M01 Morphine sulphate: Administration
advertisement

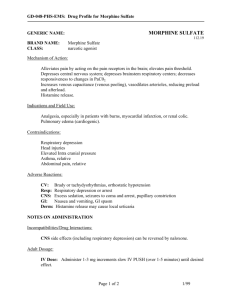
Standard Operating Procedure SOP ID M01 Version 1.0 Title Morphine Sulphate: Administration Approved by Medicines Management Group Date Issued 1st February 2013 Review Date 31st January 2015 Directorate Clinical Clinical Publication Category Mandatory - No deviation from document permissible 1. Scope 1.1 This Standard Operating Procedure (SOP) describes the process for the administration of morphine sulphate 10mg injection and morphine sulphate 10mg in 5ml oral solution by nurses and paramedics employed by the Trust. 1.2 This SOP provides additional guidance which is specific to the administration of morphine and should be read in conjunction with the SOP on Administration of Medicines. The processes which govern the administration of all other medicines apply equally to morphine. 1.3 The SOP covers choosing a route of administration, safer dosing with opioid medicines and how to make a decision about whether a patient must be conveyed to hospital or can be left on-scene. It describes the action to be taken when a dose greater than 20mg is required to provide pain relief. 1.4 This SOP applies to the administration of morphine sulphate 10mg injection and 10mg in 5ml oral solution from Trust stock. It does NOT cover the administration of patients’ own medicines, which must only be administered in accordance with a Patient Specific Direction from an independent prescriber. 1.5 This SOP does not cover administration via a syringe driver, as Trust Policy does not permit the use of syringe drivers. If a patient receiving palliative care requires additional pain relief, the clinician should consider oral or intramuscular morphine and arrange for specialist follow up. 1.6 The use of the terms nurse and paramedic within this SOP refer to registered clinicians only. 2. Responsibility 2.1 The Accountable Officer has overall responsibility for this Standard Operating Procedure and the safe management and use of controlled drugs within the Trust. 2.2 It is the responsibility of all ambulance clinicians to adhere to this Standard Operating Procedure. It must be noted that an SOP does not remove a clinician’s inherent professional responsibility and accountability. 2.3 It is the responsibility of the clinician to use their professional judgement to determine the correct route of administration and to record their reasoning and decision in the patient’s clinical record. 2.4 Individual clinicians are responsible for ensuring that morphine is administered safely in accordance with nationally recognised best practice, current legislation and Trust Policy. 3. Introduction 3.1 The overall legislative framework which applies to all medicines is the Human Medicines Regulations 2012 and associated legislation. 3.2 Controlled drugs (CDs), are additionally defined and governed by the Misuse of Drugs Act (MDA) 1971 and associated regulations - principally the Misuse of Drugs Regulations (MDRs) 2001. 3.3 The MDRs 2001 divide controlled drugs (CDs) into five Schedules, which dictate the degree to which a CD’s use is regulated. The Schedule in which a CD is placed depends upon its medicinal or therapeutic benefit balanced against its harm when misused. Schedule 1 CDs are subject to the highest level of control, morphine sulphate 10mg injection is a Schedule 2 CD, whilst oral morphine solution 10mg in 5ml is a Schedule 5 CD. 3.4 The use of CDs in medicine is permitted by the MDRs. The current version of the Regulations made under the MDA 1971 are the MDRs 2001, which came into operation in February 2002. The MDRs are periodically amended and revised and the 2001 MDRs have been subject to a number of amendments. 3.5 Paramedics are authorised to possess morphine sulphate injection (up to a maximum preparation strength of 20mg) and oral morphine, and may administer up to a total dose of 20mg of morphine (cumulative total for solution and injection) per patient for the immediate necessary treatment of sick or injured persons by the MDRs 2001: Group Authority for NHS ambulance paramedics and employing ambulance trusts. 3.6 Changes made to the MDR in April 2012 allow all nurses to possess and administer (under a PGD) morphine sulphate 10mg injection for the immediate, necessary treatment of sick or injured persons. They also allow Nurse Independent Prescribers to possess, prescribe, administer and give directions for the administration of schedule 2, 3, 4 and 5 controlled drugs. NIPs may not give verbal orders for controlled drugs. 3.7 Nurses, including NIPs, and paramedics may only administer morphine sulphate 10mg injection for the management of severe pain or to manage the pain of a myocardial infarction. 3.8 Nurses, including NIPs, and paramedics may only administer morphine sulphate 10mg in 5ml oral solution for the management of moderate to severe pain. The delay experienced before relief is obtained with oral morphine is attributable to absorption. 4. Preparation 4.1 The nurse or paramedic is responsible for ensuring that naloxone is immediately available, and the dose for the patient known, before morphine is administered, in case it is required to counteract the effects of morphine. 4.2 The patient response to morphine can vary widely and is partly dependent on previous doses received. Except in the most acute emergency, before administering morphine to a patient who has received recent doses of opioid drugs: Confirm and record on the patient clinical record details of any recent opioid dose, including the type of opioid and frequency of administration. Any other non-opioid analgesic medicines prescribed for the patient should be recorded. Check the dose of morphine to be administered, indications and contraindications. Ambulance clinicians must refer to the current Joint Royal Colleges Ambulance Liaison Committee (JRCALC) Guidelines. Nurses, who are not NIPs, must refer to the Trust PGD for morphine sulphate 10mg injection or the PGD for oral morphine, and NIPs must refer to the JRCALC Guidelines, the Trust PGDs or the current edition of the British National Formulary (BNF). Eliminate the possibility of opioid toxicity. In palliative care opioid toxicity may present as subtle agitation, seeing shadows at the periphery of the visual field, vivid dreams, visual and auditory hallucinations, confusion, and myoclonic jerks. Agitated confusion may be interpreted as uncontrolled pain and further opioids given. A vicious cycle then follows, in which the patient is given sedation and may become dehydrated, resulting in the accumulation of opioid metabolites and further toxicity. 4.3 Ensure that you are familiar with the following characteristics of morphine before administering it to a patient: Usual starting dose Frequency of administration Standard dosing increments Symptoms of overdose Common side-effects 4.4 Always use the lowest effective dose of morphine 5. IV/IO Administration of up to 20mg of Morphine Sulphate 10mg Injection 5.1 The contents of one 10mg ampoule of morphine sulphate must be drawn into a 10ml syringe and diluted to 10mls with sterile sodium chloride 0.9% for injection (saline) to prepare an injection of morphine sulphate 10mg in 10ml (1mg in 1ml). 5.2 The syringe containing the morphine sulphate 10mg in 10ml injection must immediately be labelled with a blue, pre-printed morphine label. These labels must be kept in the morphine pouch with the ampoules. 5.3 Individual nurses and paramedics can administer a maximum dose of 20mg of morphine sulphate injection to any one patient. 5.4 Warn the patient that they may feel drowsy or experience some nausea; slow titration of the dose will reduce this effect. 5.5 Adults and Children Aged 12 Years and Over 5.5.1 Administer 5mg morphine by slow IV/IO injection in conjunction with pain scoring and titrate to response. In medical cases, smaller doses of 2.5 - 5 mg tend to be more effective. Trauma patients may require larger doses of 5 - 20mg. 5.5.2 Administer at a rate of approximately 1mg per minute. The patient must be observed for the next 5-10 minutes to note the response. 5.5.3 If the pain is not reduced to a tolerable level after 5 minutes, further 2.5 to 5mg doses may be given by slow IV/IO injection at 5 minute intervals to the 20mg maximum 5.5.4 Administer an anti-emetic if clinically indicated. 5.5.5 Morphine when given IV/IO takes a minimum of 2-3 minutes to begin to work, with the peak effect not being achieved for 10 to 20 minutes. Observe the patient closely throughout any remaining treatment and transfer. 5.5.6 All patients receiving IV/IO morphine must be conveyed to hospital. SOP C09 Deployment, Supervision and Clinical Practice of ACAs, ECAs, Student Paramedics and Advanced Technicians details the level of clinician which must accompany the patient. 5.6 Children Aged Under 12 Years 5.6.1 The doses and volumes given in JRCALC and the PGD are the initial and maximum doses. Administer 0.1ml/Kg (equal to 0.1mg/Kg) as an initial slow bolus over 2-3 minutes. If the pain is not reduced to a tolerable level after 5-10 minutes then further doses of up to 0.1mg/Kg, titrated to response, may be repeated, at 5-10 minute intervals, up to the maximum dose 0.2mg/Kg. 5.6.2 Administer an anti-emetic if clinically indicated. 5.6.3 All patients receiving IV/IO morphine must be conveyed to hospital. SOP C09 Deployment, Supervision and Clinical Practice of ACAs, ECAs, Student Paramedics and Advanced Technicians details the level of clinician which must accompany the patient. 6. IM Administration of Morphine Sulphate 10mg injection 6.1 The intramuscular route of administration may be considered: In adults and children aged 12 years and over. The route of administration must be clinically justified and the rationale for the decision must be recorded in the PCR. The intramuscular route must not be used when the patient’s circulation is compromised e.g. the patient is in shock, hypothermic etc, due to the variable absorption rate of morphine given IM, and the potential for a delayed response when the circulation recovers. IV or oral routes are unavailable In a mass casualty situation 6.2 A variety of factors affect morphine absorption from the intramuscular site making the absorption rate variable. Do not use this route if patient is experiencing a myocardial infarction. 6.3 The contents of one 10mg ampoule of morphine sulphate must be drawn into a 1ml syringe and used UNDILUTED. 6.4 The syringe containing the morphine sulphate 10mg in 1ml injection must immediately be labelled with a blue, pre-printed morphine label. 6.5 Individual nurses and paramedics can administer a maximum dose of 20mg of morphine sulphate 10mg injection to any one patient. 6.6 6.7 Warn the patient that they may feel drowsy or experience some nausea. Adults and children 12 years and over: Administer 2.5 to 10mg in conjunction with pain scoring. Elderly or frail patients, or patients with a small body mass may require lower doses. 6.8 Observe the patient for at least 20 minutes after administration. 6.9 Administer an anti-emetic if clinically appropriate. 6.10 Paramedics and nurses who are not authorised to practice as an Emergency Care Practitioners (ECP) or Nurse Practitioners (NPs) must then convey the patient to hospital. SOP C09 - Deployment, Supervision and Clinical Practice of ACAs, ECAs, Student Paramedics and Advanced Technicians details the level of clinician which must accompany the patient. 6.11 Nurses and paramedics who are authorised to practice as an ECPs or NPs may decide to leave a patient at home. The individual clinician is responsible for making this decision and must feel confident and competent to do so. 6.12 If the patient is left at home they must be accompanied by a responsible adult. 6.13 The NP/ECP is responsible for: Arranging follow up. Ensuring that the patient and their carer is given written and verbal advice on what to do if their condition worsens or deteriorates Communicating with the patient’s GP, using local mechanisms, or directly, to inform him/her of the consultation, outcome and medication supplied. Leaving information that will advise another healthcare professional that morphine has been administered. 7. The Administration of Oral Morphine Sulphate 10mg in 5ml 7.1 Oral morphine solution is used to provide relief from moderate to severe pain in adults and children over 1 year of age. Oral morphine must be administered according to the Trusts PGDs. 7.2 It is presented in a sealed unit dose form (5ml) with an oral syringe. 7.3 The oral route may be more acceptable to children and prevent further distress. The oral route avoids the risk of infection associated with parenteral administration. 7.4 Oral morphine should not normally be used when pain relief is urgently required. However, if the IV, IO and IM routes are not appropriate, consider providing early analgesia using entonox whilst oral morphine has time to take effect. 7.5 Before administering warn patient, parent or carer that the medicine may cause drowsiness. Adults who are left at home should not drive or operate machinery if affected and should avoid alcoholic drink as this may increase drowsiness. Advise that morphine may cause nausea. 7.6 If the patient is vomiting before morphine is administered, administer an anti-emetic and allow to take effect before giving the dose of oral morphine. 7.7 To administer: Check bottle seal is intact. Break seal and open bottle. Draw required dose into oral syringe. Administer to patient. 7.8 Administer an anti-emetic if clinically appropriate. 7.8 Adults and Children Aged 12 Years and Over 7.8.1 Administer up to 10mg oral dose initially. This dose may be reduced to 5mg in frail elderly patients and those with reduced body mass. Note the response and if needed give a further dose of 10mg (5mg frail elderly) after 30 minutes. A total dose of up to 20mg may be administered according to response. 7.8.2 Paramedics and nurses may choose to leave an adult patient aged 16 years and over at home. The clinician is personally responsible for assessing the patient and making this decision. They must feel confident and competent to do so. 7.8.3 If the patient is left at home they must be accompanied by a responsible adult. 7.8.4 Observe patient for at least 20minutes following administration. The onset of action will be longer for oral morphine than parenteral morphine. Side-effects will not become immediately apparent and may occur up to 15 minutes after administration. 7.8.5 The nurse or paramedic is responsible for: Arranging follow up. Provision must be made to ensure appropriate analgesia after the effects of the administered oral dose have worn off. Non-NP/ECPs must consult with an NP/ECP or Doctor who is able to supply analgesia. Ensuring that the patient and their carer is given written and verbal advice on what to do if their condition worsens or deteriorates Communicating with the patient’s GP, using local mechanisms or directly, to inform him/her of the consultation, outcome and medication supplied. Leaving information that will advise another healthcare professional that morphine has been administered. 7.9 Children Aged 11 Years and Under 7.9.1 Administer according to the dose detailed in the Trust’s PGD (or British National Formulary for Children for NIPs). All children who receive oral morphine must be conveyed to hospital. SOP C09 - Deployment, Supervision and Clinical Practice of ACAs, ECAs, Student Paramedics and Advanced Technicians details the level of clinician which must accompany the patient. 8. Administration of Morphine Sulphate 10mg Injection to Partners, Family and Friends 8.1 Other than in emergencies, no clinician must administer a controlled drug to anyone with whom they have a close personal, emotional or sexual relationship. In an emergency situation, if this is unavoidable, the clinician administering the morphine is responsible for completing a Trust incident report and informing the Accountable Officer. 8.2 Any staff member who suspects that such an incident has occurred but has not been reported is responsible for alerting the Accountable Officer (SOP - Discrepancies). 9. Administration to Patients with Known or Suspected Controlled Drug Dependency Problems 9.1 Patients with known or suspected controlled drug dependency problem must not be administered morphine except when there is a genuine need for nurses or paramedics to administer morphine for pain relief in an emergency. 9.2 If a nurse or paramedic has any doubts about administering a controlled drug to a patient, they should consider the use of an alternative medicine or seek the advice of a doctor, or senior colleague before administering the morphine. The clinician must document any advice they receive on the patient clinical record or Adastra system. 10. Administration of Doses of Morphine Exceeding 20mg 10.1 Paramedics and nurses are authorised to administer a total of 20mgs of morphine to an individual patient. When morphine is administer by different routes, the total amount of morphine administered IV, IO, IM and orally by a paramedic/nurse to an individual must not exceed 20mgs. This is a legal requirement. 10.2 The Trust acknowledges that in some cases doses in excess of 20mg may be required to manage a patient’s pain. 10.3 if the attending registered nurse or registered paramedic feels that it is in the patient’s best interest to administer a total dose of morphine sulphate greater than 20mg and the patient is aged 18 years and over, a second registered paramedic or registered nurse may administer up to 20mg of morphine sulphate in addition to the 20mg administered by the first clinician. 10.4 The two clinicians must agree that a further dose is appropriate and may contact a Doctor or the Senior Clinical Advisor On-call for advice before making a decision. 10.5 The following restrictions apply: Patient must be aged 18 years or over. An initial dose of 20mg must have been administered via the IV, IO or oral route and the patient’s response recorded. Where administered, the increased time for maximal effect of oral morphine must be taken into consideration. A second dose is not authorised by the Trust if the initial 20mg dose of morphine was administered by the IM route. 20mg dose is the maximum second dose and the actual dose administered must be titrated to response. The second dose must be administered via the IV or IO routes. Further doses of IM or oral morphine are not permissible. There must be a clear rationale for further morphine being required e.g. entrapment RTC, long journey time to hospital. Both clinicians have considered any advice received and after reassessing the patient agree that it is necessary to increase the dose of morphine sulphate 10mg injection. The total maximum dose administered must not exceed 40mg 10.6 The clinicians administering the morphine are professionally accountable for the decision to administer the additional dose of morphine, even if advice is received from a Doctor or other clinician, as it is not possible to give or receive a verbal direction for care (verbal order) for morphine sulphate 10mg injection. 10.7 If the decision is made to administer additional morphine the following must be recorded: Any advice received from a Doctor or the Senior Clinical Advisor On-call The rationale for the increased dose 10.8 Both clinicians must sign the entry in the patient clinical record and both clinicians must make an entry in their personal morphine record book recording the administration which is then countersigned by their colleague. 11. Handover of a Patient who is Receiving Parenteral Morphine Sulphate 10mg 11.1 When a paramedic hands over a patient to whom they have already administered morphine sulphate 10mg injection, to another paramedic or nurse, they must retain and destroy any morphine remaining from their own personal issue. The receiving paramedic must administer the morphine from their own personal issue. 12. Disposal of Unused Morphine Doses 12.1 The clinician is responsible for ensuring that any remaining morphine in a parenteral or oral syringe is disposed of safely following an episode of care. The morphine must be discharged into a sharps bin containing absorbent material to render it irretrievable. 12.2 Disposal must be witnessed by another member of staff, another healthcare professional, police officer or carer/parent. 12.3 An entry must be made to record the disposal in the clinician’s personal morphine book. The entry must be signed by the witness (where present) with their name, position or profession printed next to their signature. 13. Record Keeping 13.1 Every administration of morphine sulphate 10mg injection must be recorded in the nurse or paramedic’s personal morphine record book. Administration of oral morphine must be recorded in the appropriate lower schedule controlled drug record book. The entry in the personal morphine book or lower schedule controlled drug record book must state: Date, time Patient’s name Incident number Dose administered Running balance updated 13.2 Entries must be made consecutively in the order that they occurred and may not be made retrospectively. All entries must be completed before the clinician leaves at the end of the shift. 13.3 As indicated above, all disposal must be recorded and witnessed. The entry must record: Date, time Patient’s name Incident number Dose administered Amount disposed of Witness Running balance updated 14. Adverse Reactions and Adverse Incidents 14.1 All adverse reactions to morphine administered by Trust clinicians or adverse incidents involving Trust morphine must be recorded on Trust Incident Reporting System. 14.2 Adverse reactions to morphine must be recorded on the Yellow Card system which can be accessed at http://yellowcard.mhra.gov.uk/ 15. Validation 15.1 This document was developed and validated within the Trust by staff who deliver the service. It was approved by the Medicines Management Group 05 September 2012 and will be reviewed in January 2015. 15.2 Any constructive feedback to improve this SOP should be made in writing to the Trust’s Medicines Management Group. 16. Professional Accountability 16.1 Standard Operating Procedures do not remove inherent professional obligations, accountability or responsibility. It is the responsibility of each professional to practice only within the bounds of their own competence. 16.2 You cannot delegate responsibility for any task under this SOP to anyone else. 17. References National Patient Safety Agency (July 2008), Reducing dosing errors with opioid medicines, accessed 14.06.12 at http://www.nrls.npsa.nhs.uk/resources/?EntryId45=59888