Low sucrose diet
for children
What is sucrose?
Sucrose is the sugar from sugar cane – also known as table sugar. There are three main
sources of sucrose in our diet:
> Table sugar we add ourselves (eg. sprinkled on cereal or added in cooking)
> Sucrose (table sugar) added by manufacturers to processed foods (eg. to cakes, biscuits
and drinks)
> Natural sucrose found in fruits and vegetables
What is sucrose intolerance?
Sucrose intolerance occurs when the body is unable to absorb sucrose well. A common
symptom of sucrose intolerance is diarrhoea. Some children also experience abdominal pain,
bloating, wind and irritability.
The diagnosis of sucrose intolerance should be confirmed by a breath hydrogen test.
Sucrose intolerance should not be confused with Sucrose-Isomaltase deficiency. SucroseIsomaltase deficiency is a rare inherited disorder that requires almost complete elimination of
sucrose from the diet and other dietary modifications. This information sheet is not intended
for children with Sucrose-Isomaltase deficiency.
Treatment
Sucrose intolerance is treated by lowering the amount of sucrose in the diet. This resource
will show you how to reduce the amount of sucrose in your child’s diet.
Tolerance
Sucrose does not need to be completely removed from the diet. Tolerance of sucrose will
vary greatly between children. Many children will tolerate small amounts of a high sucrose
food without symptoms however if large amounts are eaten symptoms may reappear.
Vitamin C
Fruits and vegetables provide most of our vitamin C. If your child is not eating many fruits and
vegetables, they may need a vitamin C supplement. Discuss this with your dietitian.
Medications
Some medications (especially flavoured ones) may contain sucrose and should be checked
before giving to your child.
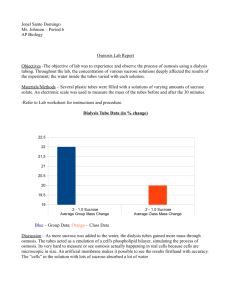
Sucrose content of foods
The following tables sort foods according to how much sucrose they contain. There are two groups:
Eat freely
Limit
These foods are low in sucrose and can be eaten freely
These foods are high in sucrose - initially limit these foods. Once symptoms resolve you can
challenge with small amounts of these foods.
Tolerance of the ‘limit’ group of foods will vary greatly between children. Many children will tolerate small amounts
of high sucrose foods without symptoms however if large amounts are eaten symptoms may reappear.
Dairy and
dairy
alternatives
Eat freely
Limit
> breastmilk
> sweetened condensed milk
> standard infant formulas and soy formulas
> S26 Soy formula
>
>
>
>
>
>
>
>
>
>
>
>
Breads and
Cereals
>
>
>
>
>
Biscuits and
cakes
Drinks
>
>
>
>
>
>
>
>
>
>
>
>
except S26 Soy (check with your dietitian)
cow’s milk (plain, unflavoured)
soy milk (plain, unflavoured)
rice milk (plain, unflavoured)
lactose free cow’s milk
cheese (including cream cheese)
natural yoghurt (plain)
diet yoghurt (plain)
cream
sour cream
evaporated milk
sugar free custard
diet jelly
plain breads
pasta
noodles
flour
cereals with no added sugar– eg. rice
cereal, puffed weat, Vita Brits, Weeties,
rolled oats
homemade low sucrose biscuits and cakes
plain dry biscuits – eg. SAO, Jatz, Ryvita,
Vitaweat, rice cakes, Salada, water crackers
tea
coffee
cocoa
diet cordial and soft drinks
diet milk flavourings
unflavoured mineral and soda water
cow’s milk (plain, unflavoured)
rice milk (plain, unflavoured)
soy milk (plain, unflavoured)
unsweetened juice
Meat / eggs
> no restrictions
Margarine,
butter, fats
and oils
> margarine and butter
> all oils
> sour cream
> flavoured milks– eg. chocolate milk
> milk toppings – eg. Milo, Aktavite
> yoghurts sweetened with sugar
> yoghurts with fruit
> ice cream
> sorbet
> frozen yoghurt
> custard
> flavoured or sweetened soy milk
> all desserts and puddings made with sugar
> jelly
> ice-blocks
> sweetened breads
> cereals with added sugar
> commercial biscuits and cakes with added
sugar
> commercial sweetened pastries
> all other juices
> regular cordial
> milk shakes
> milk flavourings – eg. Milo, Quick, Ovaltine,
> flavoured mineral water
> regular soft drink
> flavoured milks
> imitation cream (sweetened)
Spreads
> Vegemite
> jam – including 100% fruit jam
> Marmite
> marmalade
> Promite (small amounts – thin spread)
> chocolate spreads (e.g. Nutella)
> cream cheese
> peanut butter (including no added sugar
> cheese spread
varieties)
> honey
Sauces and
Confectionary
> sauces and gravies with added sugar
> table sugar – white, brown, raw, icing.
> golden syrup and maple syrup
> lollies, chocolate, toffees, liquorice
> other confectionary based on sugar
> 100’s and 1000’s
Sucrose content of fruits and vegetables
The following tables sort fruits and vegetables according to how much sucrose they contain – low, moderate and
high. When starting a low sucrose diet choose low sucrose fruit and vegetables only. Once symptoms resolve
you can then challenge with small amounts of moderate and high sucrose fruit and vegetables. Tolerance of
moderate and high sucrose foods will vary between children.
Fruit
Low
(less than 1% sucrose)
Moderate
(1-3% sucrose)
High
(more than 3% sucrose)
> avocado
> apples – fuji, royal gala,
> apples – pink lady*
> blackberries
> blueberry
> lemon
>
> lime
>
> lychee
>
> nashi pear
>
> pears – all except brown
>
> quince
>
> raspberry
>
> rhubarb
>
granny smith, red delicious,
jonathon.
brown pears
cherries
grapefruit
kiwi fruit
passionfruit
rockmelon (cantelope)
strawberries
watermelon
> all vegetables not listed in
moderate and high
columns
> banana*
> custard apple
> dried apricot and dried apple*
> honeydew melon
> mandarin
> mango*
> nectarine*
> orange
> peach*
> pineapple*
> sultanas and currants
Vegetables
> apricot
> artichoke
> beetroot*
> brussels sprouts
> creamed sweetcorn
> carrots
> gherkin – pickled
> celeriac
> green peas
> onion
> parsnip
> pumpkin – queensland blue
> pumpkin – butternut variety*
variety
> red cabbage
> sweetcorn kernels
> sweet potato
> sweetcorn fresh on the cob
* more than 5% sucrose
Note – if a fruit or vegetable is not listed it can be eaten freely
Onion, leek, garlic and legumes
Onion, leek, garlic and most legumes contain low to moderate amounts of sucrose but often can cause bloating
and discomfort in children with sucrose intolerance. These foods are best avoided initially when starting a low
sucrose diet. Once symptoms of sucrose intolerance (eg. bloating, diarrhoea) have improved they can then be
reintroduced in small amounts as tolerated.
Sugar substitutes in cooking
The following products are available to use instead of table sugar (sucrose) in food
preparation and cooking:
Glucose (dextrose)
> Available from supermarkets and pharmacies (glucose powder)
> In cooking use the following conversions for your recipes:
o
1 cup sugar = 1 ½ cups glucose powder
o
½ cup sugar = ¾ cup glucose powder
o
1 tablespoon sugar = 1 ½ tablespoons glucose powder
Artificial sweeteners
> Available from supermarkets (eg. Equal, Splenda)
> Used in some diet products to sweeten food (eg. diet soft drink, diet cordial)
> Safe to use in normal amounts – individual families have preferences about use in children
Sorbitol
> Used in many ‘diabetic’ or diet foods eg. chocolate, sugar free lollies, chewing gum
> Sorbitol and other sugar alcohols are natural laxatives and cause bloating, diarrhoea and
abdominal pain in all people when eaten in large amounts.
> Should be used in small amounts only
Fructose
> Fruit sugar – can be used in cooking as alternative to table sugar.
> For example – use dried fruit or juice instead of sugar in cooking.
Label reading
Your child may need to avoid packaged foods with large amounts of added sugars.
Ingredients on the food label are listed from the largest ingredient in the product to the
smallest. Try to avoid large amounts of foods which include sugar (eg. ‘sugar’ or ‘raw sugar’)
listed as one of the first three ingredients (Weetbix is an exception). Speak to your dietitian
for more information on label reading.
eg. Big M Strawberry Milk – Ingredients: Skim Milk, milk, sugar, emulsifier (471), flavour,
natural colour (120).
High sucrose food as sugar is one
of the first three ingredients listed
Food product information contained in this resource was up to date at the time of revision. If
you are not sure about a food, check with the manufacturer.
Produced by
Women’s and Children’s Health Network
Nutrition Department
72 King William Road
North Adelaide SA 5006
© Department of Health, Government of South Australia. All rights reserved.
Revised February 2012