Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
Health Communication
in the Latino Community:
Issues and Approaches
John P. Elder,1 Guadalupe X. Ayala,1
Deborah Parra-Medina,2 and Gregory A. Talavera1
1
Graduate School of Public Health, San Diego State University, San Diego, California
92123; email: jelder@mail.sdsu.edu, ayala@mail.sdsu.edu, gtalaver@mail.sdsu.edu
2
Institute for Health Promotion Research, Department of Epidemiology and Biostatistics
School of Medicine, University of Texas Health Science Center, San Antonio, Texas, 78230;
email: parramedina@uthscsa.edu
Annu. Rev. Public Health 2009. 30:227–51
Key Words
First published online as a Review in Advance on
January 15, 2009
Latinos, Hispanics, Hispanic Health Paradox, communicationpersuasion model, acculturation
The Annual Review of Public Health is online at
publhealth.annualreviews.org
This article’s doi:
10.1146/annurev.publhealth.031308.100300
c 2009 by Annual Reviews.
Copyright All rights reserved
0163-7525/09/0421-0227$20.00
Abstract
With reference to the Communication-Persuasion model, we describe
various research issues and challenges when considering the health of
Latinos, and implications for designing and evaluating health communication and behavior change efforts in this population. Latinos, collectively the nation’s largest minority group, vary substantially in terms of
socioeconomic and legal status, their country of origin and the extent of
ongoing contact with that country, their region of residence within the
United States, their generation status and levels of acculturation, and
psychosocial factors. Health communication efforts with Latinos need
to focus on family, cultural traditions, and collectivism while attending
to acculturation, language, generation and national origin. The most
extensive intervention topic in Latino health promotion has been the
application of the lay health advisor model. This and other fundamental
communication approaches, as well as audience and population characteristics, need to be considered within the context of dynamic and
complex societal changes.
227
ANRV370-PU30-13
ARI
15 February 2009
12:38
PART I: LATINOS IN THE
UNITED STATES
Many national health and social science studies,
including the National Health Interview Survey (NHIS) and other surveys, treat Latinos1 as
though they were a homogenous group. However, as Modiano and colleagues (75) stated,
The aggregation of culturally distinct subgroups, which have resided in the United
States for different periods of time, into a
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
more inclusive Latino category assumes that
all persons of Mexican, Cuban and Puerto
Rican origin have similar needs and experience similar barriers in using health services.
There is, however, no clear evidence for this
assumption. On the contrary, there is evidence
that each group has specific characteristics that
make it different and independent from one
another. . . . (p. 35)
Clearly, extraordinary diversity exists among
subgroups of Latinos. The immigration and acculturation experiences of Mexican or Central
American–descended Americans, South Americans, Puerto Ricans, and Cuban Americans vary
substantially from one another. The distinction
among Latino subgroups can be traced back to
highly varied experiences not only with respect
to encounters with the dominant American culture but also extending back to Spanish colonization, which began to redefine the western
hemisphere 500 years ago. Indigenous groups
in the Caribbean Islands and coastal areas
largely succumbed to Iberian diseases and aggression and were replaced by Europeans and
African slaves. Although forced to adopt much
of the culture and religion of the conquistadores, indigenous groups in central and highland areas of Mexico and further south survived
1
The field offers no consensus regarding the term to refer to
persons of Latin American heritage who live in the United
States. Both “Hispanic” and “Latino” are used extensively, although U.S. government documents, including the Census,
use the term Hispanic. Given this mixed usage in the literature, we use the term Latino to indicate, where possible, the
specific ethnic group in question.
228
Elder et al.
to a great extent. Thus, the blends of European,
African, and indigenous cultures find different
expressions in the many regions and communities of Latin America.
The historical and political interface of the
various Latin American countries and regions
with the United States also manifests distinctive paths. The long, shared border between
the United States and Mexico among populations in the southwestern states presents more
opportunity for Mexican immigrants to travel
back and forth to their Mexican homeland. A
large proportion of Mexican-derived inhabitants of Texas and New Mexico can still trace
their roots to this region following its annexation by the United States, which led to the war
between the United States and Mexico (1846–
1848). Puerto Rico has been part of the United
States since the defeat of Spain in the SpanishAmerican War in 1898, and present-day inhabitants of this island are American citizens. Many
Cuban Americans trace their migration to the
United States to the more recent conflict between the American government and Cuba under Fidel Castro, a major element of the Cold
War and one of its last vestiges. Cuban migration peaked in 1994. The history of Latino migration into the United States is diverse and, in
many ways, brief. More importantly, the population is growing. Heightened immigration
from Mexico and Central and South America along with positive birth outcomes among
native-born Latinos is transforming the demographic and economic landscape of the United
States dramatically. Over the past 30 years,
the Latino population has grown more rapidly
(337%) than the total U.S. population (41.9%)
and accounted for 39% of the net population
growth in the United States (108). In general,
Latino households are larger and younger than
non-Latino households in the United States,
which suggests that the population growth is
likely to continue (108).
Socioeconomic Realities
Upon arrival in this country, Latino immigrants
encounter vastly different socioeconomic
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
realities, some realizing middle-class status
fairly quickly, others finding themselves indefinitely at the lowest rung. These experiences
may be a function of the structure of their
home countries’ educational system, as well
as whether the immigrant is of European,
African, or indigenous native ancestry. From a
U.S. educational system perspective, Mexicans
are disadvantaged before they arrive because
fewer individuals have access to a secondary
education compared with the opportunities
to complete high school in the United States.
Access to education, in turn, affects literacy
levels. Along with Puerto Ricans and Central
Americans, most Mexican immigrants to the
United States end up as unskilled laborers
(109). However, the premigration middle- or
upper-class status of the first and largest wave
of 1960-era Cuban immigrants contributed
in part to their relatively strong economic
status as Cubans living in the United States.
Seventy-four percent of Cuban Americans
have graduated from high school, whereas
50% of Mexican Americans and 67% of Puerto
Ricans have graduated from high school
(90). Moreover, nearly one-fourth of Cuban
Americans have graduated from college, which
is identical to the college graduation rate
of the general U.S. population. In contrast,
Mexican- and Puerto Rican–origin adults
have lower college graduation rates (7%
and 11%, respectively). Despite educational
disadvantages, recent unemployment figures
for Latinos are relatively favorable, although
this appears to vary by generation status. Firstand third-generation Latinos have approximately the same employment-to-population
ratio, both substantially higher than that of
second-generation Latinos. According to the
Pew Hispanic Research Center (87), age,
geographic mobility, and family networks
as sources of employment information all
contribute to the relatively better employment
picture for foreign-born Latinos, even though
wages lag behind those of white or African
American workers. The variation observed
among Latino subgroups is arguably as great as
that which has existed among other American
subgroups, well before Latinos became the
largest American “minority.” The economic
gains recently enjoyed by Latinos are threatened by low Latino educational achievement
levels.
Regional Issues
Economic, societal, and psychosocial factors
are in dynamic flux in Latino communities
and, singly or in combination, may have an
important impact on Latino health. Johnson
et al. (49) proposed a classification system for
understanding the diverse Latino communities
in the United States that is based on the region’s
migration history and which seems to have implications for health-promotion efforts. Mature
markets include traditional immigrant gateway
states, the largest markets being California,
Arizona, Texas, Illinois, New York, and Florida.
Emerging markets are states with little to no
Latino migration prior to 1990 such as Georgia, Nevada, North Carolina, and Washington.
Incipient markets are growing rapidly and
needs are changing (Iowa, Mississippi, Rhode
Island, South Dakota). The long history of
immigration into mature markets has created
established communities that share a common
language (Spanish) and culture (Mexican in
California and Cuban in Florida), thereby
reducing language and cultural barriers when
accessing health care services, for example.
Mature markets are also multigenerational, as
reflected in the proportion of households with
extended family members as compared with
the non-Latino population (14% versus 7.5%)
(108). Thus, diverse sources of support and
influence exist in these social environments.
However, emerging and incipient markets are
dominated by young adult males, many with
wives and children in their home countries.
These immigrant males demonstrate strong
participation in the work force, with the
construction industry accounting for more
than half of new Latino jobs (56). However,
community and organizational needs change
as the families of these men join them in the
United States and begin to access health and
www.annualreviews.org • Latino Community Health
229
ARI
15 February 2009
12:38
education-related services, thus increasing
the demand for culturally competent services
in environments with limited resources and
capacity to provide them. Most public health
research emerges from Latino populations in
mature markets. A small but growing body of
research is available on public health interventions in emerging and incipient markets.
Given these differences, programs developed
for Latino populations in mature markets
may not be directly transferable to Latino
populations in other markets. These market
characteristics have implications for our approach to intervention research. One area in
which we have explored this issue is in the use
of the promotor model (see Communities and
Promotores, below).
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
Generation Status, Identity,
and Language
First- and second-generation Latinos vary substantially on their national identity. A small
percentage of first-generation Latinos use the
self-descriptor “American,” whereas more than
one-third of second-generation Latinos do
so. One-fourth of both first- and secondgeneration Latinos use “Latino” or “Hispanic”
as their primary term of self-identification.
Twice as many third-generation as secondgeneration Latinos use “American” as at least
part of their self-identity. The Pew Hispanic
Center has studied important generational differences in demographics, identity, attitudes,
and experiences. For example, first-generation
Latinos are more socially conservative, as evidenced by their attitudes toward divorce, abortion, and other social issues, which affects both
the context and the content of health messages.
The Pew Hispanic Center employs the term
Generation 1.5 to identify a phenomenon typical of many Latino immigrants. These immigrants may be categorized as having arrived
in the United States by age 10. Therefore, although they are foreign born and may plan to
return to their country of origin eventually, they
may be more similar to second-generation than
to first-generation immigrant Latinos because
230
Elder et al.
most of their formative experiences are likely to
have taken place in the United States (87).
The Pew Hispanic Center (87) also presented findings on bilingualism among Latinos
in the United States. The 2000 census showed
that the number of Latinos speaking Spanish
at home rose from ∼10.2 million in 1980 to
24.7 million in 2000. Spanish is thus becoming
an increasingly common language among U.S.
Latino households. Despite the large proportion of immigrant and native-born Latinos in
the United States, language evolution among
the Latino generations is largely similar to that
reported for other ethnic groups who have immigrated to the United States. A small percentage of second-generation Latinos speak mostly
Spanish. By the third generation, knowledge
of Spanish effectively becomes extinct. In addition, English remains the dominant language
of the United States in terms of commerce and
trade and dominates U.S. workplaces.
Language use drives the degree to which individuals are acculturated to American society,
which may influence not only how well they
respond to our behavior change initiatives but
also their selection and use of media, in general. Acculturation may be defined as a process
through which an individual’s attitudes and behaviors shift from those of his or her culture
of origin toward those of the dominant culture.
Changes that occur in attitudes, norms, and values of individuals exposed to a new culture are
an important part of this process (14) and may
provide insight into the relationship between
acculturation and health-related behaviors (60).
Addressing Health Disparities
The Healthy People 2010 objectives call for the
elimination of health disparities among racial,
ethnic, and other subgroups of the American
population (55, 110). Latino communities evidence some of the worst of these disparities (54),
being challenged not only by chronic diseases,
sexually transmitted diseases, tuberculosis, cirrhosis, and exposure to particulate matter but
also by an even wider range of health risks and
illnesses.
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
Health disparities are the product of
complex and only partly understood genetic,
biological, psychosocial, and economic factors,
compounded by discrimination and inequality
(17, 58, 96, 118). Perceptions of stigmatization
and discrimination from the community at
large and from the health care system are
frequently reported by Latinos (17, 95).
The impact of discrimination against Latino
immigrants may be compounded by language,
legal status, and other bases for bias, further
exacerbating their impact and resulting in
considerably higher levels of stress among
minorities than among whites (58). Even for
second-generation Latinos, the process of
marginalization, disempowerment, and social
exclusion known as “othering” (43, 114) may
perpetuate the negative impact of discrimination beyond the immigration experience.
Language use appears to have an impact on
the degree of disadvantage. Bilingual Latinos
have high-school graduation rates that are more
than twice that of Spanish-speaking Latino
adults. Given that English speakers are prized
more greatly in the workplace, they also enjoy higher household incomes than do Spanish speakers. Bilingual adults have incomes
roughly equal to their English-only counterparts in terms of economic advancement
(87).
In spite of socioeconomic challenges and a
variety of disparities, Latinos, individuals and
communities, evidence several positive health
outcomes, a phenomenon that continues to interest and challenge epidemiologists and social scientists. Relative to non-Hispanic whites,
Latinos have a worse socioeconomic profile and
less access to health care, but they have lower
mortality and morbidity rates in crucial areas
e.g., low birth weight (40). In terms of specific
chronic disease-related risk factors, for example, Latinos have been reported to have higher
rates of obesity, elevated blood pressure, and
serum lipids (62). Yet even with these risk factors, studies have demonstrated lower rates of
both coronary heart disease (CHD) and total
cardiovascular disease (CVD) (74). This epidemiological phenomenon has been labeled the
Hispanic Health Paradox (39, 69, 84). Census
undercounts, the healthy migrant hypothesis
(healthier individuals self-select to migrate to
the United States), and the salmon hypothesis (elderly immigrants or those with severe illnesses return to their native country to spend
their last days) can partially (25) but not fully (2,
77) explain this paradox. Other studies have not
found Latino ethnicity to serve as a protective
factor (47), in part because of socioeconomic
differences between whites and Latinos of Mexican origin (25) and the weaker relationship
between educational level and health among
Latino subgroups other than Puerto Ricans
(42, 107).
A Framework for Latino Health
Promotion through Communication
The primary themes and findings of sociodemographic, cultural, and psychological influences on Latino health are summarized in
Table 1. The individuals and subgroups in the
United States collectively labeled “Hispanics”
or “Latinos” comprise the largest minority in
the country. Nevertheless, the variations within
this group are nearly as great as those between
them and whites/Anglos or other subgroups.
Latinos vary greatly with respect to national
background and experience with immigration,
their past and current socioeconomic status, the
nature of the community in which they live
and their status within it, and acculturation and
other cultural factors. In complex and sometimes indirect ways, these factors protect or adversely impact health and contribute to narrowing or widening the Latino health disparities
gap.
The growth of the Latino population in the
United States, with the social and economic
inequities they experience, demands continued attention to their health care needs. Given
the complexities identified, a framework for
targeting improvements in Latino health is
needed. Using a theoretically based model of
communication, the second part of this article presents a framework for promoting Latino
health through families and communities.
www.annualreviews.org • Latino Community Health
231
ANRV370-PU30-13
Table 1
ARI
15 February 2009
12:38
Sociocultural health related issues by type of Latino community
Sociocultural
health-related issues
Diverse or white/Anglo
communities
Economic status of
Latino residents
Entire range
Accessing resources
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
Acculturation and
language
Assimilated, English
speaking
Gender and family
norms
Dominant Latino communities
Middle to high
socioeconomic
status
Low to middle
socioeconomic
status
Marginalized, minority
Latino communities
Low to middle
socioeconomic status
May still require
culturally sensitive
care
Need to reduce both
cultural and financial
barriers
Need a bridge
Bicultural or oriented
toward Latino
subculture of region;
Spanish-dominant or
bilingual
Less acculturated to
larger society;
Spanish-dominant
Unacculturated and
isolated; Spanish only
except for work-related
English
Shifting;
egalitarianism
Changing; conflict
Traditional
Community
characteristics
Communities
accustomed to or
unaware of diversity;
Latinos may sense little
discrimination but may
have sense of othering
Busy communities;
juggling cultural
transitions within
family; share
stressors of dominant
U.S. community but
may experience
othering
Reluctant
communities;
concerned about
what they have to
invest for return;
potential experiences
of racism or
discrimination
Hidden communities;
reluctant to disclose too
much information;
vulnerable to
discrimination and
economic exploitation
Country of origin or
background
Some but limited
influence
More frequent contact
with and ability to
travel to native
country
More frequent
contact with but
limited ability to
travel to native
country
Desire to have frequent
contact with sending
country; may be severely
limited by finances or
legal status. May be
separated from nuclear
family.
PART 2: COMMUNICATION AND
HEALTH BEHAVIOR CHANGE
Although the broader sociodemographic, cultural, and economic variables described above
are causally related to or at least correlated with
Latino health, many are not easily amenable
to change. Immigrants are not sent back to
their native countries or enrolled in American community colleges until they receive more
education, nor are they told which U.S. city
or neighborhood would be best for them to
reside in. Second-generation adolescents and
young adults can be forced neither to reject
nor to maintain their parents’ language and culture. There are few shortcuts to upward so-
232
Elder et al.
cial mobility and sometimes few means to make
any progress at all. Community leaders, public
health officials, and researchers must consider
both the challenges and the richness represented in the extensive body of relevant social science research as they develop community
health-promotion programs.
Much of the task of developing successful
community programs can be pared down to the
use of clear and effective communication with
entire communities, their organizations, and
the families and individuals who reside in them.
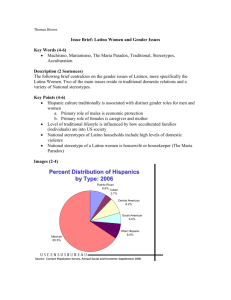
Our conceptual model (see Figure 1) depicts
the role and interaction of various theoretically
driven communication intervention approaches
ANRV370-PU30-13
ARI
15 February 2009
12:38
Behaviors
Diet
Physical activity
Sedentary behavior
Tobacco use
Sleep
Health care utilization
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
Medication use
Complimentary
medicine
Schools and families
Clinics and health care providers
Communities and promotores
Acculturation and cultural influences
Figure 1
A framework for promoting Latino health through communication.
to achieve health and environmental change in
Latino communities. Our model is informed by
Bronfenbrenner’s socioecological framework,
which illustrates the importance of interactions
among various levels of influence from the microsystem to the macrosystem (18). We focus
specifically on the interaction of places and people. Finally, our model reflects our collective
experience working primarily with Mexicans/
Mexican American populations along the U.S.Mexico border (8, 10, 11, 13, 28–33, 64) and
also in the U.S. Southeast region (12, 22, 36,
53, 70, 100, 105), as well as our leadership
and participation in national Latino research efforts (see http://www.redesenaccion.org/ and
http://www.cscc.unc.edu/hchs/).
Health Behavior Theories
In most cases, theories of behavior change grow
out of stable, middle-class societies, in turn
driving the development of psychologically
oriented interventions based on white/Anglo
norms (59). These theories, to a large degree,
emphasize the role of the individual and his/her
thought processes in the development and the
maintenance of adaptive or high-risk healthrelated behaviors. However, the applicability
of these theories to especially first-generation
Latinos outside the dominant mainstream
American culture can be questioned (28).
First, the model of individuals as relatively
autonomous beings, who weigh potential
personal outcomes, their own self-efficacy,
and their personal readiness to change, while
choosing whether to listen to or ignore pressure from peers, may have limited relevance
to more traditional cultures. Instead, Latinos
demonstrate a strong sense of identification
with and attachment to family members, both
nuclear and extended. The typical Latino
with traditional social values is someone who
prioritizes the needs of the group or family over
his or her own (68) and may not be influenced
by messages that target only the individual. For
example, in a study of Latino immigrants (1),
perceived family approval and support more
than autonomous decision making influenced
www.annualreviews.org • Latino Community Health
233
ARI
15 February 2009
12:38
an individual’s decision to participate in a hearthealth-promotion program. This collective
identity must be calculated into the development of health communication targeting
Latinos. Even when mainstream theories are
used (e.g., 97), the design of health messages
must acknowledge this attachment, which promotes loyalty, unity, reciprocity, and solidarity
within the Latino community (93). Second, in
traditional societies, the individual’s approach
to health and illness is often fatalistic (98).
Disease may be seen as an unavoidable crucible
or even as punishment for past sins and health
as a gift from God (79, 98). Because of this fatalistic orientation, Western-style modification
of unhealthy lifestyle behaviors through an
appeal to personal autonomy is less likely to be
successful, as is Western medicine in general
(61, 86).
Recent attempts in model development have
included application of the PEN3 model, which
emphasizes the importance of culture along
three interrelated, interdependent dimensions
of health beliefs and behaviors: health education (person, extended family, neighborhood),
educational diagnosis of health behavior (perceptions, enablers, and nurturers), and cultural
appropriateness of health behavior (positive,
exotic, and negative) (3–6, 48). PEN-3 incorporates socioeconomic factors (e.g., income, education, access to care), cultural beliefs, values,
and attitudes concerning lifestyle behavior and
preventive health practices. Although PEN3
was originally developed for use with African
Americans, investigators have recently applied
it to research with Latinos that explored cultural
factors impacting health behaviors (41) and to
the development of culturally appropriate interventions for cervical cancer (35). However, until
models such as PEN3 and more universally
applicable theories can be developed, established functional models prescriptive of how to
change behavior (rather than how to explain it)
may be more useful to reduce health disparities.
McGuire’s (72) communication-persuasion
model comprises one such functional
approach.
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
234
Elder et al.
The Communication-Persuasion
Model
The communication-persuasion model (72)
considers how various forms of public communication change attitudes and behaviors. The
effectiveness of a given communication effort
will depend on various inputs and their characteristics, as well as on the outputs of interest. Communication input variables applicable
to Latino communities may vary substantially
from those that appeal to the majority population. Input variables include the channel by
which the message is sent, the source of the
message, the message itself, and the characteristics of the audience to whom it is sent. Channel
factors were initially thought to vary primarily
between print (e.g., newspaper, pamphlets) and
interpersonal electronic (radio and television)
media. Source variables focus on characteristics of the individual perceived as sending the
message. Sources vary in terms of the numbers
of people sending the message, their credibility, their physical attractiveness, and characteristics they have in common with the receiver.
Messages themselves vary in their specific appeal (e.g., negative versus positive appeal), the
information they present, what is included and
what is omitted in the message, how the messages are organized, and how frequently they
are repeated. Audience factors include the demographic, behavioral, and sociocultural characteristics of the people at whom the messages
are aimed, as well as their capacity to understand and assimilate the information. Finally,
destination factors refer specifically to the target behaviors the communication is expected to
impact.
How do these variables interact with the
complex social, cultural, and economic factors
that impact the health of Latinos and contribute to the diversity among them? Oetzel
et al. (81) studied the influence of independence
and interdependence, ethnic identity (bicultural, assimilation, traditional, and marginal),
and cultural health attributions (equity and
behavioral-environmental attributions) on
source, message, and channel preferences for
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
receiving breast health information by middleaged or older Latinas. The researchers found
that these three subjective cultural factors
were significantly related to a variety of
audience preferences in terms of source of
communication, channels, and fear messages.
For example, interdependence was positively
associated with preferences for significant
other or family as a source of communication.
This and related studies strongly imply the
need for tailoring health communication and
community interventions for Latinos (67, 119).
The next section presents an articulation of
McGuire’s input variables with special characteristics of Latino communities. Specific attention will be given to (a) the channel through
which the message is communicated; (b) sources
within settings; (c) the message itself, and
(d ) audience factors.
Channels of Communication
Optimal exposure and attention to healthpromotion messages require selection of an appropriate and popular channel for delivering
messages at an appropriate time and place for
the target audience to attend to the message.
Achieving this goal requires a very careful process because mistakes can be costly. The target
audience must not only be exposed to the message, but also attend to it, as well. Health behavior communication is clearly at a disadvantage
in competition with commercial marketing because health messages by nature tend to be less
glamorous and the behavior more complicated
than the simple purchase of a consumer product. When Latinos comprise the target audience, exposing them and getting them to attend to the communication is complicated even
further.
Telephone interventions. Telephone counseling is convenient; inexpensive relative to inperson interventions; reduces the required time
commitment; overcomes geographic isolation;
requires no travel, childcare, or parking; and
can easily be offered in Spanish. Nevertheless, telephone information services using ei-
ther call-in information lines or proactive outreach approaches are largely unexplored for
Latino communities, but seem to demonstrate
some promise. Findings from the Health Information National Trends Survey (HINTS) indicated that Latinos had the highest level of
awareness of the Cancer Information Service
(CIS) language line among all racial and ethnic
subgroups studied (99). Furthermore, Latino
patients who called the CIS language line between 2002 and 2003 were more likely to seek
information about support services, referrals to
medical services, and psychosocial issues and
less likely to request specific treatment information when compared with non-Latinos (99).
Adios al Fumar (Goodbye to Smoking) was designed to increase the reach of the Spanishlanguage smoking cessation counseling service
provided by the National Cancer Institute’s CIS
and to evaluate the efficacy of a telephone-based
culturally adapted, proactive, behavioral treatment program for Spanish-speaking smokers
(116). Participants were of very low socioeconomic status (SES), and more than 90% were
immigrants. After targeted promotion, calls to
the CIS requesting smoking cessation help in
Spanish increased from 0.39 to 17.8 per month,
with a significant impact on smoking prevalence among those who received the culturally adapted counseling compared with callers
receiving standard counseling. This program
demonstrated that it is possible to reach, retain,
and deliver an adequate dose of treatment to a
very-low-SES population that has traditionally
been viewed as difficult to reach and hard to
follow.
Print and mail interventions. The Secretos de
la Buena Vida project was a randomized controlled trial targeting the diets of 357 Latinas
using a tailored communication approach. Randomly sampled and randomly assigned, the
women participated in one of three conditions:
12 weekly visits with a promotora (lay health
advisor) and 12 weekly tailored, mailed information pieces; 12 weekly tailored, mailed information pieces only; or (the control group)
12 generic, mailed information pieces. The
www.annualreviews.org • Latino Community Health
235
ARI
15 February 2009
12:38
content of the tailored print pieces included
culturally relevant behavioral strategies, tips on
how to eat healthier at a restaurant and select
healthy snacks, a lifestyle column addressing
common concerns among Latinas (e.g., time
management, finances), and a novela (story) depicting a family dealing with nutrition-related
changes, as well as inspirational quotes, colorful pictures, and other personalized information. Results at immediate postintervention indicated that the promotora condition achieved
significantly lower levels of total fat grams and
lower levels of energy intake, total saturated fat,
total carbohydrates, glucose, and fructose (30).
At the one-year follow-up, however, immediate changes observed in the promotora condition
did not persist and additional changes were observed in the tailored mailed condition (29).
In a similar fashion, Sauaia et al. (94) compared tailored print and promotora interventions in the Tepeyac Project, a church-based
project to increase breast cancer screening rates
among Latinas in Colorado. Culturally tailored
print education packages were mailed to 209
Colorado Catholic churches and contrasted to
promotoras delivering the information to four
Catholic churches personally. The investigators
compared biennial mammogram claims from
five insurance plans covering these communities over three years and found that, after adjusting for a variety of variables, women exposed to
the promotora intervention had a significantly
higher increase in biennial mammograms than
did women exposed to the print alone. However, the overall differences were modest, especially given the far greater potential reach of a
print intervention.
Fox and colleagues (38) examined the effects of a targeted low-cost mailed intervention
on mammography rates among older women.
Older, diverse, and disadvantaged women have
especially low mammography and other cancer screening rates, often because of financial
constraints. The intervention helped increase
screening rates among all elderly minority
women, and Latinas were more than twice as
likely to undergo screening relative to women
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
236
Elder et al.
in a control condition. Thus, a mailed print intervention can effectively change behavior.
Mass media interventions: special case of
the telenovela. Video interventions, in general, have proven effective at changing Latino
populations’ knowledge, attitudes, and behaviors on poison control (51), cancer screening
(120), and condom use (80). The telenovela, a
Spanish language version of a TV soap opera,
is a popular form of mass entertainment for
many Spanish-speaking households. Wilkin
and colleagues (117) examined whether this
channel would be effective for providing health
information to Spanish-speaking viewers in
the United States if presented in a dramatic,
narrative format. A breast cancer storyline
was developed for the telenovela Ladrón de
Corazones, and its effects on viewers’ knowledge
and behavioral intentions were assessed. The
approach appeared effective. Calls placed to
1-800-4-CANCER increased significantly;
viewers demonstrated significant knowledge
increments as measured through a national
survey, and men who watched the show were
significantly more likely to recommend that
women have a mammogram.
The Tú No Me Conoces (You Don’t Know
Me) social marketing campaign (82) promoted
awareness of HIV risk and testing in Latinos living on the California-Mexico border.
The eight-week campaign included Spanishlanguage radio, print media, a Web site, and a
toll-free HIV-testing referral hotline. Twentyeight percent of individuals who were subsequently tested at partner clinics specifically
identified the Tú No Me Conoces campaign, indicating the potential for the effectiveness of multiple mass media channels for even relatively
high-risk groups.
Given the size and diversity of Latino groups
throughout society, there has been an increasing need to exploit both typical print and broadcast channels, while shrinking the digital divide
and expanding the use of computer-based mass
media (65) for addressing Latino health needs.
This review suggests that interventions that do
ANRV370-PU30-13
ARI
15 February 2009
12:38
not involve face-to-face contact can be efficacious to achieve change.
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
Sources of Communication by Setting
Communities and promotores. Health care
providers may be ignored as message sources if
they are perceived to be unaware of the importance of the patient’s culture or even perceived
as siding with hostile law enforcement. This
barrier can be surmounted by the involvement
of promotores, who come from the communities
they serve and yet are sufficiently acculturated
to the host culture to be able to understand and
appreciate certain health-promotion and health
care messages that need to be communicated to
recent immigrants.
The promotor model is based on the
assumption that every community has formal
and informal social networks through which
health information is exchanged, and predisposing interpersonal environments are created.
Promotores are lay health advisors who generally
have attributes of leadership, compassion, and
familiarity with the community. Interpersonal
communication via promotores addresses the
weaknesses of impersonal mass media, which by
itself may not result in sufficient exposure, attention, or comprehension. Promotores are often
asked to communicate on a face-to-face basis
with Latino patients, reducing the likelihood
of misunderstanding of treatment or healthpromotion communication while increasing
the acceptability of the communication. These
promotores in turn are accessible should patients
need further follow-up regarding a specific issue
or should they need to be referred for additional
treatment. Through the promotor channel, information is provided about the importance of a
medical intervention, how the medical care system operates, eligibility requirements for various health programs, and even how to fill out
forms for participation. Promotores may be adept
at translating the need to alter health practices
that are culturally bound, such as eating
habits.
A recent literature review identified three
primary roles for promotores: health education,
case management, and community outreach
(101). Promotor roles range from information dissemination and health education to policy and community advocacy and negotiating
agency services to providing preventive and curative services (34, 50). In a 1994 report, the
U.S. Centers for Disease Control and Prevention defined promotores as trusted community
members whose role was to provide informal,
community-based, health-related services and
to establish vital links between health providers
and persons in the community (109). Within
these roles, promotores have improved access to
care, various health behaviors and health outcomes, health status, and knowledge; they have
also improved cost-effectiveness. However, important differences between established and
new immigrant–receiving communities seem to
warrant attention in the design of promotor interventions. A systematic review currently underway (111) identified a uniform difference
in the design of promotor-based interventions
in the United States based on where the study is
taking place. Promotor-based interventions in
the Southwest were more likely to train promotores in traditional health education roles,
whereas those in other regions of the country
were more likely to train them to help bridge
health services and other organizational systems (see Figure 2). In these emerging and incipient markets, promotores are needed to serve
as cultural brokers or intermediaries between
these larger predominantly English-speaking
service organizations and clients.
Unfortunately, as alluded to previously, this
interpersonal channel suffers by comparison
with mass media in terms of the scale or reach of
the intervention effort. Promotores may be very
effective but require a lot of professional time
for recruitment, training, and sustainability.
High dropout rates, occasional errors in health
messages, or eventual decay of acquired skills
may all characterize a promotor-led program.
Such risks are prevalent especially if the program is long term, which might require extensive new recruiting and retraining efforts. An
interesting partial solution to the public health
challenge of using promotores has been provided
www.annualreviews.org • Latino Community Health
237
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
Figure 2
Geographic distribution of 47 lay health advisor ( promotores) studies with darker map zones depicting greater concentrations of Latinos
(E = educator versus B = bridge).
by the A Su Salud program in southwestern
Texas (7). Promotores working with A Su Salud
are trained primarily to expose participants to
a health-promotion effort (e.g., smoking cessation, lowering dietary fat) and to gain initial
attention or cue patients to action by disseminating minimal information along with print
material and referring community members to
tune in to mass media messages. The more technical details of the program are then offered
via mass media channels. In this scenario, the
promotores recruit participants to join them in
listening to a particular radio show or television program that will convey the information
needed. After the program is finished, the promotor conducts a discussion group with the participants and follows up with each of them on
their own homework assignments. Using this
approach, promotores can spend more of their
238
Elder et al.
time recruiting an audience and less time training to become risk factor experts.
Clinics and health professionals. A variety
of barriers exist to providing effective medical and preventive care to Latinos, including
a lack of health insurance or a regular source of
health care and a lack of culturally and linguistically proficient clinicians. Limited English proficiency, low education, and low literacy levels can interfere with communications between
Latino patients and the health care system.
Improved provider/patient communication remains one of the biggest potentials for promoting health among Latinos, particularly immigrants (26).
Improvements in communication, however,
may require an extensive reorientation of primary care providers and the health care delivery
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
system. Cooper et al. (24) proposed a modification of the Institute of Medicine framework
to make it relevant to Latinos and other disadvantaged groups. Health disparities could be
reduced with changes in primary care provision, including increased cultural and linguistic competency and more use of community
health workers and/or certified health interpreters, improved access to care (including location, hours of operation, diversity of staff ),
better marketing of services provided, and the
inclusion of the family in care.
Brown et al. (19) put this proposal into action
in a study examining the effects of a culturally
competent diabetes self-management intervention. Two hundred and fifty-six randomly selected persons with type 2 diabetes participated
in an intervention that consisted of 52 contact
hours over 12 months delivered by bilingual
Mexican American nurses, dietitians, and community health workers. The intervention was
composed of weekly community-based instructional sessions on nutrition, self-monitoring of
blood glucose, exercise, and other self-care topics, as well as biweekly support group sessions.
The cultural competence of the program was
evidenced by its language, type of diet, social
emphasis, family participation, and incorporation of cultural health beliefs. As a result, individuals receiving the program showed significantly lower levels of HbA1c and fasting
blood glucose at 6 months and at 12 months. At
6 months, the mean HbA1c of the experimental
subjects was 1.4% below the mean of the control group, which indicated a modest yet important effect.
One example of a comprehensive cliniccentered approach to health promotion is Viva
la Vida (Live Life). Viva la Vida was developed
to improve diabetes care among Latino Medicare beneficiaries in four Southern California
counties. After researching barriers to good
diabetes care among Latino seniors, Olson
(83) designed a multifaceted program targeting
health care providers and Medicare beneficiaries through bilingual, low-literacy, and wellillustrated health education materials and tools,
community and provider partnerships, and the
mass media. Program staff participated in live
interviews on Spanish radio and television stations and placed ads and articles in Spanish
and bilingual community newspapers. Media
messages emphasized the importance of proactive diabetes control and encouraged Latinos
to discuss HbA1c testing with their physicians.
Complementary messages were placed in physician trade magazines. The project succeeded in
helping to reduce the disparity in glycosylated
hemoglobin testing between white and Latino
Medicare beneficiaries in the targeted region
(83).
Schools and families. Sembrando Salud (Sowing the Seeds of Health) entailed the evaluation
of an eight-week tobacco/alcohol use prevention program compared with a first aid/home
safety attention-control condition delivered to
youth and their parents in schools (33, 64). Six
hundred and sixty adolescents and one adult
caregiver per youth were recruited through the
federal Migrant Education Program in Southern California. Random assignment to a condition occurred at the school level in 22 schools.
Seventy 8-week intervention groups (37
tobacco/alcohol, and 33 first aid/home safety)
were conducted by bilingual/bicultural college undergraduates who served as older-toyounger peer educators. No between-group
differences in smoking or drinking following
the intervention were significant: Thirty-day
smoking started and remained at very low levels,
and the highest group prevalence at any measurement period was 4.7% and the lowest was
2.5%. However, those considered susceptible
to smoking dropped by 50% in the intervention condition versus nearly 40% in the attention control, from baseline to the final followup, with a statistically significant reduction at
final follow-up. Of interest was the attentioncontrol participants, who demonstrated significantly higher first aid skills and home safety
practices at posttest: One adolescent apparently responded effectively to an emergency
that threatened the life of a toddler sibling (21).
Treviño et al. (106) studied a school-based
diabetes mellitus prevention program on low
www.annualreviews.org • Latino Community Health
239
ARI
15 February 2009
12:38
income, Mexican American fourth-grade children in San Antonio. The Bienestar Health Program entailed health and physical education
curricula, a family program, a school cafeteria program, and an after-school health club,
all emphasizing a decrease in dietary saturated
fat intake, an increase in dietary fiber intake,
and an increase in physical activity to favorably
impact fasting capillary glucose level, percentage of body fat, physical fitness level, dietary
fiber intake, and dietary saturated fat intake. Although body fat and dietary saturated fat intake
did not differ significantly between intervention
and control children, fasting capillary glucose
levels decreased in intervention schools and
increased in control schools, whereas fitness
scores and dietary fiber intake significantly increased in intervention children and decreased
in control children.
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
The Message
Literacy issues. The U.S. Bureau of Census
has determined that more than 10% of adult
Americans are functionally illiterate in English
(meaning they read at the fourth grade or lower
level), and another 70 million are marginally
illiterate (reading levels between the fifth and
eighth grade) (108). More than half of the minority population in the United States is classified as functionally or marginally illiterate. A
major aspect of the problem of low literacy
in the United States is the fact that most recent immigrants, especially from Latin America, know little or no English upon arrival in the
United States. Their level of the English language is limited to what is required to function
in job training programs, the community, and
the workplace.
Although Guerra & Shea (44) point out that
functional health literacy may not be independently associated with perceived physical health
status or mental health status in ethnic minorities, economic and other vulnerabilities stemming from low literacy may in turn lead to
health problems. For instance, current health
instructional approaches and materials are typ-
240
Elder et al.
ically designed for relatively educated individuals who are highly literate in English. Materials available in Spanish or other non-English
languages are largely direct translations from
English and are often not culturally or even linguistically appropriate. Further, they tend to be
written at a high Spanish (or other language)
readability level, making them inappropriate
for low-level readers in the native languages
(16, 115). Such barriers apply not only to health
education materials (73) but also to instructions that go along with medication prescriptions (115) and even condom use (92). Illiteracy
may negatively affect health through incorrect
use of medication and inability to comply with
medical directions or advice, high rates of accidents, and a lack of access to health information
and services.
Health messages that concurrently promote literacy may comprise the ideal approach
to health communication for immigrants. In
“Language for Health,” Elder and colleagues
(33) wove heart health and stress management information into English as a second language (ESL) courses for recent immigrants.
While these immigrants were learning English,
they were also successful in reducing dietary
fat and, at least for a short time period, improving HDL (total cholesterol levels). Alumni
left these classes with not only improved English but improved health practices as well.
Parra-Medina and colleagues (85) used a similar approach to improve the ability of Latinos
with limited English proficiency to navigate the
U.S. health care system in appropriate, costeffective ways while improving their English
language skills. The Language for Health Care
Access educational intervention was delivered
by trained interventionists in 16 ESL classes;
11 ESL classes served as controls. The intervention was effective in improving levels of knowledge about health care access, appropriate use,
and the availability of language resources. In
comparison to the control group, the intervention also improved levels of self-efficacy related
to both health care access and language (e.g.,
using English to access and utilize services).
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
Language preference. A manifest tenet of
health communication is that messages must be
presented in the language of the audience. Yet
a Pew Hispanic Center survey (87) showed that
50% of all Latinos in the United States consider themselves to be bilingual, whereas 75%
read in both Spanish and English. Thus, appropriate message language cannot be directly
inferred by the literacy or ethnicity of the target audience or its overall acculturation level.
Kelly et al. (52) studied 249 Mexican American
middle-school youth from a U.S.-Mexico border community to examine the effectiveness of
language and theme with respect to print tobacco counter advertisements. Although a large
proportion of the students identified with the
Mexican American culture and spoke Spanish in
selected contexts, readability was greater for ads
in English, which were rated as more effective.
Collectivistic versus individualistic fear
messages. Murray-Johnson and colleagues
(78) studied what they term “individualistic”
and “collectivistic” cultural orientations by ascribing these to African Americans and Mexican
Americans, respectively. Their results suggest
that Mexican American adolescent offspring of
immigrant parents were more heavily influenced by AIDS fear messages that emphasized
harm that could come to the family of an infected person, especially through the loss of
family honor and the shame that would come to
them. African American teens, whom they characterized as relatively individualistic in orientation, were in contrast more susceptible to messages depicting individual harm (e.g., personal
shame and fear of death). Although these results
are not directly attributable to cultural orientation nor to specific behavioral outcomes, they
do suggest that at a minimum the target audience’s family orientation needs to be considered
in designing messages for Latino communities.
Multimedia vicarious learning. Ramirez and
her colleagues (71, 89) designed a unique communication strategy to promote Pap screening
and other cancer control behaviors, using
“diffusion acceleration’’ approaches in the
Texas-Mexico border region. The campaign
included 82 television segments, 67 newspaper
stories, and 48 radio programs featuring local
role models. Salud en Accion was conducted primarily in Spanish; many of the television, radio,
and newspaper messages included stories about
how and why women obtained Pap smears and
other cancer screening services. Role models’
stories were written to highlight how they came
to obtain a Pap smear. Some stories also showed
how husbands and children can help women
make decisions and how to obtain free services.
The campaign also included the participation
of 175 volunteer peer educators, female homemakers who distributed educational leaflets on
a monthly basis. The communication effort
met its goal of increasing cancer control, with a
trend toward slightly more recent adherence in
the experimental community. The proportion
of women in the highest level of Pap smear
adherence showed a relative increase of ∼10%,
whereas the proportion at the lowest level was
reduced by nearly 50%.
The Audience: A Family Focus
Effective health communication leads the target
audience through behavior change once prerequisite perceptual and cognitive factors are
addressed. For most Latino groups, that behavior change will occur in the context of the family. Families (and more globally, other household members) are often the primary sources of
social support. This is true particularly among
new Latino immigrants who may or may not
engage in other social networks within the community, given its immigrant receiving status as
described above. With longer residences in the
United States, however, the structure and nature of this social support may change. An example of changes in nature is seen in the treatment of aging family members; they may be
respected and obeyed in their home country
but are paid less heed over time and as generations progress in the United States. Aging family members may even spend their final years
in a nursing facility rather than with offspring.
Nevertheless, targeting interventions to the
www.annualreviews.org • Latino Community Health
241
ARI
15 February 2009
12:38
entire family acknowledges this longstanding
tradition of family connectedness.
From both ecological and sociological research on families, two themes have emerged
consistently as uniquely important among U.S.
Latinos: respeto and familismo (20, 45, 112). Respeto, or respect, refers to the importance of
teaching younger generations their obligations
for proper levels of courtesy and decorum required in various social contexts with people
of a particular social status, sex, or age (especially respeto a los padres, or respecting one’s parents). Familismo, or familism, refers to “feelings
of loyalty, reciprocity, and solidarity towards
members of the family, as well as the notion of
the family as an extension of self ” (88, p. 249).
This strong sense of family orientation, obligation, and cohesion appears to protect Latinos
against risk behaviors and improve their physical and educational outcomes (15, 23, 27).
Family-based researchers need to consider
the cultural orientation of both the parent
and child and the impact of acculturation on
their relationship. Among immigrant families,
clashes occur between parents and their children because children identify with the host
culture and parents are committed to the ways
of their countries of origin. This divide exacerbates the intergenerational gap in acculturation (23, 37, 102). Potential effects of this intergenerational gap include a family role reversal
(because children have better English language
capacity and are often placed in positions of
authority over parents in family business matters such as translating at the doctor, reading
materials sent home from school, or business
correspondence) and increasing disengagement
and rigidity in parent-child relationships that
previously had been flexible and cohesive
(103, 113).
Health-promotion specialists must also determine the specific roles of each family member and help youth and parents understand one
another as part of any health program or treatment regimen. Adherence to the regimen is
unlikely to occur unless the family trusts the
provider and thinks that his or her recommendations are valuable and important. Such rec-
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
242
Elder et al.
ommendations in the area of health behavior
change may especially call for the involvement
of the family, given that resistance to change
will occur if the targeted health behaviors are
widely accepted in the traditional culture (46).
Finally, despite the importance of involving all family members, recent research highlights the importance of the wife-mother, who
often serves as the primary target of healthpromotion interventions given traditional gender norms and roles. This is normative within
a largely patriarchal society and continues despite an increase in the proportion of women
employed in the labor force. The primary female often carries the brunt of change within
the family, taking the lead in bringing about
behavior change among its members (76).
In one survey on food habits and attitudes,
mothers served as the primary influence on
matters of nutrition and health (63). Research
also indicates that parents’ eating behaviors directly influence the child’s diet (i.e., modeling the appropriate behavior), whereas parent
knowledge and parent self-efficacy indirectly
influence dietary behavior among children (57).
Similarly, targeting the adult woman and addressing how her decisions on diet and physical
activity influence the behaviors of the rest of
her family are consistent with the familial orientation of the Latino culture.
A family-based diabetes program on the
U.S.-Mexico border helps illustrate the integration of these points. In this study, family
members were trained to collectively set healthbehavior goals, to overcome obstacles hindering healthy behaviors, and to develop a plan
to sustain behavior changes (104). The Familias Unidas intervention targeted increases in
protective factors (e.g., familism, parental investment, family cohesion, parent-adolescent
communication, parental monitoring, and positive parenting) and reductions in risk factors
(e.g., family conflict resulting from differential acculturation, and lack of parental monitoring of adolescents, school, and peers). The
intervention was delivered in family-centered,
multiparent groups that involved parents as
agents of change by strengthening their sense of
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
responsibility and perceived control over their
lives and the lives of their children. Intervention
messages for the parents emphasized building
cultural strengths to fortify culturally relevant
protective factors that exist within the individual, family, and community, the importance of
the family, cultural adaptation to American society, the marketing strategies of the alcohol and
tobacco industries, and life issues experienced
within an economically disadvantaged environment. The Familias Unidas approach focused on
the impact of deeply held values and beliefs on
health (23). For example, respeto may engender family harmony. At the same time respeto
may lead parents to view schools and teachers as the authority over their child’s education
and perceive and view parental interventions on
their child’s behalf at school as inappropriate
and overstepping their bounds. This conflicts
with the mainstream American value that parents are important members of the educational
team and with the expectation that they communicate with schools. Thus, part of the intervention approach was in essence to redefine
respeto within the new and less familiar cultural
context.
PART 3: DISCUSSION
We have described a framework for designing
and evaluating health communication and behavior change efforts in this large and diverse
population. Latinos vary substantially on a variety of overlapping and interactive dimensions.
These include their socioeconomic and legal
status, their country of origin or background
and the extent of ongoing contact with that
country, the nature of their receiving community or region of residence, their generation status and levels of acculturation, and psychosocial
and demographic factors such as their experiences of racism or discrimination, familismo,
collectivism, gender, and age-related issues.
In this article we have sought to bridge
the gap between this extensive and rich social and behavioral science research tradition with health communication and related
behavior-change efforts among Latinos resid-
ing in the United States. With reference to
the communication-persuasion model, Table 2
summarizes how these broader social and cultural forces translate into the selection of
health communication channels, sources and
settings, messages and their design, and delimitations of target audiences. Programs presented
in recently published literature are described
in terms of these communication-persuasion
inputs.
Much of the published literature on health
behavior change in Latino communities represents descriptions, program evaluations, or (in
some cases) empirical studies of multicomponent communication efforts. In general, multiple communication channels are employed,
for example, with print materials accompanied
by face-to-face communication or mass media.
Often, more than one source or setting is involved, such as when messages are presented by
both promotoras and providers in homes and also
in clinics. Messages themselves may be multifaceted, combining fear appeals with exhortations to put personal health behavior in the context of family and culture. These combinations
of disparate elements are understandable, given
that many studies describe earnest attempts to
ensure that community programs include all
potentially effective components. Nevertheless,
in tandem they prevent adequate definition of
independent variables.
Without well-specified independent variables, the practice of community health promotion among Latinos cannot be refined, nor can
the empirical heritage be well established. For
example, decade-old calls to close the digital
divide (6) assume that Latinos and other disadvantaged populations continue to have limited
access to the Internet. However, a recent Pew
Hispanic Center report (87) showed that 78%
of Latinos who are English dominant as well as
76% of bilingual Latinos use the Internet. Although only 32% of Spanish-dominant Latino
adults do so as well, this proportion is certain
to increase given the penetration of Internet
communication into society and the proliferation of Spanish-language Web sites. We need
to be prepared for Internet delivery of written,
www.annualreviews.org • Latino Community Health
243
ANRV370-PU30-13
Table 2
ARI
15 February 2009
12:38
Culture of origin issues and implications for communication interventions
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
Channel or medium
Setting
Source
Message
Country/culture of
origin
Mainstream versus
Latin American
TV/radio
programming
Dominant U.S.
celebrations versus
ethnic or cultural
festivals (Dı́a del Niňo,
Fiestas Patrias)
Socioeconomic and legal
status
WIC and community
clinics or emergency
rooms versus regular
providers
Larger community
settings versus
apartment complexes
and trailer parks
(which are more
private social spheres)
Avoidance of use of
government or the
word American (e.g.,
in “ACS”) as source
for communication to
first-generation or
undocumented
immigrants
Where to find health
care; adjusting
health behavior
messages to
economic reality
History of migration in
community (mature,
emerging, incipient)
and acculturation
Mainstream versus
face-face, sotto voce
TV/print versus
Internet and other
new media
Major malls, mobile
consulates, churches
and clinics versus
labor camps, tiendas,
etc.
Community political
leadership versus
religious or welfare
workers (or better yet
promotores)
Messages placed in
context of how one
fits in the broader
community
Culturally competent
care versus
institutional racism
Lawyers, activists,
politicians
Health equals
function of
empowerment,
rights
Developmental or
family specialist versus
an abuela figure
Emphasis on impact
on self versus larger
social group
Discrimination,
perceived racism, and
othering
Familismo, collectivism
Gender and age issues
Equal rights
audio, and video formats, which have typically
been limited to traditional media channels in
this group. Additionally, 59% of Latinos have
cell phones and half of these use text messaging,
indicating further potential for this and other
new media.
Further limitations will then be placed on
linking existing intervention research back to
the Hispanic Health Paradox, acculturation
and generational status, and other broader social science-based themes. Ultimately, modifications in or substitutions for Western health
behavior theories cannot be achieved, leaving
researchers to choose between conceptual systems predicated on research in other populations or no theoretical base at all.
Target audiences are also not well defined
at times. Some studies report only that “Latinos” or “Hispanics” were included without
244
Idiomatic phrasing
tailored to each
sending country’s
culture
Elder et al.
reference to country of origin, and at times
they are among other non-Latino participants.
Generational status and length of time in the
United States and the individual’s relationship
to his/her family and the broader community
are specified even less frequently (9). This inadequate description may be accompanied by
the use of convenience samples and/or nonrandom assignment in a comparison group design
or even a single-group pretest/posttest. A lack
of specification of audience/population factors
and a reliance on nonexperimental evaluations
limit the generalizability of existing findings.
These challenges face us even as the ground
shifts rapidly beneath. America’s current demographic changes are the most pronounced
in more than a century. Latinos both define
and are defined by these changes, as is their
health. For example, as the debate continues
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
regarding the validity of the concept of the
Hispanic Health Paradox, the once-apparent
health advantage of Latino ethnicity in the
United States may be diminishing, even as
risks for chronic diseases accelerate rapidly in
Mexico and other sending countries. Although
many Latin American immigrants may live in
isolated communities, most are increasingly exposed to diversity. Latinos of different generations and national backgrounds intermarry, and
youth of mixed Latino and other backgrounds
can be expected to join many in their age cohorts in self-identifying as multiracial. At the
same time, language, mass media, entertainment, religion, food preference, and other fundamental cultural characteristics have an increasingly Latin American look to them in the
United States, altering the very nature of the
acculturative impetus.
Almost accepted as truisms for health communication with Latinos is the need to focus
on family, cultural traditions, and collectivism
while attending to acculturation, language, and
generation status and national origin. The most
extensive intervention research topic in Latino
community health has been the application of
the promotor model. Yet even this area needs far
more empirical treatment, as Rhodes and colleagues (91) note in their extensive review of the
use of promotoras [which they label lay health
advisors (LHAs)],
Given the long history of using LHAs as
an approach to health promotion . . . and
the current emphasis of LHA approaches
as a potential solution to health dispari-
ties . . . Latinos/Hispanics in particular, few
rigorous studies have been published that document the effectiveness of LHAs on a variety
of public health concerns. A stronger empirical evidence base is clearly needed. (p. 418)
This lack of empirical documentation of
effective community health-promotion efforts
will continue to challenge researchers and policy makers alike in the coming years and
decades. Such research, however, must be situated in the context of broader social change
efforts to promote education and reduce discrimination, which can also promote individual
health. Although these broader forces do not require experimental evaluation, they inform relevant communication both to the Latino community and to society as a whole.
IMPLICATIONS FOR PRACTICE
Community health-promotion practitioners
working with Latino communities must start
with a thorough knowledge of their audience,
e.g., the sociocultural, economic, linguistic, and
other characteristics of the members of that
community. Specific variables to which practitioners should attend include country of origin,
generation and acculturation, socioeconomic
and legal status, and the interaction between the
broader community or region and the Latino
population. Whether programs are borrowed
from elsewhere or developed from the ground
up, this information will guide the selection of
channels, messages, sources, and settings as well
as the implementation of such programs and
will help circumvent the one-size-fits-all pitfall.
DISCLOSURE STATEMENT
The authors are not aware of any biases that might be perceived as affecting the objectivity of this
review.
ACKNOWLEDGMENTS
The authors thank Katherine Stewart for her extensive contributions to processing this manuscript
and current and former colleagues Amelie Ramirez, Nadia Campbell, Jeanette Candelaria, Elva
Arredondo, Jo Anne Earp, Eugenia Eng, and Deanne K.H. Messias for their contributions to our
research program.
www.annualreviews.org • Latino Community Health
245
ANRV370-PU30-13
ARI
15 February 2009
12:38
LITERATURE CITED
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
1. Apodaca X, Woodruff SI, Candelaria J, Elder JP, Zlot A. 1997. Hispanic health program participant and
nonparticipant characteristics. Am. J. Health Behav. 21(5):356–63
2. Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. 1999. The Latino mortality paradox: a
test of the “salmon bias” and healthy migrant hypotheses. Am. J. Public Health 89(10):1543–48
3. Airhihenbuwa CO. 1995. Health and Culture: Beyond the Western Paradigm. Thousand Oaks, CA: Sage.
152 pp.
4. Airhihenbuwa CO, Kumanyika SK, TenHave TR, Morssink CB. 2000. Cultural identity and health
lifestyles among African Americans: a new direction for health intervention research? Ethn. Dis.
10(2):148–64
5. Airhihenbuwa CO, Obregon R. 2000a. A critical assessment of theories/models used in health communication for HIV/AIDS. J. Health Commun. 5(Suppl.):5–15
6. Airhihenbuwa CO, Obregon R. 2000b. Toward a new communications framework for HIV/AIDS.
J. Health Commun. 5(Suppl.):101–11
7. Amezcua C, McAlister AL, Ramirez A, Espinoza R. 1990. A Su Salud: health promotion in a MexicanAmerican border community. In Health Promotion at the Community Level, ed. N Bracht, pp. 257–77.
Newbury Park, CA: Sage
8. Arredondo EM, Elder JP, Ayala GX, Campbell N, Baquero B, Duerksen S. 2006. Is parenting style related
to children’s healthy eating and physical activity in Latino families? Health Educ. Res. 21(6):862–71
9. Ayala GX, Baquero B, Klinger S. 2008. A systematic review of the relationship between acculturation and
diet among Latinos in the United States: implications for future research. J. Am. Diet. Assoc. 108(8):1330–
44
10. Ayala GX, Elder JP, Campbell NR, Slymen DJ, Roy N, et al. 2004. Correlates of body mass index and
waist-to-hip ratio among Mexican women in the United States: implications for intervention development. Women’s Health Issues 14(5):155–64
11. Ayala GX, Mueller K, Lopez-Madurga E, Campbell NR, Elder JP. 2005. Restaurant and food shopping
selections among Latinas in Southern California. J. Am. Diet. Assoc. 105:38–45
12. Ayala GX, Ornelas I, Rhodes SD, Amell J, Dodds J, et al. 2008. Determinants of dietary intake among
men involved in the MAN for Health study. Am. J. Public Health. In press
13. Ayala GX, Rogers M, Arredondo E, Campbell NR, Baquero B, et al. 2008. Away-from-home food intake
and risk for obesity: examining the influence of context. Obes. Res. 16(5):1002–8
14. Berry J. 2003. Conceptual approaches to acculturation. In Acculturation: Advances in Theory, Measurement,
and Applied Research, ed. K Chun, PB Organista, G Marin, pp. 17–37. Washington, DC: Am. Psychol.
Assoc.
15. Bird HR, Canino GJ, Davies M, Zhang H, Ramirez R, Lahey BB. 2001. Prevalence and correlates of
antisocial behaviors among three ethnic groups. J. Abnorm. Child Psychol. 29(6):465–78
16. Boyd M, Feldman R. 1984. Health information seeking and reading and comprehension abilities of
cardiac rehab patients. J. Cardiac Rehab. 4:343–47
17. Brondolo E, Rieppi R, Kelly KP, Gerin W. 2003. Perceived racism and blood pressure: a review of the
literature and conceptual and methodological critique. Ann. Behav. Med. 25:55–65
18. Bronfenbrenner U. 1979. The Ecology of Human Development: Experiments by Nature and Design.
Cambridge, MA: Harvard Univ. Press
19. Brown SA, Garcia AA, Kouzekanani K, Hanis CL. 2002. Culturally competent diabetes self-management
education for Mexican Americans: the Starr County border health initiative. Diabetes Care 25(2):259–68
20. Buriel R, Hurtado-Ortiz MT. 2000. Child care practices and preferences of native-and foreign-born
Latina mothers and Euro-American mothers. Hispanic J. Behav. Sci. 22(3):314–31
21. Campbell NR, Ayala GX, Litrownik AJ, Slymen DJ, Zavala F, Elder JP. 2001. Evaluation of a first
aid/home safety program for Hispanic migrant adolescents. Am. J. Prev. Med. 20(4):258–65
22. Cherrington A, Ayala GX, Sleath B, Corbie-Smith G. 2006. Examining knowledge, attitudes and beliefs
about depression among Latino adults with Type II Diabetes. Diabetes Educ. 32(4):603–13
23. Coatsworth JD, Pantin H, Szapocznik J. 2002. Familias Unidas: a family-centered ecodevelopmental
intervention to reduce risk for conduct problems and substance use among Hispanic adolescents. Clin.
Child Fam. Psychol. Rev. 5:113–32
246
Elder et al.
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
24. Cooper LA, Hill MN, Powe NR. 2002. Designing and evaluating interventions to eliminate racial and
ethnic disparities in health care. J. Gen. Intern. Med. 17(6):477–86
25. Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. 2007. Hispanic paradox in biological risk
profiles. Am. J. Public Health 97(7):1305–10
26. Davidson JA, Moreno PR, Badimon JJ, Lopez-Candalas A, Maisonet Giachello AL, et al. 2007. Cardiovascular disease prevention and care in Latino and Hispanic subjects. Endocr. Pract. 13(1):77–85 (Abstr.)
27. Dumka LE, Roosa MW, Jackson KM. 1997. Risk, conflict, mothers’ parenting, and children’s adjustment
in low-income, Mexican immigrant, and Mexican American families. J. Marriage Fam. 59(2):309–23
28. Elder JP, Apodaca JX, Parra-Medina D, Zuniga de Nuncio ML. 1998. Strategies for health education:
theoretical models. See Ref. 66, pp. 567–86
29. Elder JP, Ayala GX, Campbell NR, Arredondo EM, Slymen DJ, et al. 2006. Long-term effects of a
communication intervention for Spanish-Dominant Latinas. Am. J. Prev. Med. 31(2):159–66
30. Elder JP, Ayala GX, Campbell NR, Slymen D, Lopez-Madurga ET, et al. 2005. Interpersonal and print
nutrition communication for a Latino population. Health Psychol. 24(1):49–57
31. Elder JP, Campbell NR, Candelaria JI, Talavera GA, Mayer JA, et al. 1998. Project Salsa: development
and institutionalization of a nutritional health promotion project in a Latino community. Am. J. Health
Promotion 12(6):391–401
32. Elder JP, Campbell NR, Litrownik AJ, Ayala GX, Slymen DJ, et al. 2000. Predictors of cigarette and
alcohol susceptibility and use among Hispanic migrant adolescents. Prev. Med. 31:115–23
33. Elder JP, Candelaria JI, Woodruff SI, Criqui MH, Talavera GA, Rupp JW. 2000. Results of language
for health: cardiovascular disease nutrition education for Latino English-as-a-second-language students.
Health Educ. Behav. 27(1):50–63
34. Eng E, Parker E, Harlan C. 1997. Lay health advisor intervention strategies: a continuum from natural
helping to paraprofessional helping. Health Educ. Behav. 24(4):413–17
35. Erwin DO, Johnson VA, Trevino M, Duke K, Feliciano L, Jandorf L. 2007. A comparison of African
American and Latina social networks as indicators for culturally tailoring a breast and cervical cancer
education intervention. Cancer 109(Suppl.):368–77
36. Evenson K, Sarmiento O, Ayala GX. 2004. Acculturation and physical activity among North Carolina
Latina immigrants. Soc. Sci. Med. 59(2):2509–22
37. Félix-Ortiz M, Fernandez A, Newcomb M. 1998. The role of intergenerational discrepancy of cultural
orientation in drug use among Latina adolescents. Subst. Use Misuse 33(4):967–94
38. Fox SA, Stein JA, Sockloskie RJ, Ory MG. 2001. Targeted mailed materials and the Medicare beneficiary:
increasing mammogram screening among the elderly. Am. J. Public Health 91:55–61
39. Franzini L, Ribble JC, Keddie AM. 2001. Understanding the Hispanic paradox. Ethn. Dis. 11(3):496–518
40. Fuentes-Afflick E, Hessol NA, Perez-Stable EJ. 1999. Testing the epidemiologic paradox of low birth
weight in Latinos. Arch. Pediatr. Adolesc. Med. 153(2):147–53
41. Garces IC, Scarinci IC, Harrison L. 2006. An examination of sociocultural factors associated with health
and health care seeking among Latina immigrants. J. Immigrant Health 8:377–85
42. Goldman N, Kimbro RT, Turra CM, Pebley AR. 2006. Socioeconomic gradients in health for white and
Mexican-origin populations. Am. J. Public Health 96(12):2186–93
43. Grove NJ, Zwi AB. 2006. Our health and theirs: forced migration, othering, and public health. Soc. Sci.
Med. 62(8):1931–42
44. Guerra CE, Shea JA. 2007. Health literacy and perceived health status in Latinos and African Americans.
Ethn. Dis. 17(2):305–12 (Abstr.)
45. Harwood R, Leyendecker B, Carlson V, Asencio M, Miller A. 2002. Parenting among Latino families in
the U.S. In Handbook of Parenting: Social Conditions and Applied Parenting, ed. MH Bornstein, pp. 21–46.
Mahwah, NJ: Lawrence Erlbaum
46. Horowitz C. 1998. The role of the family and the community in the clinical setting. See Ref. 66,
pp. 163–82
47. Hunt KJ, Resendez RG, Williams K, Haffner SM, Stern MP, Hazuda HP. 2003. All-cause and cardiovascular mortality among Mexican-American and Non-Hispanic White older participants in the San
Antonio Heart Study—evidence against the “Hispanic Paradox.” Am. J. Epidemiol. 158(11):1048–57
www.annualreviews.org • Latino Community Health
247
ARI
15 February 2009
12:38
48. Jack LJ, Airhihenbuwa CO, Murphy F, Thompson-Reid P, Wheatley B, Dickson-Smith J. 1993. Cancer
among low-income African-Americans: implications for culture and community-based health promotion.
Wellness Perspect. 9(4):57–68
49. Johnson J, Sleath B, Ayala GX, Dardess M. 2006. A demographic profile of U.S. Hispanic markets. Rep.
Glaxo-Smith-Kline, Univ. N. C., Chapel Hill
50. Kahssay H, Taylor ME, Berman PA. 1998. Community Health Workers: The Way Forward. Geneva: World
Health Organ.
51. Kelly KJ, Stanley LR, Comello ML, Gonzalez GR. 2006. Tobacco counter-advertisements aimed at
bicultural Mexican American youth: the impact of language and theme. J. Health Commun. 11(5):455–76
52. Kelly NR, Huffman LC, Mendoza FS, Robinson RN. 2003. Effects of a videotape to increase use of
poison control centers by low-income and Spanish-speaking families: a randomized, controlled trial.
Pediatrics 111(1):21–26
53. Kepka D, Ayala GX, Cherrington A. 2007. Do immigrant Latinos link self-rated health with BMI and
health behaviors? Am. J. Health Behav. 31:535–44
54. Keppel KG. 2007. Ten largest racial and ethnic health disparities in the United States based on Healthy
People 2010 objectives. Am. J. Epidemiol. 166:97–103
55. Keppel KG, Pamuk E, Lynch J, Carter-Pokras O, Insun K, et al. 2005. Methodological issues in measuring
health disparities. Vital Health Stat. 2(141):1–16
56. Kochhar R. 2005. Latino Labor Report 2004: more jobs for new immigrants but at lower wages. Rep.
Pew Hisp. Cent. http://pewhispanic.org/reports/report.php?ReportID=45
57. Kratt PP, Reynolds KD, Shewchuk JM. 1998. Modeling family influence on the dietary intake of fourth
graders. Presented at Annu. Meet. Soc. Behav. Med., New Orleans
58. Krieger N. 2000. Discrimination and health. In Social Epidemiology, ed. LF Berkman, I Kawachi,
pp. 36–75. Oxford: Oxford Univ. Press
59. Krumeich A, Weijts W, Reddy P, Meijer-Weitz A. 2001. The benefits of anthropological approaches for
health promotion research and practice. Health Educ. Res. 16(2):121–30
60. Lara M, Gamboa C, Kahramanian MI, Morales LS, Hayes-Bautista DE. 2005. Acculturation and Latino
health in the United States: a review of the literature and its sociopolitical context. Annu. Rev. Public
Health 26(1):367–97
61. Latham CL, Calvillo E. 2007. A health protection model for Hispanic adults with type 2 diabetes.
J. Clin. Nurs. 16(7B):186–96
62. Liao Y, Cooper FRS, Cao G, Kaufman JS, Long AE, McGee DL. 1997. Mortality from coronary
heart disease and cardiovascular disease among adult U.S. Hispanics: findings from the National Health
Interview Survey (1986 to 1994). J. Am. Coll. Cardiol. 30(5):1200–5
63. Litman TJ. 1974. The family as the basic unit in health and medical care: a social-behavioral overview.
Soc. Sci. Med. 8:495–519
64. Litrownik AJ, Elder JP, Campbell NR, Ayala GX, Slymen DJ, et al. 2000. Evaluation of a tobacco and
alcohol use prevention program for Hispanic migrant adolescents: promoting the protective factor of
parent-child communication. Prev. Med. 31:124–33
65. Lorence DP, Park H, Fox S. 2006. Racial disparities in health information access: resilience of the digital
divide. J. Med. Syst. 30(4):241–49
66. Loue S, ed. 1998. Handbook of Immigrant Health. New York: Plenum
67. Marı́n G. 1996. Perceptions by Hispanics of channels and sources of health messages regarding cigarette
smoking. Tob. Control 5(1):30–36
68. Marı́n G, Triandis HC. 1985. Allocentrism as an important characteristic of the behavior of L.A. &
Latinos. In Cross-Cultural and National Studies of Social Psychology, ed. R Diaz-Guerrero, pp. 85–104.
Amsterdam: North Holl.
69. Markides KS, Coreil J. 1986. The health of Hispanics in the southwestern United States: an epidemiologic
paradox. Public Health Rep. 101:253–65
70. Mayo R, Parra-Medina DM, Messias D, Rhoades D. 2003. SC partnership for cancer prevention results
from formative research with Latina women at risk for cervical cancer. J. Cancer Educ. 18(3):35–36
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
248
Elder et al.
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
ARI
15 February 2009
12:38
71. McAlister AL, Fernandez-Esquer ME, Ramirez AG, Trevino F, Gallion KJ, et al. 1995. Community
level cancer control in a Texas barrio: part II-base-line and preliminary outcome findings. J. Natl. Cancer
Inst. Monogr. 18:123–26
72. McGuire WJ. 1989. Theoretical foundations of campaigns. In Public Communication Campaigns, ed. RE
Rice, CK Atkin, pp. 43–65. Newbury Park: Sage
73. Mead C, Byrd J, Lee M. 1989. Improving patient comprehension of literature on smoking. Am. J. Public
Health 79:1411–12
74. Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. 2005. State of disparities in cardiovascular
health in the United States. Circulation 111(10):1233–41
75. Modiano MR, Villar-Werstler P, Meister J, Figueroa-Vallés N. 1995. Cancer in Hispanics: issues of
concern. J. Natl. Cancer Inst. Monogr. 18:35–39
76. Moore J. 1994. The social fabric of the Hispanic community since 1965. In Hispanic Catholic Culture in
the U.S.: Issues and Concerns, ed. JP Dolan, AF Deck, pp. 6–49. Notre Dame, IN: Univ. Notre Dame
Press
77. Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. 2002. Socioeconomic, cultural, and behavioral
factors affecting Hispanic health outcomes. J. Health Care Poor Underserved 13(4):477–503
78. Murray-Johnson L, Whitte K, Liu W, Hubbell AP, Sampson J, Morrison K. 2001. Addressing cultural
orientations in fear appeals: promoting AIDS—protective behaviors among Mexican immigrant and
African American adolescents and American and Taiwanese college students. J. Health Commun. 6:335–
58
79. Neff AJ, Hoppe SK. 1995. Race/ethnicity, acculturation and psychological distress: fatalism and religiosity
as cultural resources. J. Comm. Psychol. 21:3–20
80. O’Donnell L, Sandoval A, Duran R, O’Donnell C. 1995. The effectiveness of video-based interventions
in promoting condom acquisition among STD clinic patients. Sex. Transm. Dis. 22(2):97–103
81. Oetzel J, De Vargas F, Ginossar T, Sanchez C. 2007. Hispanic women’s preferences for breast health
information: subjective cultural influence on source, message, and channel. Health Commun. 21(3):223–33
(Abstr.)
82. Olshefsky AM, Zive MM, Scolari R, Zuñiga M. 2007. Promoting HIV risk awareness and testing in
Latinos living on the U.S.-Mexico Border: The Tú No Me Conoces Social Marketing Campaign. AIDS
Educ. Prev. 19(5):422–35
83. Olson R, Sabogal F, Perez A. 2008. Viva La Vida: helping Latino medicare beneficiaries with diabetes
live their lives to the fullest. Am. J. Public Health 98(2):205–8
84. Palloni A, Morenoff JD. 2001. Interpreting the paradoxical in the Hispanic paradox: demographic and
epidemiologic approaches. Ann. N. Y. Acad. Sci. 954:140–74
85. Parra-Medina DM, Wilcox S, Thompson-Robinson M, Sargent R, Will JC. 2004. A replicable process
for redesigning ethnically relevant educational materials. J. Womens Health 13(5):579–88
86. Pepitone A. 1995. Foreword. In Spirit Versus Scalpel, ed. LL Adler, BR Mukherji, pp. xiii–xiv. London:
Bergin & Garvey
87. Pew Hispanic Cent. 2008. Statistical portrait of Hispanics in the United States, 2006. http://
pewhispanic.org/files/reports/.pdf
88. Portes A. 1995. Segmented assimilation among new immigrant youth: a conceptual framework. In
California’s Immigrant Children: Theory, Research, and Implications for Educational Policy, ed. RG Rumbaut,
WA Cornelius, pp. 71–76. San Diego: Cent. U.S.-Mex. Stud., Univ. Ca.
89. Ramirez AG, McAlister A, Gallion KJ, Ramirez V, Garza IR, et al. 1995. Community level cancer control
in a Texas barrio: Part I—Theoretical basis, implementation, and process evaluation. J. Natl. Cancer Inst.
Monogr. (18):117–22
90. Ramirez RR, de la Cruz P. 2003. The Hispanic population in the United States: March 2002, current
population reports. U.S. GPO. Rep. 20–545, Washington, DC. http://factfinder.census.gov/
91. Rhodes SD, Foley KL, Zometa CS, Bloom FR. 2007. Lay health advisor interventions among Hispanics/
Latinos: a qualitative systematic review. Am. J. Prev. Med. 33(5):418–27
92. Richwald G, Wamsley M, Coulson A, Morisky D. 1988. Are condom instructions readable? Results of
the Readability Study. Public Health Rep. 103:355–63
www.annualreviews.org • Latino Community Health
249
ARI
15 February 2009
12:38
93. Sabogal R, Marı́n G, Otero-Sabogal R, Marı́n BV, Pérez-Stable EJ. 1987. Latino familism and acculturation: What changes and what doesn’t? Latino J. Behav. Sci. 9:397–412
94. Sauaia A, Min S, Lack D, Apodaca C, Osuna D, Stowe A, et al. 2007. Church-based breast cancer
screening education: impact of two approaches on Latinas enrolled in public and private health insurance
plans. Prev. Chronic Dis. 4(4):1–10
95. Schneider KT, Hitlan RT, Radhakrishnan P. 2000. An examination of the nature and correlates of ethnic
harassment experiences in multiple contexts. J. Appl. Soc. Psychol. 85:3–12
96. Smedley BD, Stith AY, Nelson AR. 2002. Unequal Treatment: Confronting Racial and Ethnic Disparities in
Health Care. Washington, DC: Natl. Acad. Press
97. Smith C, Ryan A. 2006. Change for Life/Cambia Tu Vida: a health promotion program based on the
stages of change model for African descendent and Latino adults in New Hampshire. Prev. Chronic Dis.
3(3):A105–21
98. Spector RE. 1991. Cultural Diversity in Health and Illness. East Norwalk, CT: Appleton & Lange.
490 pp. 2nd ed.
99. Squiers L, Finney-Rutten LJ, Treiman K, Bright MA, Hesse B. 2005. Cancer patients’ information needs
across the cancer care continuum: evidence from the cancer information service. J. Health Commun.
10:15-34
100. Streng JM, Rhodes S, Ayala GX, Eng E, Arceo R, Phipps S. 2004. Realidad Latina: Latino adolescents,
their school, and a university use photovoice to examine and address the influence of immigration.
J. Interprof. Care 18(4):403–15
101. Swider SM. 2002. Outcome effectiveness of community health workers: an integrative literature review.
Public Health Nurs. 19(1):11–20
102. Szapocznik J, Kurtines W. 1980. Acculturation, biculturalism and adjustment among Cuban Americans.
In Acculturation: Theory, Models, and Some New Findings, ed. A Padilla, pp. 139–59. Boulder, CO: Praeger
103. Szapocznik J, Williams RA. 2000. Brief strategic family therapy: twenty-five years of interplay among
theory, research and practice in adolescent behavior problems and drug abuse. Clin. Child Fam. Psychol.
Rev. 3(2):117–34
104. Teufel-Shone NI, Drummond R, Rawiel U. 2005. Developing and adapting a family-based diabetes
program at the U.S.-Mexico border. Prev. Chronic Dis. 2(1):1–9
105. Torres M, Parra-Medina D, Bellinger J, Johnson A, Probst JC. 2008. Rural hospitals and Spanish speaking
patients with limited English proficiency. J. Healthc. Manag. 53(2):107–19; discussion 119–20
106. Treviño RP, Yin Z, Hernandez A, Hale DE, Garcia OA, Mobley C. 2004. Impact of the Bienestar schoolbased diabetes mellitus prevention program on fasting capillary glucose levels: a randomized controlled
trial. Arch. Pediatr. Adolesc. Med. 158(9):911–17
107. Turra CM, Goldman N. 2007. Socioeconomic differences in mortality among U.S. adults: insight into
the Hispanic paradox. J. Gerontol. 62B(3):S184–92
108. U.S. Census Bur. 2005. Summary of social, economic, and housing characteristics. Rep. U.S. GPO,
Washington, DC. http://factfinder.census.gov/
109. U.S. Dep. Health Hum. Serv. (USDHHS). 1994. Community Health Advisors: Models, Research, and Practice.
Atlanta, GA: USDHHS, Public Health Serv., Cent. Dis. Control Prev.
110. U.S. Dep. Health Hum. Serv. (USDHHS). 2000. Healthy People 2010: understanding and improving health.
http://www.healthypeople.gov/Document/tableofcontents.htm
111. Vaz L, Stoimenoff K, Ayala GX. 2003. Lay health advisors in Latino communities: A systematic review of the
evidence. Am. Public Health Assoc. Conf., San Francisco, CA
112. Vega WA. 1990. Hispanic families in the 1980s: a decade of research. J. Marriage Fam. 52:1015–24
113. Vega WA, Gil AG, Warheit GJ, Zimmerman RS, Apospori E. 1993. Acculturation and delinquent
behavior among Cuban American adolescents: toward an empirical model. Am. J. Community Psychol.
21(1):113–25
114. Viruell-Fuentes E. 2007. Beyond acculturation: immigration, discrimination, and health research among
Mexicans in the United States. Soc. Sci. Med. 65:1524–35
115. Vivian A, Robertson E. 1980. Readability of patient education materials. Clin. Ther. 3:129–36
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
ANRV370-PU30-13
250
Elder et al.
ANRV370-PU30-13
ARI
15 February 2009
12:38
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
116. Wetter DW, Mazas C, Daza P, Nguyen L, Fouladi RT, et al. 2007. Reaching and treating
Spanish-speaking smokers through the National Cancer Institute’s cancer information service. Cancer
109(Suppl.):406–13
117. Wilkin HA, Valente TW, Murphy S, Cody MJ, Huang G, et al. 2007. Does entertainment education
work with Latinos in the United States? Identification and the effects of a telenovela breast cancer
storyline. Health Commun. 21(3):223–33
118. Williams DR, Collins C. 1995. U.S. socioeconomic and racial differences in health: patterns and explanations. Annu. Rev. Sociol. 21:349–86
119. Yancey AK, Ortega AN, Kumanyika SK. 2006. Effective recruitment and retention of minority research
participants. Annu. Rev. Public Health 27:1–28
120. Yancey AK, Tanjasiri SP, Klein M, Tunder J. 1995. Increased cancer screening behavior in women of
color by culturally sensitive video exposure. Prev. Med. 24:142–48
www.annualreviews.org • Latino Community Health
251
AR370-FM
ARI
15 February 2009
12:5
Annual Review of
Public Health
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
Contents
Volume 30, 2009
Epidemiology and Biostatistics
Adaptive Designs for Randomized Trials in Public Health
C. Hendricks Brown, Thomas R. Ten Have, Booil Jo, Getachew Dagne,
Peter A. Wyman, Bengt Muthén, and Robert D. Gibbons p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 1
Social Epidemiology. Social Determinants of Health in the United
States: Are We Losing Ground?
Lisa F. Berkman p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p27
The Behavioral Risk Factors Surveillance System: Past, Present,
and Future
Ali H. Mokdad p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p43
Geographic Life Environments and Coronary Heart Disease:
A Literature Review, Theoretical Contributions, Methodological
Updates, and a Research Agenda
Basile Chaix p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p81
Health Effects of Arsenic and Chromium in Drinking Water:
Recent Human Findings
Allan H. Smith and Craig M. Steinmaus p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 107
Evidence-Based Public Health: A Fundamental Concept for Public
Health Practice
Ross C. Brownson, Jonathan E. Fielding, and Christopher M. Maylahn p p p p p p p p p p p p p p p p 175
Prioritizing Clinical Preventive Services: A Review and Framework
with Implications for Community Preventive Services
Michael Maciosek, Ashley B. Coffield, Nichol M. Edwards, Thomas J. Flottemesch,
and Leif I. Solberg p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 341
Environmental and Occupational Health
Gene by Environment Interaction in Asthma
Stephanie J. London and Isabelle Romieu p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p55
ix
AR370-FM
ARI
15 February 2009
12:5
Geographic Life Environments and Coronary Heart Disease:
A Literature Review, Theoretical Contributions, Methodological
Updates, and a Research Agenda
Basile Chaix p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p81
Health Effects of Arsenic and Chromium in Drinking Water: Recent
Human Findings
Allan H. Smith and Craig M. Steinmaus p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 107
Health Effects of Combat: A Life-Course Perspective
Barry S. Levy and Victor W. Sidel p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 123
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
Potential Health Impact of Nanoparticles
Tian Xia, Ning Li, and Andre E. Nel p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 137
Public Health Practice
Diffusion Theory and Knowledge Dissemination, Utilization,
and Integration in Public Health
Lawrence W. Green, Judith M. Ottoson, César Garcı́a, and Robert A. Hiatt p p p p p p p p p p p 151
Evidence-Based Public Health: A Fundamental Concept for Public
Health Practice
Ross C. Brownson, Jonathan E. Fielding, and Christopher M. Maylahn p p p p p p p p p p p p p p p p 175
Public Health Certification
Kristine M. Gebbie p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 203
Health Communication in the Latino Community:
Issues and Approaches
John P. Elder, Guadalupe X. Ayala, Deborah Parra-Medina,
and Gregory A. Talavera p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 227
The Delivery of Public Health Interventions via the Internet:
Actualizing Their Potential
Gary G. Bennett and Russell E. Glasgow p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 273
Social Environment and Behavior
A Crisis in the Marketplace: How Food Marketing Contributes
to Childhood Obesity and What Can Be Done
Jennifer L. Harris, Jennifer L. Pomeranz, Tim Lobstein, and Kelly D. Brownell p p p p p p 211
Health Communication in the Latino Community:
Issues and Approaches
John P. Elder, Guadalupe X. Ayala, Deborah Parra-Medina,
and Gregory A. Talavera p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 227
School-Based Interventions for Health Promotion and Weight
Control: Not Just Waiting on the World to Change
D.L. Katz p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 253
x
Contents
AR370-FM
ARI
15 February 2009
12:5
The Delivery of Public Health Interventions via the Internet:
Actualizing Their Potential
Gary G. Bennett and Russell E. Glasgow p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 273
Social Epidemiology. Social Determinants of Health in the United
States: Are We Losing Ground?
Lisa F. Berkman p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p27
Annu. Rev. Public. Health. 2009.30:227-251. Downloaded from www.annualreviews.org
by University of Illinois - Chicago on 10/16/13. For personal use only.
The Behavioral Risk Factors Surveillance System: Past, Present,
and Future
Ali H. Mokdad p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p43
Diffusion Theory and Knowledge Dissemination, Utilization,
and Integration in Public Health
Lawrence W. Green, Judith M. Ottoson, César Garcı́a, and Robert A. Hiatt p p p p p p p p p p p 151
Health Services
Cost-Sharing: A Blunt Instrument
Dahlia K. Remler and Jessica Greene p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 293
Extreme Makeover: Transformation of the Veterans Health Care System
Kenneth W. Kizer and R. Adams Dudley p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 313
Prioritizing Clinical Preventive Services: A Review and Framework
with Implications for Community Preventive Services
Michael V. Maciosek, Ashley B. Coffield, Nichol M. Edwards,
Thomas J. Flottemesch, and Leif I. Solberg p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 341
Quality-Based Financial Incentives in Health Care: Can We Improve
Quality by Paying For It?
Douglas A. Conrad and Lisa Perry p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 357
The Contribution of Hospitals and Health Care Systems
to Community Health
Stephen M. Shortell, Pamela K. Washington, and Raymond J. Baxter p p p p p p p p p p p p p p p p p p 373
Untangling Practice Redesign from Disease Management:
How Do We Best Care for the Chronically Ill?
Katie Coleman, Soeren Mattke, Patrick J. Perrault, and Edward H. Wagner p p p p p p p p p p 385
Indexes
Cumulative Index of Contributing Authors, Volumes 21–30 p p p p p p p p p p p p p p p p p p p p p p p p p p p 409
Cumulative Index of Chapter Titles, Volumes 21–30 p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p 414
Errata
An online log of corrections to Annual Review of Public Health chapters may be found
at http://publhealth.annualreviews.org/
Contents
xi