are associated with the highest DAPs and tube
potentials.
7.1.4 Example
Room diagram to calculate at wall situated at 1.5 m from Table (primary
and secondary), cubicle at 3 m (secondary), door (3.5 m – secondary),
wall 1 m behind chest stand (primary), floor below table.
For this example the total weekly workload is assumed to be 500 Gy.cm2.
includes:
•
•
•
•
This
400 films on the table at a DAP weighted average of 90 kVp
10 cross-table spine films at 100 kV directed towards wall A.
100 chest films at 125 kVp
An average DAP per chest film equal to 0.15 cGy cm2
Any other examination using the vertical bucky is ignored in this calculation. It has
been assumed that the occupancy factor of adjacent rooms and of the room below is
100%.
Wall A
Primary
10 films at 1 m FFD giving 10 µGy per film with 50% transmission through
the film plus cassette.
0.3
Transmission =
× (1.5 + 1)
52
1
10 × 0.01 × 0.5
2
= 0.72
At 100 kV the HVLs of lead and concrete are 0.276 mm and 17.5 mm
(Table 5.5) so that 0.13 mm of lead or 8 mm of concrete is required.
Secondary
Maximum scatter dose on the wall is given by equation 4.4 at 90 kVp:
[ ] × 500 = 1175 µGy per week
S max = (0.031 × 90 + 2.5) × 1
1.5
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
2
50
0.3
The required transmission is therefore given by B =
52 = 0.0049
1.175
This attenuation would be provided by 0.9 mm of lead or 70 mm of
concrete
The total thickness for this wall is based on the higher of these two values, i.e.
0.9 mm of lead or 70 mm of concrete.
Wall B
Protection is required for primary transmission through the wall behind the
bucky stand resulting form 100 films per week taken at 3.5 m FFD, with a filmto-barrier distance of 1 m.
× (1 + 3.5 )
52
3.5
100 × 0.01 × 0.25
0.3
Transmission =
2
= 0.038
This requires 4.7 HVLs which equals 1.5 mm of lead or 93 mm of concrete
using the data from Table 5.5.
Door
For a barrier at 3.5 m from the table, the scatter dose is given by:
[ ] × 500 = 216 µGy per week
S max = (0.031 × 90 + 2.5 ) × 1
3.5
2
0.3
Giving a required transmission of B =
52 = 0.026 which can be achieved
0.216
with 0.5 mm of lead.
Protective screen
The scatter dose to the protective screen at a distance of 3 m is
calculated in the same way as for the door and is equal to 294 µGy.
However, with a dose constraint of 60 µGy per year, the transmission
must be less than 0.0039. This requires 1 mm of lead.
Floor
Primary transmission has to be calculated for 400 films taken at 100 cm FFD
with a distance to the occupants in the room below equal to 3.5 m. The
transmission through the Table assembly of a 100 kVp beam from Table **
(0.09) has been used in these calculations.
× (3.5 + 1)
52
1
400 × 0.01 × 0.09
0.3
Transmission =
2
= 0.32
This requires 1.6 HVLs of concrete which is equal to 27 mm at 90 kVp.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
51
NCRP method
The NCRP method will be applied to the shielding requirements for Walls A and B and the
floor. It is assumed that the workload spectrum in Dixon and Simpkin (1998) applies and that
for there are 1.3 films per patient examination on the Table and 1.0 films per patient on the
vertical bucky. The total number of patients examined on the table is then 310 per week.
Wall A
Primary
× (1 + 1.5) 2
52
= 0.00025 .
The primary transmission should be less than
5.15 × 310 × 0.09
0.3
Assuming an average kVp of 80 kVp (the peak of the workload spectrum in Dixon and
Simpkin 1998), this requires 1.4 mm of lead. Subtracting xpre = 0.3 mm (the lead
equivalence of the shielding provided by the patient and cassette) leads to a barrier
requirement of 1.1 mm lead.
Secondary
× 1.5 2
52
= 0.0018
2.31 × 10 −2 × 310
which can be provided by 0.9 mm lead or 79 mm concrete at 80 kVp.
0.3
The secondary transmission should be less than
The total barrier thickness needs to be
Wall B
Primary radiation only will be included. Application of the Dixon and Simpkin (1998)
method requires that the primary transmission is less than
0.3 × (3.5 + 1) 2
52
= 0.00016 .
2.25 × 310
This transmission is achieved at 125 kVp with 2.7 mm of lead or 204 mm of concrete.
The equivalent shielding provided by the imaging assembly (xpre) is 0.85 mm and 72
mm of the two materials respectively (Table **) implying a wall thickness of 1.8 mm
lead or 132 mm of concrete.
Floor
The required primary transmission through the floor is less than
× (3.5 + 1) 2
52
= 0.00020
1.85 × 310
At 80 kVp this is achieved with 123 mm of concrete. For the floor, xpre = 74 mm so that
the required thickness of concrete is 49 mm.
0.3
7.1.4 Other points to consider
A&E
Skull tubes
Chest rooms
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
52
Table 7.1.1 Normalised workload and unshielded primary and secondary doses and
equivalent thicknesses of shielding in the image receptor and support from Dixon and Simpkin
(1998)
Workload per patient (mA.min)
Unshielded primary dose per
patient D1(0) mGy
Equivalent thickness xpre mm
Lead
Concrete
Unshielded secondary dose
per patient Dsec1 mGy
General radiographic room
Wall with
Floor and
All barriers
chest bucky other walls
2.45
0.601
1.85
Chest room
0.216
7.41
2.25
5.15
1.21
0.87
73
0.85
72
0.94
74
0.91
72
3.42 x 10-2
5.30 x 10-3
2.31 x 10-2
2.69 x 10-3
Table 7.1. 2
Primary attenuation
Lead equivalence
Concrete equivalence
Filtered beam transmission – A
Filtered beam transmission – B
60 kVp
0.0553
0.14
16.5
0.37
0.36
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
80 kVp
0.107
0.17
16.7
0.51
0.47
100 kVp
0.156
0.19
19.2
0.62
0.47
125 kVp
0.208
0.21
20.7
0.62
0.48
53
Table 7.1. 3
80 kVp
100 kVp
125 kVp
0.769
0.406
0.312
0.0017
0.89
0.801
0.450
0.360
0.0062
0.98
0.820
0.488
0.400
0.016
0.76
Chest
bucky
(125 kVp)
0.488
0.488
0.027
0.62
0.03
0.09
0.19
0.25
Table assembly
Tabletop primary transmission
Grid primary transmission
Combined transmission
Table assembly primary transmission
Pb equivalence of cassette holder +
table base
Transmission through cassette holder +
table base
Table 7.1.4
Examination
Lumbar spine AP
Lumber spine Lat
Lumbar spine LSJ
Chest AP
Chest PA
Chest Lat
Abdomen AP
Pelvis AP
Skull AP/PA
Skull Lat
Thoracic spine AP
Thoracic spine Lat
IVU
DAP Gy.cm2
Average
Upper limit
2.4
3.8
2.6
5.2
2.6
3.5
0.2
0.1
0.2
0.4
0.8
2.8
4.8
2.5
5.3
0.6
1.1
0.3
0.6
1.3
2.2
2.5
4.2
16
40
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
54
7.2 MAMMOGRAPHY FACILITIES
X-ray mammography possesses a number of unique properties when compared to
other x-ray modalities:
•
•
•
the maximum energy of the primary x-ray beam is in the range 25 - 35 kV, and will
typically be <30kV;
the typical unit, with a molybdenum anode and molybdenum filter is lightly filtered
(0.3 - 0.4 mm Al), giving a very low average x-ray energy;
equipment is designed so that the primary beam is constrained to fall within the
area of the image receptor, and therefore in practice only scattered radiation
needs to be considered.
Although this simplifies shielding assessments, there may be other mitigating factors
to be considered:
•
•
•
newer mammography units have multiple target/filter combinations, typically using
molybdenum/rhodium and tungsten/rhodium. These are specifically designed to
create a slightly ‘harder’ x-ray beam, with HVLs of 0.4 - 0.5 mm Al;
Health Building Notes do not give minimum sizes for mammography rooms, and
the equipment is often placed in rooms where the distance from the image
receptor to the nearest barrier will be within the range 1 - 2 metres. These rooms
will frequently be situated in or near out-patient clinics and office accommodation
where a high occupancy factor must be assumed;
mammography equipment is frequently used in mobile units as part of the Breast
Screening Programme, and thus consideration must be given to appropriate
standards of protection that will withstand the rigours of regular transportation.
IPEM Report 59 (2nd edition) (IPEM 1994) on >the commissioning and routine testing
of mammographic x-ray systems’ does not specifically deal with issues surrounding
room design, although it does refer to earlier work in the UK (Walker and Hounsell
1989). More recent information is available from the USA (Simpkin 1996).
7.2.1 Workload / Calculations
The 1986 Forrest Report on Breast Cancer Screening suggested a maximum
workload of 80 women per day, having two single-view mammograms each (or a
maximum of 160 mammograms per day). Data from a busy screening centre
suggests that 60 women per day, having an average of three films each, is a more
typical. For the purpose of this report, we will assume that the maximum is likely to be
200 films per day.
A pessimistic assumption of 30 kVp and 100 mAs per exposure has been used to
create a safety margin for actual usage (I don’t think that there is any reference for
this W&H use 35 kVp). At 30 kVp, the tube output is approximately 50 µGy mAs-1 at
1m or 140 µGy mAs-1 at 60cm, the typical distance to the image receptor.
Data from both the Walker and Hounsell (1989) and Simpkin (1996) give similar
values for the scatter ratios, although they are assessed somewhat differently.
Simpkin’s data cover a wider range of scatter angles and energies. He showed that
for an 18 x 24 cm2 film size, the maximum scatter ratio is 5.4 x 10-4 at 1630 and it is
0.9 x 10-4 at 900. The scatter ratio is defined as the ratio of scatter air kerma at 1m
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
55
from the patient to the primary dose at the image receptor.
From these data the maximum scatter air kerma (Ks) at 1 m per typical exposure at
100 mAs can be calculated:
Ks = 5.4 x 10-4 x 140 x 100 = 7.6 µGy
This is the maximum scatter intensity at 163°. For cranio-caudal views (i.e. with the
beam directed towards the floor, the scatter dose to a wall at a distance of 1 m will be
significantly less than this. However, for lateral and oblique views the dose to the wall
behind the tube will receive this level of dose. On the principle of specifying shielding
for the worst possible case, this dose will be assumed to be incident on a wall at 1 m
distance.
Multiplying by the workload data (200 films per day) and assuming 250 working days
per year, the annual incident scatter dose is shown to be 380 mGy.
7.2.2 Practical Solutions
The transmission data of section 5 can be used to determine the thicknesses of
material required to reduce the dose to the design criterion (0.3 mGy per year). The
required transmission is 0.3/380 = 7.9x10-4. Use of equation 5.1 and the data in table
5.5 results in the solutions shown in table 7.2.1. The table shows that normal building
materials and thicknesses are likely to be more than adequate to provide a sufficient
level of shielding.
No data have been presented to calculate the doses to rooms above or below the
mammography unit. Given the requirement for structural integrity for the floor or
ceiling suggests adequate protection at normal diagnostic x-ray energies, they will
certainly provide adequate protection.
The wall behind the patient will receive virtually no scattered radiation, since it will be
absorbed by the patient.
Protection of doors is a difficult issue since the amount of lead required is trivial. It is
worth noting however, that a 1 cm thick glass door will provide adequate protection
In the case of mobile units the data in Table 7.2.1 show that typical construction
materials would provide adequate shielding to fulfil the design criteria. Given the
nature of these units, the annual occupancy factor at any given location gives
additional margins for safety.
Data have not been presented to calculate the doses to the space below the mobile
mammography unit. Given the requirement for structural integrity for the floor and the
likely zero occupancy factor, adequate protection will almost certainly be guaranteed.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
56
Table 7. 2.1 Required shielding thicknesses for a wall at 1 m.
Material
Lead
Steel
Plasterboard
Wood
Concrete
Glass
Thickness (mm)
0.0814
0.4255
24.3
128
9.6
10.2
References
(1)
The commissioning and routine testing of mammographic x-ray systems. J
Law, DR Dance et al. IPEM Report 59, 2nd edition, 1994.
(2)
X-ray protection considerations for mammography screening centres. A
Walker and AR Hounsell. BJR, 1989, 62, 554-557.
(3)
Scatter radiation intensities about mammography units.
DJ Simpkin.
Health.Phys., 1996, 70(2), 238-245.
(4)
Review of mammographic equipment and its performance. NHS Breast
Screening Programme Publication 24, 1992.
7.3 R&F Rooms
Radiography and fluoroscopy rooms (R&F) are mainly used for barium contrast
studies. A typical room has an undercouch screening system with two x-ray tubes.
One is mounted in the tilting table for undercouch fluoroscopy and the second tube is
ceiling mounted and is used for radiography with a table bucky and possibly a vertical
bucky stand as well. An alternative is a system with a single column mounted
overcouch tube. For the radiation protection of the staff, this system would be used
remotely, i.e. with the Radiologist operating the set from behind the protective screen.
Other examinations which may be done in this room include ERCPs. The room may
also act as a back up for radiography, in particular it is not uncommon to use R&F
rooms for IVUs when barium contrast studies are not scheduled.
Barium contrast examinations have two parts, fluoroscopy and radiography. For
fluoroscopy the only significant radiation to be considered for shielding is scatter
because the transmitted primary will be heavily attenuated in the image intensifier
shield. Radiography contributes to as much as 90% of the total DAP (Hart et al.
1994). Images may be captured in a number of ways including directly from the
image intensifier in digital format, using a cut film camera linked to the image
intensifier output screen, or using a conventional film cassette positioned in front of
the image intensifier. In each case, the image intensifier mount provides local
shielding from the transmitted primary and shielding only needs to consider scattered
radiation.
For barium enemas large format film (35 x 43 cm2) may be needed for certain
projections. These have to be taken using a separate table bucky and x-ray tube.
However, the bucky assembly and table structure should be sufficient to attenuate the
transmitted primary radiation.
For undercouch screening tables the direction of maximum scatter is below the table
top and the table structure provides significant shielding. In addition, for scattering
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
57
angles less than 90° , there is considerable local shielding provided by the lead apron
attached to the image intensifier, the structure of the image intensifier mount, and its
shield.
Therefore, scatter doses are likely to be significantly overestimated.
Overcouch systems have little local shielding so that the doses to the walls will be
much greater.
7.3.1 Workload
Average DAPs for barium contrast studies have been published by Hart et al. (1996).
These data are reproduced in Table 1. In addition data are included for ERCPs. A
busy department might perform 25 barium enemas and 25 other contrast studies per
week, i.e. 10 patients per day. It can be seen that with these patient numbers, the
total weekly DAP would be in the region of 1000 Gy.cm2. This figure will be used for
design purposes.
7.3.2 Practical solutions
Shielding for an R&F room which is 6.5x5.9 m2 will be calculated. This is slightly
larger than Health Building Notes recommendations It will be assumed that the table
is positioned as close as possible to one of the walls at a distance of 1.6 m. The
protective screen and room doors are each 2.5 m from the centre of the table. Barium
examinations are generally carried out at high kV and an average value of 100 kV is
assumed. The maximum scatter factor (Smax) at a distance of 1 m is given by
equation (4) in Chapter 4.1. At 100 kV, Smax = 5.6 µGy (Gy.cm2)-1. This is for a wall
parallel to the central axis of the beam which will be assumed to correspond to the
geometry for each If the barriers to be considered. The maximum weekly scatter dose
at 1 m is therefore 5.6 mGy for the assumed workload (1000 Gy.cm2 per week).
Wall
2
Required transmission <
0 .3
1 .6
×
= 0.26%
5.6 × 52 1
At 100 kV this requires 1.4 mm lead or 120 mm of concrete (1800 kg m-3).
This is the specification for the wall closest to the examination table but it
would probably be applied to all walls.
Door and protective screen
2
Required transmission <
0.3
2.5
×
= 0.64%
5.6 × 52 1
At 100 kV this requires 1.0 mm lead. A 1 mm lead door is therefore sufficient
particularly as the occupancy directly behind the door will be significantly less
than 100%. However, the screen will also be used to shield films in cassettes
and a dose constraint equivalent to 60 µGy per year has been recommended.
The shielding requirement is then to provide less than 0.16% transmission
which requires 1.6 mm lead. This demonstrates that the standard 2 mm lead
protective screen should be provided in this room.
Floor/ceiling
Floor shielding should be considered for undercouch systems and ceiling
protection for overcouch. The maximum scatter is back towards the tube and
is approximately 10 µGy (Gy.cm2)-1 at a distance of 1 m. It may be assumed
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
58
that a person standing in the room below or above is at a distance equal to the
floor-to-ceiling height. This is generally not less than 3.5 m so that the
required transmission is given by:
2
<
0.3
3.5
×
= 0.70%
10.0 × 52 1
This can be achieved using 1 mm lead or 93 mm concrete (1800 kg m3). Most
modern structures will provide this level of shielding.
Other considerations
For part of the examination, particularly for barium swallows and meals, the table will
be tilted to the vertical position. This will increase the amount of scatter to the wall
behind the x-ray tube. This may need to be considered if the wall is particularly close
to the set and it may influence the shielding specified for the door if it is in this
position.
A vertical bucky may be used in the room.
required in accordance with section 7.1.
Table 7.3.1
Shielding behind the bucky may be
Typical DAP values for examinations performed in an R&F room
Barium contrast study data from Hart et al. (1996). ERCPs from
Williams (personal communication).
Examination
Barium enema
Barium follow-through
Barium meal
Barium swallow
ERCP
Ave DAP
(Gy.cm2)
27.0
12.0
13.0
9.8
11.0
7.4 C-ARM EQUIPMENT
The general dose constraint of 0.3 mGy per year. Since C-arms are not generally
used with film-screen systems, there should be no need for more stringent dose
targets. The dose constraint may be relaxed when occupancy is considered.
However, this type of room is likely to be surrounded by working areas such as
recovery rooms, nursing stations, etc. so that occupancy is unlikely to be less than
25%.
Calculation of structural shielding for C-arm x-ray sets is relatively simple because
the only significant source of radiation is scatter from the patient. There should be
no possibility of primary exposure since it is a requirement that under all operating
conditions the x-ray beam falls entirely within the area of the image intensifier face
and its surround, and that the housing has a lead equivalence of at least 2 mm.
In Chapter 4.1 it was shown that the intensity of scatter is directly related to DAP
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
59
rate and is a function of scattering angle and kV. For the situation in which the xray beam is parallel to a wall, equation (4) from Chapter 4.1 can be used to show
that the maximum dose due to scatter at a wall 1 m from the beam centre varies
from 4.7 to 5.6 µGy (Gy cm2)-1 for 70 to 100 kV x-rays respectively. This is the
approximate kV range used for the more common procedures comprising the
majority of workload for these sets. The dose is greater if the tube is angled
towards the wall and may increase to approximately 10 µGy (Gy cm2)-1. The
narrow range of values relative to the inherent uncertainties in calculation of
shielding permits the use of a single factor which for the purpose of this report is
taken as 6 µGy (Gy cm2)-1. Inverse square law (ISL) can be applied to calculate
maximum scatter doses at greater distances.
C-arms are used for a variety of procedures which include angiography,
interventional radiology, in orthopaedic surgery, and endoscopy. In these
situations, the procedure is carried out in a relatively large room to allow
unimpeded access around the patient. Health building notes recommend room
sizes of 40 m2 for an operating theatre and 38 m2 for a specialised radiology room.
It is unlikely, therefore, that any side of the room will be much less than 6 m and
since the bed or patient support is generally positioned centrally in the room, the
minimum practical distance between the centre of the beam and any wall is 2.5 m.
Although individual rooms may need special calculations, for the purpose of
general guidance it can therefore be assumed that the maximum scatter dose on
any wall is unlikely to exceed 1 µGy (Gy cm2)-1.
7.4.1 Workload
The workload is expressed in terms of total DAP. There have been a number of
published surveys of DAP arising from high dose x-ray procedures. Some of these
are summarised in Table 1. It is difficult to use these data to estimate the daily
workload for the planned new room because of the uncertainty in the mix of
procedures, local clinical practice and in the projected case numbers. Although the
dose per case is relatively high, the daily patient throughput is likely to be low
compared with other rooms because of the extended time needed for each case.
For example a busy Cardiac Lab is unlikely to exceed 10 cases in a standard (8
hour) working day. Table 2 summarises audit data collected for 5 rooms with Carm x-ray sets. These values illustrate the range which may be anticipated. The
maximum weekly DAP for these five rooms was 1750 Gy cm2.
The most common use of C-arms in theatres is in orthopaedics and the area of
most frequent use is in trauma. With modern sets fitted with last image hold, pulse
fluoroscopy, thermal printers, etc., DAP values should be low for most cases (of
the order of a few cGy cm2. However, certain procedures may require significantly
higher doses. An audit of cases in a busy trauma theatre showed that the average
weekly DAP was 22 Gy.cm2 for a total of 28 patients for whom the C-arm was
used.
7.4.2 Practical solutions
A. Cardiac Lab.
Figure 7.4.1 shows the layout drawing for a cardiac lab formed out of an existing
facility. The layout was dictated by the need to have patient access from the left
side of the room as shown in the drawing. The x-ray set was angled in order to
allow trolleys to be taken into both the preparation and recovery areas. This also
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
60
served to maximise the working space for the cardiologists. The protected area is
used during the procedure principally by the physiological measurement
technician. It is situated at the foot end of the table allowing the technician to have
a clear view of the patient and cardiologist. It was the local preference to have
open access between the x-ray room and the protected area so that there would
be direct voice communication between the technician and cardiologist without the
need for an intercom system. Access to the protected area does not need to be
through the x-ray room which is important both for radiation protection and for
control of infection. It allows ready access for other staff to observe procedures
and to communicate with those in the room.
The total area of the room is 36.6 m2 which is marginally less than is
recommended in Building Note 6. Under normal operating conditions, the nearest
distance between the area under examination and any wall is 2.6 m. It has been
assumed that at this distance the scatter dose is 1 µGy (Gy cm2)-1.
For the shielding specification, the maximum workload has been taken as 50%
greater than the maximum for a cardiac lab in Table 2, that is 2600 Gy.cm2 per
week. The resultant maximum annual scatter dose to the nearest wall is
approximately 140 mGy. With 100% occupancy, the 0.3 mGy annual dose
constraint leads to a requirement for less than 0.21% transmission. Typically
cardiac procedures are carried out at 80 kV. This shielding would be achieved
with 0.9 mm lead or 100 mm concrete (1800 kg m-3). However, it would be
prudent to assume a higher kV. At 100 kV 1.5 mm lead or 130 mm concrete
would be needed.
This example is one in which conservative assumptions on workload, occupancy,
and kV move the shielding specification towards the 2 mm of lead solution. More
realistic assumptions would however suggest that 1 mm of lead is sufficient and
this would be the preferred option for doors to the recovery and preparation areas
in which occupancy will be less than 100% and the people in the room would
normally work at least 1 m further away than the door itself.
Protection to the floor also needs to be considered. The maximum scatter dose is
likely to be 10 µGy (Gy cm2)-1 at a distance of 1 m. The midline of the patient is
approximately 1 m above the floor and with a standard floor-to-floor height of 4 m,
the distance from mid-trunk of a person standing in the room below will be about
3.5 m from the source of scatter. This annual scatter dose is then given by:
2
1
10 × 10− 3 × 2600 × 52 × ≈ 110 mGy
3. 5
For 100% occupancy this leads to a transmission specification of less than 0.27%.
This can be achieved with 90 mm concrete (1800 kg m-3). This corresponds to the
average thickness of a typical concrete slab floor.
B. Orthopaedic theatre
The following data have been assumed:
• Distance to nearest wall - 3 m
• Workload - 25 Gy.cm2 per week
• Maximum scatter dose at 1 m - 6 µGy (Gy.cm2)-1
• Dose constraint - 0.3 mGy/year
• Occupancy of adjacent areas - 33%
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
61
• Average operating potential - 90 kV
Occupancy is assumed to be less than 100% because the theatre is in 24 hour
use and no individual member of staff is liable to be in the vicinity for more than
one-third of the time that the set is in use.
The required maximum transmission level is given by:
2
3
× = 104%
−3
(25 × 0.33 × 52 × 6 × 10 ) 1
0.3
This implies that no protection is required on the walls of this theatre in order to
achieve a dose constraint of 0.3 mGy per year to adjacent areas. Even at three
times the workload, the required shielding would be achieved with 22 mm of
plasterboard showing that theatres do not normally need additional shielding even
if lightweight construction walls are used.
However, theatres used for
intraoperative interventional procedures could require significant shielding. These
procedures are likely to become more common in the future.
C. Coronary care unit
C-arms are used in coronary care units. Typically the DAP for the insertion of a
temporary pacemaker is about 5 Gy cm2 (I have made up this figure, I am getting
some better data). These are relatively infrequent procedures with normally fewer
than 2 patients per week. The average weekly DAP is therefore unlikely to exceed
10 Gy cm2. The procedures rooms in which pacing is done tend to be relatively
small so that less attenuation is provided due to ISL.
The following data have been assumed:
• Distance to nearest wall - 1.5 m
• Workload - 10 Gy.cm2 per week
• Maximum scatter dose at 1 m - 6 µGy (Gy.cm2)-1
• Dose constraint - 0.3 mGy/year
• Occupancy of adjacent areas - 25%
• Average operating potential - 80 kV
Transmission calculation:
2
0.3
.
15
× = 22%
−3
10 × 52 × 6 × 10 × 1 1
This can be achieved with 0.1 mm lead or 30 mm plasterboard. Using double
thickness plasterboard would therefore provide sufficient protection on a light
weight wall. In practice it is likely that only one area of the wall would require this
level of protection. It might also be legitimate to assume that the person on the
other side of the wall will be at a significantly greater distance than 1.5 m from the
centre of the x-ray beam.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
62
Table 7.4.1. Typical doses from angiography and interventional procedures. These
data are averages from the following sources: (1) Vano et al, BJR, 68, 1215 (1995),
(2) Marshall et al, BJR, 68, 495, (1995), (3) Steele and Temperton, BJR, 68, 452,
(1993), (4) Williams, BJR, 70, 498, (1997), (5) Broadhead et al, BJR, 70, 492, (1997),
(6) Zweers et al, BJR, 71, 672 (1997), (7) Betsou et al, BJR, 71, 634 (1997), (8)
McParland, BJR, 71, 175 (1997), (9) Ruiz Cruces et al, BJR, 71, 42 (1997) and (10)
Williams (personal communication).
Procedure
Cerebral angiography
Coronary angiography
Abdominal angiography
Femoral angiography
Cerebral embolisation
PTCA
TIPSS
Table 7.4.2
No of
studies
5
5
4
6
3
5
6
DAP
Gy cm2
53
40
120
60
110
55
260
DAP range
Gy cm2
24 - 74
23 - 67
61 - 180
30 - 88
105 - 122
13 - 88
77 - 524
Refs
1,2,3,8,10
1,5,7,10
4,8,9,10
1,3,4,8,9,10
2,8,10
1,5,7,10
1,4,6,8,10
Results of dose audit in 5 x-ray rooms used for high dose procedures.
Cardiac Lab – 1
Cardiac Lab – 2
Vascular studies
Hepato-biliary interventions
Neuroradiology
Weekly workload
No of cases
DAP Gy cm2
44
1150
35
1750
23
1700
12
850
11
450
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
63
7.5 CT INSTALLATIONS
7.5.1 INTRODUCTION
When a patient undergoes an examination in a CT scanner, the X-ray
tube is rotated in a 360o arc around the body. Tube potentials of 120-140 kVp
are employed which give high levels of Compton scattered radiation. The
dose distribution is well defined and reproducible, because the position of the
gantry is fixed and the X-ray tube follows the same path in space for each
rotation. The gantry provides shielding against the primary beam and the
scatter pattern is determined by the volume of tissue irradiated and intervening
absorber in the form of the gantry and the patient’s body. Examinations of the
trunk tend to produce more scatter than head scans because a larger volume
of tissue is irradiated, but the level of scatter behind the gantry for head scans
may be greater because there is less tissue beyond the irradiated volume to
provide attenuation. The resulting pattern of scattered radiation has the
appearance of an hour glass, which has 360o symmetry about the axis of
rotation ( figure 7.5.1). The dose distribution which depends on exposure
parameters, beam collimation, filtration and gantry shielding is characteristic
for each type of scanner. Dose distributions provided by manufacturers should
be employed to determine shielding requirements. Because the magnitude of
the dose distribution varies dramatically with position, the orientation of a
scanner within a room must be decided before shielding requirements are
finalised.
7.5.2 METHODOLOGY
Information on scatter levels provided by manufacturers usually takes
form of isodose curves for a single slice using particular scan parameters and
phantoms. Two drawings are required, one in the horizontal plane (floor plan)
and one in the vertical plane (elevation). Sometimes only a single contour at a
particular dose level is provided or a sequence of doses measured at a range
of positions at the same distance from the isocentre. In such cases it should be
assumed that the dose declines with distance from the isocentre according to
an inverse square law at distances beyond the limit of dose contour plots. The
decline in scatter with distance from the isocentre may be plotted for critical
directions to determine the dose level at relevant boundaries (figure 7.5. 2).
Scatter diagrams provided by X-ray companies would normally have been
produced using standard PMMA phantoms representing the head (16 cm
diameter) and body (32 cm diameter). Scatter from a body phantom may be
20-100% higher than that from a head phantom when the same exposure
factors are used, as a result of the greater volume of tissue irradiated and the
use of different filter options. Self-shielding by the body is generally not
included and may reduce the dose by 50% in certain directions. However, It is
not recommended that any adjustments are made to allow for this, since it will
depend on body size and the scanner will be used to scan phantoms during
QA tests.
In order to estimate dose levels from scatter plots, the workload in the
department must be predicted in terms of the scan parameters used.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
64
Information on the likely breakdown of cases between head and trunk together
with typical numbers of slices for standard examinations is required from the
department. Data on recommended scan protocols in terms of mAs and kV
should be obtained from the X-ray company. There is little difference in scatter
levels for standard and helical scans if a similar pitch is used for each (Langer
and Gray 1998), but since the time taken for helical scans may be 50% less,
there is likely to be a larger patient throughput. Current helical scanners
cannot achieve double the workload without reaching heat limits, so an
assumption of a potential 50% increase in workload when a standard scanner
is replaced by a helical one may be reasonable. Patient throughput may
increase as tube technology improves.
Scatter plots are usually given for a single slice with a typical mAs or
other specified mAs value. These should be used to determine doses at critical
positions. These will be not only at nearest distances to individual barriers
such as walls, doors and control cubicles, as in other X-ray rooms, but, more
importantly, in directions of greatest scatter. It is helpful to sketch isodose
contours onto a scaled plan of the X-ray room in order to identify parts of the
walls exposed to the highest dose levels and so the directions and angles
which are the most critical (figure 7.5. 2). These directions can then be
identified on the manufacturer’s isodose plot using a protractor and the scaled
distances read off for each dose contour. Results should be plotted in a
logarithm-linear format (figure 7.5. 3) to determine the dose at the distance of
the barrier. Isodose scatter curves are usually also provided in a vertical plane
through the scanner. It is important that consideration is given to shielding in
the floor and ceiling since the level of protection required for modern helical
scanners may be greater than that provided by a standard concrete floor
(Langer and Gray 1998).
The scatter plots provide data on doses for a standard slice and this
must be multiplied by the number of slices in a given period and the ratio of the
actual mAs to that used in deriving the scatter plot. The scatter dose is usually
directly proportional to the slice width, so a simple ratio adjustment can be
used to relate results to a standard thickness (e.g. 10 mm). The same principle
may not be true for thin slices on some scanners (e.g. 1 mm), but the
contribution made to the total workload is usually small. Relative contributions
to scatter dose from different slice widths can be assessed from values of the
computed tomography dose index (CTDI) which provides a measure of the
radiation dose per mAs from one slice. If CTDI values are similar, then dose
will be proportional to slice width. As reference patient doses are set in terms
of the weighted computed tomography dose index (CTDIW ) using CTDI values
measured at the periphery and centre of perspex whole body or head
phantoms (CEC 1997) or dose length product (DLP), it may be possible to
base exposure parameters for standard examinations upon these values.
There are differences in scatter for head and body scans. These can be
equated in terms of the ratio of scatter doses from one slice in each phantom
for a given mAs. This can be determined from the decline in scatter dose in
several directions for the two configurations. It is simplest to relate all to a set
of factors for which a scatter plot is available. The one representing the bulk of
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
65
examinations to be performed on the scanner should normally be used. In
some cases an isodose plot may only be available for either a head or body
phantom. If this is the case and no other data is available on relative scatter
levels, conservative assumptions should be made. When only data for a head
scan is available, conversion to the scatter dose for a body with similar
exposure factors should be represented by multiplication by a factor of two,
while when only data for a body scan is available, the same scatter dose per
mAs should be used for the head.
The dose permitted in each adjacent area, including occupancy factors,
should be divided by the unshielded dose from the scanner at that position to
determine the transmission required for each barrier. Once the required
transmission has been established the thickness of a barrier with the
appropriate transmission for 120 kVp or 140 kVp X-rays can be determined
from figure 5.10 or Table 5.7 These data on X-ray transmission were derived
using the formula of Archer et al (1983) fitted to results derived by Simpkin
(1990) using X-ray spectra typical of the primary beams of CT scanners at 120
kVp (filtration 5.8 mm Al, half-value layer 6.9 mm Al) and 140 kVp (filtration 6.8
mm Al, half-value layer 7.3 mm Al).
EXAMPLE
A CT scanner in a busy city hospital is to be located in a room
measuring 6.5 m x 5.8 m (area 38 m2, Building Note 6) with the operator’s
cubicle in an adjacent room. The separation of floor and ceiling slabs is 4.0 m.
Each is constructed from 140 mm thick lightweight concrete (density 1840 kg
m-3). The scanner isocentre is located 0.9 m above floor level. Isodose curves
have been provided for a 120 kVp, 250 mAs, 10 mm slice on a 320 mm
diameter PMMA body phantom and a 350 mAs, 10 mm slice on a 160 mm
diameter head phantom.
The scanner is to be located towards the right hand side of the room as
shown in the plan (figure 7.5. 2). Patients will enter through the double door on
the left hand wall. The scanner is positioned at an angle of 30o so that the
operator can obtain a good view of the lower half of the scanner. The door
from the cubicle into the room is located in the corner to minimise space
requirements and the operator cubicle window extends for most of the
remaining length of the wall to provide a complete view of the scanner and
other door.
The projected workload for the CT scanner comprises 120 body and 80
head examinations per week. An average body examination in the department
comprises 22 slices of 10 mm width at a pitch of 14 mm, with exposure factors
of 120 kVp and 250 mAs per slice.
Number of 250 mAs body slices per week = 120 x 22 = 2640 slices
An average head examination consists of ten slices of 10 mm width and five
slices of 5 mm width, with exposure factors of 120 kVp and 350 mAs per slice.
The isodose plots indicate that the scatter dose per mAs from a 10 mm slice
through the head is half that from a slice through the trunk.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
66
Number of 350 mAs, 10 mm head slices per week = [10 +(5 x 5/10)] x 80 = 1000
Equivalent no. of 250 mAs, 10 mm body slices
week
for head examinations performed each week
= 1000 x 350 = 700 slices per
250 x 2
The total workload is equivalent to 2640 + 700 = 3340 body slices of 250 mAs
and 10 mm width per week. Therefore a workload of 3340 slices per week with
parameters similar to those used to obtain the isodose plots (figure 7.5. 2) has
been assumed. Calculation of the shielding requirement for one wall (A) (figure
7.5. 2) is given below.
Wall A
The maximum dose contour extends at an angle of 150o directly
towards the wall which is at a distance of 2 m from the isocentre. The dose per
slice at the wall, determined from the plot in figure 7.5. 3, is 2.0 µGy.
The dose per week from 3340 slices = 3340 x 2.0 µGy = 6680 µGy
The dose to other persons from the scanner is to be kept below 300 µSv per
year, which is equal to 6 µSv per week. The area beyond the wall is a viewing
area, where the occupancy is estimated to be 0.5.
The required transmission for the barrier =
6
6680 x 0.5
= 0.0018
This transmission is provided by 1.8 mm of lead or 160 mm of concrete
(Chapter ?, figure 7.5. ?, Table ?).
Roof
The dose contours provided only extend to 1.5 m above the isocentre.
The highest dose contour along the length of the scanner corresponds to 2.1
µGy from a single slice at a distance of 1.7 m from the isocentre in a direction
36o from the vertical. The sensitive organs of a person on the floor above will
be 0.6 m above the ceiling if seated and so will be a height of 3.7 m above the
isocentre. The distance along the line of greatest scatter will be (3.7/cos 36o)
m = 4.6 m. Applying an inverse square law correction along the line of greatest
scatter will give:
Dose from slice at distance 4.6 m from isocentre = 2.1 x 1.72/ 4.62 µGy = 0.28 µGy
The dose per week from 3340 slices = 3340 x 0.28 µGy = 935 µGy
The space above the CT room is a ward, where patients and staff could be
present throughout the day, so an occupancy of 1.0 is assumed. If a dose
criterion of 6 µSv per week is applied.
The required transmission for the barrier = 6/935 = 0.0064
This transmission would be provided by 120 mm of standard concrete
(density 2350 kg m-3) (figure 7.5. 4) or 120 x 1840/2350 mm = 153 mm of
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
67
lightweight concrete.
The protection already present in the floor is 140 mm of lightweight
concrete. The thickness along the line of scatter is 140/cos 36o = 173 mm.
Because radiation is incident obliquely, an equivalent barrier thickness equal to
the mean of the actual thickness and that in the direction of scatter is
assumed, equal to 156 mm. Thus the protection provided by the structural
concrete in the floor is sufficient. The thickness of barrier (B) required to
attenuate radiation incident at angle θ can be calculated from the equation B =
T ( 1 + cos θ ) / 2, where T is the thickness of material to provide the required
attenuation. Thus for this example B = 153 x ( 1 + cos 36o) / 2 mm = 138 mm
of lightweight concrete.
7.5.3 THINGS TO LOOK OUT FOR
Rooms smaller than the 38 m2 recommended are frequently used and
here walls intercepting the direction of high scatter may need considerably
greater protection. It may in some cases be appropriate to include additional
lead sheets localised to the area of high scatter (Harpen 1998), but care must
be taken to ensure that additional protection of this type is located in the
correct position.
Floor and ceiling slabs in new buildings are often thinner as well as
being made from lightweight concrete and may require additional protection.
Concrete floors and ceilings are often poured on a metal base with a ridged
cross-section, giving a trapezoidal variation in thickness, for which the
minimum thickness, which should be used in calculating the protection, may
only be 800 mm.
The height of shielding in walls must be given careful consideration as
shielding to a height of 2 m is unlikely to be sufficient for a CT installation.
Shielding would normally be to the full height of a room in directions where the
scatter is high, since the level of radiation scattered from the ceiling slab into
an adjacent room may exceed the dose criterion set. This becomes of greater
importance in rooms significantly smaller than the size recommended. In
rooms with false ceilings it may be necessary to extend the wall shielding to
the roof slab. In these configurations the level of protection required in the
upper part of the room is unlikely to be as high as that in the low walls, since it
is required primarily to offer protection against secondary scattered radiation
and the process of scattering from a concrete barrier will reduce the dose-rate
to about 1% of that incident on the ceiling slab (McRobbie 1997). If the
distance between the false ceiling and the ceiling slab is large it may be more
cost effective to include the lead in the false ceiling, as this will provide
additional protection to both the floor above and adjacent rooms.
The control cubicle for a CT scanner would usually have a continuous
shielded boundary, including a protected door. If a department does not wish
to include a door, calculations must be performed to ensure that levels of
radiation scattered from adjacent walls will not result in the required dose-rate
being exceeded.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
68
REFERENCES
Archer BR, Thornby JI and Bushong SC (1983). Diagnostic X-ray shielding
design based on an empirical model of photon attenuation. Health Physics 44,
507-517.
Commission of the European Community (CEC) (1997) Quality criteria for
computed tomography. CEC Working Document EUR 16262.
Harpen MD (1998) An analysis of the assumptions and their significance in the
determination of required shielding of CT installations. Medical Physics, 25,
194-198.
Langer SG and Gray JE (1998). Radiation shielding implications of computed
tomography scatter of exposure to the floor. Health Physics 75, 193-196.
McRobbie DW (1997). Radiation shielding for spiral CT scanners. Brit. J.
Radiol. 70, 226.
Simpkin DJ (1990).
Transmission of scatter radiation from computed
tomography (CT) scanners determined by a Monte Carlo Calculation. Health
Physics 58, 363-367.
Figure Captions
Figure
Isodose contour map showing the form of the scatter dose distribution in the
7.5. 1
horizontal plane for a 10 mm slice through a head phantom using 120 kVp
and 350 mAs.
Figure
Plan (a) and elevation (b) of CT room with isodose contours sketched in for a
7.5. 2
10 mm slice using 120 kVp and 250 mAs for a phantom. Walls for which
shielding calculations have been performed are labelled A-H.
Figure
Plot of scatter dose verses distance in the directions A - H in the plan shown
7.5. 3
in figure 7.5. 2.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
69
Table 1
Data from calculation of shielding for each wall in example
Description
Code
Use of adjoining room
Distance
(m)
to
barrier
Wall
Wall
Window
Door
Wall
Door
Roof
Floor
A
B
C
D
E
F
G
H
Viewing
Room
Office
Operator
Operator
Corridor
Corridor
Ward
Plant
Room
2.3
2.2
3.5
4.6
4.2
4.3
3.1
0.9
4.6
4.2
Distance to nearest
person (m)
Dose per 250 mAs
body slice
2.0
2.1
0.43
0.20
0.43
0.056
0.30
0.36
6546
7014
1450
655
1450
187
1005
1188
0.5
1
1
0.5
0.2
0.5
1
0.2
0.0018
0.0009
0.0042
0.018
0.02
0.064
0.0064
0.02
Lead Thickness (mm)
1.8
2.1
1.5
1.0
1.0
0.6
1.4
1.0
Concrete
(mm)
160
170
120
95
Lightweight concrete
thickness (mm)
138
110
Lightweight concrete
barrier
thickness
(mm)
153
121
Dose / wk (µGy)
Occupancy
Transmission
thickness
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
90
70
Figure 7.5.1
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
71
Figure 7.5.2 a
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
72
Figure 7.5.2b
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
73
Dose per slice (microGray)
100
10
A B
C
D
1
E
F
GH
0.1
0.01
0.01
0.1
1
10
2
1/(distance)
Figure 7.5.3
7.6 DENTAL X-RAYS
Shielding design for dental radiology may be considered a trivial exercise in
comparison to medical radiology because of the relatively low radiation doses.
However, the problem should not be completely dismissed for a number of reasons.
• Dental surgeries are rarely purpose built. Surgery layout may be compromised
with, for example, the x-ray set being used close to a wall.
• It is not uncommon for a dental practice to have a single set in a separate room to
serve two or three surgeries. In these circumstances the designated room may be
very small.
• General Dental Practitioners own there own premises and additional expenditure
on shielding may represent a significant increase over the cost of the x-ray set.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
74
Intra-oral radiography
For intra-oral radiography, the following dose data may be used as guidance:
Entrance surface dose (ESD): 1 to 10 mGy
Depends on projection, patient size, film speed, kV, focus-skin distance,
etc.
Field area at tip of spacer:
28 cm2 (6 cm diameter collimator)
12 cm2 (rectangular collimator)
Dose area product (DAP): 1 to 30 cGy cm2
Based on ESD and area
Applied voltage: 50 to 70 kV
Scatter factor (S): 3 to 8 µGy (Gy cm2)-1
For a 60 kV set used with E-speed film, ESD should be approximately 2 mGy. With
circular collimation, the maximum scatter dose at a distance of 1 m would be:
Scatter dose = 2 x 10-3 x 28 x 8 = 0.45 µGy per film
The primary beam in intra-oral radiography should always be intercepted by the
patient. Transmission of the primary depends on many factors. For the purpose of
shielding calculations it can be assumed that primary transmission is no greater than
2 µGy per film.
Assuming that intra-oral films are taken with the beam pointing in one of three
directions (corresponding to the patient’s left, right and straight on), and that each of
these directions is equally probable, then the weighted average primary plus scatter
dose at a distance of 1 m is 1 µGy per film. It is recommended that this single value is
used for shielding specifications unless there is good reason to suggest that the dose
might be significantly different.
Table 7.6.1 shows the required attenuation for a range of barrier distances and weekly
workloads based on an annual dose constraint of 0.3 mGy.
An indication of the number of films taken in dental practice can be inferred from
NRPB (1994). Using data from the Dental Practice Board, it was reported that the
average number of radiographs taken in the General Dental Service in the period
1990 to 1993 was 16.47 million per year using 17,100 x-ray sets. This is equivalent to
960 films per year or just under 20 films per week on each set.
The following conclusions may be made from the data in the table:
• No shielding is required if the workload is no more than 20 films per week and the
distance between the patient and the wall is at least 2 m.
• Surgery walls using brick or blockwork should provide sufficient protection in any
circumstance. At 70 kV (generally the upper kV limit for intra-oral radiography),
100 mm concrete block with a relatively low density (1500 kg m-3) transmits less
than 0.2%.
• Partition walls with 10 mm plasterboard on both sides will provide sufficient
protection in most circumstances. 20 mm of plasterboard has approximately 25%
transmission at 70 kV. The Table indicates those situations in which this amount
of shielding may be inadequate.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
75
Panoramic radiology
For panoramic dental x-ray sets, shielding calculations need only be made for scatter
radiation since the cassette and cassette holder provide sufficient shielding for the
radiation transmitted through the patient.
DAP can be used for scatter dose calculation. For equipment working with rare earth
screens, DAP should be in the range 5 to 15 cGy cm2. The maximum scatter dose
factor for a fixed point can be calculated by integration of the scatter dose curve.
Between 30° and 150° , i.e. through a 120° rotation representing half of the full
movement, the average scatter factor is equal to 4.7 µGy (Gy cm2)-1 at 85 kV. The
maximum scatter dose at 1 m will therefore be 0.7 µGy per examination. However, it
is likely that the unit will be mounted closer to the wall than this and incident doses at
the wall between 1 and 2 µGy per examination might be expected.
Example
Distance to wall = 70 cm
Scatter dose = 0.7 / (0.7)2 ≈ 1.4 µGy
Transmission through 20 mm plasterboard = 35% (at 85 kV)
Max. no of examinations per week without additional shielding
= 300/(1.4 * 0.35 * 52) = 12
In practice this is a conservative estimate since it is unrealistic to assume
continuous occupancy directly behind the wall.
General
It may be necessary to consider shielding for windows and doors. A window with 5
mm glass provides only 50% attenuation at 70 kV. However, in practice it is unusual
to have high occupancy immediately outside a window and inverse square law is
normally a sufficient attenuator.
Internal doors could be a problem but these are also unlikely to be close to the patient
unless the x-ray room is very small. In that situation, the operator may need to stand
outside the door to be 2 m from the patient and he/she would control access to the
area outside the door.
For most intra-oral projections, the x-ray beam lies within 15° of the horizontal.
Shielding to floors and ceilings is therefore only needed for scatter radiation. Even
with a low floor-to-ceiling height (3 m) it is very unlikely that the workload would be
sufficient to require any additional shielding.
The most cost effective dose for additional shielding is generally the use of an extra
sheet of plasterboard. This would only be needed over restricted areas of the wall
towards which the beam might be directed and generally within a distance of 1.5 or 2
m from the patient.
No account of occupancy has been used in these calculation. However, within the
dental premises it is unlikely that there would be many adjacent rooms for which less
than 100% occupancy can be assumed.
Reference
NRPB (1994) Guidelines on radiological standards for primary dental care. Docs of
the NRPB, 5(3).
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
76
Table 7.6.1 Maximum transmission permitted for a dose constraint of 0.3 mSv per
year as a function of workload and barrier distance. Data based on average scatter
plus primary dose equal to 1 µGy per film at a distance of 1 m from the patient.
Films/week
10
20
50
100
200
1
0.58
0.29
0.12
0.06
0.03
Barrier distance (m)
1.5
2
2.5
0.65
0.26
0.46
0.72
0.13
0.23
0.36
0.06
0.12
0.18
3
0.71
0.35
7.7 MOBILE RADIOGRAPHY
Mobile X-ray Equipment – DRAFT 2
When it is not possible or advisable to move patients, such as those in NNU, PICU,
ITU and resuscitation rooms, mobile radiographic equipment provides the only
feasible radiographic option. In most cases, the need for primary and secondary X-ray
shielding will be obviated by the relatively low kV used, the relatively low levels of
scattered radiation produced and the infrequency of examinations. However, practical
limitations e.g. the unpredictable nature and urgency of procedures in recusitation
rooms, should be taken into account. In many ways, as far as radiation shielding is
concerned, the use of mobile or ceiling suspended X-ray equipment (as in some
resuscitation rooms) is analogous to the use of static X-ray equipment in X-ray
departments. Hence, shielding for surrounding walls, floors and ceiling can be
assessed in a similar way to that used for radiography carried in a purpose designed
X-ray room.
There are three potential sources of exposure of staff to ionising radiation: leakage
radiation; primary radiation; scattered or secondary radiation.
Leakage Radiation
Weight is an important consideration in the design of mobile X-ray equipment. The
specified upper limit of 1mGy at 1m in one hour for radiation leakage is used as a
fixed constraint in the design of X-ray tube primary shielding. Hence, at comparable Xray beam mean energies, the leakage radiation from mobile X-ray equipment will be
higher than from most static X-ray equipment. Simpkin (Simpkin, 1998) has calculated
that a primary shield thickness of 2.32mm, 2.20mm and 1.93mm of lead placed
around a diagnostic X-ray tube is sufficient to reduce the leakage air kerma to
0.87mGy at 1m for a X-ray tube in continuous operation at respectively: 150kV,
3.3mA; 125, 4mA; 100kV, 5mA. In table 1, figures adapted from Simkin (Simkin,
1998) show the leakage radiation’s air kerma values at 1m (obtained with the three
preceding shielding thickness’) for a range of kVs and for an exposure of 10mAs.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
77
kVp
150
125
100
80
60
2.32mm of Pb
10mAs (nGy)
737
426
165
3.0
<<1
and 2.20mm of Pb
10mAs (nGy)
NA
608
240
5.2
<<1
and 1.93 mm of Pb and
10mAs (nGy)
NA
NA
487
15.9
<<1
Table 1. Unshielded leakage radiation air kerma values at 1m with the minimum X-ray
tube shielding in place for an exposure of 10mAs (adapted from Simpkin, 1998).
In most cases, apart from when equipment is used at the highest kV, leakage
radiation may be neglected.
Primary and Secondary Radiation
Shielding for primary and secondary radiation is best considered in relation to the
situation in which the X-ray equipment is being used.
Mobile Radiographic Equipment used in NNU and PICU
Workload distributions
Figures 1 and figure 2 show workload distribution from one hospital’s NNU and PICU.
The distributions have been compiled from over 700 records. Although these workload
distributions should be treated with caution, it is not unreasonable to postulate that the
distributions are reasonably representative of the situation in other hospitals in the UK.
The mean kVs from the histograms are 65kV and 75kV (rough estimates). Mean
DAP values have been estimated assuming a DAP value of 0.5 cGy cm2 for each Xray.
Primary radiation
The patient, grid, cassette and bed will attenuate the primary beam significantly. In
addition, there should be, with proper collimation, no possibility of a primary X-ray
beam impinging directly surrounding structures.
Often a grid will not be used with paediatrics. However, exposure factors will be
reduced to maintain the air kerma at the required level at the film surface.
(I suggest I obtain some typical cassette doses and do some
measurements on the air kerma values on the exit side of cassettes. I
can then reinforce this with some reference to the lead equivalence of
cassettes etc. I can then make a statement similar to Jerry’s)
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
78
Secondary Radiation
Figures 3 and 4 show plots of the scattered radiation produced from a chest X-ray on
substitute anthropomorphic phantoms for a neonate and 5 year old child.
In general, compared to adult radiography, low kV and small scattering volumes lead
to low levels of scattered radiation being produced. At the side of an incubator and at
the edge of a bed in PICU, referring to figure 3 and 4, scatter radiation levels for chest
radiography are unlikely to substantially exceed a few hundred nGy per exposure. For
the incubator, levels of scattered radiation at a distance of 1m from the centre of the
phantom are insignificant (some value needed). Similarly, scattered radiation levels
at a distance of 1m from the edge of the PICU bed are likely to be less than 100nGy
per exposure. On most units, X-rays will only be taken on a relatively infrequent
basis. Hence, ordinarily, there would seem to be little need for secondary radiation
shielding. However, in NNU (although unlikely to receive significant radiation doses) it
would seem prudent, following the application of the ALARP principle, for staff who
are required to hold patients to wear protective lead coats.
Adult radiography on ITU, Wards and in resuscitation rooms
Workload figures
In figure 5 a histogram of the types and frequency of exposures carried in one
hospital’s ITU department has been included (Study underway). The mean kV
factors are ??. Mean DAP readings are also included in the figure (I can do this from
the above histogram).
Primary Radiation
The calculations relating to primary radiation should be carried out in a similar way to
that in section ? (general X-ray)
Secondary Radiation
Figure 6 shows data produced by Herman (Herman, 1980) for scattered radiation air
kerma levels around an ITU bed from a chest X-ray taken at 80kVp. The air kerma
levels at 1m from the centre of the phantom and at the side of the bed are of the
order of 400nGy per exposure. North (North, 1984) suggests that the most intense
scattered radiation is back towards the source of radiation. He suggests that the
scattered radiation intensities at 90 degrees to the beam direction are less than half
those at 165 degrees. This statement broadly agrees with Williams (Williams, 1996). A
calculation following the method given in section ?? can be made:
Secondary radiation from mobile X-rays on ITUs
Representative DAP: 0.1 Gy cm2
Work load:
10 chest X-rays a day. Factors: 80kV and 2mAs
Distance:
Maximum scatter factor:
2m
1.24 µGy ((Gy cm2)-1) (Williams, 96)
The maximum scattered radiation at 2m from the patient is of the order of 100 to 200
nGy per exposure.
The need to consider the use of secondary shielding most often arises in the case of
resuscitation rooms. This is due to the proximity of walls and adjoining beds, types of
X-ray views taken, the number of staff involved and the urgency of procedures.
Domiciliary X-rays
Although very unusual, radiography using low powered transportable X-ray equipment
is known to be carried out in patient’s homes. The requirement for radiation shielding,
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
79
outside the use of lead coats, is obviated by the one-off natures of these types of Xrays. However, the positioning of the patient and X-ray equipment should be carefully
considered and procedures should be fully referenced in local rules.
Secondary shielding for mobile X-rays
If an RPA considers that radiation shielding is required then the following approaches
are recommended.
Inter-Cubicle (or bed bay) Shielding
It is unlikely that it would be possible to designate one cubicle specifically where Xrays may be used. The question then becomes how to provide shielding economically
for a number of cubicles? Also, any shielding between cubicles must take account of
clinical staff’s need for easy access and for shelf space and visibility. The following
are offered as possible solutions:
• Fixed Screens
These offer the most elegant solution. Windows and shelving can be
installed as required. The main disadvantages are: the cost of providing
screens for a number of cubicles; clinical staff’s objections to the rigid
demarcation between cubicles.
• Mobile Screens
Mobile screens offer a degree of flexibility and potential cost savings. A purposedesigned screen is shown in figure.
Disadvantages include difficulties in
positioning and inconvenience.
< Figure 7. Photograph of premise’s screen>
• Lead Curtains
Lead curtains have the advantage of ease of use, but the disadvantages of limited
lead equivalence and a relatively poor record for structural integrity.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
80
Mobile Trailers
During the past few years, mobile trailers, with CT scanners and a limited number of
C-arm fluoroscopic units installed in them, have been increasingly used, usually on a
hire basis, by Hospitals. Initially, the trailers were primarily used to provide a first line
service. However, especially in the case of CT scanners, trailers are increasingly
being used to add additional capacity and to provide continuity in service. As far as
the design of radiation shielding for mobile trailers is concerned the situation is
complicated by restrictions in space and weight.
Shielding Calculations
The appropriate methods to be used for shielding calculations have been covered in other
section (??? and ???) of this publication. In reality, it is very unlikely that an RPA will be
asked to advise a coach building company on the requirements for radiation shielding during
the design and building of a trailer. Usually an RPA will be faced with a fait accompli and must
focus on the rules for the positioning and use of the trailer. Having said this, if shielding is
being designed the following design consideration should be borne in mind.
Figures 1 and 2 show schematics of a typical CT and cardiac catheter laboratory
trailer.
< Schematics - already obtained >
Figure 1.
Schematic of a CT mobile trailer
(courtesy of Calumet Coach Company)
Figure 2.
Schematic of a cardiac catheter laboratory mobile trailer
(courtesy of Calumet Coach Company)
In relation to figure 1 and 2 the following points should be noted:
•
when designing any shielding, reference should be made to national road
regulations governing weight per axial/tandem/spread and overall weight
including the tractor unit;
•
the floor of the trailer is 1.5m above the ground;
•
available space is severely limited. One or two extendible sides are usually used
to increase available space;
•
access to the underside of the mobile trailer is restricted by the trailer’s
undercarriage;
•
there is no easy access to the roof;
•
the patient entry door is usually only accessible via a lift;
•
there is usually a substantial amount of plant at the back end of the trailer;
Roof
Under normal circumstances and based upon the restriction of access and no
buildings directly overlooking the trailer, shielding should not be required in the
trailer’s roof.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
81
Floor
Essentially, the trailer’s floor can be divided into two areas:
• the area below which access is restricted by the trailer’s undercarriage. Shielding
should not be required in this area;
• the areas, mainly below the extendible sides, to which access is possible. The
need for shielding, to a certain degree, is obviated by the use of portable barriers.
However, this approach is generally discouraged due to a lack of direct
supervision. It would be prudent in this case to consider the installation of
shielding.
Walls
Radiation shielding should be installed in the side walls that enclose the X-ray room.
Shielding on the back wall is unlikely to be required due to the shielding effect of plant
that is usually attached in this area.
Control Room Screen
The close proximity of the control room to the X-ray source should be considered
when deciding on thickness of shielding.
Operational Considerations
Trailers will need to be parked in an area with easy access to the hospital and a
power supply. In the sighting of mobile trailers, the following additional point should
be considered:
• whenever possible, the trailer should not be sighted adjacent to buildings;
• the trailer should not be parked directly beneath buildings.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
82
References
Williams J. R., 1996. ‘Scatter dose estimation based on dose-area product and the
specification of radiation barriers’. The British Journal of radiology, 69, 1032-1037.
Simpkin D. J.; Dixon R. L.; 1998. ‘Secondary Shielding barriers for diagnostic X-ray facilities:
scatter and leakage revisited’. Health Physics, March 1998: Vol. 74, No. 3.
Herman M. W., Patrick J., Tabrisky J, 1980.; ‘A comparative study of scattered
radiation levels from 80-kVp and 240-kVp X-rays in the surgical intensive care unit’.
Radiology 137:552-553, Nov 1980.
North D., 1985. ‘Patterns of Scattered Exposure from portable radiographs’. Health
Physics, Vol. 49, No. 1 (July), 92-93
Other Thoughts
A checklist of questions to ask architects etc. would be a good thing.
Notes on Building Materials
Walls - these may be constructed in or lined with:
Brick:
External quality, preferably without a “frog” or mortar
holes.
Concrete Block:
100 or 150 mm.
Lead Sheet:
Existing low density walls may be lined with sheet lead secured
at regular intervals to reduce creeping. This is not the best
method of lead-lining and is not recommended generally.
Lead-backed
Boards:
These may be used for lining or structurally and are available in
plasterboard or plywood and different thicknesses of lead.
They may be obtained ready-finished in melamine or prepared
for skimming with plaster or for decorating. Boards must be
screw fixed. Joints must be made over lead-lined battens
having the same thickness of lead. Lead and lead-lined boards
are available in standard commercial thicknesses. Sometimes,
thinner lead shielding is adequate, but special thicknesses,
although available, are more expensive.
Mammography:
A double layer of plasterboard, with staggered joints, is
sufficient. Alternatively, aluminium sheet may be used.
Barium Plaster:
Brick or block walls may be coated in barium (X-ray) plaster.
The plaster is heavy to apply.
For both bricks and concrete blocks, the density should be > 1850 kgm-3 and the
mortar beds and perpends must be well filled to avoid cavities. In general, 100 mm
thick brick or block of the above density is equivalent to ~ 1mm lead.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
83
7.8 BONE DENSITOMETRY
Bone Densitometry units have not been considered in the past a source of particular
radiation protection problems. However, in the light of units with increasing patient and
operator doses e.g. fan beam units, this assumption must be reconsidered. No
specific layout will be given and references only made to distances from protected
persons.
Occupancy of surrounding areas with requisite shielding will be the overall planning
consideration. The specific requirements will be strongly dependent on the type of
DXA scanner used.
There should in general be no primary barrier requirements. The protection required
will be provided by secondary barriers or distance as required.
7.8.1 Methodology
Full occupancy should be assumed in the first instance. Only if the resulting barrier
requirements appear grossly excessive or excessively costly should the design
assumptions need to be examined again.
Patel, Blake, Batchelor and Fogelman[1] have investigated the dosimetry of various
DXA scanner using a mixture of real patients and phantoms. Table 7.8.1 presents
their data for spine and hip examinations.
In the case of the first two units A and B shown in Table 7.8.1 the dose limit would be
achieved under the given workloads, in the latter case by increasing the distance to
the operator or the person to be protected. In the cases C and D additional shielding
would be necessary
7.8.2 Example
A QDR 4500 is planned in a room where there is a waiting room for ante natal
patients the other side of a thin plasterboard partition barrier. Workloads of 100
patients per week are expected. The nearest member of the public will be 2 metres
away from the scanner.
From Table 7.8.1 the annual unshielded dose at 1 metre would be 3.02 mSv per
annum. At 2 metres this reduces to 0.76 mSv per annum. An attenuation factor of 0.4
is therefore required for the barrier. This would be met by 1.32 HVLs of lead. Because
of the heavily filtered nature of DXA radiation we will use data highly attenuated
beams. From table 5.5 one can conservatively assume the HVL to be 0.28 mm lead.
The required degree of shielding is therefore 0.37 mm lead, 23 mm concrete or 62
mm gypsum wall board..
For operator protection, as recommended in the study by Patel et al [1] the distance
from the unit must be increased to a least 2 metres to achieve a dose level of less
than 1 mSv per annum. The dose constraint of 0.3 mSv per year could only be
achieved by using a operator distance slightly in excess of 3 metres. Alternatively, the
use of a 0.5 mm lead protective shield would enable this requirement to be met.
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
84
The screens and doors may require protection, which should present no difficulties.
The floor concrete density and thickness will need to be considered to verify that the
specified thickness will be adequate - in most cases no additional protection will be
required. Section 5 provides appropriate information.
References
[1] Patel,R, Blake,G.M.,Batchelor,S,Fogelman,I - ref to follow.
[2] National Radiological Protection Board, Occupational Public and Medical
Exposure, Guidance on the 1990
recommendations of ICRP, Doc. NRPB, 4. No.2, 32-41, 1993, London, HMSO.
[3] International Commission on Radiological Protection (ICRP), Radiological
protection of the worker in medicine and dentistry, ICRP Publication 57, Annals of the
ICRP 20 No.3, 1989, Pergamon Press, Oxford.
Scanner
(A) Lunar DPX
Dose per Scan
(µSv)
No. patients per
week
Annual Dose at
1 metre (mSv)
Attenuation
factor for 0.3
mSv/year
0.01
(B) Hologic QDR (C)
Hologic (D)
Hologic
1000
QDR 2000 plus
QDR 4500*
0.08
0.42
0.58
100
100
100
100
0.05
0.42
2.18
3.02
not required
0.72
0.14
0.10
Table 7.7.1
Shielding Design for Diagnostic X-ray rooms Draft of June 1999
85