1. Cells and Organelles
advertisement

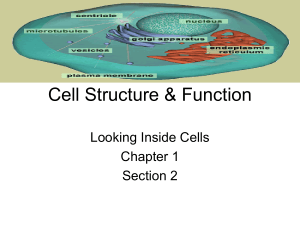
MCD Cells Alexandra Burke-Smith 1. Cells and Organelles Professor Michael Ferenczi (m.ferenczi@imperial.ac.uk) 1. Understand what constitutes a cell, and the scale of cells and molecules Cell Biology Definition of a cell- the basic unit from which living organisms are made, consisting of an aqueous solution of organic molecules enclosed by a membrane. All cells arise from existing cells, usually by a process of division. The body is made up or organs and tissues which are made up on cells and extracellular fluid; a dense material often made of protein fibres embedded in a polysaccharide gel. Some cells can live independently (protozoa), whereas some divide to form colonies of genetically identical daughter cells When cells come together, they can ‘specialise’ by differentiating to give the organism an advantage Some protozoa form occasional colonies when individual cells specialise (e.g. slime moulds, dictyostelium) Cells assemble to form tissues These cells specialise: particular genes are switched on, triggered by signals from their immediate environment (developmental biology), which cause production of mRNA, travels out of cells to manufacture a particular protein. There are about 200 different types of cells in the body These genes produce enzymes which induce the formation of specialised cytoskeleton, organelles, cell-cell contacts, secretion and absorption The distribution of organelles within a cell is unsymmetrical, i.e. one end of the cell faces the lumen and the other the basal membrane, hence polarity is established Definition of polarity- refers to a structure such as an actin filament or a fertilised egg that has an inherent asymmetry so that one end can be distinguished from the other. Scales There is an in-built developmental programme which then responds to external factors, and epigenetic modification of proteins then occurs (changes in the gene expression as a result of mechanisms other than the DNA sequence) Cells are attached to neighbouring cells by membrane junctions, which provide mechanical force and let chemicals through Size of Cells: 10-20 micrometres in diameter Volume of a cell is measured in nanolitres Mass of a cell is typically 1 nanogram. Size of a virus: 10 nanometres A small protein: 40 nanometres Size of molecules: 0.2 nanometres in diameter To see the internal structure of cells, stains are used to look at specific organelles which exploit the differences in refractive indexes of the organelles The human eye is able to distinguish dimensions of objects in the millimetre-metre range, a conventional light microscope can be used for objects in the millimetre-micrometre range (however resolving power limited by wavelengths of light- 400-700nm), otherwise light outside the EM spectrum can be used 1 MCD Cells Alexandra Burke-Smith 2. Demonstrate the following on a suitable transmission electron micrograph: nucleus; nucleolus; nuclear envelope; mitochondrion; rough endoplasmic reticulum; smooth endoplasmic reticulum; ribosomes; Golgi apparatus; secretory granule; plasma membrane; cytoskeletal components. Transmission electron microscopy- uses a beam or electrons and magnetic coils to focus the beam. Specimen is inside a vacuum and very thing. Electron-dense heavy-metal contrast is used to absorb/scatter electrons, removing them from the beam as it passes through the specimen. Minimum resolving power of 0.2nm. Definition of organelles- separate, recognizable sub-cellular structures that perform specialized functions within the cell Organelles Nucleus: Most prominent organelle of a eukaryotic cell. Enclosed within two concentric membranes and contains DNA organized into chromosomes. Nucleolus: large structure in the nucleus where ribosomal RNA is transcribed and ribosomal subunits are assembled Nuclear pores: specialised protein complexes which carefully control and filter the molecules moving between the nucleus and the cytoplasm. Note: adenoviruses have a an advantage as they can travel through/block nuclear pores. Mitochondria: membrane-enclosed organelle, about the size of a bacterium, that carries out oxidative phosphorylation and produces most of the ATP in eukaryotic cells. Vesicles: small, membrane-enclosed, spherical organelles in the cytoplasm of a eukaryotic cell Secretory granules: membrane-enclosed organelle in which molecules destined for secretion are stored prior to release. Visible as small solid object due to darkly staining contents. Golgi Apparatus: membrane-enclosed organelle in eukaryotic cells where the proteins and lipids made in the endoplasmic reticulum are modified and sorted for transport to other sites around the cell Centriole: short cylindrical array of microtubules, usually found in pairs at the centre of a centrosome in animal cells. Also found at the base of cilia and flagella (called basal bodies). Ribosome: particle composed of ribosomal RNAs and ribosomal proteins that associate with mRNA and catalyses the synthesis of protein (translation) Cytoskeleton: system of protein filaments in the cytoplasm of a eukaryotic cell that gives the cell shape and the capacity for directed movement. Its most abundant components are actin filaments, microtubules, and intermediate filaments. Lysosome: intracellular membrane-enclosed organelle containing digestive enzymes, typically those most active at the acid pH found in these organelles. Liposomes: artificially prepared vesicles made from the lipid bilayer. Plasma membrane: the membrane that surrounds a living cell. Cilia: hairlike extension on the surface of a cell with a core bundle of microtubules and capable of performing repeated beating movements. Cilia, in large numbers, drive the movement of fluid over epithelial sheets, as in the lungs. Endoplasmic reticulum: membrane-enclosed component in the cytoplasm of eukaryotic cells, where lipids and secreted and membrane-bound proteins are made Smooth endoplasmic reticulum: region of ER not associate with ribosomes, but involved in the synthesis of lipids. Rough endoplasmic reticulum: region of the ER associated with ribosomes and involved in the synthesis of secreted and membrane-bound proteins. Sarcoplasmic reticulum: specialist form of SER found in smooth and striated muscle. 2 MCD Cells Alexandra Burke-Smith 3. Describe the predominant types of molecules in a cell Cytosol Definition of cytosol- contents of the main compartment of the cytoplasm, excluding membrane-enclosed organelles and cytoskeletal components. Intracellular fluid Site of many chemical reactions including the manufacture of proteins and Glycolysis Constituents: soluble proteins, sugars, ions (K+, Na+, Mg2+, Ca2+, PO4 2-, Cl-), nucleotides (ATP, cAMP: cyclic adenosine monophosphate, GTP: guanosine triphosphate), amino acids, mRNA, t-RNA, lipids and peptides Basement Membrane Thin sheet of fibres that underties the epithelium or endothelium Selective barrier for macromolecules, type VI collagen network, laminas, type XV collagen Type XV collagen- is manufactured within cell, then transported to form membrane. Provides strength. Extracellular fluid Definition of extracellular fluid: complex network of polysaccharides (e.g. glycosaminoglycans, cellulose) and proteins (e.g. collagen) secreted by cells. A structural component of tissues that also influences their development and physiology Ions (Na+, Cl-, PO4 2-, CO3 2-, Mg2+, Ca2+) Soluble proteins, carbohydrates and sugars Vitamins, amino acids, hormones, nucleotides (ATP), lipids, cholesterol Lymph, plasma, saliva, urine, bile, sweat, milk etc 4. Identify the essential characteristics of prokaryotic and eukaryotic cells. Characteristics of all cells All have a cell membrane that separates the outside from the organised interior contain DNA as the genetic material (exceptions e.g. RNA virus) Contain several varieties of RNA molecules and proteins (mostly enzymes). Are composed of the same basic chemicals: carbohydrates, proteins, nucleic acids, minerals, fats and vitamins. Regulate the flow of nutrients and wastes that enter and leave the cell. Reproduce and are the result of reproduction. Require a supply of energy. are affected and respond to the reactions that are occurring within them and many of the environmental conditions around them; this information is continually processed to make metabolic decisions Prokaryotes/Eukaryotes Definition of a prokaryote: major category of living cells distinguished by the absence of a nucleus or other membrane-bound organelles. Single-celled organisms comprising the kingdoms archaea and bacteria. Definition of a eukaryote: living organism composed of one or more cells with a distinct nucleus and cytoplasm. Include all forms of life except archaea, bacteria, and viruses. Evolved from aggregates of prokaryotic cells that became interdependent and eventually fused to form a single larger cell Have a higher degree of organisation than prokaryotes, in that they contain many organelles or structures separated from the other cytoplasm components by a membrane Prokaryotes (Monera and Archaea ) No organelles No nucleus Have external whip-like flagella for locomotion or hair-like pili for adhesion Eukaryotes Membrane-bound organelles Nucleus May have cilia or microvilli on surface of cell membrane 3 MCD Cells Alexandra Burke-Smith Simpler, smaller, haploid Cytoskeleton Cell walls contain PEPTIDO-GLYCAN No cell wall- only cell membrane Shapes: cocci (round), bacilli (rods), and spirilla or spirochetes (helical cells). 5. Understand that movements of molecules and organelles in cells and that the movement of cells are essential processes Cells are dynamic Molecules move spontaneously by diffusion and Brownian motion, which provides the natural mixing of molecules Other forms require energy from the hydrolysis of ATP; active transport, movement of organelles, tuning of hair cells in the ear, movement of cell membranes, growth and migration of cells, nerve growth and development from CNS to target organs, cell division and movement of chromosomes, muscle contraction and the heartbeat All require specialised motor proteins Definition of a motor protein: protein such as myosin or kinesin that uses energy derived from ATP hydrolysis to propel itself along a protein filament or polymeric molecule 6. Explain the relationship of individual cells to the organisation of the whole body. Why cell biology? Development and repair is based on programming the cell cycle and turning on differentiation mechanisms Cancer is when cellular development programs are failing Infections occur when cellular defence mechanisms fail to prevent bacterial invasion Viruses take over the chemical machinery of cells 7. Understand that cancer is a disorder of cell division Definition of cancer: disease caused by abnormal and uncontrolled cell division resulting in localised growths, or tumours, which may spread throughout the body. Mutations that can lead to cancer: Switch on “divide” signals. Switch off “don’t divide” signals. Loss of correction mechanism on DNA copying Loss of escape mechanism from cell division Loss of limit on number of times a cell can divide Loss of control keeping cell within tissue boundaries Ability to evade body defence mechanisms Ability to recruit blood vessels to growing tumour Ability to migrate into blood stream of lymph vessels Ability to establish tumours in the “wrong” tissue. Not all mutations cause cancer because most mistakes which occur during the copying of the genetic code are removed/destroyed Proliferation Under a microscope, you can see migration and tighter packing of cell nuclei evidence of division and stacking of cells Eventually, secondary colonies form within the underlying connective tissue The apoptotic cells then start dying because the tumour has outgrown the supply of oxygen and nutrients 4 MCD Cells Alexandra Burke-Smith 2. Infectious Agents Professor Christoph Tang (c.tang@imperial.ac.uk) Why are we interested in infectious disease? Global cause of death: 52.2 million people/year- 17.4% of all deaths in 2006. These patients also tend to be young, therefore is a selective force from evolution pre-reproduction. Also results in decrease in life expectancy. Community infection e.g. bacterial meningitis Hospital infections e.g. clostridium difficile (C. Diff) Methicillin Resistant Staphylococcus aureus (MRSA) Rise of antimicrobial resistance e.g. mycobacterium tuberculosis Bio-terror e.g. bacillus anthracis (Anthrax) Causes of many different diseases, e.g. Helicobacter pylori causes stomach ulcers, Human papillovirus (HPV) causes cervical cancer New emerging disease e.g. H1N1- Swine Flu Improves our understanding of Biology e.g. identification of first whole genome of free living organism was H. Influenza, and identification of restriction enzymes from E.coli Why do they continue to cause a problem? Mutations: point mutation rate of virus= 10^-11, whereas human cells= 10^-5. The mutation rate is significantly faster in infectious diseases, making successful treatment more difficult Replication: replication rates of infectious diseases when compared to humans is significantly faster (E.coli=20 mins, homosapiens=26yrs), which means spread of infectious disease poses a problem 1. List the main types of infectious agents causing disease and name their distinguishing features Viruses: obligate intracellular parasite consisting of nucleic acid (RNA or DNA) enclosed in a protein coat that make use of a host cell to undergo intracellular replication, and then divide and bud out of the host cell. Viruses show host specifity but have the ability to infect almost all other life forms including bacteria. Bacteria: prokaryotes that replicate by binary fission, and contain a chromosome of DNA but no nucleus. The DNA is condensed into nucleoids. Bacteria are widely distributed in nature, but some are pathogenic Fungi: single-celled eukaryotes that exist as yeasts or filaments or both which cause cutaneous, mucosal and systemic mycoses. Yeasts bud or divide, whereas filaments (hyphae) have cross walls or septa. Systemic infections with fungi often affect immuno-comprimised people. Protozoa: unicellular, free-living, non-photosynthetic, motile eukaryotic organisms which include intestinal, blood and tissue parasites which acquired by ingestion or through a vector. They replicate in the host by binary fission or by formation of trophosoites inside a cell, and often have complex life cycles involving two hosts. Helminth parasites: Multicellular eukaryotes of the Kingdom of Metazoa, which are visible to the naked eye and have life cycles outside of the human host. 2. Give examples of the agent and the disease it causes Viruses: SARS, Influenza and HIV (use of reverse transcriptase breaks DNA makes RNA makes protein rule) Bacteria: Neisseria meningitis, mycobacterium tuberculosis, shigellosis (shigella spp. Is an invasive pathogenresponsible for 50% of deaths from diarrhoeal disease) and septicaemia (characterised by rapid progression, septic shock, severe inflammatory response) Protozoa: malaria (plasmodium spp.- vector is female anophelese mosquito which targets red blood cells) and leishmania spp. (vector is sand fly- targets white blood cells) Helminth parasites: tapeworms, flukes and roundworms 5 MCD Cells Alexandra Burke-Smith 3. List the differences between prokaryotic and eukaryotic cells Prokaryotes (Monera and Archaea ) No organelles No nucleus- but rather a condensation of DNA called a nucleoid Have external whip-like flagella for locomotion or hair-like pili for adhesion Simpler, smaller, haploid Cell walls contain PEPTIDO-GLYCAN Shapes: cocci (round), bacilli (rods), and spirilla or spirochetes (helical cells). Eukaryotes Membrane-bound organelles Nucleus May have cilia or microvilli on surface of cell membrane Cytoskeleton No cell wall- only cell membrane 6 MCD Cells Alexandra Burke-Smith 3. Cell Membranes Professor Michael Ferenczi (m.ferenczi@imperial.ac.uk) 1. Explain the formation of phospholipid bilayers in an aqueous environment. Structure of the plasma membrane In an aqueous environment, phospholipids form micelles/droplets (droplets in cells are known as liposomes) or bilayers in which their hydrophobic tails pack together to avoid water Phospholipids are amphipathic- they have a polar/hydrophilic phosphate head with hydrophobic aliphatic fatty acid chains which may be saturated or unsaturated Unsaturated hydrocarbon chains have cis-double bonds, forming a kink in the fatty acid chains. Fully saturated chains have no kinks and can be packed more densely. The fractions of saturated and unsaturated fatty acids therefore affects the rigidity/fluidity of the membrane Common constituents are phosphatidylethanolamine, phosphatidylserine, sphingomuelin and phosphotidylcholine (also known as lethicin) Membranes also contain cholesterol which increases the membrane rigidity. It has a polar head (containing a hydroxyl group) and a rigid planar steroid ring structure. The membrane is asymmetric as glycolipids (lipids with carbohydrates attached) are on the extracellular side of the membrane with negative charges on the inside of the cell. The phospholipids rarely “flip-flop” (change sides of the membrane), as this requires too much energy for the hydrophilic head to pass through the hydrophobic core, but they rapidly undergo lateral diffusion within the monolayer- moving around the distance of 1 large bacterial cell (2 micrometres) per second Properties of the membrane Selectively permeable Impermeable to macromolecules, biochemical intermediates. Permeable to water molecules and a few other small, uncharged molecules like oxygen and carbon dioxide, nutrients, waste products. Transfer of information (signal transduction). 2. Draw the structure of phosphatidylcholine and identify the component parts. 7 MCD Cells Alexandra Burke-Smith 3. Describe the permeability properties of a phospholipid bilayer with respect to macromolecules, ions, water and organic compounds (including drugs). Distinguish simple diffusion, facilitated diffusion and active transport of ions and molecules across cell membranes. Lipid bilayers are permeable to... Water Some small uncharged molecules like oxygen and carbon dioxide The lipid bilayer is more fluid than predicted, as it is coated in components giving water-absorbing properties so less energy is required for the movement of substances across and within the membrane Simple Diffusion: the movement of molecules and small particles across the semi-permeable membrane driven by a difference in the concentration of molecules on either side. Osmosis: the net movement of water molecules across a semi-permeable membrane driven by a difference in concentration of solute on either side. The membrane must be permeable to water but not to the solute molecules Active Transport: the movement of a molecule across a membrane against its concentration gradient driven by ATP hydrolysis or another form of metabolic energy Facilitated diffusion: the movement of hydrophilic (charged) molecules down their concentration gradient through protein pores that hide the ionic charges from the hydrophobic core of the lipid bilayer. Proteins (or protein assemblies) offer a water-filled channel. The channel can be ‘gated’- specific, i.e. a particular molecule may modify its structure, opening the channel allowing the substance to pass through the membrane e.g. drugs. Lipid bilayers are impermeable to... Cations (K+, Na+, Ca2+) but some do leak through, down the concetration gradient. Anions (Cl-, HCO3-) Small hydrophilic molecules like glucose Macromolecules like proteins and RNA 4. Categorise the functions of membrane proteins. Definition of a membrane protein: a protein associated with a lipid bilayer; can either be integral (transmembrane, monolayer-associated, or lipid-linked) or peripheral. Definition of a membrane transport protein: any protein embedded in a membrane that serves as a carrier of ions or small molecules from one side to the other Membrane Proteins Cell membranes and organelle membranes contain proteins, conferring new properties to the membrane. They increase the fluidity of the membrane, as their position is not fixed and they diffuse in the plane of the membrane Protein composition is different in the inner and outer leaflets of the bilayer. In the core, the proteins have a predominantly α-helical structure as they cross the lipid bilayer- as result of an orientation relating to their functions Protein composition is dependent on the cell/organelle type, i.e. myelin sheath has a lower protein percentage composition, making it more rigid and a better insulator which makes it more suited to its function Proteins (or protein assemblies) offer a water-filled channel. The channel can be ‘gated’- these specialised pores provide a route for hydrophilic substances to move across the membrane down their concentration gradient. This is known as protein mediated permeability. 8 MCD Cells Alexandra Burke-Smith Functions of the Proteins Transport (Sodium-Glucose transport) Transmission of signals Anchors to link intracellular actin filaments to extracellular matrix proteins (anchors the membrane to macromolecules on either side) Receptors for hormones and growth factors- detect chemical signals in the cell’s environment, and relay them to the cells interior Cell recognition and adhesion Electron carriers in cellular respiration and photosynthesis in mitochondria and chloroplasts Enzymes 5. Explain the movement of Na+ and K+ ions across the cell membrane against a concentration gradient and the consequences of failure of such a movement. Membrane Potential Membrane potential: voltage difference across a membrane due to a slight excess of positive charge on one side and of negative ions on the other. A typical membrane potential for an animal cell plasma membrane is -80mV (inside negative), measured relative to the surrounding fluid. The Sodium-Potassium Pump Electrostatic force due to the charge separation across the membrane tends to move ions in a direction determined by its particular charge The high concentration of fixed anions inside cells (the proteins) and their accompanying cations (e.g. chloride ions) means that water is drawn into the cells by the resulting osmotic gradient. The high concentration of Na+ in the extracellular space means that Na+ will tend to move down its concentration gradient into the cell. The sodium-potassium pump (Na+-K+ ATPase) maintains the osmotic balance and stabilises the cell volume by transporting 2K+ into the cell in exchange for 3Na+. This is electrogenic (unequal transfer of charge) therefore requires energy. It also provides a diffusion gradient for chloride ions. The chloride ions tend to move inward down their concentration gradient, but excess negative charge inside the cell (from nondiffusible proteins, lipids, and the unequal distribution of positive charge of K+ and Na+) tend to push Cl- ions back out of the cell. The sodium-potassium pump consists of two polypeptide chains, alpha and beta, with 1000 and 300 amino acids respectively. The alpha-chain spans the membrane 10 times, forming a hydrophilic pore. The K+ Na+ exchange is mediated by a series of conformational transitions of the pump molecule, which is driven by phosphorylation of an aspartyl residue followed by hydrolysis of aspartylphosphate. There are two consequences: Ionic gradients are created: less Na+ and more K+ inside the cell than outside. A charge gradient is also created, which results in the inside of the cell being at a more negative potential than the outside. The potassium channel consists of four subunits and is highly specific for K+, as it mimics the environment potassium is usually surrounded by. The high concentration of potassium inside the cell means there is a tendency to move out of the cell, but this would accentuate the voltage difference across the cell (making it more negative), therefore an equilibrium is reached when the rate of inward movement = rate of outward movement. 9 MCD Cells Alexandra Burke-Smith This equilibrium does not fully compensate for the electrogenic sodium-potassium pump, therefore the membrane potential of a nerve or muscle cell at rest is about -80mV. The Nernst equation describes how the distribution of ions leads to a membrane potential Action potentials occur in elongated cells (nerves, muscle) when the membrane potential is disrupted by a brief pulse of current which cause a massive influx of Na+ in the cell (depolarisation), which must then use metabolic energy to reinstate the membrane potential. Na+ channels become inactivated locally, preventing further Na+ entry. Voltage-gated K+ channels open, to restore the resting membrane potential. The process propagates down the nerve/muscle Specific ion pumps There are specific pumps for Na+, Ca2+ and H+, which use ATP hydrolysis to provide the energy. Some pumps can work in reverse and generate ATP from an ion gradient, e.g. the F1-ATPase in mitochondria. Other mechanisms exist for other substances that need to cross the membrane 6. Explain how the entry of glucose and amino acids into the cell against a concentration gradient is coupled to ATP dependent Na+ transport. Glucose transport Glucose is membrane-impermeant. Glucose moves down the concentration gradient into the cell Glucose binds to a specific glucose transporter which functions by a flip-flop mechanism The transport is ‘facilitated’. Several different proteins. Some are insulin-sensitive Amino acids Uses coupled transporters- symporters and antiporters Move in the opposite direction to Na+ using ATP hydrolysis Other transport mechanisms: Pinocytosis: engulfment by the membrane of extracellular solute and small molecules which end up in small intracellular membrane-bound vesicles. Phagocytosis: engulfment by the membrane of extracellular objects such as bacteria, cell debris, other cells. Again these end up in intracellular membrane-bound vesicles. Exocytosis: movement of proteins and other molecules (e.g. hormones, blood clotting factors) from intracellular vesicles towards the extracellular space by fusion with the cell membrane. 7. Explain how external chemical signals can be sensed at the interior of a cell. It is not only substances that need to cross membranes. Signals need to cross membranes too. Some use exocytosis, e.g. hormones. Others use lipid-soluble molecules that cross membranes. But other signals rely on trans-membrane receptors. 8. Be able to calculate the membrane potential from the Nernst equation Ex V = RT [ X ]o ln zF [ X ]i Where E is the membrane potential in V R = Gas constant, 8.135 J K-1 mol-1 F = Faraday‟s constant, 9.684 x 104 C mol-1 10 MCD Cells Alexandra Burke-Smith T = absolute temperature, -273 °C, At 25°C, T=298 Z = valence of the ion, 1 for Na+ 9. Understand the role of membranes in synaptic transmission, using the neuromuscular junction as an example The Neuromuscular junction The Neuromuscular junction or synapse is a highly complex structure involving pre- and post-synaptic membranes, pre-synaptic vesicles, invagination of the post-synaptic membrane, receptors and enzymes. Depolarisation of the muscular post-synaptic membrane results in a propagated action potential. The wave of depolarization extends into the t-tubules (invaginations of the cell membrane) to transmit the activation signal into the core of each muscle cell in the motor unit. Close contact with the sarcoplasmic membrane via triadic junctions involving the dihydropyridine (t-tubule membrane) and ryanodine receptors (sarcoplasmic reticulum membrane) results in calcium release from the sarcoplasmic reticulum. Calcium diffusion into the myofilaments lattice and calcium binding the troponin on the thin filaments (actin) in skeletal and cardiac muscle result in activation of the contractile machinery and contraction. A2 NOTES (neuromuscular junctions and muscle contraction) A neuromuscular junction is the point where a motor neurone meets a skeletal muscle fibre. As rapid muscle contraction is frequently essential for survival there are many neuromuscular junctions spread throughout the muscle. This ensures that contraction of muscle is rapid and powerful when simultaneously stimulated by action potentials. All muscle fibres supplied by a single motor neurone act together as a single functional unit, known as a motor unit. 1. When a nerve impulse is received at the neuromuscular junction, the synaptic vesicles fuse with the presynaptic membrane and release acetylcholine 2. The acetylcholine diffuses to the post-synaptic membrane, altering its permeability to sodium ions, depolarising the membrane 3. The acetylcholine is broken down by acetylcholinesterase to ensure that the muscle is not over-stimulated 4. The resulting choline and ethanoic acid diffuse back into the neurone, where they are recombined to form acetylcholine using energy Muscle stimulation An action potential reaches many neuromuscular junctions simultaneously, causing calcium ion channels to open and calcium ions to move into the synaptic knob Calcium ions cause the synaptic vesicles to fuse with the pre-synaptic membrane and release their acetylcholine Acetylcholine diffuses across the synaptic cleft and binds with receptors on the post-synaptic membrane, causing it to depolarise. Muscle contraction The action potential travels deep into the fibre through T-tubules that branch throughout the sarcoplasm The tubules are in contact with the sarcoplasmic reticulum, which has actively absorbed calcium ions from the sarcoplasm The action potential opens the calcium ion channels on the sarcoplasmic reticulum, flooding into the sarcoplasm down a diffusion gradient The calcium ions cause Troponin molecules to change shape, which causes the Tropomyosin molecules to pull away from the actin binding sites The ADP molecule attached to the myosin heads bind to the actin filament and form a cross-bridge The myosin heads then change their angle, pulling the actin filament along and releasing a molecule of ADP An ATP molecule attaches to each myosin head, causing it to become detached 11 MCD Cells Alexandra Burke-Smith The calcium ions then activate the enzyme ATPase, which hydrolyses ATP to ADP, providing the energy needed for the myosin head to return to its original position The myosin head with ADP then re-attaches itself further along the actin filament and the cycle is repeated as long as nervous stimulation continue 12 MCD Cells Alexandra Burke-Smith 4. Blood and Blood Cells Dr Michael Emerson (m.emerson@imperial.ac.uk) 1. List the main functions of the blood Connective tissue Transport (connects every part of body) Heat distribution Immunity Haemostasis (process whereby bleeding stops) Support (e.g. external genitalia - VIAGRA) MAINTAIN HOMEOSTASIS (constant internal environment) Blood volume (5l male; 3.5l female) How blood serves cells Acts as a transport medium which carries the products of digestion e.g. fatty acids, amino acids and glucose, hormones, vitamins and oxygen to their target cells Removes metabolic waste e.g. lactic acid and urea, carbon dioxide, excess heat and water from cells so that they can be removed from the body 2. List the major components of blood Erythrocytes- red blood cells Leukocytes- white blood cells Platelets- derived from megakaryocytes in bone marrow; involved in coagulation and clot formation Plasma- fluid component of blood which acts as the carrier for all blood cells 3. Describe the essential features of the erythrocyte and list its major functions Primary function: respiratory transport. Binds with oxygen to form oxyhaemoglobin for transport to cells. Binds with carbon dioxide to form bicarbonate from carbonic anhydrase for removal from cells. Biconcave disc maximises surface area for diffusion of oxygen No nuclei or organelles Packed with haemoglobin 7.5micrometres and flexible, important as able to penetrate through to smallest vessels Molecules on the surface confer blood group Regulation of erythrocytes Erythrocytes are regulated by the kidney in a negative feedback loop. 1. Low oxygen 2. kidney (+testosterone- hence higher levels of erythrocytes in men) produces erythropoietin (hormone) 3. bone marrow stem cells differentiate to form erythrocytes (erythropoiesis) blood 4. haemoglobin increases 5. blood oxygen increases 6. negative feedback- back to the beginning Life Cycle of erythrocytes Produced in bone marrow from precursors which produce haemoglobin then lose organelles Immature erythrocytes contain ribosomes: reticulocytes. High levels of circulating reticulocytes are useful in diagnostics e.g. anaemia, chemotherapy 13 MCD Cells Alexandra Burke-Smith Removed through reticulo-endothelial system (phagocytic macrophages in spleen) Lifespan = 120 days (short, no nuclei; 1% or 250 billion cells per day) Dependent on dietary iron (meat, egg yolk, nuts), iron deficiency causes anaemia 4. Explain the importance, basic structure and role of haemoglobin Globular protein consitisting of 4 subunits (polypeptide chains), each with a prosthetic haem group. Haem contains a ferrous iron (FE2+), each of which binds with one molecule of oxygen Hb = deoxyghaemoglobin. Hb02 = oxyhaemoglobin 100ml blood: 15.8g (male) 13.7g (female) Due to the compact conformational shape of globin molecules, haemoglobin has a low affinity for oxygen However, oxygen binding breaks the conformation and opens up the structure, allowing the second oxygen molecule to bind more easily This means in a high oxygen environment (e.g. the lungs), cooperative binding can take place which allows more oxygen to be carried Different form in foetus with higher O2 affinity, as foetus must obtain oxygen from mother’s blood Carbon monoxide combines with haem at a 200X greater affinity to form carboxyhaemoglobin, reducing oxygen binding, which can deprive cells of oxygen resulting in cell death. Key red cell Parameters Concentrations of haemoglobin (g/dl)- men: 13.5-16.5, women: 11.5-14.5 Red cell count- men 5.4x1012/l, women 4.8x1012/l Haematocrit (packed cell volume PCV): men 0.40-0.54/1.00, women 0.35-0.47/1.00 PCV is the proportion of blood which are erythrocytes Normal MCV (mean cell volume) 82-99fl Normal MCH (mean cell haemoglobin) 27-33pg Normal MCHC (mean cell haemoglobin concentration) 32-34 g/dl 5. Define anaemia and list the major causes and subclasses and relate the types of anaemia to red blood cell volume Definition of anaemia: low blood haemoglobin concentration Three main types: Microcytic (small MCV): Failure of haemoglobin synthesis (and hence smaller erythrocytes) caused by an iron deficiency as a result of gradual blood loss e.g. menstruation, GIT lesions or cancers and parasitic infection Normocytic: red blood cell production is normal, but is a result of acute blood loss Macrocytic (large MCV): During erythropoeisis, DNA synthesis and cell division fail and reduced division of progenitor cells so fewer but larger erythrocytes. Folic acid and vitamin B12 are essential for division. Caused by pregnancy (lack of folic acid), autoimmune disease, pernicious anaemia (destroys uptake of B12 in gut), and in vegetarians and vegans- all caused by lack of vitamin B12. 14 MCD Cells Alexandra Burke-Smith Sickle Cell Anaemia Haemoglobin point mutation Causes distorted erythrocytes, which are destroyed by macrophages in the spleen, resulting in anaemia. Homozygous Genotype- disease manifests. Heterozygous Genotype- sickle cell trait, partial malarial resistance. Polycythemia Excess erythrocytes, high PCV (haematocrit) Common problem living at high altitude Increased viscosity of blood leads to heart problems. 6. Explain simply the major functions of leukocytes and explain simply the concepts of immune responses and passive immunity Leukocytes 1. White blood cells Use circulation for transport Travel near capillary wall and invade tissue space to fight infection Classified by structure and dye binding (you can see the granules and nucleus) Main Types: Polymorphic granulocytes: Segmented nucleus, full of cytoplasmic granules. First on scene - adhere to blood vessels in infected area and migrate into tissue. Engulf, kill and digest microorganisms. Main types are neutrophils (phagocytic), eosinophils (allergic + asthma responses), basophils (histamine-producing). Release inflammatory mediators: toxic oxygen products, digestive enzymes, vasodilators, chemotaxins. 2. B- Lymphocytes: Mature in bone marrow- involved in Humoral (antibody-mediated) immunity. Foreign antigen → RNA synthesis → immunoglobulin (antibody) production. Immunoglobulins: IgM; IgG; IgA; IgD; IgE. Antibody-antigen reactions: assist phagocytosis by precipitation; agglutination (clumping) or coating in antibody (opsonisation) or prevent attachment of micro-organism to tissues (neutralisation). In the primary immune response, it is the first exposure, so antibodies appear after latent period, peak then fall. The Secondary response will be greater, quicker, longer response due to memory cells (long lived Blymphocytes). Passive immunity: inject immunoglobulins (vaccine) or cross placenta (colostrum in some species) 3. T- Lymphocytes: Derived in bone marrow, but migrate to thymus where they aquire surface antigenic molecules and become immunologically competent. Involved in cellular immunity: Circulate → foreign antigen → blast transformation (rapid cloning) → with receptors for antigen. Activated T-lymphocytes release chemotaxins (attract macrophages); lymphotoxin (kills cells); interferon (kills viruses). Subgroups: Cytotoxic T-cells, helper T-cells, Supressor T-cells (no info required) 4. Monocytes: Large, single horse-shoe nucleus. Appear after granulocytes and in tissue become macrophages (“big eaters”), engulfing micro-organisms, tissue debris and dead polymorphs. Secrete inflammatory mediators and stimulate angiogenesis (vessel growth = repair). Ingest and store antigens, present modifies antigen to lymphocytes 15 MCD Cells Alexandra Burke-Smith Normal Leukocyte count Total = 3.5-10.0x109/L Neutrophils 2.5-7.5 (40-75%) Eosinophils 0.04-0.4 (1-6%) Basophils 0.01-0.1 (<1%) Monocytes 0.2-0.8 (2-10%) Lymphocytes 1.5-4.0 (20-25%) Leukocytosis = raised leukocytes due to infection, cancer etc. Leukopenis = low leukocytes due to chemotherapy, HIV etc 7. Explain simply the major functions of platelets Derived from megakaryocytes 2 - 3 µm diameter (small) Normal platelet count 25 x 104/ml Life span 8 - 10 days Granules Many organelles, no nucleus Haemostasis Express surface receptors for platelet activators in the presence of collagen in vessels or thrombin from coagulation cascade They adhere to exposed collagen (in wound or atherosclerosis), and release granules which promotes platelet aggregation Coagulation cascade- Produce thromboxane A2 from cycloxygenase enzyme, which is involved in clot/thrombus formation Aspirin inhibits cycloxygenase and is therefore anti-clotting. The vascular endothelium also produces prostacyclin and nitric oxide which inhibit platelet activation. 8. List the major functions of plasma Fluid component of blood, acts as transport carrier “Organic and inorganic substances dissolved in water” Water and proteins Plasma proteins: exert osmotic pressure to maintain blood volume. Albumins + globulins are carrier molecules e.g. hormones, bile salts, water insoluble drugs. Fibrinogen is present for clotting. If the balance of proteins is changed, can lead to blood pressure and kidney function problems Serum: plasma with proteins removed due to clotting Key components Nutrients Hormones Proteins Inorganic ions Products of metabolism Glucose, Lipids, Amino acids Thyroxine, Cortisol, Erythropoietin Clotting factors, Albumin, Globulins Na, K, Ca, PO4, HCO3 Urea, Lactic acid 16