Day 1. Michael Stone - 2015 Metagenics International Congress on
advertisement

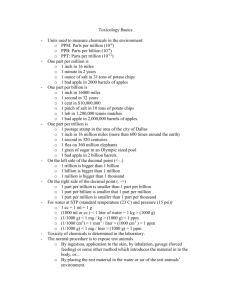
Work Up of the Toxic Patient Root causes and Imbalances P. Michael Stone, M.D., M.S. 2014 Australia Disclosure and Acknowledgements • P. MICHAEL STONE, M.D., M.S. CONSULTANT FOR INSTITUTE FOR FUNCTIONAL MEDICINE, EPIGENEATING.COM, AND IN PRIVATE PRACTICE • ACKNOWLEDGMENTS: IFM AND THE IFM DETOX TEAM: KRISTI HUGHES, ND, RICK MAYFIELD DC, DEANNA MINICH PHD, CCN, ROBERT ROUNTREE, M.D., IFM CNI TEAM AND ELIZABETH BOHAM MD,MS,RD. FUNCTIONAL MEDICINE addresses the underlying causes of disease, using a systemsoriented approach and engaging both patient and practitioner in a therapeutic partnership. Who is Looking for and dealing with Toxicants? Naturopaths J ALT COMPLEMENTARY MED 17(12)1175–1180 2011. Environmental Exposure Preventative Medicine/General Cleansing Gastrointestinal Disorders 82-50% of Patients Inflammation With These DX Fibromyalgia Were Rx with Detox Chronic Fatigue Syndrome Weight Loss Endocrine Disorders Multiple Chemical Sensitivity... Liver disease CVD Mercury Amalgam Removal J ALT COMPLEMENTARY MED 17(12)1175–1180 2011. Cleansing foods (i.e., Brassica family, beet root, dandelion, etc). Increased fruit/vegetable intake Vitamin/mineral/antioxidants Organic foods Elimination diet Probiotics Reduce environmental exposure Stool bulking agents/fiber Cholagogue herbs 91-47% Used Sauna these interventions Chelating agents Skin brushing Lymphagogue herbs Avoidance of animal products Functional Toxicology Triggers Toxicants Genomic Predisposition Mediators Chronic Disease ©2014 The Institute for Functional Medicine TOTAL TOXICANT LOAD equals Total Toxicant Exposure minus Ability to Detoxify and Eliminate Toxins ©2014 The Institute for Functional Medicine How Long How Much How Often Individual Variables Age BMI Physical Condition Smoker Drug/Alcohol Use Competitive Load ©2014 The Institute for Functional Medicine Pattern Recognition Undernourished Reduce Exposures Ensure a Safe Detox Work up of the Toxic Patient? Pattern Recognition Pattern Recognition In Patients with Toxin Associated Diagnosis Start with Condition or Symptom which is not improving with the conventional treatment - ADHD, Allergies, Alzheimers, Anemia/immune suppression, - Autism, Autoimmune Disease, Cancer, Chronic Fatigue, - Fibromyalgia, Diabetes/IR, Fertility Issues, Inflammation, - Neurobehavioral Issues, Neurodevelopment issues, - Osteoporosis, Parkinsons, Peripheral Neuropathy... Fm. Hx Mediators-Perpetuators-Drivers Genetics Triggering Events Age Birth Signs, Symptoms, Diseases Gather The History of Health and Illness on a Timeline Two Key Detox Screening Questionnaires Medical Symptoms Questionnaire (MSQ) Toxin Exposure Questionnaire (TEQ) Medical Symptom Questionnaire P: Pattern Recognition MSQ: Quantifies Symptom Severity 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. HEAD EYES EARS NOSE MOUTH/THROAT SKIN HEART LUNGS DIGESTIVE TRACT JOINTS/MUSCLE WEIGHT ENERGY/ACTIVITY MIND EMOTIONS OTHER 71 questions Scored: 0 – 4 Total: 0 – 284 Medical Symptom Questionnaire • >50 = Risk of Increased Toxicity • Concern: if 10 or more subsection points • >100: more fragile “Start slow, go low” Toxin Exposure Questionnaire Identifies Exposure Sources: 1. Community 2. Home 3. Occupational 4. Hobbies 5. Diet & Lifestyle 6. Medical/Dental Ability to Control or Alter Exposures: Identify Control Remove Mitchel Reference here also Saunders COMMUNITY HOME HOBBIES OCCUPATION PERSONAL HABITS DIET DRUGS Patterns of Exposure and Disease Occurrence Persistent Organic Pollutants RA (8X), OA, CVD(3.5X) DM (38X) Polychlorinated Biphenyls RA, OA (3X) Organochlorines-Pesticides IR ABD Obesity, Neurodegeneration 2X Food Triggered Response Celiac, High Carbohydrate Heavy Metals IR, DM, Neurodegeneration Obesity 92% children in US risk of Neurodevelop lead tox., CVD, MI, Htn, Osteoporosis, Neuropathy, Dementia. DM Pizzorno, J, J Katzinger: Clinical pathophysiology a functional perspective 3.1-3.27, 2012 Quality Context ABCD of Nutrition Evaluation -Anthropometrics -Biochemical Markers -Clinical Findings -Diet Evaluation Quantity Company Toxic Patient Physical Exam partial list of possible findings • Hair: change in luster, change in texture, change in color • Eyes: Arcus, pigmentation (copper, iron), Hippus (adrenal), Sclera (yellowed), Conjunctiva (anemias).... • Nose: rhinorrhea, boggy turbinates, altered smell, seborrheic changes... • Mouth- Lips:blue tint, cracking (vitamin A), Hypersalivation, xerostomia, soft palate/ tonsils, congenital disorders, tongue (coating, fissuring, scalloping, atrophic tastebuds, altered taste), Gums: heavy metal lines, periodontitis, Buccal Mucosa: tattoing, mucosal changes (leukoplakia, squamous cancers), Teeth: enamel dystophia, dissimilar metals... • Neck: Acanthosis nigricans, thyroid enlargement, • Lungs: decreased PEFR, Wheezing, distant breath sound,... • CV: brady cardia, tachycardia, arrhythmia, HTn, Hypotension, cardiomegaly... Toxic Patient Physical Exam partial list of possible findings • Musculoskeletal: fibromyalgia trigger points, muscle tenderness... • Skin: acne, acanthosis nigracans, xerosis, hyperkeratosis pilari, rashes, palmer changes (erythema, peeling), seborrheic keratosis, basal cell or squamous cell cancers,... • Nails: mees lines, leukonychia, leukostriae, beaus lines, psoriatic nails... • Neuro Altered level of consciousness, memory change, cognitive change, focus change, balance and sensation change, visual contrast changes, peripheral exam- small fiber pattern, large fiber pattern, mixed pattern, balance, rhomberg, tremor, change in hand writing,... Pattern Recognition Endocrine Genotoxic Neurologic Immune Metabolic The Patient’s Story Retold Physiology and Function: Organizing the Patient’s Clinical Imbalances Assimilation Antecedents Triggering Events Defense & Repair Genotoxicity Structural Integrity Energy Immunotoxicity Endocrine Toxicity Mediators/Perpetuators Communication Spiritual Biotransformation & Elimination Mitochondrial Toxicity Transport Metabolic Toxicity Personalizing Lifestyle Factors Sleep & Relaxation Neurodevelopmental Stress & Resilience Nutrition & Hydration Toxicity Exercise & Movement Name:____________________________ Date:___________ CC:_____________________________________ Relationships & Networks © Copyright 2011 Institute for Functional Medicine Work up of the Toxic Patient? Pattern Recognition Toxins from Outside Toxins from Inside Toxicants • Triggers of Imbalance • Disruptors of Function Exotoxins • Heavy Metals • Persistent Organic Pollutants • Organochlorine Pesticides • Polychlorinated Biphenyls • Mycotoxins Endotoxins • Imbalanced Phase 1, 2, or 3 • Products of Metabolism Journal of Environmental and Public Health Volume 2012, Article ID 356798 P: Pattern Recognition Disease and Toxin Associations ADHD Allergies BPA Lead Mercury Phthalates PCBs Antimony BPA Cadmium Formaldehyde Mold Nickel Phthalates Source: IFM Toolkit Alzheimer’s Aluminum Lead Mercury Anemia/ Immune Suppression Benzene Cadmium Lead PAHs Autism AI Diseases BP and Kidney Disease Mercury Arsenic Lead Mercury Mold Arsenic Lead Mercury Cancer Aluminum (breast?) Arsenic Benzene BPA Cadmium EMFs Formaldehyde HAs Lead Nickel Perchloroethylene Phthalates Solvents Vinyl chloride PVC Dioxin Disease and Toxin Associations CFS, Diabetes/IR Fibromyalgia Arsenic Benzene Cd EMR FA Pb Hg Mold Ni PCE POPs PCBs Solvents PVC Dioxin Arsenic BPA EMFs Pesticides PCBs PVC Dioxin Vinyl chloride Fertility Issues & Menstrual Disorders Arsenic BPA Cd EMF FA Pb Hg Phthalates PCBs PAHs Solvents PVC Dioxin Multiple Chemical Sensitivities Neurobehavioral issues Benzene FA Mold Pesticides PCBs Solvents Vinyl chloride PVC Dioxin Al As EMFs Pb Hg Mold Phthalate PCBs Solvents FA: Formaldehyde, PVC; Polyvinyl Chloride; Source: IFM Toolkit Neurodevelopment issues Osteoporosis As Pb Hg PCBs Solvents Cd Pb Parkinson’s Peripheral neuropathy Mn Pesticides As Pb Hg PCBs mycotoxin Pesticides Food Allergy and Reactions Barbeque: nitrosamines Gluten Heavy metal/bacteria Eggs/Pesticides... M.Stone, M.D: . Food Photos: Allergens and Toxins Images-M Stone, M.D. Contents/Reactants in Foods Protein, Carbohydrate, Lectins, Food-Pollen Homology, Fruit juice-cellulase…Many, Preservatives (citric acid), Antibiotics, Hormones, Enzymes (lactase, bread-amylase, ), colorings… Basic Contents Additives Canning, Freezing, Heating, Salting, Smoking marinating, microwave Treatments Natural Processes Protectants Pesticides Genetic Engineering Soy, Coffee, Squash, Tomato Sugar Beet, Salmon… Spoilage Bacterial, Fungal, Toxins, Histamine, Pathogens, Heavy Metals… Aging, Insects, Worms, Fungi (grapes, tomato) Fermentation (chocolate tea, malt) Pesticides, Fungicides, Antibiotics… Toxins In... Sears, M, SJ Genius: J Env Pub Health 2012, ID356798, doi:10.1155/2012/356798 Toxins In... Sears, M, SJ Genius: J Env Pub Health 2012, ID356798, doi:10.1155/2012/356798 Hg+ Dose Burden . Curr Probl Pediatr Adolesc Health Care 2010 September; 40(8):186-215 Copper + Decreased liver and plasma Cu, Reduced plasma ceruloplasmin concentration Iron Decreased Hct, Hgb, Binds ferritin and transferring, Anemia Zinc Decreased GI absorption, Disturbed Zn metabolism, inhibits Zn containing enzymes, replaces Zn: Metallothionein Calcium Osteoporosis, osteomalacia, cadmium deposition in bones, Hypercalciuria Cadmium Mitochondrial injuries, Altered Antioxidant Defense, Decreased DNA Repair, Altered Gene expression Toxic Minerals: Cd, Pb, Hg, As Damage antioxidant defense system Depletion of thiol Status ROS LIPID PROTEINS DNA Lipid Peroxidation Protein Oxidation Oxidized Nucleic Acids Membrane Damage Protein Dysfunction Impaired DNA Repair Cell DEATH Mechanism of heavy metal induced oxidative stress Mutagenicity Carcinogenesis Dirty Dozen vs. Clean 15 External Environmental Exposure “Outside Getting In” Raising Havoc metabolic, genomic, physiologic, endocrine, immune (matrix) havoc. Adverse Reactions>> Health Effect>> Disease Toxicity Internal Environmental Exposure “Inside Getting Out” Work up of the Toxic Patient? Pattern Recognition Location of Toxicity altering Function- looking for imbalance Enzyme Inhibition Toxicant Exposure Damaged Cell Membranes Endocrine disruption DNA Damage Oxidative Damage BioMarkers and Functional Labs Conventional Laboratory Functional Laboratory Conventional Laboratory Associated markers of Toxicity • CBC with differential • Magnesium – >0.7 mg/L – <2meq/dL • Gamma-glutamyltransferase – (GGT) >40 units/L • Uric acid – >8mg/dl • Homocysteine – >11 micromol/L • hsC-reactive protein – >0.7 mg/L • Antinuclear antibody titer – >1:125 • Apo B/Apo A1 – >0.6 • Hemoglobin A1c – >5.5% • 25-Hydroxyvitamin D3 – <30 ng/ml • Urinary microalbumin – >30 mg in 24 hr Conventional Lab Tests To assist in evaluation of the toxic patient • CBC – Leukopenia (Benzene, Arsenic, Strotium, hexavalent chromium, Copper, – Pancytopenia (Benzene) – Thrombocytopenia (strontium) – Anemia • Chemistry Panel – Liver Function Tests • • • • AST/ALT ALP/LD GGT Bilirubin – Renal panel, cystatin C • HbA1C Liver Enzyme Markers • • • • • ALT: alanine transaminase AST: aspartate aminotransferase ALP: alkaline phosphatase LD: L-lactate dehydrogenase GGT: γ-glutamyl transpeptidase Liver Enzyme Markers Damaged/destroyed hepatocytes leak enzymes into blood. • ALT aids protein metabolism, almost exclusively found in liver. • AST metabolizes alanine, found primarily in liver, muscle. • ALP Nonspecific: Liver bone, intestine, & placenta. • LD Nonspecific: Liver, RBC, cardiac/skeletal muscle. • ALT, AST (& LD) rise with liver damage. • ALP & GGT (& bilirubin) rise when bile flow is slow or blocked. • ALP Isolated increases are usually from liver damage. GGT / GGTP • Readily induced by medications (barbiturates, phenytoin, NSAIDs), alcohol, obesity, POPs & other toxic chemicals • Elevated levels found with liver disease, especially fatty liver and biliary disease • May be a marker for increased metabolic, cardiovascular, CKD risk & all-cause mortality Prev Cardiol. 2010 Winter;13(1):36-41 • Possible marker for oxidative stress associated with glutathione metabolism • Level of concern – Men: 30-40 IU/L increased suspicion; >50 IU significant – Women: >37.5 IU/L significant Is Serum GGT a Biomarker of Xenobiotics, Which Are Conjugated by Glutathione? Arterioscler Thromb Vasc Biol, 2008: e26-28 • Lead, cadmium, dioxins, or OC pesticides are positively and monotonically related to serum GGT in the general population without any occupational exposure • Associations between environmental pollutants and serum ALT (more specific to liver and more commonly used as a marker of NAFLD) were opposite to those of serum GGT, suggesting that the associations of serum GGT may not be related to liver toxicity. Functional Laboratory Assessing Toxicity • Identify triggers – Toxic metals: hair, blood, urine analysis pre and post DMSA challenge, occasionally fingernail/toenail clippings, fecal metals. Byproducts of metabolism- porphyrins – Organic toxicants (fat biopsy; blood, urine) – Stool analysis – Hepatic detoxification and oxidative stress profiles – Intestinal permeability testing (lactose/mannitol)(Food Allergy/hypersensitivity) • Identify mediators- or byproducts – – – – Extra and intracellular antioxidant level Porphyrins Oxidative stress markers Essential fatty acid profile Toxins inducing Porphyrinurias Environmental Toxin Urinary Porphyrin Elevation Arsenic Uroporphyrins, pentacarboxyporphyrin, coprophyrin1, High copro I:III ratio Mercury Precoproporphyrin, Pentacarboxyporphyrin, Coproporphyrin (total) Lead Aminolevulinic acid (ALA) coproporphyrin III, Coproporphyrin 1 (sometimes) zinc protoporphyrin Hexachlorobenzene Uroporphyrins Methyl chloride Coproporphyrins Dioxin Uroporphyrins Polyvinylchloride Coproporphyrins Polybrominated biphenyl Coproporphyrins (uroporphyrins) Lord Bralley Glucose Tolerance Test SI - International Units 75 gm dextrose Optimal Levels Fasting insulin 28-35 pmol/L 1/2 hour insulin <215 pmol/L 1 and 2 hour insulin <215 Fasting glucose-4.4-5.0mmol/L • • • • • • 2 hour glucose- 4.4-6.6mmol/L • • • • • • HgA1C < 0.055 • • • Diagnostic IR >85 pmol/L > 395 insulin > 350 insulin > 5.5 = hypergly >7.0 = DM2 > 11 mmol/L - 2 hour glucose > 0.06 – HgA1C JAMA 2007;297:2092-102. McAuley, K. Diabetes Care. 2001;24:460-464. Functional Lab Tests To assist the evaluation of the toxic patient Nutritional & Assimilation Toxic Damage Body Burden Genetic Susceptibility • Dysbiosis/SIBO: overgrowth of pathogenic microorganisms • Increased levels of β-glucuronidase • Markers of GI inflammation • Intestinal Permeability Functional Lab Tests To assist the evaluation of the toxic patient Nutritional & Assimilation Toxic Damage Body Burden Genetic Susceptibility Oxidative stress tests: • • • • • 8-Hydroxy-Deoxyguanosine (8-OH-dG) Thiobarbituric acid reactive substances (TBARS) Oxygen radical absorbance capacity (ORAC) Lipid Peroxides Isoprostanes Functional Lab Tests To assist the evaluation of the toxic patient Nutritional & Assimilation Toxic Damage Body Burden Genetic Susceptibility “Biomonitoring” for Body Burdens: • Measurement of exogenous agents in biological media (blood, urine, hair, nail, stool, adipose) • Measurement of markers that indicate presence or effects of an exogenous agent Test Evaluation for Environmental Toxins 1 part per million or billion? • 1 ppm • 1/1,000,000 • 0.001 mg is 1/1,000,000 of a kg. • 1 ounce in 31.25 tons • 1 minute in 1.9 years • 1 drop vodka in 80 fifths of 7-up • 1 ppb • 1/1,000,000,000 • 0.000001 mg is 1/1,000,000,000 of a kg. • 1 ounce in 31,250 tons • 1 minute in 19000 years • 1 drop vodka in 80000 fifths of 7-up • The power of small......................... • The power of really small....................... Response to Mold Immune Response ? Endocrinologic Response Biotoxin Response Mycotoxins • Aspergillus flavus(aflatoxin)-chronic exposure can cause liver, and gallbladder cancer, immune suppression. • Penicillium citrinin, Aspergillus oryzae, Monascus ruber (citrinin)-present in wheat, oats, rye, corn, barley, rice, italian sausages-nephrotoxin. • Claviceps (ergot alkaloids) • Fusarium verticillioides(Fumonison B) esophageal cancer. In corn, grits in the south. Mycotoxins • Aspergillus ochraceaus(Ochratoxin) Kidney is the target. Inhibits mitochondrial ATP production, stimulates lipid peroxidation. In port, chicken. • Penicillium patulum(patulin) blue mold on apples, pears, cherries- found in apple juice. Maximum intake 0.4mg/kg. • Fusarium, Stachybotrys (trichothecenes) moldy straw, hay, wet building material. Leads to hemorrhages, vomiting, dermititis. • Fusarium graminearum(zearalenone) increased estrogen activity. Early menarche, infertility. Mycotoxemia Metabolite Disease Organisms Health Concerns Gliotoxin Invasive aspergillosis Aspergilus, Trichoderma, Penicillium, Candida Immune toxicity, suppression, neurotoxicity Aspergillic acid, Carcinogenesis Aspergillus flavus Liver cancer, immune toxicity Aflatoxins Carcinogenesis, reye syndrome, kwashiorkor, hepatitis, cirrhosis Aspergillus, Penicillium, Fusarium Liver pathology (including cirrhosis) and cancer, immune toxicity Fumigaclavines, gliotoxin Aspergillosis Aspergillus fumigatus Lung disease, neurotoxicity, tremors, immune toxicity Mycotoxemia Metabolite Disease Organisms Health Concerns Ochratoxin A Urinary tract tumors, aspergillosis, renal cell carcinoma Aspergillus niger, penicillium, aspergillus ochraceus Nephropathology including chronic kidney disease. Trichothecenes IgA nephropathy Trichoderma Trochothecene toxicity Fumonisins CNS birth defects Fusarium merticillioides (moniliforme Neural tube defects, liver pathology, esophageal cancer. Satratoxins (FGH), Stachybotrylactams Pulmonary Bleeding Chachybotrys chartarum Respiratory bleeding, Protein synthesis, inhibition, neurotoxicity, cytotoxicity Elimination Gut-Lungs-Skin-Kidneys Deutscher 70 Imbalanced Detoxification Phase 1 CYP P450 Non-Polar Xenobiotic Phase 2 Conjugation Reactive Intermediate Inert Water-Soluble Metabolite Damage to DNA, RNA, Proteins Reactive Oxygen Species Glucuronidation Works with Sulfation, acetaminophen, low activity liver, high activity gut microflora, Gilbert. Increased colon cancer, modify heterocyclic amines Sulfation Alzheimers, Parkinsons, motor neuron disease, RA, delayed food sensitivity , Multiple Chemical Sensitivities, Diet responsive Autism Acetylation (NAT) Carcinogens from cigarette smoke, barbeque associated with breast cancers in smokers Quinone Reductase Auto exhaust, cigarette smoke, burned organic materials. Inhibited by benzopyrene, quercetin, resveratrol. Associated with Parkinsons. Key Benzene Epoxide Hydrolases Oxidative defense, Polycyclic aromatic hydrocarbons, benzopyrene. Low activity decrease lung cancer, involved in BP regulation, inflammation, CA N-,O-, S-Methylation Methylate sulfur>methionine, homocysteine. Methylation of DNA nucleotides. Inadequate methylation>Breast CA, Alzheimers, Parkinsons, CAD Amino Acid Conjugation Xenobiotic acyl CoA thioester. Heavy alcohol consumption, intestinal toxicity, toxemia of Pregnancy have inadequate amino acid conjugation Glutathione Conjugation Absence> lung & breast. Kidney, bladder, colorectal CA. Low levels. Upregulation protects against diesel exhaust. Low in HIV, ETOH, Cd,MDG. Parkinsons Functional Lab Tests To assist the evaluation of the toxic patient Nutritional & Assimilation Toxic Damage Body Burden Genetic Susceptibility 1. Nutritional & Assimilation Tests 2. Toxic Damage Assays 3. Body Burden Tests (Biomonitoring) 4. Genetic Susceptibility (SNP Tests) “Sorry Doc...I drank last night I have a headache- but a Triple Espresso, 2 Tylenol and an Aspirin...poof! works everytime!” Caffeine ASA Phase 1 Oxidation Caffeine Clearance Demethylated Products Acetaminophen Salicylic acid P450s Catechol 23 Dihydroxybenzoate Toxic Metabolite Tissue Damage (NAPQI) Phase II Conjugation Glutathione Conjugation Mercapturate Sulfation Acetaminophen Sulfate Glucuronidation Acetaminophen glucuronide Glycine Conjugation 2 hydroxyhippurate Acetaminophen with Alcohol Phase 1 and 2 Mismatch Phase I [cytochrome P450 enzymes] Lipid-soluble molecule Phase II [conjugation pathways] Activated Intermediates GSH excretory derivatives riboflavin (vitamin B2) polar CYP2E1 ( water-soluble ) ATP niacin (vitamin B3) glutathione pyridoxine (vitamin B6) glycine Serum folic acid, vitamin B12 taurine 1) Alcohol CYP2E1 Vitamin C,induces glutathione, CoQ10 glutamine Kidneys alpha lipoic acid 2) Increased Acetaminophen breakdown ornithine and branched-chain amino acids arginine Urine production of Reactive metabolite NAPQI flavonoids methyl donors phospholipids Bile N-acetylcysteine (N-acetyl-p-benzoquinoneimine) pantothenic acid cysteine 3)This is TOXIC and requires Glutathione (GSH) in Iron Selenium, Copper, Zn, Mn methionine Feces/stools the Phase 2 pathway to Clear. 4) Alcohol consumers have lower GSH levels (PHASE III) Genomic Testing Methylation SNPS • Detoxification SNPS Genetics Epigenetics (Lifestyle) Phenotype Metabolomics Work up of the Toxic Patient? Pattern Recognition Total Toxic Load (Body Burden) Over extended periods of time, small daily doses of multiple contaminants have cumulative detrimental effects on physiologic pathways that can eventually impair health and cause disease. Toxicant-Induced Loss of Tolerance (TILT) NA Ashford, Chemical Exposures: Low Levels and High Stakes, 1998 • Loss of tolerance following acute or chronic exposures to pesticides or carpet vapors • Manifests as triggering of symptoms involving multiple organ systems by minute quantities of formerly tolerated chemical substances P: Pattern Recognition Gathering and Organizing History Agent Orange DM, CRF Age Birth 22 45 ap photo/viktor pobedinsky/efrem Lukatsky March 28, 2002 Dec 6 2004 Dioxin Poisoning Endocrine Toxicity Tetrachlorodibeno-p-dioxin How Long-time How Much- dose How Often- frequency Individual variables: Birth age, body mass physical condition Smoker, drug/alcohol Chloracne 21 months Age Dioxin 2,3,7,8-tetrachlorodibenop-dioxin (TCDD) on Physical Exam • Erythema or edema face • Non infllamatory comedones straw colored cysts in a few days, occasional pustules, non infectious abscesses • Face neck, then trunk extremities, genitalia • Comedones face and neck especially below the outer side of the eye (malr crescent), postauricular triangles. • Cysts: neck, shoulders, chest-back, penis, scrotum, axilla. Nose perioral skin and supraorbital regions usually spared. • Other skin lesions: xerosis, pigmentation, porphyrinopathy, hirsutism, skin thickening palmoplantar hydrosis, palmoplantar hyperkeratosis. • Symptoms: fatigue, anorexia, neuropathy, impotence, liver dysfunction, hyperlipemia, anemia, arthritis, thyromegaly onset 2-4 weeks, last 2-3 to 15-30 years. • Chilren (<8 years) with light hair color more susceptible to chloracnegens. SGA, Stress Maternal Exposures> Fetal Exposures DM, CVD HTn, Obesity Signs, Symptoms or Diseases Reported over time until a TILT to Diagnosis Antecedents Parenthood Pregnancy Job/Economic Stress Preconception >First Month 12-18 months 10-18 yrs B Vitamin Tanner Changes Stores Androgenation Triggers or Triggering Events decrease 18-30 6-7 years Social EFA change Habits •Foods •Stress Birth Prenatal Preconception Pregnancy Cognitive changes Latency diseases •Microbes 30-50s Glucose •Toxins Intolerance •Allergens Current Concerns Latency Diseases... Or Seasons of Vulnerability Signs, Symptoms or Diseases Reported http://www.panna.org/publication/generation-in-jeopardy Age Birth Further considerations for this physical exam finding… Significant associations between low intakes of various nutrients (retinol, calcium, fiber, folate, iron, riboflavin, thiamin, vitamins A, C, and E) and keratotic skin lesion incidence in people exposed to environmental arsenic. Greater intakes of methionine, Cysteine, protein and vitamins such as thiamin and niacin increased arsenic secretion. Mekonian S et al: J Nutr 142:2126-2134,2012 Metabolic Toxicity Genotoxicity Stevens Johnsons . Photos: M.Stone,M.D Immunotoxicity The Patient’s Story Retold Physiology and Function: Organizing the Patient’s Clinical Imbalances Assimilation Antecedents Triggering Events Defense & Repair Genotoxicity Structural Integrity Energy Immunotoxicity Endocrine Toxicity Mediators/Perpetuators Communication Spiritual Biotransformation & Elimination Mitochondrial Toxicity Transport Metabolic Toxicity Personalizing Lifestyle Factors Sleep & Relaxation Neurodevelopmental Stress & Resilience Nutrition & Hydration Toxicity Exercise & Movement Name:____________________________ Date:___________ CC:_____________________________________ Relationships & Networks © Copyright 2011 Institute for Functional Medicine Work up of the Toxic Patient? Identification, Evaluation, Treatment “Cannot Detox The Burden” Overtly Undernourished Functionally Undernourished Quality Diet, Food, Nutrient Context Company History-Timeline Network Influences Symptoms, Other Signs Current Biochemical Markers Quantity Diet, Food, Nutrient The ABCDs of Functional Nutrition Evaluation (Identifying Detox Related Nutrition Concerns) Functional Nutrition Evaluation (ABCD) 1) Anthropometrics: weight, change, height, Waist,Hip circumference, routine vitals, bioelectric impedance analysis, 2) Biochemical Indicators-Labs; conventional and functional. 3) Clinical Indicators: Physical exam Hair to toenails. Functional testing: smell, peak expiratory flow rate, oxygen saturation, visual contrast testing. 4) Diet, Nutrition, and Lifestyle evaluation: includes exercise, food, timing of eating, supplement intake, medication intake, sleep, Assessing Body Composition Dx:OverVAT or OverSAT Dx: Overweight Abnormal High BMI? NO YES >25 Overwt >30 Obese NO Increased WC or WHR? YES NO YES YES YES Increased BIA Fat%? YES Increased BIA Fat%? NO NO YES Increased WHR? NO Increased WHR? Increased BIA Fat%? NO YES Increased WC? Dx: OverFAT Android Obesity (OverVAT) NO Metabolically Gynoid Possible High Increased Obese Obesity/ Muscle Mass BIA Fat%? or Large (OverVAT) overSAT Skeletal Frame YES MetSyn? YES Ideal Skinny Fat or Possible High Gynoid Metabolically Muscle Mass Obesity/ Obese or Athlete overSAT Gut/Detox/HPATGG dysfunctions? TLC Nx/ Rx Assessing Body Composition Dx:OverVAT or OverSAT Dx: Overweight YES Abnormal High BMI? YES Increased WC? >25 Overwt NO >30 Obese NO Immunotoxicity Increased WC or WHR? YES NO Increased BIA Fat%? YES YES Endocrine Toxicity Android Obesity (OverVAT) NO Metabolically Gynoid Possible High Increased Obese Obesity/ Muscle Mass BIA Fat%? or Large (OverVAT) overSAT Skeletal Frame Mitochondrial Toxicity NO YES NO Genotoxicity Increased BIA Fat%? YES NO Increased WHR? Increased BIA Fat%? YES Increased WHR? Metabolic Toxicity NO Dx: OverFAT YES MetSyn? YES Ideal Skinny Fat or Possible High Gynoid Metabolically Muscle Mass Obesity/ Obese or Athlete overSAT Gut/Detox/HPATGG dysfunctions? TLC Nx/ Rx Anthropometrics Biomarkers and Functional Labs (PFC-MVP) Clinical Indicators from Nutrition Physical Exam Diet and Lifestyle Assessment P F C M V P R A A R I I H Y O T E I T B O H Y D R N E R A T A M I T O N U T R I A T E L S N S EN TS N & O I L S Anthropometrics Biomarkers and Functional Labs (PFC-MVP) Clinical Indicators from Nutrition Physical Exam Diet and Lifestyle Assessment Core Aspects of the Nutrition Physical Exam 1) Vitals and Body Composition 2) Evaluate Smell and taste 3) Look in the Mouth 4) Look at and feel the Skin 5) Look at the Nails 6) Evaluate Peripheral Sensation Clinical Indicators Using a nutrition-focused physical exam gingivitis koilonychia Keratosis pilaris geographic Nutritional Assessment by Nutrient and Location Tongue • Geographic tongue: Folate, Vitamin B12, Zinc, Genetic • Sore, reddened tongue: Niacin, folate, vitamins B12 and B6, biotin, riboflavin • Filiform papillary atrophy: Niacin, iron, folate, vitamin B12, riboflavin • Glossitis: Riboflavin, folic acid, pyridoxine, niacin, vitamin B12, iron • Hypogeusia (diminished taste acuity): Zinc • Teeth indentations on tongue: Food allergy(ies) • Tongue fissuring: Niacin • Halitosis: Niacin Hands/Fingers/Fingernail s • Cracks and splitting of skin on fingertips: Zinc, Essential fatty acids • Slightly swollen, painful PIP joints: Glucosamine sulfate and chondroitin – Niacinamide, "Nightshade" vegetable allergies • Painful, swollen MCP joints, as well as wrists and other joints: (rheumatoid arthritis) Food allergy(ies), Niacinamide, Eicosatetraenoic acids, • Tender lumps on finger end joints: Niacinamide, vitamin B6 • Fingernails that are weak, thin, bend easily, frequently crack and chip: Underfunctioning stomach (low acid, low pepsin), Essential fatty acids, Calcium, Zinc • Transverse depigmentation: Protein Hands/Fingers/Fingernails • White pitting, Spots (leukonychia): Zinc • Psoriatic nails: Vitamin D • Fingernails that are ridging, brittle, easily broken, flattened, spoon-shaped, thin, lusterless, Beau's lines, Meuhreke's lines: Iron, copper, zinc, protein • Onycholysis: Iron, niacin • Chronic paronychia: Zinc • Splinter hemorrhages: Vitamin C • Pale nail beds: Iron Zinc • Look at clinical signs - dermatitis, hair loss, frequent infection, glossitis and nail dystrophy. • • • • • • Lab clues: Low alk. Phosphatase Low RBC / WBC Zn High copper Low vitamin A / beta carotene ratio. Plasma zinc responds to supplementation. Laboratory Tests and Diag Procedures 5th edition, 2008 Journal of Nutrition. 2000;130:1350S-1354S Prasad AS, et al. Am J Clin Nutr. 2007 Mar;85(3):837-44 Leukonychia ?? Magnesium • Neurological: sleep disturbances, over-sensitivity to light and noise, autism, ADD, ADHD, depression, anxiety, confusion, disorientation, tingling, numbness, seizures, migraine • Cardiovascular: mitral valve prolapse, hypertension, myocardial infarction, arrhythmias • Autoimmune: RA, MS, ALS • Misc. metabolic: Insulin resistance, diabetes, metabolic syn., PMS, chronic fatigue, renal stones, asthma, alcoholism • Musculoskeletal: cramps, fibromyalgia, osteoporosis • Gastrointestinal: constipation, Crohn’s, gluten enteropathy, intestinal surgery Iron Deficiency • • • • Reduced physical work capacity Impaired cognitive function Pale tongue, cheeks, and conjunctivas Angular stomatitis, filiform papillary atrophy, glossitis, temperature control issues • Fingernails that are ridging, brittle, easily broken, flattened, spoon-shaped, shaped, thin, lusterless, pale nail beds • Microcytic anemia • Plummer Vinson syndrome – esophageal constriction, weakness Vinik AL: Diabetic Neuropathy in Older Adults. Clin Geriatr Med 24(3)407-v, doi:10.1016/j.cger.2008.03.011, 2008. Nutrition and Neuropathy Nutrient Neurologic Symptoms Thiamin Beriberi (dry, wet, infantile, gastrointestinal, bariatric), Wernicke encephalopathy or Korsakoff syndrome, encephalopathy, sensorimotor distal axonal peripheral neuropathy, calf cramping, muscle tenderness, burning feet, irritability. Niacin Peripheral neuropathy, encephalopathy Pyridoxine Peripheral neuropathy, pure sensory neuropathy in toxicity Folate Similar to cobalamin deficiency, peripheral neuropathy Cobalamin Myelopathy, peripheral neuropathy, neuropsychiatric, optic neuropathy, autonomic dysfunction Vitamin D Cutaneous hyperalgesia, bone pain of osteomalacia Vitamin E Spinocerebellar syndrome, peripheral neuropathy, opthalmoplegia Copper Myelopathy/myeloneuropathy Protein Muscle wasting, weakness, hypotonia, hyporeflexia Kumar, N: Neurologic Presentations of Nutritional Deficiencies. Neurol Clin 28:107-170. 2010. Nutrition and Neuropathy Nutrient Lab Treatment Thiamin Serum Thiamin, RBC transketolase, RBC thiamin diphosphate, Urinary Thiamin Thiamin IV, IM, Oral Niacin Urinary excretion of methylated niacin metabolites Nicotinic acid oral, IM Pyridoxine Plasma pyridoxal phosphate, P5P Pyridoxine oral (P5P over Pyridoxine HCL if using higher doses) Folate Serum, RBC Folate, Plasma Hcy,…SNP- MTHFR, Urine Formiminoglutamic Acid Methyl folate, folate Cobalamin Serum Cbl, MMA, plasma Hcy, CBC, MCV… IM B12, Methyl cobalamin, Hydroxy cobalamin Vitamin D 25 OH vitamin D, 1,25 DHCC, PTH, Ionized Ca Appropriate Vitamin D dosing Vitamin E Serum Vitamin E ratio (a-tocopherol to sum serum cholesterol+TG) Vitamin E oral or IM Copper Serum, RBC, Urinary Copper, serum ceruloplasmin, CBC (anemia, neutropenia, vacuolated myeloid precursors) Oral elemental copper Glucose Fasting, 2 hour GTT, Insulin, Hgb A1C, triglycerides Low Glycemic Index, Movement, Multifactorial Kumar, N: Neurologic Presentations of Nutritional Deficiencies. Neurol Clin 28:107-170. 2010. Mitochondrial Toxicity Figure 8.9 Functional Medicine Clinical Nutrition Textbook Anthropometrics Biomarkers and Functional Labs (PFC-MVP) Clinical Indicators from Nutrition Physical Exam Diet and Lifestyle Assessment Diet, Nutrition, and Lifestyle Journal 1- Diet and Nutrition... Eat Not too much, mainly plants... 2- Lifestyle... Does it Stack Vulnerabilities by Increasing Toxicant Exposure? 3-Is there a Quality to Quantity Mismatch? Macronutrients Micronutrients & Phytonutrients Immunotoxicity Genotoxicity Mitochondrial Toxicity Endocrine Toxicity Metabolic Toxicity Neurodevelopmental Toxicity Complete Workup of the Toxic Patient • Who: symptoms, diseases use questionnaires to help • What: Exotoxins/ endotoxins-labs as needed • Where: What part of the system is affected. Physical exam and Laboratory • When: Timeline to help pinpoint exposure or ongoing issues with clearance • Why: ABCD of Nutrition Evaluation The power of identifying basic insufficiencies and excesses • Now Proceed to Treatment Restoration of Health in the Toxic Patient depends on• Pattern Recognition • Undernutrition-Correcting mismatch of nutrition requirements • Reduce Exposure • Ensure safe detoxification Functional Nutrition Fundamentals & PFC-MVP Nutrition Assessments Gather Organize Re-Tell Order/Prioritize Initiate PFC-MVP Assessments Thank you for the Opportunity to Participate in this Great Event Thank you to Institute for Functional Medicine for their contributions. I want to acknowledge the IFM Detox Team: Kristi Hughes, N.D Bob Rountree, MD Deanna Minich PhD, Rick Mayfield DC, Our Clinic Staff at at Stone Medical. mstone@ashlandmd.com